Abstract
Background
The Mini-BESTest is a recently developed balance assessment tool that incorporates challenging dynamic balance tasks. Few studies have compared the psychometric properties of the Mini-BESTest to the commonly used Berg Balance Scale (BBS). However, the utility of these scales in relationship to post stroke walking speeds has not been explored.
Objectives
The purpose of this study was to compare the sensitivity and specificity of the Mini-BESTest and BBS to evaluate walking speeds in individuals with stroke.
Design
A retrospective exploratory design.
Methods
Forty-one individuals with chronic stroke were evaluated with the Mini-BESTest, BBS, and 10-meter self-selected walk test (10MWT). Based on their self-selected gait speeds (below or above 0.8 m/s), participants were classified as slow and fast walkers.
Results
Significant linear correlations were observed between the Mini-BESTest vs. BBS (r = 0.72, p ≤ 0.001), Mini-BESTest vs. 10MWT (r = 0.58, p ≤ 0.001), and BBS vs. 10MWT (r = 0.30, p = 0.05). Independent t-tests comparing the balance scores for the slow and fast walkers revealed significant group differences for the Mini-BESTest (p =0.003), but not for the BBS (p = 0.09). The Mini-BESTest demonstrated higher sensitivity (93%) and specificity (64%) compared to the BBS (sensitivity 81%, specificity 56%) for discriminating participants into slow and fast walkers. No significant results were observed with the FMLE-M scores.
Conclusions
The Mini-BESTest has a greater discriminative ability than the BBS to categorize individuals with stroke into slow and fast walkers.
Introduction
Walking speed is an important predictor of post stroke functional recovery.1 It is also important to stroke survivors as recovery of walking is one of the primary self-reported goals for rehabilitation.2 This is not surprising as only half of the high functioning stroke survivors are able to achieve walking speeds that translate to independent community ambulation.3 One of the key determinants of walking speed is balance. Deficits in balance influences self-selected walking speeds at the time of discharge, and also affects the ability of stroke survivors to change from self-selected to fast walking speeds.4–6 Currently, the Berg Balance Scale (BBS) is the most widely used clinical assessment scales for quantifying balance post stroke.7,8 The psychometric properties of the BBS have been extensively validated, and it is well known for its validity, interrater and intrarater reliability. However, the BBS is criticized for its ceiling effects,9 its inability to predict falls,10 and its inability to identify the underlying impairment causing imbalance in stroke.11
The Mini-BESTest, the shorter version of the Balance Evaluation Systems Test (BEST), is a recently developed balance assessment tool that incorporates system-specific balance assessments.12 It has been demonstrated to have a high intrarater and interrater reliability, and is useful in evaluating balance deficits in individuals with Parkinson’s disease.13 Recently, the Mini BESTest was identified to have excellent internal consistency, and high intrarater and interrater reliability in individuals with chronic stroke.14 Although a few studies have compared the effectiveness of BBS to the Mini-BESTest for skewness and fall prediction post stroke,14,15 to our knowledge no previous study has compared the usefulness of these tests in relationship to post stroke walking speed. This is of clinical relevance as balance deficits are a key component of walking disability, and understanding the relationship between balance (as measured with the MiniBESTest) and walking speed may provide a better guidance for more directed clinical decision making. Hence in this retrospective study, our primary aim was to compare the sensitivity and specificity of the BBS and Mini-BESTest in relationship to self-selected walking ability (measured with the 10-meter walk test (10MWT)) in chronic stroke survivors.
Method
Study Overview
This study uses a retrospective comparative exploratory design. The data were collected as a part of baseline assessments for a larger ongoing randomized control trial conducted by the Brain Plasticity Laboratory at the University of Illinois at Chicago. All participants were evaluated with the Mini-BESTest, BBS, and 10MWT as part of their baseline assessments by a trained physical therapist.
