Short sleep duration, defined as sleeping <7 hours per night, is associated with poor cardiovascular (CVD) outcomes including mortality (1,2). There are known racial disparities for CVD (3) and for sleep health (4). However, racial disparities in the context of short sleep with CVD is an understudied area (2,5). The current study examined whether Black race modifies the association of sleep duration with recurrent CVD risk in patients with a history of acute coronary syndrome (ACS).
722 patients admitted for ACS (defined as ST elevation MI, non-ST elevation MI, or unstable angina) who identified as black (n = 175) or white (n = 547) were enrolled in-hospital and followed for 1 year in a single site, prospective observational cohort during 2009–2012. Columbia University Medical Center’s IRB approved this study.
One month following enrollment, participants completed the Pittsburgh Sleep Quality Index (PSQI). Sleep duration was categorized as short (<7 hours/night) versus average sleep (≥7 hours/night) following previous guidelines (1,2). Major adverse cardiovascular events (MACE) were defined as the composite of death, recurrent MI, or unstable angina.
Hazard ratios (HR) and 95% confidence intervals (CI) for MACE were estimated from a Cox regression model that included sleep duration and race as the primary predictors, their interaction term, with age, sex, GRACE risk score, and Charlson comorbidity index included as covariates, after a preliminary forward selection analysis that considered 20 potential predictors of MACE excluding sleep duration.
At 1-year follow-up, there were 62 recurrent MACE. As previously reported, short sleep duration was associated with increased risk of recurrent MACE (1). Black relative to white race was also associated with increased risk of recurrent MACE in unadjusted and multivariable adjusted models (adjusted HR (95% CI) = 2.14 (1.26–3.63), p = 0.005). Sleep duration was not associated with race in the current sample (p = 0.30). However, there was a significant interaction of race and sleep duration (p = 0.02; Figure 1) such that black patients who regularly slept <7 hours/night 1 month post-ACS had a higher risk for recurrent MACE than white patients who slept ≥7 hours/night (adjusted HR (95%CI) = 2.88 (1.51–5.50), p = 0.001) as well as the other two race × sleep duration subgroups. The interaction remained significant after excluding snorers (≥1/week snoring based on PSQI) and patients with sleep duration >9 hours/night.
Figure 1. Unadjusted Kaplan-Meier Survival Curves (Panel A)**; and Covariate-adjusted Predicted Survival Curves (Panel B)** for Time to MACE by race and sleep duration.
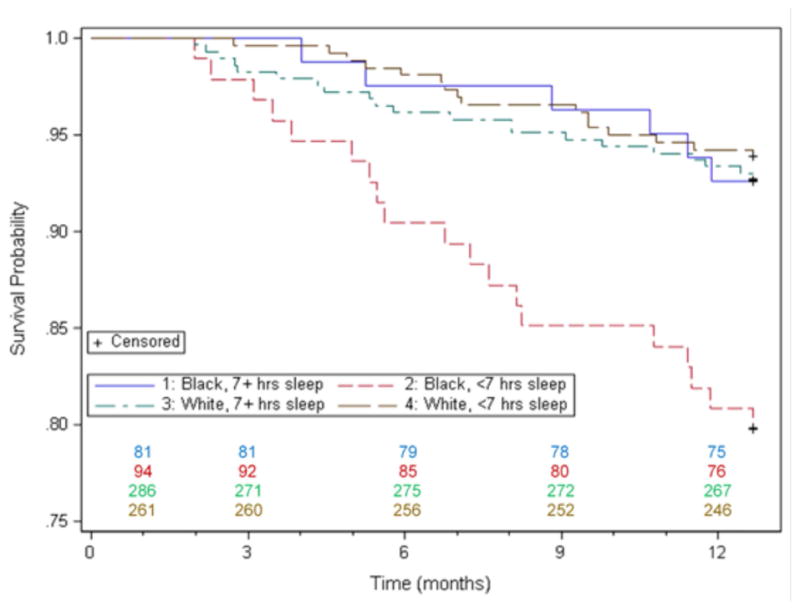
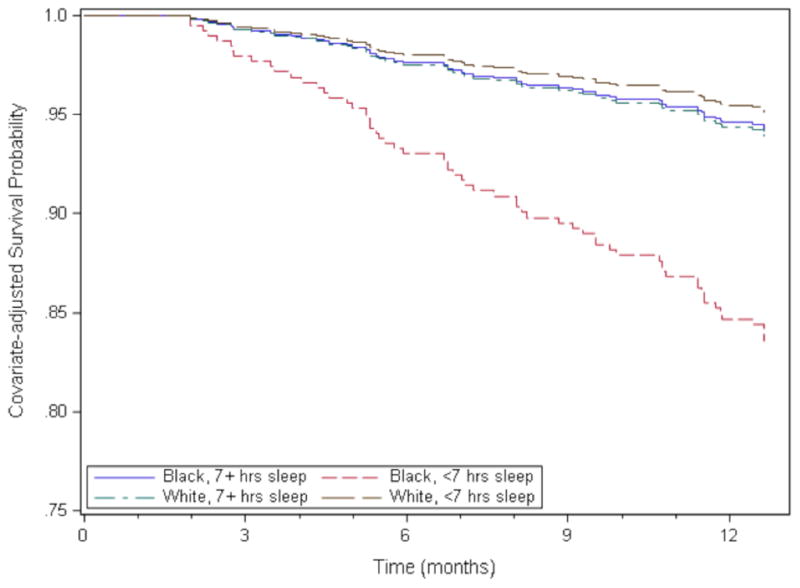
