Abstract
Importance
The United States is experiencing an opioid abuse epidemic. Opioid overprescription by physicians may contribute to this epidemic.
Objectives
To determine if there was a correlation between a postoperative patient’s 24-hour predischarge opioid use and the amount of opioids prescribed at hospital discharge and to determine the number of patients who used no opioids prior to discharge but were still prescribed opioids after hospital discharge.
Design, Setting, and Participants
This cross-sectional study performed a retrospective record review of 18 343 postoperative patients at Boston Medical Center and Lahey Hospital and Medical Center–Burlington Campus who were discharged home after a postoperative inpatient admission of at least 24 hours. Data collection spanned from May 22, 2014, to June 30, 2016, in the Boston Medical Center data set and from March 23, 2015, to September 7, 2016, in the Lahey Hospital and Medical Center–Burlington Campus data set.
Exposures
Surgery requiring a postoperative inpatient hospital stay longer than 24 hours.
Main Outcomes and Measures
The main outcome measures were the patient’s 24-hour predischarge opioid use and the total quantity of opioids prescribed at hospital discharge. Potential overprescription was defined as the number of patients who used no opioids in the 24 hours prior to hospital discharge but were still prescribed opioids after hospital discharge.
Results
Among the 18 343 patients (10 069 women and 8274 men; mean age, 52.2 years) who underwent 21 452 surgical procedures, there was wide variation in the amount of opioids prescribed at hospital discharge given a postoperative patient’s 24-hour predischarge opioid use. A total of 6548 patients (35.7%) used no opioids in the 24 hours prior to hospital discharge; however, 2988 of these patients (45.6%) were prescribed opioids at hospital discharge, suggesting potential overprescription. Services that had the highest rates of potential overprescription (obstetrics [adjusted odds ratio (AOR), 3.146; 95% CI, 2.094-4.765] and gynecology [AOR, 2.355; 95% CI, 1.663-3.390], orthopedics [AOR, 0.943; 95% CI, 0.719-1.242], and plastic surgery [AOR, 0.733; 95% CI, 0.334-1.682]) generally had the highest rates of patients still using opioids at hospital discharge. Pediatric surgery was the only service that did not have any cases of potential overprescription (AOR, 2.09 × 10−7; 95% CI, 0.000-0.016).
Conclusions and Relevance
Opioids are not regularly prescribed in a patient-specific manner to postoperative patients. Potential opioid overprescription occurs regularly after surgery among almost all surgical specialties.
This cross-sectional study examines the correlation between a postoperative patient’s 24-hour predischarge opioid use and the amount of opioids prescribed at hospital discharge, as well as the number of patients who used no opioids prior to hospital discharge but were still prescribed opioids after hospital discharge.
Key Points
Question
Is a postoperative patient’s 24-hour predischarge opioid use correlated with the amount of opioids prescribed at hospital discharge?
Findings
In this cross-sectional study that included 18 343 postoperative patients from 2 Massachusetts medical centers, there was wide variation in the amount of opioids prescribed at hospital discharge given a patient’s individual 24-hour predischarge opioid use. Of the patients who no longer used opioids prior to hospital discharge, 45.6% were nonetheless prescribed opioids at hospital discharge.
Meaning
Potential overprescription of opioids occurs frequently among postoperative patients; improved opioid prescribing practices are needed to administer opioids in a more patient-specific manner.
Introduction
The United States is experiencing an opioid abuse epidemic, with 19 000 opioid-related deaths a year. In Massachusetts, 1531 residents died of overdose of prescription opioids and heroin in 2015, a 431% increase from the 355 deaths confirmed in 2000. This number corresponds to an incidence of 24.6 deaths per 100 000 residents, which is higher than the national mean number of deaths from overdose of opioids (14.7 deaths per 100 000 residents).
More concerning is the role that physicians, surgeons, and other health care professionals likely play in contributing to this epidemic. The National Survey on Drug Use and Health has shown that 4 of 5 current heroin users report that their opioid use began with prescription opioid analgesics. In addition, 70.3% of the opioids used for nonmedical purposes are obtained from a friend or relative, suggesting that the overprescription of opioid pain relievers may contribute to this epidemic.
Evidence from the surgical literature suggests that overprescription of opioids may occur after surgery. Furthermore, the amount of opioids prescribed after certain low-risk surgical procedures has been increasing during the past decade, and surgery itself has been implicated as a risk factor for long-term opioid use.
We reviewed the medical records of 18 343 postoperative patients to determine if there was any correlation between a patient’s opioid use prior to hospital discharge and the amount of opioids prescribed at hospital discharge. In particular, we sought to characterize a subset of patients who used no opioids prior to hospital discharge but were still prescribed them at hospital discharge, suggesting potential overprescription.
Methods
Study Design
This study was designed as a cross-sectional study of patients undergoing inpatient surgery. We sought to analyze the association between a postoperative patient’s 24-hour predischarge opioid use and the quantity of opioids prescribed at hospital discharge. The Boston University Medical Center Institutional Review Board and Lahey Clinic Institutional Review Board approved this study, both of which included a waiver of patient consent for acquisition of data.
Setting
Two Massachusetts medical centers from separate health systems were involved in this study: Boston Medical Center (BMC) and Lahey Hospital and Medical Center–Burlington Campus (LHMC-B). Boston Medical Center is an urban safety-net hospital and level 1 trauma center, and LHMC-B is a suburban community-based hospital and level 2 trauma center. Boston Medical Center routinely cares for obstetric and pediatric patients, whereas LHMC-B does not. Lahey Hospital and Medical Center–Burlington Campus has an acute pain consultation service, whereas BMC does not.