Participants
Forty-one individuals with chronic stroke (mean age: 59.4 years, 31 males and 10 females) participated in this study. These participants had completed the ongoing research trial as of August 2016, and thus were included in this study. Inclusion criteria for the larger clinical trial included those with a first-ever unilateral stroke at least six months prior to participation in the study, residual hemiparetic gait deficits, ability to walk with or without an assistive device for at least five minutes, and lower limb Fugl-Meyer Motor score between 20–30. Exclusion criteria for the study included cognitive impairments (score of less than 24 on Mini-Mental State Examination (MMSE)), prior orthopedic injuries or impairments that could interfere with mobility, uncontrolled cardiorespiratory or metabolic diseases, and lesions pertaining to the brainstem or cerebellum (confirmed from medical records). All participants signed an informed consent form approved by Institutional Review Board at the University of Illinois, Chicago.
Clinical Assessments
Mini-BESTest
The Mini-BESTest is a 14-item balance scale that measures dynamic balance specifically anticipatory transitions, postural responses, sensory orientation while standing on a compliant or inclined base of support, and dynamic stability during gait.12 Each task is rated on a 2-point ordinal scale from 0 to 2; a score of 0 indicating that a person is unable to perform the task, score of 2 indicates normal performance. The maximum score for this scale is 28.
Berg Balance Scale (BBS)
The BBS is a 14-item balance scale that measures static and dynamic balance.16 It contains various items that requires the participant to maintain positions of varying difficulty and perform tasks such as standing and sitting unsupported, transfers, turning to look over shoulders, and place alternate foot on stool. Each task is scored on a 4-point ordinal scale from 0 to 4; for a maximum score of 56.
10-meter walk test (10MWT)
Participants were instructed to walk at their self-selected comfortable speed for a set distance of 10-meters for two trials. Time to walk 10-meters was measured using a simple stop watch. The average walking speed (distance divided by time) was calculated in meters per second. A speed of 0.8 m/s is indicative of community ambulation.17,18 A gait speed ≥ 0.8 m/s was considered to be a ‘fast walker’ and a speed lower than 0.8 m/s was considered to be a ‘slow walker’.
Statistical Analyses
All statistical analyses were conducted using SPSS 19.0 software (IBM Corp., Armonk, NY). Normality of each variable was confirmed with Shapiro-Wilk’s tests of normality on the studentized residuals. We used Pearson’s correlation analyses to examine the strength of relationship between the different outcomes variables. Correlation coefficients of lesser than 0.49 were interpreted as poor, between 0.50 to 0.79 as moderate, and higher than 0.80 as excellent.19 Fisher r-to-z transformations were conducted to directly compare the magnitude of correlations. An independent sample t-test was conducted to compare the Mini-BESTest and BBS between the participants divided into slow and fast walkers. An effect size estimation using Cohen’s d was performed to compare the standardized mean differences. Effect sizes were considered to be small (d = 0.2), medium (d = 0.5), and large (d = 0.8) based on benchmarks suggested by Cohen (1988).20 Finally, receiver operating characteristic (ROC) curve analysis was used to determine the relative performance of Mini-BESTest and BBS for classifying participants into two groups based on their walking speeds. The accuracy for each test was assessed using area under the curve (AUC), which can be interpreted as probability of correctly classifying participants into the designated groups (i.e. slow vs. fast walkers). An AUC of 1.00 is considered to be a perfect test, while an area of 0.5 is considered to have a low diagnostic value. The optimal cut-off points for the ROC for discriminating between the groups were chosen by selecting the best data point that maximizes the additive effect of sensitivity and specificity. An alpha level of 0.05 was considered to be significant.
Results
Relevant demographic characteristics of the study participants are summarized in Table 1. The BBS scores ranged from 35 to 55, and the Mini-BESTest scores ranged from 10 to 30 (Figure 1). We found a significant positive correlation between the Mini-BESTest and the BBS (r = 0.720, p ≤ 0.001).
Table 1.
