Abstract
Background
During radiotherapy of left-sided breast cancer, parts of the heart are irradiated, which may lead to late toxicity. We report on the experience of single institution with cardiac-sparing radiotherapy using voluntary deep inspiration breath hold (V-DIBH) and compare its dosimetric outcome with free breathing (FB) technique.
Patients and methods
Left-sided breast cancer patients, treated at our department with postoperative radiotherapy of breast/chest wall +/– regional lymph nodes between May 2015 and January 2017, were considered for inclusion. FB-computed tomography (CT) was obtained and dose-planning performed. Cases with cardiac V25Gy ≥ 5% or risk factors for heart disease were coached for V-DIBH. Compliant patients were included. They underwent additional CT in V-DIBH for planning, followed by V-DIBH radiotherapy. Dose volume histogram parameters for heart, lung and optimized planning target volume (OPTV) were compared between FB and BH. Treatment setup shifts and systematic and random errors for V-DIBH technique were compared with FB historic control.
Results
Sixty-three patients were considered for V-DIBH. Nine (14.3%) were non-compliant at coaching, leaving 54 cases for analysis. When compared with FB, V-DIBH resulted in a significant reduction of mean cardiac dose from 6.1 +/– 2.5 to 3.2 +/– 1.4 Gy (p < 0.001), maximum cardiac dose from 51.1 +/– 1.4 to 48.5 +/– 6.8 Gy (p = 0.005) and cardiac V25Gy from 8.5 +/– 4.2 to 3.2 +/– 2.5% (p < 0.001). Heart volumes receiving low (10–20 Gy) and high (30–50 Gy) doses were also significantly reduced. Mean dose to the left anterior coronary artery was 23.0 (+/– 6.7) Gy and 14.8 (+/– 7.6) Gy on FB and V-DIBH, respectively (p < 0.001). Differences between FB- and V-DIBH-derived mean lung dose (11.3 +/– 3.2 vs. 10.6 +/– 2.6 Gy), lung V20Gy (20.5 +/– 7 vs. 19.5 +/– 5.1 Gy) and V95% for the OPTV (95.6 +/– 4.1 vs. 95.2 +/– 6.3%) were non-significant. V-DIBH-derived mean shifts for initial patient setup were ≤ 2.7 mm. Random and systematic errors were ≤ 2.1 mm. These results did not differ significantly from historic FB controls.
Conclusions
When compared with FB, V-DIBH demonstrated high setup accuracy and enabled significant reduction of cardiac doses without compromising the target volume coverage. Differences in lung doses were non-significant.
Key words: breast cancer, radiotherapy, heart dose, heart sparing
Introduction
Worldwide, breast cancer is the most commonly diagnosed female malignancy and the leading cause of cancer mortality in women.1,2 Radiotherapy (RT) is an essential component of multimodal breast cancer treatment. Adjuvant irradiation to the residual breast after wide local excision of the primary tumor provides equivalent outcomes to mastectomy while ensuring superior cosmesis.3,4,5 In patients with risk factors after mastectomy, adjuvant radiotherapy improves overall survival and local control.6,7 Due to improvements in breast cancer treatment, the number of long-term survivors has increased over the past decades.8 With larger numbers surviving, more patients become at risk of developing a wide range of late radiation-related side effects. Postoperative radiotherapy in patients with left-sided breast cancer is characterized by exposure of significant portion of the heart volume to high doses of irradiation.9 Pathophysiology of radiotherapy-induced cardiac toxicity involves damage of blood vessels and interstitial fibrosis, leading to coronary artery disease, valvular abnormalities, myocardial dysfunction, pericardial disease and conductive disturbances. These changes can become clinically manifest several years or even decades after treatment, leading to increased risk for cardiac morbidity and death.10,11,12,13,14,15,16,17,18,19,20,21,22,23,24 The increased risk is proportional to the dose received by the heart, begins within years after exposure and continues for decades.12 Various radiotherapy techniques, including breath hold (BH) during treatment have been proposed to reduce the cardiac dose.25,26 It is expected that these maneuvers will result in reduced probability of late clinical manifestations of cardiac events.12,27,28 Voluntary deep inspiration breath hold (V-DIBH) radiotherapy has been studied in the setting of breast conserving treatment and post-mastectomy.25,26 Using this technique, the distance from the chest wall to the heart increases during deep inspiration, resulting in a decrease of cardiac volume in the radiotherapy field. While consistency and stability of V-DIBH has been demonstrated, real-time positional monitoring is advocated in daily practice to apply corrective actions due to intra-fractional movements.29,30 In 2015, we implemented V-DIBH for patients undergoing leftsided breast cancer radiotherapy, based on a prospective observational study protocol. This implementation in routine practice was based on the existent body of evidence in favor of V-DIBH.25,26 We aimed to ensure controlled transition to the new routine technique and to report on feasibility of this approach in our clinical setting and its dosimetric impact. Our hypothesis was that V-DIBH, when compared with free-breathing (FB) technique, will result in statistically significant reduction of the commonly reported cardiac dose-volume histogram (DVH) parameters without compromising the coverage of the target volume with prescribed dose. We also hypothesized that V-DIBH treatment results in non-inferior set-up accuracy when compared with FB. Our study was approved by the institutional Medical Research Center (Study No. 15330/15), on 14. 10. 2015 by the Hamad Medical Corporation Medical Research Centre.
