Abstract
Background
Visceral leishmaniasis (VL) caused by Leishmania infantum became a disease of urban areas in Brazil in the last 30 years and there has been an increase in asymptomatic L. infantum infection with these areas.
Methodology/Principal findings
A retrospective study of human VL was performed in the state of Rio Grande do Norte, Brazil, for the period of 1990–2014. The data were divided into five-time periods. For all VL cases, data on sex, age, nutritional status and childhood vaccination were collected. Geographic information system tools and statistical models were used to analyze the dispersion of human VL. The mean annual incidence of VL was 4.6 cases/100,000 inhabitants, with total 3,252 cases reported. The lethality rate was 6.4%. Over time the annual incidence of VL decreased in the 0–4 years (p<0.0001) and 5–9 (p <0.0001) age groups, but increased in ages 20–39 (p<0.001) and >40 years (p<0.0001). VL occurred more often in males (β2 = 2.5; p<0.0001). The decreased incidence of VL in children was associated with improved nutritional status and childhood immunizations including measles, poliomyelitis, BCG, and hepatitis B. Human VL correlated temporally and geographically with canine L. infantum infection (p = 0.002, R2 = 0.438), with rainfall and with Lutzomyia longipalpis density (r = 0.762). Overall, the incidence of VL decreased, while VL-AIDS increased, especially between 2010–2014. VL was more frequently found in areas that lacked urban infrastructure, detected by lack of garbage collection and sewers, whereas HIV infection was associated with higher levels of schooling and evidence of higher socioeconomic status.
Conclusion/Significance
The demographics of VL in northeastern Brazil have changed. Disease incidence has decreased in children and increased in adults. They were associated with improvements in nutrition, socioeconomic status and immunization rates. Concurrent VL-AIDS poses a serious challenge for the future.
Author summary
We studied factors associated with the changing demographics of visceral leishmaniasis (VL) in Northeast Brazil, including environmental and socioeconomic determinants of disease, during the period 1990 to 2014. The incidence of VL was higher in urban areas, and regions with higher levels of canine L. infantum infection. Human males were more commonly affected than females. The incidence of VL in children under age 10 decreased during the period of study, simultaneous with increased incidence in adults. Reduction in the VL incidence among children was associated with improved socioeconomic status, administration of childhood vaccines and better nutritional status. Geographic areas with higher rainfall had higher densities of Lu. longipalpis, the primary vector of L. infantum in Brazil. VL was more frequently found in areas with indicators of poverty including sparse garbage collection and lack of urban infrastructure. During the past 25 years, HIV/AIDS has spread to areas where VL is endemic and has contributed to an increased incidence of VL-AIDS co-infection in adults.
Introduction
Visceral leishmaniasis (VL) is a life-threatening disease caused by L. infantum [1], which was first recognized in Brazil in 1932 [2–4]. It is likely the parasite initially arrived in northeastern Brazil with people and/or dogs previously infected with L. infantum in southern Europe or North Africa [5;6]. Lu. longipalpis is a competent vector for L. infantum, and it is found in most countries in Latin America. Dogs are considered the major reservoirs of L. infantum. At first, cases of VL in Brazil occurred sporadically in semi-arid, rural areas of the northeast region. Most cases occurred in children under 10 years of age [7;8]. However, in the late 1980’s and early 1990’s, urban outbreaks occurred in large cities in the northeast and other regions of Brazil [9–12]. Massive migration of the population to urban regions, adaptation of Lu. longipalpis to peridomestic environments, and transport of L. infantum infected dogs to urban areas occurred during this period. The temporal occurrence of human VL has assumed a variable pattern that correlates with environmental forces including el Niño/la Niña [13;14], which influence rainfall and humidity and thus the density of sand flies.
Several studies in endemic areas of Brazil have shown that most people infected with L. infantum remain asymptomatic, if they are not immunosuppressed [15–19]. It is not clear whether people with VL or with asymptomatic L. infantum infection serve as reservoirs and contribute to the long-term maintenance of this pathogen in endemic areas. In the past, the ratio of symptomatic VL to asymptomatic L. infantum infection among children was approximately one in every six, and for adults the ratio was 1 in 18. Risk factors for developing symptomatic VL in children included malnutrition [20–22], neoplastic disorders [19;23] and viral co-infection [24]. Brazil has had freely available vaccination for all age groups since early 1980 and this has had a coverage of over 90% for routine child immunizations. This improved vaccination rate has led to decreased and/or elimination of some of the common and potentially fatal diseases of children. For instance, it is known that measles infection predisposes to opportunistic infection for years [25;26] and measles has been eliminated from Brazil for almost a decade, although there was an outbreak in 2013, which was contained [27;28].
HIV/AIDS is known to increase the risk of developing symptomatic, rather than asymptomatic VL [29–31]. HIV co-infection with VL was first noted to contribute to the increased incidence of VL in adults in Europe in the mid-1980’s [32]. VL/AIDS was recognized in Brazil in early 90’s [32–34]. Thus, a new epidemiological pattern of VL is emerging because of spread of HIV to all regions of the country. Subjects with VL-AIDS have an increased risk of VL relapse and death. The goal of the current study was to identify demographic, spatial and socioeconomic factors associated with VL in northeastern Brazil between 1990 and 2014, using VL cases reported in the state of Rio Grande do Norte. We assessed the geographic distribution of VL and its association with the spatial distribution of HIV/AIDS, and with socioeconomic factors that could influence the outcome of L. infantum infection. A better understanding of the epidemiological dynamics of L. infantum and HIV co-infections, and their determinants is essential to guide new health policies.
Methods
Study area
The study was conducted in the state of Rio Grande do Norte in northeastern Brazil. The state has an area of 52,811,126 square kilometers, with a population of 3,408,510, 77.8% of whom now live in urban areas. Most of the state has a semi-arid climate, with rainfall less than 800 mm per year and an average temperature of 27°C. A more humid climate is found along the east coast of the state, which borders the Atlantic Ocean, where the rainfall indices are greater than 1,400 mm per year. The state is grouped in 19 micro-regions (MR), each with distinct climate, topography, hydrography, population density and economy. These micro regions served as units for the current analysis.
Study design
A retrospective study of VL cases diagnosed in the state of Rio Grande do Norte was performed, and correlated with demographic and epidemiologic factors in the corresponding regions of the state. The study was divided into five time periods: (1) 1990–1994, (2) 1995–1999, (3) 2000–2004, (4) 2005–2009 and (5) 2010–2014. The association between spatial patterns of VL and HIV-AIDS was assessed using quantitative data available from 1991, 2000 and the 2010 censuses. The incidence of VL, AIDS and VL-AIDS co-infection per 100,000 inhabitants was extracted from the state records listed below. Additional variables that were collected included: (1) dates of new cases of VL, AIDS and VL-/AIDS, (2) sex, (3) age, (4) nutritional status of children under 5 years, (5) vaccination rates for measles, poliomyelitis, BCG and hepatitis B in children under 5 years. The spatial and temporal correlation between human VL and canine infection was also assessed. Environmental or socioeconomic variables considered were: (1) the association of annual rainfall and the density of Lu. longipalpis, (2) socioeconomic data from the censuses included literacy rate, education, income, city water supply, waste disposal, septic tank and presence of sewage.
