Abstract
Metastasis to the sublingual lymph nodes is very rare in oral cavity cancers. We present an early-stage floor of the mouth (FOM) cancer case with metastasis to the sublingual lymph node. Even though the rate of metastatic sublingual lymph nodes is low, the uncommon presence of sublingual lymph node metastasis in an early-stage FOM cancer case raises the question of routine FOM dissection. Further anatomic and pathologic studies addressing the rate and pattern of sublingual lymph node metastasis are warranted.
Keywords: Floor of the mouth carcinoma, squamous cell carcinoma, sublingual region, lymph node metastasis
Introduction
Floor of the mouth (FOM) is the third most common site for oral cavity cancers (1). Lesions in the anterior FOM may invade the sublingual gland or submandibular duct and thus may require continuous resection with the primary tumor. Most common sites for cervical metastasis are the submandibular nodes followed by upper jugular and submental nodes for oral cavity carcinomas (1, 2). Early-stage FOM lesions are managed with transoral resection, whereas more extensive forms may require further surgical resections including the tongue or mandible (2). The neck is usually managed with elective neck dissection if there is no evident lymph node metastasis. In-continuity resection of the oral cavity lesions has been a topic of debate because of morbidity and oncologic reasons (3). Metastasis to the sublingual lymph nodes is very rare in oral cavity cancers. In this study, we present an early-stage FOM cancer case with metastasis to the sublingual lymph nodes.
Case Presentation
A 57-year-old male patient presented with a nonhealing ulcer located in the FOM. The symptoms had a duration of seven months and the histopathological diagnosis was moderately differentiated squamous cell carcinoma (SCC). There were no lymphatic metastases in the magnetic resonance imaging or computed tomography scans (Figure 1). The preoperative clinical and radiologic staging was T1N0M0. The patient was operated under general anesthesia. The primary tumor was resected transorally, and both of the sublingual glands were resected in-continuity with the primary. Tumor-free surgical margins were confirmed with frozen sections. Bilateral selective neck dissection was performed at the same time. Neck levels I–II–III–IV were dissected in both necks. The mucosal defect was reconstructed with a full-thickness skin graft. Histopathologic examination was reported as moderately differentiated SCC (greatest diameter 1 cm). The tumor had an infiltrative macroscopic growth pattern, and there was no lymphatic, vascular, or perineural invasion. There were no metastatic lymph nodes in the neck specimens; however, one of the two lymph nodes harbored metastasis in the sublingual region. The metastatic lymph node had no extracapsular extension. The patient received postoperative adjuvant radiotherapy for lymph node metastasis. The patient was disease free at the twelfth-month follow-up visit. Informed consent was obtained from the patient.
Figure 1.
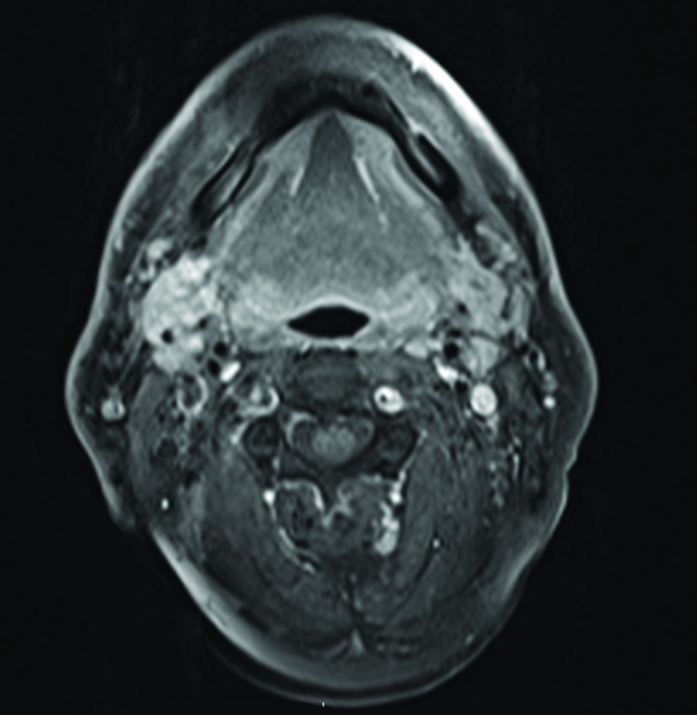
Axial MRI scan of the floor of mouth. No enlarged lymph nodes are visible
Discussion
