Abstract
Overexposure to the sun is associated with an increased risk of melanoma and nonmelanoma skin cancer, but indications of improvements in sun protection behavior are poor. Attempts to identify emerging themes in skin cancer control have largely been driven by groups of experts from a single field. In December 2016, 19 experts from various disciplines convened for Interdisciplinary Perspectives on Skin Cancer, a 2-day meeting hosted by the National Academy of Sciences. The group discussed knowledge gaps, perspectives on sun exposure, implications for skin cancer risk and other health outcomes, and new directions. Five themes emerged from the discussion: (1) The definition of risk must be expanded, and categories for skin physiology must be refined to incorporate population diversities. (2) Risky sun exposure often co-occurs with other health-related behaviors. (3) Messages must be nuanced to target at-risk populations. (4) Persons at risk for tanning disorder must be recognized and treated. (5) Sun safety interventions must be scalable. Efficient use of technologies will be required to sharpen messages to specific populations and to integrate them within multilevel interventions. Further interdisciplinary research should address these emerging themes to build effective and sustainable approaches to large-scale behavior change.
Introduction
Overexposure to sunlight is associated with increased risk of melanoma, the most commonly fatal form of skin cancer, and with nonmelanoma skin cancer, the most commonly occurring cancer in the United States.1, 2 The incidence of melanoma has risen dramatically since first recorded in 1935, as has the average cost of treatment: it is estimated that from 2007 to 2011, 5 million adults were diagnosed with skin cancer annually at an estimated cost of more than $8 billion.2 Recent research in genetics, anthropology, and medicine indicates that vulnerability to skin cancer can exist in individuals who consider themselves at low or no risk for skin cancer because of moderately pigmented skin. Furthermore, evidence suggests that sun exposure leads to some health benefits recognized by the public, such as vitamin D synthesis. In view of the emerging science, the 2014 Surgeon General’s Call to Action to Prevent Skin Cancer,2 and the National Cancer Institute’s continuing mission to make UV radiation (UVR) protection a priority in cancer control,3 the Board on Behavioral, Cognitive, and Sensory Sciences of the National Academy of Sciences hosted a meeting on December16 and 17, 2016. This meeting, Interdisciplinary Perspectives on Skin Cancer, was supported by the National Cancer Institute. Nineteen experts in dermatology, behavioral medicine, public health, adolescent medicine, clinical health psychology, anthropology, and kinesiology met with National Cancer Institute scientific staff to share interdisciplinary perspectives on sun exposure and to discuss knowledge gaps, implications for skin cancer risk and other health outcomes, and new directions for research and prevention. Five themes emerged: (1) expanding the definition of risk, with a need for refined categories for skin physiology and population diversity; (2) co-occurrence of sun overexposure and other health related behaviors; (3) the need for nuanced messages for at-risk populations; (4) recognition and treatment of those at risk for tanning disorder; and (5) creating scalability for sun safety interventions (Figure).
Figure.
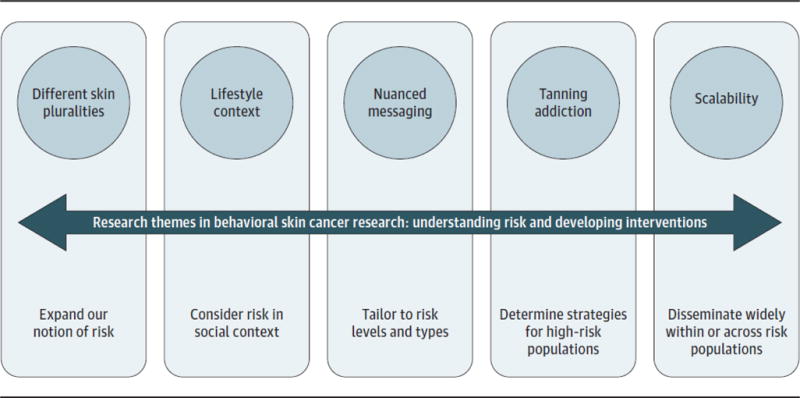
Research Themes in Behavioral Skin Cancer Research: Understanding Risk and Developing Interventions
Need for Refined Categories for Skin Physiology and Population Diversity
Recognition of the carcinogenic potential of UVR has led to the development of diverse strategies to reduce the risk of skin cancer,4 especially for individuals with lightly pigmented skin (Fitzpatrick types I and II). Routine sun safety behavior, however, has been emphasized for all people because the DNA in human skin is vulnerable to mutagenic damage that can lead to skin cancer regardless of constitutive pigmentation.5 New data from research in skin biology, cancer epidemiology, physiology, and skin pigmentation genetics are leading to a more nuanced understanding of the reactions of human skin to UVR. This information is making it possible to develop sun safety programs that emphasize assessment of individual risk based on ancestry, age, location, and lifestyle. Despite gaps in knowledge about the biological and health consequences of UVR exposure, our current understanding of human physiology, skin reactions to UVR, and the risks of skin cancer and other diseases suggests that, although the harms associated with overexposure outweigh the benefits, the beneficial effects of UVR exposure should not be ignored in developing new sun