Determining the prognosis of comatose patients is difficult, and yet this information is vital for informing treatment decisions. While fMRI offers promise as a prognostic tool, further research is needed into its use. Weijer et al. provide the first analysis of the ethical issues surrounding such research in comatose patients.
Keywords: research ethics, functional MRI, coma, traumatic brain injury, prognosis
Determining the prognosis of comatose patients is difficult, and yet this information is vital for informing treatment decisions. While fMRI offers promise as a prognostic tool, further research is needed into its use. Weijer et al. provide the first analysis of the ethical issues surrounding such research in comatose patients.
Abstract
Introduction
Estimating the likelihood of recovery of cognitive function in the acutely comatose patient is one of the most difficult challenges facing neurologists and critical care physicians. Coma, defined as a state of unarousable unconsciousness, is most commonly caused by traumatic brain injury and anoxia following cardiopulmonary arrest. Patient outcome after severe brain injury is highly variable ( Young and Schiff, 2014 ). Some patients regain high levels of functioning, whereas up to half have serious cognitive deficits and dependency. Acutely comatose patients are incapable of making decisions regarding their medical care, and thus their welfare is in the hands of both the health care team and their families. Accurate prognostic information critically informs treatment recommendations by the heath care team and decisions made on the patient's behalf by the family.
Prognosis in the acutely comatose patient is assessed using clinical examination, structural neuroimaging, biomarkers and electrophysiological testing ( Young and Schiff, 2014 ). The dynamic nature of brain injury and the potential for confounding factors, such as medication and metabolic disturbance, must be taken into account during patient assessment. Indeed, these features highlight the importance of repeated examination and integration of findings from diverse diagnostic modalities. Recent reviews have summarized current prognostic markers in the assessment of comatose survivors of cardiac arrest ( Sandroni et al. , 2013 a , b ) ( Table 1 ) and traumatic brain injury ( Table 2 ) ( Stevens and Sutter, 2013 ). Despite these indicators, a subset of patients retains an indeterminate prognosis and novel prognostic indicators—particularly those that predict neurological recovery—would be valuable.
Table 1.
Prognostic markers in the assessment of comatose survivors of cardiac arrest
| Prognostic indicator a,b | False positive rate c 95% confidence interval | |
|---|---|---|
| No therapeutic hypothermia | Presence of myoclonus at 24–48 h d | 0–3% at 24 h |
| 0–5% at 48 h | ||
| Absence of pupillary light reflex at 72 h | 0–8% | |
| Bilateral absence of SSEP N20 waveform at 24–72 h | 0–12% | |
| Low EEG voltage <20 µV at ≤72 h | 0–8% | |
| Neuron specific enolase at 48 h (>65 µg/l) or 72 h (>80 µg/l) e | 0–3% | |
| Therapeutic hypothermia | Combination of absent pupillary light reflex, corneal reflex and motor response no better than extension after rewarming | 0–8% |
| Bilateral absence of SSEP N20 waveform during hypothermia or after rewarming | 0–2% during hypothermia | |
| 0–4% after rewarming | ||
| Non-reactive EEG background after rewarming | 0–3% |
a In many studies of prognosis after cardiac arrest, the predictors being analysed were also used as the basis for withdrawal of life sustaining therapies. Therefore, a self-fulfilling prophecy may exist within these data.
b Many patients will not fulfill all criteria when considering prognostication. In this case, the convergence of results from multiple testing modalities is important for accurate prognostication.
c For prediction of Cerebral Performance Categories 3–5.
d Early myoclonic status epilepticus is likely a very poor prognostic factor. However, myoclonus associated with Lance-Adams syndrome may occur after cardiac arrest. This myoclonus is more benign with respect to prognosis for recovery of consciousness and therefore care must be taken when interpreting myoclonus in the first 72 h post cardiac arrest. Other prognostic factors should be taken into account in order to avoid inappropriately poor prognostic predictions.
e Neuron specific enolase is not available at all centres.
SSEP = somatosensory evoked potential.
Table 2.
