Abstract
Background
Implementation of a medical emergency teams has been identified as a potential strategy to reduce hospital deaths, as these teams respond to patients with acute physiological decline in an effort to prevent in-hospital cardiac arrest. However, prior studies of the association between medical emergency teams and hospital mortality have been limited and typically have not accounted for pre-implementation mortality trends.
Methods
Within the Pediatric Health Information System (PHIS) for freestanding pediatric hospitals, annual risk-adjusted mortality rates were calculated for sites between 2000 and 2015. A random slopes interrupted time series analysis then examined whether implementation of a medical emergency team was associated with lower than expected mortality rates based on pre-implementation trends.
Results
Across 38 pediatric hospitals, mean annual hospital admission volume was 15,854 (range: 6,684–33,024), and there were a total of 1,659,059 hospitalizations pre-implementation and 4,392,392 hospitalizations post-implementation. Before medical emergency team implementation, hospital mortality decreased by 6.0% annually (odds ratio [OR] of 0.94 [95% CI: 0.92–0.96]) across all hospitals. After medical emergency team implementation, hospital mortality continued to decrease by 6% annually (OR of 0.94 [95% CI: 0.93–0.95]), with no deepening of the mortality slope (i.e., not lower odds ratio) as compared with the pre-implementation trend, for the overall cohort (P of 0.98) or when analyzed separately within each of the 38 study hospitals. Five years after medical emergency team implementation across study sites, there was no difference between predicted (hospital mean of 6.18 deaths per 1000 admissions based on pre-implementation trends) and actual mortality rates (hospital mean of 6.48 deaths per 1000 admissions; P of 0.57).
Conclusion
Implementation of medical emergency teams in a large sample of pediatric hospitals in the U.S was not associated with a reduction in hospital mortality beyond existing pre-implementation trends.
Keywords: medical emergency team, rapid response team, mortality
INTRODUCTION
Medical emergency teams, also known as rapid response teams, have been implemented throughout hospitals in the United States as part of the Institute for Healthcare Improvement’s Five Million Lives Campaign to reduce hospital morbidity and mortality.1 By promptly evaluating, triaging, and treating patients with signs of acute clinical deterioration, a medical emergency team, in theory, can reduce medical complications and prevent in-hospital cardiac arrest. Since fewer than 1 in 4 patients with an in-hospital cardiac arrest survives to hospital discharge,2 many have proposed that medical emergency teams can reduce hospital mortality by reducing the incidence of in-hospital cardiac arrest.3 However, whether routine implementation of medical emergency teams in pediatric hospitals has resulted in a reduction in hospital mortality, beyond temporal trends, is unclear. Addressing this gap in knowledge is important to understand to justify the costs, training and staffing of medical emergency teams.
Prior studies examining the association of medical emergency teams with hospital mortality have been limited, especially in pediatric hospitals. One single-center study found that implementation of a medical emergency team in a pediatric hospital was associated with a 35% reduction in hospital mortality4 while another study reported 18% lower hospital mortality post-implementation.5 A recent meta-analysis, however, identified only 7 single-centered studies that have evaluated the effect of medical emergency team implementation on mortality in pediatric hospitals.6 Although this meta-analysis found that medical emergency team implementation was associated with a 21% lower hospital mortality rate, only one study adjusted for pre-intervention hospital mortality trends while the other studies simply compared aggregated rates of hospital mortality before and after medical emergency team implementation. If rates of hospital mortality were already decreasing before medical emergency team implementation due to overall improvements in cardiac resuscitation7, 8, sepsis9, 10, and intensive care11, the findings from this meta-analysis, which was not able to adjust for pre-implementation mortality trends, may have been due to existing temporal trends and not from medical emergency team implementation.
Accordingly, the goal of the present investigation was to more accurately characterize the association between medical emergency team implementation and hospital mortality across a wide range of unselected pediatric institutions. Leveraging annual hospital mortality data from the Pediatric Health Information System (PHIS), the effect of medical emergency team implementation on hospital mortality was evaluated across 38 hospitals after accounting for pre-implementation mortality trends at each hospital.
METHODS
Data Sources
PHIS is an inpatient database created by the Children’s Hospital Association to support clinical effectiveness research and quality improvement projects among 47 not-for-profit freestanding children’s hospitals.12 Data is electronically and automatically collected and include patients’ demographics and diagnoses, as well as annual mortality rates for each participating hospital. Quality and validity checks are performed on collected data, and standard proprietary methodology is used for data definitions to ensure consistency across hospitals. For this study, patient-level data from PHIS was used to calculate hospital case-mix for all admitted patients at each site for each year, which were, in turn, used to risk-adjust a hospital’s annual mortality rate.