Patients and methods
Patients and CT scanning
Formal calculation of the sample size was not performed. Instead, all consecutive left-sided breast cancer patients, treated at our department with postoperative radiotherapy between May 2015 and January 2017, were considered for V-DIBH. In this way, a clinically relevant patient cohort was enrolled during the period of V-DIBH implementation. Informed consent to treatment according to the protocol was obtained from all patients. Metastatic disease, compromised respiratory function, Eastern Cooperative Group performance status >2, need for sedation during treatment and patient refusal were exclusion criteria. Patients with cardiac V25Gy ≥ 5% on FB treatment plan were offered V-DIBH. In addition, selected cases with lower V25Gy were entered on the V-DIBH protocol. This selection was performed at discretion of the treating radiation oncologist by considering patient-related factors such as age, pre-existent ischemic cardiac events and other co-morbidities, application of cardio-toxic medications, history of smoking, diabetes mellitus, hyperlipidemia and arterial hypertension.
Our V-DIBH approach was adapted from the technique used in the UK HeartSpare study and was based on visual confirmation of the borders of the light fields, marked on the patient as surrogates of the isocenter.31 Planning scans were obtained with a 64-slice Siemens Somatom Definition CT scanner, using 5 mm slice thickness. During scanning, Patients were positioned supine with both arms above the head, using the breast board and knee rest (CIVCO Medical Solutions, © 2017 USA). Standard CT planning marks were used in all cases. They included four tattoos (superior, inferior, medial and lateral) and wires to delineate surgical scar and patient midline. First, FB CT was obtained. Following completion of FB CT, the patients, still in simulation position, underwent V-DIBH coaching. During coaching, patient’s ability to hold breath for the duration of treatment was checked. In addition, geometric consistency of BH was visually assessed using in-room lasers and skin marks. Finally, the patients were asked to practice V-DIBH technique overnight and returned the following day to complete V-DIBH CT scan. V-DIBH scans were completed using the same basic set up parameters as FB scans. During imaging, the therapists communicated with the patients by using in-room intercom. Video connection with closed-circuit camera was used for visual assessment of skin marks to ensure BH consistency; distance from tattoos to BH marks was recorded.
Contouring and dose optimization
Contouring and treatment planning was performed with Varian External Beam Planning system, version 13.7 (© 1996-2016 Varian Medical Systems, Inc, Palo Alto, USA). Planning target volume (PTV), heart and lung were contoured on FB and V-DIBH CT scans by five different radiation oncologists according to our departmental contouring guidelines, adapted from the published recommendations.32 As per our departmental practice, internal mammary lymph node chains were not included in the treatment volume. Left anterior descending coronary artery (LAD) was contoured based on the recently published contouring atlas.33 Optimized PTV (OPTV) was created by subtracting 5 mm from PTV at the skin. Analysis of contouring uncertainties was limited to volumetric comparisons (mean volumes and relative standard deviations) of delineated regions of interest between FB and V-DIBH and within each approach.
Treatment planning was completed according to our institutional practice (see below) separately for FB and V-DIBH scans. Our standard prescription was 50 Gy in 25 fractions to the OPTV. When indicated, 45 Gy in 25 fractions were applied simultaneously with breast / chest wall irradiation to the ipsilateral supra-clavicular region. OPTV irradiation was followed by electron boost of 16 Gy in 8 fractions to lumpectomy bed or postmastectomy scar. Photon boost was not used. Dose contribution from electron boost was not included in the analysis. Dose optimization did not differ between FB and V-DIBH approach and consisted of forward-planned intensity modulated field in field technique. Subfields were fitted on a weighted pair of tangents to attain OPTV dose homogeneity. Planning aims were to cover ≥ 95% of the OPTV with ≥ 95% of prescribed dose and to keep the proportion of ipsilateral lung irradiated to 20 Gy (V20Gy) < 25%, cardiac V25Gy < 5% and mean cardiac dose < 5 Gy. For hypo-fractionation (40 Gy in 15 fractions), linear quadratic model with α/β of 3Gy was applied to calculate the biologically equivalent dose constraints for the lung (V18Gy < 22%–25%) and heart (V23Gy ≤ 5% and mean D ≤ 4Gy). DVH parameters of FB and V-DIBH treatment plans were recorded and compared.
Treatment
For daily treatments, patients were positioned and immobilized identical to planning CT. BH consistency was checked in the room by using skin marks to reflect the measurements from CT and in-room lasers. Outside the treatment room, closed-circuit television camera was zoomed in to clearly define BH skin marks. Next, patients were asked to complete BH using the intercom system. Skin marks were visually checked through video connection to quantify inspiration and to ensure that the planned inspiration depth was reproduced during daily treatments. Set up verification and correction was performed through daily pre-port tangential megavoltage images and cine loop images (Varian On board imager 1.6 © 2015, Switzerland) to confirm both isocenter position and BH consistency. If corrections were required, they were applied in the room with the patient in BH position and new marks were placed on the patient’s skin. Set up errors were assessed offline for every fraction. For the first 18 patients treated with the V-DIBH technique, mean shifts and systematic and random errors were calculated. The results were compared with a retrospective cohort of patients treated at our department using the FB technique.
Statistical analysis
Mean values and standard deviations were used to present continuous numerical variables and paired sample t-test was used to test for significance of differences. Statistical tests were double sided with p-value of < 0.05 considered as the limit for significance. Miscrosoft Office Excel software was used for data analysis and statistics.
