Abstract
Context
Japanese women have substantially lower body mass index (BMI) than women in other developed countries. The BMI of Japanese women has steadily decreased over time. However, glucose metabolism in underweight Japanese women has not been fully characterized.
Objective
The aim of this study was to investigate glucose metabolism and the physical characteristics of underweight Japanese women.
Design and Participants
We recruited 31 young (20 to 29 years of age) and 30 postmenopausal (50 to 65 years of age) underweight women. We also recruited young normal-weight women (n = 13) and postmenopausal normal-weight women (n = 10) to serve as references. We administered an oral glucose tolerance test (OGTT) and evaluated intramyocellular lipid (IMCL) levels and body composition using 1H-magnetic resonance spectroscopy and dual-energy X-ray absorptiometry, respectively.
Results
Young underweight women had similar glucose tolerance as young normal-weight women. However, postmenopausal underweight women had a higher area under the curve (AUC) for glucose during OGTT than postmenopausal normal-weight women. In postmenopausal underweight women, 2-hour glucose levels during OGTT were negatively correlated with lean body mass (r = −0.55, P < 0.01) and insulinogenic index (r = −0.42, P = 0.02) and were positively correlated with IMCL levels (r = 0.40, P = 0.03). Compared with young underweight women, postmenopausal underweight women had a higher AUC for glucose during OGTT and a lower insulinogenic index and AUC for insulin during OGTT.
Conclusions
Postmenopausal underweight women had more impaired glucose tolerance than young underweight women. In postmenopausal underweight women, the degree of glucose tolerance impairment was associated with decreased lean body mass, increased IMCL accumulation, and impaired insulin secretion.
Keywords: impaired glucose tolerance, intramyocellular lipid, lean body mass, underweight
In underweight Japanese women, worsening glucose tolerance was observed after menopause. The degree of glucose intolerance is associated with decreased muscle mass/quality and insulin secretion.
Japanese women have substantially lower body mass index (BMI) than women in other developed countries [1, 2], and their BMI has steadily decreased over time [3, 4]. For example, the mean BMI of Japanese women aged 25 to 29 years is 21.25 kg/m2. The prevalence of underweight was 13.5% in 1976 through the 1980s; however, from 1996 to the 2000s, mean BMI decreased to 20.57 kg/m2, and 23.7% were underweight [4]. In addition, the BMI of Japanese women in their 30s to 60s steadily decreased over this period. However, in Japanese men in each age group, mean BMI steadily increased [3, 5]. Currently, Japan has the second highest prevalence of underweight women among developed countries, similar to the prevalence of underweight women in developing countries [1, 2, 6]. Accordingly, the number of underweight women in Japan is not too small to be ignored.
The increased number of underweight young women in Japan might be related to their desire to be thin. The mean caloric intake in young women in Japan is very low [3, 7]. On the other hand, their physical activity levels do not tend to be high [3]. Lower muscle function or volume could be anticipated in this population, which might elicit abnormalities in glucose metabolism. Indeed, some epidemiological data suggest that underweight as well as overweight might be associated with the incidence of diabetes in the Japanese population [8–10]. However, glucose metabolism in underweight Japanese women has not been fully characterized.
The current study was designed to investigate glucose metabolism in underweight Japanese women. Because the proportion of underweight women is highest among women in their 20s and because the risk of type 2 diabetes increases after menopause [11, 12], we recruited underweight women in their 20s and postmenopausal women as subjects. We also recruited normal-weight women in each category to serve as a reference group. We administered the oral glucose tolerance test (OGTT) and evaluated glucose tolerance and related muscle and metabolic parameters.
1. Research Design and Methods
A. Subjects
In this study, we recruited young and postmenopausal underweight women with BMI ranging from ≥16.0 to <18.5 kg/m2 and normal-weight women with BMI ranging from ≥18.5 to <23.0 kg/m2 through two outsourcing companies (Clinical Trial, Tokyo, Japan, and SOUKEN, Tokyo, Japan). We excluded patients with diabetes, hypertension, dyslipidemia, hyperthyroidism, surgical menopause, multiparity for young women, and any chronic diseases. We also excluded subjects taking medicines or supplements that might affect metabolism and subjects with suspected anorexia nervosa based on the Eating Attitude Test (EAT-26, Japanese version) [13].
We recruited approximately 30 underweight subjects in both age categories and 10 normal-weight women to serve as a reference group. We stopped enrolling subjects when these numbers were achieved. From October 2015 to September 2016, 60 young women and 54 postmenopausal women participated in the screening session. Among screened women, 16 young and 14 postmenopausal women were excluded; six young and seven postmenopausal women did not meet the inclusion criteria, and the remaining subjects could not participate in further examinations due to scheduling conflicts. Thus, full analysis was conducted using data from 84 subjects (Table 1). All participants gave written informed consent, and the study was approved by the ethics committee of Juntendo University. This study was carried out in accordance with the principles outlined in the Declaration of Helsinki.
Table 1.
