Abstract
Background
Significant coronary artery stenosis might cause persistently impaired longitudinal left ventricle (LV) function at rest. LV global longitudinal strain (LVGLS) can be accurately assessed by 2D speckle-tracking strain echocardiography(2D-STE).
Objective
We aimed to evaluate the diagnostic accuracy of LV global longitudinal strain obtained by 2D-STE in prediction of severity of CAD.
Methods
Eighty patients with suspected stable angina pectoris were included. They underwent transthoracic echocardiography (TTE) to measure LV ejection fraction, 2-D-STE to measure GLS and coronary angiography (CA). The patients were divided into two groups: group 1 (58 patients) with significant (>70%) CAD, and group 2 (22 patients) with non-significant (<70%) CAD. Images were obtained in the apical long-axis, four-chamber, and two chamber views. Regional longitudinal systolic strain was measured in 17 myocardial segments and averaged to provide global longitudinal strain (LVGLS).
Results
There was significant decrease in GLS in group 1 compared to group 2 (−11.86 ± 2.89% versus −18.65 ± 0.79%, P < 0.000). The optimal cutoff value of GLS for prediction of significant CAD was −15.6% [AUC 0.88, 95% CI 0.78–0.96 p < 0.000]. The sensitivity, specificity and accuracy of GLS for detecting significant CAD were 93.1%, 81.8%,and 90% respectively.There was a significant positive correlation between GLS and EF (r = 0.33; p = 0.036).There was incremental significant decrease in GLS with increasing number of coronary vessels involved.
Conclusion
Measurement of global longitudinal strain using 2D speckle tracking echocardiography is sensitive and accurate tool in the prediction of severe CAD.
Keywords: CAD, 2-D speckle tracking echocardiography, Global strain, Coronary angiography
Abbreviations: AVC, aortic valve closure; BMI, body mass index; BSA, body surface area; CA, coronary angiography; CAD, coronary artery disease; DM, diabetes mellitus; DVD, double vessel disease; EF, ejection fraction; EDV, end diastolic volume; ESV, end systolic volume; HTN, hypertension; LAD, left anterior descending; LCX, left circumflex; LV, left ventricle; RCA, right coronary artery; SVD, single vessel disease; TTE, transthoracic echocardiography, TVD, triple vessel disease; 2-DSTE, speckle-tracking strain echocardiography
1. Introduction
Noninvasive identification of patients with coronary artery disease (CAD) remains a clinical challenge despite the widespread use of imaging and provocative testing; more than 50% of patients currently referred to coronary angiography show normal or non-obstructive CAD.1 Severe CAD is known to lead to LV dysfunction. However, the LV ejection fraction is usually normal at a relatively early stage.2 Thus, establishing a more sensitive index for early-stage LV dysfunction is of great importance. The longitudinally arranged subendocardial fibers are more vulnerable due to their direct exposure to the intraventricular blood pressure and the anatomy of the coronary circulation.3, 4, 5 As a result, longitudinal function is impaired first in CAD. Measurements of longitudinal motion and deformation are therefore, the most sensitive markers of coronary artery disease especially in patients with severe coronary stenosis, where intermittent ischemia may result in subtle forms of stunning that may be detectable with strain measurements. Global longitudinal peak systolic strain (GLS) can be detected by two-dimensional speckle tracking echocardiography (2D-STE).3, 4, 5
2. Objective
The aim of this study was to evaluate the diagnostic accuracy of 2D global longitudinal strain (GLS) obtained by 2D-STE speckle tracking echocardiography in prediction of severity of CAD.
3. Patients and methods
3.1. Patients
The study was done in cardiology department in Zagazig University. It included eighty patients with suspected CAD by history of angina admitted electively for coronary angiography (CA). Exclusion criteria were; age <18 years, acute coronary syndrome, previously known CAD as a history of myocardial infarction (MI), previous percutaneous coronary intervention (PCI), open heart surgery or severe wall motion abnormalities, patients with overt heart failure & LV systolic dysfunction (patients with depressed left ventricular function (EF <45% at rest)), atrial fibrillation or frequent ventricular premature complexes, left bundle-branch block, severe valvular disease, concomitant disease as connective tissue disease or drug therapy which affect cardiac function as cytotoxic drugs and patients with poor acoustic window unsuitable for speckle tracking echo. Patients underwent transthoracic echocardiography (TTE), 2-D speckle tracking echocardiography (2D-STE) and coronary angiography. The patients were divided into two groups: group 1 (58 patients) with significant (>70%) CAD, and group 2 (22 patients) with non-significant (<70%) CAD obstruction.
