Abstract
The primary romantic relationship plays a fundamental role in health maintenance, but little is known about its role in HIV care engagement among young Black men who have sex with men (MSM) living with HIV. We examined how HIV care engagement outcomes (i.e., having a primary healthcare provider, receiving HIV treatment, taking antiretroviral medication, and medication adherence) vary by partnership status (single vs. concordant-positive vs. discordant) in a sample of young Black MSM living with HIV. Results showed mixed findings. Partnership status was significantly associated with HIV care engagement, even after adjusting for individual, social, and structural factors. While partnered men were consistently more likely than their single counterparts to have a regular healthcare provider, to receive recent treatment, and to have ever taken antiretroviral medication, they were less likely to report currently receiving antiretroviral therapy. Moreover, men with a discordant partner reported better adherence compared to men with a concordant or no partner. The association between partnership status and HIV care engagement outcomes was not consistent across the stages of the HIV Care Continuum, highlighting the complexity in how and why young Black men living with HIV engage in HIV healthcare. Given the social context of HIV disease management, more research is needed to explicate underlying mechanisms involved in HIV care and treatment that differ by relational factors for young Black MSM living with HIV.
Keywords: Young Black MSM living with HIV, Primary romantic relationship, Partner serostatus, HIV care engagement
Introduction
Engagement in HIV care is critical for reducing transmission and morbidity [1, 2], yet we know little about factors associated with outcomes of HIV care engagement among young Black men who have sex with men (MSM). Increases in HIV incidence are largely driven by increases among young Black MSM [3]. Relative to any other racial/ethnic groups of MSM, young Black MSM living with HIV fare worse in terms of HIV care engagement, which includes having a primary healthcare provider, currently receiving HIV care and treatment, ever received antiretroviral therapy (ART), currently receiving ART, and ART adherence [4–8]. Evidence on relevant factors in HIV care engagement for young Black MSM is limited and urgently needed to guide efforts to enhance treatment outcomes and reduce racial disparities in the HIV Care Continuum [6, 9].
Few studies have focused specifically on HIV care engagement in the context of the primary relationship [10–14]. The lack of published studies in this area is surprising for several reasons. First, the primary relationship has been shown to play a critical role in the outcomes of other chronic diseases like cancer [15], presumably through processes of close relationships [16] and social support [16–18]. Second, the primary relationship appears to be an important context for understanding HIV-risk particularly among MSM [19]. Third, the primary relationship can be an important component of resiliency that facilitates HIV care engagement for young Black MSM living with HIV [20, 21].
Despite limited research, extant evidence with various populations suggests that the primary romantic relationship is important to outcomes of HIV testing, HIV care retention, ART adherence, and viral suppression [22–29]. For example, couples HIV-testing among serodiscordant couples has been found to be acceptable [30]. A couples-based intervention that focused on the primary romantic relationship showed efficacy in enhancing retention in HIV care and treatment [26]. Better ART adherence was associated with patients’ positive evaluation of the primary relationship, as well as the partner’s belief in treatment efficacy [24]. The primary partner’s report of increases in patient’s ART adherence was found to be significantly associated with patients’ viral suppression [31]. Finally, in a sample of serodiscordant couples, a higher level of relational orientation (i.e., the inclusion of the partner in one’s own self-concept) in both partners was independently and positively associated with viral suppression in the partner living with HIV [29]. These studies altogether suggest the important role of the primary romantic relationship in HIV care engagement outcomes. However, none of these studies on the primary relationship specifically focused on young Black MSM and the myriad social and structural factors that impede optimal outcomes for young Black MSM living with HIV.
Individual risk-associated behaviors do not explain racial HIV disparities for young Black men [32, 33]. Instead, a confluence of social and structural factors sustains racial HIV disparities, and sexual partnership patterns may be fueling the epidemic among young Black MSM living with HIV. Sexual partnerships, combined with suboptimal treatment outcomes related to social and structural barriers in the HIV Care Continuum, confer a higher probability of exposure to HIV to sustain the high prevalence and incidence rates among young Black MSM living with HIV [34–36]. However, the importance of the primary romantic relationship vis-à-vis social and structural barriers to HIV care for young Black MSM living with HIV remains unknown.
To date, no study has focused specifically on young Black MSM living with HIV to examine the significance of the primary relationship across the HIV Care Continuum. Thus, our goal is to determine whether having a primary romantic relationship or not, as well as partner serostatus (HIV-concordant vs. HIV-discordant), is related to HIV care engagement outcomes (i.e., having a primary health-care provider, currently receiving HIV healthcare, ever received ART, currently receiving ART, and ART adherence) in a sample of young Black MSM living with HIV in the context of relevant social and structural barriers to optimal HIV care and treatment.
Methods
Sample and Procedures
Data for analysis were collected as the baseline in an efficacy trial of a community-level HIV prevention intervention for young Black MSM in Dallas and Houston, TX, between 2009 and 2014. The intervention focused on primary prevention; secondary prevention and engagement in HIV healthcare were not addressed by any intervention activities. Six independent cross-sectional surveys, approximately a year apart, were collected in each community to establish a baseline prior to implementation of the intervention. Men met survey eligibility criteria if they were between the ages of 18 and 29, identified as Black or African American, reported sex with another man in the past 12 months, were fluent in English, and lived in either the Dallas or Houston metropolitan areas. For the six cross-sectional surveys combined, 3578 young Black MSM met the inclusion criteria. Of these, 352 (10 %) young Black MSM who self-reported having tested HIV-positive from either Dallas or Houston were included in the present analysis (50 men who participated in more than one survey were only included once, i.e., data from subsequent survey[s] were not used).
Participants were recruited using a modified venue-based time-location sampling protocol modeled after that used for the National HIV Behavioral Surveillance Survey [37], and adapted based on pilot work that established its feasibility in recruiting young Black MSM in these specific communities [38, 39]. Venues included bars, dance clubs, retail establishments, restaurants and cafés, adult bookstores, bath-houses, high-traffic street locations, parks, and other locations of social or religious organizations. Venues where health and/or prevention services were provided, including HIV or other sexually transmitted infection testing, were excluded from the sampling frame. Modifications to the sampling protocol were made: (a) because of cost considerations, at least eight young Black MSM had to enter a venue during a 2 h period for the venue to be included as a sampling location, and (b) venues and sampling periods were selected to maximize representation and efficiency in sampling for a 4 h sampling time frame.
Trained study interviewers approached and screened potential participants who entered a predefined intercept area at each sampling venue. Eighty-eight percent of men who were approached agreed to eligibility screening, and 70% of those men screened eligible completed the survey. Surveys took about 20–30 min to complete. Participants were compensated $30 for completing any portion of the survey. All study procedures were approved by the institutional review board at the home institution of the principal investigator, the data collection subcontractors in Dallas and Houston, and the Centers for Disease Control and Prevention.
Measures
The survey measures included demographic characteristics, self-reported HIV serostatus, length of time since HIV diagnosis, and HIV care engagement. Given the importance of social and structural factors in the HIV-related outcomes among Black MSM, we included the following sociostructural variables in our analysis: educational attainment, employment status, annual income, incarceration history, homelessness, and self-identification as gay. Primary relationship status with a man was ascertained by the survey item, Do you currently have a boyfriend/lover (a male you feel committed to and who you have sex with)? These participants were also asked to report their partner’s HIV serostatus. HIV-discordance refers to a relationship in which the primary romantic partner is HIV-negative.