safety guidelines. Recent evidence confirms the beneficial effects of UVR, primarily in connection with cutaneous biosynthesis of vitamin D by UV-B radiation (290–320nm), and secondarily in relation to the release of vasoactive nitric oxide in the skin following exposure to UV-A radiation (320–410 nm).6, 7 The benefits of vitamin D involving the skeletal, nervous, cardiovascular, and immune systems, and the disease risks potentiated by vitamin D deficiency are imperfectly understood.8 Sun protection strategies must reflect the understanding that human skin pigmentation evolved to balance the negative and positive effects of sun exposure, with darker skin conferring more protection against high levels of UV-A and UV-B radiation near the equator and lighter (less pigmented) skin adapted to generally lower and more seasonal levels of UVR(especially of UV-B) outside the tropics.9
Skin with more eumelanin (Fitzpatrick types V and VI) experiences less carcinogenic DNA damage from UVR exposure but also must be exposed for longer periods of time to maximize vitamin D production.9 Long-distance migrations, urbanization, and major changes in lifestyles, especially in the past 500 years, have affected patterns of human behavior in relation to the sun as well as the real and perceived risks of exposure. Longer life spans increase the potential for mutagenic DNA damage leading to skin cancer. Special attention must be paid to persons with lighter (Fitzpatrick type I or II) skin who engage in incautious, episodic exposure to intense sunlight; to people—generally those with darker (Fitzpatrick type V or VI) skin—who do not consider themselves at risk for sun-induced skin damage or skin cancer; and to those of lower socioeconomic status, regardless of skin color, who often lack education, cancer and skin cancer awareness, and access to health care.
Co-occurrence of Sun Overexposure and Other Health-Related Behaviors
Behaviors that occur when people are outdoors in the sun have been largely studied in isolation from other health behaviors. For example, melanoma incidence has been associated with physical activity (ostensibly via increased risk of sunburn), but physical activity is associated with reduced risk for many other forms of cancer.10 Reducing risk for one disease should not come at the cost of increasing risk for another. Some healthy behaviors co-occur (e.g., wearing sunscreen and sunglasses), as do some unhealthy behaviors (e.g., unprotected sun exposure and alcohol intake). Particular healthy behaviors can reduce there in forcing value of other behaviors (e.g., protective clothing becomes aversive while running outside) or reinforce the value of an unhealthy behavior (e.g., use of exercise and tanning to improve body image). Measuring the patterns and the contexts of co-occurring healthy and unhealthy behaviors can inform and increase the impact of sun safety efforts. For example, concurrent unhealthy behaviors tend to share contexts, such as elevated alcohol consumption while vacationing,11 when people may be at high risk for unprotected sun exposure and sunburn. Alternatively, people may pair healthy with unhealthy behavior, adopting a compensatory approach (e.g., “sun exposure/tanning while exercising is OK”), or suspend their usual sun protection behavior on special occasions (e.g., sunbathing on vacation, indoor tanning before a prom or wedding).12 These examples represent new opportunities to increase understanding of sun protection by studying physical environments, multiple health behaviors, and multiple underlying social, affective, and cognitive processes and by assessing motivation for using sun protection. Informed by the specific context where they co-occur, bundled messaging can target multiple health behaviors. For example, in vacation and recreational settings, messaging focused on how sun protection can augment immediate pleasure (“get the most of out your vacation”) may resonate better than messaging focused on how it may.
Physical activity is one such health-enhancing behavior that deserves attention in sun safety research for it is associated with sunburn, which is reported by more than 40% of adults and 67% of teens annually.13 Sunburn is the best proximal biomarker of melanoma, with hazard ratios rivaling those of tanning bed exposure.14 Athletes report that forgetting to apply sunscreen and not liking how sunscreen feels during physical activity are barriers to use14; protective clothing may also be perceived to reduce performance or enjoyment. Individuals may believe that an active lifestyle reduces cancer risk, negating the need for other health behaviors. Also, placing a high value on physical appearance may be a driver for both prevent tanning and exercise, as may be stress reduction, another pathway by which these behaviors co-occur.
