Abstract
Importance
Recognizing malpractice trends in the field of dermatology is important for establishing safeguards for patient care and minimizing liability. However, there is a lack of published data on malpractice claims against dermatologists.
Objective
To determine characteristics of medical professional liability claims in the field of dermatology and to compare these claims with those against all physicians.
Design, Setting, and Participants
We examined malpractice liability data collected on dermatologists and other physicians insured by companies that report data to the Physician Insurers Association of America Data Sharing Project (PIAA-DSP), a nationally representative liability claims registry. Data analyzed spanned the years 1991 through 2015.
Main Outcomes and Measures
Demographic characteristics of dermatologists subject to claims, characteristics of closed claims, medical errors associated with closed claims, and patient outcomes leading to closed claims.
Results
Data on a total of 90 743 closed claims were analyzed, 1084 (1.2%) against dermatologists and 89 659 (98.8%) against nondermatologists. More lawsuits were brought against male (n = 753, 69.5%) than female dermatologists (n = 270, 24.9%); 5.6% of claims (n = 61) did not identify the physician’s sex. Full-time practitioners (n = 1035, 95.5%) and those in solo practice (n = 600, 55.4%) were more likely to be sued than those in group practices (n = 429, 39.6%) and institutions (n = 31, 2.9%). Most claims against dermatologists were abandoned, withdrawn, or dismissed (n = 735, 67.8%). Between 2006 and 2015, trial verdicts favoring defendants exceeded trial verdicts favoring plaintiffs by a factor of 7. Errors that occurred during a procedure spawned the most claims (n = 305), of which 102 were paid. Misdiagnoses comprised the second-highest number of claims (n = 192), of which 62 were paid. The average recovery per claim was $238 145. The most common procedure leading to claims was skin operations (420 claims, of which 130 were paid). The most common adverse patient outcome associated with claims was dyschromia, resulting in 171 claims, of which 40 were paid.
Conclusions and Relevance
Male dermatologists were sued more often than female dermatologists. Overall, alleged errors in procedures and misdiagnosis gave rise to the most lawsuits. Dyschromia was the most common adverse outcome alleged in lawsuits.
This study analyzes 24 years of data through 2015 from a nationally representative liability claims registry to compare the medical liability claims against dermatologists vs nondermatologists.
Key Points
Question
What are the characteristics of medical professional liability claims against dermatologists, and how do they compare with claims against physicians in all specialties?
Findings
Analysis of malpractice data from a national registry revealed that improper performance of a procedure and misdiagnosis were the 2 most common medical errors associated with 1084 closed medical liability claims in dermatology and all fields of medicine. Dermatologists were responsible for a small proportion of all closed claims (1.2%) over the past decade.
Meaning
Enhancing dermatologists’ understanding of characteristics of malpractice claims can foster implementation of safeguards that improve patient care and potentially reduce malpractice liability.
Introduction
Medical professional liability affects clinicians in all specialties, and dermatologists are no exception. While dermatologists are generally sued less frequently than those in other specialties, it is estimated that, even for physicians in specialties less prone to litigation, approximately 36% will be sued at least once by age 45 years. Enhancing dermatologists’ awareness of medical malpractice liability can affect clinical decision making and practice. This knowledge can be used to foster improvement in the quality of patient care and reduce the incidence of preventable malpractice claims in the future.
Medical liability is an important topic; however, there is a gap in the literature concerning malpractice lawsuits against dermatologists. A previous study using data from 1985 through 2008 showed that dermatologists were responsible for 1.1% of all closed liability claims across specialties. The health care landscape has changed since then, and we currently lack data on malpractice trends during this time. With this update, we aim to examine characteristics of medical professional liability claims in dermatology and compare medical professional liability lawsuits against dermatologists with those against physicians in all specialties.
Methods
To examine professional liability risks among dermatologists, we used data gathered by the Physician Insurers Association of America (PIAA) in Rockville, Maryland. The Data Sharing Project (DSP) is a registry of claims information from PIAA member organizations. These organizations include multiple malpractice insurance companies, which submit claims data to the DSP twice each year. The PIAA collects claims information involving physicians, residents, and advanced practice professionals (nurse practitioners and physician assistants) in 28 physician specialties, including dermatology.
