Abstract
Introduction
Racial disparities in adult flu vaccination rates persist with African Americans falling below Whites in vaccine acceptance. Although the literature has examined traditional variables including barriers, access, attitudes, among others, there has been virtually no examination of the extent to which racial factors including racial consciousness, fairness, and discrimination may affect vaccine attitudes and behaviors.
Methods
We contracted with GfK to conduct an online, nationally representative survey with 819 African American and 838 White respondents. Measures included risk perception, trust, vaccine attitudes, hesitancy and confidence, novel measures on racial factors, and vaccine behavior.
Results
There were significant racial differences in vaccine attitudes, risk perception, trust, hesitancy and confidence. For both groups, racial fairness had stronger direct effects on the vaccine-related variables with more positive coefficients associated with more positive vaccine attitudes. Racial consciousness in a health care setting emerged as a more powerful influence on attitudes and beliefs, particularly for African Americans, with higher scores on racial consciousness associated with lower trust in the vaccine and the vaccine process, higher perceived vaccine risk, less knowledge of flu vaccine, greater vaccine hesitancy, and less confidence in the flu vaccine. The effect of racial fairness on vaccine behavior was mediated by trust in the flu vaccine for African Americans only (i.e., higher racial fairness increased trust in the vaccine process and thus the probability of getting a flu vaccine). The effect of racial consciousness and discrimination for African Americans on vaccine uptake was mediated by perceived vaccine risk and flu vaccine knowledge.
Conclusions
Racial factors can be a useful new tool for understanding and addressing attitudes toward the flu vaccine and actual vaccine behavior. These new concepts can facilitate more effective tailored and targeted vaccine communications.
Although immunization rates for seasonal influenza have increased over the past decade, racial disparities in adult influenza immunization rates persist with rates for non-Hispanic Black adults consistently lower than for non-Hispanic White adults [1]. In 2014–15, the Centers for Disease Control and Prevention (CDC) estimated that only 39% of Black adults were vaccinated compared to 47% of White adults [2]. Researchers have attempted to explain the disparity by documenting multiple factors on which racial groups differ: barriers to healthcare access and missed opportunities for vaccination [3, 4]; beliefs and attitudes [5, 6]; perceived risks of vaccination [7–9]; and socioeconomic status [1]. However, it is clear that traditional models cannot fully explain vaccine disparities.
As an alternative, we introduce an exploratory conceptual model that explores the role of race in vaccine decisions. We developed the model based on our previous survey research including our socio-ecological model on vaccine acceptance [10] and extensive qualitative research with African Americans and Whites. Figure 1 outlines the hypothesized connections among measures of racial factors that relate to the experience of being either African American or White in the United States, vaccine knowledge and attitudes, and vaccine behaviors. While the concept of race is fundamental in health disparities research, many researchers have been hesitant to critically explore race. A review of public health literature demonstrated that while race was one of the most commonly used variables, it was frequently used “uncritically” and “without definition” [11]. Alternatively, we employ Public Health Critical Race Praxis, which seeks to understand the inequalities that create health disparities and to eliminate the power hierarchies that structure them [12, 13]. In practice, this means emphasizing the role of race as a social construct, one that has been historically shaped and continues to be socially reinforced, and foregrounding research around the lived experience of inequality and racism as they contribute to negative health outcomes [12, 14]. This approach also means viewing race as a variable that captures shared experiences of racism and racial discrimination, since as a social construct, racial classification is based on phenotype and all dark-skinned individuals share the lived experience of being “black” as they navigate life in a racialized society [15].
Figure 1.
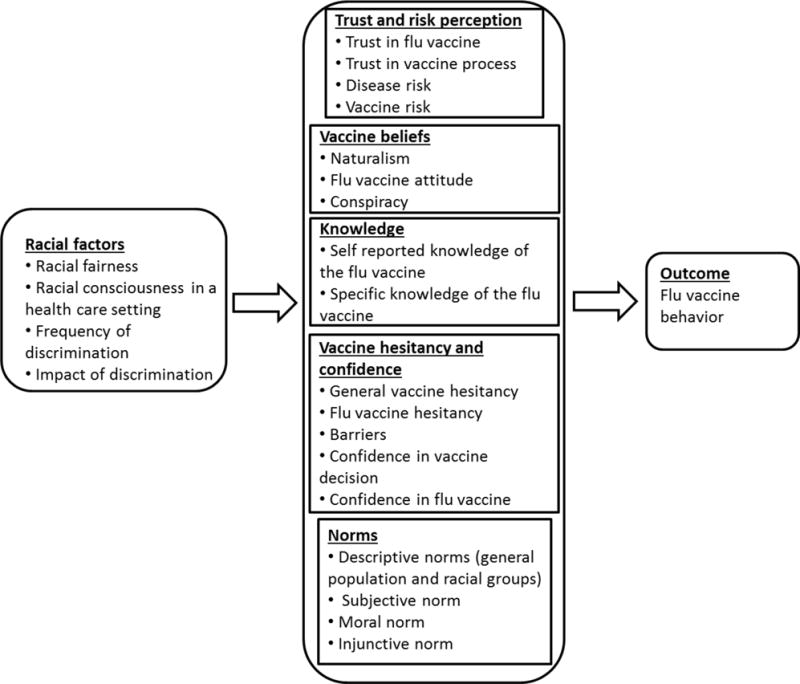
Exploratory Model for Understanding Vaccine Disparities
Evidence suggests that racial factors could affect vaccine uptake. Research demonstrates that racism is a fundamental determinant of health in the U.S. [16], operating through multiple pathways to directly and indirectly contribute to negative health outcomes [16, 17]. While institutionalized and cultural racism circumscribe socioeconomic opportunities for people of color and indirectly influence health, racism may be directly experienced through prejudice, stereotypes, stigma, and discrimination [16]. Experiences of discrimination in health care contribute to medical distrust, and both perceived discrimination and distrust are associated with a lower likelihood of receiving preventive health services, including seasonal influenza vaccines[18, 19]. Macintosh and colleagues (2013) found that survey participants labeled as white, regardless of their self-identified race, were more likely to get both flu and pneumococcal vaccines [20]. Recent work by Bleser and colleagues found that among chronically ill adults, those who reported perceived discrimination were about half as likely to have received a flu vaccine as those who did not report discrimination [21].
