Abstract
Objective
To identify characteristics and readmission risk associated with opting-out of a social work-driven transition intervention.
Study Design
Secondary data analysis of a randomized controlled pilot study at a large, non-profit urban community hospital.
Methods
Hospitalized English-speaking, cognitively intact, adults aged ≥65 years with expected discharge back to community were eligible for enrollment. Additionally, patients met at least one of the three eligibility criteria: (1) ≥75 years old; (2) taking 5+ medications; or (3) had 1or more prior inpatient stay in previous 6 months. The transition intervention consisted of up to two in-home visits (first within 48 hours after discharge) and up to four telephone follow-up calls (maximum of six contacts) by transition social worker. This study analyzed participants randomized to the intervention arm. Measures included demographics, medical diagnoses, presence of advance directive, and all cause 30-day hospital readmission.
Results
Of the 90 patients randomized to the Social Work Intervention Focused on Transitions (SWIFT) intervention group, nearly one-third refused (opted out of) the home intervention, and 10% were readmitted within 30-days. Multivariate analyses revealed that those opt-outing out of the intervention had three times greater odds of having a respiratory condition as compared to intervention recipients (OR=3.098, 95% CI 1.091–8.796, p=.034). Additionally, opting-out of the intervention (OR=6.75, 95% CI 1.05–43.52, p=.045) and having a diagnosis of cancer (OR=29.59, 95% CI 2.01–435.45, p=.014) significantly predicted readmission.
Conclusions
Findings suggest that some at-risk patients may not be receptive to services and programs aimed at improving care transitions, resulting in higher risk for readmission.
Keywords: Older adults, Transitional Care, Intervention refusal, 30-day readmissions, Randomized controlled trial
INTRODUCTION
Transitions between care settings have been identified as vulnerable exchange points that have been associated with increased risk for hospital readmissions,1–5 medication errors,6,7 lapses in care and safety,8 poor satisfaction with care,9 unmet needs,10 and subsequently high rates of additional costly health service use, many of which may have been avoided.5,7 Older adults are at highest risk for poor transitions and subsequent hospital readmissions. A benchmark study found that 20 percent of hospitalized Medicare beneficiaries were readmitted within 30 days and 34 percent readmitted within 90 days of their index hospitalization.11 This high rate of readmission among older adults served as the impetus for the Hospital Readmissions Reduction Program (HRRP) as part of the Affordable Care Act (ACA) since 2012, which imposes penalties among hospitals with greater than expected rates of 30 day readmissions among older adults with certain conditions (heart attack, pneumonia, and heart failure, during this study period). Subsequently, a study conducted following implementation of HRRP payment penalties found that readmission rates have declined to 17.8% for HRRP targeted conditions.12 Although some have challenged these findings by attributing reductions in readmission rates to rising observation rates,13 it is clear that hospitals have made some improvements in 30-day readmission rates.12,14,15
Although many hospitals have implemented transitional care interventions targeting older adults,16–18 the continued penalties raise hospital interest to identify additional mechanisms to further reduce readmissions. While some hospitals have seen significant reductions in 30-day rehospitalization rates,16–18 recent studies and reports highlight several challenges in the ability of hospitals to impact readmission rates and associated HRRP penalties. These concerns include: patient-level factors (e.g. sociodemographic factors, patient preference, and access to community-based supportive services) beyond the hospital’s control influencing recidivism;19–23 readmissions that are appropriate and unavoidable;23 and lack of risk-adjustment for uncontrollable factors that influence recidivism (resulting in disproportionate penalties on safety-net hospitals).15,19,23 Administrators and researchers are calling for HRRP reform, however in the meantime, hospitals continue to grapple with which patients constitute the high-risk pool that should be targeted for transitional care services and provide interventions to reduce readmissions and improve quality.23
This study is a secondary analysis of patients randomized to the care transition intervention arm of the Social Work Intervention Focused on Transitions (SWIFT) pilot study conducted among older adults identified as high risk for readmission. This analysis aims to identify the characteristics and risk factors associated with opting-out of a social work driven transition intervention. Increased knowledge of the factors associated with intervention refusal can help hospitals identify those patients that appear resistant to interventions. With hospitals accountable for 30-day readmissions, information from this study may provide insight to hospitals on patient groups that could benefit from alternate strategies to reduce readmissions, such as education and interventions provided during the hospital stay or in the primary care setting following discharge. Findings from this study may inform hospital practice and Centers for Medicare and Medicaid Services policies and funding priorities.
The question guiding this research is: What characteristics and risk factors are associated with opting-out of transitions intervention services?
METHODS
This study is a secondary data analysis of the SWIFT randomized controlled pilot study conducted at a large (625-bed), non-profit, teaching hospital located in the Los Angeles area between February 2011 and September 2013. The study was approved by the Institutional Review Board at the hospital study site and the academic research institution executing the study.