The PIAA-DSP collects numerous data points, including the number of closed claims, outcomes that lead to resolution of claims, paid claims, and total recovery. The term claims refers to lawsuits that have been filed. Closed claims are lawsuits that have been resolved. For a claim to be closed, it must fall within 1 of the following 3 categories: (1) the lawsuit is filed but is subsequently abandoned, withdrawn, or dismissed; (2) the lawsuit is settled; or (3) the lawsuit goes to trial and results in a verdict. Closed claims are distinct from paid claims. A closed claim does not necessarily result in compensation for the claimant (the individual filing the lawsuit). In a paid claim, recovery refers to compensation given to the claimant from the defendant or the defendant’s insurer to cover the claimant’s damages. Damages refers to compensation for injuries to the claimant that may include past and future medical costs, lost wages, emotional distress, and pain and suffering.
The PIAA-DSP also gathers information regarding chief medical factors, or specific medical errors that lead to claims. Adverse patient outcomes commonly responsible for lawsuits are also recorded in terms of summary statistics and costs.
We used claims data from 2006 through 2015 to analyze physician characteristics associated with closed claims. We compared physician characteristics for dermatologists with those in all health care specialties. We assessed yearly and aggregate statistics for closed claims, paid claims, and total, average, and largest recovery against dermatologists between 1991 and 2015. Using the available data reported between 2006 and 2015, we examined medical errors and patient outcomes that were most prevalent and expensive. These data parameters were analyzed for dermatologists and compared with those of practitioners in all health care specialties. Data regarding physician characteristics, errors, and outcomes were not available from 1991 through 2004. Institutional review board approval was not requested or obtained because we used database information that could be acquired by the public. Therefore, no written informed consent was required.
Results
Clinician Characteristics Associated With Closed Claims Between 2006 and 2015
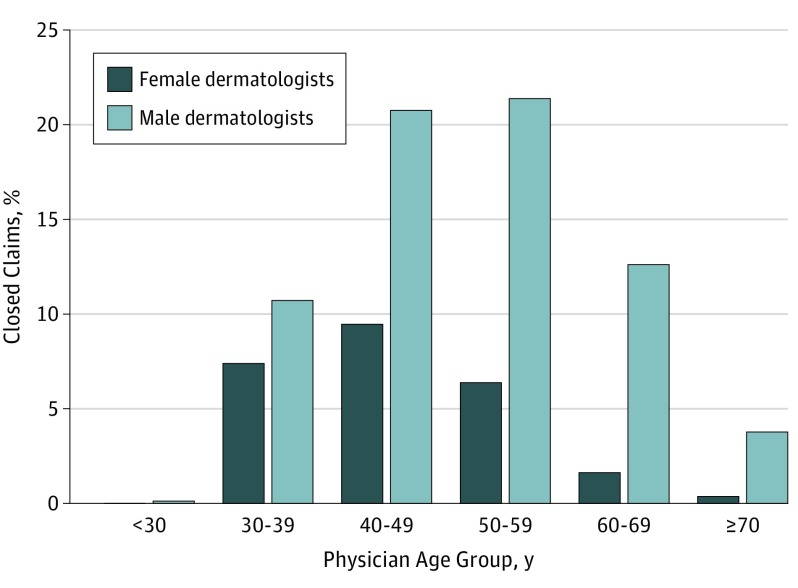
Understanding the demographic characteristics of dermatologists in the registry is important for risk management. A total of 52.9% of dermatologists are male. Between 2006 and 2015, disproportionately more lawsuits were brought against male dermatologists than female dermatologists (753 of 1084, 69.5% vs 270 of 1084, 24.05%; 5.6% of claims, n = 61, did not identify the physician’s sex). This sex imbalance was also seen in other specialties, where 77.3% of closed claims (n = 70 125) involved male defendants. When stratified by sex and age, we found that among male dermatologists, those aged 50 to 59 years had the greatest number of closed claims (232 of 1084, 21.4%) (Figure). Among female dermatologists, those aged 40 to 49 years had the greatest number of closed claims (102 of 1084, 9.4%).