We are interested in the impact of one’s race and racism in the health care setting on vaccine associated knowledge, attitudes, beliefs and norms. Our conceptual model explores novel measures that aim to understand racial factors, defining racial consciousness in the health care setting as the awareness of oneself as a racial being in that setting, and racial fairness as perceptions of whether treatment, either by government or within a health care setting, is fair to one’s race. Other measures included frequency and impact of discrimination [22].
Our research questions include: 1) Are there differences between African Americans and Whites regarding the influenza vaccine in terms of vaccine knowledge and attitudes including trust, risk perception, vaccine beliefs, vaccine hesitancy and confidence, and social norms? 2) Do racial factors associated with being an African American or White in the U.S. relate to vaccine knowledge and attitudes including trust, risk perception, vaccine beliefs, vaccine hesitancy and confidence, and social norms? 3) Do racial factors relate to vaccine behaviors, and does vaccine knowledge and attitudes including trust, risk perception, vaccine beliefs, vaccine hesitancy and confidence, and social norms, mediate that relation?
Methods
We contracted with GfK to conduct this survey with target samples of 800 African American and 800 White non-institutionalized US adults over 18. GfK uses an address based sampling methodology to develop its KnowledgePanel, which is representative of the U.S.
Measures
We developed most of the survey instrument based on qualitative research, including 28 semi-structured interviews and focus groups (9 groups; n=90) with African Americans and Whites. We conducted 16 cognitive interviews with Whites and African Americans to test and clarify items. Table 2 identifies all items and their measurement. Demographics included age, race/ethnicity, gender, income, education, whether the respondent had health insurance and a regular health care provider. We utilized exploratory factor analysis to finalize our measures.
Table 2.
Survey Measures
| Concept/Variable | Type of scale & # of Items | Cronbach’s alpha | Abbreviated Item Wording | Response categories (# of Scale Points) |
|---|---|---|---|---|
| OUTCOME: Flu vaccine behavior | 1 | – | Did you get a flu vaccine this season | No or Yes (0 or 1) |
| RACIAL FACTORS | ||||
| Racial fairness* | Mean of 2 items | 0.702 |
|
Never (1) - Very often (5) |
| Racial consciousness in health care setting* | Mean of 4 items | 0.743 |
|
Never (1) - Very often (5) |
| Frequency of discrimination | 1 | – | How often have you experienced racial discrimination in healthcare settings | Never (1) - Frequently (3) |
| Impact of discrimination | 1 | – | How much has racial discrimination interfered with your getting good health care | Not at all (1) – A lot (4) |
| TRUST & RISK PERCEPTION | ||||
| Trust in the flu vaccine | 1 | – | Overall how much do you trust the flu vaccine | Not at all (1) - Completely (5) |
| Trust in the vaccine process | Mean of 5 items | 0.925 | When it comes to the vaccine process, how much do you trust: (1) the World Health Organization, (2) the pharmaceutical or drug companies, (3) the U.S. Food and Drug Administration (FDA), (4) the Centers for Disease Control and Prevention (CDC), and (5) the professionals who give the flu vaccine | Not at all - (5) (1) Completely |
| Perceived disease risk (conditional on actual vaccine behavior) | Mean of 4 items | 0.836 |
|
4 and 5-point scales |
| Perceived vaccine risk (conditional on actual vaccine behavior) | Mean of 4 items | 0.842 |
|
4 and 5-point scales |
| Perceived disease risk (conditional on actual vaccine behavior) | Mean of 4 items | 0.836 |
|
4 and 5-point scales |
| Perceived vaccine risk (conditional on actual vaccine behavior) | Mean of 4 items | 0.842 |
|
4 and 5-point scales |
| VACCINE BELIEFS | ||||
| Belief in naturalism | 1 | – | I use home remedies instead of vaccines to prevent the flu | Does not describe me (1) - Describes very well (4) |
| Flu vaccine attitude | 1 | – | In general how much do you favor or oppose the flu vaccine | Strongly oppose (1) - strongly favor (5) |
| Belief in conspiracy theories | Mean of 5 items | 0.881 |
|
Not at all true (1) - Definitely true (4) |
| FLU VACCINE KNOWLEDGE | ||||
| Self-reported flu knowledge | 1 | – | How much would you say you know about the flu vaccine | Nothing (1) - A great deal (5) |
| Specific flu knowledge | Count of # true-false statements correct (7) | – |
|
True or False |
| VACCINE HESITANCY & CONFIDENCE | ||||
| General vaccine hesitancy | 1 | – | Overall, how hesitant are you about getting vaccinations | Not at all hesitant (1) - Very hesitant (4) |