3.2. Methods
3.2.1. Transthoracic echocardiographic (TTE)
Examination was done by using General Electric VIVID 9 with M4S transducer, with a frequency of 1.5–4.3 MHz and high frame rate (60–90 frame/s), LV volumes were traced manually at end-diastole and end-systole in apical four- and two-chamber views and LVEF was derived from the modified biplane Simpson’s method.6
3.2.2. Strain analyses
Two consecutive heart cycles at rest, from the three standard apical planes (four-chamber, two-chamber, and long-axis), were considered by conventional 2D gray scale echocardiography. In each of the apical views, the endocardial contour was manually drawn and tracking of deformation was automatically performed by the software, once visual confirmation of good quality tracking was given by the operator.
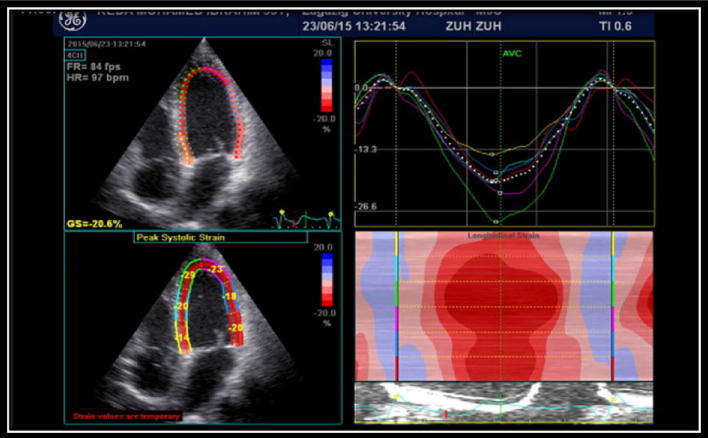
The software algorithm automatically segmented the LV into six equidistant segments and selected suitable speckles in the myocardium for tracking. The software algorithm then tracked the speckle patterns on a frame by frame basis using the sum of absolute difference algorithm. Regional longitudinal peak systolic strain (RLS) was measured in all views between aortic valve opening and closing for the 6 basal, 6 midventricular, and 4 apical segments and 17th segment was apical cap and averaged from the 17 segments to provide global longitudinal peak systolic strain (GLS) (Fig. 1).6.
Figure 1.
Left panel demonstrates apical four-chamber view. Corresponding strain curves are shown in the right panel. GLS is normal with strain values of 20.6%. End-systole is defined by aortic valve closure (AVC), and is marked with a vertical green line.
3.2.3. Coronary Angiography (CA)
Coronary Angiography (CA) was performed by the percutaneous femoral approach. Coronary angiograms were obtained for each coronary vessel in ⩾2 projections, and stenosis with ⩾70% reduction in the arterial lumen area was considered significant. The analysis of the coronary angiograms was performed visually by an experienced operator who was blinded to the results of the echocardiographic examinations.7
4. Ethics
An informed written consent was obtained from each patient according to the declaration of Helsinki and the rules of the Local Ethics Committee of Faculty of Medicine, Zagazig University, Egypt.
5. Statistical analysis
All analyses were made using the “SPSS 17 for Windows” software package. Continuous variables were expressed as mean ± standard deviation; categorical variables were expressed as percentages. Independent T-test was used to compare means, ANOVA to compare multiple groups. Chi-square test was used to compare percentages. Pearson’s correlation coefficients were used to assess the strength of relationship between continuous variables. ROC curve was plotted to get cutoff value, sensitivity and specificity. We used multiple linear regression analysis, A p value of less than 0.05 was considered significant.
6. Results
The patients were divided into two groups, group 1 (58 patients) with significant CAD+ >70% stenosis, and group 2 (22 patients) with non-significant CAD.