Figure. Percentage of Liability Claims Closed by Physician Age Group and Sex (2006-2015).
Male dermatologists aged 50 to 59 years had the greatest number of closed claims (21.4%; n = 232). For female dermatologists, those aged between 40 and 49 years had the greatest number of closed claims (9.4%; n = 102).
Most closed claims were filed against full-time dermatologists (1035 of 1084, 95.5%), which was similar to the findings among physicians in all specialties (87 271 of 90 743, 96.2%). As to practice setting, most closed claims were filed against dermatologists in solo practices (600 of 1084, 55.4%), followed by group practices (429 of 1084, 39.6%), and institutions (31 of 1084, 2.9%). In contrast, for all specialties, most closed claims were filed against physicians belonging to group practices (45 952 of 90 743, 50.6%), followed by solo practices (36 798 of 90 743, 40.6%) and institutions (4787 of 90 743, 5.3%). The registry also analyzed claims data based on the physician’s country of medical education. We found that most closed claims were filed against dermatologists who received their medical education in the United States (840 of 1084, 77.5%), likely because most dermatologists have been educated in the United States.
Claims Outcomes Between 2006 and 2015
Between 2006 and 2015, most claims against dermatologists were abandoned, withdrawn, or dismissed (735 of 1084, 67.8%). Less prevalent means of resolving claims included settlement (261 of 1084, 24.1%), trial verdict favoring the defense (45 of 1084, 4.2%), unknown (21 of 1084, 1.9%), dispute resolution or contract (16 of 1084, 1.5%), and trial verdict favoring the plaintiff (6 of 1084, 0.6%). Notably, trial verdicts favoring defendants exceeded trial verdicts favoring plaintiffs by a factor of 7. A similar distribution was reported for all medical specialties.
Contribution of Dermatology Claims to Overall Medical Professional Liability
Assessing the proportion of closed claims against dermatologists helps to define the extent to which dermatology contributes to the overall medical professional liability burden. The Association of American Medical Colleges reports that dermatologists make up 1.4% of all physicians. As documented in the PIAA-DSP, dermatologists have accounted for only a small percentage of the number of closed claims against practitioners from all specialties during the past decade. Between 2006 and 2015, dermatologists were sued in only 1084 of the 90 743 closed claims against physicians in all specialties (1.2% of total closed claims), ranking dermatology at 21 of the 28 specialties in the registry. Over the last 20 years, there has been a 2.5% net reduction in the number of closed claims against dermatologists, which was less than the 17.9% reduction seen for all specialties.
In the present study, dermatologists were responsible for only a small percentage of paid claims from all specialties, representing 281 of 24 106 paid claims (1.2%) between 2006 and 2015. Furthermore, analysis of the last 2 decades of data reveals net 29.2% and 31.2% decreases in the number of paid claims against dermatologists and physicians from all specialties, respectively.
Total, Average, and Largest Recovery
To understand the financial burden of malpractice claims, it is helpful to assess the proportion of claims that resulted in recoveries. Between 2006 and 2015, recovery was paid in 25.9% of closed claims for dermatologists (281 of 1084) and 26.6% of closed claims for all specialties (24 106 of 90 743).
Total recovery represents the aggregated sum of payments made to all claimants. From 2006 through 2015, the total recovery against dermatologists was $71 819 605, which represents 0.8% of the total recovery for all specialties.
The average recovery is the mean payment made to claimants. From 2006 through 2015, the average recovery paid by dermatologists was $238 145, which is lower than the $335 578 average recovery for all specialties. Notably, analysis of the last 20 years of data showed a net 51.4% increase in the average recovery against dermatologists, compared with an increase of 18.0% against physicians in all specialties.
The largest recovery is the highest amount of compensation paid to a claimant to resolve a lawsuit. From 2006 through 2015, the largest payment made by an insurer on behalf of a dermatologist was $2 611 554, which is substantially lower than the $13 000 000 largest payment for all specialties. Over the last 20 years, the largest recovery for all specialties, including dermatology, increased by a factor of approximately 1.6.