| Flu vaccine hesitancy | Mean of 2 items | 0.622 |
|
None at all (1) - A great deal (4) |
| Flu vaccine confidence | Mean of 4 items | 0.928 | Rating of adjectives describing the flu vaccine: (1) Necessary (2) Important (3) Safe (4) Effective | Not at all (1) - Very much (4) |
| Flu vaccine barriers | Mean of 2 items | 0.894 | Rating of adjectives describing the flu vaccine: (1) Affordable (2) Convenient | Not at all (1) - Very much (4) |
| Confidence in vaccine decision | 1 | – | How confident were you in your decision about the flu vaccine (wording conditional on their actual decision) | Not at all confident (1) - Very confident (4) |
| PERCEIVED SOCIAL NORMS | ||||
| Descriptive norm (US pop) | 1 | – | How many {of the people in the US} do you think get a flu vaccine every year | Few (1) - Nearly All (5) |
| Descriptive norm (my race) | 1 | – | How many {of people of your race} do you estimate get a flu vaccine every year | Few (1) - Nearly All (5) |
| Subjective norm | 1 | – | Of the people close to you what proportion want you to get a flu vaccine | Few (1) - Nearly all (5) |
| Moral norm | 1 | – | It is my moral obligation to other people to get a flu vaccine | Agreement: Not at all (1) - Very strongly (4) |
| Injunctive norm | 1 | – | What is the expectation at your workplace when it comes to the flu vaccine | No expectation (1) - Encouraged - Required (3) |
All questions were applicable to both black and white respondents since they use “people of my race” as a referent
For our Measures of Lived Experience (Racial Factors), exploratory factor analysis (principal component analysis with promax rotation) of 6 questions addressing issues of race and racism identified two factors, labeled “racial fairness” and “racial consciousness in a health care setting.” We also conducted principal axis factoring with oblique rotation of 6 items addressing vaccine attitudes, identifying two factors, labeled “flu vaccine confidence” and “barriers to the flu vaccine.” The scales were coded so that increasing values indicated greater confidence and increased barriers to getting the flu vaccine.
Analyses
The GfK data file included design-based weights to account for the recruitment, as well as both panel-based and study-specific post-stratification weights benchmarked against the 2014 Current Population Survey with respect to demographic and geographic distributions of the population over 18. Post-stratification weights were available to adjust for nonresponse as well as for under- and over-sampling of specific subpopulations imposed by the sampling design (e.g., by age, education, race, sex); all analyses were weighted to be nationally representative. Missingness ranged from 0% to about 3% for each variable, and was accommodated in each analysis as described below.
For the first research question, the sample-weighted means of these variables for both racial groups were compared using general linear models (i.e., simple regressions) with race as the explanatory variable, allowing for the proper accommodation of sampling weights. For the second question, measured variable path analysis was conducted using the Mplus software within each race group separately to assess the direct effects of the racial factor variables (racial fairness, racial consciousness in a health care setting, frequency and impact of discrimination) on vaccine attitudes and knowledge. For the third question, the direct effects of racial factors on vaccination behavior, along with the indirect effects via vaccine attitudes and knowledge, were assessed in a single path model. We did not do any modeling, in the path models, around demographics such as SES or education as confounders or modifiers. The rationale is that those variables are not viewed as precursors to racial factors, having spurious or moderating effects, but rather are intermediate sequelae of racial factors. As such, controlling for these sequelae would actually eliminate some of the pathways through which racial factors are believed to have their effects on the outcomes of interest. In the path models, full information maximum likelihood estimation was used to accommodate missingness, with rescaling corrections to standard errors to deal with potential nonnormality in the data; sampling weights were also incorporated into all analyses.
Results
Sample
For Whites, 1,329 were sampled, resulting in 838 respondents (completion rate of 63.1%). For African Americans, 1,599 were sampled, with 819 respondents (completion rate of 51.2%). Of the 1,657 completed surveys, 1,643 cases were valid for final analyses (see Table 1 for sample description). Participants received a cash-equivalent of $5.
Table 1.
