Abstract
Background
Transfusion-associated circulatory overload is characterised by acute respiratory distress, tachycardia, increased blood pressure, acute pulmonary oedema and/or evidence of positive fluid balance occurring within 6 hours after transfusion. Transfusion-associated circulatory overload is a serious, underreported reaction, which makes this iatrogenic condition difficult to prevent. We present an audit of patients admitted to a medical emergency unit, aiming to investigate: (i) the incidence of transfusion-associated circulatory overload; and (ii) whether cases were reported to the haemovigilance system. The clinical implications are discussed within the frame of the Early Warning Score.
Methods
We conducted a retrospective audit of electronic hospital medical records of patients receiving blood transfusion in a single medical emergency unit. Patients were admitted during a 6-month period and data on symptoms and vital signs were extracted from the records.
Results
Of 4,353 consecutively admitted patients, 156 patients were transfused with a total of 411 blood components. The audit identified five cases of transfusion-associated circulatory overload (incidence 3.2%) and four cases of transfusion-associated dyspnoea. Vital signs and changes in dyspnoea and blood pressure were registered within the frame of the Early Warning Score, and one case was documented as being transfusion-related in the medical record. No cases were reported to the haemovigilance system.
Discussion
The incidence of transfusion-associated circulatory overload in acute emergency patients was similar to that in other clinical studies. Lack of recognition and reporting was marked, even though changes in vital signs were monitored in the context of the Early Warning Score. This study points to a missing link in the transfusion chain, namely recognising the vital signs of circulatory overload during or shortly after transfusion as being a serious adverse transfusion reaction.
Keywords: TACO, blood transfusion, chronic diseases, renal failure, early warning
Introduction
In non-bleeding patients, transfusion may be associated with increased morbidity and, more rarely, increased mortality1–3. In the past decade, national haemovigilance systems identified transfusion-associated circulatory overload (TACO) as one of the most serious risks in transfusion medicine4,5. The pathophysiology of TACO originates from volume overload and increased hydrostatic blood pressure, leading to fluid leakage into the alveolar space. The clinical signs and symptoms include dyspnoea, orthopnoea, tachycardia, hypertension, and elevated central venous pressure, which may progress to manifest pulmonary oedema5.
The incidence of TACO is rising, which can partly be explained by more attention being paid to this condition and the related transfusion-related acute lung injury (TRALI), defined as acute dyspnoea with hypoxia and bilateral pulmonary infiltrates during or within 6 hours of transfusion, not due to circulatory overload or other likely causes6. The more consistent reporting to haemovigilance databases2 points to the relevance of integrating a haemovigilance system and a transfusion safety officer in large hospitals, as described by Simon et al.7 However, when comparing the incidences of TACO in haemovigilance reports with those in randomised clinical trials, a gap is seen between the passive reporting to haemovigilance databases and the prospective data collection in such trials. In a review of the incidence and clinical features of TACO in Ireland, Piccin et al. showed that TACO was the most frequent complication of various serious adverse events reported, but was clinically identified by staff in half of the cases identified by surveillance5.
The haemoglobin transfusion trigger is known to influence the incidence of TACO. Hébert et al. found a significantly higher incidence of pulmonary oedema among critically ill patients transfused at a trigger threshold of 9.0 g/dL compared with the incidence in similar patients transfused at 6.9 g/dL3. In another randomised controlled trial, by Villanueva et al., the incidence of TACO among patients with acute upper gastrointestinal bleeding was eight times higher in the liberal transfusion group8.
TACO is considered to be potentially avoidable if risk factors and vital signs are taken into account, both when prescribing and administering transfusions2. However, Piccin et al. found an element of human error, including a lack of good clinical practice in monitoring vital signs, and a lack of knowledge or recognition of early symptoms of imminent volume overload, which potentially worsen the clinical impact of TACO5. Prevention and management of TACO are important safety issues for patients. Nurses play a significant role in the transfusion decision process and in monitoring patients during and after transfusion; however, evidence regarding their bedside practice in recognising TACO is limited9.
In the last decade, several studies showed that acute physical deterioration in hospitalised patients may be preceded by discrete changes in vital signs and level of consciousness, and that such signs may be present 6–24 hours before a severe adverse event occurs10,11. These changes can be used to calculate an Early Warning Score (EWS), which is intended to assist with the detection of patients at risk of deterioration11–13 by connecting changes in physiological vital parameters (e.g. pulse, blood pressure, temperature and respiratory rate) with an algorithm for increased surveillance and medical action13. The EWS has been widely used across countries and specialties11, including in the Medical Emergency Unit (MEU) in which the current study was performed, on a representative, mixed elderly population of acute emergency patients.
