Abstract
BACKGROUND:
Diabetes mellitus (DM) is one of the most prevalent diseases all over the world. Prevalence of DM in Turkey is 13.7%. Depression is another condition which has a high prevalence. All over the world, an estimated 300 million people of all ages suffer from depression. The relevance between depression and DM is a well - known condition.
AIM:
We aimed in this study to find out the prevalence of depression symptoms for DM in an attempt to better manage the disease.
METHODS:
We preferred the Beck Depression Index (BDI) to evaluate the depression symptoms.
RESULTS:
The number of patients introduced the study were 171 (101 (59.1%) female). As a results of BDI 67 (39.2%) patients evaluated as normal [29 (28.7%) female], 54 (31.6%) had poor symptoms [35 (34.7%) female], 46 (26.9%) had moderate symptoms [34 (33.7%) female] and lastly only 4(2.3%) had strong symptoms 3 (3.0%) female]. So 50 (29.2%) of patients had median plus strong symptoms. There were statistically significant association between HbA1c stages and depression (P = 0.018).
CONCLUSION:
Being a patient with DM is a strong indicator that the patient may have a depressive disorder. So the physician who takes care patients with DM should be alert about depression, and the simplest way to accomplish is BDI.
Keywords: Diabetes mellitus, Depression, Beck Depression Index, A1c, Turkey
Introduction
Diabetes mellitus (DM) is one of the most prevalent diseases all over the world and has devastating complications for patients and economic burden for nations [1]. Prevalence of DM in Turkey has increased from 7.2% [2] to 13.7% [3] in 8 years.
Depression is also a condition with high prevalence. All over the world, an estimated 300 million people of all ages suffer from depression [4]. Also, the World Health Organization (WHO; 2010) declared that major depression carries the heaviest burden of disability among mental and behavioural disorders (3.7 % of all U.S. disability-adjusted life years; and 8.3% of all U.S. years lived with disability) [5].
A study conducted in Istanbul determined that 40.1% of all participants have moderate to severe depressive symptoms [6]. Furthermore, it is observed to be prevalent in the city that the study is conducted.
The correlation between depression and DM is a well - known condition which is investigated by many researchers [7]. Prevalence of depression in patients with DM may vary according to the type of DM, gender and conditions they live in. While the DM is a serious and important condition, depression must be recognised to manage better and improve the condition to prevent devastating outcomes well known for DM.
This study aims to reveal the prevalence of depressive symptoms among patients with diabetes in our region. This way, we can rightly presume and diagnose depression in patients with DM and manage it more precisely to improve outcome.
Methods
We selected patients randomly who came for their routine Diabetes control as outpatients. After evaluation of biochemical parameters along with patient’s condition and informing the patient about the test, the Beck Depression Index form was given to the patient to fill out either at the clinic or to take home. Data of 171 diabetic patients were collected, recorded and evaluated on SPSS 20 statistical program.
The study was conducted in a cross-sectional manner to find out if a correlation exists between depression symptoms and DM. Parameters used were HbA1c values along with independent parameters like age, gender and educational background. The study was carried out in Sakarya Research and Training Hospital in Turkey from December 2016 to January 2017. All the patients had diabetes. The exclusion criteria for patients were a diagnosis of depression and using any antidepressant drug.
The sample population consisted of 171 patients with diabetes. Within this population, 96 typed 2 using the oral antidiabetic drug (OAD), 61 were using OAD plus insulin, 5 patients were using insulin only, 2 were prediabetic, and 7 were type 1. We used the Beck Depression Index (BDI) to evaluate depression symptoms.
BDI was developed by Aron T. Beck. In BDI there are 21 questions and 4 answers to choose, and each question is graded from 0 - 3. The total points are calculated and assigned ranging 0-9 is normal, 10 - 16 poor, 16 - 30 modest and over 30 is strong [14][15].