HIV care engagement was assessed using the following items that corresponded with linkage, retention, ART uptake, and adherence stages in the HIV Care Continuum, rated on a binary, Yes/No, scale: (a) Do you have a primary healthcare provider (someone you see regularly for HIV-related healthcare); (b) Have you received any healthcare or treatment for HIV in the past six months i.e., currently receiving healthcare (c) Have you ever taken any HIV medicines prescribed by a doctor; (d) Are you currently taking any HIV medicine [2]. Participants were also asked, In the past 30 days, how often did you miss taking a dose of any of your HIV medicine(s) rated on a 1–5 Likert-type scale (1, Never, to 5, Very Often) later dichotomized into, Never (i.e., No Missed Doses reported) and all other responses (i.e., Missed Doses reported) for consistency in analyses across items. To preserve meaningful comparisons [2], each item included only those participants who reported, Yes to the previous item (e.g., only men who reported Yes to currently taking any HIV medicine were considered in the analysis of the subsequent item on medication adherence).
Data Analysis
There were two analysis goals. We first examined whether there were differences in HIV care engagement between men who were Single, men with a Concordant partner, and men with a Discordant partner. Simple logistic regression models were conducted to estimate the odds of HIV care engagement with 95% confidence intervals (CIs) to further describe the size of the estimates.
First, we examined the HIV care engagement outcomes by a three-category partnership status variable (Single, HIV-Concordant, and HIV-Discordant). Next, we dichotomized the partnership status variable (Single or in a relationship) to better indicate where the largest differences were found on the first four of the five HIV care engagement outcomes. For the last outcome (No Missed Doses), we dichotomized the partnership variable into men who had a discordant partner versus not, since the largest difference was observed between men with a discordant partner and men who were either single or had a concordant partner.
Second, we examined whether partnership-based differences in HIV care engagement would persist upon adjusting for the effects of sociostructural and individual factors important in HIV-related outcomes for young Black MSM. As suggested by a social epidemiological framework [40], sociostructural factors include educational attainment, employment status, income, history of incarceration, history of homelessness, and sexual orientation, and individual factors include age, city, year of data collection, and time since HIV diagnosis [41].
Results
Sample Characteristics
Of the 350 men who reported their relationship status, 48.9% (171) reported not having a primary romantic relationship partner; 30.3% (106) reported having a HIV-concordant partner; and 20.8% (73) had a HIV-discordant partner (Table 1). Among the men with a primary romantic partner, mean relationship duration was 29.52 months (SD = 36.54, interquartile range = 4–40; Table 1). Engagement in the HIV care and treatment did not differ between city and year (across the six annual cross-sectional assessments), and fluctuations in self-reported HIV prevalence over time were not statistically significant.
Table 1.
Demographic characteristics and HIV care engagement outcomes of young Black men who have sex with men living with HIV in Dallas and Houston, Texas, 2009–2014
| Variable | Categories | na | % | M | SD |
|---|---|---|---|---|---|
| Relational | |||||
| Partnership status (n = 350) | Single | 171 | 48.9 | ||
| In a primary relationship | 179 | 51.1 | |||
| concordant-positive | 106 | 59.2 | |||
| Discordant | 73 | 40.8 | |||
| Individual | |||||
| Age (n = 352) (years) | 24.6 | 2.9 | |||
| 18–20 | 30 | 8.5 | |||
| 21–23 | 104 | 29.5 | |||
| 24–26 | 106 | 30.1 | |||
| 27–29 | 112 | 31.8 | |||
| City | Dallas | 173 | 49.1 | ||
| Houston | 179 | 50.9 | |||
| Survey wave | 2009 | 52 | 14.8 | ||
| 2010 | 66 | 18.8 | |||
| 2011 | 55 | 15.6 | |||
| 2012 | 59 | 16.8 | |||
| 2013 | 58 | 16.5 | |||
| 2014 | 62 | 17.6 | |||
| Time Since HIV Diagnosis (n = 339) | 37.9 | 39.1 | |||
| 0–12 months | 111 | 32.7 | |||
| 13–24 months | 47 | 13.9 | |||
| 25–60 months | 105 | 31.0 | |||
| > 5 years | 76 | 22.4 | |||
| Sociostructural | |||||
| Educational attainment (n = 348) | Grade 11 or less | 70 | 20.1 | ||
| Grade 12 or GED | 103 | 29.6 | |||
| > Grade 12 | 175 | 50.3 | |||
| Employment status (n = 350) | Full-time | 177 | 50.6 | ||
| Part-time | 67 | 19.1 | |||
| Unemployed or disabled | 106 | 30.3 | |||
| Annual income (n = 347) | < $10,000 | 118 | 34.0 | ||
| $10,000–$19,999 | 49 | 14.1 | |||
| $20,000–$39,999 | 109 | 31.4 | |||
| $40,000 or more | 71 | 20.5 | |||
| Incarceration (n = 343) | In past year | 70 | 20.4 | ||
| > 1 year ago | 49 | 14.3 | |||
| Never | 224 | 65.3 | |||
| Homelessness (n = 346) | In past year | 50 | 14.5 | ||
| > 1 year ago | 31 | 9.0 | |||
| Never | 265 | 76.6 | |||
| Sexual orientation (n = 352) | Gay-identified | 285 | 81.0 | ||
| Other-identified | 67 | 19.0 | |||
n may be less than 352 due to missing data by survey item
M mean, SD standard deviation
Of the sample of 352 young Black MSM living with HIV, 86.6% (304) reported having a primary healthcare provider, 81.8% (288) reported currently receiving HIV healthcare, and 67.6% (238) reported that they had ever received ART. Of the 238 men who had ever received ART, 70.6% (168) reported that they were currently receiving ART. Of the 168 men who reported that they were currently receiving ART, 52.4% (88) reported adhering to their HIV medication regimen (i.e., not having missed a dose in the past 30 days).
Main Findings
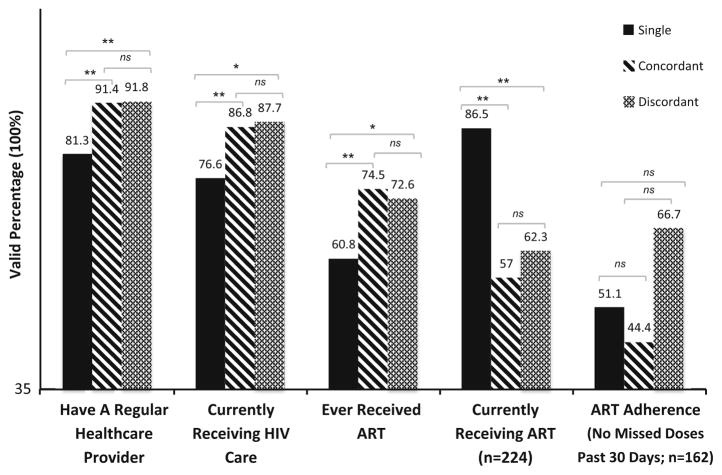
We examined bivariate relationships for each of the five HIV care engagement outcomes with a three-category partnership status variable (Single, HIV-Concordant, and HIV-Discordant; Table 2) and then by a two-category partnership status variable (Table 3). Simple logistic regressions revealed that men with a primary romantic partner were more likely than single men to report having a regular healthcare provider, currently receiving healthcare, and having ever received ART. Among participants who had ever received ART, single men were more likely to report currently receiving ART than men with either a concordant or a discordant partner. In terms of ART adherence among men currently on ART, men with a discordant romantic partner were more likely to report perfect adherence, that is, not missing any doses in the past 30 days relative to men who were single or who had a concordant romantic partner. Single men did not significantly differ from partnered men on adherence; however, ART adherence among single men was more similar to men with a concordant partner than to men with a discordant partner. In other words, on the first four of the five outcomes, the largest difference was observed between single versus partnered men, whereas on the last outcome of ART adherence, the largest difference was observed between men with a discordant partner versus all other men (Fig. 1).