Prognostic markers in the assessment of patients with severe traumatic brain injury
| Prognostic indicator a | Pertinent statistics b | |
|---|---|---|
| Clinical examination, biomarkers and electrophysiology | Bilaterally absent SSEP N20 at 3–7 days | Positive predictive value for poor outcome c = 99% |
| Neuron specific enolase at 0–3 days | Sensitivity for poor outcome = 76%; Specificity for poor outcome = 66% | |
| Glasgow Coma Scale motor subscore | AUC for poor outcome at 6 months = 83% | |
| Full Outline of Unresponsiveness (FOUR) score | AUC for poor outcome at 6 months = 85% | |
| Combinations of individual computerized tomography predictors at admission | Status of basal cisterns | AUC for mortality at 6 months = 77% |
| Midline shift | ||
| Traumatic subarachnoid haemorrhage | ||
| Intraventricular haemorrhage | ||
| Mass lesions | ||
| Extradural versus intradural lesions |
a Because traumatic brain injury is very heterogeneous, individual prognostic tests are less reliable. Outcome prediction tools, such as the IMPACT or CRASH models, may be used to gain a better understanding of the expected outcome for a population of patients. However, these scores do not apply specifically to any individual patient.
b Because the evidence base supporting prognostic decision making in severe traumatic brain injury is far more heterogeneous than that for hypoxic ischaemic injury, the statistics are also heterogeneous. Thus, the data are presented differently from in Table 1 .
c Poor outcome refers to Cerebral Performance Categories 4–5.
AUC = area under the curve; SSEP = somatosensory evoked potential.
Prognostic uncertainty in the acutely comatose patient is associated with considerable practice variation in the withdrawal of life-sustaining therapy. Turgeon et al. (2011) studied 720 patients with severe traumatic brain injury in six Canadian level-one trauma centres. The mortality rate in this group of patients was 32% and in the majority of cases (70%) death was preceded by the withdrawal of life-sustaining therapy. Many decisions to withdraw life-sustaining therapy were made within 3 days of injury and, according to the authors, ‘[i]n some instances, this may be too early for accurate neuroprognostication’ ( Turgeon et al. , 2011 ). Additionally, hospital mortality rates differed substantially—ranging from 10.8% to 44.1%—and the variation was not explained by patient risk factors. The authors conclude that ‘[t]his raises the concern that differences in mortality between centres may be partly due to variation in physicians’ perceptions of long-term prognosis’ ( Turgeon et al. , 2011 ). Clearly, new methods are required to improve prognostication in acute coma.
Functional MRI research
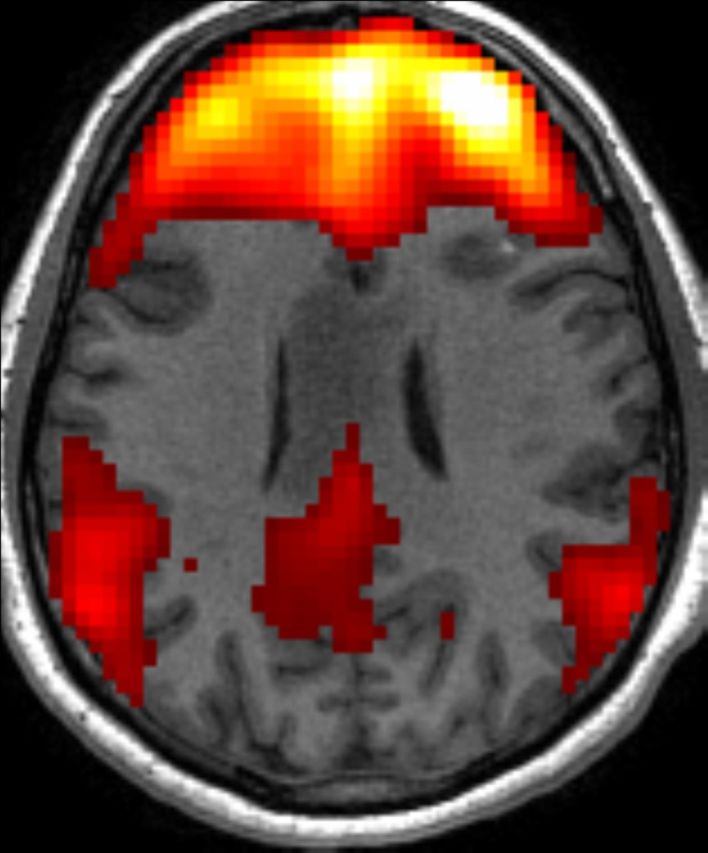
Functional MRI is a promising experimental diagnostic and prognostic modality in patients who have suffered severe brain injuries. Functional MRI has been used to map resting state networks and residual cognitive function in patients with chronic disorders of consciousness, including minimally conscious and vegetative patients. In one study, 17% of patients diagnosed as vegetative were found to be covertly aware ( Monti et al. , 2010 ). In addition to diagnostic information, functional MRI may also provide useful prognostic information. Coleman et al. (2009) used a hierarchical speech processing task in 41 patients with disorders of consciousness 2 to 108 months post injury. The level of speech and semantic processing revealed on functional MRI was strongly correlated with behavioural recovery 6 months after the scan. However, functional MRI has only been used infrequently in the context of acute coma. Functional MRI is difficult to perform in critically ill patients who are mechanically ventilated and may be medically unstable and, as a result, few research teams have the necessary experience to use this technique effectively.