Before using the BDI, the conducting physician has been trained by psychologists. The BDI questionnaire forms were given to patients at the time of regular visit and had been collected for review. All the forms were recorded together with other parameters on SPSS 20 statistical program and then evaluated. A p-value ≤ 0.05 was accepted as statistically significant. Parameters such as gender, age, marital status, and educational background, the age of patient’s diabetes, diabetes therapy, HbA1c and other biochemical parameters that were collected in 3-month intervals were recorded. These were then reviewed to determine the relationship between these parameters and depression symptoms.
HbA1c is the strongest indicator for DM status and is used to find out the control level of the disease and to direct therapy [13]. HbA1c is analysed with the PremierHb9210™ HbA1c analyser. We stratified HbA1c in five stages as 5.0 - 6.5, 6.5 - 7.0, 7.0 - 8.0, 8.0 - 9.5 and over 9.5 [12] and we calculate a mean value of A1c for each patient collected in years to determine the relevant stage of A1c.
The study protocol was approved by ethics committee of Sakarya University. Approval was obtained on July 31 of 2016 with the number of 71522473/050.01.04/18. Before giving the questionnaire forms, all patients were informed about the test, and their approvals were taken.
Results
There were 171 patients. The majority of patients were female (n = 101; 59.1%).The mean age was 59.11yrs with a min 30yrs, and a max 79yrs and the majority of patients were under 65 years old (77.2%). fifteen (8.8%) patients were illiterate, 100 (58.5%) elementary school, 18 (10.5%) middle school, 28 (17.0%) high school and 9 (5.3%) had college degrees. The marital status of patients were 2 (1.2%) single, 157 (91.8%) married, 2 (1.2%) divorced and 10 (5.8%) widowed. Most of the patients were housewives (94; 55%), and the rest were retired (26.9%), and 28 patients had other jobs, and only 3 were jobless. Smoking status of patients was 96 (56.1%) never smoked, 34 (19.9%) currently smoking and 41 (24%) had smoked before. Alcohol status of the patients was; 160 (93.6%) were alcohol naïve, 8 (4.7%) had rarely used, and 3 (1.8%) had previously used. Mean duration of diabetes was 13.47 years (ranging from newly diagnosed to 36 years). Data were collected over a mean period of 7. 68 years.
DM treatment profile of patients were Oral Antidiabetic Drug (OAD) 97 (56.7%), insulin 12 (7%) and OAD + insulin 62 (36.3%). Most of the patients had concurrent diseases especially hypertension [118 (69%)] and dyslipidemia [141 (82.5 %)]. Further 16 (9.4%) patients had ischemic heart disease (IHD), and 16 (9.4%) hypothyroid, and also 1 had allergic asthma, 1 colitis, 1 hepatitis carrier, 1 chronic obstructive pulmonary disease, 1 ischemic heart disease + asthma bronchial, 1 larynx carcinoma (CA), 1 has had tuberculosis, 1 premature menopause, 1 prostate CA, 2 rheumatoid arthritis and 1 ulcerative colitis.
As mentioned before we tried a new method of staging HbA1c (We stratified HbA1c in five stages as 5.0 - 6.5, 6.5 - 7.0, 7.0 - 8.0, 8.0 - 9.5 and over 9.5) to reveal the association between HbA1c and depression. The relevance is depicted in the table. Also as shown in Figure 1, there was a statistically significant association between HbA1c stages and depression p = 0.018.
Figure 1.