Recognizing that sun protection may pose unique challenges to active individuals who vary in exercise type (e.g., competitive sports, recreational activity), skin type, and age reinforces the need to study the nuanced associations among exercise, sunburn, and reasons for inadequate sun protection. Devices such as Smartphone, remote sensors, and electronic diaries can also improve understanding of physical activity. Sun protection and co-occurring behaviors can be linked together in real time, in known physical contexts, and in social contexts.3 Furthermore, the same devices can deliver messages targeted to individual locations or activities.
Finally, at the macro level, little is known about how individual level approaches to sun safety fit into the backdrop of current public health messages, which strongly encourage exercise to promote health and prevent disease.
The Need for Nuanced Messages for At-Risk Populations
In the United States, sun safety messaging has mostly used a one size-fits-all approach: everyone is encouraged to restrict time in the sun during peak UV hours and to routinely wear sunscreen and protective clothing despite the heterogeneity of the population.15 Nuanced messaging may be more successful when population segments with specific risk profiles are targeted with tailored messages delivered in specific environments. Risk factors related to environment (e.g., geographic, seasonal) and lifestyle (e.g., outdoor work, exercise) also have implications for sun safety messaging. Contending with varying motivations for UVR exposure, including perceptions that a tan improves appearance, helps relieve stress, or provides health benefits, is challenging to the development of clear messages.
A shift toward nuanced messaging, or “precision targeting,” has considerable potential. First, various risk factors can facilitate or undermine receptivity to specific protection recommendations, and current messaging may fail to address environments, motivations, and behaviors that confer the greatest risk for a given individual. For example, reminding an office worker to wear sunscreen daily may not decrease his or her high-risk sunbathing during vacations. Second, decades of research in tobacco control, cancer screening, and physical activity show that people are more persuaded when messages are tailored to personal values, motivations, or other individual characteristics and risk factors.16 Finally, nuanced messages can allow individuals choice in how they protect themselves, which is critical for behavior change.17
Overall, it is important to understand how decisions about sun protection are made in the real world when developing messages that target these behaviors. Multiple contextual factors (e.g., place, weather, and availability of shade) contribute to complexity in decisions about sun protection and could inform messaging.18 With more detailed information about a person, nuanced messages can ideally be constructed by considering the intersection of that individual’s context, preferences, and types of sun protection available. For example, sun safety messages specifically for vacationers may stress simplicity to fit their desire to escape normal daily responsibilities by delivering photographs of diverse sun protection options that highlight relaxation. Nuanced messaging is also used in Australia, where solar UV alerts are based on environmental factors, such as geographic location and daily UV index.18 Nuanced messaging could include information about the value and salience of the UV index for making decisions about recreation and sun protection while acknowledging that this information may drive different behaviors across exposure contexts and individual preferences.
Technology may facilitate delivery of nuanced messages and help personalize content based on individual risk factors, values, and motivations at the precise time and location the individual in a high-risk context makes a decision relevant to sun safety. For example, wearable dosimeters can track UVR exposure and provide feedback similarly to wearable devices that track physical activity. Social media platforms, such as Facebook and Twitter, may deliver and disseminate nuanced messages to specific population segments, such as teenagers, to help counteract pro-tanning messaging from tanning salons and fashion magazines.19 Mobile applications could deliver “just-in-time” nuanced messages20 based on UVR exposure and use of sun protection, shade, sunscreen, and location and time outdoors. Research exploring technology to reduce skin cancer risk is nascent, but much may be learned from more currently used technological applications for diet and exercise.
