Abstract
Background and Objectives:
The ability to obtain adequate tissue of solid pancreatic lesions by EUS-guided remains a challenge. The aim of this study was to compare the performance characteristics and safety of EUS-FNA for evaluating solid pancreatic lesions using the standard 22-gauge needle versus a novel EUS biopsy needle.
Methods:
This was a multicenter retrospective study of EUS-guided sampling of solid pancreatic lesions between 2009 and 2015. Patients underwent EUS-guided sampling with a 22-gauge SharkCore (SC) needle or a standard 22-gauge FNA needle. Technical success, performance characteristics of EUS-FNA, the number of needle passes required to obtain a diagnosis, diagnostic accuracy, and complications were compared.
Results:
A total of 1088 patients (mean age = 66 years; 49% female) with pancreatic masses underwent EUS-guided sampling with a 22-gauge SC needle (n = 115) or a standard 22-gauge FNA needle (n = 973). Technical success was 100%. The frequency of obtaining an adequate cytology by EUS-FNA was similar when using the SC and the standard needle (94.1% vs. 92.7%, respectively). The sensitivity, specificity, and diagnostic accuracy of EUS-FNA for tissue diagnosis were not significantly different between two needles. Adequate sample collection leading to a definite diagnosis was achieved by the 1st, 2nd, and 3rd pass in 73%, 92%, and 98% of procedures using the SC needle and 20%, 37%, and 94% procedures using the standard needle (P < 0.001), respectively. The median number of passes to obtain a tissue diagnosis using the SC needle was significantly less as compared to the standard needle (1 and 3, respectively; P < 0.001).
Conclusions:
The EUS SC biopsy needle is safe and technically feasible for EUS-FNA of solid pancreatic mass lesions. Preliminary results suggest that the SC needle has a diagnostic yield similar to the standard EUS needle and significantly reduces the number of needle passes required to obtain a tissue diagnosis.
Keywords: EUS, FNA, fine-needle biopsy, core, pancreatic mass
INTRODUCTION
The incidence of pancreatic cancer has been steadily increasing over the past decade. Approximately 53,000 new cases of pancreatic cancer will be diagnosed in 2016, with pancreatic cancer projected to surpass breast cancer as the third leading cause of cancer-related death in the United States. With a 5-year survival rate of only 8%, early and accurate pathological diagnosis is vital to guide subsequent patient management.[1] In patients with a suspicious pancreatic lesion, EUS-FNA allows for tissue acquisition and cytological verification of malignancy and is the current standard for diagnosis at most centers. The diagnostic accuracy of EUS-FNA varies from 78% to 95%.[2,3,4] As evidenced in the literature, several factors are known to influence the diagnostic accuracy of EUS-FNA, including diameter of needle, number of passes required, and presence of a cytopathologist who can provide rapid on-site evaluation (ROSE).[5,6,7,8,9,10] Increased expense and resources associated with ROSE have been an obstacle to the universal implementation of this technique, and in the absence of ROSE, multiple passes are often needed to acquire adequate tissue.[11,12]
New EUS fine-needle biopsy (EUS-FNB) designs in recent years have advanced the ability to obtain adequate core tissue with preserved tissue architecture for histological analysis.[13,14,15,16,17] A recent meta-analysis found the sensitivity and specificity of EUS-FNB in differentiating malignant from benign pancreatic masses to be 0.84 (95% confidence interval [CI], 0.82–0.87) and 0.98 (95% CI, 0.93–1.00), respectively.[18] Except decreased number of needles passes, studies have failed to show a diagnostic advantage in using EUS-FNB needles over standard EUS-FNA needles.[19,20]
A recent tissue acquisition device to gain FDA approval is the SharkCore™ FNB device (SC-FNB), used as part of the Beacon EUS Delivery System (Medtronic). Initial experience with the novel EUS core biopsy needle has been promising with pathologic diagnostic yield of 87% for pancreatic lesions.[21]
The objective of this multicenter retrospective cohort study was to compare the performance characteristics and safety of the standard 22-guage EUS needle (EUS-FNA) versus the EUS 22-gauge SC-FNB for the diagnosis of solid pancreatic lesions.