In 2012–13 a Patient Blood Management programme was implemented in the hospitals in the Copenhagen Capital region of Denmark, with the purpose of reducing liberal red blood cell transfusion in non-bleeding patients14. During this intervention, the nurses initiated this study in order to investigate: (i) the incidence of TACO among a population of elderly patients with acute medical problems; and (ii) whether TACO cases were reported to the haemovigilance system. We discuss whether the EWS contributes to early recognition of TACO cases in the MEU.
Materials and methods
This was a descriptive study based on retrospective auditing of electronic hospital medical records of patients receiving blood transfusion during their admission to the MEU, a part of the Emergency Department at Bispebjerg Hospital (700 beds), the university hospital of Copenhagen. At the time of data collection, the MEU was a 23-bed unit receiving acutely ill patients aged 16 and above in need of immediate medical assessment and diagnosis. The patients had a large diversity of medical conditions, except acute cardiac or neurological conditions. Physicians on duty or on call from the hospital’s cardiology, internal medicine, gastroenterology and pulmonary departments provided the medical service at the MEU, whereas in-house nursing staff provided the stationary care. Patients generally stayed in the MEU for less than 24 hours. Approximately half of the patients were then discharged to an out-patient clinic, and the other half were transferred to the relevant specialty departments. Patients admitted to the MEU from January 1, 2012 to June 30, 2012 who had received blood transfusions (red blood cells, platelets or fresh-frozen plasma) during this admission were eligible, and these cases were identified in the hospital’s patient information system. Transfused patients were identified from the blood bank’s IT system, which is 99% precise, as Danish law requires traceability from donor to recipient. Detailed clinical information (e.g., demographics, diagnosis, comorbidities, haemoglobin concentration, transfusion indication, blood transfusions, complications, vital signs, medical treatment) was manually retrieved from the electronic medical records, and entered into paper audit forms and finally an EXCEL spreadsheet (Microsoft, Copenhagen, Denmark). The Charlson Comorbidity Index15, which predicts the 1-year mortality for a patient who may have a range of comorbid conditions (a total of 22 conditions), such as heart disease, autoimmune immunodeficiency syndrome, or cancer, was calculated on the basis of data gathered from the medical records.
Identifying transfusion-associated circulatory overload and vital signs
TACO is a clinical diagnosis and no final consensus exists concerning its diagnostic criteria2,16,17. In this study, the International Society of Blood Transfusion (ISBT, www.isbtweb.org) criteria were applied to categorise data and identify TACO. Accordingly, TACO was characterised by any four of the following symptoms occurring within 6 hours after completion of a transfusion: acute respiratory distress, increased blood pressure, tachycardia, onset or exacerbation of acute pulmonary oedema (verified by chest X-ray, if possible), and a positive fluid balance. Importantly, any other cause of pulmonary oedema must be excluded (Table I)6. Incidents emerging more than 6 hours after transfusion but within 24 hours were classified as transfusion-associated dyspnoea (TAD)6.
Table I.
Current International Society of Blood Transfusion criteria for transfusion-associated circulatory overload6.
| Any four of the following within 6 hours of transfusion |
|---|
| Acute respiratory distress |
| Tachycardia |
| Increased blood pressure |
| Acute or worsening pulmonary oedema |
| Evidence of positive fluid balance |
We defined respiratory distress as a respiratory rate above 20 breaths per minute, tachycardia as 100 or more beats per minute, increased blood pressure as a systolic pressure of more than 140 mmHg and a diastolic pressure over 90 mmHg, and positive fluid balance as a minimum +1,000 mL. These definitions are pragmatic, except for the definition of hypertension, which was based on the review of TACO by Liebermann et al.18 and correlates with European guidelines for treating hypertension19. Patients with clinical deterioration, thus triggering intensified levels of nursing attention and/or medical observation within 24 hours after transfusion, were identified based on EWS data (Table II). The EWS was applied to all MEU patients, with no specific thresholds for blood transfusion20,21. Any medical treatment given for circulatory overload was recorded, as was therapeutic outcome, morbidity, and mortality possibly related to TACO. Data were independently extracted and analysed by two nurses: a nurse with expert training in transfusion auditing (FG) and a clinical nurse specialist (MR) from the MEU. Suspected cases of TACO and other pulmonary and/or severe complications were evaluated and validated by a specialist transfusion medicine specialist (AN).