Table 2.
HIV Care engagement by relationship and partnership status (Single, concordant-positive, discordant) among young Black men who have sex with men living with hiv in Dallas and Houston, Texas, 2009–2014
| Outcome | Total n (% Yes) | By partnership status | Simple logistic regression | ||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| n | % Yes | OR | 95 % CI | p | |||
| Have a regular healthcare providera | 349 (88.2) | Single | 171 | 81.3 | 1.00 | ||
| Concordant | 105 | 91.4 | 2.46 | 1.12–5.38 | .05 | ||
| Discordant | 73 | 91.8 | 2.57 | 1.03–6.45 | .05 | ||
| Currently receiving hiv careb | 350 (83.7) | Single | 171 | 76.6 | 1.00 | ||
| Concordant | 106 | 86.8 | 2.01 | 1.03–3.90 | .05 | ||
| Discordant | 73 | 87.7 | 2.17 | 0.99–4.75 | .10 | ||
| Ever received ARTc | 350 (69.3) | Single | 171 | 60.8 | 1.00 | ||
| Concordant | 106 | 74.5 | 1.89 | 1.11–3.22 | .05 | ||
| Discordant | 73 | 72.6 | 1.71 | 0.94–3.11 | .10 | ||
| Currently receiving ARTd | 236 (68.6) | Single | 104 | 86.5 | 1.00 | ||
| Concordant | 79 | 57.0 | 0.21 | 0.10–0.42 | .001 | ||
| Discordant | 53 | 62.3 | 0.26 | 0.12–0.57 | .01 | ||
| ART Adherence (No Missed Doses past 30 days)e | 168 (54.1) | Single | 90 | 51.1 | 1.00 | ||
| Concordant | 45 | 44.4 | 0.77 | 0.37–1.57 | ns | ||
| Discordant | 33 | 66.7 | 1.91 | 0.83–4.40 | ns | ||
n may be less than 352 due to missing data by survey item
OR odds ratio, AOR adjusted odds ratio, CI confidence interval, ART antiretroviral therapy
Discordant versus concordant 1.05 (0.36–3.08)
Discordant versus concordant 1.08 (0.44–2.65)
Discordant versus concordant 0.91 (0.46–1.78)
Discordant versus concordant 1.25 (0.61–2.54)
Discordant versus concordant 0.54 (0.98–6.35)
Table 3.
HIV Care engagement by relationship and partnership serostatus (single, in a relationship) among young Black men who have sex with men living with hiv in Dallas and Houston, Texas, 2009–2014
| Outcome | Partnership status | Simple logistic regression | Multiple logistic regression | ||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| OR | 95 % CI | p | AOR | 95 % CI | p | ||
| Have a regular healthcare provider | Single | 1.00 | 1.00 | ||||
| In a relationship (concordant/discordant) | 2.50 | 1.30–4.81 | .005 | 2.58 | 1.20–5.54 | .02a | |
| Currently receiving HIV care | Single | 1.00 | 1.00 | ||||
| In a relationship (concordant/discordant) | 2.07 | 1.18–3.64 | .01 | 2.21 | 1.14–4.29 | .02b | |
| Ever received ART | Single | 1.00 | 1.00 | ||||
| In a relationship (concordant/discordant) | 1.81 | 1.15–2.85 | .01 | 1.70 | 1.01–2.88 | .05c | |
| Currently receiving ART | Single | 1.00 | 1.00 | ||||
| In a relationship (concordant/discordant) | 0.23 | 0.12–0.44 | < 001 | 0.36 | 0.17–0.79 | .01d | |
| ART adherence (No Missed Doses past 30 days) | Single/concordant | 1.00 | 1.00 | ||||
| Discordant | 2.09 | 0.94–4.65 | .06 | 2.45 | 0.94–6.38 | .07e | |
OR odds ratio, AOR adjusted odds ratio, CI confidence interval, ART antiretroviral therapy
n = 325, Hosmer–Lemeshow goodness of fit test p-value = 0.34
n = 326, Hosmer–Lemeshow goodness of fit test p-value = 0.89
n = 326, Hosmer–Lemeshow goodness of fit test p-value = 0.74
n = 224, Hosmer–Lemeshow goodness of fit test p-value = 0.52
n = 162, Hosmer–Lemeshow goodness of fit test p-value = 0.25
Fig. 1.
Bivariate associations among HIV Care engagement outcomes among single men, men with a concordant-positive partner, and men with a HIV-discordant partner from a sample of young, Black men who have sex with men living with hiv in Dallas and Houston, Texas, 2009–2014. Note: **p ≤ .05; *p ≤ .10; ns statistically non-significant, ART antiretroviral therapy
Adjusting for the effects of individual and sociostructural factors, we found that partnered men were more likely than their single counterparts to have a regular healthcare provider, to receive current HIV care, and to have ever received ART (Table 3). However, the association between having a primary romantic partner and HIV care engagement outcomes was not consistent across the HIV Care Continuum. While partnered men appeared to be better engaged than single men in an earlier stage of HIV care and treatment, they actually reported worse outcomes in later stages: Partnered men were less likely to report current ART compared to single men. On the measure of current ART, men with a discordant partner were more likely to report perfect adherence than either single men or men with a concordant partner; this pattern approached statistical significance in both bivariate and multivariate analyses.
Tables 4, 5, 6, 7 and 8 in Appendices 1–5 show the full simple and multiple logistic regression models with covariates for each of the five outcomes. In the multivariable analyses, no covariate was statistically significant in the presence of Partnership Status except for the outcome, Ever Received ART (Appendix 3), for which time since HIV diagnosis remained a statistically significant covariate.
Discussion
The present study examined the association between having a primary romantic relationship, partner serostatus, and HIV care engagement outcomes in a sample of young Black MSM living with HIV. Results also showed that HIV care engagement outcomes varied meaningfully by partnership status even after controlling for the effects of individual and sociostructural factors. The primary relationship was associated with better engagement in some HIV care engagement outcomes, but not all. In fact, having a primary romantic partner was associated with worse HIV care engagement in terms of current ART, on which single men appeared better engaged. Partner serostatus was also associated with HIV care engagement, such that men with a HIV-discordant primary romantic partner were relatively better at adhering to ART than either single men or men with a HIV-concordant partner. These findings fill a knowledge gap on the importance of the relational context in HIV care engagement, and is the first to do so that focuses on young Black MSM living with HIV.
Over half of the men in our sample reported having a primary romantic partner. In terms of having a healthcare provider, receiving HIV healthcare, and ever received ART, partnered men were better engaged, whereas in terms of currently receiving ART and ART adherence, single men were better engaged. Having a primary romantic partner potentially offers important instrumental as well as emotional support for the HIV-positive partner that enhance his engagement in HIV care and treatment [23, 28]. Notably, the opportunity to engage in dyadic HIV care wherein both HIV-positive partners are involved in each other’s care (e.g., accompanying each other to appointments, establishing routines) may facilitate positive relationship dynamics that enhance HIV care outcomes for both partners, particularly when they make HIV care engagement an explicit relationship goal [21, 27].
Partner serostatus appeared to be an important component of HIV care engagement in this study. Men with a discordant partner were more likely to report perfect ART adherence than men with a concordant partner or no partner; this pattern approached statistical significance in both bivariate and multivariate analyses. Behavioral risk studies with MSM suggest that, at least among men with a primary romantic partner, fear of transmitting HIV to one’s HIV-negative partner, to whom they are committed, may drive ART adherence to achieve viral suppression [42]. That is, men in a discordant relationship may be more motivated and committed to stay adherent than men who are not in a relationship and men in a concordant-positive relationship, where one’s partner is already HIV-positive [42].