METHODS
Patient selection
We conducted a dual-center retrospective cohort study of all EUS-guided sampling of solid pancreatic lesions performed between June 2009 and October 2015. ROSE was available for all procedures. During the study, a total of 1088 consecutive patients with solid pancreatic lesions underwent EUS-guided sampling with either a 22-gauge SC-FNB or 22-gauge FNA needle (EchoTip Ultra 3 needle; Wilson-Cook Medical, Winston-Salem, North Carolina) for diagnosis depending on the year of their presentation (the 22-gauge SC-FNB needle was introduced at our institutions in February 2013 and since that time has been used exclusively for all EUS-guided sampling). The medical records of the patients were reviewed using a standard data entry form that included patients’ demographics, technical success, performance characteristics of EUS-FNA, location of lesion, size, number of needle passes required to obtain a diagnosis, cytology results, and procedural complications. The results of EUS-guided sampling were confirmed using surgical histopathology when available. This study was approved by the Institutional Review Board of the participating institutions.
EUS guided sampling technique
All EUS-FNAs were performed by experienced faculty who had performed >500 EUS procedures. The pancreatic lesion was initially identified using the curvilinear echoendoscope (Olympus GF-UCT180, 160, or 140, Center Valley, PA) after which the EUS-FNA was performed. Lesions were sampled with either a transgastric or transduodenal approach based on lesion location. As previously mentioned, either the 22-gauge SC-FNB needle or the standard 22-gauge FNA needle was used to sample the target lesion.
Technique for using the 22-gauge EUS-FNA needle
The 22-gauge EUS-FNA needle device was passed through the echoendoscope biopsy channel and then advanced into a target lesion under ultrasound guidance with the stylet within the needle. The stylet was removed and 10 cc of suction was applied. Ten actuations were performed. Suction was released before removal of the needle to avoid contamination of GI mucosa. Aspirated cellular material was expressed onto the slide by advancing the stylet, and the remainder was expressed into a cell block preparation using saline or air flush.
Technique for using the 22-gauge EUS-FNA SharkCore™ needle
Targets were localized on EUS and punctured with the stylet in place. The stylet was pulled back 5 cm from the needle tip and the needle was held in place for 30 s. Four actuations were performed. The stylet was completely removed and four more actuations were performed. The needle was withdrawn from the mass without the application of suction. Aspirated cellular material was expressed onto a slide using an air-filled 10 cc syringe.
Cytological preparation
Aspirates were placed onto glass slides and preserved with Diff-Quik stain (American Scientific Products, McGraw Park, Illinois, USA). In addition, a smear was also placed in alcohol for Papanicolaou staining. Any additional material was sent for cell block processing. The cytology technician on-site verified adequacy of specimens. Each cytological aspirate obtained by either the SC-FNB or EUS-FNA needle was evaluated by an expert cytopathologist for ROSE and classified as malignant, benign, or an inadequate specimen based on cytological smear. A specimen was considered adequate if there were an adequate number of representative cells from the target lesion.
Cytologic assessment of samples
Patients in the current study were classified as having a benign versus a malignant lesion. A final diagnosis of a pancreatic malignancy was based on (1) cytologic or histologic evidence of malignancy based on material obtained using EUS-FNA, ERCP, surgical or percutaneous biopsy OR (2) clinical course based on follow-up in which that patient developed radiographic evidence of local or distant metastasis, or death attributed to a malignant pancreatic lesion based on clinical records if the cytology or surgical pathology results were inconclusive. A lesion was defined as being benign based on EUS-FNA results, clinical follow-up, and lack of disease progression over a period of at least 6 months. When a final diagnosis could not be established due to the lack of a criterion standard or adequate follow-up (n = 42), patients were excluded when calculating operating characteristics.