Eligibility and Recruitment
Study eligibility criteria included English-speaking, community-dwelling, older adults age 65 or older living within a 20-mile radius of the hospital. Additionally, participants had to meet at least one of the following criteria: (1) advanced age (75 years old or more); (2) taking five or more prescription medications; and/or (3) having one or more hospitalizations or emergency department visits in the previous six months. These criteria have been used in previous social work case management24 and hospital-to-home care transitions interventions25 to identify individuals at “high risk” for hospital readmission. Patients were ineligible for the SWIFT study if they were homeless, lived in an environment where they received skilled care (long-term care setting or hospice recipient), were cognitively impaired (as determined by a Short Portable Mental Status Questionnaire (SPMSQ)27–29 score of five or more errors out of 10 questions) or diagnosed with Alzheimer’s disease, severe dementia, or end-stage renal disease. Patients with end-stage renal disease were excluded from the SWIFT study due to their elevated risk of death and the associated level of need for skilled nursing care that is outside the skillset of social workers.26
We identified potentially eligible patients age 65 and over by reviewing daily hospital census reports (excluding the Intensive/Critical Care Unit) one to two time per day Monday through Friday. Direct referrals also were made by a social worker conducting rounds in the nursing units. Electronic medical records were reviewed to determine number of medications and previous medical service use. Patients meeting the eligibility criteria were approached at hospital bedside by master’s level research assistants who administered the SPMSQ to establish mental competency. Initial (and if needed, subsequent) patient contact was made at varying points during the patient’s hospitalization course due to non-continuous census screening, patients sometimes being out of their room for a procedure or test, and some patients requesting a revisit (e.g. feeling unwell or requested family be present during discussion). Eligible patients were invited to participate and asked to sign informed consent and HIPAA Authorization documents.
SWIFT Intervention
The SWIFT intervention builds on previous transitional care research,25,30,31 and integrates social work practice approaches. The intervention consists of in-home visits (a maximum of two in-home visits) and telephone follow-up calls (up to four telephone contacts) conducted by the study social worker. Patients receive a minimum of two contacts (one in-person, and one phone call) and a maximum of six contacts with the social worker. The purpose of the first home visit is to conduct an initial assessment and develop and implement a plan of care. Activities performed by the social worker during this visit are guided by an intervention checklist and includes a psychosocial evaluation, home safety check, medication inventory for reconciliation, review of hospital discharge instructions, health goal setting and problem solving, coaching around scheduling follow-up physician appointments, and referrals to home and community based service. The second in-home visit is conducted if problems identified at the initial home visit are not sufficiently resolved or are extensive enough that telephone contact is not adequate to resolve the problem.
In addition to the in-home visit(s), SWIFT intervention patients receive up to four telephone calls from the social worker. The aim of these calls is to follow-up on issues identified at the home visit, discuss outcomes from physician office visits, review established health goals (drafting new ones, when applicable), determine success of linkages/referrals to community-based services, and problem-solve around new issues.
Measures
The study researchers collected data from the hospital electronic database and through patient survey. To ensure reliability, they were formally trained in data gathering and extracting methods, and the safe and ethical conduct of human subjects research. They used the hospital’s electronic medical records (EMR) to obtain data on previous emergency department visits and hospitalizations, all cause 30-day readmission (planned and unplanned), and presence of an advance directive. Research assistants collected patient demographics and other characteristics including age, gender, marital status, and disease diagnoses (via a ‘yes/no’ inventory of 10 common conditions) through patient surveys conducted at bedside. Asthma and chronic obstructive pulmonary disease (COPD) were consolidated into a single variable renamed ‘respiratory disease.’ Similarly, ‘cardiac disease’ represented a consolidation of heart disease and chronic heart failure (CHF), and all cancers were included in a single ‘cancer’ variable.
Following hospital discharge, research assistants obtained EMR data on hospital length-of-stay and if home-health care services were ordered at discharge.
Study participants randomized to the SWIFT intervention who did not receive in-home intervention visits were considered “opt-outs”. Opt-outs were identified through social workers in their outreach to SWIFT intervention participants. SWIFT social workers documented patient stated reasons for opting out of SWIFT intervention home visits during their initial patient contact following hospital discharge.
Analysis
Descriptive statistics were used to describe the sample and bivariate tests (χ2 and Mann-Whitney U) were performed to analyze differences between the participants that opted-out of the intervention and those that received the intervention. Two logistic regressions were performed to identify characteristics associated with opting-out of the SWIFT intervention and to determine risk factors for 30-day readmission. We used results of the bivariate analyses and previous research to guide inclusion of variables in the regressions to maintain the most parsimonious model given the small sample size. Regression models to determine predictors of opting out of the SWIFT intervention included the following independent variables: respiratory condition, cardiac condition, cancer, length of stay (index hospitalization), presence of advance directive, and discharge to home without home healthcare services (self-care). We included the same variables, with the addition of the intervention opt-out variable, in the second logistic regression to determine predictors of 30-day readmission.