Table II.
Modified Early Warning Score (MEWS).
| MEWS | 3 | 2 | 1 | 0 | 1 | 2 | 3 |
|---|---|---|---|---|---|---|---|
| Systolic blood pressure (mmHg) | <70 | 71–80 | 81–100 | 101–199 | ≥200 | ||
| Heart rate (bpm) | <40 | 41–50 | 51–100 | 101–110 | 111–129 | ≥130 | |
| Respiratory rate (bpm) | <9 | 9–14 | 15–20 | 21–29 | ≥30 | ||
| Temperature (°C) | <35 | 35–38.4 | ≥38.5 | ||||
| AVPU score | Alert | Reacting to Voice | Reacting to Pain | Unres-ponsive |
With permission from Subbe et al. 200113.
Statistics
We used descriptive statistics for categorical data and numerical data are presented as medians with ranges. No power calculation was made prior to the audit to determine the population sample size and no statistical tests (p values) were performed to compare the TACO cases and the background population of transfused recipients. Ninety-five percent confidence intervals (95% CI) were added to incidences of transfusion reactions.
Results
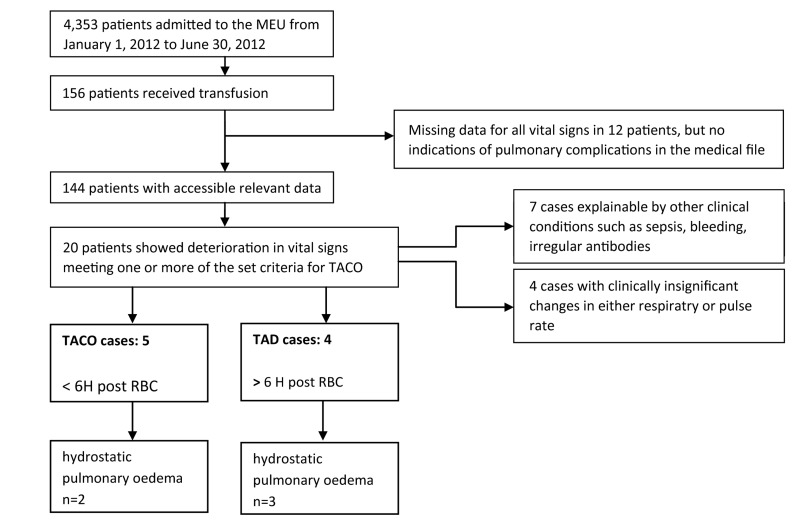
A total of 4,353 consecutive patients were admitted to the MEU during the study period from January 1, 2012 to June 30, 2012. No patients suffered from acute or major bleeding. The 156 patients who received blood transfusions were admitted within the following diagnostic categories of internal medicine: endocrinology (n=64, 41.0%), gastroenterology (n=38, 24.4%), pulmonary medicine (n=36, 23.0%) and cardiology (n=18, 11.5%). A total of 411 transfusion components were administered (395 units of red blood cells, two units of pooled platelet concentrates, and 14 units of FFP - including two units given to one patient, with an International Normalised Ratio of 6–7, to reverse the effects of warfarin). Based on transfusion tracking labels, all blood components were administered within the region’s standard maximum timeframe of 4 hours from delivery. Figure 1 shows an outline of the audit. Table III lists the patients’ characteristics. The median age of all the study participants was 75 years. The majority (73%) had one or more comorbidities. The average haemoglobin level on admission, prior to the first transfusion, was 7.4 g/dL. No patients were described as hypervolaemic on admission and no pre-risk assessments of potential transfusion-related complications were noted in the records of any patients. The EWS data coverage for documentation of vital signs was above 85% during the first 24 hours of observation.
Figure 1.
Outline for the audit.
MEU: Medical Emergency Unit; TACO: transfusion-associated circulatory overload; RCB: red blood cell transfusion; TAD: transfusion-associated dyspnoea.
Table III.