Data Sources
Data were obtained through retrospective database queries of the electronic medical records of BMC and LHMC-B. Both institutions currently use the same electronic medical record application (Epic, Epic Systems Corp). Data collection spanned from May 22, 2014, to June 30, 2016, for the BMC data set and from March 23, 2015, to September 7, 2016, for the LHMC-B data set.
Income data for each patient’s home zip code was obtained via the Internal Revenue Service, Statistics of Income division. Distance from the hospital was calculated from the patient’s home zip code to the hospital where the surgery was performed.
Patient Selection Criteria
Inclusion criteria consisted of any patient who underwent surgery during an inpatient admission with a postoperative length of stay longer than 24 hours who was subsequently discharged home. Exclusion criteria consisted of patients discharged to a skilled nursing or rehabilitation facility and surgical subspecialties with fewer than 5 cases.
Opioid Dose Calculations
For the patients in this study, the amount of short-acting opioid medications that were administered to the patient during the admission and the amount of opioids prescribed at hospital discharge were recorded. For comparison purposes, opioids were converted to equianalgesic doses of morphine sulfate (morphine milligram equivalents [MMEs]) using standard ratios. Long-acting opioids (methadone hydrochloride, buprenorphine hydrochloride, transdermal fentanyl citrate patches, and extended-release formulations of any opioid) were excluded because their administration was primarily indicated for long-term maintenance and not related to acute postoperative pain. Intraoperative or immediate perioperative opioid doses (intraoperative administrations, intravenous fentanyl, and patient-controlled analgesia) were also excluded because these doses do not accurately represent the type of analgesia that patients receive just prior to hospital discharge and at home. Opioids given intrathecally, intra-articularly, or through epidurals were also excluded because their effects were generally not still present during the predischarge period, in addition to the difficulty of converting these doses into MMEs. This study focused on opioid use and did not specifically investigate the use of nonopioid analgesics or multimodal regimens.
Excluding extended-release formulations of opioids may affect a patient’s opioid use and prescription and may potentially affect the rates of potential overprescription. However, we found that only 2.0% of admissions (400 of 20 035) had an extended-release opioid administered in the 24 hours prior to hospital discharge and that inclusion of these medications in our calculations had only a minor association with overall 24-hour predischarge opioid use (4.2%; 33 MME without extended-release opioids vs 35 MME with extended-release opioids), total opioids prescribed (3.9%; 343 MME without extended-release opioids vs 357 MME with extended-release opioids), and potential overprescription rate (–0.1%; 3051 of 6981 [43.70%] with extended-release opioids vs 3038 of 6957 [43.67%] without extended-release opioids).
Excluding patient-controlled analgesia and intravenous fentanyl doses could also affect the amount of opioids administered in the 24 hours before discharge and thus affect the potential rate of overprescription. Nonetheless, we found that 92.3% of admissions (14 093 of 15 275) in which patient-controlled analgesia or fentanyl had been used did not feature any doses administered in the final 24 hours before hospital discharge and that including these doses had a minimal association with the potential rate of overprescription (0.1% decrease, from 43.7% [3051 of 6981] to 43.6% [2949 of 6763]).
Potential Opioid Overprescription
Few guidelines have been established to recommend the quantity of opioids a patient should be prescribed at hospital discharge, making an objective assessment of overprescription or underprescription difficult. We defined a patient as no longer using opioids if he or she did not receive any short-acting opioids in the 24 hours prior to hospital discharge. We chose to define potential overprescription using the relatively conservative criteria of being prescribed opioids despite no longer using any opioid medications during the 24 hours prior to hospital discharge. We are aware that this definition may underestimate the actual prevalence of overprescription because patients who used minimal opioid medications (ie, 5 mg of oxycodone hydrochloride within 24 hours of hospital discharge) but were prescribed an excessive amount at hospital discharge (300 mg of oxycodone hydrochloride) would not be captured by this criteria. Requiring that a patient use no opioids during the 24 hours prior to hospital discharge to be considered for potential overprescription also prevents the classification of delayed-onset pain secondary to the fading effects of any regional nerve blocks because patients who started using opioids just prior to hospital discharge would be excluded.
Statistical Analysis
For comparison of continuous data, a 2-tailed t test was performed. Correlation was calculated using either the Pearson or Kendall correlation coefficients with a 2-tailed test for significance. P < .05 was considered statistically significant.
Linear regression analysis was performed via log transformations (log [x + 1]) of opioid use during the 24 hours before hospital discharge and the quantity of opioids prescribed at hospital discharge. Binomial logistic regression analysis was performed for patients who did not use any opioids during the 24 hours before hospital discharge. The dependent variable was whether the patient was prescribed opioids (potential overprescription) or not prescribed opioids. For categorical values (hospital, sex, regional or epidural anesthesia, insurance, and surgical service), we chose the following reference values: BMC, male, no regional or epidural anesthesia, Medicare, and general surgery. All statistical analysis was performed using R statistical software, version 3.3.2, with the openxlsx, tidyr, parallel, beepr, ggmap, and matrixStats extension packages.
Results
Surgical Patient Characteristics at BMC vs LHMC-B
A total of 18 343 patients who had 21 452 surgical procedures during 20 035 admissions with a postoperative length of stay of at least 24 hours met our admission criteria (Table 1). Compared with patients undergoing surgery at LHMC-B, patients at BMC were more likely to be younger (44.7 vs 61.1 years), female (6144 of 9795 [62.7%] vs 3925 of 8548 [45.9%]), reside in a lower-income area ($41 000 vs $57 000), live closer to the hospital (43 vs 82 km), and rely on government-assisted insurance or be uninsured (58% vs 7% Medicaid or uninsured) (eTable in the Supplement).