RESULTS
Demographics
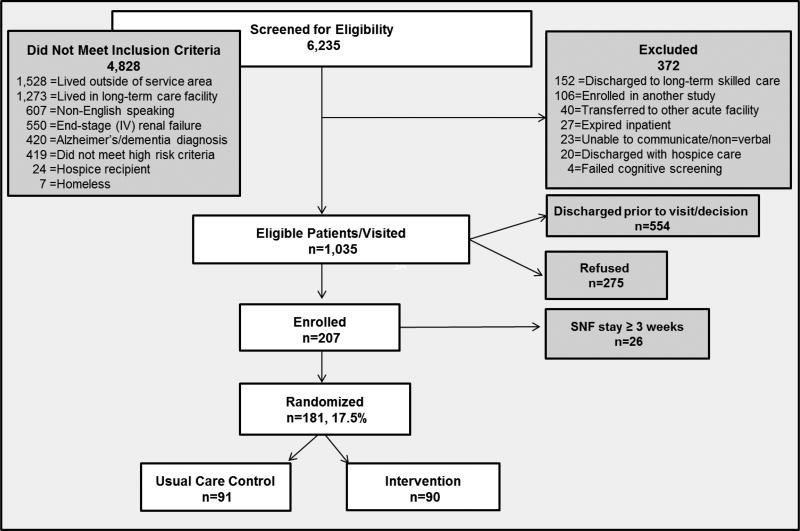
Overall, 90 participants were randomized to the SWIFT intervention group (see Figure 1). SWIFT intervention group participants were mostly Caucasian (63.6%), males (56.1%), living in their own house or apartment (89.7%). The average age of participants was 78.4 years (±7.8 years). Educational attainment was high; the vast majority (87.6%) completed high school or beyond, and 46.3% held a bachelor’s degree or higher.
Figure 1.
Consort Diagram
Among the 90 participants randomized to the intervention group, nearly one-third opted-out (31.1%) of the intervention. Participants identified the following reasons for opting out of the SWEIFT intervention: feel home visit/follow-up care is not needed (n=12, 42.9%); don’t want a home-visit (n=8, 28.6%); were hoping to be randomized to the usual care arm (n=6, 21.4%); and were unreachable (n=2, 7.1%). We queried this subsample of participants (n=26) to further understand their reasons for opting-out of the home intervention. Several reported not needing the home visit because they were feeling very good (n=7) or were already well cared for by family and/or caregiver(s) (n=2). Three indicated that they were not usually “sick” and did not need home visits. Others no longer wanted the SWIFT home visit because they were prescribed visits from home health (n=6) and felt that additional visitors were unnecessary. Two participants reported “fatigue” with clinicians and medical encounters in general. The six participants that had hoped to be randomized to the usual care arm of the study unanimously stated that they only enrolled to either “help the hospital” or “help the researchers,” explaining that this “level of care” (i.e. home visits) was unnecessary for them but could help “someone who could really use it” in the future if it became “normal care for all seniors.”
Comparison of characteristics of those enrolled in the SWIFT intervention and those opting out revealed few differences: opt-outs were more likely to have a respiratory disease as compared to intervention recipients (52.2% of opt-out versus 28.3% of intervention; p=0.04). A greater proportion of opt-outs were readmitted to the hospital within 30-days (n=5, 18.5% versus n=4, 6.3% of intervention recipients), but this trend did not reach statistical significance (p=0.08). Of the nine readmissions among all participants randomized to the SWIFT intervention, only one was planned (intervention recipient with planned hospitalization for a fiberoptic bronchoscopy). See Table 1.
Table 1.