Conceptually, functional MRI could be used in three different ways to assess acutely comatose patients (or, the broader group of patients with acute impairment of consciousness after brain injury). First, resting state functional MRI can be used to assess functional interactions between different brain regions when a patient is not exposed to any particular stimulus, nor asked to perform any specific task. Second, cognitive functions that do not require consciousness, such as sound processing, visual processing, speech recognition and semantic processing, can be assessed by passive paradigms that do not require the cooperation of the patient. Third, cognitive functions that do require consciousness, such as memory, executive function, and command following, may be assessed by active paradigms requiring patient cooperation. A central hypothesis of functional MRI research in acutely comatose patients is that evidence of preserved neural connectivity and cognitive function will predict neurological recovery.
To date, four published studies have used functional MRI in acutely comatose patients (defined as a Glasgow Coma Scale score ≤8 at enrolment). In the three studies that looked at patient outcome, functional MRI results were correlated with neurological recovery. Gofton et al. (2009) measured blood oxygen level-dependent (BOLD) values in the somatosensory cortex (S1) contralateral to painful stimulation of the hand (a passive paradigm) in 19 comatose patients 2 to 6 days after cardiac arrest. The BOLD signal in S1 was positively correlated with neurological recovery at 3 months following cardiac arrest. Norton et al. (2012) used resting state functional MRI to assess default mode network connectivity in 13 acutely comatose patients 1 to 6 days after cardiac arrest. All patients with reversible coma (2/13) had a present and intact default mode network, whereas patients with irreversible coma (11/13) had a disrupted neural network. Koenig et al. (2014) followed up on these findings by studying default mode network connectivity in 17 patients 4 to 7 days after cardiac arrest who had an indeterminate prognosis by standard clinical measures. The strength of neural connectivity was greater in patients with a good outcome (8/17) than in those with a poor outcome (9/17).
A recent study by Mikell et al. (2015) examined resting state networks in nine comatose and 16 awake patients within 14 days of intracerebral or subarachnoid haemorrhage. They concluded that functional network disruption, rather than structural injury, accounted for coma after haemorrhagic stroke but drew no conclusions regarding functional MRI findings and patient outcome.
We believe that functional MRI research in acutely comatose patients has considerable promise. Such studies are, however, not only technically challenging, but pose difficult ethical issues. In this paper, we present the first ethical analysis of functional MRI research in the intensive care unit. We describe six issues in the ethical design and conduct of functional MRI studies that ought to be considered by researchers and research ethics committees.