**p<0.001 by log rank test
This study found that the occurrence of MACE was significantly greater among blacks who reported short sleep (<7 hours/night) 1-month post ACS than among whites with short sleep and those who slept 7 hours or more/night (both blacks and whites). There was not a significant difference in sleep duration between blacks and whites in the current sample; however, previous work indicates that Blacks are more than twice as likely to report short sleep duration than whites (4,5). A recent review suggests that sleep may be fundamental to understanding some of the racial disparities in cardiovascular risk (5). These data support and extend that hypothesis, showing that race modifies the adverse cardiac prognosis associated with short sleep duration.
Recent work has begun to delineate possible psychophysiological mechanisms linking short sleep to CVD, including increased allostatic load (2,4) from chronic short sleep contributing to elevated cortisol and inflammation (2). Less is known regarding the mechanisms linking Black race to both CVD and short sleep, although recent proposals have indicated greater exposure to discrimination and neighborhood factors such as noise and reduced safety may be important contributors (2,5).
One limitation of this study is the reliance on self-reported sleep duration. Future work should use multiple measures of sleep, including objective measures. Also, participants were drawn from one particular hospital setting in an urban metropolitan city, potentially limiting generalizability. Despite these limitations, the current report advances the science of cardiovascular health disparities and suggests that sleep may be a potential modifiable behavioral target for reducing racial health disparities.
Abbreviations
- CVD
Cardiovascular Disease
- ACS
Acute Coronary Syndrome
- MI
Myocardial Infarction
- PSQI
Pittsburgh Sleep Quality Index
- MACE
Major Adverse Cardiovascular Events
- HR
Hazard Ratio
- CI
Confidence Interval
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Alcántara C, Peacock J, Davidson KW, Hiti D, Edmondson D. The association of short sleep after acute coronary syndrome with recurrent cardiac events and mortality. Int J Cardiol. 2014;171(2):e11–12. doi: 10.1016/j.ijcard.2013.11.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.St-Onge MP, Grandner MA, Brown D, et al. Sleep Duration and Quality: Impact on Lifestyle Behaviors and Cardiometabolic Health: A Scientific Statement from the American Heart Association. Circulation. 2016;134(18):e367–86. doi: 10.1161/CIR.0000000000000444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Safford MM, Brown TM, Muntner PM, et al. Association of race and sex with risk of incident acute coronary heart disease events. JAMA. 2012;308(17):1768–74. doi: 10.1001/jama.2012.14306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ruiter ME, DeCoster J, Jacobs L, Lichstein KL. Normal sleep in African-Americans and Caucasian-Americans: a meta-analysis. Sleep medicine. 2011;12(3):209–14. doi: 10.1016/j.sleep.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 5.Jackson CL, Redline S, Emmons KM. Sleep as a Potential Fundamental Contributor to Cardiovascular Health Disparities. Annual review of public health. 2015;36:417–440. doi: 10.1146/annurev-publhealth-031914-122838. [DOI] [PMC free article] [PubMed] [Google Scholar]