Data collection
Data on human VL were obtained from the Notifiable Diseases Information System (SINAN). This federal government system catalogs the reported cases and coordinates investigations of diseases for which reporting is mandated by the Brazilian government, as defined by specific legislation. The data are captured in the Health Post Centers and/or hospitals and are sent to state Secretary of Health, whose office uploads the information in SINAN. The list of notifiable disease is updated as new outbreaks occur. For example, the recent epidemic of Zika virus infections led this virus to be added to the list of mandatory reportable diseases. Data on Lu. longipalpis density and rates of infection in domestic dogs were obtained from the Surveillance and Leishmaniasis Control Program, Secretary of Health. Data on HIV or AIDS were obtained by crossing information from SINAN with the Brazilian Mortality Information System database and release of medications for HIV. Nutritional data on children younger than 5 years were obtained from the Brazilian Minister of Health. Those data were available for all 19 micro-regions of the state of Rio Grande do Norte.
Data about immunization coverage were obtained from the Brazilian National Program of Immunization Information System. The vaccination coverage percentage was calculated per estimated population at the age group targeted to be vaccinated and the doses of vaccines administered in each municipality, and grouped into the 19 micro regions for this analysis.
Data variables gathered from censuses included education level, income, local health facility, piped water supply, garbage collection, street cleaning, sewer system, septic tank, urbanization and population density. Those data were collected from the Instituto Brasileiro de Geografia e Estatística (IBGE) website (http://www.ibge.gov.br/home/). Annual rainfall data in the municipalities were obtained from the State of Rio Grande do Norte Agricultural Research Company, EMPARN, (http://www.emparn.rn.gov.br/).
Statistical analysis
The effect of sex and micro-region (MR) on the temporal variation in the incidence VL from 1990 to 2014 were evaluated by a general linear model with categorical explanatory variables [35] according to the following formula: Yti = β0 + β1t + β2I(Sex) + θiMR(i|19) + error, (model 1) where the dependent variable was the incidence of VL (Yti) per 100,000 inhabitants, in the year t and in the micro-region i. The independent variables were the time (t) in years, the categorical variables were sex (1 if male) and micro-region (1–19) MR (i |19). The β1 coefficient measured the average annual increase in the incidence of VL, whereas β2 measured the differential incidence of VL between male and female. Micro-region 19 was considered the reference, since it was the site of the first VL outbreak in the state of Rio Grande do Norte. The micro-region parameter was considered when evaluating the existence of spatial aggregation. The temporal incidence of VL considering the patient's age was analyzed by linear regression using the following statistical model: Zt = β0 + β1t + error (model 2). The Zt is the rate of cases per 100,000 inhabitants in year t, and β1 is the slope of the adjusted line that defined the secular trend of the incidence of VL for the subsequent year. A rising trend in cases/unit of time unit was observed when β1>0, whereas a downward trend in case rates/time was observed when β1<0. The case rate over time was stationary if β1 = 0. The model was adjusted in each of the following age groups: 0–4 years, 5–9 years, 10–19 years; 20–39 years and ≥40 years. The incidence/time unit was calculated within each age group.
The impact of vaccination coverage on the incidence of VL
The impact of routine vaccination of the population, including vaccines for measles, poliomyelitis, BCG and hepatitis B, on the incidence of VL was analyzed in children under 5 years of age between 2000 and 2014. We evaluated these data for each micro-region. Vaccination rate data were superimposed on micro-region VL incidence data to determine whether vaccination coverage correlated with VL, particularly in children under age 5. We used an adjusted linear regression model as defined by the formula: Yti = β0 + β1t + β2Xti + θiMR(i|19) + error, (model 3). Similar to model 1, the independent variable Xti was the vaccination coverage in micro-region i during year t. Because they were strongly correlated, an analysis of principal components was made and the vaccination coverage was represented by the score of the first component.
The impact of nutritional status on the incidence of VL in children
The nutritional status was considered by the proportion pi of children whose weight for age was categorized as very low(p1), low(p2), appropriate(p3) and high(p4). From those, a Nutritional Status Index—NSI was built considering a weighted proportion with zero sum weights w = (-1, -1/3, 1/3, 1) defined by , ranging between -1 and 1. A value of NSI close to -1 point is a very low status while a value close to 1 point is a very high status. The influence of nutrition on VL development was assessed by a model similar to model 3, where Xti is NSIti. (Model 4).
Spatial relationships between canine and human VL, and between HIV and human VL
The relationship between the incidence of human VL with canine VL in micro-regions/time was performed by adjusting a simple linear regression model defined by the formula: Yt = β0 + β1Xt + error, (model 5). The dependent variable, Yt was set to log (rate human VL+ 0.5) in the year t in which there was canine examination, and the independent variable was Xt the corresponding level of canine infection (LCI). The level of canine infection was defined as a weighted proportion of infected dogs, using weights ranging from zero to 100 depending on the total number of dogs examined versus the number that had Leishmania infection, model 6, as follows:
The spatial dependence and the association between response variables was performed by modeling the distribution of human VL case events with the spatial distribution of canine VL and social predictive factors, by adjusting mixed autoregressive spatial linear models (Spatial Lag Model Autoregressive-SAR) that captured the self-spatial correlation through a single ρ parameter (rho) added to the regression model; this was chosen to model factors in the same test: i.e., temporal variation in VL, effect of sex, and geographic micro-region. The equation was expressed as: y = ρXy + XBeta + error, (Model 7), where y is incidence of VL per 100,000 inhabitants at micro-region level. ρ (rho) measures the spatial dependence the VL incidence, W is the weight matrix modeling the spatial structure, X is the matrix of predictor variables, β is the regression coefficient vector which evaluated the association between Y and X, and error represents the residuals. The log transformation was applied to normalize the response distribution. The same analytical approach was applied to the spatial distribution of HIV/AIDS. The predictor variable data (X) was collected in the censuses 2000 and 2010. All statistical models tested herein are shown in S1 Supporting Information.
Software used
We used Excel 2013 in the construction of the database, Statistica StatSoft version 7.0, in the estimation of linear models (Models 1 to 7) and Quantum GI version 2.12.e-Lyon (http://www.gnu.org.licenses) in the construction of maps and R System version 3.2.2 (https://www.r-project.org) for the mixed autoregressive linear models.
The source of base layers used to build the figures was found at http://censo2010.ibge.gov.br/resultados and https://mapas.ibge.gov.br/bases-e-referenciais/bases…/. The softwares used to build the maps were QGis version 2.12.e-Lyon (https://www.gnu.org/licenses/) and R System version 3.2.2 (https://www.r-project.org)
Ethical considerations
This study was reviewed and approved by the Universidade Federal do Rio Grande do Norte Ethical review board CAAE12584513.1.0000.5537. Data were anonymous records and exempted from signed consent.