Ethical considerations in functional MRI research
General ethical principles govern the design and conduct of medical research. All research involving human participants ought to be conducted in accord with the ethical principles of respect for persons, beneficence and justice. These principles are grounded in ethical theories and the research ethics literature, and they are expressed in national and international ethics guidelines.
The application of ethical principles and rules to research in the intensive care unit is difficult. Critically ill patients are typically incapable of making decisions regarding research participation, and informed consent must be sought from a surrogate decision maker. It may be difficult, however, to obtain surrogate consent in the time frame required in some studies. Beyond this, some have questioned the legal authority of surrogates to consent to research participation. Further, patients in the intensive care unit, by virtue of their medical condition, may be unduly susceptible to the risks of research participation and this must be taken into account in the assessment of study benefits and harms. Finally, by virtue of decisional incapacity and susceptibility to harm, critically ill patients constitute a vulnerable group. While this does not preclude research in the intensive care unit, vulnerable research participants are entitled to additional protections.
Functional MRI research on acutely comatose patients shares these ethical challenges, and is further complicated by current uncertainty regarding functional MRI results and patient prognosis, the risks associated with intra-hospital transport of critically ill patients, and the potential for functional MRI results to impact decision making regarding the withdrawal of life-sustaining therapy. While functional MRI research holds considerable promise for improving our ability to predict neurological improvement, researchers and research ethics committees must ensure that ethical concerns are adequately addressed. We argue that six ethical issues ought to be addressed in any prospective functional MRI study in this setting ( Table 3 ).
Table 3.
A summary checklist for use in ethics applications, indicating page number in study protocol where an ethical issue is being addressed
| Ethical issue | Relevant considerations | Study protocol (page #) |
|---|---|---|
| (1) Is functional MRI a therapeutic or non-therapeutic procedure in the study context? |
|
|
| (2) Have the risks of research participation, including the risks of intrahospital transport, been minimized consistent with sound scientific design? |
|
|
| (3) Are the risks of non-therapeutic procedures no more than a minor increase above minimal risk? |
|
|
| (4) Have study participants been selected equitably? |
|
|
| (5) Will valid surrogate consent for study participation be obtained? |
|
|
| (6) Are adequate plans in place to share summary and individual research results with the responsible physician or the family? |
|
Is functional MRI a therapeutic or non- therapeutic procedure in the study context?
The ethical analysis of the benefits and harms of study participation begins with the classification of study procedures as either therapeutic or non-therapeutic ( Weijer and Miller, 2004 ). Therapeutic procedures in the context of research are study interventions designed to treat, diagnose or prevent illness that are administered on the basis of evidence sufficient to justify the belief that they may benefit research participants. Therapeutic procedures are justified if they satisfy clinical equipoise, that is, at the start of the study there must be honest, professional disagreement in the community of expert practitioners as to the preferred treatment or diagnostic modality. Non-therapeutic procedures in research do not hold out the reasonable prospect of direct benefit to study participants and are administered solely to address the scientific question. The risks of non-therapeutic procedures must be minimized consistent with scientific design, and be judged reasonable in relation to study benefits. Additionally, when the study population is vulnerable, the risks of non-therapeutic procedures should not exceed a minor increase over minimal risk, where minimal risk is understood as the risks of daily life.
Should functional MRI in the context of research on acutely comatose patients be considered a therapeutic or non-therapeutic procedure? The question is important because differing moral standards are invoked and—broadly speaking—standards for therapeutic procedures are less restrictive than those for non-therapeutic procedures. We believe the answer will differ from one study to the next and, accordingly, the study protocol should clearly identify and justify the use of functional MRI as a therapeutic or non-therapeutic procedure. A number of factors can usefully guide the appropriate classification of functional MRI as a study procedure. Where is the study in the translational trajectory of functional MRI research in acute coma? As the classification depends on the evidence supporting functional MRI as a prognostic modality, early studies in the translational trajectory of functional MRI will tend to involve non-therapeutic uses of functional MRI, whereas later studies will tend to involve therapeutic applications. Is the evidence base sufficient to justify the belief that the use of functional MRI in the study may benefit research participants? Does the study question seek to further our understanding of acute coma (in which case, functional MRI is more likely non-therapeutic) or does it seek to establish the prognostic value of functional MRI (more likely therapeutic)? Is the study population broadly inclusive of acutely comatose patients (in which case, functional MRI is more likely non-therapeutic) or is it restricted to those with an indeterminate prognosis (more likely therapeutic)? The research ethics committee should review the classification of functional MRI and the justification provided in the study protocol.