Table 1. Demographics, Opioid Use, and Opioid Prescription.
| Demographic | Postoperative Length of Stay >24 h | No Opioids Within 24 h Before Discharge | Not Overprescribed | Potential Overprescription | P Valuea |
|---|---|---|---|---|---|
| Patients, No. | 18 343 | 6548 | 3691 | 2988 | <.001 |
| Admissions, No. | 20 035 | 6981 | 3930 | 3051 | .49 |
| Surgical procedures, No. | 21 452 | 7607 | 4346 | 3261 | <.001 |
| Age, mean (range), y | 52.2 (0 to 101) | 58.6 (0 to 101) | 59.7 (0 to 101) | 57.4 (4 to 100) | <.001 |
| Male, No. (%) | 8274 (45.1) | 3463 (52.9) | 2068 (56.0) | 2988 (49.4) | <.001 |
| Body mass index, mean (range)b | 29.8 (9.8 to 80) | 28.5 (9.8 to 80) | 27.9 (9.8 to 70.5) | 29.3 (12.9 to 80) | <.001 |
| Medicaid or uninsured, No. (%) | 6343 (34.6) | 1632 (24.9) | 877 (23.8) | 778 (26.0) | .02 |
| Median income by zip code (in 1000), mean (range), $ | 48 (19 to 175) | 51 (19 to 139) | 52 (22 to 139) | 50 (19 to 139) | <.001 |
| Distance to hospital, mean (range), km | 60 (0.6 to 5044) | 61 (0.6 to 4985) | 59 (0.6 to 4976) | 63 (1.1 to 4985) | .49 |
| Procedures with regional or epidural anesthesia, No. (%) | 3117 (14.5) | 625 (8.2) | 212 (4.9) | 413 (12.7) | <.001 |
| Length of procedure, mean (range), min | 143 (0 to 1437) | 129 (1 to 1437) | 95 (1 to 1437) | 175 (1 to 778) | <.001 |
| Length of stay, mean (range), d | 5 (1 to 302.4) | 5.7 (1 to 302.4) | 6.1 (1 to 302.4) | 5.2 (1 to 200) | <.001 |
| Length of stay after surgery, mean (range), d | 4.4 (1 to 294.4) | 4.9 (1 to 294.4) | 5 (1 to 294.4) | 4.8 (1 to 200) | .38 |
| Opioid consumption and prescription | |||||
| Discharges home with opioids, No. | 14 652 | 3051 | 0 | 3051 | <.001 |
| 24-h Predischarge opioid use, mean (range), MME | 33 (0 to 1365) | 0 (0 to 0) | 0 (0 to 0) | 0 (0 to 0) | NA |
| Opioid discharge quantity, mean (range), MME | 343 (0 to 37 500) | 150 (0 to 13 500) | 0 (0 to 0) | 343 (34 to 13 500) | <.001 |
| Total opioids prescribed, MME | 6 881 492 | 1 045 616 | 0 | 1 045 616 | <.001 |
| Last opioid from surgery, mean (range), d | 3.4 (−20 to 122) | 2.4 (−20 to 122) | 2.2 (−20 to 122) | 2.6 (−8.5 to 106) | .02 |
| Last opioid from discharge, mean (range), d | −1 (−172 to 0) | −2.7 (−172 to 0) | −3.2 (−172 to 0) | −2.3 (−123 to 0) | <.001 |
Abbreviations: MME, morphine milligram equivalents, NA, not applicable.
Not overprescribed vs potential overprescription.
Calculated as weight in kilograms divided by height in meters squared.
Association Between Predischarge Opioid Use and Amount Prescribed at Hospital Discharge
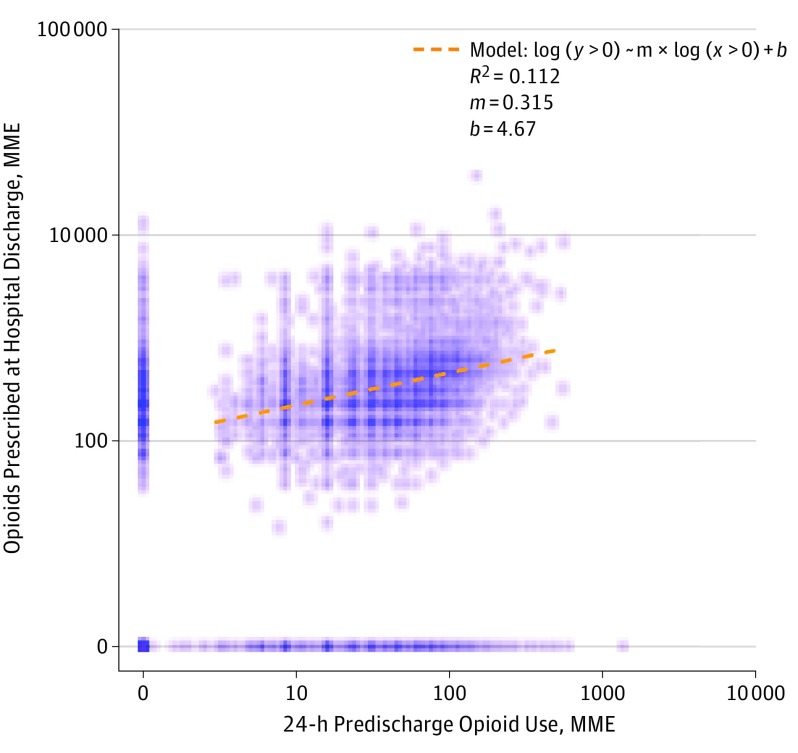
We found a wide variation in the amount of opioids prescribed at hospital discharge for any 24-hour predischarge amount of opioid use. For all amounts of opioids used in the 24 hours before hospital discharge, patients were prescribed a mean of 343 MME (range, 0-37 500 MME) (Table 1). Performing a log transformation of both the predischarge opioid use and quantity of opioids prescribed at hospital discharge revealed 3 distinct clusters (Figure 1).