Recognition and Treatment of Those at Risk for Tanning Disorder
A small proportion of the population engages in excessive tanning behavior,21 making these individuals highly vulnerable to skin cancers. The hallmarks of addictivetanning,termed “tanningdisorder,”22 include difficulty quitting,22 guilt about tanning too much, social problems related to tanning, and physically hazardous tanning. In addition to the behavioral parallels, tanning disorder has biological and genetic features similar to those seen in other substance and behavioral addictions.23 Experiments document that UV light has reinforcing properties24: UVR exposure leads to the release of endogenous opioids,23 and tanning sessions increase blood flow to brain areas associated with the drug-induced reward system.21 In preclinical studies, UVR-exposed mice exhibited classic symptoms of opioid withdrawal after administration of naloxone and demonstrated evidence of tolerance.25 Furthermore, tanning of the skin and upregulation of β-endorphin, the so-called feel-good peptide, are both stimulated by the most carcinogenic part of the UV spectrum. Persons with the symptoms of tanning disorder also tend to have the ANKK1 gene, which is associated with substance and alcohol dependence.26
Recognizing excessive tanning as an addiction suggests that there may be benefits to testing pharmacological treatments that have been studied for other conditions. For example, opioid antagonists such as naloxone have been used to treat a variety of behavioral addictions, including gambling disorder, compulsive buying, and internet pornography addiction.22 Selective serotonin reuptake inhibitor and selective serotonin-noradrenaline reuptake inhibitor antidepressants decrease compulsive repetition and depression, common comorbid symptoms of behavioral addictions, through serotoninergic regulation.22 Mood stabilizers such as carbamazepine may also offer some potential benefit.22 Although glutamatergic modulators, which affect reward pathways, have been used in small trials to treat gambling disorder,22 research suggests that N-acetylcysteine may increase metastasis of malignant melanoma.27 Caution should be used when considering this as a treatment for tanning disorder. These agents have not been studied for treating behavioral addictions in children and should be considered only when there are comorbid conditions for which they are already indicated.
An important implication of the recognition and treatment of tanning disorder is the need to educate clinicians to properly identify, diagnose, and treat excessive tanning. Although pharmacologic treatment of behavioral addictions is managed primarily by psychiatrists, primary care physicians, dermatologists, and other health care professionals are well positioned to identify excessive tanning behavior and refer patients to be screened for tanning disorder.
Creating Scalability for Sun Safety Interventions
To achieve population-level skin cancer prevention, evidence based interventions will need scaling up to increase the impact of successful interventions to benefit more people on a lasting basis, which is a Department of Health and Human Services Strategic Plan goal.28 Although several frameworks can guide scale-up, we point to RE-AIM (Reach, Effectiveness, Adoption, Implementation, and Maintenance) as a robust and well-known program dissemination framework that can inform the translation and public health impact of scale-up at organizational and individual levels.29
Most research in skin cancer prevention has focused on intervening in controlled community-based settings such as individual or small groups of schools, workplaces, outdoor recreation areas, and clinics. Unless effective interventions are disseminated and implemented more widely, there is little chance to achieve sustained changes as the at-risk population ages and the costs of skin cancer treatment rise. Change, however, will require more than replication in large populations. Research must identify the most appropriate intermediary organizations to implement evidence based interventions at scale and ways to promote implementation, such as adopting policies that clarify personal and organizational responsibilities (e.g., who provides and pays for sunscreen and protective clothing).
Scaled-up interventions must lower costs and increase reach to provide greater access to benefits. To build capacity and influence decision makers who determine whether evidence-based interventions are implemented, research on intervention scalability must examine reach, retained effectiveness, and costs.
Existing knowledge on skin cancer interventions at scale is limited to interventions delivered in multicomponent programs comprising individual, policy, environmental, and mass media elements and through television advertising.4 We lack data about the potential impact of digital communication technologies, such as the internet, Smartphone, and social media. Digital communication technologies and social media platforms can achieve large reach beyond individual settings, particularly with younger populations, with standardized, engaging content and increased portability at affordable costs.30
Given its large scope, it may be challenging to devote the resources needed to study intervention scalability. Population-wide skin cancer prevention interventions, such as the SunSmart campaign in Australia or the national campaign in Denmark,31, 32 can provide insights into scalability that may be transferred to the United States. Content analyses and online natural exposure surveys could be conducted with modest resources to better understand digital communication channels’ reach to at-risk populations, the type of messages conveyed, and the size and scope of their influence on, for example, indoor tanning and sun protection, especially in relation to the more established television advertising campaigns. Prospective trials on scalability should be considered. Metrics for effective scale-up should include the combination of how effective an intervention is when disseminated and the costs of scale-up (which are usually considerable). Thus, scalability research in skin cancer prevention should focus on improving the cost-effectiveness of reach, implementation, and behavior change.
Common themes from the Interdisciplinary Perspectives on Skin Cancer expert meeting centered on defining appropriate risk groups for interventions; the co-occurrence of risky sun exposure with other health-related behaviors; nuancing messages for specific at-risk populations; added emphasis on highest-risk populations, such as persons with tanning addiction; and a broader dissemination plan. It is clear that efficient use of technologies will be required to sharpen and disseminate messages to specific populations and to integrate the messages within multilevel interventions. Future expert meetings should concentrate more exclusively on sun protection in the pediatric population, ranging from early years through late teens. Further interdisciplinary research is needed to address the themes discussed, with the goal of building engaging, effective, and sustainable approaches to decrease the burden of skin cancer.