Characteristics and Glucose Metabolism Parameters in Young Women and Postmenopausal Women
| Young Women |
Postmenopausal Women |
P
a
|
|||
|---|---|---|---|---|---|
| Underweight (n = 31) | Normal Weight (n = 13) | Underweight (n = 30) | Normal Weight (n = 10) | ||
| Age, y | 24.7 ± 2.7b | 25.2 ± 3.4 | 56.2 ± 3.3 | 56.8 ± 5.4 | <0.01 |
| Menstruation cycle, d | 5.6 ± 1.4 | 4.6 ± 1.4 | |||
| Years since menopause | 5.8 ± 3.9 | 5.7 ± 4.3 | |||
| Height, cm | 159.5 ± 4.5 | 159.9 ± 6.3 | 157.7 ± 5.7 | 155.0 ± 4.3 | 0.16 |
| Body weight, kg | 45.2 ± 4.1 | 53.0 ± 4.8 | 43.8 ± 3.6 | 49.9 ± 3.0 | 0.18 |
| Peak body weight, kg | 49.8 ± 4.3 | 55.6 ± 5.0 | |||
| Age at peak body weight, y | 27.6 ± 12.0 | 34.4 ± 5.2 | |||
| Minimum body weight, kg | 41.1 ± 3.9 | 44.0 ± 3.7 | |||
| Age at minimum body weight, year | 41.7 ± 13.4 | 31.8 ± 14.9 | |||
| BMI, kg/m2 | 17.4 ± 0.9 | 20.4 ± 1.2 | 17.1 ± 0.7 | 20.3 ± 1.0 | 0.29 |
| Total body fat mass, kg | 9.7 ± 2.2 | 12.4 ± 2.6 | 8.6 ± 2.1 | 12.5 ± 2.6 | 0.06 |
| Total body fat content, % | 21.3 ± 3.9 | 23.5 ± 4.5 | 19.7 ± 4.9 | 25.2 ± 4.9 | 0.16 |
| Lean body mass, kg | 33.6 ± 3.0 | 38.4 ± 4.4 | 33.5 ± 3.6 | 35.5 ± 3.0 | 0.95 |
| Appendicular lean body mass, kg | 14.0 ± 1.6 | 16.2 ± 2.6 | 14.0 ± 2.0 | 14.8 ± 2.2 | 0.98 |
| Skeletal muscle mass index, kg/m2 | 5.5 ± 0.5 | 6.4 ± 0.9 | 5.6 ± 0.6 | 6.2 ± 0.7 | 0.39 |
| Triglycerides, mg/dL | 50.5 ± 16.4 | 52.5 ± 21.4 | 59.5 ± 22.2 | 78.9 ± 28.7 | 0.08 |
| Fasting plasma glucose, mg/dL | 85.4 ± 6.0 | 86.0 ± 6.8 | 90.9 ± 6.2 | 93.2 ± 11.2 | <0.01 |
| Fasting plasma insulin, μU/mL | 3.6 ± 1.2 | 4.1 ± 1.8 | 3.4 ± 1.3 | 4.5 ± 1.7 | 0.54 |
| Insulinogenic index | 0.9 ± 0.6 | 1.0 ± 0.7 | 0.6 ± 0.6 | 0.4 ± 0.2 | 0.04 |
| AUC for glucose during OGTT, mg/min/dL × 103 | 14.0 ± 2.3 | 13.8 ± 2.5 | 16.2 ± 3.0 | 14.7 ± 1.1 | <0.01 |
| AUC for insulin during OGTT, μU/min/mL × 103 | 5.1 ± 3.1 | 4.2 ± 1.5 | 3.2 ± 0.9 | 3.2 ± 1.4 | <0.01 |
| Impaired glucose tolerance, n (%) | 4 (12.9) | 2 (15.4) | 11 (36.7) | 0 (0.0) | 0.03 |
| Impaired fasting glycemia, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | - |
| HbA1c, % | 5.2 ± 0.2 | 5.1 ± 0.3 | 5.5 ± 0.3 | 5.6 ± 0.2 | <0.01 |
| Total cholesterol, mg/dL | 170.6 ± 29.3 | 168.5 ± 25.2 | 213.8 ± 30.6 | 219.8 ± 33.4 | <0.01 |
| HDL cholesterol, mg/dL | 68.4 ± 12.5 | 63.6 ± 9.2 | 77.0 ± 13.4 | 75.5 ± 12.8 | 0.01 |
| LDL cholesterol, mg/dL | 94.0 ± 24.7 | 95.5 ± 29.5 | 124.6 ± 28.0 | 129.0 ± 37.0 | <0.01 |
| Aspartate aminotransferase, IU/L | 18.4 ± 5.3 | 16.8 ± 2.2 | 20.3 ± 4.1 | 20.9 ± 3.7 | 0.11 |
| Alanine aminotransferase, IU/L | 15.3 ± 9.7 | 12.4 ± 4.1 | 14.1 ± 5.2 | 16.0 ± 2.7 | 0.54 |
| TA IMCL, S-fat/Cre | 2.9 ± 1.3 | 2.9 ± 1.9 | 2.5 ± 1.1 | 3.7 ± 2.6 | 0.30 |
| SOL IMCL, S-fat/Cre | 6.5 ± 2.4 | 7.4 ± 1.1 | 6.8 ± 3.6 | 4.7 ± 2.1 | 0.68 |
| Intrahepatic lipid, % | 0.3 ± 0.6 | 0.3 ± 0.5 | 0.8 ± 2.0 | 0.5 ± 1.2 | 0.19 |
| Physical activity, METs/h/d | 2.4 ± 1.2 | 3.2 ± 1.1 | 2.6 ± 1.4 | 2.9 ± 0.9 | 0.67 |
| VO2peak, mL/kg/min | 32.6 ± 3.9 | 32.0 ± 4.1 | 33.3 ± 3.8 | 28.2 ± 5.2 | 0.53 |
| Isokinetic strength, Nm/kg | 176.9 ± 31.9 | 159.6 ± 22.9 | 161.0 ± 22.3 | 157.2 ± 24.9 | 0.03 |
| Hand grip strength, kg | 23.2 ± 4.9 | 24.6 ± 4.3 | 23.2 ± 3.5 | 23.8 ± 4.8 | 0.99 |
| Dietary intake, kcal | 1442.2 ± 439.1 | 1722.4 ± 309.6 | 1904.3 ± 482.2 | 1899.0 ± 429.8 | <0.01 |
| Protein intake, g | 53.3 ± 17.9 | 63.6 ± 14.4 | 67.4 ± 16.5 | 73.7 ± 12.5 | <0.01 |
| Fat intake, g | 53.6 ± 18.9 | 64.8 ± 16.6 | 68.6 ± 25.3 | 73.1 ± 24.2 | <0.01 |
| Carbohydrate intake, g | 180.6 ± 56.8 | 213.3 ± 49.8 | 238.0 ± 58.2 | 224.7 ± 45.8 | <0.01 |
Abbreviations: Cre, creatine; HbA1c, hemoglobin A1c; LDL, low-density lipoprotein; SOL, soleus; VO2peak, peak oxygen consumption.