Sample Demographics and Flu Vaccination Behavior and Intentions
| Overall U.S. Sample (N=1643) | White Non-Hispanic (N=834) | African American Non-Hispanic (N=809) | Chi-Square Test or t-test | |
|---|---|---|---|---|
| % | % | % | (Sig.) | |
| Sex | ||||
| Male | 47.7 | 50.5 | 44.7 | 0.011 |
| Female | 62.3 | 49.5 | 55.3 | |
| Age | ||||
| 18–29 | 16.4 | 14.9 | 17.9 | 0.007 |
| 30–44 | 18.9 | 18.6 | 19.3 | |
| 45–59 | 29.0 | 27.0 | 31.1 | |
| 60+ | 35.7 | 39.6 | 31.6 | |
| Mean Age (SD) | 51.2 (17.2) | 52.7 (17.8) | 49.7 (16.4) | <.001 |
| Marital Status | ||||
| Married/Living with partner | 54.3 | 65.9 | 42.3 | <.001 |
| Widowed/Divorced/Separated | 20.4 | 16.5 | 24.4 | |
| Never married | 25.3 | 17.5 | 33.4 | |
| Education | ||||
| Less than high school | 7.4 | 5.6 | 9.1 | <.001 |
| High School | 31.2 | 31.4 | 30.9 | |
| Some College | 29.8 | 26.1 | 33.5 | |
| Bachelor’ Degree or higher | 31.7 | 36.8 | 26.5 | |
| Income | ||||
| Less than $20,000 | 19.8 | 11.9 | 28.1 | <.001 |
| $20,000 to $39,999 | 20.3 | 17 | 23.6 | |
| $40,000 to $84,999 | 32.6 | 34.2 | 30.9 | |
| $85,000 or more | 27.3 | 36.9 | 17.4 | |
| Vaccine Behavior & Intentions | ||||
| Got flu shot | 49.0 | 53.4 | 44.4 | <.001 |
| Did not get flu shot | 51.0 | 46.6 | 55.6 | |
| Did not get flu shot but intend to | 13.1 | 9.7 | 16.8 |
Note. All numbers and percentages are unweighted. The significant levels are measuring the mean differences between Whites and African Americans.
Table 3 presents results for the first research question on differences between African Americans and Whites in vaccine attitudes and knowledge. The corresponding standardized effect size estimates and statistical significance (based on pooled and unpooled variance t-tests) are presented, with most vaccine-related variables demonstrating some level of statistical significance (i.e., p < .05). Whites had significantly higher trust in the flu vaccine and the vaccine process, as well as higher perceived risk of the disease and lower perceived risk of the vaccine. In contrast, African Americans perceived a higher risk of vaccine side effects, and lower risk from flu itself. African Americans were statistically significantly higher on naturalism and conspiracy, and less likely to favor the vaccine. Whites were significantly higher in both self-reported and specific knowledge. African Americans were significantly more hesitant about vaccines generally and the flu vaccine specifically, while perceiving more barriers to vaccination. There were no differences between African Americans and Whites in vaccine confidence. On social norms, Whites believed that higher proportions of their own race got the flu vaccine but lower proportion of the general population did; conversely, African Americans reported that a higher proportion of the general population were vaccinated but a lower proportion of African Americans were. More Whites believed a higher proportion of those close to them wanted them to get a flu vaccine. There were no statistically significant racial differences in moral and injunctive norms.
Table 3.
Weighted Means and Standardized Effect Size Estimates for African Americans and Whites
| AA | W |
|
||
|---|---|---|---|---|
| Outcome | ||||
| Flu vaccine behavior | 0.40 | 0.51 | 0.22*** | |
| Racial factors | ||||
| Racial fairness | 3.11 | 4.00 | 0.97*** | |
| Racial consciousness in health care settings | 2.36 | 1.90 | 0.57*** | |
| Frequency of discrimination | 1.34 | 1.08 | 0.80*** | |
| Impact of discrimination | 1.44 | 1.11 | 0.64*** | |
| Trust and risk perception | ||||
| Trust in flu vaccine | 2.89 | 3.18 | 0.25*** | |
| Trust in vaccine process | 3.00 | 3.23 | 0.25*** | |
| Risk of disease | 1.99 | 2.10 | 0.14* | |
| Risk of vaccine | 1.98 | 1.75 | 0.30*** | |
| Attitudes and beliefs | ||||
| Naturalism | 1.59 | 1.34 | 0.33*** | |
| Flu vaccine attitude | 3.41 | 3.72 | 0.26*** | |
| Conspiracy | 1.98 | 1.77 | 0.30*** | |
| Knowledge | ||||
| General knowledge | 3.12 | 3.29 | 0.16* | |
| Specific knowledge | 5.14 | 5.91 | 0.63*** | |
| Vaccine hesitancy and confidence | ||||
| General vaccine hesitancy | 1.98 | 1.70 | 0.31*** | |
| Flu vaccine hesitancy | 1.79 | 1.61 | 0.24** | |
| Barriers | 2.04 | 1.90 | 0.16** | |
| Confidence in flu vaccine | 2.97 | 3.03 | 0.07 | |
| Confidence in vaccine decision | 2.53 | 2.60 | 0.06 | |
| Norms | ||||
| Descriptive norm (general pop.) | 2.99 | 2.69 | 0.34*** | |
| Descriptive norm (race) | 2.55 | 2.88 | 0.37*** | |
| Subjective norm | 2.45 | 2.79 | 0.21** | |
| Moral norm | 1.97 | 2.00 | 0.03 | |
| Injunctive norm | 1.30 | 1.27 | 0.04 |
Note.
p<.05;
p<.01;
p<.001.
AA = African American; W = White. = Cohen’s estimated standardized effect size.