Most Common and Expensive Medical Errors Between 2006 and 2015
Claims can be categorized by practitioner errors or adverse outcomes that prompted patients to file claims. Of the patient outcomes leading to claims, some resulted from medical errors, others from proper clinical interventions.
It is imperative for dermatologists to become familiar with the most common errors made by their colleagues so that necessary precautions may be taken to protect against liability. The registry indicates that errors occurring during procedures resulted in the most closed claims (n = 305, of which 102 were paid) (Table 1). The second most common error was misdiagnosis, which resulted in 192 closed claims, of which 62 were paid, and the largest total recovery, which was $29 052 182.
Table 1. Top 10 Medical Errors Resulting in Dermatology Liability Claims (2006-2015).
| Medical Error | Closed Claims, No. | Paid Claims, No. | Total Recovery, $ |
|---|---|---|---|
| Improper performance of procedures | 305 | 102 | 13 112 486 |
| Errors in diagnosis | 192 | 62 | 29 053 182 |
| Medication errors | 71 | 23 | 5 370 500 |
| Failure to supervise or monitor case | 51 | 15 | 2 233 156 |
| Failure to recognize a complication of treatment | 40 | 15 | 4 513 499 |
| Improper supervision of residents or other staff | 34 | 10 | 1 325 874 |
| Procedure performed when not indicated or contraindicated | 21 | 11 | 680 640 |
| Failure to instruct or communicate with patient | 18 | 15 | NR |
| Wrong patient or body part | 13 | 8 | 177 849 |
| Failure or delay in referral or consultation | 10 | 5 | 1 099 000 |
Abbreviation: NR, not reported.
Most Common and Expensive Procedures Resulting in Claims Between 2006 and 2015
Procedures can range from history taking and physical examination to prescribing medications and surgical interventions. Operative skin procedures led to the most closed claims (n = 420, of which 130 were paid), as well as the highest recovery of $22 872 950 (Table 2). Diagnostic skin procedures led to the second most closed claims (n = 129, of which 36 were paid).
Table 2. Top 10 Procedures Resulting in Dermatology Liability Claims (2006-2015).
| Medical Procedure | Closed Claims, No. | Paid Claims, No. | Total Recovery, $ |
|---|---|---|---|
| Operative procedures on the skin, excluding skin grafts | 420 | 130 | 22 872 950 |
| Diagnostic procedures of the skin | 129 | 36 | 11 726 804 |
| Prescription of medication | 95 | 29 | 10 077 800 |
| Diagnostic interview, evaluation, or consultation | 90 | 7 | 2 249 999 |
| General physical examination | 62 | 17 | 6 597 498 |
| Injections and vaccinations | 39 | 7 | 800 500 |
| Miscellaneous physical procedures | 24 | 9 | 860 990 |
| Microscopic examinations | 16 | 5 | 1 555 001 |
| Operative procedures involving blood vessels, excluding heart | 8 | 2 | 102 500 |
| Operative procedures on nose, nasal bones, or nasal cavity |
6 | NR | NR |
Abbreviation: NR, not reported.
Most Common and Expensive Patient Outcomes Resulting in Claims Between 2006 and 2015
Adverse patient outcomes refer to adverse results of medical errors or proper interventions. The most common adverse patient outcome was dyschromia, resulting in 171 closed claims, of which 40 were paid (Table 3). The second most common adverse outcome was malignant neoplasms of the skin, resulting in 127 closed claims, of which 43 were paid. Malignant neoplasms of the skin also resulted in the largest total recovery, which was $13 035 997.
Table 3. Top 10 Adverse Outcomes Resulting in Dermatology Liability Claims (2006-2015).
| Adverse Outcome | Closed Claims, No. | Paid Claims, No. | Total Recovery, $ |
|---|---|---|---|
| Dyschromia | 171 | 40 | 2 467 892 |
| Malignant neoplasms of the skin | 127 | 43 | 13 035 997 |
| Malignant melanoma | 58 | 22 | 10 008 001 |
| Burn of face, head, or neck | 34 | 11 | 701 500 |
| Emotional distress only | 33 | 7 | 1 034 761 |
| Postoperative infection | 23 | 3 | 717 500 |
| Unhappy with results of plastic surgery | 17 | 2 | NR |
| Substance not elsewhere classified | 12 | 1 | NR |
| Cardiac or cardiorespiratory arrest | 9 | 4 | 1 950 000 |
| Desire for plastic surgery | 9 | 1 | NR |
Abbreviation: NR, not reported.