Characteristics of study participants
| Mean (SD) | |
|---|---|
| Age (years)* | 59.4 (9.05) |
| Sex (male/female) | 31/10 |
| Time since stroke (years)* | 5.68 (4.29) |
| Type of stroke (ischemic/hemorrhagic) | 35/6 |
| Hemiplegic side (right/left) | 21/20 |
| Assistive Device for walking 10 meters (none/cane) | 38/3 |
| MMSE (/30)* | 28.43(1.94) |
| FMLE-M (/68)* | 50.59(6.17) |
| BBS (/56)* | 48.51(4.84) |
| Mini-BESTest (/28)* | 19.02(4.51) |
| 10 MWT (FW/SW) | 16/25 |
values are presented as means and standard deviations, others are categorical values. Mini-Mental State Examination (MMSE), Fugl Meyer Lower Extremity Motor Score (FMLE-M), Berg Balance Scale (BBS), Mini-Balance Evaluation Systems Test (Mini-BESTest), 10-meter walk test (10MWT). Participants were classified into fast walkers (FW, ≥ 0.8m/s) and slow walkers (SW, < 0.8m/s).
Figure 1.
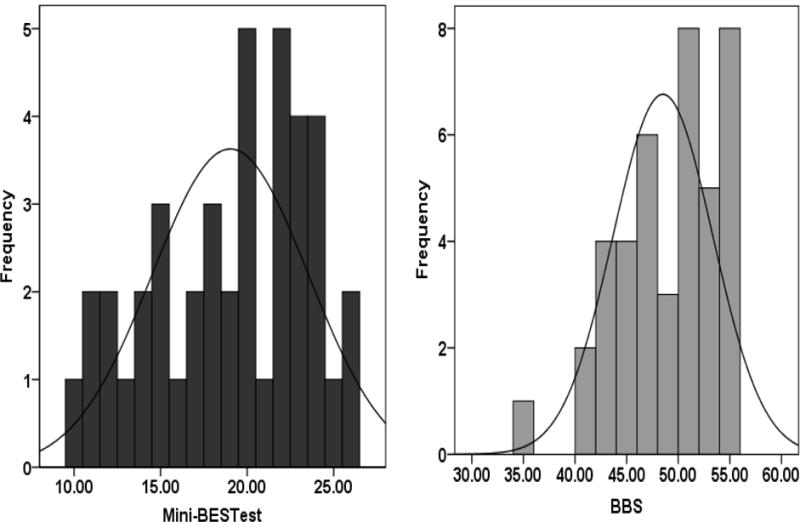
Frequency distribution of scores for the Mini-Balance Evaluations Systems test (Mini-BESTest) and Berg Balance Scale (BBS). Mini-BESTest: skewness = −0.401, kurtosis = −0.907; BBS: skewness = −0.665, kurtosis = −0.110.
The Mini-BESTest and BBS also showed a significant linear relationship with the 10 MWT (Mini-BEST: r = 0.576, p ≤ 0.001; BBS: r = 0.303, p < 0.05; Figure 2). A Fisher r-to-z transformation for direct comparison of r values revealed that the z score for the Mini-BESTest (z=0.663) was higher than the BBS (z=0.256). Based on our apriori cut-off speed of 0.8 m/s, 25 participants were classified as slow walkers, and 16 participants as fast walkers. Independent t-tests comparing the balance test scores for the slow and fast walkers showed significant group differences for the Mini-BESTest (t = 3.235, p =0.003, d = 1.1.4) but not the BBS (t = 1.731, p = 0.09, d = 0.59) (Figure 3). The effect size for the Mini-BESTest was found to exceed Cohen’s (1988) convention for a large effect (d=0.80).
Figure 2.