Oral cavity cancers tend to metastasize to the levels I–III, thus supraomohyoid neck dissection is the usual procedure carried out for elective neck dissection (4). The presence of lymph nodes along the FOM was first reported by Rouviere in 1938 as median and lateral lingual lymph nodes (5). Nowadays these lymph nodes are more commonly named as sublingual lymph nodes, however both definitions are correct. Few reports of lingual lymph node metastasis exist in the medical literature. First, Ozeki et al. (6) reported three cases of carcinoma of the tongue with metastasis to the lingual lymph nodes in 1985. This report was followed by one case of oral tongue SCC with lateral lingual node metastasis in 2002 by Dutton et al. (3) and one case of oral tongue SCC with lingual lymph node metastasis in 2008 by Han et al. (7). Woolgar (8) reviewed 326 neck dissections of 253 patients with intraoral/oropharyngeal SCC. He reported two positive median lingual nodes in 60 lateral tongue tumors and a positive median lingual node and two positive lateral lingual nodes in 39 tongue ventral tumors (8). Zhang et al. (9) reported two cases of early tongue cancer with sublingual lymph nodes metastasis. Umeda et al. (10) reported two FOM SCC cases with lingual lymph node metastasis (10).
In-continuity resection carries greater morbidity and a higher risk for fistula formation in oral cavity cancers. However, it should also be noted that the sublingual glands and sublingual region are continuous with the submandibular region. For this reason, the lymph node-bearing soft tissue of the FOM could be postulated as a single unit. Additionally, most of the advanced-stage FOM cancers require pull-through procedures, thus the FOM is resected in-continuity with the neck lymphatics. Woolgar (8) suggests that pull-through resection offers the best chance of cancer ablation because it is likely that some of the intraoral recurrences are related to the remaining lingual lymph nodes during standard neck dissection. Leemans et al. (11) analyzed and compared 27 patients who underwent 28 discontinuous dissections and 34 patients who underwent 40 in-continuity dissections for T2 anterior tongue or FOM carcinoma. They reported that 5-year survival was lower in the discontinuous dissection group, and they did not recommend discontinuous neck dissection in oral cancer. On the contrary, Tesseroli et al. (12) reported that discontinuous neck dissection seems not to change the disease-free or disease-specific survival when compared to in-continuity neck dissection. However, they concluded that a prospective randomized trial was necessary to confirm the results.
Tumor features and their relation to sublingual lymph node metastasis are not clearly defined; however, this relation is better defined in oral tongue cancer. Zhang et al. (9) reported that both of their cases with sublingual lymph node metastasis had deeply endophytic lesions located in the ventral tongue.
The frequency of metastasis to the sublingual lymph nodes is rare in oral cavity cancers, and this case is the second reported FOM cancer case with a metastasis to the sublingual lymph nodes. Because sublingual lymph nodes are located above the mylohyoid muscle, they are not removed during routine discontinuous neck dissection. The sublingual lymph nodes can be removed with the sublingual glands with little morbidity and in case of metastasis, postoperative adjuvant therapy is necessary as sublingual metastasis is considered as a regional lymph node metastasis to improve survival.
Conclusion
Even though the rate of metastatic sublingual lymph nodes is low, the presence of a sublingual lymph node metastasis in an early-stage FOM cancer case raises the question of routine FOM dissection. Further anatomic and pathologic studies addressing the rate and pattern of sublingual lymph node metastasis are warranted.