Comparison of the basic characteristic of the study population in patients with and without significant coronary obstruction is summarized in Table 1. Regarding age, it was 51.3 ± 8.8 in group 1 versus 53.7 ± 5.8 in group 2 p = 0.23. Sex, and risk factors were comparable in both groups. Group 1 had significant decrease in both GLS (−11.86 ± 2.89% vs −18.65 ± 0.79% p < 0.000) and LVEF (59.3 ± 3.2% vs 65.7 ± 4.7%) compared to group (2).
Table 1.
Comparison of the basic characteristic of the study population.
| Significant obstruction Group (1) N = (58) |
Not Significant obstruction Group (2) N = (22) |
X2 | P | ||
|---|---|---|---|---|---|
| Age (y) | Mean ± SD | 51.62 ± 8.37 | 55.54 ± 6.45 | t = −1.401 | 0.169 |
| BSA (m2) | Mean ± SD | 1.92 ± 0.11 | 1.87 ± 0.07 | 1.24 | 0.21 |
| BMI (kg/m2) | Mean ± SD | 30.34 ± 4.5 | 27.3 ± 3.41 | 2.10 | 0.047 |
| Gender | F | 20 (34.5%) | 4 (36.4%) | 0.012 | 0.91 |
| M | 38 (65.5%) | 7 (63.6%) | |||
| Smoking | 42 (72.4%) | 10 (45.5%) | 2.54 | 0.11 | |
| DM | 28 (48.3%) | 10 (45.5%) | 0.02 | 0.87 | |
| Family history | 2 (3.4%) | 2 (9.1%) | 0.53 | 0.46 | |
| HTN | 34 (58.6%) | 6 (27.3%) | 3.13 | 0.07 | |
| Dyslipidemia | 32 (55.2%) | 4 (18.2%) | 4.4 | 0.03 | |
| Resting ECG | 23.9 | 0.9 | |||
| Positive | 42(72.4%) | 16(72.7%) | |||
| Normal | 16(27.6%) | 6 (27.3%) | |||
| LVEDV/BSA (ml/m2) | |||||
| Mean ± SD | 52.17 ± 4.52 | 48.54 ± 0.52 | 2.629 | 0.012 | |
| LVESV/BSA (ml/m2) | |||||
| Mean ± SD | 33.51 ± 5.4 | 29.18 ± 1.77 | 2.587 | 0.014 | |
| EF (%) | |||||
| Mean ± SD | 59.31 ± 3.24 | 65.72 ± 4.71 | −4.916 | 0.000 | |
| GLS (%) | |||||
| Mean ± SD | −11.86 ± 2.89 | −18.65 ± 0.79 | −7.626 | 0.000 | |
Angiographic findings of the study population are summarized in Table 2: 22 patients (27.5%) with non-significant CAD− and 58 patients (72.5%) with significant CAD+, 58 patients (100%) had LAD, 36 patients (62%) had LCX, 32 patients (55.1%) had RCA, 20 patients (34.4%) had SVD, 14 patients (24.1%) had DVD, and 24 patients (41.3%) had TVD.
Table 2.
Angiographic findings of the study population.
| Angiographic findings | N (%) |
|---|---|
| Non-significant (group 2) | 22 (27.5%) |
| Significant (group 1) | 58 (72.5%) |
| • LAD | 58 (100%) |
| • LCX | 36 (62%) |
| • RCA | 32 (55.1%) |
| – SVD | 20 (34.4%) |
| – DVD | 14 (24.1%) |
| – TVD | 24 (41.3%) |
Diagnostic performance of GLS in predicting significant CAD (Table 3, Fig. 2). The optimal cutoff value of GLS was −15.6% [AUC 0.88, 95% CI 0.78–0.96 p < 0.000]. The sensitivity, specificity, positive predictive value, negative predictive value and accuracy of mean GLS were 93.1%, 81.8%, 93.1%, 81.8% and 90% respectively for predicting significant CAD.
Table 3.
Diagnostic performance of GLS for detection of significant CA obstruction.
| AUC | 95%CI | P | Sensitivity | Specificity | PVV | NPV | Accuracy | |
|---|---|---|---|---|---|---|---|---|
| GLS (%) < −15.6 | 0.88 | 0.78–0.96 | 0.000 | 93.1% | 81.8% | 93.1% | 81.8% | 90% |
Figure 2.