Results
Incidence and spatial distributions of human VL and AIDS in the state of Rio Grande do Norte, Brazil
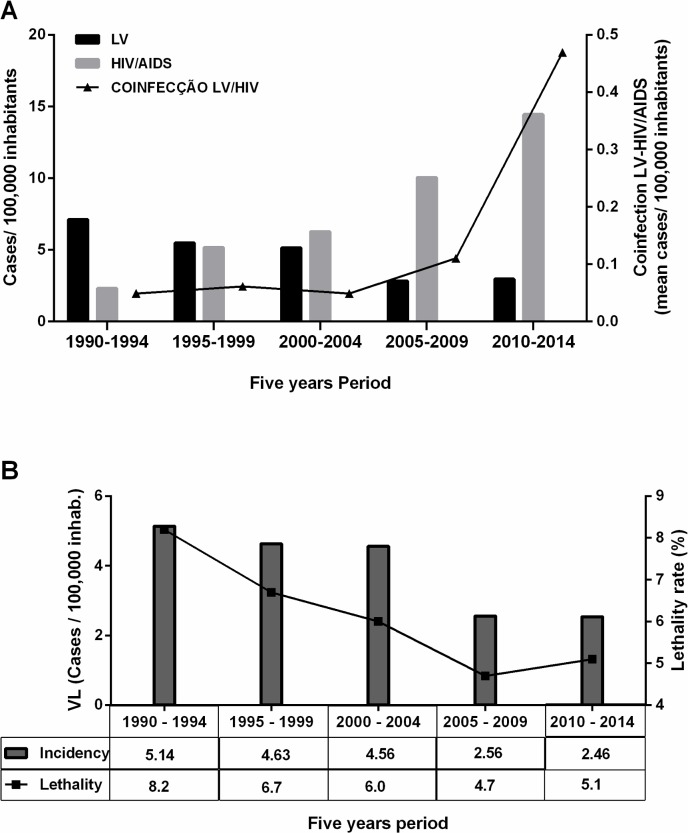
A total of 3,252 cases of VL were reported in the state of Rio Grande do Norte, northeast Brazil, between the years of 1990 and 2014. The mean annual incidence was 4.6 VL cases/100,000 inhabitants. Fig 1A shows the incidence of VL, AIDS and VL/AIDS by 5-year period. The overall VL lethality rate was 6.4%, with a total of 210 deaths (210/3,252). However, the highest lethality rate was 8.2% in the period 1990–1994 and was associated with the highest incidence of VL (Fig 1B).
Fig 1. Analysis of a 25-year time series of visceral leishmaniasis, VL/AIDS and HIV in the state of Rio Grande do Norte, Brazil.
A. Incidence of VL, AIDS, and VL-AIDS co-infections in Rio Grande do Norte 1990 to 2014. B. VL incidence by 100,000 inhabitants and the percent of VL lethality by five-year period.
There were 5,777 cases of AIDS with an average incidence of 8.1 cases/100,000 inhabitants (Fig 1A) between 1990 and 2014. During the study period, the average incidence of concurrent VL/AIDS was 0.16 per 100,000 inhabitants. However, on the 5th period (2010–2014) it reached 0.46/100,000 (Fig 1A).
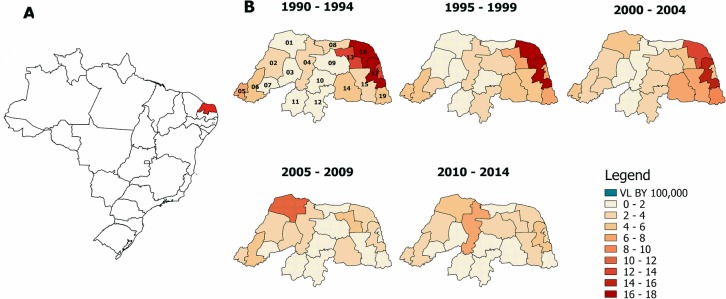
VL cases were predominantly found between 1990–1994 in the eastern coastal region of Rio Grande do Norte, but the disease subsequently spread to the Northeastern Coast (θ16 = 5.983; p<0.0001) and to other areas (θ17 = 6.256; p<0.0001, model 1), Table 1 and Fig 2. Although there has been an increase in areas reporting VL, there was a mean decrement of 0.135 VL cases/per year (β1 = -0.135, p<0.0001) (Table 1).
Table 1. Effect of time, sex and micro-region on the incidence of VL in accordance to model 1.
|
Predictors |
Estimates of parameters β e θ | Standard Error | P | Density mean Inhab./Km2 |
|---|---|---|---|---|
| Intercept (β0) | 275.597 | 45.517 | <0.0001 | - |
| Year (β1) | -0.135 | .023 | <0.0001 | - |
| [Sex = Male] (β2) | 2.498 | .328 | <0.0001 | - |
| Microrregions | ||||
| 1- Mossoró (θ1) | 0.427 | 1.011 | 0.673 | 340.8 |
| 2- Chapada do Apodi(θ2) | -2.405 | 1.011 | 0.018 | 85.4 |
| 3- MédioOeste(θ3) | -3.116 | 1.011 | 0.002 | 65.0 |
| 4- Vale do Açu(θ4) | -1.265 | 1.011 | 0.211 | 133.3 |
| 5- Serra de São Miguel(θ5) | 0.260 | 1.011 | 0.797 | 302.0 |
| 6- Pau dos Ferros(θ6) | -1.289 | 1.011 | 0.202 | 208.2 |
| 7 -Umarizal(θ7) | -2.743 | 1.011 | 0.007 | 196.9 |
| 8- Macau(θ8) | -3.197 | 1.011 | 0.002 | 124.9 |
| 9- Angicos(θ9) | -1.927 | 1.011 | 0.057 | 61.7 |
| 10 -Serra de Santana(θ10) | -3.417 | 1.011 | 0.001 | 97.5 |
| 11 –Seridó Ocidental(θ11) | -3.761 | 1.011 | 0.000 | 146.7 |
| 12 -Seridó Oriental(θ12) | -2.840 | 1.011 | 0.005 | 151.4 |
| 13 -Baixa Verde(θ13) | 1.608 | 1.011 | 0.112 | 149.1 |
| 14 –Borborema Potiguar(θ14) | -0.666 | 1.011 | 0.510 | 160.7 |
| 15- Agreste Potiguar(θ15) | -0.846 | 1.011 | 0.403 | 296.4 |
| 16—Northeastern littoral (θ16) | 5.983 | 1.011 | 0.000 | 145.5 |
| 17—Macaíba(θ17) | 6.256 | 1.011 | 0.000 | 586.4 |
| 18—Natal and perimetropolitan area (θ18) | 0.950 | 1.011 | 0.347 | 10202.9 |
Model (1): Yti = β0 + β1t + β2I(Sex) + θiMR(i|19) + error
Reference: 19 –South coast (Density 415.5)
Fig 2. The spread of visceral leishmaniasis by micro region in a 25-year period.
A. Map of Brazil showing in yellow the state of Rio Grande do Norte. Temporal and spatial distributions of human VL in the state of Rio Grande do Norte, 1990 to 2014, (cases/100,000 inhabitants).