Results
Patients and treatment
Sixty-three patients were considered for V-DIBH radiotherapy. Nine (14.3%) were excluded at the time of coaching due to non-compliance with the V-DIBH protocol. Additional two (3.2%) were unable to hold breath after the treatment start and reverted from V-DIBH to FB technique, but their DVH parameters are included in final analysis. In summary, the overall ability to complete radiotherapy using the V-DIBH technique was 82.5% and 54 cases were included in the DVH analysis. All patients were female and median age was 41 years (range: 30-64 years). The irradiated volume included residual breast after organ conserving surgery in 31 (57%) and chest wall after mastectomy in 23 (43%) cases. All patients received electron boost of 16 Gy in 8 fractions to the lumpectomy cavity or mastectomy scar. Left supra-clavicular region was included in the radiation fields in all 24 (100%) post-mastectomy and in 7 (22.6%) post-lumpectomy cases. Patients were required to perform 11 breath holds on an average daily treatment. Mean couch shifts and setup errors for the V-DIBH technique were not significantly different when compared with our historic cohort of patients, treated with FB approach (Table 1). Largest mean shift for initial patient setup was in longitudinal direction (2.7 mm), followed by the lateral (2.1 mm) and vertical direction (1.2 mm). Population systematic and random error was the highest for the longitudinal direction (2.1 and 0.7 mm, respectively).
Table 1.
Vertical, longitudinal and lateral couch shifts and corresponding systematic and random errors for the initial 18 patients treated with voluntary deep inspiration breath-hold (V-DIBH) and a historic control treated with free-breathing (FB) technique. Differences between the two approaches were non-significant.
| Vertical [mm] | Longitudinal [mm] | Lateral [mm] | ||||
|---|---|---|---|---|---|---|
| Setup parameter | FB | V-DIBH | FB | V-DIBH | FB | V-DIBH |
| Mean shift | 1 | 1.2 | 2.8 | 2.7 | 1.9 | 2.1 |
| Systematic error | 0.7 | 1.5 | 1.6 | 2.1 | 0.8 | 1.3 |
| Random error | 0.6 | 0.6 | 2.1 | 0.7 | 1.1 | 0.4 |
FB = free breathing; V-DIBH = voluntary deep inspiration breath hold
Dose volume histogram parameters
V-DIBH technique resulted in a significant increase of delineated left lung volume when compared with FB (1557 +/– 389 cm3 vs. 914 +/– 207.7 cm3; p < 0.001). Inter-observer variation of lung contouring was comparable between the two approaches with a relative standard deviation of 23% and 25% on FB and V-DIBH CT, respectively. Global volumetric analysis revealed statistically significant inter-approach (intra-observer) variation of contoured cardiac volumes: mean volume of the heart on FB and V-DIBH CT was 567 +/– 82 cm3 and 547 +/–91 cm3, respectively (p < 0.05) (Figure 1). Interobserver variation of cardiac and LAD volumes was comparable between the FB and V-DIBH scans as demonstrated by non-significantly different relative standard deviations (heart volume: 14.4% vs. 16.7%, LAD volume: 29.5% on both scans). Mean volume of PTV contours on FB CT did not differ significantly from the PTV as delineated on V-DIBH scans (985 +/– 405 cm3 vs. 960 +/– 369 cm3; p = 0.08). Results of the DVH parameters analysis are presented in Table 2. When compared with FB, V-DIBH resulted in a statistically significant reduction of all analyzed DVH parameters for the heart and LAD. Differences between FB- and V-DIBH-derived lung doses and V95% for the OPTV were non-significant (Table 2). Impact of elective nodal radiotherapy on the analyzed cardiac and lung DVH parameters is summarized in Table 3. There was no significant difference in cardiac DVH parameters between patients receiving left supraclavicular fossa radiotherapy and patients treated with breast/chest wall radiotherapy alone. Mean dose to the left lung and lung volumes receiving 10, 20 and 30 Gy, were significantly higher in subgroup with inclusion of supraclavicular fossa both in V-DIBH and FB treatment plans (Table 3).
Figure 1.
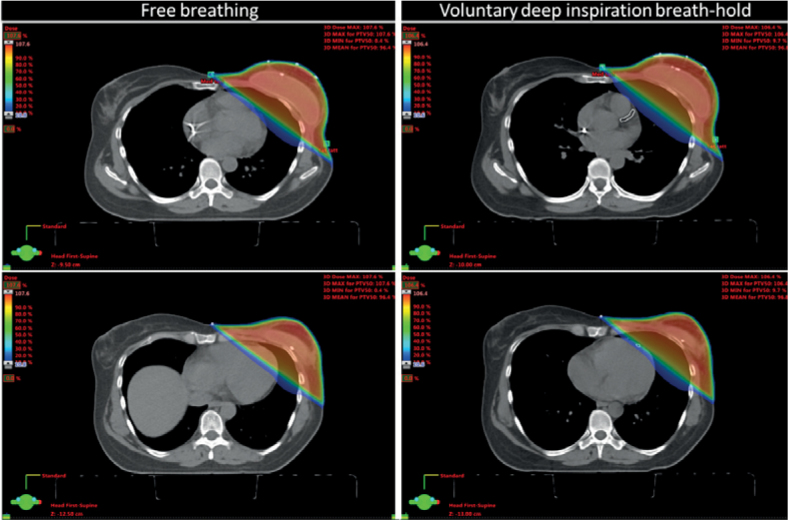
Impact of deep inspiration on cardiac dose during postoperative radiotherapy for left-sided breast cancer. Doses from 0% to three-dimensional dose maximum are depicted by color wash. Upper two slices are taken at mid-breast level and the lower pair 6 slices below. At both levels, the proportion of cardiac volume is reduced by voluntary deep inspiration breath-hold.
Table 2.