Discussion
In this comprehensive study of claims data in the field of dermatology between 1991 and 2015, most malpractice cases against dermatologists were abandoned, withdrawn, or dismissed. There was a net 29.2% reduction in paid claims for dermatologists and a comparable reduction for physicians of all specialties between the 1991-1995 period and the 2011-2015 period. The largest payment made by a dermatologist’s insurer from 2006 through 2015 was $2 611 554. A mistake while performing a procedure was the most common medical error leading to a claim. Misdiagnosis was the second most common medical error and the one associated with the highest recovery. The most common patient outcome resulting in claims was dyschromia. A tertiary finding was that male dermatologists were named as defendants more frequently than female dermatologists. Most male and female dermatologists who were sued were aged 50 to 59 years and 40 to 49 years, respectively. There were higher rates of closed claims among solo dermatology practitioners than among other types.
The finding that most malpractice cases were abandoned, withdrawn, or dismissed may be explained by the burden of medical malpractice litigation being on the plaintiff to prove the following 4 elements: (1) the physician owed the patient a duty of care; (2) the physician breached this duty; (3) the breach caused the plaintiff injury or harm; and (4) the plaintiff suffered physical, emotional, and/or financial damages as a result of the injury. Proving negligence is often difficult.
The net reduction found in paid claims for dermatologists and all specialties between the 1991-1995 and 2011-2015 periods supports the downward trend in paid claims documented in other studies. Several factors may have contributed to this decline in paid claims over time. Tort reforms passed in the interim, including caps on damages and statutes of limitation, are one potential explanation. Caps on damages refers to a maximum limit on the amount of recovery a plaintiff can receive. If the potential recovery does not justify the legal expenses associated with pursuing a claim through trial, the plaintiff is likely to abandon the claim. However, investigators have had difficulty consistently linking declines in paid claims with such reforms.
Another possible explanation is the implementation of patient safety practices, such as organized handoffs and checklists, which may reduce medical error rates. Disclosure, apology, and offer programs, in which compensation is made to a patient before the patient files a formal claim, are also gaining popularity and may explain this decline in paid claims.
After searching the Westlaw database for trial verdicts from 2006 through 2015, we found that the largest recovery against a dermatologist was $10 500 000. In this case, the dermatologist did not recognize an invasive basal cell carcinoma, resulting in severe morbidity for the patient. Malpractice insurance for most physicians only covers up to $1 000 000 per case and $3 000 000 per year. While the largest recovery against a dermatologist from 2006 through 2015 exceeded $10 million, the largest amount paid by an insurer in this timespan was reported to be $2 611 554. If a patient’s monetary damages exceed the physician’s insurance coverage, the physician may have to personally cover the excess damages. In the rare instances in which this occurs, excess damages are not usually high enough to lead to bankruptcy. For example, in an 18-year period in Texas, only 77 of 12 383 closed claims required physicians to make out-of-pocket payments. Only 19 of these out-of-pocket payments exceeded $250 000, possibly because many defendants will accept settlement offers within insurance coverage limits to avoid the risk of going to trial.
To translate malpractice claims data into improved patient care, it is critical to know what errors are made and which adverse outcomes more often lead to litigation. An error that occurs while performing a procedure is the most common medical error leading to a claim. Dermatologists perform an increasingly large number of procedures, and some of these can lead to lasting and measurable adverse outcomes. Survey data from 1995 through 2010 reveal that an average of 26.8 million dermatologic procedures were performed each year. Of those procedures, 91% were noncosmetic. The most common noncosmetic procedures included local excisions and biopsies; the most common cosmetic procedure was botulinum toxin injection. The finding that operative and diagnostic skin procedures resulted in the most claims may be a reflection of the fact that these procedures are performed most frequently. An increasingly large number of nondermatologists are performing dermatologic procedures. In a study that compared lawsuits between dermatologists and nondermatologists for the procedure of laser hair removal, board-certified dermatologists performed two-thirds of these procedures and were responsible for a quarter of the liability claims.