Study Population
The study cohort included 47 pediatric hospitals that participated in PHIS between January 1, 2000 and December 31, 2015. For each hospital, we obtained information on the calendar year in which a medical emergency team was implemented from a member of its medical emergency or acute resuscitation (‘Code Blue’) team. Nine hospitals were excluded as their medical emergency team was implemented prior to participation in PHIS and therefore had no pre-implementation mortality data available for analysis. Thus, the primary analysis of the association between medical emergency team implementation and hospital mortality included 38 hospitals.
Study Outcomes
The primary outcome was risk-adjusted hospital mortality after medical emergency team implementation. Hospital mortality was defined as deaths per 1000 admissions and calculated for each calendar year, adjusted by the case-mix of patients admitted to the hospital that calendar year (see below).
Statistical Analysis
Summary statistics were used to describe baseline characteristics of hospitals in the study sample. Within each PHIS hospital, annual mortality rates were determined for each site and included all patients, regardless of do-not-resuscitate status. Next, risk-adjusted annual mortality rates for each calendar year at each site were calculated. This was accomplished by multiplying the observed mortality rate during a given year at a hospital by that hospital’s observed to expected mortality rate. The expected mortality rate was determined by applying previously developed mortality weights based on illness severity and one of 322 All Patients Refined Diagnosis Related Groups (APR-DRGs) to each admitted patient during a calendar year.13,14
Because most prior studies have simply performed aggregate pre-implementation and post-implementation comparisons, secular hospital trends in cardiac resuscitation quality improvement, sepsis and intensive care management, and other factors unrelated to medical emergency team implementation which could have had an impact on overall hospital mortality rates, were not accounted for. We therefore conducted an interrupted time series analysis, within a hierarchical logistic regression framework, to compare mortality trends before and after medical emergency team implementation. In this analysis, trend lines (slope and intercept) were estimated for each hospital before and after medical emergency team implementation, with the year of implementation designated as the reference year (“time zero”). Nonlinearity was assessed using restricted cubic splines but was non-significant (p=0.39), so straight-line trends were fitted. The slopes and intercepts were treated as correlated random effects within the hierarchical model using an unstructured covariance matrix. The resultant “average” slope and intercept from the model represented the overall population trend, and a joint statistical test was performed to assess whether the average mortality intercept or slope differed after medical emergency team implementation compared with pre-implementation trends. Specifically, a more negative slope would indicate a decrease in hospital mortality after medical emergency team implementation beyond what would be expected based on pre-implementation hospital mortality trends). To facilitate interpretability, we compared mortality rates for hospitals 5 years after medical emergency team implementation with projected estimates based on pre-implementation trends alone. Moreover, interactions between implementation of a medical emergency team and small and large hospital size (<250 beds vs. ≥250 beds) and U.S. Census region were examined to assess whether the effect of medical emergency teams on hospital mortality differed by these characteristics. As a sensitivity analysis, within each calendar year, we compared aggregated risk-adjusted mortality rates for hospitals which had already implemented a medical emergency team compared with hospitals which had not yet implemented their team.
Additionally, comparisons were performed within each hospital, using the estimated effects from the hierarchical model, to determine whether medical emergency team implementation was associated with a lower mortality rate for any individual hospital. F-tests for each hospital assessed for a difference in slopes or intercepts after medical emergency team implementation. The p-values from these tests were assessed for significance after accounting for multiple testing, using a step-up approach constraining the false discovery rate to be ≤5% (i.e. adjusted p<0.05).15
Finally, we conducted simulations to determine the minimum effect (change in slope of risk-adjusted mortality post-implementation) that we would have been able to detect with 80% power in our sample population. Data were simulated using the existing observed pre-implementation mortality rates and randomly generating post-implementation rates for each hospital based on parameter estimates from the primary analysis model augmented with a constant acceleration term to simulate the effect of implementation on the mortality slope.
For each analysis, we evaluated the null hypothesis at a 2-sided significance level of 0.05 and calculated 95% confidence intervals (CIs) using robust standard errors. All analyses were performed using SAS version 9.4 (SAS Institute, Cary, North Carolina) and R version 3.3.1 (R Foundation for Statistical Computing, Vienna, Austria).16 The institutional review board of Saint Luke’s Hospital approved the study and waived the requirement for informed consent as the analyses involved use of de-identified data.
RESULTS
Of 38 pediatric hospitals, 37 (97.4%) were academic hospitals, and the majority (29 [76.3%]) had 250 or more beds. Hospitals were distributed across the U.S., with 5 (13.2%) from the Northeast, 10 (26.3%) from the Midwest, 14 (36.8%) from the South, and 9 (23.7%) from the West (Table 1).