The second research question examined whether racial factors (as assessed by racial fairness, racial consciousness, frequency and impact of discrimination) affect the potential mediating vaccine attitudes and knowledge. Table 4 depicts the standardized path coefficients from the measured variable path analyses conducted separately for both samples, conveying the magnitude and statistical significance of the relations between the racial factors and each potential mediator. Racial fairness had stronger direct effects on the vaccine-related variables, as evident in the larger standardized path coefficients. For both groups, positive coefficients indicate that higher perceived racial fairness contributed to higher trust in the flu vaccine and the vaccine process, a more positive attitude toward the flu vaccine, higher confidence in the flu vaccine, and the perception that a higher proportion of those close to them wanted them to get a flu vaccine. Negative coefficients indicate that higher perceived racial fairness was associated with lower perceived risk of the flu vaccine, less belief in conspiracy theory, lower vaccine hesitancy in general, and lower perceived barriers to vaccine. However, the effects of racial fairness on some variables were statistically significant (p < .05) for African Americans but not for Whites, and vice versa. African Americans who reported higher perceived racial fairness also reported more positive vaccine norms for their race (.14). For Whites, higher perceived racial fairness was associated with less use of naturalism in lieu of vaccines (−.09), higher vaccine knowledge (self-reported, .10, and specific, .19), and higher agreement on their moral norm or obligation to other people to get a flu vaccine (.14).
Table 4.
Standardized Effects of Racial Factors on Attitudes, Beliefs, Norms, Knowledge about the Influenza Vaccine, and Vaccine Hesitancy
| Fairness | Consciousness | Frequency | Impact | |||||
|---|---|---|---|---|---|---|---|---|
| AA | W | AA | W | AA | W | AA | W | |
| Trust and risk perception | ||||||||
| Trust in flu vaccine | .22*** | .22*** | −.17*** | −.03 | −.04 | −.01 | .08 | .05 |
| Trust in vaccine process | .19** | .34*** | −.21*** | −.01 | −.03 | .00 | .01 | −.08 |
| Risk of disease | .06 | .08 | −.05 | −.01 | .11* | .06 | .07 | .04 |
| Risk of vaccine | −.10* | −.11** | .14** | .03 | .18*** | .01 | −.06 | .14* |
| Attitudes and beliefs | ||||||||
| Naturalism | −.01 | −.09* | .21*** | −.03 | .02 | −.03 | .04 | .28*** |
| Flu vaccine attitude | .11* | .14*** | −.12** | −.04 | −.06 | .04 | .06 | −.07 |
| Conspiracy | −.20*** | −.26*** | .28*** | .06 | .12* | .09 | .03 | .10 |
| Knowledge | ||||||||
| General knowledge | −.06 | .10* | .00 | −.08 | .06 | .05 | −.04 | .03 |
| Specific knowledge | .03 | .19*** | −.17*** | −.08 | −.09 | −.00 | .11* | −.16** |
| Vaccine hesitancy and confidence | ||||||||
| General vaccine hesitancy | −.10* | −.14*** | .17** | −.00 | −.02 | .07 | .10 | .02 |
| Flu vaccine hesitancy | .05 | −.05 | .01 | .03 | .00 | .01 | .14** | .19** |
| Barriers | −.16** | −.21*** | .14** | .05 | .02 | .02 | .04 | .02 |
| Confidence in flu vaccine | .16** | .22*** | −.16** | −.04 | −.03 | .01 | .01 | −.02 |
| Confidence in vac. decision | .00 | .05 | −.06 | −.05 | −.04 | .07 | −.00 | −.09* |
| Norms | ||||||||
| Descriptive norm (gen. pop.) | .05 | .03 | .05 | .01 | .01 | .03 | −.02 | .04 |
| Descriptive norm (race) | .14** | .08 | .03 | .04 | .08 | .02 | .02 | .03 |
| Subjective norm | .10* | .09* | −.03 | −.02 | .04 | .07 | .00 | −.05 |
| Moral norm | .11 | .14*** | −.04 | .08* | −.11* | .02 | .18** | .04 |
| Injunctive norm | .00 | −.02 | −.11* | .02 | −.02 | .02 | .03 | −.07* |
Note.
p<.05;
p<.01;
p<.001.
AA = African American; W = White.
Based on the magnitudes of the coefficients, racial consciousness in a health care setting emerged as a more powerful influence for African Americans, with higher scores on racial consciousness associated with lower trust in the vaccine (−.17) and the vaccine process (−.21), higher perceived vaccine risk (.14), greater use of naturalism (.21), a less positive attitude toward the flu vaccine (−.12), more belief in conspiracies (.28), less knowledge of flu vaccine (−.17), greater vaccine hesitancy (.17) and perception of barriers (.14), less confidence in the flu vaccine (−.16), and a lower injunctive norm, which relates to workplace expectation of getting the flu vaccine (−.11). The effect of racial consciousness on the moral norm was statistically significant for Whites only (.08), although the difference between the coefficients for the two groups was very small. Frequency of discrimination positively affected disease risk (.11) and vaccine risk perception (.18), conspiracy theory (.12), and negatively affected the perception of a moral norm (−.11) for African Americans only. Impact of discrimination had a statistically significant effect for African Americans on moral norms (.18), while its effects on vaccine risk (.14), naturalism (.28), confidence in one’s vaccine decision (−.09), and injunctive norms (−.07) were significant only for the Whites. Higher impact of discrimination appeared to increase flu vaccine hesitancy for both groups, but had different effects on knowledge of flu vaccine (i.e., increasing knowledge for African Americans and decreasing for Whites).