Population characteristics (n=156).
| Gender, n (%) | |
|---|---|
| Female | 94 (60%) |
| Male | 62 (40%) |
|
| |
| Age: median (range), years | 75 (23–98) |
|
| |
| Charlson’s comorbidity index, n (%)15 | |
| Charlson’s index=0 | 41 (27) |
| Charlson’s index=1 | 32 (21) |
| Charlson’s index=2 | 42 (27) |
| Charlson’s index=3 | 18 (12) |
| Charlson’s index=4 | 16 (10) |
| Charlson’s index >5 | 7 (4) |
|
| |
| Haemoglobin at admission: mean (SD), g/dL | 7.4 (1.30) |
|
| |
| Blood component transfusion: n | 411 |
| Red cells: total (median; range per person) | 395 (2; 1–6) |
| Fresh-frozen plasma: total (median; range per person) | 14 (2; 1–4) |
| Pooled platelet concentrates: total | 2 |
|
| |
| Vital signs at onset of transfusion | |
| Respiratory rate <20*: n | 103 |
| Respiratory rate >20*: n | 33 |
| Tachycardia, no†: n | 118 |
| Tachycardia, yes†: n | 21 |
| Hypertension, no‡: n | 129 |
| Hypertension, yes‡: n | 4 |
|
| |
| Pulmonary oedema at admission: n | 0 |
Not documented n= 20;
Not documented n= 17;
Not documented n=23.
SD: standard deviation; n: number.
No other clinical data or record entries suggested any impact of blood transfusion on morbidity or deterioration among patients with missing documentation on vital signs. Data on fluid balance were at best scanty or nonexistent in most cases. For some patients, data regarding prescribed intravenous (IV) fluids were written in their medical records, but no reliable records could be found on the amount of IV fluid administered to the patients.
Transfusion-related reactions occurred in seven women and two men, comprising five definitive TACO cases (3.2%) (95% CI: 0.005–0.059) and four TAD (2.5%) (95% CI: 0.001–0.049). Overall, these reactions involved 5.7% of the transfusion recipients (95% CI: 0.021–0.085) and their incidence was 2.19 (95% CI: 0.011–0.043) per 100 transfusions. One case of TAD developed pulmonary stasis verified by X-ray after receiving 2,000 mL IV fluids and two units of red blood cells within 15 hours without any changes in vital signs detected (Table IV: TAD4).
Table IV.
Vital signs in patients who developed transfusion-associated circulatory overload or transfusion-associated dyspnoea prior to and after red blood cell transfusion.
| Admission diagnosis | Charlson’s index | Hb at transfusion* (RBC) | BP at transfusion onset | HR at transfusion onset | Dyspnoea (RR) at transfusion onset | RBC provided | Dyspnoea exacerbated (RR) | Tachycardia exacerbated/(HR) | Hypertension exacerbated/BP | Pulmonary oedema | Renal dysfunction: serum creatinine >90 μmol/L ** | Treatment | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Transfusion-associated circulatory overload (TACO) (Median age: 88 years; range, 68–95) | |||||||||||||
| TACO1 | COPD. dyspnoea | 2 | 7.8 | 180/95 | 112 | Yes (28) | 2 | Yes (38) | Yes (160) | Yes 205/120 | No/rhonchi | 83 | Solumedrole IV |
| TACO2 | COPD. septicaemia | 1 | 9.1 | 91/53 | 105 | Yes (25) | 1 | Yes (40) | Yes (160) | Yes 178/100 | Yes/desaturation | 101↑ | Furosemide 80 mg IV |
| TACO3 | Anaemia | 0 | 4.3 | 135/55 | 80 | Yes (25) | 2 | Yes (28) | No (93) | Yes 186/95 | Yes | 78 | Furosemide 40 mg IV |
| TACO4 | Congestive heart failure | 1 | 7.5 | 130/58 | 88 | No (16) | 1 | Yes (40) | No (90) | Yes 172/85 | No/stridor | 127↑ | Nitroglycerine/upright position |
| TACO5 | Congestive heart failure | 2 | 8.5 | 170/115 | 85 | No (17) | 1 | Yes (36) | No (123) | Yes 250/100 | No | 87 | Furosemide/nitroglycerine |
| Transfusion-associated dyspnoea (TAD) (Median age: 86 years; range, 81–98) | |||||||||||||
| TAD1 | Congestive heart failure | 3 | 8.6 | 135/68 | 61 | Yes (23) | 2 | Yes (33) | No (88) | No (172/82) | Yes¶ | 248↑ | Furosemide 40×3 mgi IV, nitroglycerine |
| TAD2 | Pneumonia | 2 | 7.2 | <140/90 | <100 | Yes (25) | 2 | Yes (36) | Yes (110) | Yes 212/109 | Yes¶ | 116↑ | Furosemide 80 – 160 mg IV |
| TAD3 | Congestive heart failure | 1 | 6.7 | 132/88 | 88 | No (20) | 3 | Yes (>26) | No (82) | No (125/60) | No/desaturation** | 47 | Nasal oxygen/furosemide IV |
| TAD4 | Infection/dehydration | 0 | 4.6 | <85/50§§ | <100 | Yes (36)§§ | 5 | No (18) | No (43) | No (100/55) | Yes||| | 149↑ | (See text note) |
Haemoglobin in g/dL at onset of transfusion; RBC: red blood cells; RR: respiratory rate; HR: heart rate; BP: blood pressure; ¶ 20–24 hours after transfusion;
oxygen desaturation;
dyspnoea on admission;
pulmonary congestion following 2 RBC units;
serum creatinine reference value (50–90 μmol/L).
