Key Points
Question
How common are fetal alcohol spectrum disorders in the United States?
Findings
In this cross-sectional study of 13 146 first-grade children in 4 regions of the United States surveyed between 2010 and 2016, the most conservative prevalence estimate for fetal alcohol spectrum disorders ranged from 11.3 to 50.0 per 1000 children. Using a weighted approach, the estimated prevalence was 31.1 to 98.5 per 1000 children.
Meaning
These findings may represent more accurate US prevalence estimates than previous studies but may not be generalizable to all communities.
Abstract
Importance
Fetal alcohol spectrum disorders are costly, life-long disabilities. Older data suggested the prevalence of the disorder in the United States was 10 per 1000 children; however, there are few current estimates based on larger, diverse US population samples.
Objective
To estimate the prevalence of fetal alcohol spectrum disorders, including fetal alcohol syndrome, partial fetal alcohol syndrome, and alcohol-related neurodevelopmental disorder, in 4 regions of the United States.
Design, Setting, and Participants
Active case ascertainment methods using a cross-sectional design were used to assess children for fetal alcohol spectrum disorders between 2010 and 2016. Children were systematically assessed in the 4 domains that contribute to the fetal alcohol spectrum disorder continuum: dysmorphic features, physical growth, neurobehavioral development, and prenatal alcohol exposure. The settings were 4 communities in the Rocky Mountain, Midwestern, Southeastern, and Pacific Southwestern regions of the United States. First-grade children and their parents or guardians were enrolled.
Exposures
Alcohol consumption during pregnancy.
Main Outcomes and Measures
Prevalence of fetal alcohol spectrum disorders in the 4 communities was the main outcome. Conservative estimates for the prevalence of the disorder and 95% CIs were calculated using the eligible first-grade population as the denominator. Weighted prevalences and 95% CIs were also estimated, accounting for the sampling schemes and using data restricted to children who received a full evaluation.
Results
A total of 6639 children were selected for participation from a population of 13 146 first-graders (boys, 51.9%; mean age, 6.7 years [SD, 0.41] and white maternal race, 79.3%). A total of 222 cases of fetal alcohol spectrum disorders were identified. The conservative prevalence estimates for fetal alcohol spectrum disorders ranged from 11.3 (95% CI, 7.8-15.8) to 50.0 (95% CI, 39.9-61.7) per 1000 children. The weighted prevalence estimates for fetal alcohol spectrum disorders ranged from 31.1 (95% CI, 16.1-54.0) to 98.5 (95% CI, 57.5-139.5) per 1000 children.
Conclusions and Relevance
Estimated prevalence of fetal alcohol spectrum disorders among first-graders in 4 US communities ranged from 1.1% to 5.0% using a conservative approach. These findings may represent more accurate US prevalence estimates than previous studies but may not be generalizable to all communities.
This community-based cohort study used active-case ascertainment to estimate the prevalence of fetal alcohol spectrum disorders among first-graders living in 4 diverse communities in the United States.
Introduction
Fetal alcohol spectrum disorders, composed of fetal alcohol syndrome, partial fetal alcohol syndrome, and alcohol-related neurodevelopmental disorder, are leading causes of developmental disabilities worldwide. The commonly accepted estimate for the United States of 10 per 1000 children affected was derived from clinic-based studies or studies of single communities using small samples and different research methods.
Estimating the prevalence of fetal alcohol spectrum disorders is challenging using routine surveillance methods; one recent US study suggested that children with fetal alcohol spectrum disorders are frequently not diagnosed (80%) or misdiagnosed (7%). As a result, standard methods of passive record surveillance or clinic-based studies may have led to underestimates.
By contrast, active-case ascertainment methods that have been applied in several other countries have resulted in higher prevalence estimates. Similarly, a 2007-2009 single-site, active-case ascertainment study conducted in US communities showed a prevalence rate for fetal alcohol syndrome and partial fetal alcohol syndrome of 10.0 per 1000 children; another 2010-2011 single site, active-case ascertainment study showed a prevalence rate for fetal alcohol spectrum disorders of 24.0 per 1000 children. These data have highlighted the need for a larger study with broader representation of US communities with general population samples.
In 2010, the US National Institute on Alcohol Abuse and Alcoholism initiated the Collaboration on Fetal Alcohol Spectrum Disorders Prevalence consortium, which was challenged to use the best available research methods to establish prevalence estimates in US communities. These data are needed to help determine the public health burden, identify the need for clinical resources, and establish a baseline prevalence against which to measure progress in prevention.
This article describes the prevalence of fetal alcohol spectrum disorders across 4 US sites using an active case–ascertainment approach and applying standardized consensus criteria for case classification.
Methods
Two research teams, both funded by the National Institute on Alcohol Abuse and Alcoholism to establish the consortium, were charged with determining the prevalence of fetal alcohol spectrum disorders in US communities using similar sampling methods and identical assessment and classification criteria. To this end, the investigators were asked to establish and implement a common set of standards to define fetal alcohol spectrum disorders, including full or partial fetal alcohol syndrome and alcohol-related neurodevelopmental disorder.
Study Design
Active-case ascertainment with a cross-sectional design was used at 4 community sites, a convenience sample that was selected based on the investigators’ ability to engage the individual communities and on the feasibility of conducting the study in that community. In each site, first-grade children in public and private schools were recruited across 2 academic years, yielding 8 independent samples. Data collection took place between November 15, 2010, and July 12, 2016.