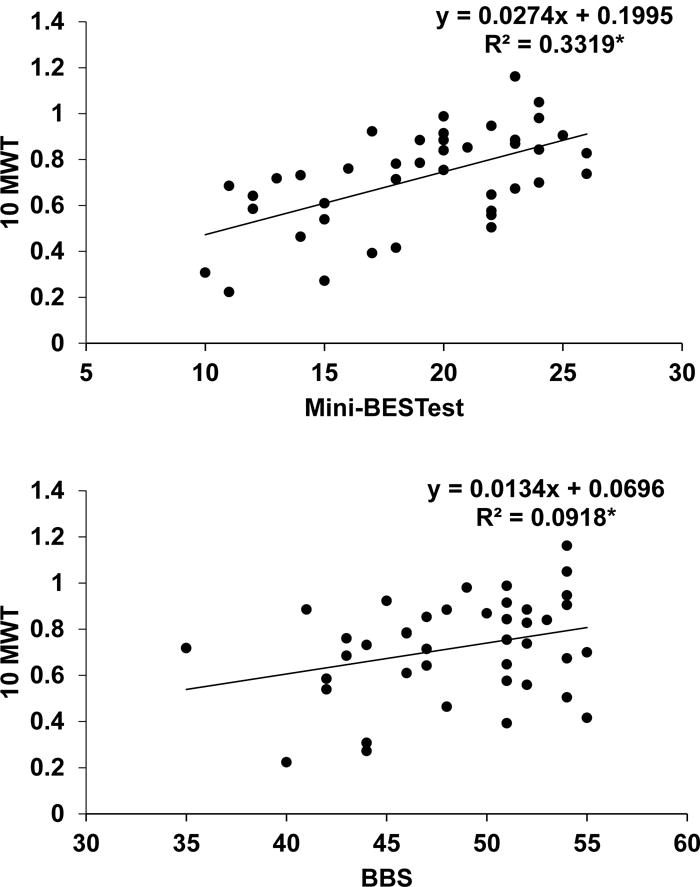
Scatterplots showing the relationship between 10-meter walk test, and the clinical balance scales: Mini-BESTest and Berg Balance Scale (BBS). (*) represents p ≤ 0.05
Figure 3.
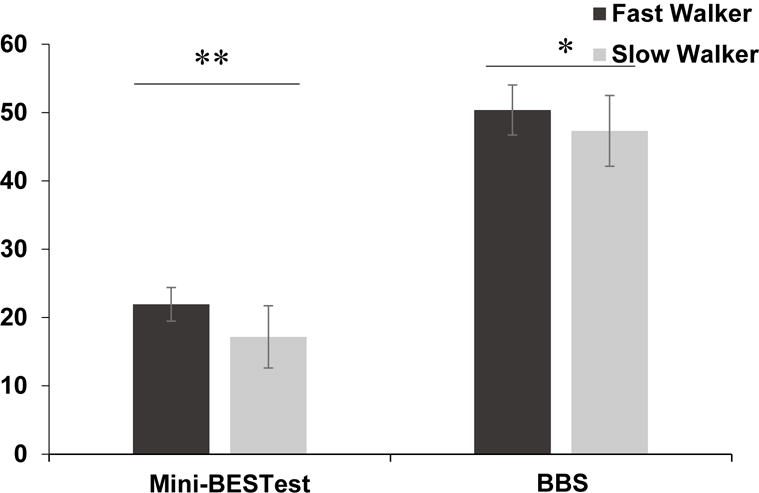
ndependent sample t-tests demonstrated significant differences between the Fast Walkers (FW) and Slow Walkers (SW)) for the Mini-BESTest and BBS. Bars are means and error bars are standard deviations. (*) represents p ≤ 0.05; (**) represents p ≤ 0.01.
ROC analyses was used to further evaluate the discriminative ability of the Mini-BESTest and BBS to classify participants into slow and fast walkers. The AUC for the BBS was 0.671 ± 0.08 (p = 0.06) and the AUC for the Mini-BESTest was 0.809 ± 0.06 (p = 0.001) (Figure 4). The optimal cut-off point for the Mini-BESTest was determined to be 18.5 (out of 28), resulting in a sensitivity of 93% and specificity of 64%. The optimal cut-off point for the BBS was determined to be 47.5 (out of 56), producing a sensitivity of 81% and specificity of 56%.
Figure 4.