Our third research question examined whether racial factors affected vaccine behaviors and specifically, how vaccine attitudes and knowledge mediated that relation. Table 5, which depicts standardized direct and indirect effects between racial factors and vaccine behavior as mediated by vaccine attitudes and knowledge, shows that for both groups, all direct effects were not significant as were most indirect effects. Exceptions, all relatively small in magnitude, include the effect of racial fairness as mediated by trust in the flu vaccine for African Americans only (i.e., higher racial fairness increased trust in the vaccine process and thus the probability of getting a flu vaccine, .04). For Whites, the effect of racial fairness was mediated by confidence in the flu vaccine (i.e., higher racial fairness was associated with higher confidence in the flu vaccine, which was further associated with a lower probability of getting vaccinated, −.03). However, the association with lower probability of vaccination was very slightly negative (−0.004 with p = 0.958), which is likely due to random fluctuation. For African Americans, the effect of racial consciousness on flu vaccine behavior was significantly mediated by perceived vaccine risk (i.e., higher racial consciousness increased the perception of vaccine risk, which in turn decreased the chance of getting the flu vaccine, −.02) and by flu vaccine knowledge (i.e., higher racial consciousness was associated with lower flu vaccine knowledge, which was associated with lower probability of getting a flu vaccine, −.03). Finally, for African Americans, the effect of frequency of discrimination was significantly mediated by perceived vaccine risk (i.e., the higher the perception of discrimination the higher his perceived vaccine risk, and in turn the lower the probability of getting the flu vaccine, −.03).
Table 5.
Standardized Direct and Indirect Effects of Racial Factors on Influenza Vaccine Behavior
| Fairness | Consciousness | Frequency | Impact | |||||
|---|---|---|---|---|---|---|---|---|
| AA | W | AA | W | AA | W | AA | W | |
| Direct effect | −.05 | −.01 | −.01 | .01 | .06 | .02 | −.04 | −.03 |
| Indirect effect via… | ||||||||
| Trust and risk perception | ||||||||
| Trust in flu vaccine | .04* | .00 | −.03 | −.00 | −.01 | .00 | .01 | .00 |
| Trust in vaccine process | .01 | −.02 | −.01 | .00 | −.00 | .00 | .00 | .00 |
| Risk of disease | .01 | .02 | −.01 | −.00 | .03 | .01 | .02 | .01 |
| Risk of vaccine | .02 | .02 | −.02* | −.00 | −.03* | −.00 | .01 | −.03 |
| Attitudes and beliefs | ||||||||
| Naturalism | .00 | .01 | −.01 | .00 | −.00 | .00 | −.00 | −.02 |
| Flu vaccine attitude | .01 | .01 | −.01 | −.00 | −.00 | .00 | .00 | −.01 |
| Conspiracy | −.01 | .00 | .02 | −.00 | .01 | −.00 | .00 | −.00 |
| Knowledge | ||||||||
| General knowledge | −.00 | .00 | .00 | −.00 | .00 | .00 | −.00 | .00 |
| Specific knowledge | .00 | −.01 | −.03** | .00 | −.02 | .00 | .02 | .00 |
| Vaccine hesitancy and confidence | ||||||||
| General vaccine hesitancy | .00 | −.01 | −.00 | .00 | .00 | .00 | −.00 | .00 |
| Flu vaccine hesitancy | −.00 | .00 | .00 | .00 | .00 | .00 | −.00 | .00 |
| Barriers | −.00 | .02 | .00 | −.01 | .00 | −.00 | .00 | −.00 |
| Confidence in flu vaccine | −.00 | −.03* | .00 | .01 | .00 | −.00 | .00 | .00 |
| Confidence in vac. decision | .00 | .02 | −.02 | −.02 | −.01 | .03 | −.00 | −.04 |
| Norms | ||||||||
| Descriptive norm (gen. pop.) | .00 | −.00 | .00 | −.00 | .00 | −.00 | −.00 | −.00 |
| Descriptive norm (race) | −.00 | .01 | .00 | .00 | −.00 | .00 | .00 | .00 |
| Subjective norm | .01 | .01 | −.00 | −.00 | .01 | .01 | .00 | −.01 |
| Moral norm | −.00 | .00 | .00 | .00 | .00 | .00 | −.00 | .00 |
| Injunctive norm | .00 | −.04 | −.01 | .01 | −.00 | .01 | .00 | −.02 |
Note.
p<.05;
p<.01.
AA = African American; W = White.
Discussion
Our effort to explore concepts of racial fairness, racial consciousness in a health care setting, and the frequency and impact of discrimination grew from significant differences between African Americans and Whites in our qualitative research. The measures for racial fairness and racial consciousness specifically arose from distinctly different perspectives in which we heard White respondents responding to our queries from what we came to see as a place of White privilege. Specifically, we mean that they were far less likely to question vaccines or their interactions with health care providers. For African Americans overall, they brought a higher degree of skepticism and concern about the flu vaccine and the process, and referenced the infamous Tuskegee Syphilis Study as one rationale for their concern. Indeed, our survey results validate that racial factors are more relevant for African Americans than Whites.