Intervention Patient Demographic Characteristics (n=90)
| Frequency (%)
|
||||
|---|---|---|---|---|
| Received Intervention (n=63) |
Refused Intervention (n=27) |
Overall Intervention Group (n=90) |
P-value | |
| Agea | 78.3 ± 8.2 | 78.4 ± 7.1 | 78.4 ± 7.8 | 0.989 |
|
| ||||
| Gender | ||||
| Male | 32 (52.5) | 18 (64.3) | 50 (56.1) | 0.208 |
| Female | 29 (47.5) | 10 (35.7) | 30 (43.8) | |
|
| ||||
| Highest education | ||||
| 8th grade or less | 4 (7.0) | 1 (4.3) | 5 (6.3) | 0.692 |
| 9th–11th grade | 3 (5.3) | 2 (8.7) | 5 (6.3) | |
| High school graduate | 10 (17.5) | 3 (13.0) | 13 (16.3) | |
| Some college | 15 (26.3) | 5 (21.7) | 20 (25.0) | |
| College graduate | 13 (22.8) | 6 (26.1) | 19 (23.8) | |
| Graduate degree | 8 (14.0)) | 6 (26.1) | 14 (17.5) | |
| Doctoral degree | 4 (7.0) | 0 (0) | 4 (5.0) | |
|
| ||||
| Ethnicity | ||||
| African American | 11 (18.0) | 3 (11.1) | 14 (15.9) | 0.736 |
| Caucasian | 38 (62.3) | 18 (66.7) | 56 (63.6) | |
| Latino | 5 (8.2) | 4 (14.8) | 9 (10.2) | |
| Native American | 1 (1.6) | 0 (0) | 1 (1.1) | |
| Asian/PI | 1 (1.6) | 1 (3.7) | 2 (2.3) | |
| Other | 5 (8.2) | 1 (3.7) | 6 (6.8) | |
|
| ||||
| Marital status | ||||
| Married | 29 (49.2) | 16 (57.1) | 45 (51.7) | 0.622 |
| Single | 10 (16.9) | 6 (21.4) | 16 (18.4) | |
| Divorced | 6 (10.2) | 1 (3.6) | 7 (8.0) | |
| Widowed | 14 (23.7) | 5 (17.9) | 19 (21.8) | |
|
| ||||
| Living situation | ||||
| Own house/apartment | 51 (86.4) | 27 (96.4) | 78 (89.7) | 0.317 |
| Living in family member's home | 5 (8.5) | 1 (3.6) | 6 (6.9) | |
| Other | 3 (5.1) | 0 (0) | 3 (3.4) | |
|
| ||||
| Who do you live with? | ||||
| Alone | 13 (22.4) | 7 (25.9) | 20 (23.5) | 0.300 |
| Spouse/partner | 27 (46.6) | 16 (59.3) | 43 (50.6) | |
| Child | 9 (15.5) | 4 (14.8) | 13 (15.3) | |
| Paid caregiver | 1 (1.7) | 0 (0) | 1 (1.2) | |
| Other | 8 (13.8) | 0 (0) | 8 (9.4) | |
|
| ||||
| Who is your primary caregiver? | ||||
| No one/self | 24 (40.7) | 9 (33.3) | 33 (38.4) | 0.907 |
| Spouse | 16 (27.1) | 8 (29.6) | 24 (27.9) | |
| Significant other | 3 (5.1) | 1 (3.7) | 4 (4.7) | |
| Child | 6 (10.2) | 5 (18.5) | 11 (12.8) | |
| Paid caregiver | 4 (6.8) | 2 (7.4) | 6 (7.0) | |
| Other | 6 (10.2) | 2 (7.4) | 8 (9.3) | |
|
| ||||
| Annual income | ||||
| Under $10,000 | 8 (12.9) | 1 (3.6) | 9 (10.0) | 0.529 |
| $10,000 – $19,000 | 7 (11.3) | 3 (10.7) | 10 (11.1) | |
| $20,000 – $29,000 | 4 (6.5) | 1 (3.6) | 5 (5.6) | |
| $30,000 – $39,000 | 1 (3.7) | 0 (0) | 1 (1.1) | |
| $40,000– $49,000 | 0 (0) | 1 (3.6) | 1 (1.1) | |
| $50,000 or more | 6 (9.7) | 3 (10.7) | 9 (10.0) | |
| Refused to reply | 36 (55.9) | 19 (67.8) | 55 (61.1) | |
|
| ||||
| Length-of-staya (days) | 3.8 ± 8.1 | 3.0 ± 2.6 | 3.5 ± 4.2 | 0.959 |
|
| ||||
| # Prior inpatient stays (last 6 months)a | 0.5 ± 1.0 | 0.6 ± 1.1 | 0.6 ± 1.0 | 0.798 |
|
| ||||
| # Prior ED visits (last 6 months)a | .03 ± 0.6 | 0.5 ± 0.7 | 0.3 ± 0.6 | 0.309 |
|
| ||||
| # Daily medicationsa | 7.5 ± 3.4 | 9.1 ± 4.3 | 7.9 ± 3.7 | 0.122 |
|
| ||||
| # Health conditionsa | 5.9 ± 3.2 | 6.2 ± 2.9 | 5.9 ± 3.1 | 0.515 |
p<.05;
p<.01;
p<.001
Mann-Whitney U-Test
Intervention Opt-out
Using binary logistic regression, we investigated characteristics associated with opting-out of the SWIFT intervention. Results revealed that the odds of opting-out of the SWIFT intervention were significantly higher for participants with respiratory conditions (OR=3.29, 95% CI 1.09–.90, p=0.034). See Table 2. No other variables were significantly associated with opting out.
Table 2.