Figure 1. Amount of Opioids Used 24 Hours Before Hospital Discharge vs Quantity Prescribed at Discharge.
The opioid discharge quantity is compared with the patient’s 24-hour predischarge use. Note the log axes. Each point represents an individual admission, and clusters of densely spaced points are represented by darker shades. The central cluster represents patients who used opioids before hospital discharge and were discharged with a prescription for opioids. The orange dashed line represents a linear regression of the log transformation of discharge quantity as a function of the log transformation of predischarge opioid use for this cluster (values >0), excluding the zero effects along the x-axis and y-axis. The cluster along the x-axis represents patients who were not prescribed opioids at hospital discharge. The cluster along the y-axis represents patients who were potentially overprescribed opioids (no predischarge use but prescribed opioids at hospital discharge). MME indicates morphine milligram equivalents.
The largest cluster, representing 11 603 of 20 035 admissions (57.9%), consisted of patients who used opioids before hospital discharge and were discharged with a prescription for opioids (Figure 1). A regression analysis of this cluster showed that there was a subtle association between the log units of predischarge opioid use and the log units of the quantity of opioids prescribed at hospital discharge (Figure 1). Nevertheless, this model was able to account for only 11% of the variance in this cluster.
The second cluster consisted of patients who were not discharged with a prescription for opioids, representing 5383 of 20 035 admissions (26.9%) (Figure 1). Most of these patients (3930 [73.0%]) did not receive opioids at hospital discharge because they had no predischarge opioid use. The remainder of the group was discharged home without a prescription for opioids despite using them before hospital discharge. Although we were unable to ascertain the exact underlying reasons, we speculate that no prescription occurred owing to reasons such as patient or clinician preference or already having a supply of opioids from prior to surgery.
The third cluster consisted of patients who had no opioid use before hospital discharge but were prescribed opioids at hospital discharge (Figure 1). We termed this anomaly as potential opioid overprescription; this group represented 15.2% (3051 of 20 035) of all admissions.
Potential Overprescription of Opioids at Hospital Discharge
As patients who no longer use opioids for 24 hours have likely recovered from their acute postoperative pain, we found it peculiar that a substantial amount of these patients were still being prescribed opioids at hospital discharge. Of the 20 035 admissions with a postoperative length of stay longer than 24 hours, 6981 (34.8%) did not have any opioid medications administered during the last 24 hours before hospital discharge (Table 1). However, 3051 of these admissions (43.7%) had a mean of 343 MME prescribed at hospital discharge, suggesting that these patients were potentially overprescribed opioids. This occurrence accounted for 15.2% (1 045 616 of 6 882 016 MME) of all opioids prescribed in our cohort.
There are, however, certain situations when prescribing an opioid may be indicated despite a patient not using any opioids prior to hospital discharge, such as for patients living a far distance from the hospital or for patients whose pain is currently controlled by regional nerve blocks that may wear off after hospital discharge. We found that patients who were potentially overprescribed opioids lived a similar mean distance from the hospital compared with those who were not overprescribed opioids (63 vs 59 km; P = .49).
Use of regional or epidural anesthesia was more common for patients who were potentially overprescribed opioids compared with patients who were not (413 of 3261 [12.7%] vs 212 of 4346 [4.9%]; P < .001) (Table 1). However, most surgical procedures (2848 of 3261 [87.3%]) that resulted in potential overprescription were performed without regional or epidural anesthesia.