Study Population, Ethics, and Assessment of Participants
Four study sites, representing diverse areas of the United States, included a Midwest community with a population of 172 000, a Rocky Mountain site with a population of 60 000, a Southeast site with a population of 206 000, and an urban city in the Pacific Southwest with a population of 1.4 million (for additional demographic details, see eTable 1 in the Supplement). The specific locations of the sites could not be disclosed due to confidentiality requirements of the community and school administrators at the sites.
Study approvals were secured from school administrators at each site, and institutional review board approvals were obtained at the investigators’ respective academic institutions. Federal certificates of confidentiality were obtained from the National Institutes of Health. Parents or guardians provided oral or written informed consent for screening and written consent for full evaluations; children 7 years or older provided written assent. Participants were provided monetary and nonmonetary incentives for study completion that were commensurate with the amount of time and travel required to complete the study. Parents or guardians received summary information on their child’s evaluations and were provided referrals for services.
Assessment tools were selected for the 4 domains germane to the spectrum of fetal alcohol spectrum disorders: growth, dysmorphology, neurodevelopment, and prenatal alcohol exposure.
Dysmorphology was evaluated by a team of experienced dysmorphologists or clinical geneticists. The dysmorphologists were blinded to the child’s prenatal alcohol history and neurodevelopmental performance at the time of the examinations. Children were measured for weight, height, and head circumference and were evaluated for the facial features of fetal alcohol syndrome and other minor anomalies using a standard checklist (eFigure 1 in the Supplement). Neurodevelopmental performance was assessed by school psychologists or study psychometrists using a cognitive and behavioral testing battery of standardized, age-appropriate instruments available in English and Spanish and suitable for single-session administration. The selected tests evaluated cognition, academic achievement, behavior, and adaptive skills (eFigure 2 in the Supplement).
Prenatal alcohol exposure was assessed through maternal interviews conducted by trained study staff, in person or over the telephone. Alcohol consumption questions were embedded in a common core of queries regarding maternal health. Specific questions assessed alcohol use prior to pregnancy recognition and during pregnancy, by quantity, frequency, and gestational timing. Social, legal, or medical problems related to alcohol were included as indicators of alcohol use. Interview data were collected from consented collateral sources, such as a close relative, if the biological mother was absent. Cofactors of maternal risk were also captured, including demographics, prenatal care, maternal nutrition, and tobacco and recreational drug use. Preexisting neurobehavioral diagnoses were elicited from parents or guardians. Race/ethnicity was captured as one of the demographic characteristics for an epidemiological study. Race/ethnic group was obtained from the parent or guardian of the participating child and categorized according to predefined National Institutes of Health categories.
Standardized Classification Criteria
Classification criteria based on facial features, growth, and child performance were selected by consensus among consortium members. The clinical criteria were consistent with the published “Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders.” However, as applied in this epidemiological study, a less stringent cutoff of more than 1 standard deviation below the mean for specific learning impairment was used as 1 of the criteria for fetal alcohol spectrum disorders. This modification was adopted by the consortium to represent a balance of sensitivity and specificity for classification among children in the first-grade age range (eBox in the Supplement).
Cutoff criteria defining risky levels of alcohol consumption in pregnancy were also established. Although documented alcohol exposure was not required when children had sufficient physical traits to be classified as having full or partial fetal alcohol syndrome, alcohol exposure during pregnancy at the predefined cutoff levels was required for alcohol-related neurodevelopmental disorder.
Sampling Methods
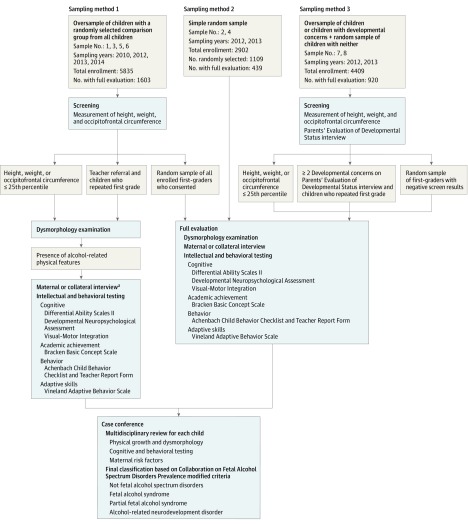
Sampling and consenting processes varied across sites and academic years based on local agreement, school access requirements, and policies resulting in the different sampling methods that were used (Figure).
Figure. Sampling Methods, Evaluations, and Review of First-Graders for Diagnosing Fetal Alcohol Syndrome Disorders .
aCollateral interviews were conducted with close relatives or others when the biological mother was not available.
In sampling method 1, used at the Midwest and Rocky Mountain sites, all elementary schools in the school district participated. At the Southeastern county site, all 5 schools in 1 school district participated; in the second school district in the county, 9 of 19 elementary schools were randomly selected for participation. All first-grade children whose parents or guardians allowed their child to participate were measured for weight, height, and head circumference. Those whose measurements were at the 25th percentile or lower received a dysmorphology examination. In addition, a random sample of all children enrolled in first-grade classes was selected, and those whose parent or guardian granted permission for their participation received a dysmorphology examination. Those children who exhibited alcohol-related physical features on the dysmorphology examination and all randomly selected children went on to receive neurobehavioral testing, and their mothers or collaterals were asked to complete interviews. In addition, when a twin was selected for full evaluation by any of the established screening criteria, his/her co-twin was also selected for full evaluation. Similarly, children referred by their teacher or repeating first grade were also selected for full evaluation (Figure).