EUS-FNA cytology samples were interpreted as malignant, suspicious for malignancy, atypical cells, benign, and nondiagnostic. Patients with suspicious or malignant cytology were classified as “true positive “if the final diagnosis was malignancy, and those considered benign on the final diagnosis were classified as “false positive.”[14] Similarly, lesions classified as benign by EUS-FNA with a final diagnosis of benign were considered “true negative” and those considered malignant on final diagnosis were false negative. Atypical cytology with final diagnosis as benign was considered “true negative” and those malignant as “false negative.”
Diagnostic accuracy was defined as the ratio between the sum of true positive and true negative values, divided by the total number of samples. The adequacy rate was calculated by the following formula: number of adequate samples divided by total number of samples.
Statistical analysis
Patients were stratified into two groups: (1) those that underwent sampling of the pancreatic lesion using the 22-gauge EUS-FNA Needle and (2) those that underwent sampling using the 22-gauge EUS-FNB. Summary statistics were calculated in the two groups, using means and standard deviations for continuous variables and counts and percentages for categorical variables.
A two-tailed sample size calculation was performed with the type I error rate (α) set at 0.05 to attain 80% power for a 20% difference in diagnostic yield for each pass. The targeted sample size needed was 46 patients in the FNA group and 46 patients in the FNB group.
The overall operating characteristics of each needle were analyzed for sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and diagnostic accuracy. Proportions were compared using a Z-test. Each pass was analyzed for adequacy and an odds ratio was calculated. The mean number of needle passes needed to achieve diagnosis on cytological smear was analyzed with a two-tailed-t-test. Statistical significance was taken as P < 0.05. Statistical analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, North Carolina, USA).
RESULTS
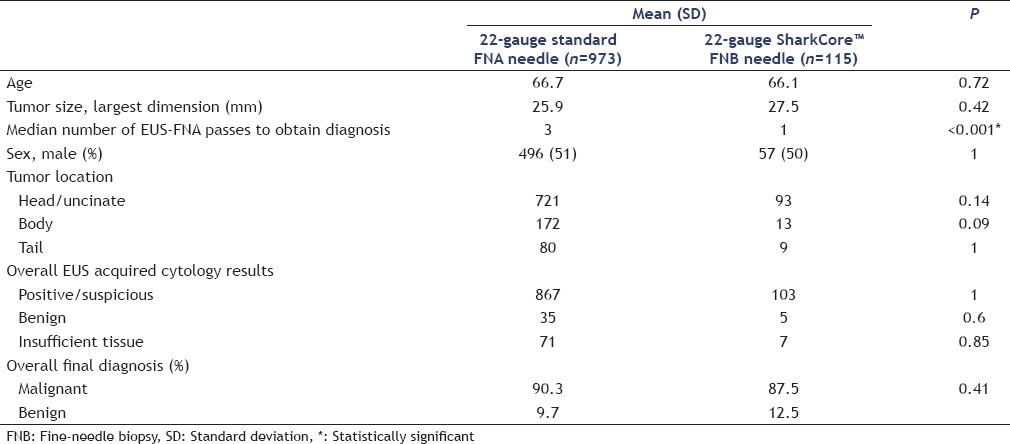
A total of 1088 patients (Thomas Jefferson University = 1026 patients and University of Utah = 62 patients) underwent EUS-guided sampling for the evaluation of solid pancreatic mass lesions. Of these patients, 973 underwent EUS-FNA using the standard 22-gauge FNA needle, whereas the 22-gauge SC-FNB needle was utilized in 115 patients. Demographic data of the study population and characteristics of the mass lesions are shown in Table 1. The mean age of subjects was 66 years, and 49% were female. Totally, 814 lesions were located in the head/uncinate process of the pancreas, 185 were in the pancreatic body, and 89 were in the pancreatic tail. The mean lesion size was 29 mm (range 7–83). There was no significant difference between the two groups with regard to gender, age, lesion size, or location.