Logistic Regression: Factors Associated with Intervention Opt-out
| Model 1
|
Model 2
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Diagnosis | OR | SE | P | CI | OR | SE | P | CI |
|
|
|
|||||||
| Respiratory condition | 2.97 | 0.530 | 0.040* | 1.05–8.37 | 3.29 | 0.56 | 0.034* | 1.09–9.90 |
| Cardiac condition | 0.76 | 0.62 | 0.658 | 0.23–2.55 | 0.76 | 0.64 | 0.665 | 0.22–2.64 |
| Cancer | 1.55 | 0.66 | 0.503 | 0.43–5.62 | 1.550 | 0.68 | 0.521 | 0.41–5.89 |
|
|
|
|||||||
| Length-of-stay | 1.04 | 0.09 | 0.633 | 0.88–1.24 | ||||
| Has advance directive | 1.53 | 0.55 | 0.438 | 0.52–4.49 | ||||
| Home, self-care | 4.18 | 0.90 | 0.110 | 0.72–24.15 | ||||
|
|
|
|||||||
| −2Log likelihood | 87.35 | 83.24 | ||||||
| R2 | 0.08 | 0.11 | ||||||
| Hosmer and Lemeshow χ2 | 2.57 | 10.62 | ||||||
p<.05;
p<.01;
p<.001
Any 30-Day Readmission
We conducted a second logistic regression to examine variables associated with all cause readmission to the hospital within 30-days of index hospital discharge. Results revealed that, while controlling for other confounding variables, having a cancer diagnosis and opting-out of the SWIFT intervention predicted 30-day hospital readmission (p=0.01 and p=0.05, respectively). SWIFT participants diagnosed with cancer had nearly 30-times higher odds of being readmitted within 30-days of discharge (OR=29.59, 95% CI 2.01–435.45), and those that opted-out of the home intervention had more than six times higher odds of being readmitted within 30-days of discharge (OR=6.75, 95% CI 1.05–43.53). See Table 3.
Table 3.
Logistic Regression: Factors Associated with 30-day Readmission
| Model 1
|
Model 2
|
Model 3
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | SE | P | CI | OR | SE | P | CI | OR | SE | P | CI | |
|
|
|
|||||||||||
| Respiratory condition | 0.90 | 0.81 | 0.893 | 0.18–4.37 | 1.01 | 0.86 | 0.992 | 0.19–5.40 | 0.50 | 1.04 | 0.503 | 0.07–3.83 |
| Cardiac condition | 0.35 | 0.69 | 0.408 | 0.03–4.14 | 0.20 | 1.45 | 0.267 | 0.01–3.40 | 0.27 | 1.47 | 0.368 | 0.02–4.78 |
| Cancer | 15.75 | 5.96 | 0.015* | 1.72–143.90 | 26.84 | 1.34 | 0.014* | 1.94–372.22 | 29.59 | 1.37 | .014* | 2.01–435.45 |
|
|
|
|
||||||||||
| Length-of-stay | 1.19 | 0.11 | 0.110 | 0.96–1.48 | 1.21 | 0.12 | 0.118 | 0.95–1.55 | ||||
| Has advance directive | 0.70 | 0.81 | 0.661 | 1.45–3.40 | 0.54 | 0.87 | 0.477 | 0.10–2.98 | ||||
| Home, self-care | 2.850 | 1.13 | 0.353 | 0.31–25.83 | 3.57 | 1.31 | 0.331 | 0.27–46.37 | ||||
|
|
|
|
||||||||||
| Opted-out of intervention | 6.75 | 0.95 | 0.045* | 1.05–43.52 | ||||||||
|
|
|
|
||||||||||
| −2Log likelihood | 46.86 | 44.09 | 39.65 | |||||||||
| R2 | 0.220 | 0.28 | 0.37 | |||||||||
| Hosmer and Lemeshow χ2 | 2.20 | 7.75 | 9.05 | |||||||||
p<.05;
p<.01;
p<.001
DISCUSSION
This study aimed to identify the characteristics and risk factors associated with opting-out of a social work-driven transitions intervention. Findings suggest that some at-risk patients may not be receptive to in-home transitions interventions, with nearly a third of patients opting-out of a home visit after consenting to participate in the study.
We found that participants that opted-out of the intervention were significantly more likely to have a respiratory condition. There is a dearth of literature pertaining to the medical diagnoses of older adults that decline or drop out of interventions. However, a recent study examining recruitment of hospitalized Medicare patients for behavioral research found that patients who reported a perceived inability to control important life domains (i.e. “In the last week, how often have you felt that you are unable to control the important things in your life?”32), had low expectations of recovery, or reported confusion with the researcher’s questions were significantly less likely to consent to the research.32 The authors suggest that stress, self-expectations for recovery, and health literacy are potential influences on older adults’ decision to participate in behavioral research.32
Although participants in the present study did originally consent to the research and later opted-out of the home intervention aspect of the study, the constructs that Voss et al. describe may be particularly prevalent among older adults with respiratory conditions. For example, chronic obstructive pulmonary disease (COPD) is a common respiratory condition found to be most prevalent among older adults aged 65–74 years33 and was the second leading cause of death in 2015.33 Exacerbations of COPD can be significant events that can cause patients with this condition to be hospitalized and may require any number of inpatient interventions, each which are considered to have fatal risks.34,35 The constructs of perceived stress, recovery, and health literacy offered by Voss et al. could be impacted by the severity of COPD exacerbations and hospital course of care—in addition to psychosocial risk factors such as depression and socioeconomic status36—and later translate to intervention opt-outs.32,37,38
Another reason why participants with a respiratory condition may have opted-out of the SWIFT intervention was because they were feeling better after their hospital stay. The most common reason for opting-out of the SWIFT intervention was that the home visits were not needed because the participant was feeling good or did not consider them self to be a “sick” person that needed home visits. This possibility is corroborated by previous research by van Grunsven et al.37 Interestingly, while we found that respiratory disease was significantly associated with opting out of the intervention but not with having a 30-day readmission, others have found high readmission rates (30-days and beyond) among patients with COPD.39–41 Further research among older patients with COPD and other respiratory conditions is needed.