In sampling method 2, no screening was undertaken. A simple random sample was selected from first-grade children enrolled at all elementary schools in the community. All selected children with consent were offered the full evaluation, including the dysmorphology examination, neurobehavioral testing, and the maternal or collateral interview.
In sampling method 3, the large population of the Pacific Southwestern site required that a subsample of schools be selected. A convenience sample of 27 schools was selected to participate. Of these, 25 were selected from the 120 regular elementary schools and 1 from the 26 charter schools in the public school district. In addition, 1 of the 55 private or special needs schools in the city participated. These schools were identified as representing diverse socioeconomic and geographic areas and were led by school principals who indicated willingness to participate in the study. From these schools, parents or guardians were first asked for written permission to be contacted. Among those who agreed to be contacted, consent was obtained for screening for weight, height, or head circumference that was at or lower than the 25th percentile. In addition, a child development screening tool, Parents Evaluation of Development Status, was administered to each participating parent or guardian. A report of 2 or more developmental concerns was considered a positive screen result. A random sample was drawn from participating children who had negative results for both growth and the Parents Evaluation of Development Status. Children who had positive screen results and those who had been selected among the group who had negative screen results were then invited, if their parents or guardians agreed, to receive the dysmorphology examination, neurobehavioral testing, and the maternal or collateral interview. In addition, co-twins and teacher referrals or children repeating first grade were eligible for the full evaluation as described in sampling method 1.
In sampling methods 1 and 3, the strategy of initial screening on growth, developmental concerns, or both narrowed the pool of children eligible for the full fetal alcohol spectrum disorders evaluation. This allowed for more efficient use of resources by only providing full evaluations to those children who could have met 1 of the required criteria for 1 or more classifications. This strategy was coupled with a random sampling to include children not selected through the screening process. This additional strategy provided the opportunity to identify children who would have been missed on either screening measure, particularly those children who may have alcohol-related neurodevelopmental disorder.
Consistent Application of Criteria
The collective data on all evaluated children were reviewed by the respective study teams in case conferences, and a fetal alcohol spectrum disorder classification was assigned (see the eBox in the Supplement). The 2 study teams also exchanged information and assigned a second independent classification to each qualifying case and a sample of noncases to ensure consistent and accurate application of fetal alcohol spectrum disorders criteria for all children.
Statistical Analysis
Prevalence was estimated in 2 ways. The first method estimated the minimum or most conservative prevalence and 95% CIs using the total number of children classified within the fetal alcohol spectrum disorders continuum for a given sample as the numerator and the total number of eligible children at that site for that year as the denominator. In sampling methods 1 and 3, the term eligible children was defined as all children enrolled in the participating first-grade classes in that year. In sampling method 2, the denominator was defined as the total number of children who were selected randomly at each site (consented and not consented). The conservative approach assumed that children who were not evaluated did not have fetal alcohol spectrum disorders. These prevalence estimates represented the minimum prevalence for a community in a given year (formulas are in the Formulas for Calculation of the Prevalence by Sampling Method section of the Supplement).
The second set of estimates used a weighting technique to consistently estimate the prevalence and 95% CIs accounting in sampling methods 1 and 3 for the proportions of children who screened positive for growth or developmental concerns or who were randomly selected and restricting the denominators in all 3 sampling methods to children with sufficient information to be classified as having a fetal alcohol spectrum disorder. In this approach data were assumed to be missing completely at random, ie, children who were not evaluated had the same prevalence of fetal alcohol spectrum disorders as those completing the evaluation. This included children not consented and those who did not complete all components of the evaluation. Open-source statistical programming language and environment R version 3.4.1 was used.
Weighted estimates of the prevalence of fetal alcohol spectrum disorders and its continuum of specific diagnoses were generally of the form ΣJj = 1wjXj/nj, for which J represents the number of subpopulations from which the samples were drawn; Xj represents the number of children with fetal alcohol spectrum disorders or other specific diagnosis identified among the nj children who had been fully evaluated and drawn from subpopulation j, wj = Nj/N, for which Nj represents the size of the subpopulation j; and N represents the size of the total population so that ΣJj = 1wj = 1. This is equivalent to weighting by the inverse probability of sampling. As a special case, in sampling method 2, for which simple random sampling was used, J = 1 and w1= 1. In sampling method 1, J = 3 for both full and partial fetal alcohol syndrome, and the subpopulations were (1) small (ie, weight, height, or head circumference ≤25th percentile), (2) not small, and (3) twin or referral. For alcohol-related neurodevelopmental disorder and total fetal alcohol spectrum disorders in sampling method 1, J = 4 and the subpopulations were (1) small and with alcohol-related physical features, (2) small but without alcohol-related physical features, (3) not small, and (4) twin or referral. For total fetal alcohol spectrum disorders and for j =2, X2 was the number of children with alcohol-related neurodevelopmental disorder in the corresponding subsample. In sampling method 3, J = 2, and the subpopulations were (1) positive screen result and (2) negative screen result. More computational details, sampling diagram, and a working example are provided in the Formula for Calculation of the Prevalence by Sampling Method section and eFigure 3 of the Supplement.
To obtain CIs for the prevalence estimates, the variance of the estimated prevalence was estimated by ΣJj = 1w2j var(p_hat), for which pj = Xj/nj. For sampling methods 1 and 2, var(pj) = pj(1−pj)/nj. For sampling method 3, cluster sampling (for which cluster indicates school) was accounted for using nonparametric bootstrap, by resampling with replacement clusters (ie, schools) with 10 000 bootstrap runs. Log-log transformation and normal approximation were then used to obtain CIs of the prevalence. See the Variance Estimates and Confidence Intervals section in the Supplement.