Table 1.
Baseline demographic characteristics of study cohort
Surgical histopathology was available 301 (31%) patients in the 22-gauge FNA group and 26 (30%) cases in the 22-gauge SC-FNB group. The final pathology diagnosis was adenocarcinoma in 81.8% of cases, neuroendocrine tumor 4.7%, intra-ductal papillary mucosal neoplasms with dysplasia in 5.4%, metastatic disease in 4.4%, and benign cells in 3.7%. Approximately one-third of the patients (327; 30%) with a pancreatic mass underwent successful curative surgery which further confirmed the diagnosis of malignancy.
The procedural technical success rate was 100% in both groups. There was no significant difference in the ability to obtain adequate tissue cytology when using the SC-FNB and the standard FNA needle (94.1% and 92.7%, respectively; P = 0.85).
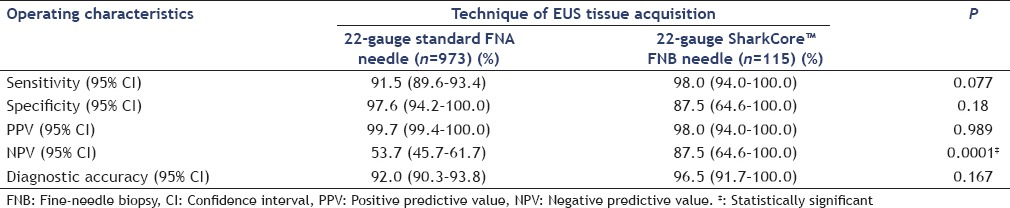
Operating characteristics of the individual EUS needles are summarized in Table 2. Both groups showed high sensitivities and specificities. The FNB needle had a higher sensitivity to diagnose malignancy compared to the 22-gauge standard FNA needle (98% vs. 91.5%, respectively; P = 0.077); this difference approached but did not reach statistical significance. Both groups had similar specificities (P = 0.98). The FNB and standard FNA needle both had a high PPV to diagnose a cancer (98% vs. 99.7%; P = 0.99). Conversely, the FNB needle had a significantly superior NPV to diagnose a cancer (97.5%) as compared to the standard FNA needle (53.7%) (P = 0.0001). Although the diagnostic accuracy of the FNB was also superior compared to the standard FNA needle, this did not reach statistical significance (96.5% vs. 92%, respectively; P = 0.167).
Table 2.
Operating characteristics of individual EUS needles
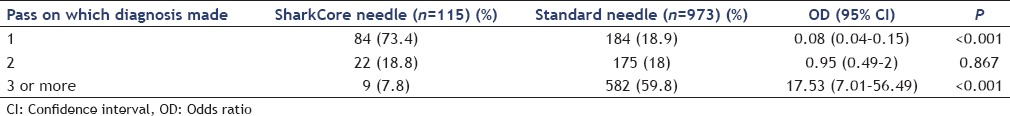
The per pass analysis for the two different needles is shown in Table 3 as analyzed by a Poisson regression. Adequate sample collection leading to a definite diagnosis was achieved by the 1st, 2nd, and 3rd passes in 73%, 92%, and 98% of procedures, respectively, when using the SC needle, as opposed to and 20%, 37%, and 94% procedures, respectively, when using the standard needle (P < 0.001). The median number of passes to obtain a tissue diagnosis using the SC needle was significantly less as compared to the standard needle (1 and 3, respectively; P < 0.001).
Table 3.
Per pass analysis
The overall rates in the FNB and standard FNA needle were 2 (1.7%) versus 12 (1.2%) (P = 0.65). Complications of the FNB group were post-FNA pancreatitis (n = 2). Complications of the standard FNA needle group were post-FNA pancreatitis (n = 5), self-limited abdominal pain (n = 4), and minor bleeding after FNA (n = 3).