All but one 30-day readmission among our SWIFT intervention study participants was unplanned. We found significantly higher odds of 30-day readmission among participants diagnosed with cancer. Recent studies of hospitalized cancer patients also found significantly higher 30-day rehospitalization rates.42, 43 These findings and that of the present study suggest that effects of cancer and its treatment may place patients with cancer at increased risk for unplanned 30-day rehospitalization. Additionally, our finding of higher odds of 30-day readmission among participants opting out of our SWIFT intervention lends to the question of the role of patient self-determination in hospital readmissions. Patients cited several reasons for opting out of the SWIFT intervention—lack of perceived need, lack of interest, health provider fatigue—all reflecting personal preference toward less or no additional care. This finding is consistent with another study that found that patients who did not keep their outpatient appointments following hospital discharge have greater readmission rates.44 Other studies also have highlighted the variability in 30-day hospitalization rates driven by the risk and composition of the patient population they serve, the patient’s access to care, and the availability of community resources.20–22 In fact, studies have found that low income, demographic factors (e.g. older age), and psychosocial factors (e.g. baseline depression) are related to higher rates of hospital readmissions.36
With patient-level and community factors accounting for a high portion of readmission rates, penalizing hospitals for aspects they cannot control may be misguided. Moreover, although many hospitals have successfully undertaken efforts to improve transitional care provided to patients, some interventions have been found to be associated with an increase in readmission rates, believed to be caused by improved access to care and patient satisfaction.22,45
Limitations
Results of the study may be limited in several ways. First, the sample size may weaken the statistical power to detect differences between intervention opt-outs and intervention recipients. Secondly, study participants were recruited from a single, large, non-profit, urban hospital, and results may not be generalizable to other areas. Similarly, while our inclusion/exclusion criteria may have introduced selection bias that could impact generalizability of findings (i.e. excluding those with advance dementia or Alzheimer’s disease, homeless individuals, etc.), these criteria are appropriate for the skillset of social workers conducting a home-based intervention. Non-continuous patient eligibility screening and enrollment efforts (resulting in a large number of patients being discharged before making a participation determination) as well as the use of a single electronic medical record are also limitations of the present study. Self-reported patient data posed limitations as well: we could not fully understand the reasons that at-risk patients opted-out of the intervention, and we did not obtain patient self-reports to document emergency room visits and inpatient hospital stays to supplement the electronic medical records Additional electronic medical records and/or Medicare claims data would strengthen these findings. Also, due to the nature of the pilot study, only cognitively intact, English-speaking older adults were eligible to participate and, therefore, this sample may not be representative of hospitalized older adult patients.
Policy and Practice Implications
Findings here provide insight into characteristics and risk factors associated with opting-out of a care transitions intervention and suggest that some at-risk patients may not be receptive to in-home transitions interventions. Additionally, opting-out of a transition intervention may be associated with higher odds of hospital readmission. Current policies have charged hospitals with the task of reducing 30-day readmission rates, however, these results suggest that it may not be reasonable to place this burden solely on hospitals. Hospital readmissions are a costly phenomenon. Given the current ACA provisions, there would be a considerable benefit to being able to identify the patients that are resistant to interventions and opt-out to better inform resource allocation (including CMS funds, potential grant allocation, and hospital resources). More research is needed to confirm these findings and better understand patient characteristics associated with intervention opt-out among at-risk older adults.
Take-Away Points.
Current policies have charged hospitals with the task of reducing 30-day readmission rates, however, results of the present study contribute to growing research suggesting that it may not be reasonable to place this burden solely on hospitals.
Some at-risk patients at-risk for hospital readmission may not be receptive to in-home transitions interventions, but intervention refusal may be associated with higher odds of readmission.
Participants that opted-out of the intervention or those diagnosed with cancer were more likely to be readmitted within 30-days.
Participants with a respiratory condition were more likely to opt-out of the intervention.