The most common patient outcome resulting in claims was dyschromia, which was an important finding because clinicians may not associate dyschromia with substantial morbidity. This finding suggests that clinician and patient perception of adverse outcomes may differ. Also, properly informing patients of potential adverse effects from medical or procedural treatments is critical. For example, drugs like tetracycline, and procedures such as laser therapy and chemical peels, can cause dyschromia.
Preventive measures to avoid procedural and diagnostic errors include eliciting a thorough history, assessing for personal biases, and creating safety guidelines (Table 4). There are also ways to minimize the risk of liability when adverse outcomes do occur, such as contritely disclosing the error, addressing the error, and maintaining a strong relationship with the patient and family.
Table 4. Safeguards to Minimize Liability.
| Safeguards to Minimize Liability | Explanation | Sample From Which Safeguard Was Derived |
|---|---|---|
| Establish strong rapport with each patient by engaging in patient-centered communication | Strong rapport with one’s patients is a key protective factor against being sued. Patient-centered communication facilitates development of this rapport. This type of communication involves eliciting and validating patient input and providing encouragement and reassurance. | 59 Primary care physicians |
| Elicit a thorough history to help avoid misdiagnosis | 40% of clinicians indicated that they could attribute diagnostic errors to inadequate history elicitation. It is essential for a physician to effectively communicate with the patient at this point of clinical assessment. | Survey of 4613 physicians of all specialties, 1025 nurse practitioners, and 512 physician assistants |
| Assess for anchoring bias to help avoid misdiagnosis | This is 1 of the 2 most common biases linked with diagnostic errors. Anchoring bias is relying on the first diagnosis that comes to mind, even if new evidence discredits that diagnosis. | 41 Internal medicine residents |
| Assess for availability bias to help avoid misdiagnosis | Availability bias entails arriving at the most common diagnosis without fully exploring the possibility of less common diagnoses. | 41 internal medicine residents |
| Reconsider differential diagnoses to help avoid misdiagnosis | Physicians should ask themselves if there is information that conflicts with their diagnosis, if other diagnoses could be justified, or if multiple diagnoses could simultaneously be responsible. | 100 Cases of diagnostic error involving internal medicine physicians |
| Treatment plans should be effectively communicated to the patient | The clinician must bear in mind that the health literacy of 36% of the population is below intermediate level. Thus, clinicians should take extra care to ensure that each patient fully understands the treatment plan. | Not Based on a specific study sample |
| Effectively counsel each patient before performing any intervention | Patients may be more likely to sue if they are caught off guard by an adverse outcome. Communicating potential adverse outcomes may help reduce the risk of lawsuits. | 2704 Closed claims involving dermatologists |
| Obtain additional training for high-risk procedures and create safety guidelines to help prevent errors while performing a procedure | Dermatologists can follow examples established in other fields to reduce liability associated with high-risk procedures. For example, a safety protocol implemented by obstetricians over a 10-year prospective study reduced the number of claims by more than half. | 44 Claims involving obstetricians |
| Disclose medical errors to the affected patient | More patients asserted that they would pursue litigation if they found out a physician concealed an error than if the physician notified them of an error. | Survey of 149 internal medicine patients |
| Provide appropriate care to address adverse outcomes and maintain a good relationship with the patient and family | A 2015 survey found that 35% of physician respondents reported that their patients who experienced adverse outcomes did not pursue litigation. The majority of the physicians attributed this result to having established strong rapport with the patient prior to the incident, providing appropriate care to address the adverse outcome, and maintaining a good relationship with the patient and the patient’s family after the incident. | Survey of 2276 physicians of all specialties |
As of 2015, there were 11 696 practicing dermatologists in the United States, 52.9% of whom were male. In our study, male dermatologists were sued more frequently than female dermatologists. Other studies have suggested similar findings. Unwin et al found that male physicians across medical specialties were 2.5 times more likely to be sued in medical malpractice actions than female physicians. It has been postulated that a strong rapport with one’s patients is a key protective factor against being sued, and that effective communication facilitates development of this rapport. A meta-analysis on sex differences in medical communication found that female physicians are more likely to actively engage in “patient-centered” communication. That is, female physicians more often elicit and validate patient input and provide encouragement and reassurance. All physicians can practice and improve patient-centered communication, which may help enhance patient satisfaction and outcomes. Most male and female dermatologists who were sued were aged 50 to 59 years and 40 to 49 years, respectively. This correlates with the finding that most practicing male dermatologists are aged 50 to 59 years, and most practicing female dermatologists are aged 40 to 49 years.