Results
Participating classrooms had an enrollment of 13 146 children over all years. Of these, 6054 children were screened on growth, development, or both. An additional 585 were randomly selected in the sampling method 2 sites to receive the dysmorphology examination. A total of 3083 dysmorphology examinations were provided, 1898 maternal or collateral interviews were completed, 2173 children completed the cognitive-behavioral battery, and 2962 children were evaluated for a fetal alcohol spectrum disorder classification in case conferences (eTable 2 in the Supplement). Data from 1 academic year (2010-2011) in the first Midwestern sample have been published but were incorporated into the overall prevalence estimates using the more current consortium criteria for classification. Consent rates for screening among eligible children ranged from 36.9% to 92.5% and averaged 59.9% across all sites.
Characteristics of the mothers who completed the maternal interview and their children by site are shown in Table 1. Sampling method 1 was used at 3 sites, 2 for only 1 academic year and 1 for both academic years. Sampling method 2 was used at 2 sites for 1 academic year each. Sampling method 3 was used at 1 site for both academic years (Table 2).
Table 1. Maternal and Child Characteristics of Consortium Study Participants at 4 Community Sites in the United Statesa.
| Midwestern City | Rocky Mountain City | Southeastern Countyb | Pacific Southwestern City | |
|---|---|---|---|---|
| Children | ||||
| Age, mean (SD), mo | 81.8 (4.4) | 83.3 (5.5) | 81.5 (4.3) | 87.5 (6.7) |
| Boys, No. (%) | 186 (51.1) | 132 (50.0) | 190 (50.0) | 418 (51.6) |
| Mothers | ||||
| Current age, mean (SD), y | 35.7 (5.5) | 34.3 (5.8) | 34.9 (5.9) | 36.5 (6.8) |
| Hispanic ethnicity, No. (%) | 15 (3.9) | 8 (3.0) | 78 (20.1) | 486 (60.1) |
| Race, No. (%) | ||||
| White | 347 (91.3) | 232 (87.5) | 283 (74.7) | 668 (82.6) |
| Black | 11 (2.9) | 5 (1.9) | 68 (17.9) | 20 (2.5) |
| Asian or Pacific Islander | 5 (1.3) | 5 (1.9) | 10 (2.6) | 82 (10.1) |
| Native American/Alaska Native | 12 (3.2) | 19 (7.2) | 3 (0.8) | 3 (0.4) |
| Mixed/other | 5 (1.3) | 4 (1.5) | 15 (3.9) | 36 (4.4) |
| Estimated current annual household income, US $, No. (%) | ||||
| 0-9999 | 12 (3.4) | 15 (6.5) | 17 (5.1) | 36 (4.7) |
| 10 000-14 999 | 5 (1.4) | 9 (3.9) | 16 (4.8) | 66 (8.6) |
| 15 000-19 999 | 13 (3.7) | 9 (3.9) | 16 (4.8) | 79 (10.3) |
| 20 000-24 999 | 7 (2.0) | 18 (7.8) | 23 (6.9) | 84 (11.0) |
| 25 000-34 999 | 28 (7.9) | 21 (9.1) | 46 (13.8) | 96 (12.6) |
| 35 000-49 999 | 44 (12.4) | 35 (15.2) | 44 (13.2) | 89 (11.6) |
| 50 000-74 999 | 66 (18.5) | 47 (20.3) | 50 (13.2) | 88 (11.5) |
| ≥75 000 | 181 (50.8) | 77 (33.3) | 122 (36.5) | 226 (29.6) |
| Parity, mean (SD) | 2.7 (1.1) | 2.6 (1.2) | 2.7 (1.2) | 2.6 (1.2) |
| Maternal marital status, No. (%) | ||||
| Married | 291 (77.6) | 196 (75.4) | 244 (64.9) | 500 (61.8) |
| Widowed | 1 (0.3) | 1 (0.4) | 0 | 9 (1.1) |
| Divorced | 26 (6.9) | 19 (7.3) | 19 (5.1) | 65 (8.0) |
| Separated | 7 (1.9) | 7 (2.7) | 19 (5.1) | 48 (5.9) |
| Single | 39 (10.4) | 19 (7.3) | 41 (10.9) | 76 (9.4) |
| Unmarried, living with partner | 11 (2.9) | 18 (6.9) | 53 (14.1) | 111 (13.7) |
Percentages may not sum to 100 due to rounding.
Consists of 1 county that included 3 midsized to small cities and rural areas.