Footnotes
Informed Consent: Written informed consent was obtained from patient who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - K.Ö., İ.K.; Design - İ.K., G.T.; Supervision - K.Ö., İ.K.; Resource - İ.K., G.T.; Materials - K.Ö., İ.K., G.T.; Data Collection and/or Processing - G.T.; Analysis and/or Interpretation - K.Ö., İ.K., G.T.; Literature Search - K.Ö., G.T.; Writing - G.T.; Critical Reviews - K.Ö., İ.K.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Gonzales D, Robbins KT. Carcinoma of the Oral Cavity, Pharynx, and Esophagus. In: Chan Y, Goddard JC, editors. KJ Lee’s Essentieal Otolaryngology. 11th ed. McGraw-Hill; 2016. pp. 701–26. [Google Scholar]
- 2.Wein RO, Weber RS. Malignant Neoplasms of the Oral Cavity. In: Flint PW, Haughey BH, Robbins KT, Thomas JR, Niparko JK, Lund VJ, Lesperance MM, editors. Cummings Otolaryngology Head and Neck Surgery. 6th ed. Philadelphia, PA: Elsevier Saunders; 2015. pp. 1359–87. [Google Scholar]
- 3.Dutton JM, Graham SM, Hoffman HT. Metastatic cancer to the floor of mouth: the lingual lymph nodes. Head Neck. 2002;24:401–5. doi: 10.1002/hed.10026. https://doi.org/10.1002/hed.10026. [DOI] [PubMed] [Google Scholar]
- 4.Ferlito A, Silver CE, Rinaldo A. Elective management of the neck in oral cavity squamous carcinoma: current concepts supported by prospective studies. Br J Oral Maxillofac Surg. 2009;47:5–9. doi: 10.1016/j.bjoms.2008.06.001. https://doi.org/10.1016/j.bjoms.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 5.Rouviere H. Lymphatics of the tongue and of the salivary glands. In: Tobies MJ, translator. Anatomy of the Human Lymphatic System. Ann Arbor, MI: Edwards Brother, Inc.; 1938. p. 44. [Google Scholar]
- 6.Ozeki S, Tashiro H, Okamoto M, Matsushima T. Metastasis to the lingual lymph node in carcinoma of the tongue. J Maxillofac Surg. 1985;13:277–81. doi: 10.1016/s0301-0503(85)80064-3. https://doi.org/10.1016/S0301-0503(85)80064-3. [DOI] [PubMed] [Google Scholar]
- 7.Han W, Yang X, Huang X, Hu Q, Wang Z. Metastases to lingual lymph nodes from squamous cell carcinoma of the tongue. Br J Oral Maxillofac Surg. 2008;46:376–8. doi: 10.1016/j.bjoms.2007.12.002. https://doi.org/10.1016/j.bjoms.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 8.Woolgar JA. Histological distribution of cervical lymph nodes from intraoral/oropharyngeal squamous cell carcinomas. Br J Oral Maxillofac Surg. 1999;37:175–80. doi: 10.1054/bjom.1999.0036. https://doi.org/10.1054/bjom.1999.0036. [DOI] [PubMed] [Google Scholar]
- 9.Zhang T, Ord RA, Wei WI, Zhao J. Sublingual lymph node metastasis of early tongue cancer: report of two cases and review of the literature. Int J Oral Maxillofac Surg. 2011;40:597–600. doi: 10.1016/j.ijom.2010.12.009. https://doi.org/10.1016/j.ijom.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 10.Umeda M, Minamikawa T, Shigeta T, Oguni A, Kataoka T, Takahashi H, et al. Metastasis to the lingual lymph node in patients with squamous cell carcinoma of the floor of the mouth: a report of two cases. Kobe J Med Sci. 2010;55:67–72. [PubMed] [Google Scholar]
- 11.Leemans CR, Tiwari R, Nauta JJ, Snow GB. Discontinuous vs in-continuity neck dissection in carcinoma of the oral cavity. Arch Otolaryngol Head Neck Surg. 1991;117:1003–6. doi: 10.1001/archotol.1991.01870210075014. https://doi.org/10.1001/archotol.1991.01870210075014. [DOI] [PubMed] [Google Scholar]
- 12.Tesseroli MA, Calabrese L, Carvalho AL, Kowalski LP, Chiesa F. Discontinuous vs. in-continuity neck dissection in carcinoma of the oral cavity. Experience of two oncologic hospitals. Acta Otorhinolaryngol Ital. 2006;26:350–5. [PMC free article] [PubMed] [Google Scholar]