Our first research question used novel measures to explore vaccine attitudes and knowledge. Not surprisingly, Whites had higher trust in the vaccine, the vaccine process, and when coupled with their higher level of perceived disease risk and lower risk of the vaccine, resulted in greater vaccine acceptance. On our descriptive norm, the perspectives of both groups mirrored one another. Whites believed that greater proportions of their race get vaccinated compared to the general population; African Americans believed higher proportions of the general population were vaccinated, with lower vaccination rates among their own race. These perceptions reflect national data that documents the racial disparity. African Americans and Whites differed significantly on the subjective norm in a manner consistent with each group’s attitudes and beliefs. African Americans were more likely to report barriers to vaccination, were more hesitant about vaccines in general and the flu vaccine specifically, more likely to believe in conspiracy theories and use naturalism as an alternative to getting vaccinated. Although some of these results are confirmed in other studies [7, 23], no other study is as comprehensive in measuring so many of these factors. Our exploration of naturalism and conspiracy theories are not typically measured, and thus far, most research on vaccine hesitancy and confidence has focused on childhood, not adult vaccination.
In our second question, we explored new racial factors to seek to understand what, if any, impact these factors have on vaccine attitudes and knowledge. Interestingly, racial fairness has a significant impact on multiple positive attitudes and beliefs about the flu vaccine for both racial groups. Not surprisingly, the influence of racial consciousness in a health care setting was most powerful for African Americans with higher levels of racial consciousness associated with important factors that affect vaccine acceptance. Although the frequency and impact of discrimination influenced the two racial groups differently on several variables, discrimination is associated with increasing vaccine hesitancy in both groups. Surprisingly, discrimination was associated with contrasting levels of knowledge, increasing knowledge for African Americans and decreasing knowledge for Whites. Racial fairness seems to have the most powerful association for both races, suggesting perceived unfair treatment by a health care professional can discourage vaccination while efforts to enhance the sense of fairness and respect in a health care setting can yield a positive impact on variables that enhance vaccination acceptance.
For our third question exploring the effects of racial factors on vaccine behavior as mediated by vaccine knowledge and attitudes, we found limited direct and indirect effects. Not surprisingly, the effect of racial variables was more evident with our African American sample. Higher perceptions of fairness mediated greater trust in the vaccine, contributing to greater vaccination. For African Americans, racial consciousness in a health care setting and perceived discrimination emerged as important influences on key issues such as perceived vaccine risk, lower knowledge and reduced likelihood of vaccine acceptance. Although the effect sizes were not substantial, this suggests that these racial factors may work through attitudes and knowledge, without a direct effect on behavior. However, we uncovered some important results that will warrant further exploration. Additionally, because these racial factors are novel concepts, further research in order to refine their measurement is warranted. To our knowledge, no other research has attempted to measure the impact of racial factors on vaccine knowledge and attitudes for any racial/ethnic group.
Exploring racial factors in the context of vaccine disparities is a novel area of inquiry that may offer insights for training of health care professionals to serve racially diverse patients. Additionally, our study suggests that a deeper consideration of how race and racism affect African Americans and Whites could facilitate more effective tailored and targeted health communication for African Americans in particular. While our research was targeted to influenza vaccine disparities between African Americans and Whites, these methods could be adapted to other racial/ethnic groups with suboptimal influenza vaccination rates such as Hispanics [2]. Our study provides an innovative look at factors that may underlie disparities in vaccine acceptance, and with further research to understand how racial factors affect flu vaccine attitudes and behavior, can ultimately contribute to reducing such disparities.
Contributor Information
Sandra Crouse Quinn, Professor, Department of Family Science, School of Public Health, University of Maryland, 4200 Valley Drive, College Park, MD.
Amelia Jamison, University of Maryland
Vicki S. Freimuth, University of Georgia
Ji An, University of Maryland
Gregory R. Hancock, University of Maryland
Don Musa, University of Pittsburgh
References
- 1.Lu P-J, O’Halloran A, Bryan L, Kennedy ED, Ding H, Graitcer SB, et al. Trends in racial/ethnic disparities in influenza vaccination coverage among adults during the 2007–08 through 2011–12 seasons. American Journal of Infection Control. 2014;42:763–9. doi: 10.1016/j.ajic.2014.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Flu Vaccination Coverage, United States, 2015-16 Influenza Season. 2016 Accessed from: http://www.cdc.gov/flu/fluvaxview/coverage-1516estimates.htm. Accessed November 18, 2016.