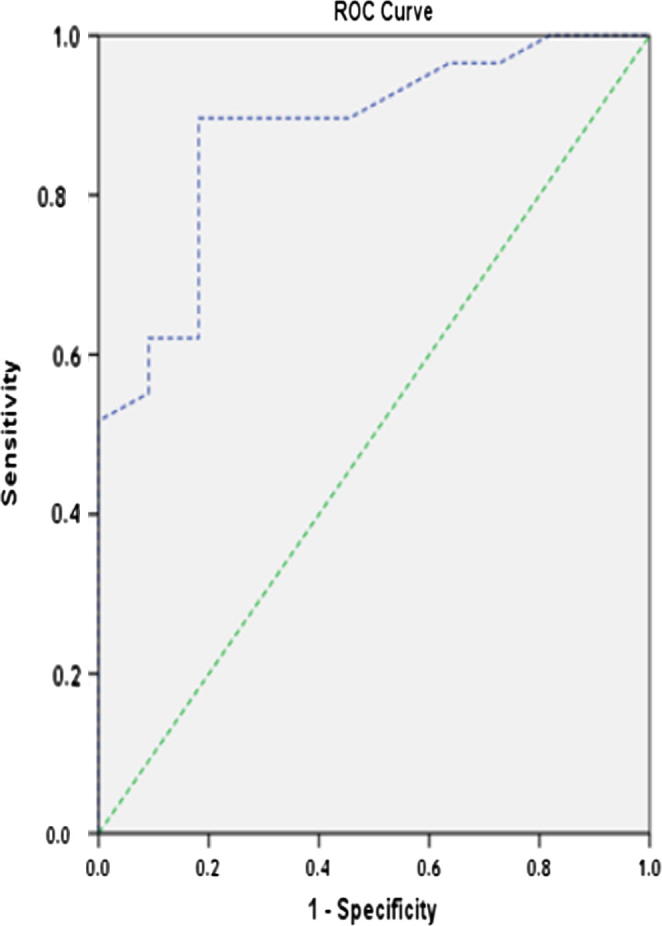
ROC curve for predicting significant CAD using GLS.
GLS declined incrementally with increasing number of stenotic coronary arteries (GLS −18.65 ± 0.79, −15.13 ± 0.68, −12.25 ± 0.9 and −9.1 ± 1.94) for patients with non-significant CAD, SVD, DVD and TVD, respectively p < 0.000 (Table 4).
Table 4.
Relation between GLS and severity of coronary angiographic findings.
| Not significant | SVD | DVD | TVD | F | P | |
|---|---|---|---|---|---|---|
| N (22) | N (20) | N (14) | N (24) | |||
| GLS (%) | −18.65 ± 0.79 | −15.13 ± 0.68 | −12.25 ± 0.9 | −9.1 ± 1.94 | 68.18 | 0.000 |
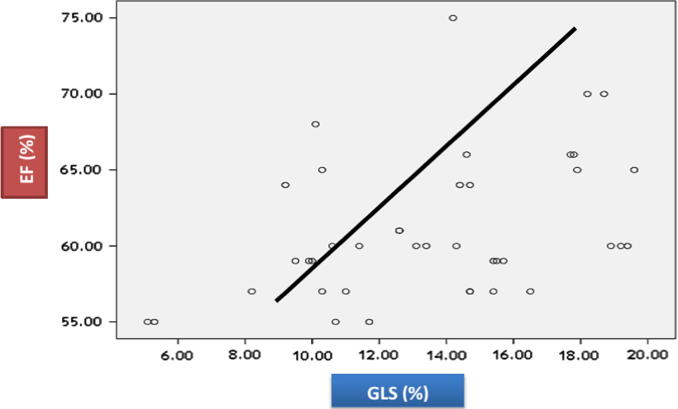
GLS has highly significant positive correlation with EF (r 0.33; p = 0.036). (Table 5, Fig. 3.)
Table 5.