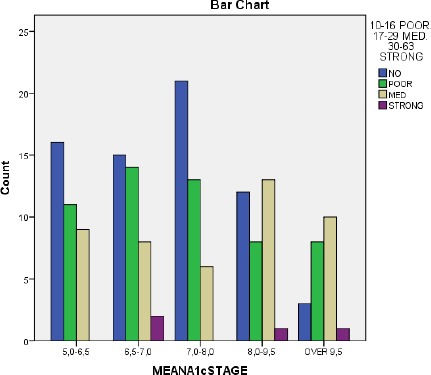
Relation between depression and mean A1c stage
As a results of Beck Depression Index 67 (39.2%) patients appreciated as normal [29 (28.7%) female and 38 (54.3%) male], 54 (31.6%) had poor symptoms [35 (34.7%) female and 19 (27.1%) male], 46 (26.9%) had moderate symptoms [34 (33.7%) female and 12%) male] and lastly only 4 (2.3%) had strong symptoms [3 (3.0%) female and 1 (1.4%) male]. Therefore, 50 (29.2%) of patients had shown median plus strong symptom (Table 1).
Table 1.
Correlation between depression symptoms and gender, education, DM age and HbA1c levels
| Normal | Poor Symptoms | Med Symptoms | Strong Symptoms | P | ||
|---|---|---|---|---|---|---|
| Subjects | Total N=171 | 67(39.18%) | 54(31.57%) | 46(26.90%) | 4(2.33%) | |
| Gender | Female n=101 (59.06%) | 29(28.7%) | 35(34.7%) | 34(33.66%) | 3(2.97%) | 0.007 |
| Male n=70 (40.93%) | 38(54.3%) | 19(27.1%) | 12(17.1%) | 1(1.4%) | ||
| Education | No Education n=15 (8.77%) | 4(26.7%) | 6(40.0%) | 4(26.7%) | 1(6.7%) | 0.459 |
| Pre n=100 (58.47%) | 40(40%) | 25(25%) | 32(32%) | 3(3.0%) | ||
| Med n=18 (10.52%) | 6(33.3%) | 7(38.9%) | 5(27.8%) | 0(0.0%) | ||
| High n=29 (16.95%) | 14(48.3%) | 11(37.9%) | 4(13.8%) | 0(0.0%) | ||
| University n=9 (5.26%) | 3(33.3%) | 5(55.6%) | 1(11.1%) | 0(0.0%) | ||
| DM Age | 0-5 Years n=16 (9.4%) | 7(43.75%) | 6(37.5%) | 3(18.75%) | 0(0%) | 0.863 |
| 6-10 Years n=47 (27,4%) | 21(44.68%) | 14(29.78%) | 11(23.40%) | 1(2.12%) | ||
| 11 Years And Over n=108 (63.2%) | 39(33.33%) | 40(34.18%) | 35(29.91%) | 3(2.56%) | ||
| HbA1c Levels | %5,0-6,5 n=36 (21.05%) | 16(44.4%) | 11(30.6%) | 9(25.0%) | 0(0.0%) | 0.018 |
| %6.5-7.0 n=39 (22.80%) | 15(38.5%) | 14(35.9%) | 8(20.5%) | 2(5.1%) | ||
| %7.0-8.0 n=40 (23.39%) | 21(52.5%) | 13(32.5%) | 6(15.0%) | 0(0.0%) | ||
| %8,0-9.5 n=34 (19.88%) | 12(35.3%) | 8(23.5%) | 13(38.2%) | 1(2.9%) | ||
| %9,5> n=22 (12.86%) | 3(13.6%) | 8(36.4%) | 10(45.5%) | 1(4.5%) | ||
While the relationship between DM type and depression symptoms was not statistically significant in a general mean (P = 0.892) statistically significant differences between patients with type 2 OAD (25% moderate plus strong symptoms) and patients with type 2 OAD plus Insulin (32.8 % moderate plus strong symptoms) was noted (Table 2).
Table 2.