Table 2. Conservative Prevalence Estimates for Specific Classifications of Fetal Alcohol Spectrum Disorders for 8 Samples at 4 Community Sites in the United States (Prevalence per 1000 Children)a.
| Site and Sample No. | Sampling Method | Year Initiated | No. of Eligible Childrenb | Fetal Alcohol Syndrome | Partial Fetal Alcohol Syndrome | Alcohol-Related Neurodevelopmental Disorder | Total Fetal Alcohol Spectrum Disorders | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Cases | Prevalence (95% CI) | No. of Cases | Prevalence (95% CI) | No. of Cases | Prevalence (95% CI) | No. of Cases | Prevalence (95% CI) | ||||
| Midwestern City | |||||||||||
| 1 | 1 | 2010 | 2033 | 11 | 5.4 (4.0-7.2) | 21 | 10.3 (8.3-12.8) | 4 | 2.0 (1.2-3.2) | 36 | 17.7 (15.0-20.8) |
| 2 | 2 | 2012 | 709c | 0 | 0.0 (0.0-4.2) | 2 | 2.8 (1.3-5.5) | 6 | 8.5 (5.5-12.5) | 8 | 11.3 (7.8-15.8) |
| Rocky Mountain City | |||||||||||
| 3 | 1 | 2012 | 915 | 3 | 3.3 (1.8-5.7) | 10 | 10.9 (7.9-14.8) | 5 | 5.5 (3.4-8.4) | 18 | 19.7 (15.5-24.7) |
| 4 | 2 | 2013 | 400c | 1 | 2.5 (0.8-6.3) | 12 | 30.0 (22.3-39.4) | 7 | 17.5 (11.8-25.0) | 20 | 50.0 (39.9-61.7) |
| Southeastern Countyd | |||||||||||
| 5 | 1 | 2013 | 1339 | 3 | 2.2 (1.2-3.9) | 10 | 7.5 (5.4-10.1) | 15 | 11.2 (8.6-14.4) | 28 | 20.9 (17.3-25.1) |
| 6 | 1 | 2014 | 1548 | 5 | 3.2 (2.0-5.0) | 6 | 3.9 (2.5-5.7) | 10 | 6.5 (4.7-8.8) | 21 | 13.6 (10.9-16.8) |
| Pacific Southwestern City | |||||||||||
| 7 | 3 | 2012 | 2238 | 1 | 0.4 (0.2-1.1) | 19 | 8.5 (6.7-10.6) | 22 | 9.8 (7.9-12.1) | 42 | 18.8 (16.1-21.8) |
| 8 | 3 | 2013 | 2171 | 3 | 1.4 (0.8-2.4) | 24 | 11.1 (9.0-13.5) | 22 | 10.1 (8.1-12.4) | 49 | 22.6 (19.5-25.9) |
Conservative prevalence estimated by number of cases per the number of eligible children × 1000.
Eligible children were defined as all children enrolled in first-grade classes for sampling methods 1 and 3 and all children enrolled in first-grade classes who were randomly selected for sampling method 2.
The total number of children enrolled in first grade for sample 2 was 2014, from which 709 were randomly selected for participation in the study; the total number of children enrolled in first grade for sample 4 was 888, from which 400 were randomly selected for participation in the study.
Consists of 1 county that included 3 midsized to small cities and rural areas.
Applying the study diagnostic criteria across all samples, 222 children were classified with a fetal alcohol spectrum disorder. Of these, 27 met criteria for fetal alcohol syndrome, 104 met criteria for partial fetal alcohol syndrome, and 91 met criteria for alcohol-related neurodevelopmental disorder (Table 2). Only 2 of the 222 children classified with a fetal alcohol spectrum disorder had been diagnosed previously with the disorder, although many parents and guardians were aware of the learning and behavioral challenges facing their children.
The conservative prevalence estimates and 95% CIs for fetal alcohol spectrum disorders for the samples across all study sites are presented in Table 2. The total number of fetal alcohol spectrum disorder cases in the numerator for sampling method 1 was 103 children; for sampling method 2, 28 children; and for sampling method 3, 91 children. The prevalence estimates varied by sample, site, and sampling method. The conservative estimate of fetal alcohol spectrum disorders prevalence ranged from a low of 11.3 (95% CI, 7.8-15.8) per 1000 children in 1 Midwestern sample to a high of 50.0 (95% CI, 39.9-61.7) per 1000 children in 1 Rocky Mountain sample.
Total estimated prevalence of fetal alcohol spectrum disorders using the weighted approach ranged from a low of 31.1 per 1000 children (95% CI, 16.1-54.0) in 1 Southeastern sample to a high of 98.5 per 1000 children (95% CI, 57.5-139.5) in 1 Rocky Mountain sample (Table 3). Fetal alcohol spectrum disorders prevalence estimates using the weighted approach were substantially higher than the conservative estimates due to the use of denominators restricted to those children who had received a full evaluation. These restricted denominators represented between 19% and 50% of the larger eligible number of children used as the denominators for the more conservative estimates. The weighted estimates assumed that the estimated prevalence of fetal alcohol spectrum disorders among evaluated children was applicable to those children not evaluated.
Table 3. Estimated Weighted Prevalence for Specific Classifications of Fetal Alcohol Spectrum Disorders for 8 Samples at 4 Community Sites in the United States (Prevalence per 1000 Children)a.