P value for difference between young underweight women and postmenopausal underweight women. Boldface P values: P < 0.05.
Data are means ± SD and number (%).
B. Study Design
All participants underwent a full day of examinations after overnight fasting. On the experimental day, we measured intramyocellular lipid (IMCL) and intrahepatic lipid (IHL) levels using 1H-magnetic resonance spectroscopy (MRS). Total body fat mass and lean body mass were measured using dual-energy X-ray absorptiometry (DXA). The subjects underwent OGTT, and isokinetic strength of the quadriceps and peak oxygen consumption were evaluated using a dynamometer and cycle ergometer, respectively. In young women, these tests were performed during the early follicular phase. Energy intake and dietary composition were evaluated using a 3-day dietary log. The mean physical activity level was estimated over 7 days with an accelerometer before or after the experimental day (Lifecorder; Suzuken, Nagoya, Japan) [14, 15].
C. 1H-MRS
IMCL levels in the right tibialis anterior (TA) and soleus muscles were measured using 1H-MRS (VISART EX V4.40; Toshiba, Tokyo, Japan) as previously described [16, 17]. After the examination, IMCL was quantified based on the methylene signal intensity (S-fat), with the creatine signal as the reference. An S-fat/creatinine ratio was calculated. IHL was quantified by S-fat and H2O as the internal reference. IHL was calculated as H2O + S-fat [S-fat × 100/(H2O + S-fat)] (%) [16, 17].
D. DXA
Body composition, including fat mass and nonbone lean mass, was evaluated using DXA (Hologic Discovery-A; Hologic, Inc., Bedford, MA) [18]. After the DXA examination, the skeletal muscle mass index was calculated by dividing appendicular muscle mass (kg) by height in meters squared [19].
E. OGTT
Subjects underwent a standard 75 g OGTT [20]. Blood samples were obtained before and 30, 60, 90, and 120 minutes after ingesting 75 g of glucose to determine plasma glucose and serum insulin levels. Impaired glucose tolerance (IGT) was defined as a 2-hour glucose level ≥140 mg/dL according to World Health Organization criteria. The insulinogenic index was calculated using the following equation: (insulin at 30 min − fasting insulin)/(plasma glucose at 30 min − fasting plasma glucose) [21–23].
F. Measurements of Isokinetic Muscle Strength and Fitness Level
Quadricep isokinetic strength was measured using a dynamometer (Biodex System 3; Biodex Medical Systems, Upton, NY). Isokinetic strength was measured for knee extension (angular velocity of 60°/s). Leg extension power was calculated by dividing isokinetic strength by body weight [24, 25]. Hand grip strength was measured using a hand grip dynamometer (Takei Digital Grip Strength Dynamometer; Takei Scientific Instruments Co., Ltd, Tokyo, Japan). Maximum oxygen uptake was estimated with incremental exercise testing involving a cycle ergometer (AEROBIKE 75XL; COMBI, Tokyo, Japan) [26].
G. Statistical Analysis
All values are expressed as means ± SD or number (%). We analyzed the correlation between 2-hour glucose levels during OGTT and characteristics of underweight women in each group using Pearson correlation coefficients. Multiple linear regression was used to identify independent determinants of 2-hour glucose levels during OGTT. We compared young underweight women with postmenopausal underweight women using the unpaired t test, Mann-Whitney U test, or χ2 test as appropriate. All statistical tests were two-sided with a 5% significance level. SPSS version 23 (SPSS Statistics; IBM, Tokyo, Japan) was used for statistical analysis.
2. Results
A. Characteristics and Glucose Metabolism Parameters in Underweight Young and Postmenopausal Women
Among young women, underweight subjects had lower dietary intake and physical activity levels than normal-weight subjects (Table 1). Among postmenopausal women, underweight and normal-weight subjects had similar dietary intake and physical activity levels. Among young women, underweight subjects weighed on average 7.8 kg less than normal-weight subjects despite being of similar height. This difference was mostly due to lower body fat mass (2.7 kg) and lower lean body mass (4.8 kg). In contrast, among postmenopausal women, underweight subjects weighed on average 6.1 kg less than normal-weight subjects despite being of similar height. This difference was mostly due to lower body fat mass (3.9 kg) and lower lean body mass (2.0 kg). Thus, lower body weight in young underweight women was likely due to lower lean body mass rather than lower fat mass, whereas in postmenopausal women lower body weight was likely due to lower body fat mass rather than lower muscle mass.
Self-reported peak body weight and BMI values of postmenopausal underweight women were 49.8 ± 4.3 kg and 20.1 ± 1.8 kg/m2, respectively, at 27.6 ± 12.0 years of age. In addition, 23 of 30 (76.7%) postmenopausal underweight women were of normal weight during their period of peak body weight. Minimum body weight (41.1 ± 3.9 kg) occurred at 41.7 ± 13.4 years of age in postmenopausal underweight women. These data suggested that ~80% of postmenopausal women in the study who are currently underweight were normal-weight around 30 years of age and became underweight later.