Our study findings should be understood in the context of sociostructural factors that produce suboptimal HIV care engagement outcomes among young Black MSM living with HIV. While the majority of the young Black MSM living with HIV in our study had a healthcare provider and received current HIV care, more than a third had never received ART. Of the men who reported past ART, a third were not currently receiving ART. Of the men who were currently receiving ART, only about half reported perfect ART adherence. In order to reduce racial HIV disparities, HIV care engagement interventions must consider sociostructural factors that produce suboptimal HIV care engagement outcomes among young Black men living with HIV in conjunction with proximal factors at the dyadic and individual levels [11, 43].
Although we explored HIV care engagement outcomes only by partnership status rather than relationship dynamics, partnership status may be an indicator of the presence or absence of dynamics and resources involved in social support. For instance, the presence of a relationship partner can be a source of tangible, instrumental support specific to HIV care (e.g., medication organization and monitoring, transportation to medical providers, reminders about appointments) [23] as well as emotional support (e.g., adaptive stress and coping strategies) [20, 44]. By showing the associations between partnership status and HIV care engagement outcomes, our study is among the first to address a gap in the literature on HIV care engagement in the context of the primary romantic relationship.
Limitations
It is important to note that HIV status may be under-reported due to men being unaware of their seropositivity. Moreover, social desirability biases may have skewed participants’ responses on HIV care engagement. We attempted to address underreporting and social desirability effects by making the survey anonymous and using self-administered surveys (CASI) so the person administering the survey did not see individual responses.
Due to the cross-sectional study design of the study, we cannot infer causality. However, our goal was descriptive in nature. We aimed to describe patterns of HIV care engagement among young Black MSM living with HIV vis-à-vis partnership status. Our small sample size may contribute to diminished power to detect meaningful differences, particularly given marginal statistically significant results in the our ART adherence outcome. Also, our analysis was based on two cities in Texas; thus, our results are not generalizable to the US population of young Black MSM living with HIV.
Future Research and Implications for Enhancing HIV Engagement in Care
Engagement in the HIV Care Continuum in the current sample was less than optimal: In terms of past and current ART and adherence, a third to half of the men were less than optimally engaged, respectively. Because of existing racial disparities in HIV prevalence, increases in testing and linkage among young Black MSM living with HIV would not eliminate racial HIV disparities [9, 45]. Therefore, interventions for enhancing access and adherence to ART for young Black MSM living with HIV should be developed as part of the concerted effort to reduce racial HIV disparities.
Indeed, racial disparities in HIV exist at multiple levels of analysis—including at the dyadic level [11]. Understanding and remediating racial disparities in HIV care engagement and treatment among young Black MSM living with HIV require a multilevel approach that captures the complex ways in which individual behaviors, relationship dynamics, community and sociostructural factors interact to produce and perpetuate these disparities [11, 43, 46]. Analyses using multilevel modeling and the actor-partner interdependence model (APIM) can advance our understanding of multilevel factors in HIV care engagement among young Black MSM living with HIV [47].
HIV care engagement is multiply influenced. More work is needed to delineate the processes by which these factors predict HIV care engagement and in order to inform interventions aimed at improving HIV care engagement among young Black MSM. The present study suggests different mechanisms underlying HIV care engagement between men with concordant and discordant primary romantic partners. For example, fear of infecting one’s partner may be an impetus for adhering to ART [28, 48, 49], but more research is warranted in order to understand the various goals and the potential facilitators and barriers of HIV care engagement for intervention development [50]. Men with a concordant-positive primary partner may benefit from interventions that involve both partners in each other’s HIV care that can in turn facilitate emotional and instrumental social support and strengthens relationship dynamics such as a sense of solidarity and intimacy [28, 42]. Given the social context of HIV disease management, relational factors should be considered in future research as part of the complexity and dynamism in how and why young Black men living with HIV engage in HIV care [21, 29].
Acknowledgments
We wish to acknowledge the subcontractors in Dallas and Houston who collected the data, Catherine Troisi, Ph.D. and Paige Wermuth from the University of Texas, Houston and Anne Freeman, MA, Douglas Sheehan, MA, Doug Kershaw, and Stephen Brown, MA from the University of Texas Southwestern. This research was funded by grants from the CDC (5UR6PS000334) and the National Institute for Mental Health (R01MH096690). Dr. Tan was supported by a National Institute of Mental Health (NIMH) Mentored Research Scientist Development Award (K01MH106416).
Appendix 1
See Table 4
Table 4.
Bivariate, multivariable analyses of having a regular healthcare provider and partnership status among young, Black men who have sex with men living with HIV in Dallas and Houston, Texas, 2009–2014
| Variable | Category | N | Bivariatea | Multivariableb | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| % Yes | p | AOR | 95 % CI | |||
| Relational | ||||||
| Partnership status | 0.006 | |||||
| Single | 171 | 81.3 | 1.00 | |||
| In a relationship | 178 | 91.6 | 2.58 | 1.20–5.54 | ||
| Individual | ||||||
| City | 0.715 | |||||
| Dallas | 173 | 87.3 | 1.00 | |||
| Houston | 178 | 86.0 | 0.70 | 0.33–1.48 | ||
| Survey | 0.679 | |||||
| 2009 | 51 | 84.3 | 1.00 | |||
| 2010 | 66 | 83.3 | 0.83 | 0.24–2.80 | ||
| 2011 | 55 | 83.6 | 1.03 | 0.29–3.67 | ||
| 2012 | 59 | 88.1 | 1.57 | 0.40–6.27 | ||
| 2013 | 58 | 87.9 | 1.10 | 0.30–4.06 | ||
| 2014 | 62 | 91.9 | 1.96 | 0.47–8.21 | ||
| Age (years) | 0.439 | |||||
| 18–20 | 30 | 83.3 | 1.00 | |||
| 21–23 | 104 | 82.7 | 1.08 | 0.29–3.96 | ||
| 24–26 | 106 | 89.6 | 1.81 | 0.44–7.36 | ||
| 27–29 | 111 | 88.3 | 1.27 | 0.31–5.26 | ||
| Time since HIV diagnosis | 0.580 | |||||
| 0–12 months | 111 | 87.4 | 1.00 | |||
| 13–24 months | 47 | 87.2 | 0.95 | 0.31–2.94 | ||
| 25–60 months | 104 | 85.6 | 0.59 | 0.25–1.42 | ||
| > 5 years | 76 | 92.1 | 1.47 | 0.48–4.50 | ||
| Sociostructural | ||||||
| Educational attainment | 0.183 | |||||
| < Grade 12 | 70 | 80.0 | 1.00 | |||
| Grade 12 | 102 | 87.3 | 1.64 | 0.55–4.89 | ||
| > Grade 12 | 175 | 89.1 | 1.30 | 0.47–3.61 | ||
| Employment status | 0.048 | |||||
| Full-time | 176 | 90.9 | 1.00 | |||
| Part-time | 67 | 83.6 | 0.60 | 0.22–1.68 | ||
| Unemployed/disabled | 106 | 81.1 | 0.63 | 0.24–1.66 | ||
| Annual income | 0.465 | |||||
| < $10,000 | 117 | 84.6 | 1.00 | |||
| $10,000–$19,999 | 49 | 87.8 | 0.82 | 0.25–2.75 | ||
| $20,000–$39,999 | 109 | 84.4 | 0.52 | 0.19–1.39 | ||
| $40,000 or more | 71 | 91.5 | 0.73 | 0.19–2.76 | ||
| Incarceration | 0.068 | |||||
| In the past year | 69 | 78.3 | 1.00 | |||
| > 1 year ago | 49 | 83.7 | 0.84 | 0.27–2.64 | ||
| Never | 224 | 89.3 | 2.46 | 0.95–6.38 | ||
| Homelessness | 0.341 | |||||
| In the past year | 49 | 85.7 | 1.00 | |||
| > 1 year ago | 31 | 77.4 | 0.35 | 0.08–1.44 | ||
| Never | 265 | 87.5 | 0.93 | 0.30–2.89 | ||
| Sexual orientation | 0.685 | |||||
| Gay-identified | 284 | 87.0 | 1.00 | |||
| Other-identified | 67 | 85.1 | 1.39 | 0.51–3.78 | ||
| Total | 351 | 86.6 | ||||
OR odds ratio, CI confidence interval
P-value is for χ2 statistic for omnibus test assessing relationship between variable and outcome in a simple logistic regression analysis
AOR with 95 % CI (N = 325, Hosmer–Lemeshow goodness of fit test p-value = 0.34)
Appendix 2
See Table 5
Table 5.