Risk Factors for Potential Overprescription of Opioids
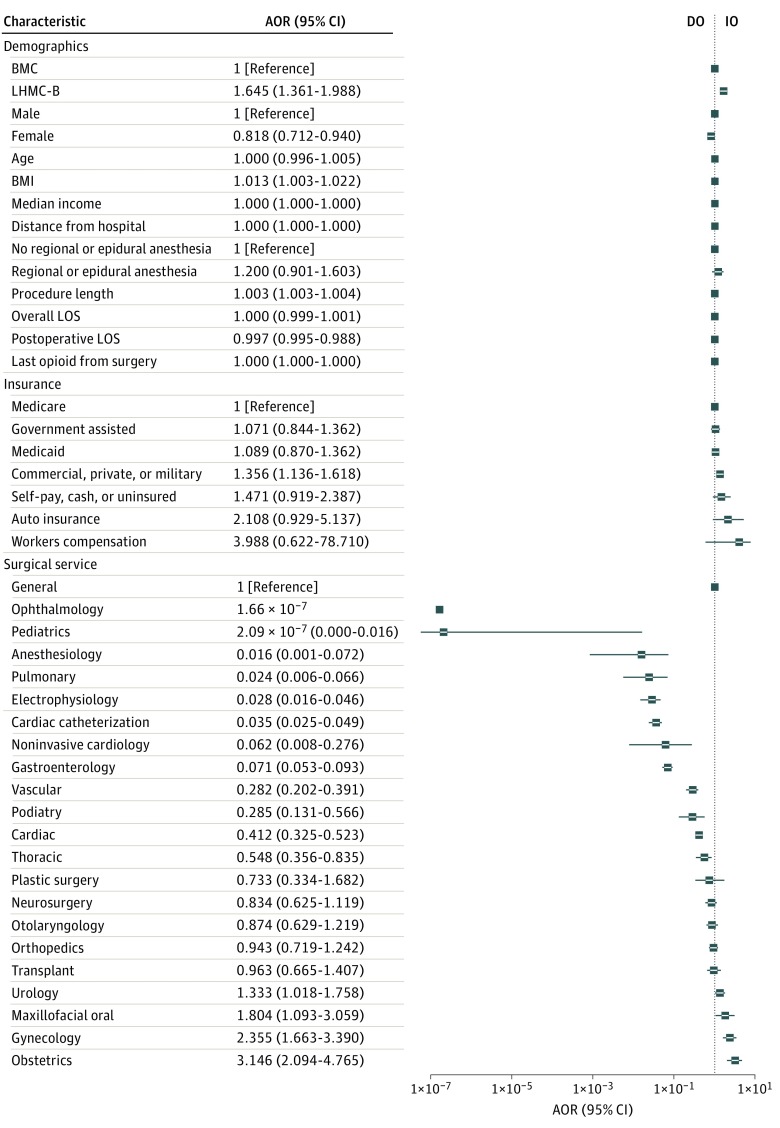
Using logistical regression, we sought to identify any possible risk factors for overprescription of opioids. Surgical service was most significantly associated with potential overprescription, with ophthalmology and pediatric surgery being associated with a lower risk of overprescription and obstetrics and gynecology associated with the highest risk of overprescription (Figure 2). Patients who were insured through worker’s compensation or automobile insurance were also associated with increased odds of potential overprescription. Aside from insurance status and surgical service, there were no particularly large associations of any patient demographic factors with the odds of potential overprescription.
Figure 2. Adjusted Odds Ratios (AORs) for Potential Overprescription.
Adjusted odds ratios were obtained from a binomial logistic regression analysis performed for patients who did not use any opioids during the 24 hours before hospital discharge. The dependent variable was whether the patient was prescribed opioids (potential overprescription) or not prescribed opioids. For categorical variables, chosen reference variables are shown by the solid squares. Error bars represent 95% CIs. Values of the AORs are displayed next to each label. Note the log-scaled x-axis. BMC indicates Boston Medical Center; BMI, body mass index; DO, decreased odds; IO, increased odds; LHMC-B, Lahey Hospital and Medical Center–Burlington Campus; and LOS, length of stay.
Potential Overprescription by Service
Further investigating the pattern of potential overprescription, we analyzed the prevalence of potential overprescription by surgical service (Table 2). Of the services with more than 5 cases in our series, only BMC’s pediatric surgery service did not have any cases of potential overprescription. Obstetrics and gynecology had the highest rates of potential overprescription. Regional or epidural anesthesia was commonly used in the obstetrics service (1662 of 1889 procedures [88.0%]), suggesting that this practice may be a factor underlying the prescription of opioids to patients who did not receive any before hospital discharge. However, epidural anesthesia and regional anesthesia were less frequently used in other services with high rates of potential overprescription (gynecology, 130 of 1025 [12.7%]; orthopedics, 854 of 2971 [28.7%]).
Table 2. Opioid Consumption and Prescription by Surgical Service and Insurance Type.
| Characteristic | Postoperative Length of Stay >24 h, No. | No Opioids Within 24 h Prior to Discharge, No. (%) | No Opioids Within 24 h Prior to Discharge and Discharged Without Opioids, No. | Potential Overprescription, No. (%) |
|---|---|---|---|---|
| Service | ||||
| Anesthesiology (BMC) | 224 | 136 (60.7) | 133 | 3 (2.2) |
| Cardiac | ||||
| BMC | 297 | 114 (38.4) | 63 | 51 (44.7) |
| LHMC-B | 918 | 430 (46.8) | 181 | 249 (57.9) |
| Cardiac catheterization (LHMC-B) | 995 | 805 (80.9) | 751 | 54 (6.7) |
| Electrophysiology (LHMC-B) | 414 | 360 (87.0) | 336 | 24 (6.7) |
| Gastroenterology | ||||
| BMC | 254 | 161 (63.4) | 147 | 14 (8.7) |
| LHMC-B | 1194 | 879 (73.6) | 794 | 85 (9.7) |
| General | ||||
| BMC | 2627 | 656 (25.0) | 312 | 344 (52.4) |