Mean values +/– standard deviations of dose volume histogram (DVH) parameters for heart, left anterior descending coronary artery (LAD), lung and optimized planning target volume (OPTV) achieved by the free breathing and breath-hold technique.
| DVH parameter | Free breathing | Breath-hold | P-value |
|---|---|---|---|
| Heart | |||
| Dmean [Gy] | 6.1 +/– 2.5 | 3.2 +/– 1.4 | |
| Dmax [Gy] | 51.1 +/– 1.4 | 48.5 +/– 6.8 | |
| V50Gy [%] | 0.7 +/– 1.1 | 0.2 +/– 0.6 | |
| V40Gy [%] | 6.2 +/– 3.5 | 2.1 +/– 1.9 | |
| V30Gy [%] | 7.8 +/– 4 | 2.8 +/– 2.3 | < 0.05 |
| V25Gy [%] | 8.5 +/– 4.2 | 3.2 +/– 2.5 | |
| V20Gy [%] | 9.2 +/– 4.4 | 3.6 +/– 2.7 | |
| V15Gy [%] | 10 +/– 4.6 | 4.1 +/– 2.9 | |
| V10Gy [%] | 11.2 +/– 5 | 4.9 +/– 3.2 | |
| Left lung | |||
| Dmean [Gy] | 11.3 +/– 3.2 | 10.6 +/– 2.6 | |
| Dmax [Gy] | 51.6 +/– 1.8 | 50.6 +/– 1.1 | |
| V30Gy [%] | 17.9 +/– 6.3 | 17 +/– 4.6 | NS |
| V20Gy [%] | 20.5 +/– 7 | 19.5 +/– 5.1 | |
| V10Gy [%] | 25.9 +/– 8.1 | 25.4 +/– 5.8 | |
| LAD | |||
| Dmean [Gy] | 23.0 +/– 6.7 | 14.8 +/– 7.6 | |
| Dmax [Gy] | 49.7 +/– 3.4 | 44.3 +/– 12.2 | < 0.05 |
| D50% [Gy] | 20.4 +/– 17.6 | 8.4 +/– 11.1 | |
| OPTV | |||
| V95% [%] | 95.6 +/– 4.1 | 95.2 +/– 6.3 | NS |
Dmax = maximal dose; Dmean = mean dose; Dx% = dose received by x% of volume; LAD = left anterior descending coronary artery; NS = non-significant; VxGy = relative volume, receiving a dose of x Gy; Vx% =relative volume, receiving x% of the prescribed dose
Table 3.
Impact of supraclavicular fossa (SCF) radiotherapy on heart and lung dose volume histogram (DVH) parameters
| DVH parameter | Free breathing | p-value | Breath hold | p-value | ||
|---|---|---|---|---|---|---|
| No SCF (n = 23) | SCF (n = 31) | No SCF (n = 23) | SCF (n = 31) | p-value | ||
| Heart | Heart | |||||
| Dmean [Gy] | 5.5 +/– 2.2 | 6.6 +/– 2.7 | 2.9 +/– 1.1 | 3.5 +/– 1.6 | ||
| Dmax [Gy] | 51.1 +/– 1.5 | 51.1 +/– 1.3 | 48.2 +/– 7.8 | 48.8 +/– 5.9 | ||
| V50Gy [%] | 1 +/– 1.3 | 0.5 +/– 0.9 | 0.3 +/– 0.7 | 0.2 +/– 0.3 | ||
| V40Gy [%] | 5.9 +/– 3.6 | 6.5 +/– 3.4 | NS | 1.6 +/– 1.4 | 2.4 +/– 2.2 | NS |
| V30Gy [%] | 7.2 +/– 4.1 | 8.3 +/– 3.9 | 2.3 +/– 1.8 | 3.3 +/– 2.6 | ||
| V25Gy [%] | 7.8 +/– 4.2 | 9.1 +/– 4.1 | 2.6 +/– 1.9 | 3.7 +/– 2.8 | ||
| V20Gy [%] | 8.4 +/– 4.4 | 9.8 +/– 4.4 | 2.9 +/– 2.1 | 4.2 +/– 3 | ||
| V15Gy [%] | 9.2 +/– 4.7 | 10.6 +/– 4.5 | 3.4 +/– 2.3 | 4.7 +/– 3.2 | ||
| V10Gy [%] | 10.4 +/– 5.1 | 12 +/– 4.8 | 4.2 +/– 2.6 | 5.6 +/– 3.5 | ||
| Lung | Lung | |||||
| Dmean [Gy] | 9 +/– 2.6 | 13.2 +/– 2.2 | < 0.05 | 9.3 +/– 3.2 | 11.8 +/– 2.4 | < 0.05 |
| Dmax [Gy] | 51.1 +/– 1.4 | 52 +/– 2.1 | NS | 50.4 +/– 1.1 | 50.8 +/– 1.1 | NS |
| V30Gy [%] | 13.4 +/– 4.9 | 21.7 +/– 4.7 | 14 +/– 4 | 19.6 +/– 3.3 | ||
| V20Gy [%] | 15.5 +/– 5.3 | 24.9 +/– 5.1 | < 0.05 | 16.3 +/– 4.4 | 22.3 +/– 3.8 | < 0.05 |
| V10Gy [%] | 19.8 +/– 6.1 | 31.2 +/– 5.5 | 21.5 +/– 5.5 | 28.8 +/– 3.6 | ||
NS = non-significant
Discussion
Adjuvant radiotherapy improves the treatment outcome after breast cancer surgery, but it also carries a risk for late cardiac toxicity in left sided tumors.3,4,5,6,7,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24 Various techniques were suggested to reduce this effect.25,26 In our present study, the implementation of V-DIBH technique achieved statistically significant reduction of cardiac doses without affecting the PTV coverage. V-DIBH radiotherapy was characterized by excellent patient compliance and high set-up accuracy which was non-inferior to the historic FB control.