Dermatologists practicing in institutions faced fewer claims than those in other practice settings, which may be because institutions often have legal departments that implement disclosure, apology, and offer programs. Also, patients may sue the institution, which has greater financial resources than the dermatologist responsible.
Limitations
The PIAA-DSP database is a nationally representative registry that provides comprehensive data on closed claims across medical specialties in the United States. However, these data have limitations. Not all information regarding physician and claims characteristics was available. For example, 5.6% of claims (n = 61) did not identify the physician’s sex. Also, 14.7% of claims (n = 159) did not identify the country in which the physicians received their medical education. Additionally, the database treated settlement and alternative dispute resolution or contract as separate categories, even though many would consider them synonymous.
Conclusions
Handling medical malpractice liability claims can be a stressful and costly process. Determining characteristics of medical liability claims is the first step toward identifying areas of improvement to enhance patient outcomes, minimize patient harm, and decrease clinician liability. Future studies need to focus on evidence-based interventions to reduce claims and improve dermatologists’ competencies in communication and clinical skills.
References
- 1.Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011;365(7):629-636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moshell AN, Parikh PD, Oetgen WJ. Characteristics of medical professional liability claims against dermatologists: data from 2704 closed claims in a voluntary registry. J Am Acad Dermatol. 2012;66(1):78-85. [DOI] [PubMed] [Google Scholar]
- 3.D’Souza LS, Jalian HR, Jalian C, et al. . Medical professional liability claims for Mohs micrographic surgery from 1989 to 2011. JAMA Dermatol. 2015;151(5):529-532. [DOI] [PubMed] [Google Scholar]
- 4.Jalian HR, Jalian CA, Avram MM. Common causes of injury and legal action in laser surgery. JAMA Dermatol. 2013;149(2):188-193. [DOI] [PubMed] [Google Scholar]
- 5.Jalian HR, Jalian CA, Avram MM. Increased risk of litigation associated with laser surgery by nonphysician operators. JAMA Dermatol. 2014;150(4):407-411. [DOI] [PubMed] [Google Scholar]
- 6.Bal BS. An introduction to medical malpractice in the United States. Clin Orthop Relat Res. 2009;467(2):339-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Association of American Medical Colleges (AAMC) 2016. Physician Specialty Data Report. https://www.aamc.org/data/workforce/reports/457712/2016-specialty-databook.html. Accessed September 27, 2017.
- 8.Mello MM, Studdert DM, Kachalia A. The medical liability climate and prospects for reform. JAMA. 2014;312(20):2146-2155. [DOI] [PubMed] [Google Scholar]
- 9.Schaffer AC, Jena AB, Seabury SA, Singh H, Chalasani V, Kachalia A. Rates and characteristics of paid malpractice claims among us physicians by specialty, 1992-2014. JAMA Intern Med. 2017;177(5):710-718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kachalia A, Mello MM. New directions in medical liability reform. N Engl J Med. 2011;364(16):1564-1572. [DOI] [PubMed] [Google Scholar]
- 11.Haynes AB, Weiser TG, Berry WR, et al. ; Safe Surgery Saves Lives Study Group . A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360(5):491-499. [DOI] [PubMed] [Google Scholar]
- 12.Pronovost PJ, Cleeman JI, Wright D, Srinivasan A. Fifteen years after To Err is Human: a success story to learn from. BMJ Qual Saf. 2016;25(6):396-399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Starmer AJ, Spector ND, Srivastava R, et al. ; I-PASS Study Group . Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803-1812. [DOI] [PubMed] [Google Scholar]
- 14.Kachalia A, Kaufman SR, Boothman R, et al. . Liability claims and costs before and after implementation of a medical error disclosure program. Ann Intern Med. 2010;153(4):213-221. [DOI] [PubMed] [Google Scholar]
- 15.Anderson vs Gruber, 28 NJ. J.V.R.A. 8:C1, 2007 WL 8026109 (N.J. Super. L.).