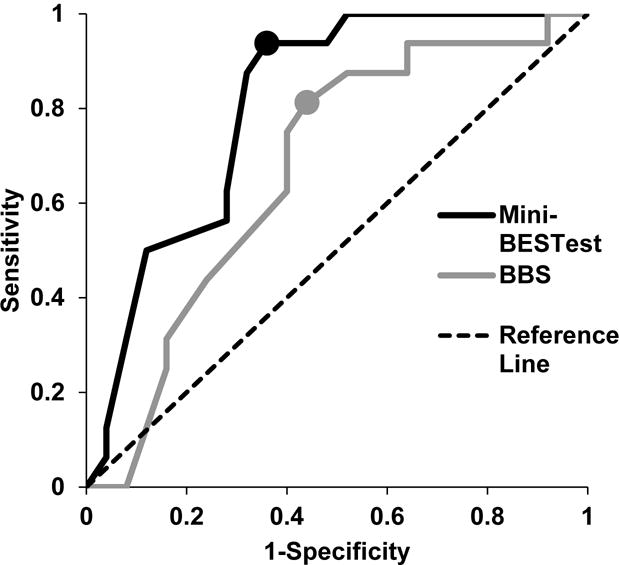
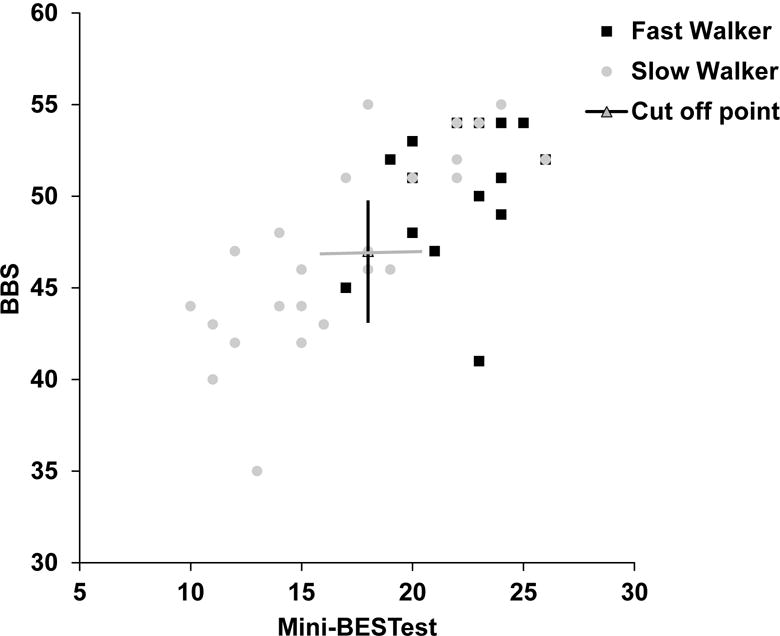
(4A) Receiver operating characteristic curves of the Mini-BESTest (black line) and BBS (gray line) for classifying participants into fast and slow walkers. The filled circles indicate the cut-off points for differentiating participants into fast and slow walkers based on their self-selected gait speeds. (4B) Scatter plot of Mini-BESTest and BBS for fast and slow walkers. The gray circles denotes slow walkers and filled squares depict fast walkers. The cut-off points for the Mini-BESTest and BBS are represented by black vertical and gray horizontal lines respectively.
Discussion
In this study, we compare the discriminative ability of two balance tests to categorize walking speeds in a cohort of chronic stroke survivors. Our results suggest that the Mini-BESTest may have a greater discriminative ability than the BBS to categorize chronic stroke survivors into slow and fast walkers. This is the first study to compare the newly developed Mini-BESTest with the BBS in individuals with chronic stroke.
The BBS is a commonly used tool for measuring balance post stroke. It is reliable, valid and can be utilized even in individuals who do not demonstrate independent walking function.7 Since it was originally intended to assess balance in older frail adults, the BBS does not include challenging tasks that test dynamic balance, leading to ceiling effects in individuals who exhibit moderate recovery.9,21 The Mini-BESTest, a shorter version of the original Balance Evaluations System Test, was developed to assess functional balance, and focusses on tasks that involve walking and dynamic balance.12 It was developed with an intent to assist clinicians to identify the underlying postural deficits in individuals with poor balance.22 Since the first publication of the Mini-BESTest in 2011, many studies have examined the psychometric properties of the Mini-BESTest, providing support for its reliability and validity in individuals with Parkinson’s disease and stroke.23 Tsang et al. (2013) reported the Mini-BESTest to be an instrument with high reliability and validity with no floor or ceiling effects in community dwelling stroke survivors.14 Only few studies have compared the responsiveness of the Mini-BESTest with standard scales such as the BBS,13,24 and to the best of our knowledge none have compared the performance of both instruments in individuals with chronic stroke especially in the context of walking recovery.