Correlation between GLS and EF.
| GLS (%) |
||
|---|---|---|
| R | P | |
| EF (%) | 0.33 | 0.036 |
Figure 3.
Showing positive correlation between GLS and EF.
Multivariate logistic regression analysis found that the most predictive parameter for severity of CAD is GLS cutoff −15.6% (OR 1.52, p < 0.000) (Table 6).
Table 6.
Multivariate regression analysis for prediction severity of CAD.
| Odds ratio (OR) | P | |
|---|---|---|
| LVEDV | 1.02 | 0.88 |
| LVESV | 1.05 | 0.66 |
| EF (%) | 0.99 | 0.92 |
| GLS (%) | 1.52 | 0.000 |
7. Discussion
The present study revealed that GLS was significantly lower among patients with significant CAD than those with non-significant CAD with mean values of (GLS) were (−11.86 ± 2.89 vs −18.65 ± 0.79, p < 0.000). Also we found that GLS less than -15.6% may predict significant obstructive CAD (stenosis >70%) in 90% of patients with sensitivity and specificity (93.1%, 81.8%). (Table 3) So we found that GLS measurements at rest had high diagnostic accuracy in predicting CAD+ among patients presenting with chronic stable chest pain.
Previous studies8, 9, 10, 11, 12, 13, 14, 15, 16 evaluated patients with suspected CAD, to assess rest GLS to predict obstructive CAD following invasive angiography; they found significant decrease in GLS in patients with significant CAD compared to non-significant CAD. This finding was similar to our results. On the contrary side they found that GLS measurements at rest only have modest diagnostic accuracy in predicting obstructive CAD which is different from our results. This difference could be explained by lower cutoff value of GLS (−15.6%) in our study than others studies where their cutoff level of GLS for prediction of CAD+ varied between −17.4% and −19.7%.
Ng et al.8 enrolled 177 patients evaluated for stable CAD. They found that mean value of resting (GLS) was (−16.3 ± 2.4) in patients with CAD+ and (−19.1 ± 2.9) in patients with CAD- (p = 0.001).
Nucifora et al.9 included 182 patients without known CAD, and they showed GLS ⩽ −17.4 may predict significant obstruction (>50%) of CAD by multislice computed tomography (MSCT) coronary angiography, with sensitivity 83% and specificity 77%.
Shimoni et al.10 included 97 patients with suspected CAD. They found that GLS was significantly lower among patients with significant CAD than those with non-significant CAD− with mean values of (GLS) were (−17.3 ± 2.4 vs −20.8 ± 2.3 p < 0.000). Also they showed that GLS ⩽ −19.7 may predict significant obstruction (>50%) of CAD with sensitivity 81% and specificity 67%.
Montgomery et al.11 found that GLS was significantly lower among patients with significant CAD than those with non-significant CAD with mean values of (GLS) were (−16.8 ± 3.2 vs −19.1 ± 3.4, p < 0.000). They showed that GLS ⩽ −17.8 may predict significant obstruction (>50%) of CAD, with sensitivity 66% and specificity 76%.
Smedsrud et al.12 included 86 patients with stable chest pain. They found GLS value was (−17.9 ± 3.5) in patients with CAD+ and (−20.1 ± 2.9) in patients with CAD -. The cutoff value of GLS for prediction significant CAD (>50%) was −17.4% with sensitivity (51%) and specificity (81%).
Biering-Soerensen et al.13 enrolled 296 patients with suspected stable angina pectoris found that GLS was significantly lower among patients with significant CAD than those with non-significant CAD with mean values of (GLS) were (−17.1 ± 2.5 vs −18.8 ± 2.6, p < 0.000). They showed that GLS ⩽ −18.4% may predict significant obstruction (>70%) of CAD, with sensitivity 74% and specificity 58%.
Evensen et al.14 studied 31 patients with suspected CAD. They found that mean value of GLS was (−15.0 ± 2.7) in patients with CAD+ vs (−19.5 ± 2.2) in patients with CAD -. Also they found the endocardial strain (GLS) value less than −16.7% may predict significant obstruction (>50%) of CAD with sensitivity 80% and specificity 60%.