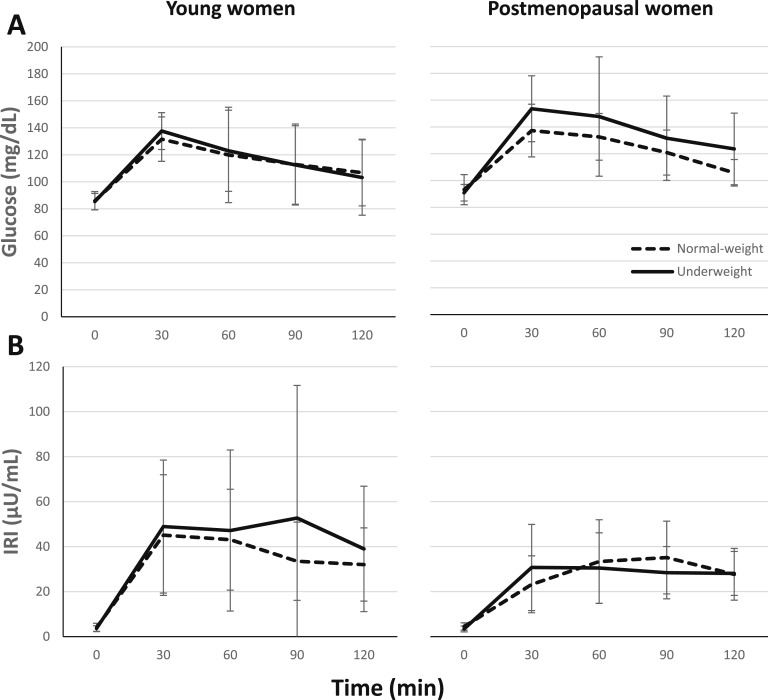
None of the subjects in either group had impaired fasting glucose (Table 1). On the other hand, whereas the prevalence of IGT in young normal-weight women was 15% (2/13) and 13% (4/31) in young underweight women, the prevalence of IGT was 0% (0/10) in postmenopausal normal-weight women and 37% (11/30) in postmenopausal underweight women. Similarly, although the area under the curve (AUC) for glucose during OGTT was similar between young underweight and normal-weight women, it was higher in postmenopausal underweight women than in postmenopausal normal-weight women (Table 1, Fig. 1A). On the other hand, the AUC for insulin during OGTT was similar in both age groups (Table 1, Fig. 1B).
Figure 1.
Glucose (A) and insulin (B) levels during an oral glucose tolerance test in young and postmenopausal women. IRI, immunoreactive insulin.
B. Factors Associated With 2-Hour Glucose Levels During OGTT in Underweight Women
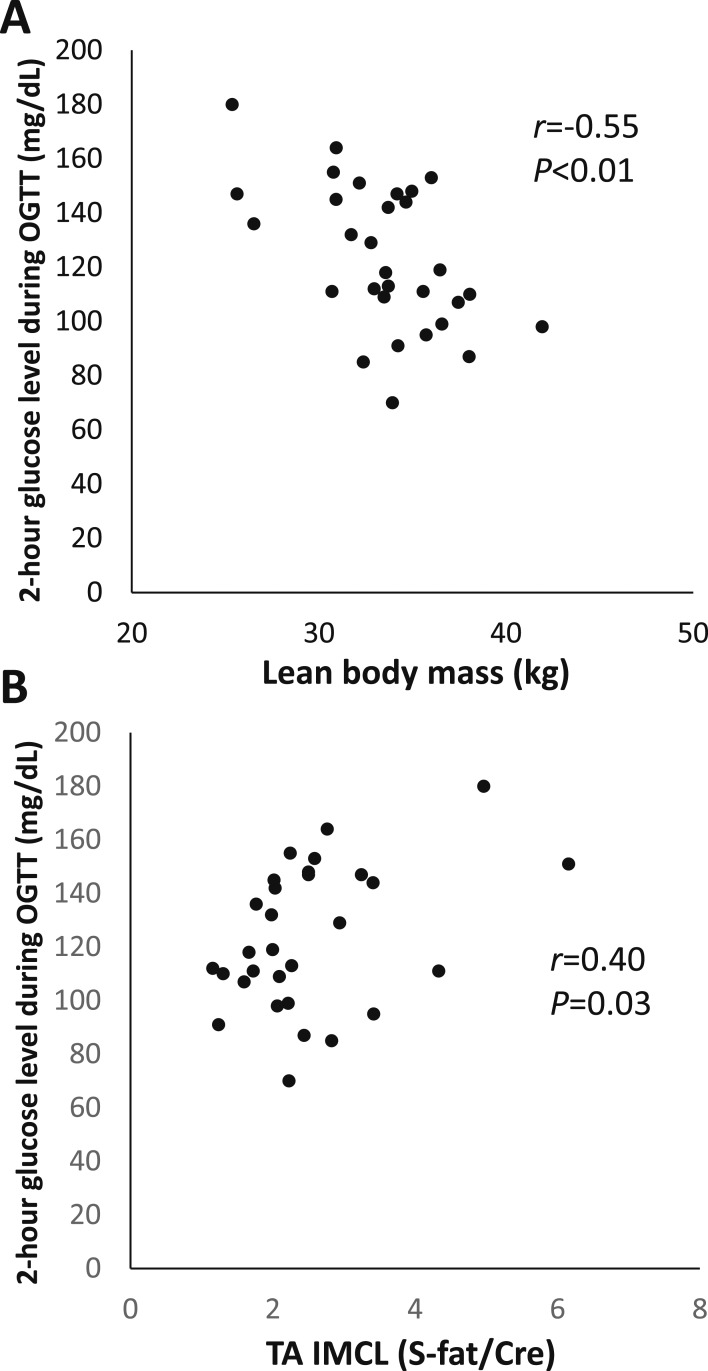
We investigated the correlation between characteristics of underweight women and 2-hour glucose levels during OGTT. In young underweight women, insulinogenic index and high-density lipoprotein (HDL) cholesterol were negatively correlated, and AUC for glucose during OGTT was positively correlated with 2-hour glucose levels during OGTT (Table 2). In postmenopausal underweight women, height, body weight, lean body mass, insulinogenic index, and hemoglobin A1c were negatively correlated, and AUC for glucose during OGTT and TA IMCL levels were positively correlated with 2-hour glucose levels during OGTT (Table 2, Fig. 2).