In the present study, we found the Mini-BESTest to be moderately correlated with the BBS. It was interesting to note that in our cohort of 41 participants, only 2 had reached the maximum score on the BBS, and none for the Mini-BESTest. This was also reflected in the slightly decreased skewness of the Mini-BESTest compared to the BBS.
The primary aim of this study was to compare the discriminative abilities of the two balance instruments to evaluate sub-classifications of gait speeds. Walking recovery following stroke has been reported as a key indicator of functional status and clinical improvement.25 In the present study, we found both the instruments to be significantly and positively correlated with self-selected gait speeds. This is not surprising as balance is a key component for recovery of walking.26 Our results are concurrent with other studies that have reported the BBS to predict variance in walking ability at the time of discharge and initial walking function in acute stroke survivors,4,27 as well as walking speeds in chronic stroke survivors.17,28 This finding also supports the concurrent validity of the Mini-BESTest as a balance assessment tool in stroke. The Mini-BESTest had a slightly higher correlation to walking speed, perhaps because some components of this instrument involves more dynamic tasks, especially the single leg standing task which encourages participants to use their affected leg. Although the BBS also includes the single leg standing task, the participant has the option to use either leg for the test thereby diminishing the effectiveness of this task. The difference between the two scales was apparent when comparing their capacity to evaluate gait speeds. The Mini-BESTest scores were different for the cohort of slow vs. fast walkers, while there was no difference with the BBS. The AUC was significant and higher for the Mini-BESTest compared to the BBS. The cut-off point to identify stroke survivors who had fast gait speeds (0.8 m/s or greater) for the Mini-BESTest was 18.5 and for the BBS was 47.5. Previously numerous cut-off points have been reported for the BBS. A cut-off score of lesser than 31 on the BBS is an indication of fall risk in stroke,29 and less than 19 indicates stroke survivors with low function.15 We are the first to report cut-off points for the BBS and Mini-BESTest to identify fast walkers. It is interesting to note the different cut-off scores established for the BBS for assessment of post stroke function. However, it is beyond the scope of this paper to provide insight into potential contributors for this incongruence, and future research may provide further understanding.
Based on these cut-off points for walking speeds, a comparable specificity was found between both scales but the Mini-BESTest showed a higher sensitivity than the BBS. Specificity is the likelihood of correctly identifying a non-existent risk (such as identifying people who do not fall or those who are community ambulators). Sensitivity is the likelihood of correctly identifying an existent risk (i.e. people who will fall or people who will not be community ambulators). Our findings indicate that a score greater than 19 on the Mini-BESTest may more correctly identify individuals with stroke who may achieve community ambulation. This might be of relevance for clinicians as walking speeds and balance are well associated.4,5 For example, if a patient achieves a score of 19 and greater on the Mini-BESTest but does not have walking speeds greater than 0.8 m/s, then this may indicate that individuals with stroke maybe slowing down their walking due to an underlying problem other than balance, such as strength deficits, fear of falling or cognitive processing. The clinician could use this information to target appropriate treatment activities to achieve faster walking speeds. On the other hand, if a patient scores lesser than 19 on the Mini-BESTest, then appropriate treatment activities targeting balance should be implemented before focusing on improving walking speed. However, we acknowledge that the causes for balance impairment and walking recovery are complex in nature. The clinical implications suggested in this study are the first step towards further research using the Mini-BESTest in chronic stroke survivors.
Conclusions
In this study, we found both the Mini-BESTest and the Berg Balance Scale were significantly correlated with self-selected gait velocity, but the Mini-BESTest demonstrated higher sensitivity than the BBS to discriminate slow and fast walkers. A Mini-BESTest score of 18.5 can be used to identify individuals with stroke who have the capacity to ambulate at speeds higher than 0.8 m/s. This cut-off score could indicate that stroke survivors slower than 0.8 m/s are capable of improving their walking speeds with more directed therapy, under the assumption that there no other factors impeding walking ability. Further research is needed to understand whether this cut-off score can translate to faster walking speeds with appropriate therapies.