Bivariate, multivariable analyses of currently receiving HIV healthcare and partnership status among young, Black men who have sex with men living with HIV In Dallas and Houston, Texas, 2009–2014
| Variable | Category | N | Bivariatea | Multivariableb | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| % Yes | p | AOR | 95 % CI | |||
| Relational | ||||||
| Partnership status | 0.010 | |||||
| Single | 171 | 76.6 | 1.00 | |||
| In a relationship | 179 | 87.2 | 2.21 | 1.14–4.29 | ||
| Individual | ||||||
| City | 0.900 | |||||
| Dallas | 173 | 82.1 | 1.00 | |||
| Houston | 179 | 81.6 | 0.83 | 0.43–1.59 | ||
| Survey | 0.428 | |||||
| 2009 | 52 | 76.9 | 1.00 | |||
| 2010 | 66 | 80.3 | 0.96 | 0.33–2.80 | ||
| 2011 | 55 | 76.4 | 0.95 | 0.32–2.78 | ||
| 2012 | 59 | 83.1 | 1.74 | 0.53–5.76 | ||
| 2013 | 58 | 89.7 | 3.13 | 0.88–11.14 | ||
| 2014 | 62 | 83.9 | 1.26 | 0.40–3.96 | ||
| Age (Years) | 0.448 | |||||
| 18–20 | 30 | 80.0 | 1.00 | |||
| 21–23 | 104 | 79.8 | 0.95 | 0.28–3.17 | ||
| 24–26 | 106 | 86.8 | 1.76 | 0.48–6.47 | ||
| 27–29 | 112 | 79.5 | 0.72 | 0.20–2.68 | ||
| Time since HIV diagnosis | 0.208 | |||||
| 0–12 months | 111 | 76.6 | 1.00 | |||
| 13–24 months | 47 | 85.1 | 2.05 | 0.75–5.62 | ||
| 25–60 months | 105 | 86.7 | 1.53 | 0.70–3.36 | ||
| >5 years | 76 | 85.5 | 2.28 | 0.90–5.77 | ||
| Sociostructural | ||||||
| Educational attainment | 0.868 | |||||
| <Grade 12 | 70 | 80.0 | 1.00 | |||
| Grade 12 | 103 | 81.6 | 1.28 | 0.47–3.48 | ||
| >Grade 12 | 175 | 82.9 | 0.96 | 0.37–2.46 | ||
| Employment status | 0.482 | |||||
| Full-time | 177 | 84.2 | 1.00 | |||
| Part-time | 67 | 79.1 | 0.56 | 0.22–1.43 | ||
| Unemployed/disabled | 106 | 79.2 | 0.84 | 0.35–2.04 | ||
| Annual income | 1.000 | |||||
| <$10,000 | 118 | 81.4 | 1.00 | |||
| $10,000–$19,999 | 49 | 81.6 | 0.71 | 0.25–2.05 | ||
| $20,000–$39,999 | 109 | 81.7 | 0.74 | 0.30–1.86 | ||
| $40,000 or more | 71 | 81.7 | 0.56 | 0.18–1.76 | ||
| Incarcerationc | 0.017 | |||||
| In the past year | 70 | 78.6 | 1.00 | |||
| >1 year ago | 49 | 67.3 | 0.40 | 0.14–1.10 | ||
| Never | 224 | 85.3 | 1.84 | 0.76–4.44 | ||
| Homelessness | 0.536 | |||||
| In the past year | 50 | 84.0 | 1.00 | |||
| >1 year ago | 31 | 74.2 | 0.32 | 0.08–1.23 | ||
| Never | 265 | 81.9 | 0.64 | 0.23–1.80 | ||
| Sexual orientation | 0.674 | |||||
| Gay-identified | 285 | 81.4 | 1.00 | |||
| Other-identified | 67 | 83.6 | 1.61 | 0.65–3.98 | ||
| Total | 352 | 81.8 | ||||
p ≤ .05 are indicated in boldface type
OR odds ratio, CI confidence interval
P-value is for χ2 statistic for omnibus test assessing relationship between variable and outcome in a simple logistic regression analysis
AOR with 95 % CI (N = 326, Hosmer–Lemeshow goodness of fit test p-value = 0.89)
Never versus >1 year ago: OR = 4.63 (95% CI 1.99–10.81)
Appendix 3
See Table 6
Table 6.