- 16.Silver C, Hyman DA, Black BS, Paik M. Policy limits, payouts, and blood money: Medical malpractice settlements in the shadow of insurance. UC Irvine Law Rev. 2015;5(3):559-586. [Google Scholar]
- 17.Hyman DA, Black B, Silver C. Settlement at policy limits and the duty to settle: evidence from Texas. J Empir Leg Stud. 2011;8(1):48-84. [Google Scholar]
- 18.Ahn CS, Davis SA, Dabade TS, Williford PM, Feldman SR. Noncosmetic skin-related procedures performed in the United States: an analysis of national ambulatory medical care survey data from 1995 to 2010. Dermatol Surg. 2013;39(12):1912-1921. [DOI] [PubMed] [Google Scholar]
- 19.Callender VD, St Surin-Lord S, Davis EC, Maclin M. Postinflammatory hyperpigmentation: etiologic and therapeutic considerations. Am J Clin Dermatol. 2011;12(2):87-99. [DOI] [PubMed] [Google Scholar]
- 20.Dereure O. Drug-induced skin pigmentation. Epidemiology, diagnosis and treatment. Am J Clin Dermatol. 2001;2(4):253-262. [DOI] [PubMed] [Google Scholar]
- 21.Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Proc (Bayl Univ Med Cent). 2003;16(2):157-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levinson W, Roter DL, Mullooly JP, Dull VT, Frankel RM. Physician-patient communication: the relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997;277(7):553-559. [DOI] [PubMed] [Google Scholar]
- 23.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA. 2002;288(6):756-764. [DOI] [PubMed] [Google Scholar]
- 24.MacDonald OW. Physician perspective on preventing diagnostic error. https://www.quantiaMD.com. Accessed May 2, 2017.
- 25.Rush JL, Helms SE, Mostow EN. The CARE approach to reducing diagnostic errors. Int J Dermatol. 2017;56(6):669-673. [DOI] [PubMed] [Google Scholar]
- 26.Graber ML, Franklin N, Gordon R. Diagnostic error in internal medicine. Arch Intern Med. 2005;165(13):1493-1499. [DOI] [PubMed] [Google Scholar]
- 27.Pettker CM, Thung SF, Lipkind HS, et al. . A comprehensive obstetric patient safety program reduces liability claims and payments. Am J Obstet Gynecol. 2014;211(4):319-325. [DOI] [PubMed] [Google Scholar]
- 28.Witman AB, Park DM, Hardin SB. How do patients want physicians to handle mistakes? a survey of internal medicine patients in an academic setting. Arch Intern Med. 1996;156(22):2565-2569. [PubMed] [Google Scholar]
- 29.Paskewich B, McCormack J MLMIC’s Claims Free Discount Survey Results. Dateline: A Newsletter for MLMIC-Insured Physicians & Facilities. Vol 14: Medical Liability Mutual Insurance Co (MLMIC); 2015:6-7. https://www.mlmic.com/wp-content/uploads/2014/04/Dateline-Fall-2015.pdf. Accessed September 27, 2017.
- 30.Unwin E, Woolf K, Wadlow C, Potts HW, Dacre J. Sex differences in medico-legal action against doctors: a systematic review and meta-analysis. BMC Med. 2015;13:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jacobson CC, Resneck JS Jr, Kimball AB. Generational differences in practice patterns of dermatologists in the United States: implications for workforce planning. Arch Dermatol. 2004;140(12):1477-1482. [DOI] [PubMed] [Google Scholar]