The median age of patients with TACO or TAD was 88 years, whereas it was 75 in the total study population. The haemoglobin trigger was similar between TACO and TAD cases (7.14 g/dL; SD 1.70) and the total study population (7.4 g/dL; SD 1.80). Red blood cells were the most frequent blood component to be transfused. TACO and TAD cases in this audit were related solely to red blood cell units transfused for low haemoglobin levels: below 8.0 g/dL in six of the nine (67%) cases, and for higher haemoglobin levels in the remaining three cases. There was no difference in average pre-transfusion haemoglobin levels between TACO or TAD cases and the whole population of transfused recipients.
Ninety percent (90%) of patients with TACO or TAD had at least one comorbid condition (Charlson Comorbidity Index ≥1); this prevalence of comorbid conditions did not differ statistically from that in the study group population without TACO or TAD.
The clinical signs most frequently occurring in patients with TACO were dyspnoea and raised blood pressure. Five cases of manifest pulmonary oedema (X-ray verified) were identified in TACO or TAD cases with renal dysfunction, as judged by the serum creatinine levels found in four. No immediate deaths occurred in the course of transfusions or TACO or TAD reactions. Treatment with diuretics and/or steroids and nitroglycerine was provided in all TACO or TAD cases. Only one case of TACO was correctly identified as such. None of the cases was reported to the haemovigilance system.
Discussion
By retrospective audit, this study showed that 5.7% (n=9) of transfused patients in a MEU developed TACO or TAD. This is fairly consistent with findings from a large, retrospective study of 129,839 hospitalised patients, in which the prevalence of fluid overload including TACO was 3.2%22, and other clinical studies in anaesthetised patients or patients admitted to an intensive care unit in which the prevalences were from 3.0 to 6.0%23,24. In accordance with Piccin et al.5 and Clifford et al.23, we found that older age appeared to be associated with increased risk of TACO or TAD. One TACO case was confirmed as such in the patient’s records, but otherwise there were no signs indicating that the cases of clinical deterioration had been related to the prior transfusion. We used the definitions of TACO/TAD proposed by the ISBT6, although the updated definitions of TACO used by the Serious Hazards of Transfusion (SHOT)25 propose that cases meeting the ISBT definition of TACO, but appearing more than 6 hours after transfusion, may be called “TACO beyond 6 hours”. If applying this definition, the TAD2 case in our study would be “TACO beyond 6 hours”, and thus six cases would be labelled TACO and three cases TAD. The incidence of TACO in this audit is multiple times higher than those registered in Danish and nationwide haemovigilance databases2,4,5. In 2012, 2013 and 2014, TACO was the second most reported transfusion-related adverse reaction in the Danish haemovigilance database with three, 11, and two cases reported, respectively, out of 250,000–300,000 blood transfusions administered annually26. None of the TACO or TAD cases in this study had been reported to the Danish haemovigilance database, which reflects the significant gap and underreporting of transfusion-related adverse reactions between surveillance and clinical investigations2,5,22,23.