Acknowledgments
Funding/Support: This study was supported in part by award HHSN263201200074I, task order HHSN26300098 from the National Institutes of Health (NIH) to the National Academy of Sciences.
References
- 1.Rogers HW, Weinstock MA, Feldman SR, Coldiron BM. Incidence estimate of nonmelanoma skin cancer (keratinocyte carcinomas) in the U.S. population, 2012. JAMA Dermatol. 2015;151(10):1081–1086. doi: 10.1001/jamadermatol.2015.1187. [DOI] [PubMed] [Google Scholar]
- 2.US Department of Health & Human Services. The Surgeon General’s Call to Action to Prevent Skin Cancer. Washington, DC: US Dept of Health and Human Services, Office of the Surgeon General; 2014. [Google Scholar]
- 3.Perna FM, Dwyer LA, Tesauro G, et al. Research on skin cancer–related behaviors and outcomes in the NIH grant portfolio, 2000–2014: skin cancer intervention across the cancer control continuum. JAMA Dermatol. 2017;153(5):398–405. doi: 10.1001/jamadermatol.2016.6216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Community Preventive Services Task Force. Community-wide interventions to prevent skin cancer: recommendation of the Community Preventive Services Task Force. Am J Prev Med. 2016;51(4):540–541. doi: 10.1016/j.amepre.2016.03.019. [DOI] [PubMed] [Google Scholar]
- 5.Jablonski NG, Chaplin G. Colloquium paper: human skin pigmentation as an adaptation to UV radiation. Proc Natl Acad Sci U S A. 2010;107(suppl2):8962–8968. doi: 10.1073/pnas.0914628107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson RS, Titze J, Weller R. Cutaneous control of blood pressure. Curr Opin Nephrol Hypertens. 2016;25(1):11–15. doi: 10.1097/MNH.0000000000000188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu D, Fernandez BO, Hamilton A, et al. UVA irradiation of human skin vasodilates arterial vasculature and lowers blood pressure independently of nitric oxide synthase. J Invest Dermatol. 2014;134(7):1839–1846. doi: 10.1038/jid.2014.27. [DOI] [PubMed] [Google Scholar]
- 8.Parra EJ. Human pigmentation variation: evolution, genetic basis, and implications for public health. Am J Phys Anthropol. 2007;134(suppl 45):85–105. doi: 10.1002/ajpa.20727. [DOI] [PubMed] [Google Scholar]
- 9.Tadokoro T, Yamaguchi Y, Batzer J, et al. Mechanisms of skin tanning in different racial/ethnic groups in response to ultraviolet radiation. J Invest Dermatol. 2005;124(6):1326–1332. doi: 10.1111/j.0022-202X.2005.23760.x. [DOI] [PubMed] [Google Scholar]
- 10.Moore SC, Lee IM, Weiderpass E, et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern Med. 2016;176(6):816–825. doi: 10.1001/jamainternmed.2016.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neighbors C, Atkins DC, Lewis MA, et al. Event-specific drinking among college students. Psychol Addict Behav. 2011;25(4):702–707. doi: 10.1037/a0024051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buller DB, Andersen PA, Walkosz BJ, Scott MD, Beck L, Cutter GR. Effect of an intervention on observed sun protection by vacationers in a randomized controlled trial at North American resorts. Prev Med. 2017;99:29–36. doi: 10.1016/j.ypmed.2017.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holman DM, Berkowitz Z, Guy GP, Jr, Hartman AM, Perna FM. The association between demographic and behavioral characteristics and sunburn among U.S. adults—National Health Interview Survey, 2010. Prev Med. 2014;63:6–12. doi: 10.1016/j.ypmed.2014.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jinna S, Adams BB. Ultraviolet radiation and the athlete: risk, sun safety, and barriers to implementation of protective strategies. Sports Med. 2013;43(7):531–537. doi: 10.1007/s40279-013-0021-5. [DOI] [PubMed] [Google Scholar]
- 15.Linos E, Keiser E, Fu T, Colditz G, Chen S, Tang JY. Hat, shade, long sleeves, or sunscreen? rethinking US sun protection messages based on their relative effectiveness. Cancer Causes Control. 2011;22(7):1067–1071. doi: 10.1007/s10552-011-9780-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Noar SM, Benac CN, Harris MS. Does tailoring matter? meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133(4):673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- 17.Ng JY, Ntoumanis N, Thogersen-Ntoumani C, et al. Self-determination theory applied to health contexts: ameta-analysis. Perspect Psychol Sci. 2012;7(4):325–340. doi: 10.1177/1745691612447309. [DOI] [PubMed] [Google Scholar]