We found that V-DIBH, when compared with FB technique, achieved significant reduction of all analyzed DVH parameters for LAD and heart (Table 2). In our patient cohort, the mean cardiac dose was reduced by 50% and V25Gy by 64% (Table 2). The heart-sparing effect afforded by the V-DIBH did not come at a cost of inferior dose-coverage of the OPTV when compared with the FB treatment plans (Table 2). Covariates that impact the cardiac dose during radiotherapy include the radiotherapy technique (intensity modulated vs. 3D conformal), use of cardiac sparing techniques, patient position, regional irradiation and boost.34 It should be emphasized that direct comparisons between different studies and our current report are challenging due to differences in the listed factors, including treatment volumes and heart sparing methodologies used. Hjelstuen et al. analyzed the DVH parameters of 17 patients treated with DIBH technique using a commercially available gating system. When compared with the FB technique, DIBH reduced the planned mean heart dose from 6.2 to 3.1 Gy and cardiac V25Gy from 6.7% to 1.2% (p < 0.001). Mean V95% for the PTV did not differ significantly between the FB (98.9 +/– 0.5%) and DIBH (98.8 +/– 0.5) plans. Of note, regional lymph nodes, including the internal mammary chain, were included in the target volume in all patients in this study.35 In our work, internal mammary chain was not included, making direct comparisons challenging. In another study of left-sided breast cancer patients treated with DIBH or FB, similar reduction of cardiac doses was obtained while the target volume coverage was even slightly improved.36 In a cohort of 22 patients, Stranzl et al. found a low mean heart dose of 2.3 Gy on FB, which further improved to 1.3 Gy with DIBH using the Real-time Positioning Management System™ (RPM; © Varian Medical Systems).24 Using V-DIBH, we achieved significant reduction of all analyzed DVH parameters for LAD (Table 2). In breast cancer radiotherapy, damage to left anterior ventricular wall and LAD play an important role, given their anatomical position in relation to the radiation fields.23 In a study by Wang et al., mean dose to LAD was 20.47 Gy on FB compared to 5.94 Gy on DIBH plans, with a relative reduction of 71%.37 Hayden at al. achieved a 31% dose reduction for the mean LAD dose using DIBH technique.38 Several other studies demonstrated similar improvements for different cardiac DVH parameters, including dose to LAD.39,40,41 Keeping the challenges related to comparisons of monoinstitutional retrospective studies in mind, we can summarize that our results compare favourably with the published reports.
In patients without previous cardiac events, we used the heart V25Gy ≥ 5% as threshold for inclusion on the V-DIBH protocol. But the evidence suggests that there is no threshold dose below which the late cardiac effects do not occur. A recent study by Darby et al. used a population-based case-control model to look at major coronary events and ischemic cardiac deaths following breast cancer radiotherapy. The investigators estimated the cardiac doses in 963 patients with major coronary events and 1205 controls. Dosimetric findings were correlated with clinical outcomes. The study suggested that the probability of major coronary events increases linearly with increasing mean heart dose at a rate of 7.4% / Gy (95% confidence interval 2.9–14.5; p < 0.01). This increase began within 5 years after treatment and continued for at least 20 years. The relative effect per Gray was independent of the presence of cardiac risk factors, but the absolute increase was higher in women with pre-existing morbidity.12 Therefore, all left-sided breast cancer patients requiring radiotherapy should in principle be offered one of the cardiac sparing treatment techniques.25 We suggest that implementation of new methods such as V-DIBH is carefully planned, because it demands time and additional human resources, especially during the learning curve period. The V25Gy inclusion threshold of 5% used in our study was selected based on our infrastructural capabilities. Analysis of our workforce and linear accelerator capacities was balanced against the projected workload during the study. This analysis showed that setting the V25Gy threshold at 5% leads to inclusion of approximately 33% of patients with highest cardiac doses, which was the maximal acceptable workload increase. Based on the positive results of our present study and the favorable experience gained, we adopted V-DIBH radiotherapy as standard treatment for all left-sided breast cancer patients. This implementation was reflected in a corresponding increase of our planned staffing requirements. However, it required no infrastructural investments because the V-DIBH technique can be applied without any additional special equipment. Relatively high average number of breath-holds observed in our study (11 breath holds per daily treatment) can be attributed to the learning curve at the early stage of V-DIBH implementation.
Average cardiac volume as delineated on V-DIBH scans (547 +/–91 cm3) was significantly smaller when compared with FB scans (567 +/– 82 cm3) (p = 0.016), which could be attributed to the physiologic effect of V-DIBH. While statistically significant, the absolute average difference between contoured volumes was small (20 cm3), but there was a substantial spread of individual differences (st. dev: 61 cm3), indicating large variation between FB and V-DIBH based cardiac volumes in individual study cases. Contouring variation is one of the major sources of uncertainties in radiotherapy. In spite of the use of contouring guidelines, high quality imaging and participation of trained observers, complete elimination of contouring variation is an unrealistic aim.42 Therefore, the magnitude of contouring variation needs to be quantified and considered during the interpretation of DVH results. While the DVH parameters reported in our present study were based on relative cardiac volumes, the mean absolute volume was smaller on V-DIBH when compared with FB. Therefore, cardiac sparing afforded by V-DIBH technique is likely to be an underestimation of the actual sparing effect. This can be regarded as a supporting argument for the confirmation of our study hypothesis. The inter-observer (intra-approach) variation of cardiac contouring was comparable between the FB and V-DIBH scans as demonstrated by similar relative standard deviation of around 15%. Consequently, the impact of contouring variation on uncertainties of the DVH parameters was similar for both simulation approaches, making our results clinically relevant.