Table 2.
Results of Correlation Analysis Between 2-Hour Glucose Level During OGTT and Each Parameter in Underweight Women
| Characteristic | Young Women |
Postmenopausal Women |
||
|---|---|---|---|---|
| r a | P | r | P | |
| Age, y | −0.20 | 0.28 | 0.27 | 0.15 |
| Years since menopause | 0.08 | 0.67 | 0.24 | 0.20 |
| Height, cm | 0.19 | 0.30 | −0.54 | <0.01 |
| Body weight, kg | 0.10 | 0.60 | −0.62 | <0.01 |
| BMI, kg/m2 | −0.04 | 0.84 | −0.35 | 0.06 |
| Total body fat mass, kg | 0.11 | 0.57 | −0.12 | 0.54 |
| Total body fat content, % | 0.03 | 0.86 | 0.11 | 0.56 |
| Lean body mass, kg | 0.06 | 0.74 | −0.55 | <0.01 |
| Appendicular lean body mass, kg | −0.09 | 0.62 | −0.51 | <0.01 |
| Skeletal muscle mass index, kg/m2 | −0.22 | 0.23 | −0.35 | 0.06 |
| Fasting plasma glucose, mg/dL | 0.12 | 0.51 | 0.04 | 0.84 |
| Fasting plasma insulin, μU/mL | 0.05 | 0.80 | 0.27 | 0.15 |
| Insulinogenic index | −0.40 | 0.02 | −0.42 | 0.02 |
| AUC glucose during OGTT, mg/min/dL × 103 | 0.79 | <0.01 | 0.75 | <0.01 |
| AUC insulin during OGTT, μU/min/mL × 103 | −0.09 | 0.62 | −0.13 | 0.50 |
| HbA1c, % | 0.29 | 0.11 | −0.46 | 0.01 |
| Triglycerides, mg/dL | −0.05 | 0.81 | −0.30 | 0.11 |
| Total cholesterol, mg/dL | −0.24 | 0.19 | −0.20 | 0.30 |
| HDL cholesterol, mg/dL | −0.46 | <0.01 | 0.08 | 0.68 |
| LDL cholesterol, mg/dL | −0.04 | 0.82 | −0.22 | 0.24 |
| Aspartate aminotransferase, IU/L | 0.18 | 0.34 | 0.20 | 0.29 |
| Alanine aminotransferase, IU/L | 0.29 | 0.11 | 0.07 | 0.73 |
| TA IMCL, S-fat/Cre | 0.01 | 0.95 | 0.40 | 0.03 |
| SOL IMCL, S-fat/Cre | 0.03 | 0.90 | 0.19 | 0.32 |
| Intrahepatic lipid, % | −0.23 | 0.25 | 0.06 | 0.75 |
| Bone mineral density, kg/cm2 | −0.04 | 0.82 | −0.05 | 0.81 |
| Physical activity, METs/h/d | −0.09 | 0.65 | 0.08 | 0.68 |
| VO2peak, mL/kg/min | −0.34 | 0.06 | 0.27 | 0.18 |
| Isokinetic strength, Nm/kg | −0.01 | 0.96 | 0.06 | 0.77 |
| Hand grip strength, kg | 0.16 | 0.44 | −0.15 | 0.44 |
| Dietary intake, kcal | −0.07 | 0.73 | −0.02 | 0.93 |
| Protein intake, g | −0.10 | 0.62 | −0.08 | 0.69 |
| Fat intake, g | −0.01 | 0.96 | −0.02 | 0.93 |
| Carbohydrate intake, g | −0.09 | 0.68 | 0.05 | 0.78 |
Abbreviations: Cre, creatine; HbA1c, hemoglobin A1c; LDL, low-density lipoprotein; MET, metabolic equivalent; SOL, soleus; VO2peak, peak oxygen consumption.
Correlation analysis was performed with Pearson correlation coefficients. Boldface r and P values: P < 0.05.
Figure 2.
Correlation between 2-hour glucose levels during OGTT and lean body mass (A) and IMCL (B) levels in underweight postmenopausal women.
We investigated independent determinants of 2-hour glucose levels in underweight women using multiple linear regression. Given the small number of study subjects, we included a limited number of covariates in the multiple regression analysis: insulinogenic index and HDL cholesterol for young women and lean body mass, TA IMCL, and insulinogenic index for postmenopausal women. Lean body mass (β = −0.43, P < 0.01), TA IMCL levels (β = 0.30; P = 0.05), and insulinogenic index (β = −0.43, P < 0.01) were identified as independent determinants of 2-hour glucose levels in postmenopausal underweight women, whereas only HDL cholesterol was significant in young underweight women (HDL cholesterol: β = −0.37, P = 0.04; insulinogenic index: β = −0.28, P = 0.11).