Factors influencing human visceral leishmaniasis: Age, sex, nutrition, vaccination and canine visceral leishmaniasis
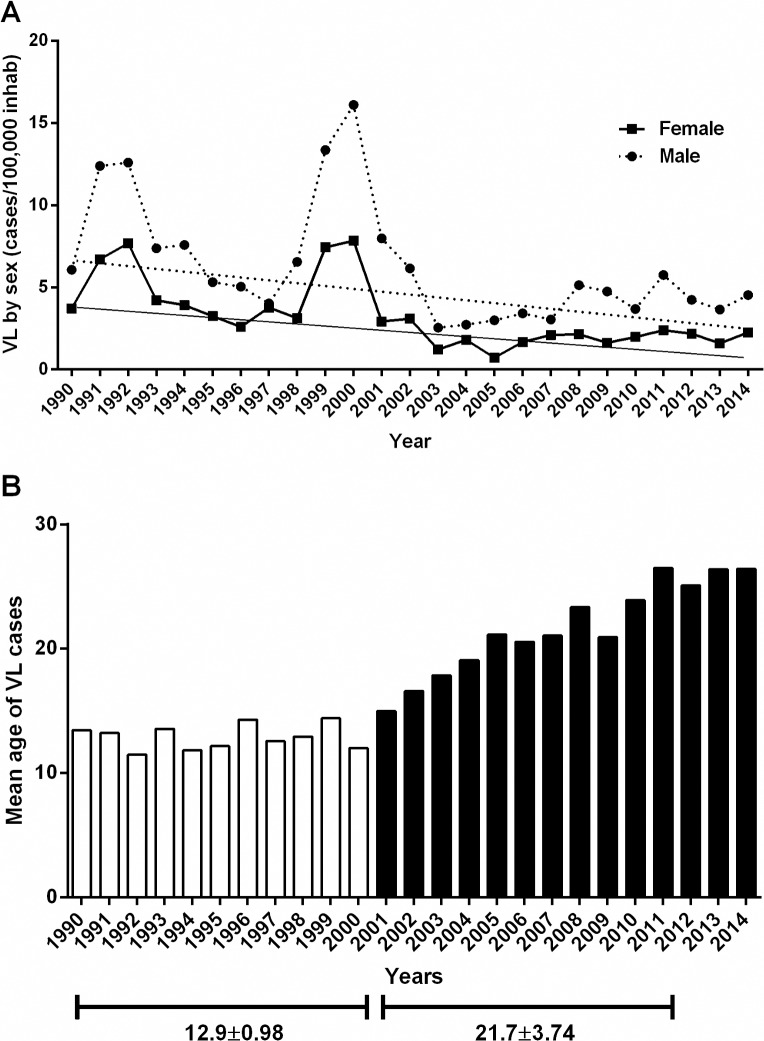
Over time there was a decreasing trend in the incidence of VL in both sexes. However, the male incidence was uniformly higher by approximately 2.5 per 100,000 (β2 = 2.498; p<0.0001), (Table 1; Fig 3A). There were two major peaks of VL, the first in 1991–1992 and the second in the 1999–2000 (Fig 3A).
Fig 3. Incidence of VL by sex and year.
A. The incidence was higher in males than females (Beta = 2.498, p<0.0001). B. Mean age of VL per year.
The temporal incidence of VL decreased significantly 0–4 and 5–9 among the age groups (β1 = -0.0117, p<0.0001 and β1 = -0.0042, p<0.0001, respectively) between 1990 and 2014, with significant increase in the 20–39 and >40 age groups (β1 = 0.0071, p<0.0001 and β1 = 0.0105, p<0.0001, respectively), Table 2. At the same time, the VL incidence was stationary in the 10–19 age group (β1 = -0.0016, p = 0.1320), (Table 2, Fig 3B). The mean age of VL increased linearly during the period of study, (age = (-1392.657) + 0.704 (year), p<0.001), with an annual increase of 0.704 years (8.4 months). The mean age of VL prior to 2000 was 12.9 ± 0.98 (SD) years, whereas from 2000 to 2014, the mean age was 21.7 ± 3.74 (SD) years (p<0.005), Fig 3B.
Table 2. Mean temporal variation of VL cases / 100,000 inhabitants according to the age group(*) (model 2).
| Age group (years) |
(intercept) | R2 | |||
|---|---|---|---|---|---|
| Estimate | p | Estimate | P | ||
| 0–4 | 0.5267 | <0.0001 | -0.0117 | <0.0001 | 0.6564 |
| 5–9 | 0.1829 | <0.0001 | -0.0042 | 0.0001 | 0.4740 |
| 10–19 | 0.1470 | <0.0001 | -0.0016 | 0.1320 | 0.0958 |
| 20–39 | 0.1385 | <0.0001 | 0.0071 | <0.0001 | 0.5636 |
| ≥40 | 0.0049 | 0.7400 | 0.0105 | <0.0001 | 0.8309 |
(*) Adjusting the model (2): Zt = β0 + β1t + errorineachagegroup
The adjustment of model 3 for spatial dispersion of VL showed that, by correcting for the effect of trends and differences between micro-regions, there was a strong negative association between the incidence of VL and the score of the vaccine coverage (β2 = -4.805; p = 0.0003). The score in year t and the micro-region i representing the vaccination coverage, at this time and place was calculated by Xti = 0.0989BCGti + 0.3993POLIOti + 0.3181MEASLESti + 0.3915HEPATITISti, obtained from the first principal component. This means that an increase in one unit in the vaccination coverage score was associated with a reduction of 4.8 in the incidence rate of VL in children younger than five years. There is a strong association between the two variables estimated by a third-degree polynomial relationship (Fig 4A).
Fig 4. Risk factors for visceral leishmaniasis.