This audit was performed in a MEU with an implemented system for collecting the EWS. We noted that changes in dyspnoea and blood pressure were the two vital parameters most frequently involved in TACO or TAD. However, in three of the five cases of TACO (60%) the patients were dyspnoeic (respiratory rate >20) before red blood cell transfusion, and despite a rapid increase in the respiratory rate this did not affect the EWS score because of the threshold for dyspnoea in the current EWS system13. In only two of the five cases (40%) did the blood pressure reach the EWS threshold (>200 mmHg systolic) which would have increased the EWS score by one point even though physiological changes in blood pressure were detected in all five (100%) TACO cases and in two (50%) of the cases of TAD. Of clinical importance, we found that five of the nine cases (55%) of TACO/TAD had markedly elevated serum creatinine on the day of transfusion, which is in line with findings of renal dysfunction in 44% of patients in a retrospectively analysed cohort of 100 TACO cases18. Moreover our study showed that data on fluid balance were lacking, thus representing another important shortfall in quality, both relating to fluid balance and renal function in general and with a potential bearing on the prevention of TACO and TAD in particular. The UK SHOT databases from 2008–2010 similarly show absent documentation on fluid data in 42/92 (45.7%) patients27. The fact that positive fluid balance is a major risk factor for developing TACO clearly points to a missing link in the chain, and underscores the importance of improved clinical awareness and performance in nursing clinical practice. Collectively, our data indicate that the EWS tool in its present form is unlikely to detect TACO among acutely ill medical patients and that MEU patients have a diverse group of medical conditions that may reach the EWS trigger threshold for various reasons other than those related to blood transfusion12,28. TACO is a significant complication and should be picked up by monitoring the course of a transfusion regularly, regardless of the EWS. The present study did, however, reveal that the MEU staff acted upon clinical signs and provided medical treatment for all the cases of TACO/TAD and pulmonary oedema, although they did not recognise transfusion as being causative.
The widespread implementation of the EWS as the general assessment tool for clinical deterioration prompted us to investigate its usefulness for the detection of TACO, although we could not subsequently prove that the EWS actually contributed to the recognition of TACO or TAD. Therefore, and in order to improve pre-transfusion risk assessment and monitoring for patients in need of blood components, we recommend that clinicians pay much more attention to the recent TACO checklist from SHOT, which may easily guide clinicians to prevent future cases of TACO25.
The retrospective design of this study limits insight into the relation between the staffs’ reaction and response to changes in vital signs and the emergence of TACO and TAD as recognised clinical conditions10,11,28. Moreover, the relatively limited sample size makes it difficult to prove cause-effect relationships and to provide precise estimates of incidences and effects, such as mortality rates. Efforts were made in the present study to prevent observer bias by double data extraction and by strictly defining the ISBT criteria for TACO and TAD before extracting and analysing the data6. On the other hand, applying the ISBT criteria may have caused us to overlook other potential adverse circulatory effects of transfusions (such as silent cardiac ischaemia), and all non-circulatory transfusion adverse effects.
This study also has strengths. It covered the entire population admitted to the hospital’s MEU for 6 months, and identified all transfused patients because of the high level of traceability in the patient administrative system and the blood bank’s IT system. There was a relatively high level of documentation in the records regarding the patients’ vital parameters, EWS and medication (except for fluid balance). This allowed a relatively detailed description of the clinical situation surrounding these TACO and TAD cases.
Transfusion medicine, estimation of individual patients’ risk factors, monitoring during and after transfusion, and combining these observations may be viewed as marginal in nurses’ natural curriculum. The present investigation advocates for an urgent need to prospectively investigate the effects of nurses’ basic assessment competences and coordinated adequate responses29 to, for example, EWS triggers on TACO development. This may represent a challenge for MEU with their wide diversity of patients and diagnoses, amplified by short-term consultative visits by physicians across clinical specialties. However, it may also represent an opportunity to improve transfusion practice and early detection of transfusion-related serious adverse reactions, thereby potentially preventing these clinically significant iatrogenic complications.
Conclusions
TACO is a potentially life-threatening event and clinicians should be aware of this before prescribing blood components. An audit showed that the incidence of TACO in the medical emergency population was similar to that found previously in clinical trials, and that underreporting was marked. Irrespectively of use of the EWS and the documented detection and management of clinical deterioration, the study points to a missing link in the transfusion chain, namely recognising clinical deterioration during or shortly after transfusion, as being a serious adverse transfusion reaction. By addressing this, future cases of TACO and their associated clinical consequences could potentially be avoided. A haemovigilance officer should be in place in larger university hospitals in order to improve detection, registration and prevention of severe circulatory adverse reactions to transfusion.
Acknowledgements
The Authors would like to acknowledge the staff and leaders at the Department of Medicine, Bispebjerg University Hospital, Copenhagen for making the clinical audit possible in order to enhance clinical awareness in transfusion practice.