C. Comparison Between Underweight Young and Postmenopausal Women
Postmenopausal underweight women had higher AUC for glucose during OGTT and a higher prevalence of IGT compared with young underweight women (Table 1). Although 2-hour glucose levels during OGTT were associated with decreased lean body mass and increased IMCL in postmenopausal underweight women (Table 2), these parameters were comparable between postmenopausal and young underweight women (Table 1). Thus, to investigate why postmenopausal underweight women had worse glucose metabolism than young underweight women, we compared other metabolic factors of the two groups. Compared with young underweight women, in addition to higher fasting glucose, hemoglobin A1c, and AUC for glucose during OGTT, postmenopausal underweight women had lower insulinogenic index and AUC for insulin during OGTT (Table 1).
3. Discussion
In the current study, young underweight women had similar glucose tolerance as young normal-weight women. However, postmenopausal underweight women seemed to have elevated AUC for glucose during OGTT compared with their normal-weight counterparts. In postmenopausal underweight women, worsening of glucose tolerance is associated with lower lean body mass and insulinogenic index and higher TA IMCL. Compared with young underweight women, postmenopausal underweight women had impaired glucose tolerance and lower insulinogenic index and AUC for insulin during OGTT.
In this study, based on simple numerical comparisons, we found a higher prevalence of IGT (37%) among postmenopausal underweight women than among postmenopausal normal-weight women. A previous study demonstrated that the prevalence of IGT in Japanese women aged between 55 to 64 years was 16.7% [27]. Thus, the prevalence of IGT in postmenopausal underweight women seemed to be relatively higher than in the age- and sex-matched general population. Because some epidemiological data suggest that being underweight as well as being overweight might be associated with the incidence of diabetes in the Japanese population [8–10], it is not surprising that the prevalence of IGT in postmenopausal underweight women is higher than that in postmenopausal normal-weight women. However, because the current study is a pilot study with a small number of subjects, further study is required to clarify the prevalence of IGT in underweight women.
Deterioration of glucose tolerance with aging is partly due to decreased insulin secretion [28–31]. Indeed, the capacity for insulin secretion among nondiabetic individuals in their 80s is expected to be 75% of the capacity of those in their 20s [29]. We consistently observed that underweight postmenopausal women had a lower insulinogenic index and AUC for insulin during OGTT compared with underweight young women. In addition, 2-hour glucose levels during OGTT were significantly correlated with insulinogenic index in postmenopausal underweight subjects. Thus, impaired insulin secretion seems to be an important factor in the deterioration of glucose tolerance in postmenopausal underweight women.
We found that lower lean body mass was associated with higher 2-hour glucose levels during OGTT in postmenopausal underweight women. Lean body mass, also called metabolic body size, reflects muscle volume [32]. Skeletal muscle is one of the main glucose-consuming organs during OGTT [33]. Thus, smaller metabolic body size in underweight subjects may be a risk factor for hyperglycemia. In fact, lower muscle mass has been consistently associated with impaired glucose tolerance [34–37]. These data suggest that lower lean body mass might contribute to hyperglycemia in postmenopausal underweight women. In addition, self-reported weight data demonstrated that most postmenopausal underweight women in this study were previously of normal weight and that their body weight decreased with age, suggesting that the progression of muscle loss might contribute to IGT in postmenopausal underweight women.
We also observed that IMCL levels in postmenopausal underweight women were positively correlated with 2-hour glucose levels during OGTT, but this effect was not seen in young underweight women. IMCL accumulation has been demonstrated to cause insulin resistance in nonobese subjects [38, 39]. In addition, myotubes collected from postmenopausal women are more susceptible to developing lipid accumulation and defective insulin signaling after chronic saturated fatty acid exposure than myotubes collected from premenopausal women [40]. However, we did not directly measure insulin sensitivity using a hyperinsulinemic euglycemic clamp, which is the gold standard for evaluating insulin sensitivity. Thus, additional studies to detect subtle differences in muscle insulin sensitivity are required to clarify the role of IMCL in impaired glucose metabolism in this population.
This study has several limitations. The first limitation is the small number of subjects. However, this study was designed as a pilot study; taking this context into consideration, the number of the recruited subjects was reasonable. Second, we used the results of a single OGTT and did not confirm the reproducibility of OGTT in underweight women. Finally, we used a cross-sectional study design. Interventional studies are required to confirm the direction of causality for the parameters identified in the current study.
In summary, among underweight Japanese women, lower glucose tolerance was observed in postmenopausal subjects compared with young subjects. The degree of IGT observed in postmenopausal underweight women was associated with lower lean body weight, higher IMCL, and impaired insulin secretion.
Acknowledgments
We thank Miyuki Iwagami, Naoko Daimaru, Hiroko Hibino, Mitsuko Isoe, and Eriko Magoshi for excellent technical assistance.
Financial Support: This work was supported by a Strategic Research Foundation at Private Universities (to R.K.); by KAKENHI (Grant-in-Aid for Scientific Research 17K01868) from the Ministry of Education, Culture, Sports, Science and Technology of Japan (to J.S.); and by a grant from the Society for Women's Health Science Research (to Y.S.).
Disclosure Summary: The authors have nothing to disclose.
Glossary
Abbreviations:
- AUC
area under the curve
- BMI
body mass index
- DXA
dual-energy X-ray absorptiometry
- HDL
high-density lipoprotein
- IGT
impaired glucose tolerance
- IHL
intrahepatic lipid
- IMCL
intramyocellular lipid
- MRS
magnetic resonance spectroscopy
- OGTT
oral glucose tolerance test
- S-fat
methylene signal intensity
- TA
tibialis anterior
References and Notes
- 1.WHO Global database on body mass index. World Health Organization. 2017. Accessed 23 August 2017. http://apps.who.int/bmi/index.jsp.