Acknowledgments
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under award numbers 5 R21 AG034557-02 (ClinicalTrials.gov registry number NCT02232126) and partially by award number K99AG052647-02. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Additionally, the authors would like to thank Huntington Senior Care Network and Huntington Memorial Hospital for partnering with us to conduct this work, and each of the study participants that generously gave their time.
Footnotes
The authors have no conflict of interest to disclose.
References
- 1.Anderson MA, Helms LB, Hanson KS, DeVilder NW. Unplanned hospital readmissions: A home care perspective. Nurs Res. 1999;48(6):299–307. doi: 10.1097/00006199-199911000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Coleman EA. Falling through the cracks: Challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51(4):549–555. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- 3.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 4.Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital. CMAJ. 2004;170(3):345–349. [PMC free article] [PubMed] [Google Scholar]
- 5.Friedman B, Basu J. The rate and cost of hospital readmissions for preventable conditions. Med Care Res Rev. 2004;61(2):225–240. doi: 10.1177/1077558704263799. [DOI] [PubMed] [Google Scholar]
- 6.Coleman EA, Mahoney E, Parry C. Assessing the quality of preparation for posthospital care from the patient's perspective: The care transitions measure. Med Care. 2005;43(3):246–55. doi: 10.1097/00005650-200503000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Cornish PL, Knowles SR, Marchesano R, et al. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med. 2005;165:424–429. doi: 10.1001/archinte.165.4.424. [DOI] [PubMed] [Google Scholar]
- 8.Moore C, Wisnivesky J, Williams S, McGinn T. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18(8):646–651. doi: 10.1046/j.1525-1497.2003.20722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coleman EA, Williams MV. Executing high-quality care transitions: A call to do it right. J Hosp Med. 2007;2(5):287–290. doi: 10.1002/jhm.276. [DOI] [PubMed] [Google Scholar]
- 10.Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The importance of transitional care in achieving health reform. Health Aff. 2011;30(4):746–754. doi: 10.1377/hlthaff.2011.0041. [DOI] [PubMed] [Google Scholar]
- 11.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 12.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med. 2016;374(16):1543–1551. doi: 10.1056/NEJMsa1513024. [DOI] [PubMed] [Google Scholar]
- 13.Woolhandler S, Himmelstein DU. The hospital readmissions reduction program. N Engl J Med. 2015;375(5):493. doi: 10.1056/NEJMc1606658. [DOI] [PubMed] [Google Scholar]
- 14.U.S. Department of Health and Human Services. New HHS data shows major strides in patient safety, leading to improved care and savings. 2014 May 7; https://innovation.cms.gov/Files/reports/patient-safety-results.pdf.
- 15.Carey K, Lin M. Hospital readmission reductions program: Safety-net hospitals show improvement, modifications to penalty formula still needed. Health Aff. 2016;35(10):1918–1923. doi: 10.1377/hlthaff.2016.0537. [DOI] [PubMed] [Google Scholar]
- 16.Naylor M, Brooten D, Campbell R, et al. Comprehensive discharge planning and home follow-up of hospitalized elders. JAMA. 1999;281(7):613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 17.Coleman EA, Parry C, Chalmers S, Min S. The care transitions intervention: Results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 18.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: A randomized trial. Ann Internl Med. 2009;150(3):178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sheingold SH, Zuckerman R, Shartzer A. Understanding medicare hospital readmission rates and differeing penalties between safety-net and other hospitals. Health Aff. 2016;35(1):124–131. doi: 10.1377/hlthaff.2015.0534. [DOI] [PubMed] [Google Scholar]
- 20.Joynt KE, Jha AK. Research letter: Characteristics of hospitals receiving penalties under the hospital readmissions reduction program. JAMA. 2013;23(30):342–343. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 21.Joynt KE, Orav EJ, Jha AK. Thrity-day readmission rates for medicare beneficiaries by race and site of care. JAMA. 2011;305:675–81. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Joynt KE, Jha AK. Thirty-day readmissions — truth and consequences. N Engl J Med. 2012;366(15):1366–1369. doi: 10.1056/NEJMp1201598. http://dx.doi.org/10.1056/NEJMp1201598. [DOI] [PubMed] [Google Scholar]
- 23.American Hospital Association (AHA) TrendWatch: Rethinking the hospital readmissions reduction program. American Hospital Association; 2015. Mar, pp. 1–12. [Google Scholar]