- 18.Shuk E, Burkhalter JE, Baguer CF, et al. Factors associated with inconsistent sun protection in first-degree relatives of melanoma survivors. Qual Health Res. 2012;22(7):934–945. doi: 10.1177/1049732312443426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Falzone AE, Brindis CD, Chren MM, et al. Teens, tweets, and tanning beds: rethinking the use of social media for skin cancer prevention. Am J Prev Med. 2017;53((3S1)(suppl 1)):S86–S94. doi: 10.1016/j.amepre.2017.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nahum-Shani I, Smith SN, Spring BJ, et al. Just-in-time adaptive interventions (JITAIs) in mobile health: key components and design principles for ongoing health behavior support [published online September 23, 2016] Ann Behav Med. doi: 10.1007/s12160-016-9830-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stapleton JL, Hillhouse J, Coups EJ. Addicted to UV: evidence for tanning addiction. In: Petry NM, editor. Behavioral Addictions: DSM-5® and Beyond. NewYork, NY: Oxford University Press; 2016. pp. 193–220. [Google Scholar]
- 22.Petry N. Behavioral Addictions: DSM-5® and Beyond. New York, NY: Oxford University Press; 2016. [Google Scholar]
- 23.Stapleton JL, Hillhouse J, Levonyan-Radloff K, Manne SL. Review of interventions to reduce ultraviolet tanning: need for treatments targeting excessive tanning, an emerging addictive behavior [published online June 22, 2017] Psychol AddictBehav. doi: 10.1037/adb0000289. Medline:28639816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feldman SR, Liguori A, Kucenic M, et al. Ultraviolet exposure is a reinforcing stimulus in frequent indoor tanners. J AmAcad Dermatol. 2004;51(1):45–51. doi: 10.1016/j.jaad.2004.01.053. [DOI] [PubMed] [Google Scholar]
- 25.Fell GL, Robinson KC, Mao J, Woolf CJ, Fisher DE. Skin β-endorphin mediates addiction to UV light. Cell. 2014;157(7):1527–1534. doi: 10.1016/j.cell.2014.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cartmel B, Dewan A, Ferrucci LM, et al. Novel gene identified in an exome-wide association study of tanning dependence. Exp Dermatol. 2014;23(10):757–759. doi: 10.1111/exd.12503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Le Gal K, Ibrahim MX, Wiel C, et al. Antioxidants can increase melanoma metastasis in mice. Sci Transl Med. 2015;7(308):308re8. doi: 10.1126/scitranslmed.aad3740. [DOI] [PubMed] [Google Scholar]
- 28.Glasgow RE, Vinson C, Chambers D, Khoury MJ, Kaplan RM, Hunter C. National Institutes of Health approaches to dissemination and implementation science: current and future directions. Am J Public Health. 2012;102(7):1274–1281. doi: 10.2105/AJPH.2012.300755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kessler RS, Purcell EP, Glasgow RE, Klesges LM, Benkeser RM, Peek CJ. What does it mean to “employ” the RE-AIM model? Eval Health Prof. 2013;36(1):44–66. doi: 10.1177/0163278712446066. [DOI] [PubMed] [Google Scholar]
- 30.Buller DB, Berwick M, Lantz K, et al. Smartphone mobile application delivering personalized, real-time sun protection advice: a randomized clinical trial. JAMA Dermatol. 2015;151(5):497–504. doi: 10.1001/jamadermatol.2014.3889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Montague M, Borland R, Sinclair C. Slip! Slop! Slap! and SunSmart, 1980–2000: Skin cancer control and 20 years of population-based campaigning. Health Educ Behav. 2001;28(3):290–305. doi: 10.1177/109019810102800304. [DOI] [PubMed] [Google Scholar]
- 32.Koster B, Thorgaard C, Philip A, Clemmensen H. Sunbed use and campaign initiatives in the Danish population, 2007–2009: a cross-sectional study. J Eur Acad Dermatol Venereol. 2011;25(11):1351–1355. doi: 10.1111/j.1468-3083.2010.03960.x. [DOI] [PubMed] [Google Scholar]