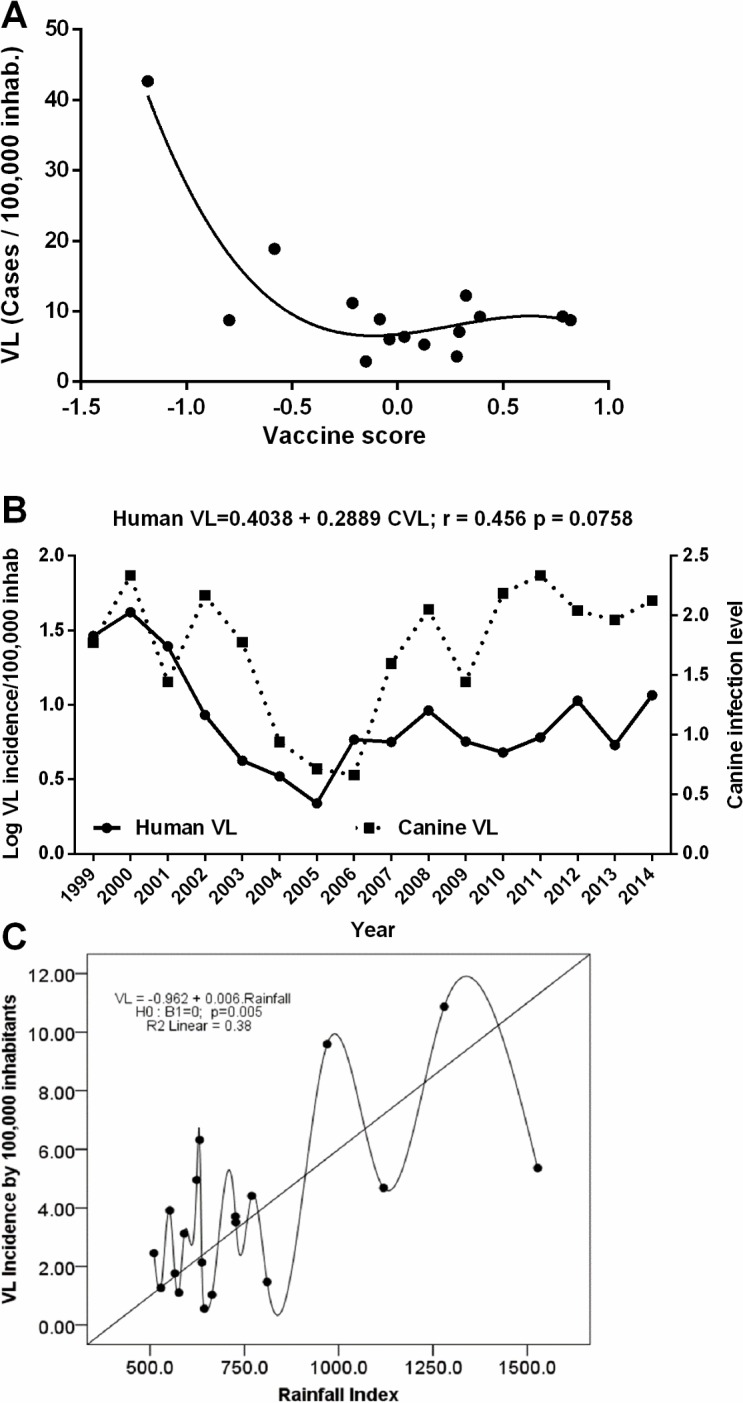
A. Association of Vaccination coverage with decreased the incidence of visceral leishmaniasis in children. Association between VL incidence(y) and vaccine coverage (x). y = 6.574 + 11.481x2 − 10.13x3, R2 = 0.82. B. Correlation between human VL and L. infantum infected dogs. C. Variation in rainfall index and its relation to the incidence of VL.
The association between the Nutritional Status Index-NSI and the incidence rate of VL in children less than 5 years was evaluated by adjusting for other parameters, models 3 and 4. There was a trend toward an inverse correlation between better nutritional status and VL in children, but this did not reach statistical significance, (β2 = -141.76; p = 0.1136). In contrast, there was a positive linear correlation between the incidence of human VL and canine VL (Human VL = 0.4038 + 0.2889LCI; r = 0.456, p = 0.0758), evaluated by the level of L. infantum canine infection (LCI) per models 5 and 6, as described in the methods session (Fig 4B). An increase of one LCI unit was associated with an increase in the incidence rate of human VL.
Environmental determinants of visceral leishmaniasis
There was a positive correlation between the density of sand flies and the rainfall index (r = 0.762, p<0.0001), according to model 5. In addition, an increase in annual rainfall index correlated with increased annual incidence of VL (r = 0.616, p = 0.005). The fluctuation in rainfall index explained 38% of the variation in the incidence of VL, with a100 mm increment in annual rainfall associated with an increase of 0.6 in VL/100,000 inhabitants (Fig 4C).
Socioeconomic determinants of human visceral leishmaniasis and HIV/AIDS
Among the socioeconomic variables that correlated with the incidence of VL was the percentage of households with garbage collection (β = -0.1684; p = 0.0116 in the 2000 census and β = -0.0341, p = 0.0153 in the 2010 census) and the percentage of households connected in the general water supply network (β = -0.3514; p = 0.100 in the 2010). In contrast, the incidence of AIDS correlated positively with garbage collection (β = 0.0358, p = 0.0005 in 2000 census and β = 0.0270, p = 0.0130 in the 2010 census), with higher sanitation level (β = 0.0407, p = 0.0007, in the 2000 census and β = 0.0418, p = 0.041in the 2010 census), with literacy rate (β = 0.0648, p = 0.0056 in 2010 census), with access to city water (β = 0.0431, p = <0.0001 in the 2000 census), adjusted model 7.
Discussion
Transmission of VL occurs in settings where the infected sand fly vector lives in proximity to a mammalian reservoir and susceptible humans [36], or through other means of transmission such as blood transfusion [37]. Despite efforts of health officials to interrupt the routes of transmission of L. infantum, VL continues to be a major health problem in Brazil after Malaria [38]. The demographics have changed substantially since VL was first reported in the 1930’s [2]. During early years, the disease occurred predominantly in rural areas of the Northeast region, with most cases of VL occurring in children younger than 10 years [7]. Mass migration of the population to urban areas beginning in the 1980s was accompanied by a change in the pattern of transmission to peri-urban regions of large cities in the Northeast and the southeast regions of the country [39].
The state of Rio Grande do Norte in northeastern Brazil, provides an example of the changing epidemiology of VL. There was a significant increase in the age at disease diagnosis, with an increase in adult VL. The disease decreased in children under age 10 years and increased in adults, mainly from period 3 of this study. The average age at diagnosis of VL in Rio Grande do Norte rose from 12.9 years prior to 2000 to 21.7 years in 2014 (Fig 3B). An increase in the average age of VL has also been observed in other Brazilian states [39;40]. Human VL has been associated with poverty and malnutrition in children [20–22;41]. We hypothesized that multiple socioeconomic factors might contribute to the significant reduction in childhood VL in the less than 10 age groups. Since 1999, social programs to decrease poverty and economic measures to control inflation have been successfully implemented in Brazil, with a coincident improvement in many measures of health [42]. Interventions have included supplementation of micronutrients, including iron and vitamin A in pregnant women and children aged 6–18 months, as well as fortification of wheat and corn flours with iron and vitamins [43]. There is an increase in vaccine coverage, with more uniform administration of vaccines as polio, measles, BCG and others. Those measures have been associated with increased average birth weight [22;44], decreased childhood diarrheal diseases [45;46]. The improved health could lead to healthier gut brush border, better absorption of nutrients and protection against opportunistic pathogens such as Leishmania. As an example, studies have shown that the vaccine-preventable disease measles can induce immunosuppression for years [26;47].
In previous studies in the state of Rio Grande do Norte, we found that children and adults were infected at comparable rates with L. infantum, as detected by positive anti-leishmanial serology and/or positive skin test response to Leishmania antigens [15]. Since a majority of L. infantum infections are asymptomatic, it is likely that the above-mentioned health interventions have resulted in enhanced development of protective Type 1 immune responses to Leishmania spp. and other pathogens, with a decreased likelihood that L. infantum infection will progress to VL in young children. In addition, improved socioeconomic status, improved living conditions, and expansion of urban regions may be responsible for decreased sand fly density and transmission in some areas.