Have the risks of research participation, including the risks of intra-hospital transport, been minimized consistent with sound scientific design?
The transport of critically ill patients from the intensive care unit to the MRI scanner is associated with risk. Transport may impact the patient in two broad ways ( Fanara et al. , 2010 ). First, changes in posture, and acceleration and deceleration have potential haemodynamic, respiratory and neurological consequences. Second, moving the patient out of the protective environment of the intensive care unit and changing equipment (such as switching to a portable ventilator) generate additional stresses for the patient and open the possibility of equipment failure. Comparing epidemiological studies of the risks of intra-hospital transport is difficult due to differences in definitions, patient acuity, patient location (e.g. intensive care unit versus emergency department) and transport protocols. Reported rates of serious adverse events range from 4.2% to 8.9%, and cardiac arrest rates range from 0.34% to 1.6% ( Fanara et al. , 2010 ).
Given the risks of intra-hospital transport of critically ill patients, researchers must ensure that appropriate steps are taken to protect the safety of all participants in functional MRI studies. Professional guidelines set out minimum standards for patient safety in intra-hospital transport ( Fanara et al. , 2010 ). High safety standards are promoted by plans that stabilize the patient before transport, require communication and coordination among staff prior to transport, use trained staff to transport patients, use equipment adapted for transport purposes, collect detailed information on the patient before, during and after transport, and undergo periodic evaluation for quality improvement ( Fanara et al. , 2010 ). Training and careful planning have a measurable impact on patient safety. A recent study demonstrated that a 4-h educational program for transport staff and the routine use of a safety checklist decreased serious adverse events in intra-hospital transport by 42.9%, from 9.1% to 5.2% ( Choi et al. , 2012 ).
Special care must be taken in studies in which functional MRI is a non-therapeutic procedure. In these cases the risks of transporting the participant to the MRI scanner cannot be offset by the prospect of direct benefit. Accordingly, researchers must take all reasonable steps to ensure that risks to study participants are minimized consistent with sound scientific design. As discussed below, acutely comatose patients who may be at undue risk of a serious adverse event should be excluded from the study. Additionally, where feasible, functional MRI scans should be combined with clinically indicated structural MRI scans. This simple strategy protects patients from the risks of multiple transports to the MRI scanner. As the transport is clinically indicated, ‘piggy-backing’ a research scan on a clinically indicated structural scan reduces the research-related risk to the additional time required in the MRI scanner (perhaps 45 to 60 min). We recognize that the practicalities of scheduling MRI scanner time in a busy clinical environment may not allow such ‘dual purpose’ scans in all cases.
Are the risks of non- therapeutic procedures no more than a minor increase above minimal risk?
Acutely comatose patients in the intensive care unit are a vulnerable population and, accordingly, are entitled to additional protections. A central protection for vulnerable research participants is a limit on the amount of non-therapeutic risk to which they may be exposed. In Canada the threshold is ‘minimal risk’, understood as the risks of the daily lives of the eligible study population; in the United States, the threshold is ‘a minor increase above minimal risk’ where minimal risk is understood as the risks of the daily lives of healthy persons ( Weijer and Miller, 2004 ). The meaning of minimal risk and what non-therapeutic research procedures legitimately fall within the bounds of minimal risk is a topic of considerable debate in the literature. It has been argued that an MRI scan in a healthy child falls under the minimal risk threshold, but the addition of contrast or sedation to the MRI scan exceeds this threshold ( Schmidt et al. , 2011 ).