| LHMC-B | 2061 | 822 (39.9) | 206 | 616 (74.9) |
| Gynecology | ||||
| BMC | 746 | 184 (24.7) | 51 | 133 (72.3) |
| LHMC-B | 279 | 109 (39.1) | 18 | 91 (83.5) |
| Maxillofacial oral (BMC) | 644 | 99 (15.4) | 33 | 66 (66.7) |
| Neurosurgery | ||||
| BMC | 668 | 163 (24.4) | 87 | 76 (46.6) |
| LHMC-B | 689 | 176 (25.5) | 54 | 122 (69.3) |
| Noninvasive cardiology (LHMC-B) | 28 | 19 (67.9) | 17 | 2 (10.5) |
| Obstetrics (BMC) | 1889 | 374 (19.8) | 96 | 278 (74.3) |
| Ophthalmology (BMC) | 29 | 15 (51.7) | 14 | 1 (6.7) |
| Orthopedics | ||||
| BMC | 1540 | 155 (10.1) | 62 | 93 (60.0) |
| LHMC-B | 1431 | 227 (15.9) | 78 | 149 (65.6) |
| Otolaryngology | ||||
| BMC | 602 | 254 (42.2) | 178 | 76 (29.9) |
| LHMC-B | 195 | 68 (34.9) | 13 | 55 (80.9) |
| Pediatrics (BMC) | 91 | 75 (82.4) | 75 | 0 |
| Plastic surgery | ||||
| BMC | 88 | 16 (18.2) | 5 | 11 (68.8) |
| LHMC-B | 124 | 19 (15.3) | 8 | 11 (57.9) |
| Podiatry (BMC) | 221 | 96 (43.4) | 79 | 17 (17.7) |
| Pulmonary (LHMC-B) | 127 | 90 (70.9) | 85 | 5 (5.6) |
| Thoracic (BMC) | 431 | 138 (32.0) | 88 | 50 (36.2) |
| Transplant | ||||
| BMC | 168 | 77 (45.8) | 50 | 27 (35.1) |
| LHMC-B | 324 | 103 (31.8) | 16 | 87 (84.5) |
| Urology | ||||
| BMC | 434 | 115 (26.5) | 61 | 54 (47.0) |
| LHMC-B | 1064 | 399 (37.5) | 73 | 326 (81.7) |
| Vascular | ||||
| BMC | 339 | 105 (31.0) | 68 | 37 (35.2) |
| LHMC-B | 317 | 168 (53.0) | 114 | 54 (32.1) |
| Total | 21 452 | 7607 (35.5) | 4346 | 3261 (42.9) |
| Insurance | ||||
| Automobile insurance | ||||
| BMC | 176 | 30 (17.0) | 9 | 21 (70.0) |
| LHMC-B | 35 | 5 (14.3) | 3 | 2 (40.0) |
| Commercial/private/military | ||||
| BMC | 2405 | 585 (24.3) | 293 | 292 (49.9) |
| LHMC-B | 4790 | 1746 (36.5) | 919 | 827 (47.4) |
| Government-assisted health care | ||||
| BMC | 172 | 34 (19.8) | 15 | 19 (55.9) |
| LHMC-B | 1058 | 634 (59.9) | 392 | 242 (38.2) |
| Medicaid | ||||
| BMC | 6076 | 1509 (24.8) | 839 | 670 (44.4) |
| LHMC-B | 662 | 217 (32.8) | 120 | 97 (44.7) |
| Medicare | ||||
| BMC | 1872 | 656 (35.0) | 400 | 256 (39.0) |
| LHMC-B | 3516 | 2047 (58.2) | 1294 | 753 (36.8) |
| Self-pay, cash, or uninsured | ||||
| BMC | 489 | 116 (23.7) | 45 | 71 (61.2) |
| LHMC-B | 42 | 19 (45.2) | 14 | 5 (26.3) |
| Workers compensation | ||||
| BMC | 102 | 3 (2.9) | 1 | 2 (66.7) |
| LHMC-B | 57 | 6 (10.5) | 2 | 4 (66.7) |
| Total | 21 452 | 7607 (35.5) | 4346 | 3261 (42.9) |
Abbreviations: BMC, Boston Medical Center; LHMC-B, Lahey Hospital and Medical Center–Burlington Campus.
Patients used and were prescribed opioids after percutaneous or scope-based procedures performed by medical services, albeit at a lower rate than more traditional surgical services. In these cases, opioids may have been prescribed if the procedure was more invasive than a standard diagnostic procedure (eg, colonoscopy with biopsy or tumor embolization) or if the presenting symptom was pain (eg, gallstones).
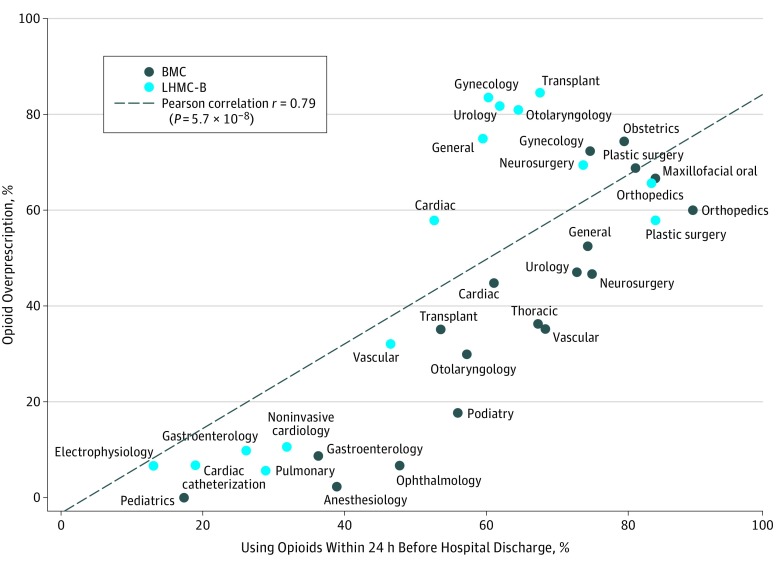
Overall, we found a strong correlation between services with higher rates of patients who were still using opioids at hospital discharge having higher rates of potential overprescription (Pearson correlation coefficient r = 0.79) (Figure 3). No significant correlation was found when patients were similarly grouped by insurance status (Pearson correlation coefficient r = 0.38; P = .12).