DISCUSSION
In the absence of ROSE, inadequate specimens are obtained in as many as 29% of patients who undergo EUS-FNA.[22] While historical data have cited a low rate of false positive diagnosis of malignancy (0%–1%), recent studies suggest that the false positive rate of FNA cytology is as high as 5%–7%.[23,24,25] Studies have also reported up to 30% of patients with clinical and imaging findings suggestive of pancreatic malignancy having negative cytology on EUS-FNA.[26,27] To overcome these limitations of cytological aspirates, novel EUS core biopsy needles have been developed in efforts to reliably obtain intact core tissue and increase specimen adequacy and diagnosis, thereby obviating or at least reducing the need for and dependence on an onsite cytopathologist.
Although initial studies of both the first-generation (Quick-Core, Cook Medical Inc., Winston Salem, North Carolina) and second-generation (ProCore, Cook Endoscopy) core biopsy needles were promising, additional studies have failed to demonstrate a diagnostic advantage of either needle over standard EUS-FNA needles.[19,28,29] Furthermore, design limitation and lack of maneuverability of the tru-cut biopsy needle have largely limited its use in clinical practice.[30]
To the best of our knowledge, our multicenter retrospective cohort study is the largest study to date to evaluate the diagnostic yield (with respect to cytological aspirate) and performance of the SC FNB against the standard 22-gauge FNA needle. Our study failed to demonstrate the superiority of the SC needle over the standard needle in terms of overall diagnostic accuracy. However, it was noted that fewer passes were required in the FNB group to establish a pathologic diagnosis. This finding is in keeping with results obtained by previous studies that have demonstrated that while the ProCore™ FNB needle had a similar diagnostic accuracy to the 22-gauge standard EUS needle, fewer passes were required to achieve diagnostic adequacy.[19,31,32]
This finding is significant in its implications for patient safety and cost efficiency, as fewer passes over many examinations decrease risk to patients and may save both the endoscopist and cytologist time in terms of samples needing to be collected and processed.
Data presented in several abstracts on SC-FNB have demonstrated excellent pathologic as well as diagnostic yield. Initial experience with SC-FNB needles from a multicenter study presented in abstract form demonstrated a pathologic diagnostic yield of 87% for pancreatic lesions with a minimum number of passes. A total of 87 lesions were biopsied in 78 patients of which 41 lesions were located in the pancreas. A visible core was present in 95% of pancreatic lesions biopsied (39/41) and a cytologic diagnosis was rendered in 76% (22/29), with a median number of 2 passes for pathology. Two patients experienced adverse events, mild pancreatitis in a patient with a benign pancreatic head mass (sampled with 22-gauge SC-FNB needle), and abdominal pain in a patient with pancreatic head adenocarcinoma (25G SC-FNB needle).[21] Larsen et al. noted the SC-FNB needle provided a core sample for histological evaluation in the majority of cases, with an overall diagnostic accuracy of over 88%.[33] Similar to our study, EUS-FNB was technically feasible in all cases were reported.
In another study, Kandel et al. compared the histological yield of EUS-FNB sampling using the SC-FNB needle to EUS-FNA in patients who had solid pancreatic and nonpancreatic lesions.[34] A total of 156 patients were included in the study, of which 39 patients underwent sampling using the SC-FNB needle and 117 using the standard EUS-FNA needle. Similar to the results of our study, there was a statistically significant difference in median number of passes (SC FNB, 2 passes, vs. EUS-FNA, 4 passes, P = 0.001). Histology yield was also noted to be significantly higher using the SC-FNB needle compared with the EUS-FNA needle (95% vs. 59%, P = 0.01).