When functional MRI in studies on acutely comatose patients is a therapeutic procedure, its use is justified by satisfaction of clinical equipoise. The minimal risk (or minor increase above minimal risk) threshold only applies in studies in which functional MRI is a non-therapeutic procedure. Given the vulnerability of the patient population (and the restrictiveness of the minimal risk threshold), researchers must take all feasible steps to minimize non-therapeutic risks. Researchers and research ethics committees must ensure that non-therapeutic risks within the study do not exceed the threshold for permissible risk. This will require addressing a number of questions. What are the non-therapeutic risks in the study? How much time in the MRI scanner is involved? Are the risks of intra-hospital transport included within the non-therapeutic risks (or are research scans coupled with clinically indicated scans)? What risk threshold is set out in relevant regulations? Does minimal risk refer to the daily lives of healthy persons or of the eligible study population? Are the non-therapeutic study risks comparable to the risks of daily life of the relevant referent group?
Have study participants been selected equitably?
The principle of justice requires that the benefits and burdens of research be distributed fairly. Researchers must ensure that potential participants who are unduly susceptible to research risks are excluded. Additionally, researchers may not exclude without good reason those who may benefit from study participation. As acutely comatose patients are mechanically ventilated and may be medically unstable, prudent judgment must be applied when enrolling patients and determining the timing of the functional MRI scan. As with all intra-hospital transport involving critically ill patients, steps must be taken before transport to ensure the patient is medically stable. When the study involves functional MRI as a non-therapeutic procedure, a high degree of caution must be applied to the selection of patients for study participation as study risks are not offset by the prospect of direct benefit. Patients who have a higher risk of serious adverse events during transport may not be appropriate candidates for participation in these studies ( Fanara et al. , 2010 ). In all functional MRI studies, patients must be able to tolerate lying flat in the scanner, and this may preclude the participation of patients with increased intracranial pressure or congestive heart failure. Additionally, the participation of patients receiving high doses of a sedative or with seizure activity may be deferred, as these will interfere with study results.
In studies whose primary objective is to determine the prognostic value of functional MRI (and in which functional MRI is a therapeutic procedure), study eligibility may be restricted to acutely comatose patients with an indeterminate prognosis based on standard clinical measures. In this way, the study population will more closely resemble the target clinical population.
Will valid surrogate consent for study participation be obtained?
As acutely comatose patients are incapable of decision making, informed consent for research participation must be obtained from a surrogate decision maker, usually the next of kin. Provision of surrogate consent for medical treatment is typically defined in provincial or state legislation. While few statutes specifically consider surrogate consent for research participation, it is now generally accepted that the legally authorized surrogate for medical decisions may make decisions regarding research participation. The families of patients who have suffered a severe brain injury are themselves vulnerable, due to emotional trauma, difficulty understanding complex medical information regarding the patient's condition, the unfamiliar setting of the intensive care unit and lack of sleep. Judgment and sensitivity must be applied to the suitability and timing of approaching a family regarding patient participation in a functional MRI study. Typically, the responsible physician will determine who may be approached and will confirm this with one or more family members. The researcher should ensure that an appropriate room is available and adequate time is set aside to meet with family members.
The use of functional MRI in chronic disorders of consciousness patients has received considerable media attention. As a result, both therapeutic misconception—the mistaken belief that non-therapeutic aspects of a study hold the prospect of direct patient benefit—and therapeutic misestimation—mistakenly inflating the likelihood or magnitude of direct benefit—are a challenge for informed consent in functional MRI studies. Researchers can take a number of steps to improve the comprehension of study information and thereby reduce the risk of therapeutic misconception. Researchers should ensure that consent materials clearly identify functional MRI as either non-therapeutic or therapeutic, and present the prospect for benefit (if any) in cautious and evidence-based language. The informed consent document should be short and written at a grade eight reading level ( Nishimura et al. , 2013 ). The Acute Respiratory Distress Syndrome Clinical Trials Network has published an informed consent template for research in the intensive care unit that is short and uses simple language ( Silverman et al. , 2005 ). Researchers should also ensure that family members are provided with adequate time to discuss the study with trained research staff ( Nishimura et al. , 2013 ). Other interventions to improve comprehension of study information, including multimedia materials and testing comprehension with feedback of test results, are associated with inconsistent results or methodologically flawed studies ( Nishimura et al. , 2013 ).