Bivariate, multivariable analyses of ever receiving antiretroviral therapy and partnership status among young, Black men who have sex with men living with HIV in Dallas and Houston, Texas, 2009–2014
| Variable | Category | N | Bivariatea | Multivariableb | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| % Yes | p | AOR | 95 % CI | |||
| Relational | ||||||
| Partnership status | 0.010 | |||||
| No partner | 171 | 60.8 | 1.00 | |||
| Have a partner | 179 | 73.7 | 1.70 | 1.01–2.88 | ||
| Individual | ||||||
| City | 0.112 | |||||
| Dallas | 173 | 63.6 | 1.00 | |||
| Houston | 179 | 71.5 | 1.33 | 0.79–2.26 | ||
| Survey | 0.081 | |||||
| 2009 | 52 | 57.7 | 1.00 | |||
| 2010 | 66 | 62.1 | 1.22 | 0.51–2.94 | ||
| 2011 | 55 | 61.8 | 1.29 | 0.53–3.14 | ||
| 2012 | 59 | 71.2 | 2.34 | 0.90–6.09 | ||
| 2013 | 58 | 70.7 | 1.72 | 0.66–4.46 | ||
| 2014 | 62 | 80.6 | 3.20 | 1.18–8.67 | ||
| Age (years) | 0.129 | |||||
| 18–20 | 30 | 66.7 | 1.00 | |||
| 21–23 | 104 | 58.7 | 0.73 | 0.27–1.99 | ||
| 24–26 | 106 | 71.7 | 1.26 | 0.44–3.59 | ||
| 27–29 | 112 | 72.3 | 1.18 | 0.40–3.47 | ||
| Time since HIV diagnosisc | 0.003 | |||||
| 0–12 months | 111 | 55.9 | 1.00 | |||
| 13–24 months | 47 | 70.2 | 1.81 | 0.81–4.05 | ||
| 25–60 months | 105 | 75.2 | 2.11 | 1.11–4.02 | ||
| > 5 years | 76 | 78.9 | 2.56 | 1.20–5.44 | ||
| Sociostructural | ||||||
| Educational attainment | 0.496 | |||||
| < Grade 12 | 70 | 67.1 | 1.00 | |||
| Grade 12 | 103 | 64.1 | 1.13 | 0.51–2.54 | ||
| > Grade 12 | 175 | 70.9 | 0.89 | 0.41–1.94 | ||
| Employment status | 0.351 | |||||
| Full-time | 177 | 70.6 | 1.00 | |||
| Part-time | 67 | 67.2 | 1.38 | 0.63–2.99 | ||
| Unemployed/disabled | 106 | 62.3 | 1.09 | 0.54–2.23 | ||
| Annual income | 0.153 | |||||
| < $10,000 | 118 | 61.9 | 1.00 | |||
| $10,000–$19,999 | 49 | 65.3 | 1.30 | 0.56–3.02 | ||
| $20,000–$39,999 | 109 | 68.8 | 1.20 | 0.57–2.52 | ||
| $40,000 or more | 71 | 77.5 | 1.56 | 0.61–3.99 | ||
| Incarceration | 0.080 | |||||
| In the past year | 70 | 67.1 | 1.00 | |||
| > 1 year ago | 49 | 53.1 | 0.43 | 0.17–1.06 | ||
| Never | 224 | 70.1 | 0.98 | 0.48–2.02 | ||
| Homelessness | 0.939 | |||||
| In the past year | 50 | 68.0 | 1.00 | |||
| > 1 year ago | 31 | 64.5 | 0.68 | 0.23–2.08 | ||
| Never | 265 | 67.5 | 0.93 | 0.41–2.07 | ||
| Sexual orientation | 0.930 | |||||
| Gay-identified | 285 | 67.7 | 1.00 | |||
| Other-identified | 67 | 67.2 | 0.92 | 0.47–1.79 | ||
| Total | 352 | 67.6 | ||||
p ≤ .05 are indicated in boldface type
OR odds ratio, CI confidence interval
P-value is for χ2 statistic for omnibus test assessing relationship between variable and outcome in a simple logistic regression analysis
AOR with 95 % CI (N = 326, Hosmer-Lemeshow goodness of fit test p-value = 0.74)
Multivariable OR and CI: 25–60 months versus 13–24 months 1.17 (0.51–2.73) >5 years versus 13–24 months 1.39 (0.54–3.57) >5 years versus 25–60 months 1.18 (0.53–2.64)
Appendix 4
See Table 7
Table 7.
Bivariate, multivariable analyses of currently receiving antiretroviral therapy and partnership status among young, Black men who have sex with men living with HIV in Dallas and Houston, Texas, 2009–2014
| Variable | Category | N | Bivariatea | Multivariableb | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| % Yes | p | AOR | 95 % CI | |||
| Relational | ||||||
| Partnership status | <0.001 | |||||
| No partner | 104 | 86.5 | 1.00 | |||
| Have a partner | 132 | 59.1 | 0.36 | 0.17–0.79 | ||
| Individual | ||||||
| City | 0.247 | |||||
| Dallas | 110 | 74.5 | 1.00 | |||
| Houston | 127 | 67.7 | 1.25 | 0.59–2.64 | ||
| Survey | 0.229 | |||||
| 2009 | 30 | 66.7 | 1.00 | |||
| 2010 | 41 | 65.9 | 1.49 | 0.36–6.19 | ||
| 2011 | 33 | 63.6 | 1.05 | 0.28–3.87 | ||
| 2012 | 42 | 66.7 | 1.56 | 0.39–6.26 | ||
| 2013 | 41 | 85.4 | 3.22 | 0.69–14.95 | ||
| 2014 | 50 | 74.0 | 1.65 | 0.40–6.74 | ||
| Age (years) | 0.289 | |||||
| 18–20 | 20 | 55.0 | 1.00 | |||
| 21–23 | 61 | 75.4 | 1.54 | 0.32–7.41 | ||
| 24–26 | 75 | 74.7 | 1.11 | 0.22–5.50 | ||
| 27–29 | 81 | 67.9 | 1.02 | 0.21–5.02 | ||
| Time since HIV diagnosis | 0.411 | |||||
| 0–12 months | 62 | 64.5 | 1.00 | |||
| 13–24 months | 33 | 72.7 | 1.23 | 0.40–3.82 | ||
| 25–60 months | 79 | 77.2 | 1.84 | 0.69–4.92 | ||
| >5 years | 59 | 69.5 | 1.93 | 0.66–5.62 | ||
| Sociostructural | ||||||
| Educational attainment | 0.001 | |||||
| <Grade 12 | 47 | 48.9 | 1.00 | |||
| Grade 12 | 65 | 73.8 | 3.17 | 1.07–9.44 | ||
| >Grade 12 | 124 | 78.2 | 1.98 | 0.73–5.34 | ||
| Employment status | 0.020 | |||||
| Full-time | 124 | 76.6 | 1.00 | |||
| Part-time | 45 | 75.6 | 1.14 | 0.36–3.58 | ||
| Unemployed/disabled | 66 | 57.6 | 0.35 | 0.13–0.93 | ||
| Annual income | 0.008 | |||||
| <$10,000 | 73 | 63.0 | 1.00 | |||
| $10,000–$19,999 | 32 | 84.4 | 1.53 | 0.38–6.10 | ||
| $20,000–$39,999 | 75 | 81.3 | 0.79 | 0.25–2.50 | ||
| $40,000 or more | 54 | 61.1 | 0.29 | 0.09–1.00 | ||
| Incarceration | 0.001 | |||||
| In the past year | 47 | 48.9 | 1.00 | |||
| >1 year ago | 26 | 69.2 | 1.77 | 0.50–6.30 | ||
| Never | 156 | 78.8 | 1.97 | 0.79–4.86 | ||
| Homelessness | <0.001 | |||||
| In the past year | 34 | 38.2 | 1.00 | |||
| >1 year ago | 20 | 75.0 | 3.88 | 0.77–19.53 | ||
| Never | 178 | 77.5 | 3.86 | 1.23–12.13 | ||
| Sexual orientation | 0.163 | |||||
| Gay-identified | 192 | 72.9 | 1.00 | |||
| Other-identified | 45 | 62.2 | 0.65 | 0.26–1.65 | ||
| Total | 237 | 67.3 | ||||
p ≤ .05 are indicated in boldface type
OR odds ratio, CI confidence interval
P-value is for χ2 statistic for omnibus test assessing association between variable and outcome in a simple logistic regression analysis
AOR with 95 % CI (n = 224, Hosmer–Lemeshow goodness of fit test p-value = 0.52)
Appendix 5
See Table 8
Table 8.