Correlation between depression symptoms and DM type, HT and dyslipidemia
| Normal | Poor Symptoms | Med Symptoms | Strong Symptoms | P | ||
|---|---|---|---|---|---|---|
| Prediabetes | n=2 (1.16%) | 1(1.5%)C↓ | 0(0.0%) | 1(2.2%) | 2(1.2%) | 0.879 |
| (50%)R→ | (0.00%) | (50%) | (0.00%) | |||
| Type 1 Diabetes | n=7 (4.09%) | 1(1.5%) | 2(3.7%) | 4(8.7%) | 0(0.0%) | |
| (14.2%) | (28.57%) | (57.1%) | (0.00%) | |||
| Type 2 DM (OAD) | n=96 (56.14%) | 39(58.2%) (40.62%) | 33(61.1%) (34.37%) | 22(47.8%) (22.91%) | 2(50.0%) (2.08%) | |
| Type 2 DM (Insulin) | n=5 (2.92%) | 2(3.0%) | 2(3.7%) | 1(2.2%) | 0(0.00%) | |
| (40.00%) | (40%) | (20%) | (0.00%) | |||
| Tip 2 DM OAD&Insulin | n=61 (35.67%) | 24(35.8%) | 17(31.5%) | 18(39.1%) | 2(50.0%) | |
| (39.34%) | (27.86%) | (29.50%) | (3.27%) | |||
| Hypertension | Yes n=118 (69.00%) | 49 (41.5%) | 34 (28.8%) | 32 (27.1%) | 3 (2.5%) | 0.675 |
| No n=53 (30.99%) | 18 (34%) | 20 (37.7%) | 14 (26.4%) | 1 (1.9%) | ||
| Dyslipidemia | Yes n=141 (82.45%) | 54 (38.3%) | 45 (31.9%) | 39 (27.7%) | 3 (2.1%) | 0.916 |
| No n=30 (17.54%) | 13 (43.3%) | 9 (30%) | 7 (23.3%) | 1 (3.3%) | ||
Although high school (13.8%) and college (11.1%) degree patients had less moderate depression symptoms, it should be kept in mind that most of the patients (n = 100) had elementary school degree. P = 0.59 (Table 1).
The association between dyslipidemia and hypertension is detailed in Table 2 respectively.
Discussion
This study investigated depression symptoms and its association with some parameters in patients with DM. This study revealed that 29.2 % of patients with DM have depression symptoms. It should be kept in mind that BDI results given here are not diagnostic but rather to give direction for further referral to a specialist. Most of the patients who have depression symptoms were female. Some studies found a high prevalence between depression and DM [8] and the results of our study complied with these results.
DM patients with depression are more prone to poor glycemic control in general. This vulnerability is yet to be explicitly understood. It is thought that depression is caused by changes of the neurotransmitters in the brain. These are dopamine, serotonin and norepinephrine. These affect mood and behaviour. Counterregulatory hormones such as catecholamines, glucocorticoids, glucagon and growth hormones are secreted during psychological stress [9]. Activation of counter-regulatory hormones counteract the insulin action and can worsen glucose excursion. Increasing glucose levels may complicate the control of diabetes. And poor glycemic control especially in DM with complications could worsen depression symptoms and could lessen the response to antidepressant therapy [10]. While the relationship between depression and DM is well known, only 31% of patients with DM and depression use antidepressant therapy [11].
In our study based on BDI, we found that 29.2% of patients with DM had depression symptoms with prevalence higher in females (36.7% moderate plus strong symptoms) when compared to males (18.5% moderate plus strong symptoms), p = 0.001.