Are adequate plans in place to share summary and individual research results with the responsible physician or the family?
The right of patients to receive summary research results once a study has been completed is widely recognized. Researchers conducting functional MRI studies should, therefore, plan to share summary results with patients or their next-of-kin once the study has been peer-reviewed and published.
In the planning stages of the study, researchers should consider carefully whether individual functional MRI results will be shared with health providers or family members. A number of factors—including uncertainty regarding functional MRI results and patient prognosis, and the need to preserve scientific validity—may argue against disclosure of individual results in a particular study. If individual research results are to be shared, the study protocol should contain an adequate plan outlining when and with whom results will be shared. We believe that the treating neurologist is in the best position to integrate prognostically relevant functional MRI findings with standard clinical measures to derive a balanced assessment of the patient's prognosis. The nature of the functional MRI results, in terms of preserved neural networks and cognitive functions, as well as the evidence base at the time of the study correlating such findings with neurological recovery will be key in this determination. Importantly, in studies in which the primary objective is determining the prognostic value of functional MRI in acute coma, the scientific ends of the study may require either a protocolized approach to withdrawal of life-sustaining therapy or blinding the treating physician to functional MRI results. Both approaches may serve to avoid confounding the study's outcome measure.
Individual research results should not be routinely shared with family members. We have argued elsewhere that individual research results should only be shared when four criteria are satisfied: (i) disclosure doesn’t undermine the scientific validity of the study; (ii) the results are informative and reasonably reliable; (iii) the potential benefits of disclosure outweigh the potential harms; and (iv) the participant (or his or her surrogate) consents to be informed of the results ( Graham et al. , 2015 ). Thus, the decision to share individual research results will depend on the study question, study design and the evidence base supporting functional MRI as a prognostic measure. Researchers who plan to share individual functional MRI results with family members should reference these criteria when justifying this decision in the study protocol. Additionally, the protocol should present a detailed plan as to the timing of disclosure, who will disclose the results and answer any questions, and the resources that will be available to support families receiving study results.
Conclusion
In this article we present the first ethical analysis of functional MRI research in acutely comatose patients in the intensive care unit. Determining the prognosis of the acutely comatose patient is a difficult challenge for the critical care physician, and novel prognostic indicators of neurological recovery are urgently needed. Functional MRI holds considerable promise as evidence of preserved neural networks or cognitive function may predict a good patient outcome. Designing and conducting functional MRI studies in this context raises serious technical and ethical challenges. In this paper, we have outlined six ethical issues that ought to be addressed by researchers and research ethics committees.
Acknowledgements
The authors thank Anthony Belardo for his assistance editing the manuscript, and two anonymous reviewers for their helpful comments.
Funding
This work was supported by the Canadian Institutes of Health Research (grant number MOP133705). CW holds a Tier I Canada Research Chair and AMO holds a Canada Excellence Research Chair.