- 3.Logan JL. Disparities in influenza immunization among US adults. Journal of the National Medical Association. 2009;101:161. doi: 10.1016/S0027-9684(15)30830-0. [DOI] [PubMed] [Google Scholar]
- 4.Maurer J, Harris KM, Uscher-Pines L. Can routine offering of influenza vaccination in office-based settings reduce racial and ethnic disparities in adult influenza vaccination? Journal of General Internal Medicine. 2014;29:1624–30. doi: 10.1007/s11606-014-2965-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Groom HC, Zhang F, Fisher AK, Wortley PM. Differences in adult influenza vaccine-seeking behavior: the roles of race and attitudes. Journal of Public Health Management and Practice. 2014;20:246–50. doi: 10.1016/j.vaccine.2012.08.036. [DOI] [PubMed] [Google Scholar]
- 6.Wooten KG, Wortley PM, Singleton JA, Euler GL. Perceptions matter: Beliefs about influenza vaccine and vaccination behavior among elderly white, black and Hispanic Americans. Vaccine. 2012;30:6927–34. doi: 10.1016/j.vaccine.2012.08.036. 0.1016/j.vaccine.2012.08.036. [DOI] [PubMed] [Google Scholar]
- 7.Chen J, Fox S, Cantrell C, Stockdale S, Kagawa-Singer M. Health Disparities And Prevention: Racial/ethnic Barriers To Flu Vaccinations. Journal of Community Health. 2007;32:5–20. doi: 10.1007/s10900-006-9031-7. [DOI] [PubMed] [Google Scholar]
- 8.Santibanez TA, Kennedy ED. Reasons given for not receiving an influenza vaccination, 2011–12 influenza season, United States. Vaccine. 2016;34:2671–8. doi: 10.1016/j.vaccine.2016.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ojha RP, Stallings-Smith S, Flynn PM, Adderson EE, Offutt-Powell TN, Gaur AH. The Impact of Vaccine Concerns on Racial/Ethnic Disparities in Influenza Vaccine Uptake Among Health Care Workers. American Journal of Public Health. 2015;105:e35–e41. doi: 10.2105/AJPH.2015.302736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar S, Quinn SC, Kim KH, Musa D, Hilyard KM, Freimuth VS. The social ecological model as a framework for determinants of 2009 H1N1 influenza vaccine uptake in the United States. Health Education & Behavior. 2012;39:229–43. doi: 10.1177/1090198111415105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dressler WW, Oths KS, Gravlee CC. Race and ethnicity in public health research: models to explain health disparities. Annual Review of Anthropology. 2005;34:231. doi: 10.1146/annurev.anthro.34.081804.120505. [DOI] [Google Scholar]
- 12.Ford CL, Airhihenbuwa CO. Critical race theory, race equity, and public health: toward antiracism praxis. American Journal of Public Health. 2010;100:S30–S5. doi: 10.2105/AJPH.2009.171058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thomas SB, Quinn SC, Butler J, Fryer CS, Garza MA. Toward a fourth generation of disparities research to achieve health equity. Annual Review of Public Health. 2011;32:399. doi: 10.1146/annurev-publhealth-031210-101136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones CP, Truman BI, Elam-Evans LD, Jones CA, Jones CY, Jiles R, et al. Using “socially assigned race” to probe white advantages in health status. Ethnicity & Disease. 2008;18:496. Accessed from: http://ww.ishib.org/journal/18-4/ethn-18-04-496.pdf. Accessed: November 30, 2016. [PubMed] [Google Scholar]
- 15.Jones CP. Invited Commentary: “Race,” Racism, and the Practice of Epidemiology. American Journal of Epidemiology. 2001;154:299–304. doi: 10.1093/aje/154.4.299. [DOI] [PubMed] [Google Scholar]
- 16.Williams DR, Mohammed SA. Racism and health I: Pathways and scientific evidence. American Behavioral Scientist. 2013 doi: 10.1177/0002764213487340. 0002764213487340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krieger N. Does racism harm health? Did child abuse exist before 1962? On explicit questions, critical science, and current controversies: an ecosocial perspective. American Journal of Public Health. 2003;93:194–9. doi: 10.2105/AJPH.93.2.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Musa D, Schulz R, Harris R, Silverman M, Thomas SB. Trust in the health care system and the use of preventive health services by older black and white adults. American Journal of Public Health. 2009;99:1293–9. doi: 10.2105/AJPH.2007.123927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Trivedi AN, Ayanian JZ. Perceived discrimination and use of preventive health services. Journal of General Internal Medicine. 2006;21:553–8. doi: 10.1111/j.1525-1497.2006.00413.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MacIntosh T, Desai MM, Lewis TT, Jones BA, Nunez-Smith M. Socially-assigned race, healthcare discrimination and preventive healthcare services. PloS one. 2013;8:e64522. doi: 10.1371/journal.pone.0064522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bleser WK, Miranda PY, Jean-Jacques M. Racial/Ethnic Disparities in Influenza Vaccination of Chronically Ill US Adults: The Mediating Role of Perceived Discrimination in Health Care. Medical Care. 2016;54:570–7. doi: 10.1097/MLR.0000000000000544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quinn SC, Kumar S, Freimuth VS, Kidwell K, Musa D. Public willingness to take a vaccine or drug under Emergency Use Authorization during the 2009 H1N1 pandemic. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science. 2009;7:275–90. doi: 10.1089/bsp.2009.0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lindley MC, Wortley PM, Winston CA, Bardenheier BH. The Role of Attitudes in Understanding Disparities in Adult Influenza Vaccination. American Journal of Preventive Medicine. 2006;31:281–5. doi: 10.1016/j.amepre.2006.06.025. [DOI] [PubMed] [Google Scholar]