In the current study males accounted for most VL cases (67%). Greater susceptibility of males to VL has also observed in other human studies [8,40] and in experimental models of Leishmania infection, hamster and murine models of VL [48]. Higher levels of testosterone have been associated with increased risk of VL caused by L. donovani in India and Sudan [49;50] possibly mediated by increased IL-10 production and down regulation of Th1 responses.
Domestic dogs are thought to be the primary reservoir of L. infantum in Brazil [51]. A correlation between human and canine VL was observed in the current study, and in reports from other areas in Brazil and Northern Africa [52–54]. Further studies are needed to better define the roles of dogs and asymptomatically infected humans as reservoirs for L. infantum in the epidemiology of VL in Brazil.
Higher rainfall indices correlated temporally and geographically with a higher incidence of human VL, especially in areas close to the Atlantic Ocean. An association between VL with increased rainfall has been reported in other regions of Brazil [55;56]. However, some cases of VL occurred in areas with lower humidity, higher temperatures and lower rainfall indices. It is likely that variations in the microenvironment provided niches in which sand flies were nonetheless able to thrive in proximity to humans and a dog reservoir.
HIV/AIDS occurred predominantly in males in the initial stage of the pandemic, although recently more women have become infected with HIV in Brazil [57]. The highest incidence of HIV/AIDS occurs in urban regions, coinciding with regions that have a higher incidence of VL. HIV/AIDS has been expanding throughout Brazil since 1990, and has now spread to all areas of Rio Grande do Norte. Coinfection with HIV and Leishmania spp. has contributed to the increased incidence of VL in adults in southern Europe in Spain, France, Italy and Portugal [31;58;59]. Consistently, in this report we document the presence of VL/AIDS in Rio Grande do Norte since 1990, but there was a considerable increase in coinfection in the third period (2000–2004), presumably because HIV infections spread to areas that were endemic for L. infantum infection. A large number of individuals are asymptomatically infected with L. infantum in the state of Rio Grande do Norte [15;17;60], and people with asymptomatic L. infantum and HIV seem to be at greater risk of developing VL and of death [61]. Therefore, it is imperative that strategies and guidelines be developed to prevent the development of VL during HIV infection. In summary, the demographics of VL in northeastern Brazil have changed substantially over the past 25 years. The incidence has decreased in children in association with improved nutrition, socioeconomic status, childhood immunizations, and overall health. In contrast, the incidence of VL in adults has increased. The latter could be explained in part by failure to develop immunity to the parasite as a child, and the geographic coincidence of HIV infection and VL. The emergence of concurrent VL-AIDS poses a serious health challenge for the future.
Supporting information
(DOCX)
(DOC)
Acknowledgments
We thank the State of Rio Grande do Norte Public Health Secretariat for making the records on visceral leishmaniasis available for our studies. We also thank Ms Tatiana Bernardo Pereira (State of RN Public Health Secretariat, DST/AIDS) for helping with information about AIDS and HIV.
Data Availability
All relevant data are within the paper and its Supporting information files.
Funding Statement
This work was supported in part by a grant from National Institutes of Health (AI-030639). The funder had no role in study design, data collection and analysis, decision to publish or preparation of this manuscript.
References
- 1.Wilson ME, Jeronimo SM, Pearson RD. Immunopathogenesis of infection with the visceralizing Leishmania species. Microb Pathog 2005. April;38(4):147–60. doi: 10.1016/j.micpath.2004.11.002 [DOI] [PubMed] [Google Scholar]
- 2.Chagas E. Visceral Leishmaniasis in Brazil. Science 1936. October 30;84(2183):397–8. [DOI] [PubMed] [Google Scholar]
- 3.de Alencar JE. Visceral Leishmaniasis in Brazil. Rev Assoc Med Bras 1958. August;4(3):222–36. [PubMed] [Google Scholar]
- 4.Deane LM, Deane MP. Visceral leishmaniasis in Brazil: geographical distribution and transmission. Rev Inst Med Trop Sao Paulo 1962. May;4:198–212. [PubMed] [Google Scholar]
- 5.Mauricio IL, Howard MK, Stothard JR, Miles MA. Genomic diversity in the Leishmania donovani complex. Parasitology 1999. September;119 (Pt 3):237–46. [DOI] [PubMed] [Google Scholar]
- 6.Mauricio IL, Stothard JR, Miles MA. The strange case of Leishmania chagasi. Parasitol Today 2000. May;16(5):188–9. [DOI] [PubMed] [Google Scholar]
- 7.Badaro R, Jones TC, Lorenco R, Cerf BJ, Sampaio D, Carvalho EM, et al. A prospective study of visceral leishmaniasis in an endemic area of Brazil. J Infect Dis 1986. October;154(4):639–49. [DOI] [PubMed] [Google Scholar]
- 8.Evans TG, Teixeira MJ, McAuliffe IT, Vasconcelos I, Vasconcelos AW, Sousa AA, et al. Epidemiology of visceral leishmaniasis in northeast Brazil. J Infect Dis 1992. November;166(5):1124–32. [DOI] [PubMed] [Google Scholar]
- 9.Costa CH, Pereira HF, Araujo MV. Visceral leishmaniasis epidemic in the State of Piaui, Brazil, 1980–1986. Rev Saude Publica 1990. October;24(5):361–72. [DOI] [PubMed] [Google Scholar]
- 10.Jeronimo SM, Oliveira RM, Mackay S, Costa RM, Sweet J, Nascimento ET, et al. An urban outbreak of visceral leishmaniasis in Natal, Brazil. Trans R Soc Trop Med Hyg 1994. July;88(4):386–8. [DOI] [PubMed] [Google Scholar]
- 11.Genaro O, da Costa CA, Williams P, Silva JE, Rocha NM, Lima SL, et al. Occurrence of kala-azar in the urban area of Grande Belo Horizonte, Minas Gerais. Rev Soc Bras Med Trop 1990. April;23(2):121 [DOI] [PubMed] [Google Scholar]
- 12.Marzochi MC, Marzochi KB, Carvalho RW. Visceral leishmaniasis in Rio de Janeiro. Parasitol Today 1994. January;10(1):37–40. [DOI] [PubMed] [Google Scholar]