Our V-DIBH technique requires no additional equipment, ensures precise setup and is feasible, as demonstrated by the 82.5% compliance with coaching instructions. We found that the mean shifts for initial patient setup with V-DIBH technique were from 1.2 to 2.8 mm and the systematic and random setup errors were ≤ 2.1 mm. These favorable results did not differ significantly from our past experience with FB approach (Table 1). Real-time monitoring ensured high precision setup throughout the beam-on time. Although not formally analyzed, our experience with the V-DIBH confirms excellent reproducibility, constancy and stability of this treatment technique.29,30 Our results compare favorably with reports by other authors using similar approaches. The HeartSpare study was a randomized comparison between V-DIBH and deep-inspiratory breath-hold with Active Breathing Coordinator™ (ABC-DIBH; © Elekta).31 Twenty three patients were randomized to receive one technique for the first seven and the second technique for the following 8 fractions of hypofractionated regimen delivering 40 Gy in 15 fractions. Differences between V-DIBH and ABC-DIBH based setup errors were non-significant. Systematic errors derived from electronic portal imaging were ≤ 1.8 mm for v-DIBH and ≤ 2 mm for ABC-DIBH, while the respective random errors were ≤ 2.5 mm and ≤ 2.2 mm. Furthermore, V-DIBH was preferred by patients and staff, took less time to deliver and achieved similar normal tissue sparing at lower cost when compared with the ABC-DIBH.31 Similarly, Borst et al. reported on high feasibility and small setup variability of V-DIBH technique, with the largest systematic (2.9 mm) and random error (2 mm) in direction perpendicular to the field.40 In a study by Gierga et al., three-dimensional surface imaging was used to correct the daily set up of 20 patients treated with 443 fractions of DIBH radiotherapy. Mean shifts for initial patient setups were from 0.3 to 2 mm in different directions, while random and systematic errors were less than 4 mm.43
Conclusions
When compared with free-breathing radiotherapy, voluntary deep inspiration breath-hold enabled significant reduction of cardiac doses without compromising the target volume coverage in our cohort of left-sided breast cancer patients. Treatment setup shifts and population systematic and random errors were small and not significantly different from the historic controls treated with the free-breathing technique. Our systematic approach to patient coaching was reflected in low rate of conversion to free-breathing radiotherapy. Based on the positive results of our present study and experience gained, we adopted V-DIBH radiotherapy as standard treatment for all left-sided breast cancer patients. Long follow up is needed to confirm the clinical impact of the presented favorable dosimetric benefit.
Acknowledgments
The authors are grateful to Ahmed Mahmud Moallim and Satheesh Prasad Paloor, from Department of Radiation Oncology, Department of Radiation Oncology, NCCCR, HMC, Doha, Qatar, for their contribution to this study.
Footnotes
Disclosure: No potential conflicts of interest were disclosed.
References
- 1.Torre LA, Siegel RL, Ward EM, Jemal A.. Global cancer incidence and mortality rates and trends - an update. Cancer Epidemiol Biomarkers Prev. 2016;25:16–27. doi: 10.1158/1055-9965. [DOI] [PubMed] [Google Scholar]
- 2.Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JWW, Comber H. et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49:1374–403. doi: 10.1016/j.ejca.2012.12.027. [DOI] [PubMed] [Google Scholar]
- 3.Clarke M, Collins R, Darby S, Davies C, Elphinstone P, Evans V. et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomized trials. Lancet. 2005;366:2087–106. doi: 10.1016/S0140-6736(05)67887-7. [DOI] [PubMed] [Google Scholar]
- 4.Fisher B, Anderson S, Bryant J, Margoloese RG, Deutsch M, Fisher ER. et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347:1233–41. doi: 10.1056/NEJMoa022152. [DOI] [PubMed] [Google Scholar]
- 5.Early Breast Cancer Trialists’ Collaborative Group. Effect of radiotherapy after breast conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011;378:1707–16. doi: 10.1016/S0140-6736(11)61629-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Early Breast Cancer Trialists’ Collaborative Group. Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet. 2014;383:2127–35. doi: 10.1016/S0140-6736(14)60488-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Danish Breast Cancer Cooperative Group. Nielsen HM, Overgaard M, Grau C, Jensen AR, Overgaard J.. Study of failure pattern among high-risk breast cancer patients with or without postmastectomy radiotherapy in addition to adjuvant systemic therapy: long-term results from the Danish Breast Cancer Cooperative Group DBCG 82 b and c randomized studies. J Clin Oncol. 2006;24:2268–75. doi: 10.1200/JCO.2005.02.8738. [DOI] [PubMed] [Google Scholar]