- 24.Alkema GE, Wilber KH, Shannon GR, Allen D. Reduced mortality: The unexpected impact of a telephone-based care management intervention for older adults in managed care. Health Serv Res. 2007;42(4):1632–50. doi: 10.1111/j.1475-6773.2006.00668.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. J Am Geriatr Soc. 2004;52(5):675–684. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- 26.Charytan D, Kuntz RE. The exclusion of patients with chronic kidney disease from clinical trials in coronary artery disease. Kidney Int. 2006;70(11):2021–2030. doi: 10.1038/sj.ki.5001934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23(10):433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 28.Foreman MD. Reliability and validity of mental status questionnaires in elderly hospitalized patients. Nurs Res. 1987;36(4):216–20. [PubMed] [Google Scholar]
- 29.Roccaforte WH, Burke WJ, Bayer BL, Wengel SP. Reliability and validity of the short portable mental status questionnaire administered by telephone. J Geriatr Psychiarty Neurol. 1994;7(1):33–8. [PubMed] [Google Scholar]
- 30.Naylor MD, Brooten D, Campbell R, Jacobsen BS, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: A randomized clinical trial. JAMA. 1999;281(7):613–20. doi: 10.1001/jama.281.7.613. http://search.proquest.com.libproxy.usc.edu/docview/211347699?accountid=14749. Accessed 9/13/2013 1:27:59 AM. [DOI] [PubMed] [Google Scholar]
- 31.Coleman EA, Smith JD, Frank JC, Min S, Parry C, Kramer AM. Preparing patients and caregivers to participate in care delivered across settings: The care transitions intervention. [Accessed 9/13/2013];J Am Geriatr Soc. 2004 52(11):1817–1825. doi: 10.1111/j.1532-5415.2004.52504.x. 12:53:00 AM. [DOI] [PubMed] [Google Scholar]
- 32.Voss R, Gavenstein S, Baier R, et al. Recruiting hospitalized patients for research: How do participants differ from eligible nonparticipants? J Hosp Med. 2013;8(4):204–14. doi: 10.1002/jhm.2024. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. [Accessed December 2, 2016];FastFacts: Leading causes of death. http://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm. Published October 7, 2015. Updated October 7, 2016.
- 34.Chenna PR, Mannino DM. Outcomes of severe COPD exacerbations requiring hospitalization. Seminars in Respiratory and Critical Care Medicine. 2010;31(3):286–94. doi: 10.1055/s-0030-1254069. [DOI] [PubMed] [Google Scholar]
- 35.Mannino DM, Braman S. The epidemiology and economics of chronic obstructive pulmonary disease. Proceedings of the American Thoracic Society. 2007;4:502–506. doi: 10.1513/pats.200701-001FM. [DOI] [PubMed] [Google Scholar]
- 36.Coventry PA, Gemmell I, Todd CJ. Psychosocial risk factors for hospital readmission in COPD patients on early discharge services: A cohort study. BMC Pulmonary Medicine. 2011;11(49):1–10. doi: 10.1186/1471-2466-11-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van Grunsven PM, can Schayck CP, van Kollengurg HJ, et al. The rold of "fear of corticosterioids" in nonparticipation in early intervention with inhaled corticosterioids in asthma and COPD in general practice. Eur Respir J. 1998;11:1178–1181. doi: 10.1183/09031936.98.11051178. [DOI] [PubMed] [Google Scholar]
- 38.Rennard SI, Vestbo J. COPD: The dangerous underestimate of 15% The Lancet. 2006;367(9518):1216–1219. doi: 10.1016/S0140-6736(06)68516-4. doi: http://dx.doi.org/10.1016/S0140-6736(06)68516-4. [DOI] [PubMed] [Google Scholar]
- 39.Genao L, Durheim MT, Mi X, Todd JL, Whitson HE, Curtis LH. Early and long-term outcomes of older adults after acute care encounters for chronic obstructive pulmonary disease exacerbation. Annals ATS. 2015;12(12):1805–1812. doi: 10.1513/AnnalsATS.201504-250OC. http://dx.doi.org/10.1513/AnnalsATS.201504-250OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kon SSC, Jones SE, Schofield SJ, et al. Gait speed and readmission following hospitalisation for acute exacerbations of COPD: A prospective study. Thorax. 2015;70(12):1131–1137. doi: 10.1136/thoraxjnl-2015-207046. [DOI] [PubMed] [Google Scholar]
- 41.Laverty AA, Elkin SL, Watt HC, et al. Impact of a COPD discharge care bundle on readmissions following admission with acute exacerbation: Interrupted time series analysis. PLoS One. 2015;10(2):e0116187. doi: 10.1371/journal.pone.0116187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chiang LY, Liu J, Flood KL, et al. Geriatric assessment as predictors of hospital readmission in older adults with cancer. J Geriatr Oncol. 2015;6:254–261. doi: 10.1016/j.jgo.2015.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Allaudeen N, Vidyarthi A, Maselli J, Auerbach A. Redefining readmission risk factors for general medicine patients. J Hosp Med. 2011;6(2):54–60. doi: 10.1002/jhm.805. [DOI] [PubMed] [Google Scholar]
- 44.Nelson EA, Maruish ME, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatric Services. 2000;51:885–889. doi: 10.1176/appi.ps.51.7.885. [DOI] [PubMed] [Google Scholar]
- 45.Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? N Engl J Med. 1996;334:1441–7. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]