Billehaug Norum et al.15 used 6 studies (778 patients with suspected CAD), which aimed to assess the diagnostic accuracy of GLS to predict significant coronary artery disease. They found that GLS was significantly lower among patients with significant CAD, with mean values of GLS were (−17.2 ± 2.6% vs −19.2 ± 2.8, p < 0.000. The cutoff level of GLS for prediction of CAD+ varied between −17.4% and −19.7% with a sensitivity from 51% to 81% and specificity between 58% and 81%. So they concluded GLS measurements at rest only have modest diagnostic accuracy in predicting CAD+ among patients presenting with chest pain. This finding possibly could be explained by the effect of diastolic function and afterload on GLS, and there was overlap in distribution of GLS values between the CAD+ and CAD− groups.
Gaibazzi et al.16 found that GLS using vendor-independent software has similar accuracy compared with stress-echo wall motion analysis for the prediction of significant CAD. Patients with CAD group had significantly reduced rest GLS (−19 + 2.4 vs −22.7 + 2.4, P = 0.001) compared with patients with non-significant CAD. They showed that GLS ⩽ −20.7 may predict significant obstruction (>50%) of CAD, with sensitivity 81.6% and specificity 84.9%.
The optimal GLS diagnostic cutoff value varies significantly among previous studies could be explained by GLS may depend on the clinical characteristics of patients, the effect of diastolic function and their hemodynamic parameters (i.e., blood pressure) during image acquisition,17 by using different equipment, different design, vendor-dependent 2D-STE software and operator skills.9, 11, 12, 18
Another data have indicated that GLS is more dependent on the 2D-STE software used, rather than ultrasound equipment used to acquire images19, 20, 21, which makes the use of vendor-independent software particularly attractive to standardize GLS for widespread use. The possibility of using a fixed diagnostic GLS cutoff value to diagnose obstructive CAD, independent of the ultrasound equipment used for images acquisition, would be required to increase the clinical usefulness of strain imaging.
In the present study, we found that GLS declined incrementally with increasing severity of CAD defined by increasing number of stenotic coronary vessels. So the risk of multivessels disease increases with decreasing GLS.
This finding was similar to results of Biering-Soerensen et al.,13 who showed that (GLS −18.8 ± 2.6 versus 18.0 ± 2.4 versus 16.7 ± 2.7 versus −16.3 ± 2.3) P = < 0.001; for patients with no significant CAD, 1-vessel disease, 2-vessel disease, and 3-vessel disease respectively. Also the studies reported by Gaibazzi et al.16 and Choi et al.18 who showed similar GLS values through different CAD categories. Patients with normal coronaries had a mean GLS of −22 ± 1.5%, single or double vessel disease −19.4 ± 2.4%, and triple-vessel or left main disease −18 ± 2.3%.
We found that patients with significant CAD had significant decrease in the ejection fraction (EF) [59.31 ± 3.24 vs 65.72 ± 4.71, p < 0.000] compared non-significant CAD. This finding is in agreement with Sharma et al.22
The study found that GLS had highly significant positive correlation with EF. This result is in concordant with results of Delgado et al.,23 Biering-Soerensen et al.13 and Evensen et al.14
Delgado et al.23 showed a good correlation between GLS and biplane LVEF for the overall study population, 222 patients with CAD (r = 0.83; p < 0.001). However, in patients with STEMI and patients with heart failure the correlation was less strong (r = 0.42 and r = 0.62) respectively suggesting that these two parameters reflect different aspects of systolic LV function.
8. Limitations
(1) Small sample size and single center study. (2) There is potential selection bias due to the need of enrolling only patients with normal wall motion at baseline echocardiogram. (3) Since the study was cross-sectional in design, the clinical endpoints were not followed so prognostic value of GlS was not determined. (4) Segmental RLS was not assessed because there were different methods used for obtaining regional strain. As a 16-segment or a 17-segment anatomical model for LV the results represent a problem as this anatomical model does not necessarily reflect the individual coronary artery distribution because there is individual variability in the coronary blood supply to myocardial segment, and also we need for proper standardization of how to uniformly obtain regional longitudinal strain (RLS) data.