- 8.Kanapuru B, Ershler WB, Hesdorffer C, Jemal A, Yates JW.. Long-term survival of older breast cancer patients: population-based estimates over three decades. Breast Cancer Res Treat. 2012;134:853–7. doi: 10.1007/s10549-012-2115-4. [DOI] [PubMed] [Google Scholar]
- 9.Taylor CW, Brønnum D, Darby SC, Gagliardi G, Hall P, Jensen MB. et al. Cardiac dose estimates from Danish and Swedish breast cancer radiotherapy during 1977-2001. Radiother Oncol. 2011;100:176–83. doi: 10.1016/j.radonc.2011.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duma MN, Molls M, Trott KR.. From heart to heart for breast cancer patients - cardiovascular toxicities in breast cancer radiotherapy. Strahlenther Onkol. 2014;190:5–7. doi: 10.1007/s00066-013-0465-4. [DOI] [PubMed] [Google Scholar]
- 11.Carlson RG, Mayfield WR, Normann S, Alexander JA.. Radiation-associated valvular disease. Chest. 1991;99:538–45. doi: 10.1378/chest.99.3.538. http://dx.doi.org/10.1378/chest.99.3.538 [DOI] [PubMed] [Google Scholar]
- 12.Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, Brønnum D. et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368:987–98. doi: 10.1056/NEJMoa1209825. [DOI] [PubMed] [Google Scholar]
- 13.Heidenreich PA, Hancock SL, Vagelos RH, Lee BK, Schnittger I.. Diastolic dysfunction after mediastinal irradiation. Am Heart J. 2005;150:977–82. doi: 10.1016/j.ahj.2004.12.026. [DOI] [PubMed] [Google Scholar]
- 14.Orzan F, Brusca A, Gaita F, Giustetto C, Figliomeni MC, Libero L.. Associated cardiac lesions in patients with radiation-induced complete heart block. Int J Cardiol. 1993;39:151–6. doi: 10.1016/0167-5273(93)90027-E. [DOI] [PubMed] [Google Scholar]
- 15.Larsen RL, Jakacki RI, Vetter VL, Meadows AT, Silber JH, Barber G.. Electrocardiographic changes and arrhythmias after cancer therapy in children and young adults. Am J Cardiol. 1992;70:73–7. doi: 10.1016/0002-9149(92)91393-I. [DOI] [PubMed] [Google Scholar]
- 16.Giordano SH, Kuo YF, Freeman JL, Buchholz TA, Hortobagy GN, Goodwin JS.. Risk of cardiac death after adjuvant radiotherapy for breast cancer. J Natl Cancer Inst. 2005;97:419–24. doi: 10.1093/jnci/dji067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheng YJ, Nie XY, Ji CC, Lin XX, Liu J, Chen XM. et al. Long-Term Cardiovascular Risk After Radiotherapy in Women With Breast Cancer. J Am Heart Assoc. 2017;6:e005633. doi: 10.1161/JAHA.117.005633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Højris I, Overgaard M, Christensen JJ, Overgaard J.. Morbidity and mortality of ischaemic heart disease in high-risk breast-cancer patients after adjuvant postmastectomy systemic treatment with or without radiotherapy: analysis of DBCG 82b and 82c randomised trials. Radiotherapy Committee of the Danish Breast Cancer Cooperative Group. Lancet. 1999;354:1425–30. doi: 10.1016/S0140-6736(99)02245-X. [DOI] [PubMed] [Google Scholar]
- 19.McGale P, Darby SC, Hall P, Adolfsson J, Bengtsson NO, Bennet AM. et al. Incidence of heart disease in 35,000 women treated with radiotherapy for breast cancer in Denmark and Sweden. Radiother Oncol. 2011;100:167–75. doi: 10.1016/j.radonc.2011.06.016. [DOI] [PubMed] [Google Scholar]
- 20.Taylor C, Correa C, Duane FK, Aznar MC, Anderson SJ, Bergh J. et al. Estimating the risks of breast cancer radiotherapy: evidence from modern radiation doses to the lungs and heart and from previous randomized trials. J Clin Oncol. 2017;35:1641–9. doi: 10.1200/JCO.2016.72.0722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paszat LF, Mackillop WJ, Groome PA, Boyd C, Schulze K, Holowaty E.. Mortality from myocardial infarction after adjuvant radiotherapy for breast cancer in the surveillance, epidemiology, and end-results cancer registries. J Clin Oncol. 1998;16:2625–31. doi: 10.1200/JCO.1998.16.8.2625. [DOI] [PubMed] [Google Scholar]
- 22.Lee MS, Finch W, Mahmud E.. Cardiovascular complications of radiotherapy. Am J Cardiol. 2013;112:1688–96. doi: 10.1016/j.amjcard.2013.07.031. [DOI] [PubMed] [Google Scholar]
- 23.Correa CR, Litt HI, Hwang WT, Ferrari VA, Solin LJ, Harris EE.. Coronary artery findings after left-sided compared with right-sided radiation treatment for early-stage breast cancer. J Clin Oncol. 2007;25:3031–7. doi: 10.1200/JCO.2006.08.6595. [DOI] [PubMed] [Google Scholar]
- 24.Stranzl H, Zurl B.. Postoperative irradiation of left-sided breast cancer patients and cardiac toxicity. Strahlenther Onkol. 2008;184:354–8. doi: 10.1007/s00066-008-1852-0. [DOI] [PubMed] [Google Scholar]
- 25.Shah C, Badiyan S, Berry S, Khan AJ, Goyal S, Schulte K. et al. Cardiac dose sparing and avoidance techniques in breast cancer radiotherapy. Radiother Oncol. 2014;112:9–16. doi: 10.1016/j.radonc.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 26.Latty D, Stuart KE, Wang W, Ahern V.. Review of deep inspiration breath-hold technique for the treatment of breast cancer. J Med Radiat Sci. 2015;62:74–81. doi: 10.1002/jmrs.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marks LB, Yorke ED, Jackson A Ten Haken RK, Constine LS, Eisbruch A. et al. Use of normal tissue complication probability models in the clinic. Int J Radiat Oncol Biol Phys. 2010;76:10–9. doi: 10.1016/j.ijrobp.2009.07.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Korreman SS, Pederson AN, Aarup LR, Nøttrup TJ, Specht L, Nyström H.. Reduction of cardiac and pulmonary complication probabilities after breathing adapted radiotherapy for breast cancer. Int J Radiat Oncol Biol Phys. 2006;65:1375–80. doi: 10.1016/j.ijrobp.2006.03.046. [DOI] [PubMed] [Google Scholar]