A limitation of our study is the limited sample size in the SC-FNB needle group. Additional limitations include its retrospective nature and the inability to blind the endoscopist to the type of needle used. Furthermore, as patients were divided chronologically into two groups according to the period during which the needles were used, it is difficult to account for time-related improvements that may be attributed to an individual endoscopist technique. In addition, there is no standard technique utilizing either the 22-gauge SC-FNB or 22-gauge EUS-FNA needle in published literature, and techniques employed at individual institutions continue to evolve. We also recognize that there is an unequal distribution of the number of patients in the groups. The reason for this is that we had a large existing cohort of patients who had undergone EUS-FNA with the standard needle. The 22-gauge SC-FNB has only been on the market for <2 years, and when we reached a critical threshold of FNB cases, we decided to evaluate the 2 needles. Finally, an added limitation of our study may be that we did not specifically attempt to evaluate the SC device for its ability to provide adequate core biopsy material for histology.
CONCLUSIONS
The SC FNB device is safe and technically feasible for EUS-FNA of solid pancreatic mass lesions. Preliminary results suggest that the SC-FNB has a diagnostic yield similar to the standard EUS needle and on pass per pass basis outperforms the standard EUS needle, making it an attractive alternative for failed EUS-FNA with standard needles. Larger multicenter prospective trials are needed for cost analysis and to evaluate the diagnostic accuracy of the needle in comparison to existing needles.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66:7–30. doi: 10.3322/caac.21332. [DOI] [PubMed] [Google Scholar]
- 2.Yoshinaga S, Suzuki H, Oda I, et al. Role of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) for diagnosis of solid pancreatic masses. Dig Endosc. 2011;23(Suppl 1):29–33. doi: 10.1111/j.1443-1661.2011.01112.x. [DOI] [PubMed] [Google Scholar]
- 3.Itoi T, Sofuni A, Itokawa F, et al. Current status of diagnostic endoscopic ultrasonography in the evaluation of pancreatic mass lesions. Dig Endosc. 2011;23(Suppl 1):17–21. doi: 10.1111/j.1443-1661.2011.01132.x. [DOI] [PubMed] [Google Scholar]
- 4.Eloubeidi MA, Chen VK, Eltoum IA, et al. Endoscopic ultrasound-guided fine needle aspiration biopsy of patients with suspected pancreatic cancer: Diagnostic accuracy and acute and 30-day complications. Am J Gastroenterol. 2003;98:2663–8. doi: 10.1111/j.1572-0241.2003.08666.x. [DOI] [PubMed] [Google Scholar]
- 5.Haba S, Yamao K, Bhatia V, et al. Diagnostic ability and factors affecting accuracy of endoscopic ultrasound-guided fine needle aspiration for pancreatic solid lesions: Japanese large single center experience. J Gastroenterol. 2013;48:973–81. doi: 10.1007/s00535-012-0695-8. [DOI] [PubMed] [Google Scholar]
- 6.Kim J, Ryu JK, Park JM, et al. Clinical factors associated with accuracy of EUS-FNA for pancreatic or peripancreatic solid mass without on-site cytopathologists. J Gastroenterol Hepatol. 2014;29:887–92. doi: 10.1111/jgh.12497. [DOI] [PubMed] [Google Scholar]
- 7.Madhoun MF, Wani SB, Rastogi A, et al. The diagnostic accuracy of 22-gauge and 25-gauge needles in endoscopic ultrasound-guided fine needle aspiration of solid pancreatic lesions: A meta-analysis. Endoscopy. 2013;45:86–92. doi: 10.1055/s-0032-1325992. [DOI] [PubMed] [Google Scholar]