Acknowledgments
Sources of Funding: National Institutes of Health under award number R01HD75777 (SM)
Footnotes
Part of this work has been presented as a poster at the 2016 Annual Meeting for the American Society of Rehabilitation Medicine in Chicago, Illinois.
References
- 1.Richards C, Malouin F, Dumas F, Tardif D. Gait velocity as an outcome measure of locomotor recovery after stroke. Gait Analysis: Theory and Application St Louis, Mo: Mosby. 1995:355–364. [Google Scholar]
- 2.Bohannon R, Andrews A, Smith M. Rehabilitation goals of patients with hemiplegia. International Journal of Rehabilitation Research. 1988;11:181–182. [Google Scholar]
- 3.Jørgensen HS, Nakayama H, Raaschou HO, Vive-Larsen J, Støier M, Olsen TS. Outcome and time course of recovery in stroke. Part I: Outcome. The Copenhagen stroke study. Archives of Physical Medicine and Rehabilitation. 1995;76(5):399–405. doi: 10.1016/s0003-9993(95)80567-2. [DOI] [PubMed] [Google Scholar]
- 4.Bland MD, Sturmoski A, Whitson M, et al. Prediction of Discharge Walking Ability From Initial Assessment in a Stroke Inpatient Rehabilitation Facility Population. Archives of Physical Medicine and Rehabilitation. 2012;93(8):1441–1447. doi: 10.1016/j.apmr.2012.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Middleton A, Braun CH, Lewek MD, Fritz SL. Balance impairment limits ability to increase walking speed in individuals with chronic stroke. Disability and rehabilitation. 2016:1–6. doi: 10.3109/09638288.2016.1152603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Langhammer B, Lindmark B, Stanghelle JK. The relation between gait velocity and static and dynamic balance in the early rehabilitation of patients with acute stroke. Advances in Physiotherapy. 2006;8(2):60–65. [Google Scholar]
- 7.Blum L, Korner-Bitensky N. Usefulness of the Berg Balance Scale in stroke rehabilitation: a systematic review. Physical therapy. 2008;88(5):559–566. doi: 10.2522/ptj.20070205. [DOI] [PubMed] [Google Scholar]
- 8.Tyson S, Connell LA. How to measure balance in clinical practice. A systematic review of the psychometrics and clinical utility of measures of balance activity for neurological conditions. Clinical Rehabilitation. 2009 doi: 10.1177/0269215509335018. [DOI] [PubMed] [Google Scholar]
- 9.Knorr S, Brouwer B, Garland SJ. Validity of the Community Balance and Mobility Scale in community-dwelling persons after stroke. Archives of physical medicine and rehabilitation. 2010;91(6):890–896. doi: 10.1016/j.apmr.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 10.Belgen B, Beninato M, Sullivan PE, Narielwalla K. The association of balance capacity and falls self-efficacy with history of falling in community-dwelling people with chronic stroke. Archives of physical medicine and rehabilitation. 2006;87(4):554–561. doi: 10.1016/j.apmr.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 11.Leroux A, Pinet H, Nadeau S. Task-oriented intervention in chronic stroke: changes in clinical and laboratory measures of balance and mobility. American journal of physical medicine & rehabilitation. 2006;85(10):820–830. doi: 10.1097/01.phm.0000233179.64769.8c. [DOI] [PubMed] [Google Scholar]
- 12.Franchignoni F, Horak F, Godi M, Nardone A, Giordano A. Using psychometric techniques to improve the Balance Evaluation Systems Test: the mini-BESTest. Journal of rehabilitation medicine. 2010;42(4):323–331. doi: 10.2340/16501977-0537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.King LA, Priest KC, Salarian A, Pierce D, Horak FB. Comparing the Mini-BESTest with the Berg Balance Scale to evaluate balance disorders in Parkinson’s disease. Parkinson’s Disease. 2012 doi: 10.1155/2012/375419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsang CS, Liao L-R, Chung RC, Pang MY. Psychometric properties of the Mini-Balance Evaluation Systems Test (Mini-BESTest) in community-dwelling individuals with chronic stroke. Physical therapy. 2013;93(8):1102–1115. doi: 10.2522/ptj.20120454. [DOI] [PubMed] [Google Scholar]