- 13.Franke CR, Ziller M, Staubach C, Latif M. Impact of the El Nino/Southern Oscillation on visceral leishmaniasis, Brazil. Emerg Infect Dis 2002. September;8(9):914–7. doi: 10.3201/eid0809.010523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nieto P, Malone JB, Bavia ME. Ecological niche modeling for visceral leishmaniasis in the state of Bahia, Brazil, using genetic algorithm for rule-set prediction and growing degree day-water budget analysis. Geospat Health 2006. November;1(1):115–26. doi: 10.4081/gh.2006.286 [DOI] [PubMed] [Google Scholar]
- 15.Jeronimo SM, Duggal P, Braz RF, Cheng C, Monteiro GR, Nascimento ET, et al. An emerging peri-urban pattern of infection with Leishmania chagasi, the protozoan causing visceral leishmaniasis in northeast Brazil. Scand J Infect Dis 2004;36(6–7):443–9. [DOI] [PubMed] [Google Scholar]
- 16.Michel G, Pomares C, Ferrua B, Marty P. Importance of worldwide asymptomatic carriers of Leishmania infantum (L. chagasi) in human. Acta Trop 2011. August;119(2–3):69–75. doi: 10.1016/j.actatropica.2011.05.012 [DOI] [PubMed] [Google Scholar]
- 17.Lima ID, Queiroz JW, Lacerda HG, Queiroz PV, Pontes NN, Barbosa JD, et al. Leishmania infantum chagasi in northeastern Brazil: asymptomatic infection at the urban perimeter. Am J Trop Med Hyg 2012. January;86(1):99–107. doi: 10.4269/ajtmh.2012.10-0492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dos Santos Marques LH, DA Rocha IC, Reis IA, DA Cunha GM, Oliveira E, Pfeilsticker TR, et al. Leishmania infantum: illness, transmission profile and risk factors for asymptomatic infection in an endemic metropolis in Brazil. Parasitology 2016. November 29;1–11. [DOI] [PubMed] [Google Scholar]
- 19.Badaro R, Carvalho EM, Rocha H, Queiroz AC, Jones TC. Leishmania donovani: an opportunistic microbe associated with progressive disease in three immunocompromised patients. Lancet 1986. March 22;1(8482):647–9. [DOI] [PubMed] [Google Scholar]
- 20.Harrison LH, Naidu TG, Drew JS, de Alencar JE, Pearson RD. Reciprocal relationships between undernutrition and the parasitic disease visceral leishmaniasis. Rev Infect Dis 1986. May;8(3):447–53. [DOI] [PubMed] [Google Scholar]
- 21.Cerf BJ, Jones TC, Badaro R, Sampaio D, Teixeira R, Johnson WD Jr. Malnutrition as a risk factor for severe visceral leishmaniasis. J Infect Dis 1987. December;156(6):1030–3. [DOI] [PubMed] [Google Scholar]
- 22.Maciel BL, Lacerda HG, Queiroz JW, Galvao J, Pontes NN, Dimenstein R, et al. Association of nutritional status with the response to infection with Leishmania chagasi. Am J Trop Med Hyg 2008. October;79(4):591–8. [PubMed] [Google Scholar]
- 23.Cencini E, Lazzi S, Fabbri A. Atypical clinical presentation of visceral leishmaniasis in a patient with non-Hodgkin lymphoma. Eur J Haematol 2015. February;94(2):186 doi: 10.1111/ejh.12312 [DOI] [PubMed] [Google Scholar]
- 24.Alvar J, Blazquez J, Najera R. Association of visceral leishmaniasis and human immunodeficiency virus infections. J Infect Dis 1989. September;160(3):560–1. [DOI] [PubMed] [Google Scholar]
- 25.Mina MJ, Metcalf CJ, de Swart RL, Osterhaus AD, Grenfell BT. Long-term measles-induced immunomodulation increases overall childhood infectious disease mortality. Science 2015. May 8;348(6235):694–9. doi: 10.1126/science.aaa3662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tielemans SMAJ, de Melker HE, Hahne SJM, Boef AGC, van der Klis FRM, Sanders EAM, et al. Non-specific effects of measles, mumps, and rubella (MMR) vaccination in high income setting: population based cohort study in the Netherlands. BMJ 2017. August 30;358:j3862 doi: 10.1136/bmj.j3862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lemos DR, Franco AR, de Sa Roriz ML, Carneiro AK, de Oliveira Garcia MH, de Souza FL, et al. Measles epidemic in Brazil in the post-elimination period: Coordinated response and containment strategies. Vaccine 2017. March 23;35(13):1721–8. doi: 10.1016/j.vaccine.2017.02.023 [DOI] [PubMed] [Google Scholar]
- 28.Leite RD, Barreto JL, Sousa AQ. Measles Reemergence in Ceara, Northeast Brazil, 15 Years after Elimination. Emerg Infect Dis 2015. September;21(9):1681–3. doi: 10.3201/eid2109.150391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Scarlata F, Li V, V, Abbadessa V, Giordano S, Infurnari L, Saporito L, et al. [Serological screening for Leishmania infantum in asymptomatic blood donors and HIV+ patients living in an endemic area]. Infez Med 2008. March;16(1):21–7. [PubMed] [Google Scholar]
- 30.Alvar J, Gutierrez-Solar B, Molina R, Lopez-Velez R, Garcia-Camacho A, Martinez P, et al. Prevalence of Leishmania infection among AIDS patients. Lancet 1992. June 6;339(8806):1427. [DOI] [PubMed] [Google Scholar]
- 31.Alvar J, Gutierrez-Solar B, Pachon I, Calbacho E, Ramirez M, Valles R, et al. AIDS and Leishmania infantum. New approaches for a new epidemiological problem. Clin Dermatol 1996. September;14(5):541–6. [DOI] [PubMed] [Google Scholar]
- 32.Agostoni C, Dorigoni N, Malfitano A, Caggese L, Marchetti G, Corona S, et al. Mediterranean leishmaniasis in HIV-infected patients: epidemiological, clinical, and diagnostic features of 22 cases. Infection 1998. March;26(2):93–9. [DOI] [PubMed] [Google Scholar]
- 33.Rabello A, Orsini M, Disch J. Leishmania/HIV co-infection in Brazil: an appraisal. Ann Trop Med Parasitol 2003. October;97 Suppl 1:17–28. [DOI] [PubMed] [Google Scholar]
- 34.Nascimento ET, Moura ML, Queiroz JW, Barroso AW, Araujo AF, Rego EF, et al. The emergence of concurrent HIV-1/AIDS and visceral leishmaniasis in Northeast Brazil. Trans R Soc Trop Med Hyg 2011. May;105(5):298–300. doi: 10.1016/j.trstmh.2011.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pagano M, Gauvreau K. Principles of Biostatistics. 2nd ed. Belmont, CA: Brooks/Cole CENGAGE Learning; 2000. [Google Scholar]
- 36.de Oliveira EF, Oshiro ET, Fernandes WS, Ferreira AM, de Oliveira AG, Galati EA. Vector Competence of Lutzomyia cruzi Naturally Demonstrated for Leishmania infantum and Suspected for Leishmania amazonensis. Am J Trop Med Hyg 2017. January 11;96(1):178–81. doi: 10.4269/ajtmh.16-0191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dey A, Singh S. Transfusion transmitted leishmaniasis: a case report and review of literature. Indian J Med Microbiol 2006. July;24(3):165–70. [PubMed] [Google Scholar]