Figure 3. Potential Overprescription Rate by Service vs Percentage of Patients Using Opioids at Hospital Discharge.
The potential overprescription rate by surgical service is compared with the percentage of patients who still used opioids within 24 hours before hospital discharge. Each point represents a single surgical service. The dashed line is a linear fit of the different points, weighted by the number of surgical procedures performed by each service. BMC indicates Boston Medical Center; LHMC-B, Lahey Hospital and Medical Center–Burlington Campus.
Discussion
This study shows that the prescription of opioids is only moderately correlated with a patient’s 24-hour predischarge opioid use. To our knowledge, this is the first study to examine the association of predischarge opioid use with the amount of opioids prescribed at hospital discharge across all types of inpatient surgical procedures. We found a subtle, nonlinear association between these 2 factors that is likely some form of a power law. Although we were unable to fully ascertain the factors underlying this association, we speculate that this association may reflect the general clinical judgment of clinicians regarding a patient’s likely opioid use.
To our knowledge, this study is also the first to highlight the problem of potential opioid overprescription at our institutions. Although in most cases (3560 of 6548 [54.4%]) clinicians did not prescribe opioids to patients who no longer used opioids before hospital discharge, a significant proportion of patients (2988 of 6548 [45.6%]) not using any opioids before hospital discharge were nevertheless potentially overprescribed opioids at hospital discharge (2988 of all 18 343 admissions [16.3%]).
Patients who do not use any opioids prior to hospital discharge have a higher likelihood of being potentially overprescribed opioids if they underwent a procedure performed by a surgical service that frequently discharged patients using opioids prior to hospital discharge (Figure 3). These findings suggest that prescribers of all specialties may not be able to easily identify patients who are no longer using opioids at hospital discharge, particularly those prescribers who routinely discharge patients still using opioids.
Strengths and Limitations
The strengths of this study are its broad sample size, encompassing patients of all demographic and insurance types, among all surgical specialties at 2 medical centers with differing patient populations. This study also examined opioid use throughout a patient’s hospital stay, a longer period than most other studies that examined opioid use only in the postanesthesia care unit or through only the first postoperative day.
Limitations of this study include its retrospective nature, its geographical limitation to eastern Massachusetts, and its inability to fully account for any opioid-sparing effects of nonopioid analgesics. All data used in this study were collected on a prospective basis as part of standard medical documentation practices, minimizing any potential selection, information, or recall biases. Regarding the effects of nonopioid analgesics, patients are routinely prescribed these types of medications as first-line treatment for pain at both hospitals. Any effects of these analgesics should theoretically be reflected in the patient’s opioid use, although we were unable to specifically study these effects.
Other Cases of Excessive Opioid Prescription
Several studies have highlighted the prevalence of excess prescription of opioids after surgery, demonstrating that 70% to 80% of patients do not fill or finish their opioids prescribed at hospital discharge and that a significant amount of opioids prescribed at hospital discharge go unconsumed. Additional studies have also reported wide variation in the amount of opioids prescribed for any single procedure as well as across different clinicians.
To our knowledge, only 1 other study has previously examined both a patient’s 24-hour predischarge opioid use and the amount of opioids prescribed at hospital discharge. Similar to our findings, that study also reported a poor correlation between predischarge opioid use and the amount of opioids prescribed at hospital discharge because they found no significant difference in the amount of opioids prescribed at hospital discharge between their “high-use” and “low-use” cohorts.
Reasons for Potential Overprescription
Although most physicians and other health care professionals are well aware of the need to prescribe opioids judiciously, there is little evidence available to help guide the quantity of opioids that a patient will use after surgery, especially after major inpatient procedures. Thus, it is generally up to individual clinicians to prescribe an appropriate quantity of opioids at their discretion.
Our finding that services with higher rates of patients who were still using opioids at hospital discharge had higher rates of potential overprescription suggests a possible service-based cultural bias toward overprescribing or perhaps an inability to effectively identify patients who are no longer using them. We did not find any nonsurgical patient demographic factors that had a considerable effect on the odds of potential overprescription.
Patients who were overprescribed opioids often underwent longer procedures in our data set (175 vs 95 minutes), a factor that has been previously associated with increased opioid use. In addition, the services with higher rates of potential overprescription (obstetrics and gynecology, general surgery, and orthopedic surgery) are generally associated with more painful operations. This finding suggests that prescribers who routinely care for patients undergoing more invasive surgical procedures may be more accustomed to regularly prescribing opioids and thus may be less vigilant about identifying patients who are not taking opioids at the time of hospital discharge.
Areas for Improvement
To prescribe opioids more accurately, a better understanding of opioid use after surgery is needed. In this study, we performed a broad analysis across more than 20 surgical specialties. However, the course of postoperative pain varies with type of procedure and patient demographic factors; thus, further investigation is necessary into how these factors affect patients in a more specific manner. Although several studies have found that most patients only fill a single prescription for opioids after surgery, it has been reported that patients may use opioids for more than 1 month after surgery, with some going on to become long-term users. Therefore, further in-depth research into patients’ postoperative pain experience and opioid use should reveal a better understanding of the quantity of opioids used for adequate, but not excessive, pain control.