9. Conclusions
Global longitudinal strain (GLS) assessed by 2D-STE at rest is a predictor of significant CAD. GLS has high sensitivity 93% for early detection of significant CAD. 2D-STE has the potential to improve the value of echocardiography in the detection of the CAD, identifying high-risk patients and to provide more information for clinical physician.
10. Recommendation
Further studies are needed to determine the clinical role of reduced rest GLS, despite its significant diagnostic accuracy to detect patients affected by obstructive CAD.
Author contributions
Hanan Radwan contributed to study conception and design; Hanan Radwan and Ekhlas Hussein contributed to data acquisition, data analysis, interpretation, writing of article, reviewing and final approval of article.
Declaration of interest
The authors declare that there is no conflict of interest.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Acknowledgment
The authors thank the staff of cardiovascular department of Zagazig University Hospital for their expert input and detailed evaluations, as well as our patients who participated in the study.
Footnotes
Peer review under responsibility of Egyptian Society of Cardiology.
Contributor Information
Hanan Radwan, Email: hananradwan67@yahoo.com.
Ekhlas Hussein, Email: card_20002000@yahoo.com.
References
- 1.Patel M.R., Peterson E.D., Dai D., Brennan J.M., Redberg R.F., Anderson H.V. Low diagnostic yield of elective coronary angiography. New Engl J Med. 2010;362:886–895. doi: 10.1056/NEJMoa0907272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parato V.M., Mehta A., Delfino D. Resting echocardiography for the early detection of acute coronary syndromes in chest pain unit patients. Echocardiography. 2010;27:597. doi: 10.1111/j.1540-8175.2010.01166.x. [DOI] [PubMed] [Google Scholar]
- 3.Tsai W.C., Liu Y.W., Huang Y.Y. Diagnostic value of segmental longitudinal strain by automated function imaging in coronary artery disease without left ventricular dysfunction. J Am Soc Echocardiogr. 2010;23:1183–1189. doi: 10.1016/j.echo.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Hoit B.D. Strain and strain rate echocardiography and coronary artery disease. Circul Cardiovasc Imag. 2011;4:179–190. doi: 10.1161/CIRCIMAGING.110.959817. [DOI] [PubMed] [Google Scholar]
- 5.Jasaityte R., Heyde B., D’hooge J. Current state of three-dimensional myocardial strain estimation using echocardiography. J Am Soc Echocardiogr. 2013;26:15–28. doi: 10.1016/j.echo.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 6.Lang R.M., Badano L.P., Mor-Avi V. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1–39. doi: 10.1016/j.echo.2014.10.003. [e14] [DOI] [PubMed] [Google Scholar]
- 7.Lincoff A.M., Topol E.J. The illusion of reperfusion. Does anyone achieve optimal myocardial reperfusion? Circulation. 1993;87:1792–1805. doi: 10.1161/01.cir.88.3.1361. [DOI] [PubMed] [Google Scholar]
- 8.Ng A.C., Sitges M., Pham P.N. Incremental value of 2-dimensional speckle tracking strain imaging to wall motion analysis for detection of coronary artery disease in patients undergoing dobutamine stress echocardiography. Am Heart J. 2009;158:836–844. doi: 10.1016/j.ahj.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 9.Nucifora G., Schuijf J.D., Delgado V., Bertini M., Scholte A.J., Ng A.C. Incremental value of subclinical left ventricular systolic dysfunction for the identification of patients with obstructive coronary artery disease. Am Heart J. 2010;159:148–157. doi: 10.1016/j.ahj.2009.10.030. [DOI] [PubMed] [Google Scholar]
- 10.Shimoni S., Gendelmann G., Ayzenberg O. Differential effects of coronary artery stenosis of myocardial function: the value of myocardial strain analysis for the detection of coronary artery disease. J Am Soc Echocardiogr. 2011;24:748–757. doi: 10.1016/j.echo.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 11.Montgomery D.E., Puthumana J.J., Fox J.M., Ogunyankin K.O. Global longitudinal strain aids the detection of non-obstructive coronary artery disease in the resting echocardiogram. Euro Heart J Cardiovasc Imag. 2012;13:579–587. doi: 10.1093/ejechocard/jer282. [DOI] [PubMed] [Google Scholar]