Footnotes
Ethics approval and consent to participate
The study was approved by the Danish Data Protection Agency (J. No. 30-1299). The hospital management provided institutional approval. The data were based on anonymous clinical auditing and the regional ethics committee of Copenhagen waived the need for consent (journal number H-4-2014-FSP).
Authorship contributions
All Authors contributed substantially to the study’s conception and design, as well as to the acquisition or analysis and interpretation of data. The first (FG), second (AN) and last author (TM) analysed the data, drafted the manuscript and discussed the content and corrections with all co-authors. FG and M-BR collected clinical data from patients’ records. The senior transfusion medical specialist (AN) validated transfusion reactions. CR, M-BR, FG and JS facilitated institutional resources and gave educational feedback to staff at scheduled meetings during the study period to support clinical improvement and implementation of transfusion and EWS guidelines.
The Authors declare no conflicts of interest.
References
- 1.Johansson PI, Stensballe J, Oliveri R, et al. How I treat patients with massive hemorrhage. Blood. 2014;124:3052–8. doi: 10.1182/blood-2014-05-575340. [DOI] [PubMed] [Google Scholar]
- 2.Bolton-Maggs PH, Cohen H. Serious Hazards of Transfusion (SHOT) haemovigilance and progress is improving transfusion safety. Br J Haematol. 2013;163:303–14. doi: 10.1111/bjh.12547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hebert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999;340:409–17. doi: 10.1056/NEJM199902113400601. [DOI] [PubMed] [Google Scholar]
- 4.Bolton-Maggs PH. Conference report: the 2015 SHOT symposium and report - what’s new? Transfus Med. 2015;25:295–8. doi: 10.1111/tme.12257. [DOI] [PubMed] [Google Scholar]
- 5.Piccin A, Cronin M, Brady R, et al. Transfusion-associated circulatory overload in Ireland: a review of cases reported to the National Haemovigilance Office 2000 to 2010. Transfusion. 2015;55:1223–30. doi: 10.1111/trf.12965. [DOI] [PubMed] [Google Scholar]
- 6.Popovsky MRP, Schipperus M, Stainsby D, et al. Proposed standard definitions for surveillance of non infectious adverse transfusion reactions. 2011. [Accessed on 24/11/2015]. Available at: http://www.isbtweb.org/fileadmin/user_upload/Proposed_definitions_2011_surveillance_non_infectious_adverse_reactions_haemovigilance_incl_TRALI_correction_2013.pdf.
- 7.Simon TL, McCullough J, Snyder EL, et al. Rossi’s Principles of Transfusion Medicine. 5th edition. Chichester, West Sussex; Hoboken, NJ: John Wiley & Sons Inc; 2016. [Google Scholar]
- 8.Villanueva C, Colomo A, Bosch A, et al. Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med. 2013;368:11–21. doi: 10.1056/NEJMoa1211801. [DOI] [PubMed] [Google Scholar]
- 9.Andrzejewski C, Jr, Popovsky MA, Stec TC, et al. Hemotherapy bedside biovigilance involving vital sign values and characteristics of patients with suspected transfusion reactions associated with fluid challenges: can some cases of transfusion-associated circulatory overload have proinflammatory aspects? Transfusion. 2012;52:2310–20. doi: 10.1111/j.1537-2995.2012.03595.x. [DOI] [PubMed] [Google Scholar]
- 10.McGaughey J, Alderdice F, Fowler R, et al. Outreach and Early Warning Systems (EWS) for the prevention of intensive care admission and death of critically ill adult patients on general hospital wards. Cochrane Database Syst Rev. 2007:CD005529. doi: 10.1002/14651858.CD005529.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Alam N, Hobbelink EL, van Tienhoven AJ, et al. The impact of the use of the Early Warning Score (EWS) on patient outcomes: a systematic review. Resuscitation. 2014;85:587–94. doi: 10.1016/j.resuscitation.2014.01.013. [DOI] [PubMed] [Google Scholar]
- 12.Odell M. Detection and management of the deteriorating ward patient: an evaluation of nursing practice. J Clin Nurs. 2015;24:173–82. doi: 10.1111/jocn.12655. [DOI] [PubMed] [Google Scholar]
- 13.Subbe CP, Davies RG, Williams E, et al. Effect of introducing the Modified Early Warning score on clinical outcomes, cardio-pulmonary arrests and intensive care utilisation in acute medical admissions. Anaesthesia. 2003;58:797–802. doi: 10.1046/j.1365-2044.2003.03258.x. [DOI] [PubMed] [Google Scholar]