Bivariate, multivariable analyses of No Missed Doses in past 30 days and partnership status among young, Black men who have sex with men living with HIV in Dallas and Houston, Texas, 2009–2014
| Variable | Category | N | Bivariatea | Multivariableb | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| % Yes | p | AOR | 95 % CI | |||
| Relational | ||||||
| Partnership status | 0.064 | |||||
| No/concordant partner | 135 | 48.9 | 1.00 | |||
| Discordant | 33 | 66.7 | 2.45 | 0.94–6.38 | ||
| Individual | ||||||
| City | 0.527 | |||||
| Dallas | 82 | 54.9 | 1.00 | |||
| Houston | 86 | 50.0 | 0.79 | 0.37–1.68 | ||
| Survey | 0.330 | |||||
| 2009 | 20 | 55.0 | 1.00 | |||
| 2010 | 27 | 63.0 | 0.91 | 0.20–4.06 | ||
| 2011 | 21 | 33.3 | 0.41 | 0.09–1.78 | ||
| 2012 | 28 | 53.6 | 0.69 | 0.17–2.85 | ||
| 2013 | 35 | 45.7 | 0.60 | 0.14–2.51 | ||
| 2014 | 37 | 59.5 | 1.01 | 0.26–3.92 | ||
| Age (years) | 0.448 | |||||
| 18–20 | 11 | 36.4 | 1.00 | |||
| 21–23 | 46 | 58.7 | 5.23 | 0.84–32.59 | ||
| 24–26 | 56 | 55.4 | 4.37 | 0.70–27.10 | ||
| 27–29 | 55 | 47.3 | 3.21 | 0.49–20.95 | ||
| Time since HIV diagnosis | 0.580 | |||||
| 0–12 months | 40 | 62.5 | 1.00 | |||
| 13–24 months | 24 | 50.0 | 0.52 | 0.16–1.69 | ||
| 25–60 months | 61 | 50.8 | 0.51 | 0.19–1.36 | ||
| >5 years | 41 | 48.8 | 0.47 | 0.16–1.36 | ||
| Sociostructural | ||||||
| Educational attainment | 0.748 | |||||
| <Grade 12 | 23 | 52.2 | 1.00 | |||
| Grade 12 | 48 | 47.9 | 0.76 | 0.21–2.77 | ||
| >Grade 12 | 97 | 54.6 | 1.02 | 0.32–3.26 | ||
| Employment status | 0.350 | |||||
| Full-time | 95 | 52.6 | 1.00 | |||
| Part-time | 34 | 61.8 | 1.67 | 0.59–4.69 | ||
| Unemployed/disabled | 38 | 44.7 | 0.79 | 0.30–2.10 | ||
| Annual income | 0.945 | |||||
| <$10,000 | 46 | 52.2 | 1.00 | |||
| $10,000–$19,999 | 27 | 55.6 | 0.79 | 0.25–2.48 | ||
| $20,000–$39,999 | 61 | 54.1 | 0.89 | 0.30–2.62 | ||
| $40,000 or more | 33 | 48.5 | 0.90 | 0.25–3.23 | ||
| Incarceration | 0.288 | |||||
| In the past year | 23 | 39.1 | 1.00 | |||
| >1 year ago | 18 | 61.1 | 2.14 | 0.50–9.14 | ||
| Never | 123 | 55.3 | 1.66 | 0.56–4.86 | ||
| Homelessness | 0.809 | |||||
| In the past year | 13 | 61.5 | 1.00 | |||
| >1 year ago | 15 | 53.3 | 0.86 | 0.14–5.13 | ||
| Never | 138 | 52.2 | 0.79 | 0.19–3.29 | ||
| Sexual orientation | 0.782 | |||||
| Gay-identified | 140 | 52.9 | 1.00 | |||
| Other-identified | 28 | 50.0 | 1.26 | 0.47–3.37 | ||
| Total | 168 | 52.4 | ||||
p ≤ .05 are indicated in boldface type
OR odds ratio, CI confidence interval
P-value is for χ2 statistic for omnibus test assessing relationship between variable and outcome in a simple logistic regression analysis
AOR with 95% CI (n = 162, Hosmer–Lemeshow goodness of fit test p-value = 0.25)
Footnotes
Compliance with Ethical Standards
Conflict of interest The authors declare that they have no conflict of interest.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
References
- 1.Christopoulos KA, Das M, Colfax GN. Linkage and retention in HIV care among men who have sex with men in the United States. Clin Infect Dis. 2011;52(suppl 2):S214–22. doi: 10.1093/cid/ciq045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gardner EM, McLees MP, Steiner JF, del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for disease control and prevention. [Accessed 20 Sept 2016];HIV among African American gay and bisexual men. 2014 http://www.cdc.gov/hiv/group/msm/bmsm.html.
- 4.Mugavero MJ, Lin HY, Allison JJ, et al. Racial disparities in HIV virologic failure: do missed visits matter? J Acquir Immune Defic Syndr. 2009;50(1):100–8. doi: 10.1097/QAI.0b013e31818d5c37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clin Infect Dis. 2013;57(8):1164–71. doi: 10.1093/cid/cit420. [DOI] [PubMed] [Google Scholar]
- 6.Maulsby C, Millett G, Lindsey K, et al. HIV among black men who have sex with men (MSM) in the United States: a review of the literature. AIDS Behav. 2014;18(1):10–25. doi: 10.1007/s10461-013-0476-2. [DOI] [PubMed] [Google Scholar]
- 7.Simoni JM, Huh D, Wilson IB, et al. Racial/ethnic disparities in ART adherence in the United States: findings from the MACH14 study. J Acquir Immune Defic Syndr. 2012;60(5):466–72. doi: 10.1097/QAI.0b013e31825db0bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mayer KH, Wang L, Koblin B, et al. Concomitant socioeconomic, behavioral, and biological factors associated with the disproportionate HIV infection burden among Black men who have sex with men in 6 US cities. PLoS ONE. 2014;9(1):e87298. doi: 10.1371/journal.pone.0087298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matthews DD, Herrick A, Coulter RW, et al. Running backwards: consequences of current HIV incidence rates for the next generation of Black MSM in the United States. AIDS Behav. 2016;20(1):7–16. doi: 10.1007/s10461-015-1158-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peterson JL, Bakeman R, Sullivan P, et al. Social discrimination and resiliency are not associated with differences in prevalent HIV infection in Black and White men who have sex with men. J Acquir Immune Defic Syndr. 2014;66(5):538–43. doi: 10.1097/QAI.0000000000000203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sullivan PS, Peterson J, Rosenberg ES, et al. Understanding racial HIV/STI disparities in Black and White men who have sex with men: a multilevel approach. PLoS ONE. 2014;9(3):e90514. doi: 10.1371/journal.pone.0090514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goodreau SM, Carnegie NB, Vittinghoff E, et al. What drives the US and peruvian HIV epidemics in men who have sex with men (MSM)? PLoS ONE. 2012;7(11):e50522. doi: 10.1371/journal.pone.0050522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23(9):1153–62. doi: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]
- 14.Mitchell JW, Petroll AE. HIV testing rates and factors associated with recent HIV testing among male couples. Sex Transm Dis. 2012;39(5):379–81. doi: 10.1097/OLQ.0b013e3182479108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hagedoorn M, Sanderman R, Bolks HN, Tuinstra J, Coyne JC. Distress in couples coping with cancer: a meta-analysis and critical review of role and gender effects. Psychol Bull. 2008;134(1):1. doi: 10.1037/0033-2909.134.1.1. [DOI] [PubMed] [Google Scholar]
- 16.Pietromonaco PR, Uchino B, Dunkel Schetter C. Close relationship processes and health: implications of attachment theory for health and disease. Health Psychol. 2013;32(5):499. doi: 10.1037/a0029349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Umberson D, Montez JK. Social relationships and health: a flashpoint for health policy. J Health Soc Behav. 2010;51(Suppl):S54–66. doi: 10.1177/0022146510383501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uchino BN, Bowen K, Carlisle M, Birmingham W. Psychological pathways linking social support to health outcomes: a visit with the “ghosts” of research past, present, and future. Soc Sci Med. 2012;74(7):949–57. doi: 10.1016/j.socscimed.2011.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mitchell JW. HIV-negative and HIV-discordant gay male couples’ use of HIV risk-reduction strategies: differences by partner type and couples’ HIV-status. AIDS Behav. 2013;17(4):1557–69. doi: 10.1007/s10461-012-0388-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gamarel KE, Revenson TA. couple Resilience. Berlin: Springer; 2015. Dyadic adaptation to chronic illness: the importance of considering context in understanding couples’ resilience; pp. 83–105. [Google Scholar]