| Site and Sample | Sampling Method | Year Initiated | No. of Children Classifiedb | Fetal Alcohol Syndrome | Partial Fetal Alcohol Syndrome | Alcohol-Related Neurodevelopmental Disorder | Total Fetal Alcohol Spectrum Disorders | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Cases | Prevalence (95% CI) | No. of Cases | Prevalence (95% CI) | No. of Cases | Prevalence (95% CI) | No. of Cases | Prevalence (95% CI) | ||||
| Midwestern City | |||||||||||
| 1 | 1 | 2010 | 512 | 11 | 7.8 (4.2-13.5) | 21 | 31.0 (14.6-57.6) | 4 | 9.7 (2.1-30.4) | 36 | 48.5 (27.8-77.7) |
| 2 | 2 | 2012 | 236 | 0 | 0.0 (0.0-12.7) | 2 | 8.4 (0.0-20.2) | 6 | 25.4 (5.3-45.5) | 8 | 33.9 (10.8-57.0) |
| Rocky Mountain City | |||||||||||
| 3 | 1 | 2012 | 265 | 3 | 6.6 (1.9-17.9) | 10 | 22.2 (11.6-38.5) | 5 | 37.7 (13.9-81.2) | 18 | 66.5 (36.5-108.6) |
| 4 | 2 | 2013 | 203 | 1 | 4.9 (0.0-14.6) | 12 | 59.1 (26.7-91.6) | 7 | 34.5 (9.4-59.6) | 20 | 98.5 (57.5-139.5) |
| Southeastern Countyc | |||||||||||
| 5 | 1 | 2013 | 382 | 3 | 2.6 (0.7-7.2) | 10 | 13.8 (4.9-32.0) | 15 | 50.4 (25.3-88.3) | 28 | 66.8 (38.3-105.8) |
| 6 | 1 | 2014 | 444 | 5 | 3.8 (1.5-8.5) | 6 | 8.9 (2.3-25.4) | 10 | 18.4 (7.3-38.8) | 21 | 31.1 (16.1-54.0) |
| Pacific Southwestern City | |||||||||||
| 7 | 3 | 2012 | 424 | 1 | 2.0 (0.2-10.9) | 19 | 38.8 (26.1-55.1) | 22 | 49.2 (28.8-77.5) | 42 | 90.0 (65.9-118.6) |
| 8 | 3 | 2013 | 496 | 3 | 4.9 (1.3-13.7) | 24 | 41.4 (28.4-58.1) | 22 | 38.2 (21.2-62.8) | 49 | 84.4 (61.2-112.3) |
See supplemental materials for detailed methods and example calculations.
Number of children classified is the number of children reviewed in case conferences. Those with sufficient information from the full evaluation to classify as fetal alcohol spectrum disorders are included in the denominators for the weighted prevalence estimates.
Consists of 1 county that included 3 midsized to small cities and rural areas.
With respect to the specific categories, shown in Table 3, the weighted prevalence estimates for fetal alcohol syndrome ranged from 0 (95% CI, 0.00-12.7) to 7.8 (95% CI, 4.2-13.5) per 1000 children and accounted for less than 20% of the overall prevalence of fetal alcohol spectrum disorders in any sample. The prevalence estimates for partial fetal alcohol syndrome ranged from 8.4 (95% CI, 0.0-20.2) to 59.1 (95% CI, 26.7-91.6) per 1000 children. The prevalence estimates for alcohol-related neurodevelopmental disorder ranged from 9.7 (95% CI, 2.1-30.4) to 50.4 (95% CI, 25.3-88.3) per 1000 children.
Within sampling strategy, the weighted prevalence estimates for fetal alcohol spectrum disorders in sampling methods 1 and 3 were more consistent with overlapping CIs. Sampling method 2 produced the most divergent fetal alcohol spectrum disorder prevalence estimates with CIs that did not overlap.
Discussion
The primary finding was a conservatively estimated prevalence of fetal alcohol spectrum disorders across 4 sites in the United States that ranged from 11.3 (95% CI, 7.8-15.8) to 50.0 (95% CI, 39.9-61.7) per 1000 children. Using a weighted prevalence approach with the denominator restricted to children who received a full evaluation and therefore had a defined outcome, estimates across the same 4 communities were substantially higher. Prevalence estimates using this approach ranged from 31.1 (95% CI, 16.1-54.0) to 98.5 (95% CI, 57.5-139.5) per 1000 children.
Three recent systematic reviews and meta-analyses of global data on the worldwide prevalence of fetal alcohol syndrome or fetal alcohol spectrum disorders have been published. However, there were few US studies included in these meta-analyses, and those studies that met criteria for inclusion were predominately clinic based or used passive surveillance. All previous studies were conducted at single sites, and only 5 used complete active case ascertainment, including 1 sample that was incorporated into the present study. Among the 5 active case ascertainment studies included in these meta-analyses, varying diagnostic criteria were used to classify cases, and only 1 study assessed children for alcohol-related neurodevelopmental disorder.
This consortium study, to our knowledge, was the first to apply active case ascertainment, common methodology, a single classification system and expert in-person evaluation for a continuum of fetal alcohol spectrum disorders including alcohol-related neurodevelopmental disorder to a large number of children from communities across the United States. These prevalence estimates are consistent with mounting evidence that harmful fetal alcohol exposure is common in the United States today and highlight the public health burden due to fetal alcohol spectrum disorders. Placed in the context of another common developmental disorder, the Centers for Disease Control and Prevention estimated in 2012 that the prevalence of autism spectrum disorders among 8-year-old children in 11 surveillance sites across the United States was 14.6 per 1000 children.
Data from the National Epidemiologic Survey of Alcohol and Related Conditions documented an increase in alcohol use among women between the 2001-2002 and 2012-2013 survey years. In particular, consumption of 4 or more standard drinks at least weekly in the past 12 months increased by 14% to 37% in women aged 18 through 44 years. In a US Behavioral Risk Factor Surveillance System survey administered between 2011 and 2013 that included 198 098 nonpregnant women of reproductive age, an estimated 53.6% of respondents reported recent alcohol consumption and 18.2% reported drinking 4 or more standard drinks on at least 1 occasion (ie, binge episodes) in the past 30 days. Among the 8383 pregnant women in the sample, an estimated 10.2% reported any recent drinking and 3.1% reported at least 1 binge episode in the last 30 days. A pattern of binge drinking in pregnancy is thought to present the highest risk of fetal alcohol spectrum disorders among offspring.