- 14.van Hoeven LR, Janssen MP, Rautmann G. The collection, testing and use of blood and blood components in Europe: 2012 report. Strasbourg: European Directorate for the Quality of Medicines & Health Care of the Council of Europe (EDQM); 2015. [Accessed on 20/06/2016]. Available at: https://www.edqm.eu/sites/default/files/the_collection_testing_and_use_of_blood_and_blood_components_in_europe_2012_report.pdf. [Google Scholar]
- 15.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 16.Gajic O, Gropper MA, Hubmayr RD. Pulmonary edema after transfusion: how to differentiate transfusion-associated circulatory overload from transfusion-related acute lung injury. Crit Care Med. 2006;34(5 Suppl):S109–13. doi: 10.1097/01.CCM.0000214311.56231.23. [DOI] [PubMed] [Google Scholar]
- 17.Renaudier P, Rebibo D, Waller C, et al. [Pulmonary complications of transfusion (TACO-TRALI)]. Transfus Clin Biol. 2009;16:218–32. doi: 10.1016/j.tracli.2009.04.008. [In French.] [DOI] [PubMed] [Google Scholar]
- 18.Lieberman L, Maskens C, Cserti-Gazdewich C, et al. A retrospective review of patient factors, transfusion practices, and outcomes in patients with transfusion-associated circulatory overload. Transfus Med Rev. 2013;27:206–12. doi: 10.1016/j.tmrv.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 19.2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC) ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens. 2013;31:1925–38. doi: 10.1097/HJH.0b013e328364ca4c. [DOI] [PubMed] [Google Scholar]
- 20.Fuhrmann L, Lippert A, Perner A, Ostergaard D. Incidence, staff awareness and mortality of patients at risk on general wards. Resuscitation. 2008;77:325–30. doi: 10.1016/j.resuscitation.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 21.Groarke JD, Gallagher J, Stack J, et al. Use of an admission early warning score to predict patient morbidity and mortality and treatment success. Emerg Med J. 2008;25:803–6. doi: 10.1136/emj.2007.051425. [DOI] [PubMed] [Google Scholar]
- 22.Magee G, Zbrozek A. Fluid overload is associated with increases in length of stay and hospital costs: pooled analysis of data from more than 600 US hospitals. Clinicoecon Outcomes Res. 2013;5:289–96. doi: 10.2147/CEOR.S45873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clifford L, Jia Q, Yadav H, et al. Characterizing the epidemiology of perioperative transfusion-associated circulatory overload. Anesthesiology. 2015;122:21–8. doi: 10.1097/ALN.0000000000000513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li G, Rachmale S, Kojicic M, et al. Incidence and transfusion risk factors for transfusion-associated circulatory overload among medical intensive care unit patients. Transfusion. 2011;51:338–43. doi: 10.1111/j.1537-2995.2010.02816.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bolton-Maggs PHB, editor; Poles D, et al. on behalf of the Serious Hazards of Transfusion (SHOT) Steering Group. The 2015. Annual SHOT Report. 2016. [Accessed on 17/05/2016]. Available at: http://www.shotuk.org/wp-content/uploads/SHOT-2015-Annual-Report-Web-Edition-Final-bookmarked.pdf.
- 26.Annual Dart Report 2014 - Summary. [Accessed on 24/11/15]. Available at: http://dski.dk/files/English-summary-2014.pdf.
- 27.Ball J, Cohen H, Knowles S. A retrospective audit of fluid balance recording in transfusion-associated circulatory overload (TACO) reports analysed by the Serious Hazards of Transfusion (SHOT) scheme. 2011. [Accessed on 17/05/2016]. Available at: http://www.shotuk.org/wp-content/uploads/2011/10/Poster-draft-BBTSfinalHCto-printer.pdf.
- 28.Smith ME, Chiovaro JC, O’Neil M, et al. Early warning system scores for clinical deterioration in hospitalized patients: a systematic review. Ann Am Thorac Soc. 2014;11:1454–65. doi: 10.1513/AnnalsATS.201403-102OC. [DOI] [PubMed] [Google Scholar]
- 29.Moller T, Moser C, Adamsen L, et al. Early warning and prevention of pneumonia in acute leukemia by patient education, spirometry, and positive expiratory pressure: a randomized controlled trial. Am J Hematol. 2016;91:271–6. doi: 10.1002/ajh.24262. [DOI] [PMC free article] [PubMed] [Google Scholar]