- 21.Montgomery CM, Watts C, Pool R. HIV and dyadic intervention: an interdependence and communal coping analysis. PLoS ONE. 2012;7(7):e40661. doi: 10.1371/journal.pone.0040661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stumbo S, Wrubel J, Johnson MO. A qualitative study of HIV treatment adherence support from friends and family among same sex male couples. Psychol Educ. 2011;2(4):318–22. doi: 10.4236/psych.2011.24050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wrubel J, Stumbo S, Johnson MO. Male same-sex couple dynamics and received social support for HIV medication adherence. J Soc Pers Relat. 2010;27(4):553–72. doi: 10.1177/0265407510364870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson MO, Dilworth SE, Taylor JM, Darbes LA, Comfort ML, Neilands TB. Primary relationships, HIV treatment adherence, and virologic control. AIDS Behav. 2012;16(6):1511–21. doi: 10.1007/s10461-011-0021-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wrubel J, Stumbo S, Johnson MO. Antiretroviral medication support practices among partners of men who have sex with men: a qualitative study. AIDS Patient Care STDS. 2008;22(11):851–8. doi: 10.1089/apc.2008.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Remien RH, Stirratt MJ, Dolezal C, et al. Couple-focused support to improve HIV medication adherence: a randomized controlled trial. AIDS. 2005;19(8):807–14. doi: 10.1097/01.aids.0000168975.44219.45. [DOI] [PubMed] [Google Scholar]
- 27.Goldenberg T, Clarke D, Stephenson R. “Working together to reach a goal”: MSM’s perceptions of dyadic HIV care for same-sex male couples. J Acquir Immune Defic Syndr. 2013;64(Suppl 1):S52–61. doi: 10.1097/QAI.0b013e3182a9014a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goldenberg T, Stephenson R. “The more support you have the better”: partner support and dyadic HIV care across the continuum for gay and bisexual men. J Acquir Immune Defic Syndr. 2015;69(Suppl 1):S73–9. doi: 10.1097/QAI.0000000000000576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gamarel KE, Neilands TB, Golub SA, Johnson MO. An omitted level: an examination of relational orientations and viral suppression among HIV serodiscordant male couples. J Acquir Immune Defic Syndr. 2014;66(2):193–6. doi: 10.1097/QAI.0000000000000148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wall KM, Canary L, Workowski K, et al. Acceptability of couples’ voluntary HIV testing among HIV-infected patients in care and their HIV-negative partners in the United States. Open AIDS J. 2016;10:1. doi: 10.2174/1874613601610010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson MO, Dilworth SE, Neilands TB. Partner reports of patients’ HIV treatment adherence. J Acquir Immune Defic Syndr. 2011;56(4):e117–8. doi: 10.1097/QAI.0b013e31820bd2ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Millett GA, Peterson JL, Wolitski RJ, Stall R. Greater risk for HIV infection of Black men who have sex with men: a critical literature review. Am J Public Health. 2006;96(6):1007. doi: 10.2105/AJPH.2005.066720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among Black and White men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21(15):2083. doi: 10.1097/QAD.0b013e3282e9a64b. [DOI] [PubMed] [Google Scholar]
- 34.Beer L, Oster AM, Mattson CL, Skarbinski J. Medical Monitoring Project. Disparities in HIV transmission risk among HIV-infected Black and White men who have sex with men, United States, 2009. AIDS. 2014;28(1):105–14. doi: 10.1097/QAD.0000000000000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Millett GA, Peterson JL, Flores SA, et al. Comparisons of disparities and risks of HIV infection in Black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–8. doi: 10.1016/S0140-6736(12)60899-X. [DOI] [PubMed] [Google Scholar]
- 36.Kelley CF, Rosenberg ES, O’Hara BM, et al. Measuring population transmission risk for HIV: an alternative metric of exposure risk in men who have sex with men (MSM) in the US. PLoS ONE. 2012;7(12):e53284. doi: 10.1371/journal.pone.0053284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gallagher KM, Sullivan PS, Lansky A, Onorato IM. Behavioral surveillance among people at risk for HIV infection in the US: the national HIV behavioral surveillance system. Pub Health Rep. 2007 doi: 10.1177/00333549071220S106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huebner DM, Kegeles SM, Rebchook GM, et al. Social oppression, psychological vulnerability, and unprotected intercourse among young Black men who have sex with men. Health Psychol. 2014;33(12):1568. doi: 10.1037/hea0000031. [DOI] [PubMed] [Google Scholar]
- 39.Scott HM, Pollack L, Rebchook GM, Huebner DM, Peterson J, Kegeles SM. Peer social support is associated with recent HIV testing among young Black men who have sex with men. AIDS Behav. 2013;18(5):1–8. doi: 10.1007/s10461-013-0608-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Poundstone KE, Strathdee SA, Celentano DD. The social epidemiology of human immunodeficiency virus/acquired immunodeficiency syndrome. Epidemiol Rev. 2004;26:22–35. doi: 10.1093/epirev/mxh005. [DOI] [PubMed] [Google Scholar]
- 41.Hosmer DW, Jr, Lemeshow S. Applied logistic regression. New York: John Wiley & Sons; 2004. [Google Scholar]
- 42.Gamarel KE, Golub SA. Intimacy motivations and pre-exposure prophylaxis (PrEP) adoption intentions among HIV-negative men who have sex with men (MSM) in romantic relationships. Ann Behav Med. 2015;49(2):177–86. doi: 10.1007/s12160-014-9646-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eaton LA, Driffin DD, Kegler C, et al. The role of stigma and medical mistrust in the routine health care engagement of Black men who have sex with men. Am J Public Health. 2015;105(2):e75–82. doi: 10.2105/AJPH.2014.302322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Revenson TA, Kayser KE, Bodenmann GE. Couples coping with stress: emerging perspectives on dyadic coping. Washington: American Psychological Association; 2005. [Google Scholar]
- 45.Rosenberg ES, Millett GA, Sullivan PS, del Rio C, Curran JW. Understanding the HIV disparities between Black and White men who have sex with men in the USA using the HIV care continuum: a modelling study. Lancet HIV. 2014;1(3):e112–8. doi: 10.1016/S2352-3018(14)00011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ayala G, Bingham T, Kim J, Wheeler DP, Millett GA. Modeling the impact of social discrimination and financial hardship on the sexual risk of HIV among Latino and Black men who have sex with men. Am J Public Health. 2012;102(S2):S242–9. doi: 10.2105/AJPH.2011.300641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kenny DA, Kashy D, Cook WL. Dyadic data analysis. New York: Guilford Press; 2006. [Google Scholar]
- 48.Bauermeister JA, Carballo-Dieguez A, Ventuneac A, Dolezal C. Assessing motivations to engage in intentional condomless anal intercourse in HIV risk contexts (“bareback sex”) among men who have sex with men. AIDS Educ Prev. 2009;21(2):156–68. doi: 10.1521/aeap.2009.21.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Van de Ven P, Mao L, Fogarty A, et al. Undetectable viral load is associated with sexual risk taking in HIV serodiscordant gay couples in Sydney. AIDS. 2005;19(2):179–84. doi: 10.1097/00002030-200501280-00010. [DOI] [PubMed] [Google Scholar]
- 50.Muessig KE, Cohen MS. Advances in HIV prevention for serodiscordant couples. Curr HIV/AIDS Rep. 2014;11(4):434–46. doi: 10.1007/s11904-014-0225-9. [DOI] [PMC free article] [PubMed] [Google Scholar]