- 29.Colgan R, James M, Bartlett FR, Kirby AM, Donovan EM.. Voluntary breath-holding for breast cancer radiotherapy is consistent and stable. Br J Radiol. 2015;88:1–8. doi: 10.1259/bjr.20150309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kapanen M, Laaksomaa M, Pehkonen J, Haltamo M, Luukkanen H. et al. Effects of multiple breath hold reproducibility on treatment localization and dosimetric accuracy in radiotherapy of left-sided breast cancer with voluntary deep inspiration breath hold technique. Med Dosim. 2017;42:177–84. doi: 10.1016/j.meddos.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 31.Bartlett FR, Colgan RM, Carr K, Donovan EM, McNAir HA, Locke I. et al. The UK HeartSpare Study: randomised evaluation of voluntary deep-inspiratory breath-hold in women undergoing breast radiotherapy. Radiother Oncol. 2013;108:242–7. doi: 10.1016/j.radonc.2013.04.021. [DOI] [PubMed] [Google Scholar]
- 32.Radiation Therapy Oncology Group (RTOG). Breast cancer atlas for radiation therapy planning: consensus definitions. [cited 15 Avg 2017]. Available at. http://www.rtog.org/LinkClick.aspx?fileticket=vzJFhPaBipE%3d&tabid=236 [Google Scholar]
- 33.Duane F, Aznar M, Bartlett F, Cutter DJ, Darby SC, Jagsi R. et al. A cardiac contouring atlas for radiotherapy. Radiother Oncol. 2017;122:416–22. doi: 10.1016/j.radonc.2017.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pierce LJ, Feng M, Griffith KA, Jaqsi R, Boike T, Dryden D. et al. Recent time trends and predictors of heart dose from breast radiation therapy in a large quality consortium of radiation oncology practices. Int J Radiat Oncol Biol Phys. 2017;99:1154–61. doi: 10.1016/j.ijrobp.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 35.Hjelstuen MH, Mjaaland I, Vikstrom J, Dybvik Kl.. Radiation during deep inspiration allows loco-regional treatment of left breast and axillary, supraclavicular, and internal mammary lymph nodes without compromising target coverage or dose restrictions to organs at risk. Acta Oncol. 2012;51:333–44. doi: 10.3109/0284186X.2011.618510. [DOI] [PubMed] [Google Scholar]
- 36.Nissen HD, Appelt AL.. Improved heart, lung, and target dose with deep inspiration breath hold in a large clinical series of breast cancer patients. Radiother Oncol. 2013106:28–32. doi: 10.1016/j.radonc.2012.10.016. [DOI] [PubMed] [Google Scholar]
- 37.Wang W, Purdie TG, Rahman M, Marshal A, Liu FF, Fyles A.. Rapid automated treatment planning process to select breast cancer patients for active breathing control to achieve cardiac dose reduction. Int J Radiat Oncol Biol Phys. 2012;82:386–93. doi: 10.1016/j.ijrobp.2010.09.026. [DOI] [PubMed] [Google Scholar]
- 38.Hayden AJ, Rains M, Tiver K.. Deep inspiration breath hold technique reduces heart dose from radiotherapy for left-sided breast cancer. J Med Imaging Radiat Oncol. 2012;56:462–72. doi: 10.1111/j.1754-9485.2012.02405.x. [DOI] [PubMed] [Google Scholar]
- 39.Reardon KA, Read PW, Morris MM, Reardon MA, Geesy C, Wijesooriya K.. A comparative analysis of 3D conformal deep inspiratory-breath hold and free-breathing intensity-modulated radiation therapy for left-sided breast cancer. Med Dosim. 2013;38:190–5. doi: 10.1016/j.meddos.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 40.Borst GR, Sonke JJ, den Hollander S, Betgen A, Remeijer P, van Giersbergen A. et al. Clinical results of image-guided deep inspiration breath hold breast irradiation. Int J Radiat Oncol Biol Phys. 2010;78:1345–51. doi: 10.1016/j.ijrobp.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 41.McIntosh A, Soushtari AN, Benedict SH, Read PW, Wijesooriya K.. Quantifying the reproducibility of heart position during treatment and corresponding delivered heart dose in voluntary deep inspiration breath hold for left breast cancer patients treated with external beam radiotherapy. Int J Radiat Oncol Biol Phys. 2008;81:569–76. doi: 10.1016/j.ijrobp.2011.01.044. [DOI] [PubMed] [Google Scholar]
- 42.Segedin B, Petric P.. Uncertainties in target volume delineation in radiotherapy - are they relevant and what can we do about them? Radiol Oncol. 2016;50:254–62. doi: 10.1515/raon-2016-0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gierga DP, Turcotte JC, Sharp GC, Sedlacek DE, Cotter CR, Taghian AG.. A voluntary breath-hold treatment technique for the left breast with unfavorable cardiac anatomy using surface imaging. Int J Radiation Oncol Biol Phys. 2012;84:663–8. doi: 10.1016/j.ijrobp.2012.07.2379. [DOI] [PubMed] [Google Scholar]