- 8.Song TJ, Kim JH, Lee SS, et al. The prospective randomized, controlled trial of endoscopic ultrasound-guided fine-needle aspiration using 22G and 19G aspiration needles for solid pancreatic or peripancreatic masses. Am J Gastroenterol. 2010;105:1739–45. doi: 10.1038/ajg.2010.108. [DOI] [PubMed] [Google Scholar]
- 9.Erickson RA, Sayage-Rabie L, Beissner RS. Factors predicting the number of EUS-guided fine-needle passes for diagnosis of pancreatic malignancies. Gastrointest Endosc. 2000;51:184–90. doi: 10.1016/s0016-5107(00)70416-0. [DOI] [PubMed] [Google Scholar]
- 10.Matynia AP, Schmidt RL, Barraza G, et al. Impact of rapid on-site evaluation on the adequacy of endoscopic-ultrasound guided fine-needle aspiration of solid pancreatic lesions: A systematic review and meta-analysis. J Gastroenterol Hepatol. 2014;29:697–705. doi: 10.1111/jgh.12431. [DOI] [PubMed] [Google Scholar]
- 11.LeBlanc JK, Ciaccia D, Al-Assi MT, et al. Optimal number of EUS-guided fine needle passes needed to obtain a correct diagnosis. Gastrointest Endosc. 2004;59:475–81. doi: 10.1016/s0016-5107(03)02863-3. [DOI] [PubMed] [Google Scholar]
- 12.Schmidt RL, Walker BS, Howard K, et al. Rapid on-site evaluation reduces needle passes in endoscopic ultrasound-guided fine-needle aspiration for solid pancreatic lesions: A risk-benefit analysis. Dig Dis Sci. 2013;58:3280–6. doi: 10.1007/s10620-013-2750-6. [DOI] [PubMed] [Google Scholar]
- 13.Hébert-Magee S. Is there a role for endoscopic ultrasound-guided fine-needle biopsy in pancreatic cancer? Endoscopy. 2015;47:291–2. doi: 10.1055/s-0034-1391441. [DOI] [PubMed] [Google Scholar]
- 14.Wiersema MJ, Levy MJ, Harewood GC, et al. Initial experience with EUS-guided trucut needle biopsies of perigastric organs. Gastrointest Endosc. 2002;56:275–8. doi: 10.1016/s0016-5107(02)70193-4. [DOI] [PubMed] [Google Scholar]
- 15.Varadarajulu S, Bang JY, Hebert-Magee S. Assessment of the technical performance of the flexible 19-gauge EUS-FNA needle. Gastrointest Endosc. 2012;76:336–43. doi: 10.1016/j.gie.2012.04.455. [DOI] [PubMed] [Google Scholar]
- 16.Iglesias-Garcia J, Poley JW, Larghi A, et al. Feasibility and yield of a new EUS histology needle: Results from a multicenter, pooled, cohort study. Gastrointest Endosc. 2011;73:1189–96. doi: 10.1016/j.gie.2011.01.053. [DOI] [PubMed] [Google Scholar]
- 17.Larghi A, Iglesias-Garcia J, Poley JW, et al. Feasibility and yield of a novel 22-gauge histology EUS needle in patients with pancreatic masses: A multicenter prospective cohort study. Surg Endosc. 2013;27:3733–8. doi: 10.1007/s00464-013-2957-9. [DOI] [PubMed] [Google Scholar]
- 18.Yang Y, Li L, Qu C, et al. Endoscopic ultrasound-guided fine needle core biopsy for the diagnosis of pancreatic malignant lesions: A systematic review and meta-analysis. Sci Rep. 2016;6:22978. doi: 10.1038/srep22978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bang JY, Hawes R, Varadarajulu S. A meta-analysis comparing ProCore and standard fine-needle aspiration needles for endoscopic ultrasound-guided tissue acquisition. Endoscopy. 2016;48:339–49. doi: 10.1055/s-0034-1393354. [DOI] [PubMed] [Google Scholar]