- 2. Sugawara A, Saito K, Sato M, Kodama S, Sone H. Thinness in Japanese young women. Epidemiology. 2009;20(3):464–465. [DOI] [PubMed] [Google Scholar]
- 3.The National Health and Nutrition Survey. Ministry of Health, Labour and Welfare. 2016. Accessed 23 August 2017. http://www.nibiohn.go.jp/eiken/english/research/project_nhns.html.
- 4. Takimoto H, Yoshiike N, Kaneda F, Yoshita K. Thinness among young Japanese women. Am J Public Health. 2004;94(9):1592–1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Funatogawa I, Funatogawa T, Nakao M, Karita K, Yano E. Changes in body mass index by birth cohort in Japanese adults: results from the National Nutrition Survey of Japan 1956-2005. Int J Epidemiol. 2009;38(1):83–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Madanat HN, Lindsay R, Hawks SR, Ding D. A comparative study of the culture of thinness and nutrition transition in university females in four countries. Asia Pac J Clin Nutr. 2011;20(1):102–108. [PubMed] [Google Scholar]
- 7. Okubo H, Sasaki S. Underreporting of energy intake among Japanese women aged 18-20 years and its association with reported nutrient and food group intakes. Public Health Nutr. 2004;7(7):911–917. [DOI] [PubMed] [Google Scholar]
- 8. Sairenchi T, Iso H, Irie F, Fukasawa N, Ota H, Muto T. Underweight as a predictor of diabetes in older adults: a large cohort study. Diabetes Care. 2008;31(3):583–584. [DOI] [PubMed] [Google Scholar]
- 9. Tsugane S, Sasaki S, Tsubono Y.. Under- and overweight impact on mortality among middle-aged Japanese men and women: a 10-y follow-up of JPHC study cohort I. Int J Obes Relat Metab Disord. 2002;26:529–537. [DOI] [PubMed] [Google Scholar]
- 10. Tatsumi Y, Ohno Y, Morimoto A, Nishigaki Y, Maejima F, Mizuno S, Watanabe S. U-shaped relationship between body mass index and incidence of diabetes. Diabetol Int. 2012;3(2):92–98. [Google Scholar]
- 11. Heianza Y, Arase Y, Kodama S, Hsieh SD, Tsuji H, Saito K, Shimano H, Hara S, Sone H. Effect of postmenopausal status and age at menopause on type 2 diabetes and prediabetes in Japanese individuals: Toranomon Hospital Health Management Center Study 17 (TOPICS 17). Diabetes Care. 2013;36(12):4007–4014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Szmuilowicz ED, Stuenkel CA, Seely EW. Influence of menopause on diabetes and diabetes risk. Nat Rev Endocrinol. 2009;5(10):553–558. [DOI] [PubMed] [Google Scholar]
- 13. Ujiie T, Kono M. Eating attitudes test in Japan. Jpn J Psychiatry Neurol. 1994;48(3):557–565. [DOI] [PubMed] [Google Scholar]
- 14. Togo F, Watanabe E, Park H, Yasunaga A, Park S, Shephard RJ, Aoyagi Y. How many days of pedometer use predict the annual activity of the elderly reliably? Med Sci Sports Exerc. 2008;40(6):1058–1064. [DOI] [PubMed] [Google Scholar]
- 15. Abel M, Hannon J, Lillie T, Sell K, Anderson D, Conlin G. Comparison of Kenz Lifecorder versus actigraph physical activity output in free-living conditions. J Phys Act Health. 2009;6(Suppl 1)S141–S147. [DOI] [PubMed] [Google Scholar]
- 16. Tamura Y, Tanaka Y, Sato F, Choi JB, Watada H, Niwa M, Kinoshita J, Ooka A, Kumashiro N, Igarashi Y, Kyogoku S, Maehara T, Kawasumi M, Hirose T, Kawamori R. Effects of diet and exercise on muscle and liver intracellular lipid contents and insulin sensitivity in type 2 diabetic patients. J Clin Endocrinol Metab. 2005;90(6):3191–3196. [DOI] [PubMed] [Google Scholar]
- 17. Sato F, Tamura Y, Watada H, Kumashiro N, Igarashi Y, Uchino H, Maehara T, Kyogoku S, Sunayama S, Sato H, Hirose T, Tanaka Y, Kawamori R. Effects of diet-induced moderate weight reduction on intrahepatic and intramyocellular triglycerides and glucose metabolism in obese subjects. J Clin Endocrinol Metab. 2007;92(8):3326–3329. [DOI] [PubMed] [Google Scholar]
- 18. Bazzocchi A, Ponti F, Albisinni U, Battista G, Guglielmi G. DXA: technical aspects and application. Eur J Radiol. 2016;85(8):1481–1492. [DOI] [PubMed] [Google Scholar]
- 19. Sanada K, Miyachi M, Tanimoto M, Yamamoto K, Murakami H, Okumura S, Gando Y, Suzuki K, Tabata I, Higuchi M. A cross-sectional study of sarcopenia in Japanese men and women: reference values and association with cardiovascular risk factors. Eur J Appl Physiol. 2010;110(1):57–65. [DOI] [PubMed] [Google Scholar]
- 20. Bartoli E, Fra GP, Carnevale Schianca GP. The oral glucose tolerance test (OGTT) revisited. Eur J Intern Med. 2011;22(1):8–12. [DOI] [PubMed] [Google Scholar]
- 21. Matsumoto K, Miyake S, Yano M, Ueki Y, Yamaguchi Y, Akazawa S, Tominaga Y. Glucose tolerance, insulin secretion, and insulin sensitivity in nonobese and obese Japanese subjects. Diabetes Care. 1997;20(10):1562–1568. [DOI] [PubMed] [Google Scholar]