- 12.Smedsrud M.K., Sarvari S., Haugaa K.H., Gjesdal O., Ørn S., Aaberge L. Duration of myocardial early systolic lengthening predicts the presence of significant coronary artery disease. J Am Coll Cardiol. 2012;60:1086–1093. doi: 10.1016/j.jacc.2012.06.022. [DOI] [PubMed] [Google Scholar]
- 13.Biering-Sørensen T., Hoffman S., Mogelvang R. Myocardial strain analysis by 2-Dimensional speckle tracking echocardiography improves diagnostics of coronary artery stenosis in stable angina pectoris. Circ Cardiovasc Imag. 2014;7:58–65. doi: 10.1161/CIRCIMAGING.113.000989. [DOI] [PubMed] [Google Scholar]
- 14.Evensen K., Sarvari S., Rønning M. Carotid artery intima-media thickness is closely related to impaired left ventricular function in patients with coronary artery disease: a single-centre, blinded, non-randomized study. Cardiovas Ultrasound. 2014;12:39. doi: 10.1186/1476-7120-12-39. doi:org/10.1186/1476-7120-12-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Billehaug N., Vidar R., Edvardsen T. Diagnostic accuracy of left ventricular longitudinal function by speckle tracking echocardiography to predict significant coronary artery stenosis. BMC Med Ima. 2015;15:25. doi: 10.1186/s12880-015-0067-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gaibazzi N, Pigazzani F, Reverberi C, Porter Thomas R. Rest global longitudinal 2D strain to detect coronary artery disease in patients undergoing stress echocardiography: a comparison with wall-motion and coronary flow reserve responses. Echo Res Pract 2014;(December):61–70, doi:http://dx.doi.org/10.1530/ERP-December.14-0020. [DOI] [PMC free article] [PubMed]
- 17.Burns A.T., La Gerche A., D’hooge J., MacIsaac A.L., Prior D.L. Left ventricular strain and strain rate: characterization of the effect of load in human subjects. Euro J Echocardiogr. 2010;11:283–289. doi: 10.1093/ejechocard/jep214. [DOI] [PubMed] [Google Scholar]
- 18.Choi J.O., Cho S.W., Song Y.B., Cho S.J., Song B.G., Lee S.C. Longitudinal 2D strain at rest predicts the presence of left main and three vessel coronary artery disease in patients without regional wall motion abnormality. Euro J Echocardiogr. 2009;10:695–701. doi: 10.1093/ejechocard/jep041. [DOI] [PubMed] [Google Scholar]
- 19.Risum N., Ali S., Olsen N.T., Jons C., Khouri M.G., Lauridsen T.K. Variability of global left ventricular deformation analysis using vendor dependent and independent two-dimensional speckle-tracking software in adults. J Am Soc Echocardiogr. 2012;25:1195–1203. doi: 10.1016/j.echo.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 20.Sun J.P., Lee A.P., WuC Lam.Y.Y., Hung M.J., Chen L., Hu Z. Quantification of left ventricular regional myocardial function using two-dimensional speckle tracking echocardiography in healthy volunteers – a multi-center study. Int J Cardiol. 2012;167:495–501. doi: 10.1016/j.ijcard.2012.01.071. [DOI] [PubMed] [Google Scholar]
- 21.Negishi K., Lucas S., Negishi T., Hamilton J., Marwick T.H. What is the primary source of discordance in strain measurement between vendors: imaging or analysis? Ultrasound Med Biol. 2013;39:714–720. doi: 10.1016/j.ultrasmedbio.2012.11.021. [DOI] [PubMed] [Google Scholar]
- 22.Sharma M., Ganguly N.K. Premature coronary artery disease in Indians and its associated risk factors. Vasc Health Risk Manage. 2005;1:217–225. [PMC free article] [PubMed] [Google Scholar]
- 23.Delgado V., Sjoerd A., Claudia Y. Relation between global left ventricular longitudinal strain assessed with novel automated function imaging and biplane left ventricular ejection fraction in patients with coronary artery disease Department of Cardiology, Leiden University Medical Center, Leiden, The Netherlands. J Am Soc Echocardiogr. 2008;21:1244–1250. doi: 10.1016/j.echo.2008.08.010. [DOI] [PubMed] [Google Scholar]