References
- Choi HK, Shin SD, Ro YS, Kim do K, Shin SH, Kwak YH . A before- and after-intervention trial for reducing unexpected events during the intrahospital transport of emergency patients . Am J Emerg Med 2012. ; 30 : 1433 – 40 . [DOI] [PubMed] [Google Scholar]
- Coleman MR, Davis MH, Rodd JM, Robson T, Ali A, Owen AM, et al. . Towards the routine use of brain imaging to aid the clinical diagnosis of disorders of consciousness . Brain 2009. ; 132 : 2541 – 52 . [DOI] [PubMed] [Google Scholar]
- Fanara B, Manzon C, Barbot O, Desmettre T, Cappelier G . Recommendations for the intra-hospital transport of criticially ill patients . Crit Care 2010. ; 14 : R87 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gofton TE, Chouinard PA, Young GB, Bihari F, Nicolle MW, Lee DH, et al. . Functional MRI study of the primary somatosensory cortex in comatose survivors of cardiac arrest . Exp Neurol 2009. ; 217 : 320 – 7 . [DOI] [PubMed] [Google Scholar]
- Graham M, Weijer C, Peterson A, Naci L, Cruse D, Fernández-Espejo D, et al. . Acknowledging awareness: Informing families of individual research results for patients in vegetative states . J Med Ethics 2015. ; 41 : 534 – 8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig MA, Holt JL, Ernst T, Buchthal SD, Nakagawa K, Stenger VA, et al. . MRI default mode network connectivity is associated with functional outcome after cardiopulmonary arrest . Neurocrit Care 2014. ; 20 : 348 – 57 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikell CB, Banks GP, Frey HP, Youngerman BE, Nelp TB, Karas PJ, et al. . Frontal networks associated with command following after hemorrhagic stroke . Stroke 2015. ; 46 : 49 – 57 . [DOI] [PubMed] [Google Scholar]
- Monti MM, Vanhaudenhuyse A, Coleman MR, Boly M, Pickard JD, Tshibanda L, et al. . Willful modulation of brain activity in disorders of consciousness . N Engl J Med 2010. ; 362 : 579 – 89 . [DOI] [PubMed] [Google Scholar]
- Nishimura A, Carey J, Erwin PJ, Tilburt JC, Murad MH, McCormick JB . Improving understanding in the research informed consent process: a systematic review of 54 interventions tested in randomized control trials . BMC Med Ethics 2013. ; 14 : 28 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton L, Hutchison RM, Young GB, Lee DH, Sharpe MD, Mirsattari SM . Disruptions of functional connectivity in the default mode network of comatose patients . Neurology 2012. ; 78 : 175 – 81 . [DOI] [PubMed] [Google Scholar]
- Sandroni C, Cavallaro F, Callaway CW, Sanna T, D'Arrigo S, Kuiper M, et al. . Predictors of poor neurological outcome in adult comatose survivors of cardiac arrest: a systematic review and meta-analysis. Part 1: patients not treated with therapeutic hypothermia . Resuscitation 2013a. ; 84 : 1310 – 23 . [DOI] [PubMed] [Google Scholar]
- Sandroni C, Cavallaro F, Callaway CW, D'Arrigo S, Sanna T, Kuiper MA, et al. . Predictors of poor neurological outcome in adult comatose survivors of cardiac arrest: a systematic review and meta-analysis. Part 2: Patients treated with therapeutic hypothermia . Resuscitation 2013b. ; 84 : 1324 – 38 . [DOI] [PubMed] [Google Scholar]
- Schmidt MH, Marshall J, Downie J, Hadskis MR . Pediatric magnetic resonance research and the minimal-risk standard . IRB 2011. ; 33 : 1 – 6 . [PubMed] [Google Scholar]
- Silverman HJ, Luce JM, Lanken PN, Morris AH, Harabin AL, Oldmixon CF, et al. . Recommendations for informed consent forms for critical care clinical trials . Crit Care Med 2005. ; 33 : 867 – 82 . [DOI] [PubMed] [Google Scholar]
- Stevens RD, Sutter R . Prognosis in severe brain injury . Crit Care Med 2013. ; 41 : 1104 – 23 . [DOI] [PubMed] [Google Scholar]
- Turgeon AF, Lauzier F, Simard JF, Scales DC, Burns KE, Moore L, et al. . Mortality associated with withdrawal of life-sustaining therapy for patients with severe traumatic brain injury: a Canadian multicentre cohort study . CMAJ 2011. ; 183 : 1581 – 8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weijer C, Miller PB . When are research risks reasonable in relation to anticipated benefits? Nat Med 2004. ; 10 : 570 – 3 . [DOI] [PubMed] [Google Scholar]
- Young GB, Schiff ND . Disorders of consciousness . In: Filippi M, Simon JH , editors. Imaging acute neurologic disease . Cambridge: : Cambridge University Press; ; 2014. . p. 1 – 18 . [Google Scholar]