- 22. Yoneda H, Ikegami H, Yamamoto Y, Yamato E, Cha T, Kawaguchi Y, Tahara Y, Ogihara T. Analysis of early-phase insulin responses in nonobese subjects with mild glucose intolerance. Diabetes Care. 1992;15(11):1517–1521. [DOI] [PubMed] [Google Scholar]
- 23. Phillips DI, Clark PM, Hales CN, Osmond C. Understanding oral glucose tolerance: comparison of glucose or insulin measurements during the oral glucose tolerance test with specific measurements of insulin resistance and insulin secretion. Diabet Med. 1994;11(3):286–292. [DOI] [PubMed] [Google Scholar]
- 24. Harbo T, Brincks J, Andersen H. Maximal isokinetic and isometric muscle strength of major muscle groups related to age, body mass, height, and sex in 178 healthy subjects. Eur J Appl Physiol. 2012;112(1):267–275. [DOI] [PubMed] [Google Scholar]
- 25. Zawadzki J, Bober T, Siemieński A. Validity analysis of the Biodex System 3 dynamometer under static and isokinetic conditions. Acta Bioeng Biomech. 2010;12(4):25–32. [PubMed] [Google Scholar]
- 26. Satonaka A, Suzuki N, Kawamura M. Validity of submaximal exercise testing in adults with athetospastic cerebral palsy. Arch Phys Med Rehabil. 2012;93(3):485–489. [DOI] [PubMed] [Google Scholar]
- 27. Sekikawa A, Tominaga M, Takahashi K, Eguchi H, Igarashi M, Ohnuma H, Sugiyama K, Manaka H, Sasaki H, Fukuyama H, Kato T, Kiyohara Y, Fujishima M. Prevalence of diabetes and impaired glucose tolerance in Funagata area, Japan. Diabetes Care. 1993;16(4):570–574. [DOI] [PubMed] [Google Scholar]
- 28. Oya J, Nakagami T, Yamamoto Y, Fukushima S, Takeda M, Endo Y, Uchigata Y. Effects of age on insulin resistance and secretion in subjects without diabetes. Intern Med. 2014;53(9):941–947. [DOI] [PubMed] [Google Scholar]
- 29. Iozzo P, Beck-Nielsen H, Laakso M, Smith U, Yki-Järvinen H, Ferrannini E; European Group for the Study of Insulin Resistance . Independent influence of age on basal insulin secretion in nondiabetic humans. J Clin Endocrinol Metab. 1999;84(3):863–868. [DOI] [PubMed] [Google Scholar]
- 30. Chang AM, Halter JB. Aging and insulin secretion. Am J Physiol Endocrinol Metab. 2003;284(1):E7–E12. [DOI] [PubMed] [Google Scholar]
- 31. Basu R, Breda E, Oberg AL, Powell CC, Dalla Man C, Basu A, Vittone JL, Klee GG, Arora P, Jensen MD, Toffolo G, Cobelli C, Rizza RA. Mechanisms of the age-associated deterioration in glucose tolerance: contribution of alterations in insulin secretion, action, and clearance. Diabetes. 2003;52(7):1738–1748. [DOI] [PubMed] [Google Scholar]
- 32. Zurlo F, Larson K, Bogardus C, Ravussin E. Skeletal muscle metabolism is a major determinant of resting energy expenditure. J Clin Invest. 1990;86(5):1423–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. DeFronzo RA. Lilly lecture 1987. The triumvirate: beta-cell, muscle, liver: a collusion responsible for NIDDM. Diabetes. 1988;37(6):667–687. [DOI] [PubMed] [Google Scholar]
- 34. Srikanthan P, Karlamangla AS. Relative muscle mass is inversely associated with insulin resistance and prediabetes. Findings from the third National Health and Nutrition Examination Survey. J Clin Endocrinol Metab. 2011;96(9):2898–2903. [DOI] [PubMed] [Google Scholar]
- 35. Kalyani RR, Metter EJ, Ramachandran R, Chia CW, Saudek CD, Ferrucci L. Glucose and insulin measurements from the oral glucose tolerance test and relationship to muscle mass. J Gerontol A Biol Sci Med Sci. 2012;67(1):74–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kwankaew J, Saetung S, Chanprasertyothin S, Leelawattana R, Rattarasarn C. Lean mass inversely predicts plasma glucose levels after oral glucose load independent of insulin secretion or insulin sensitivity in glucose intolerance subjects. Endocr J. 2014;61(1):77–83. [DOI] [PubMed] [Google Scholar]
- 37. Barsalani R, Brochu M, Dionne IJ. Is there a skeletal muscle mass threshold associated with the deterioration of insulin sensitivity in sedentary lean to obese postmenopausal women? Diabetes Res Clin Pract. 2013;102(2):123–128. [DOI] [PubMed] [Google Scholar]
- 38. Shulman GI. Ectopic fat in insulin resistance, dyslipidemia, and cardiometabolic disease. N Engl J Med. 2014;371(12):1131–1141. [DOI] [PubMed] [Google Scholar]
- 39. Yki-Järvinen H. Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol. 2014;2(11):901–910. [DOI] [PubMed] [Google Scholar]
- 40. Abildgaard J, Henstridge DC, Pedersen AT, Langley KG, Scheele C, Pedersen BK, Lindegaard B. In vitro palmitate treatment of myotubes from postmenopausal women leads to ceramide accumulation, inflammation and affected insulin signaling. PLoS One. 2014;9(7):e101555. [DOI] [PMC free article] [PubMed] [Google Scholar]