- 20.Jani BS, Rzouq F, Saligram S, et al. Endoscopic ultrasound-guided fine-needle aspiration of pancreatic lesions: A systematic review of technical and procedural variables. N Am J Med Sci. 2016;8:1–11. doi: 10.4103/1947-2714.175185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dimaio CJ, Kolb JM, Benias PC, et al. Initial experience with a novel EUS-guided core biopsy needle (SharkCore): A North American multicenter study. Gastrointest Endosc. 2015;81:AB540. doi: 10.1055/s-0042-112581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin M, Hair CD, Green LK, et al. Endoscopic ultrasound-guided fine-needle aspiration with on-site cytopathology versus core biopsy: A comparison of both techniques performed at the same endoscopic session. Endosc Int Open. 2014;2:E220–3. doi: 10.1055/s-0034-1377611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hawes RH. The evolution of endoscopic ultrasound: Improved imaging, higher accuracy for fine needle aspiration and the reality of endoscopic ultrasound-guided interventions. Curr Opin Gastroenterol. 2010;26:436–44. doi: 10.1097/MOG.0b013e32833d1799. [DOI] [PubMed] [Google Scholar]
- 24.Gleeson FC, Kipp BR, Caudill JL, et al. False positive endoscopic ultrasound fine needle aspiration cytology: Incidence and risk factors. Gut. 2010;59:586–93. doi: 10.1136/gut.2009.187765. [DOI] [PubMed] [Google Scholar]
- 25.Savides TJ, Donohue M, Hunt G, et al. EUS-guided FNA diagnostic yield of malignancy in solid pancreatic masses: A benchmark for quality performance measurement. Gastrointest Endosc. 2007;66:277–82. doi: 10.1016/j.gie.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 26.Eloubeidi MA, Varadarajulu S, Desai S, et al. Aprospective evaluation of an algorithm incorporating routine preoperative endoscopic ultrasound-guided fine needle aspiration in suspected pancreatic cancer. J Gastrointest Surg. 2007;11:813–9. doi: 10.1007/s11605-007-0151-x. [DOI] [PubMed] [Google Scholar]
- 27.Turner BG, Cizginer S, Agarwal D, et al. Diagnosis of pancreatic neoplasia with EUS and FNA: A report of accuracy. Gastrointest Endosc. 2010;71:91–8. doi: 10.1016/j.gie.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 28.Sakamoto H, Kitano M, Komaki T, et al. Prospective comparative study of the EUS guided 25-gauge FNA needle with the 19-gauge Trucut needle and 22-gauge FNA needle in patients with solid pancreatic masses. J Gastroenterol Hepatol. 2009;24:384–90. doi: 10.1111/j.1440-1746.2008.05636.x. [DOI] [PubMed] [Google Scholar]
- 29.Wittmann J, Kocjan G, Sgouros SN, et al. Endoscopic ultrasound-guided tissue sampling by combined fine needle aspiration and trucut needle biopsy: A prospective study. Cytopathology. 2006;17:27–33. doi: 10.1111/j.1365-2303.2006.00313.x. [DOI] [PubMed] [Google Scholar]
- 30.Levy MJ, Wiersema MJ. EUS-guided Trucut biopsy. Gastrointest Endosc. 2005;62:417–26. doi: 10.1016/j.gie.2005.04.044. [DOI] [PubMed] [Google Scholar]
- 31.Witt BL, Adler DG, Hilden K, et al. A comparative needle study: EUS-FNA procedures using the HD ProCore(™) and EchoTip(®) 22-gauge needle types. Diagn Cytopathol. 2013;41:1069–74. doi: 10.1002/dc.22971. [DOI] [PubMed] [Google Scholar]
- 32.Korenblit J, Singh H, Butt M, et al. 1018 prospective randomized trial of the 22G EchoTip ProCore needle versus the 22G cook echotip ultra needle in patients with solid mass lesions undergoing EUS-guided fine needle aspiration (FNA) Gastrointest Endosc. 2013;77:AB178. [Google Scholar]
- 33.Larsen CF, Pless T, Ainsworth A, et al. Euro EUS 2016. Marseille, France: 2016. Feasibility, Yield and Safety of a New EUS – Fine-Needle Biopsy Device (SharkCore): Results from a Single Center Study. [Google Scholar]
- 34.Kandel P, Tranesh G, Nassar A, et al. EUS-guided fine needle biopsy sampling using a novel fork-tip needle: A case-control study. Gastrointest Endosc. 2016;84:1034–9. doi: 10.1016/j.gie.2016.03.1405. [DOI] [PubMed] [Google Scholar]