Conclusions
This study found broad variation in opioid prescribing across multiple surgical specialties at our institutions. Opioids were not prescribed in a patient-specific manner to postoperative patients. Finally, we found that potential overprescription occurs regularly after surgery.
eTable. Demographics, Opioid Consumption, and Prescription by Hospital
References
- 1.Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2016;64(50-51):1378-1382. [DOI] [PubMed] [Google Scholar]
- 2.Massachusetts Department of Public Health Data brief: opioid-related overdose deaths among Massachusetts residents. http://www.mass.gov/eohhs/docs/dph/quality/drugcontrol/county-level-pmp/opioid-related-overdose-deaths-among-ma-residents-august-2016.pdf. Accessed October 13th, 2016.
- 3.Barnett ML, Olenski AR, Jena AB. Opioid-prescribing patterns of emergency physicians and risk of long-term use. N Engl J Med. 2017;376(7):663-673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muhuri PK, Gfroerer JC, Davies MC. Associations of nonmedical pain reliever use and initiation of heroin use in the United States. CBHSQ Data Review Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/sites/default/files/DR006/DR006/nonmedical-pain-reliever-use-2013.htm. Published August 2013. Accessed November 3, 2017.
- 5.Jones CM, Paulozzi LJ, Mack KA. Sources of prescription opioid pain relievers by frequency of past-year nonmedical use: United States, 2008-2011. JAMA Intern Med. 2014;174(5):802-803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bates C, Laciak R, Southwick A, Bishoff J. Overprescription of postoperative narcotics: a look at postoperative pain medication delivery, consumption and disposal in urological practice. J Urol. 2011;185(2):551-555. [DOI] [PubMed] [Google Scholar]
- 7.Rodgers J, Cunningham K, Fitzgerald K, Finnerty E. Opioid consumption following outpatient upper extremity surgery. J Hand Surg Am. 2012;37(4):645-650. [DOI] [PubMed] [Google Scholar]
- 8.Hill MV, McMahon ML, Stucke RS, Barth RJ Jr. Wide variation and excessive dosage of opioid prescriptions for common general surgical procedures. Ann Surg. 2017;265(4):709-714. [DOI] [PubMed] [Google Scholar]
- 9.Wunsch H, Wijeysundera DN, Passarella MA, Neuman MD. Opioids prescribed after low-risk surgical procedures in the United States, 2004-2012. JAMA. 2016;315(15):1654-1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sun EC, Darnall BD, Baker LC, Mackey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016;176(9):1286-1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med. 2012;172(5):425-430. [DOI] [PubMed] [Google Scholar]
- 12.Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014;348:g1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carroll I, Barelka P, Wang CK, et al. . A pilot cohort study of the determinants of longitudinal opioid use after surgery. Anesth Analg. 2012;115(3):694-702. [DOI] [PubMed] [Google Scholar]
- 14.Internal Revenue Service, US Department of the Treasury SOI tax stats—individual income tax statistics—2014 ZIP code data (SOI). https://www.irs.gov/statistics/soi-tax-stats-individual-income-tax-statistics-2014-zip-code-data-soi. Updated August 25, 2017. Accessed November 3, 2017.
- 15.McPherson ML. Demystifying Opioid Conversion Calculations: A Guide for Effective Dosing. Bethesda, MA: American Society of Health-System Pharmacists; 2009. [Google Scholar]
- 16.Mitra S, Sinatra RS. Perioperative management of acute pain in the opioid-dependent patient. Anesthesiology. 2004;101(1):212-227. [DOI] [PubMed] [Google Scholar]
- 17.Chou R, Gordon DB, de Leon-Casasola OA, et al. . Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council [published correction appears in J Pain. 2016;17(4):508-510]. J Pain. 2016;17(2):131-157. [DOI] [PubMed] [Google Scholar]
- 18.R Core Team R: A Language and Environment for Statistical Computing, version 3.3.2. Vienna, Austria: R Foundation for Statistical Computing; 2016. [Google Scholar]
- 19.Newman MEJ. Power laws, Pareto distributions and Zipf’s law. Contemp Phys. 2005;46(5):323-351. doi: 10.1016/j.cities.2012.03.001 [DOI] [Google Scholar]
- 20.Bartels K, Mayes LM, Dingmann C, Bullard KJ, Hopfer CJ, Binswanger IA. Opioid use and storage patterns by patients after hospital discharge following surgery. PLoS One. 2016;11(1):e0147972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harris K, Curtis J, Larsen B, et al. . Opioid pain medication use after dermatologic surgery: a prospective observational study of 212 dermatologic surgery patients. JAMA Dermatol. 2013;149(3):317-321. [DOI] [PubMed] [Google Scholar]
- 22.Kim N, Matzon JL, Abboudi J, et al. . A prospective evaluation of opioid utilization after upper-extremity surgical procedures: identifying consumption patterns and determining prescribing guidelines. J Bone Joint Surg Am. 2016;98(20):e89. [DOI] [PubMed] [Google Scholar]
- 23.Washington Agency Medical Director’s Group Interagency guideline on prescribing opioids for pain. http://www.agencymeddirectors.wa.gov/Files/2015AMDGOpioidGuideline.pdf. Accessed May 17, 2017.
- 24.Gagliese L, Gauthier LR, Macpherson AK, Jovellanos M, Chan VW. Correlates of postoperative pain and intravenous patient-controlled analgesia use in younger and older surgical patients. Pain Med. 2008;9(3):299-314. [DOI] [PubMed] [Google Scholar]
- 25.Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. 2013;118(4):934-944. [DOI] [PubMed] [Google Scholar]
- 26.Ip HYV, Abrishami A, Peng PW, Wong J, Chung F. Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology. 2009;111(3):657-677. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Demographics, Opioid Consumption, and Prescription by Hospital