In this study, 2 of 222 children with fetal alcohol spectrum disorders were known to have been previously diagnosed with the disorder. These data confirm that missed diagnoses and misdiagnoses of children are common. Similarly, in a previous school-based US sample, only 1 of 7 children identified with fetal alcohol syndrome had a previous diagnosis; in another, only 2 of 26 children identified with full or partial fetal alcohol syndrome had a previous diagnosis.
This study has several strengths. First, active case ascertainment was used in first-grade cohorts to obtain general population prevalence data in 4 communities. Second, the 5- to 7-year age range was optimal for identification of physical features associated with fetal alcohol spectrum disorders and suitable for early evaluation of neurobehavioral problems linked to alcohol exposure. Third, children were identified using face-to-face, blinded examinations provided by dysmorphologists with extensive experience in fetal alcohol spectrum disorders and the ability to rule out other disorders with similar phenotypes. Fourth, standardized neurobehavioral testing was conducted in a blinded manner by locally certified examiners. Fifth, maternal and collateral interviews used validated techniques for capturing detailed information on alcohol use in pregnancy and maternal risks. Sixth, a priori common criteria for classification were agreed upon by multidisciplinary researchers and advisors for the consortium, and they were applied consistently across sites. In addition, data were collected in such a manner that other diagnostic schema for fetal alcohol spectrum disorders that are currently in use or that are developed in the future could be applied.
Limitations
This study has several limitations. First, due to local policy variations in the modes of access allowed for recruitment of children, as well as variability in willingness to consent, no individual sample evaluated the entire eligible population. Consent rates for screening ranged from 36.9% to 92.5% in individual samples and overall consent rates for screening averaged only 59.9% of eligible children (eTable 2 in the Supplement). If nonconsented children differed from consented, this could have biased prevalence estimates in either direction. Second, the numbers of cases of each category of fetal alcohol spectrum disorders in each sample are small, leading to wide CIs. Third, neurobehavioral testing at this age may have missed some children with deficits that would not become apparent until later ages, which could have led to underestimation of rates. Fourth, this cross-sectional study was neither a longitudinal nor a clinical sample. More comprehensive, repeated measures at older ages may have identified more children. This limitation highlights the need for longitudinal prevalence studies. Fifth, the criteria defining neurobehavioral impairment in this study were selected to balance sensitivity for deficits that have functional consequences with specificity for the characteristic neurobehavioral domains known to be affected by prenatal alcohol exposure. The objective was to produce prevalence estimates across multiple communities using a one-time evaluation to identify children with measurable deficits consistent with prenatal alcohol exposure. However, in the absence of a definitive biomarker for fetal alcohol spectrum disorders, it is impossible to know what proportion of these deficits were caused by fetal alcohol exposure. Therefore, prevalence estimates, particularly for alcohol-related neurodevelopmental disorder, could be overestimated. In addition, the 4 communities in this study may not be representative of the United States overall. The sample-by-sample variability in prevalence estimates may be due in part to the low absolute number of children classified in each category of fetal alcohol spectrum disorders. However, variability across sites may also be representative of the diversity that would be seen elsewhere, similar to the variability in risky alcohol consumption reported among women across the United States.
Conclusions
Estimated prevalence of fetal alcohol spectrum disorders among first-graders in 4 US communities ranged from 1.1% to 5.0% using a conservative approach. These findings may represent more accurate US prevalence estimates than previous studies, but may not be generalizable to all communities.
eBox. Updated Criteria for the Classification of Fetal Alcohol Spectrum Disorders Modified for Use in the CoFASP Consortium
eMethods. Sampling Methods, Examination Categories, and Calculation Formulas
eTable1. Demographic Indicators by Consortium Site and US
eTable2. Detailed Characteristics of the Consortium Sites and Samples
eFigure1. Dysmorphology Checklist
eFigure2. Neurobehavioral Testing Battery and Cut Off Criteria
eFigure3. Subsample Membership in SM1 Coded by Color
eReferences
References
- 1.Popova S, Lange S, Probst C, Gmel G, Rehm J. Estimation of national, regional, and global prevalence of alcohol use during pregnancy and fetal alcohol syndrome. Lancet Glob Health. 2017;5(3):e290-e299. [DOI] [PubMed] [Google Scholar]
- 2.Lange S, Probst C, Gmel G, Rehm J, Burd L, Popova S. Global prevalence of fetal alcohol spectrum disorder among children and youth. JAMA Pediatr. 2017;171(10):948-956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roozen S, Peters GJ, Kok G, Townend D, Nijhuis J, Curfs L. Worldwide prevalence of fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2016;40(1):18-32. [DOI] [PubMed] [Google Scholar]
- 4.Stratton KR, Howe CJ, Battaglia FC, eds. Fetal Alcohol Syndrome: Diagnosis, Epidemiology, Prevention, and Treatment. Washington, DC: National Academies Press; 1996. [Google Scholar]