- 38.Duarte EC, Ramalho WM, Tauil PL, Fontes CJ, Pang L. The changing distribution of malaria in the Brazilian Amazon, 2003–2004 and 2008–2009. Rev Soc Bras Med Trop 2014. November;47(6):763–9. doi: 10.1590/0037-8682-0274-2014 [DOI] [PubMed] [Google Scholar]
- 39.Maia-Elkhoury AN, Alves WA, Sousa-Gomes ML, Sena JM, Luna EA. Visceral leishmaniasis in Brazil: trends and challenges. Cad Saude Publica 2008. December;24(12):2941–7. [DOI] [PubMed] [Google Scholar]
- 40.Cavalcante IJ, Vale MR. Epidemiological aspects of visceral leishmaniasis (kala-azar) in Ceara in the period 2007 to 2011. Rev Bras Epidemiol 2014. December;17(4):911–24. [DOI] [PubMed] [Google Scholar]
- 41.Mengesha B, Endris M, Takele Y, Mekonnen K, Tadesse T, Feleke A, et al. Prevalence of malnutrition and associated risk factors among adult visceral leishmaniasis patients in Northwest Ethiopia: a cross sectional study. BMC Res Notes 2014. February 4;7:75 doi: 10.1186/1756-0500-7-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Andrade IG, Queiroz JW, Cabral AP, Lieberman JA, Jeronimo SM. Improved sanitation and income are associated with decreased rates of hospitalization for diarrhoea in Brazilian infants. Trans R Soc Trop Med Hyg 2009. May;103(5):506–11. doi: 10.1016/j.trstmh.2008.12.017 [DOI] [PubMed] [Google Scholar]
- 43.Ministerio da Saude. Manual de Condutas Gerais do Programa Nacional de Suplementação de Vitamina A. 2013. Brasilia: Ministério da Saúde. [Google Scholar]
- 44.Maciel BL, Valverde JG, Rodrigues-Neto JF, Freire-Neto F, Keesen TS, Jeronimo SM. Dual immune modulatory effect of vitamin A in human visceral leishmaniasis. PLoS One 2014;9(9):e107564 doi: 10.1371/journal.pone.0107564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lima AA, Leite AM, Di MA, Lima NL, Soares AM, Abreu CB, et al. Determinant Variables, Enteric Pathogen Burden, Gut Function, and Immune-Related Inflammatory Biomarkers Associated with Childhood Malnutrition: A Prospective Case-Control Study in Northeastern Brazil. Pediatr Infect Dis J 2017. February 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Guerrant RL, Leite AM, Pinkerton R, Medeiros PH, Cavalcante PA, DeBoer M, et al. Biomarkers of Environmental Enteropathy, Inflammation, Stunting, and Impaired Growth in Children in Northeast Brazil. PLoS One 2016;11(9):e0158772 doi: 10.1371/journal.pone.0158772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mina MJ. Measles, immune suppression and vaccination: direct and indirect nonspecific vaccine benefits. J Infect 2017. June;74 Suppl 1:S10–S17. [DOI] [PubMed] [Google Scholar]
- 48.Anuradha, Pal R, Katiyar JC. Sex-influenced population kinetics of Leishmania donovani in hamsters. Indian J Exp Biol 1990. September;28(9):876–9. [PubMed] [Google Scholar]
- 49.Nackers F, Mueller YK, Salih N, Elhag MS, Elbadawi ME, Hammam O, et al. Determinants of Visceral Leishmaniasis: A Case-Control Study in Gedaref State, Sudan. PLoS Negl Trop Dis 2015. November;9(11):e0004187 doi: 10.1371/journal.pntd.0004187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mukhopadhyay D, Mukherjee S, Ghosh S, Roy S, Saha B, Das NK, et al. A male preponderance in patients with Indian post kala-azar dermal leishmaniasis is associated with increased circulating levels of testosterone. Int J Dermatol 2016. May;55(5):e250–e255. doi: 10.1111/ijd.13048 [DOI] [PubMed] [Google Scholar]
- 51.de AJ. Prevention of kala-azar in Ceara, Brazil. Rev Inst Med Trop Sao Paulo 1961. July;3:175–80. [PubMed] [Google Scholar]
- 52.Moreno J, Alvar J. Canine leishmaniasis: epidemiological risk and the experimental model. Trends Parasitol 2002. September;18(9):399–405. [DOI] [PubMed] [Google Scholar]
- 53.Zoghlami Z, Chouihi E, Barhoumi W, Dachraoui K, Massoudi N, Helel KB, et al. Interaction between canine and human visceral leishmaniases in a holoendemic focus of Central Tunisia. Acta Trop 2014. November;139:32–8. doi: 10.1016/j.actatropica.2014.06.012 [DOI] [PubMed] [Google Scholar]
- 54.Paranhos-Silva M, Freitas LA, Santos WC, Grimaldi GJ, Pontes-de-Carvalho LC, Oliveira-dos-Santos AJ. A cross-sectional serodiagnostic survey of canine leishmaniasis due to Leishmania chagasi. Am J Trop Med Hyg 1996. July;55(1):39–44. [DOI] [PubMed] [Google Scholar]
- 55.Viana GM, Nascimento MD, Rabelo EM, Diniz Neto JA, Binda Junior JR, Galvao CS, et al. Relationship between rainfall and temperature: observations on the cases of visceral leishmaniasis in Sao Luis Island, State of Maranhao, Brazil. Rev Soc Bras Med Trop 2011. November;44(6):722–4. [DOI] [PubMed] [Google Scholar]
- 56.Thompson RA, Wellington de Oliveira LJ, Maguire JH, Braud DH, Scholl DT. Climatic and demographic determinants of American visceral leishmaniasis in northeastern Brazil using remote sensing technology for environmental categorization of rain and region influences on leishmaniasis. Am J Trop Med Hyg 2002. December;67(6):648–55. [DOI] [PubMed] [Google Scholar]
- 57.Coelho L, Grinsztejn B, Castilho JL, De BR, Quintana MS, Campos DP, et al. Mortality in HIV-infected women, heterosexual men, and men who have sex with men in Rio de Janeiro, Brazil: an observational cohort study. Lancet HIV 2016. October;3(10):e490–e498. doi: 10.1016/S2352-3018(16)30052-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Alvar J, Verdejo J, Osuna A, Najera R. Visceral leishmaniasis in a patient seropositive for HIV. Eur J Clin Microbiol 1987. October;6(5):604–6. [DOI] [PubMed] [Google Scholar]
- 59.Gramiccia M. The identification and variability of the parasites causing leishmaniasis in HIV-positive patients in Italy. Ann Trop Med Parasitol 2003. October;97 Suppl 1:65–73. [DOI] [PubMed] [Google Scholar]
- 60.Costa CH, Werneck GL, Rodrigues L Jr., Santos MV, Araujo IB, Moura LS, et al. Household structure and urban services: neglected targets in the control of visceral leishmaniasis. Ann Trop Med Parasitol 2005. April;99(3):229–36. doi: 10.1179/136485905X28018 [DOI] [PubMed] [Google Scholar]
- 61.Moreno J, Canavate C, Chamizo C, Laguna F, Alvar J. HIV—Leishmania infantum co-infection: humoral and cellular immune responses to the parasite after chemotherapy. Trans R Soc Trop Med Hyg 2000. May;94(3):328–32. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting information files.