In conclusion, the prevalence of depression symptoms in patients with diabetes in a region where Turkish people live was somewhat higher than reported for other countries. Being a diabetic especially a female and having a poor managed DM were strong indicators that the patient may have depressive disorder. Hence the physician who takes care of patients with DM should be alert to the possibility of depression and the simplest way to accomplish this is the Beck Depression Index.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Diabetes Care. 2015;37(Supplement 1):S14–S80. [Google Scholar]
- 2.Satman I, Yilmaz T, Sengül A, et al. Population-Based Study of Diabetes and Risk Characteristics in Turkey. Diabetes Care. 2002;25(9):1551–1556. doi: 10.2337/diacare.25.9.1551. https://doi.org/10.2337/diacare.25.9.1551 PMid:12196426. [DOI] [PubMed] [Google Scholar]
- 3.Satman I, Omer B, Tutuncu Y, Kalaca S, Gedik S, Dinccag N, Karsidag K, Genc S, Telci A, Canbaz B, Turker F, Yilmaz T, Cakir B, Tuomilehto J, TURDEP-II Study Group Twelve-year trends in the prevalence and risk factors of diabetes and prediabetes in Turkish adults. Eur J Epidemiol. 2013;28(2):169–80. doi: 10.1007/s10654-013-9771-5. https://doi.org/10.1007/s10654-013-9771-5 PMid:23407904 PMCid: PMC3604592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization April 2017 declaration. http://www.who.int/mediacentre/factsheets/fs369/en/
- 5.National Institute of Mental Health. https://www.nimh.nih.gov/health/statistics/prevalence/major-depression-among-adults.shtml .
- 6.Onal AE, Tümerdem Y, Ari D. Investigation of Depression Prevalence in the Population of 4 Years Old and Above with Beck Depression Inventory in Halkah-lstanbul and Evaluation of the Internal Consistency of the Inventory. Turkiye Klinikleri J Med Res. 2001;19(2):94–9. [Google Scholar]
- 7.Ali S, Stone MA, Peters JL, Davies MJ, Khunti K. The prevalence of co-morbid depression in adults with Type 2 diabetes: a systematic review and meta-analysis. Diabet Med. 2006;23(11):1165–1173. doi: 10.1111/j.1464-5491.2006.01943.x. https://doi.org/10.1111/j.1464-5491.2006.01943.x PMid:17054590. [DOI] [PubMed] [Google Scholar]
- 8.Li C, Ford ES, Strine TW, Mokdad AH. Prevalence of depression among U.S. adults with diabetes: findings from the 2006 behavioral risk factor surveillance system. Diabetes Care. 2008;31(1):105–107. doi: 10.2337/dc07-1154. https://doi.org/10.2337/dc07-1154 PMid:17934145. [DOI] [PubMed] [Google Scholar]
- 9.Grisel JE, Rasmussen PR, Sperry L. Anxiety and depression: physiological and pharmacological considerations. J Individ Psychol. 2006;62(4):398–416. [Google Scholar]
- 10.Lustman PJ, Clouse RE. Depression in diabetic patients: the relationship between mood and glycemic control. J Diabetes Complications. 2005;19(2):113–122. doi: 10.1016/j.jdiacomp.2004.01.002. https://doi.org/10.1016/j.jdiacomp.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 11.Katon WJ. The comorbidity of diabetes mellitus and depression. Am J Med. 2008;121(11 Suppl 2):S8–15. doi: 10.1016/j.amjmed.2008.09.008. https://doi.org/10.1016/j.amjmed.2008.09.008 PMid:18954592 PMCid: PMC2717744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kuo IC, Lin HY, Niu SW, Hwang DY, Lee JJ, Tsai JC, Hung CC, Hwang SJ, Chen HC. Glycated hemoglobin and outcomes in patients with advanced diabetic chronic kidney disease. Scientific reports. 2016;6:20028. doi: 10.1038/srep20028. https://doi.org/10.1038/srep20028 PMid:26818011 PMCid: PMC4730215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DeFronzo RA, Ferrannini E, Alberti KG, Zimmet P, Alberti G. International Textbook of Diabetes Mellitus, 2 Volume Set. John Wiley &Sons; 2015 May 18; https://doi.org/10.1002/9781118387658. [Google Scholar]
- 14.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. (1961) An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. https://doi.org/10.1001/archpsyc.1961.01710120031004 PMid:13688369. [DOI] [PubMed] [Google Scholar]
- 15.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8(1):77–100. https://doi.org/10.1016/0272-7358(88)90050-5. [Google Scholar]