- 5.Sampson PD, Streissguth AP, Bookstein FL, et al. Incidence of fetal alcohol syndrome and prevalence of alcohol-related neurodevelopmental disorder. Teratology. 1997;56(5):317-326. [DOI] [PubMed] [Google Scholar]
- 6.May PA, Gossage JP, Kalberg WO, et al. Prevalence and epidemiologic characteristics of FASD from various research methods with an emphasis on recent in-school studies. Dev Disabil Res Rev. 2009;15(3):176-192. [DOI] [PubMed] [Google Scholar]
- 7.Chasnoff IJ, Wells AM, King L. Misdiagnosis and missed diagnoses in foster and adopted children with prenatal alcohol exposure. Pediatrics. 2015;135(2):264-270. [DOI] [PubMed] [Google Scholar]
- 8.May PA, Fiorentino D, Phillip Gossage J, et al. Epidemiology of FASD in a province in Italy. Alcohol Clin Exp Res. 2006;30(9):1562-1575. [DOI] [PubMed] [Google Scholar]
- 9.Viljoen DL, Gossage JP, Brooke L, et al. Fetal alcohol syndrome epidemiology in a South African community. J Stud Alcohol. 2005;66(5):593-604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.May PA, Blankenship J, Marais AS, et al. Approaching the prevalence of the full spectrum of fetal alcohol spectrum disorders in a South African population-based study. Alcohol Clin Exp Res. 2013;37(5):818-830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Petković G, Barišić I. Prevalence of fetal alcohol syndrome and maternal characteristics in a sample of schoolchildren from a rural province of Croatia. Int J Environ Res Public Health. 2013;10(4):1547-1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.May PA, Keaster C, Bozeman R, et al. Prevalence and characteristics of fetal alcohol syndrome and partial fetal alcohol syndrome in a Rocky Mountain Region City. Drug Alcohol Depend. 2015;155:118-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.May PA, Baete A, Russo J, et al. Prevalence and characteristics of fetal alcohol spectrum disorders. Pediatrics. 2014;134(5):855-866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Institute on Alcohol Abuse and Alcoholism strategic plan 2017-2021. https://www.niaaa.nih.gov/strategic-plan. Accessed August 1, 2017.
- 15.Landgren M. How much is too much? The implications of recognising alcohol as a teratogen. Acta Paediatr. 2017;106(3):353-355. [DOI] [PubMed] [Google Scholar]
- 16.Case Ascertainment to Estimate the U.S. Prevalence of Fetal Alcohol Spectrum Disorders in Young Children. https://grants.nih.gov/grants/guide/rfa-files/RFA-AA-10-005.html. Published 2010. Accessed January 3, 2017.
- 17.United States Census Bureau QuickFacts. https://www.census.gov/quickfacts/fact/table/PST045216. Accessed August 15, 2017.
- 18.Hoyme HE, Kalberg WO, Elliott AJ, et al. Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders. Pediatrics. 2016;138(2):e20154256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Woolfenden S, Eapen V, Williams K, Hayen A, Spencer N, Kemp L. A systematic review of the prevalence of parental concerns measured by the Parents’ Evaluation of Developmental Status (PEDS) indicating developmental risk. BMC Pediatr. 2014;14:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bakhireva LN, Leeman L, Savich RD, et al. The validity of phosphatidylethanol in dried blood spots of newborns for the identification of prenatal alcohol exposure. Alcohol Clin Exp Res. 2014;38(4):1078-1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bakhireva LN, Sharkis J, Shrestha S, Miranda-Sohrabji TJ, Williams S, Miranda RC. Prevalence of prenatal alcohol exposure in the state of Texas as assessed by phosphatidylethanol in newborn dried blood spot specimens. Alcohol Clin Exp Res. 2017;41(5):1004-1011. [DOI] [PubMed] [Google Scholar]
- 22.Surveillance for fetal alcohol syndrome using multiple sources—Atlanta, Georgia, 1981-1989. MMWR Morb Mortal Wkly Rep. 1997;46(47):1118-1120. [PubMed] [Google Scholar]
- 23.Fetal alcohol spectrum disorders: data and statistics. https://www.cdc.gov/ncbddd/fasd/data.html. Accessed January 3, 2017.
- 24.McCormack C, Hutchinson D, Burns L, et al. Prenatal alcohol consumption between conception and recognition of pregnancy. Alcohol Clin Exp Res. 2017;41(2):369-378. [DOI] [PubMed] [Google Scholar]
- 25.Green PP, McKnight-Eily LR, Tan CH, Mejia R, Denny CH. Alcohol-exposed pregnancies—United States, 2011-2013. MMWR Morb Mortal Wkly Rep. 2016;65(4):91-97. [DOI] [PubMed] [Google Scholar]
- 26.Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013. JAMA Psychiatry. 2017;74(9):911-923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tan CH, Denny CH, Cheal NE, Sniezek JE, Kanny D. Alcohol use and binge drinking among women of childbearing age—United States, 2011-2013. MMWR Morb Mortal Wkly Rep. 2015;64(37):1042-1046. [DOI] [PubMed] [Google Scholar]
- 28.Christensen DL, Baio J, Van Naarden Braun K, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2012. MMWR Surveill Summ. 2016;65(3):1-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clarren SK, Randels SP, Sanderson M, Fineman RM. Screening for fetal alcohol syndrome in primary schools: a feasibility study. Teratology. 2001;63(1):3-10. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eBox. Updated Criteria for the Classification of Fetal Alcohol Spectrum Disorders Modified for Use in the CoFASP Consortium
eMethods. Sampling Methods, Examination Categories, and Calculation Formulas
eTable1. Demographic Indicators by Consortium Site and US
eTable2. Detailed Characteristics of the Consortium Sites and Samples
eFigure1. Dysmorphology Checklist
eFigure2. Neurobehavioral Testing Battery and Cut Off Criteria
eFigure3. Subsample Membership in SM1 Coded by Color
eReferences