- 15.Chinsongkram B, Chaikeeree N, Saengsirisuwan V, Viriyatharakij N, Horak FB, Boonsinsukh R. Reliability and validity of the Balance Evaluation Systems Test (BESTest) in people with subacute stroke. Physical therapy. 2014;94(11):1632–1643. doi: 10.2522/ptj.20130558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berg KO, Maki BE, Williams JI, Holliday PJ, Wood-Dauphinee SL. Clinical and laboratory measures of postural balance in an elderly population. Archives of physical medicine and rehabilitation. 1992;73(11):1073–1080. [PubMed] [Google Scholar]
- 17.Joa KL, Kwon SY, Choi JW, Hong SE, Kim CH, Jung HY. Classification of walking ability of household walkers versus community walkers based on K-BBS, gait velocity and upright motor control. Eur J Phys Rehabil Med. 2015;51(5):619–625. [PubMed] [Google Scholar]
- 18.Perry J, Garrett M, Gronley JK, Mulroy SJ. Classification of walking handicap in the stroke population. Stroke. 1995;26(6):982–989. doi: 10.1161/01.str.26.6.982. [DOI] [PubMed] [Google Scholar]
- 19.Pearson K. Notes on the history of correlation. Biometrika. 1920;13:25–45. [Google Scholar]
- 20.Cohen J. Statistical power analysis for the behavioral sciences. Vol. 1988. Hilsdale. NJ: Lawrence Earlbaum Associates; p. 2. [Google Scholar]
- 21.Salbach NM, Mayo NE, Higgins J, Ahmed S, Finch LE, Richards CL. Responsiveness and predictability of gait speed and other disability measures in acute stroke. Archives of Physical Medicine and Rehabilitation. 2001;82(9):1204–1212. doi: 10.1053/apmr.2001.24907. [DOI] [PubMed] [Google Scholar]
- 22.Horak FB, Wrisley DM, Frank J. The Balance Evaluation Systems Test (BESTest) to differentiate balance deficits. Phys Ther. 2009;89(5):484–498. doi: 10.2522/ptj.20080071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Di Carlo S, Bravini E, Vercelli S, Massazza G, Ferriero G. The Mini-BESTest: a review of psychometric properties. International Journal of Rehabilitation Research. 2016;39(2):97–105. doi: 10.1097/MRR.0000000000000153. [DOI] [PubMed] [Google Scholar]
- 24.Godi M, Franchignoni F, Caligari M, Giordano A, Turcato AM, Nardone A. Comparison of reliability, validity, and responsiveness of the mini-BESTest and Berg Balance Scale in patients with balance disorders. Physical therapy. 2013;93(2):158–167. doi: 10.2522/ptj.20120171. [DOI] [PubMed] [Google Scholar]
- 25.Roth EJ, Merbitz C, Mroczek K, Dugan SA, Suh WW. Hemiplegic gait: Relationships between walking speed and other temporal parameters1. American journal of physical medicine & rehabilitation. 1997;76(2):128–133. doi: 10.1097/00002060-199703000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Woollacott MH, Pei-Fang T. Balance control during walking in the older adult: research and its implications. Physical therapy. 1997;77(6):646. doi: 10.1093/ptj/77.6.646. [DOI] [PubMed] [Google Scholar]
- 27.Makizako H, Kabe N, Takano A, Isobe K. Use of the Berg Balance Scale to predict independent gait after stroke: a study of an inpatient population in Japan. PM&R. 2015;7(4):392–399. doi: 10.1016/j.pmrj.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 28.Patterson SL, Forrester LW, Rodgers MM, et al. Determinants of walking function after stroke: differences by deficit severity. Archives of physical medicine and rehabilitation. 2007;88(1):115–119. doi: 10.1016/j.apmr.2006.10.025. [DOI] [PubMed] [Google Scholar]
- 29.Maeda N, Urabe Y, Murakami M, Itotani K, Kato J. Discriminant analysis for predictor of falls in stroke patients by using the Berg Balance Scale. Singapore medical journal. 2015;56(5):280. doi: 10.11622/smedj.2015033. [DOI] [PMC free article] [PubMed] [Google Scholar]