Table 1. Summary Characteristics of Study Hospitals.
| Total N = 38 |
|
|---|---|
| Academic | 37 (97.4%) |
| Staffed beds | |
| 126 to 249 | 9 (23.7%) |
| 250 to 592 | 29 (76.3%) |
| Census region | |
| Northeast | 5 (13.2%) |
| Midwest | 10 (26.3%) |
| South | 14 (36.8%) |
| West | 9 (23.7%) |
During the study period, the mean number of admissions at each site was 15,854 (range: 6,684–33,024), and medical emergency team implementation at sites occurred between 2005 and 2013. The mean duration of the pre-implementation and post-implementation periods was 3.0 years (range: 0.9–4.7) comprising 1,659,059 hospitalizations and 7.4 years (range: 2.1–9.8) comprising 4,392,392 hospitalizations, respectively.
Effect of Medical Emergency Teams on Hospital Mortality
Unadjusted and adjusted hospital mortality rates by when each hospital implemented its medical emergency team are displayed in Figure 1. The mean (95% CI) unadjusted hospital mortality rate was 8.5 (7.6, 9.5) deaths per 1000 admissions 2 years prior to medical emergency team implementation, 8.0 (7.2, 8.9) deaths per 1000 admissions during the year of hospitals’ implementation of their medical emergency team, and 6.2 (5.7, 6.7) deaths per 1000 admissions 5 years after medical emergency team implementation (Table 2). After adjustment for case-mix severity of all hospital admissions, the mean risk-adjusted hospital mortality rate was 9.5 (9.0, 10.1), 8.8 (8.3, 9.3), and 6.5 (6.2, 6.8) deaths per 1000 admissions at 2 years before, during, and 5 years after medical emergency team implementation, respectively.
Figure 1. Unadjusted and Risk-Adjusted Annual Mortality Rates for Each Hospital.
Unadjusted (A) and risk-adjusted (B) annual mortality data are presented by years before, the year of (red vertical dashed line), and years after medical emergency team implementation at each site. The dashed and solid trend lines represent the mean projected and actual mortality rates, respectively, for the study hospitals after medical emergency team implementation.
Table 2. Hospital Mortality Rates Before and After Medical Emergency Team Implementation.
Mean unadjusted and risk-adjusted hospital mortality rates 2 years before, the year of, and 5 years after implementation of medical emergency teams in study hospitals are summarized.
| Mean Hospital Mortality Rates | ||
|---|---|---|
| Deaths per 1000 admissions | Unadjusted (95% CI) | Adjusted (95% CI) |
| 2 years pre-initiation | 8.5 (7.6, 9.5) | 9.5 (9.0, 10.1) |
| Year of initiation (intercept) | 8.0 (7.2, 8.9) | 8.8 (8.3, 9.3) |
| 5 years post-initiation | 6.2 (5.7, 6.7) | 6.5 (6.2, 6.8) |
A comparison of pooled risk-adjusted hospital mortality rates found no difference in model intercepts or slopes after medical emergency team implementation (Table 3). Model intercepts for hospital mortality (time zero denotes year of medical emergency team implementation) before and after medical emergency team implementation were 8.4 (95% CI: 7.8, 9.0) and 8.8 (95% CI: 8.3, 9.3) deaths per 1000 admissions (P for difference between the two periods of 0.11), and model slopes for hospital mortality (odds ratio per calendar year) before and after medical emergency team implementation were 0.94 (95% CI: 0.92, 0.96) and 0.94 (95% CI: 0.93, 0.95) (P for difference between the two periods of 0.98). The latter suggests that the hospital mortality rate across all 38 hospitals before medical emergency team implementation was decreasing at 6.0% per year before medical emergency team implementation and continued to decrease at 6.0% per year after medical emergency team implementation. At 5 years after medical emergency team implementation, the mean risk-adjusted hospital mortality rate was predicted to be 6.18 (95% CI: 5.23, 7.29) deaths per 1000 admissions based on pre-implementation risk-adjusted mortality trends alone, which was similar (P = 0.57) to the actual mean risk-adjusted hospital mortality rate of 6.48 (95% CI: 6.19, 6.79) deaths per 1000 admissions after medical emergency team implementation (see Table 2). Simulation analyses revealed that our study had 80% power to detect a post-implementation slope of 0.913 versus the observed pre-implementation slope of 0.940, which suggests our study had 80% power to detect an absolute decrease of approximately 2 deaths per 10,000 admissions annually (based on a baseline risk-adjusted mortality rate of 8.8 deaths per 1000 admissions during the year of implementation and a 2.7% relative annual decrease in mortality attributable to implementation of a medical emergency team).
Table 3. Impact of Medical Emergency Team on Risk-Adjusted Hospital Mortality.
Mortality trends before and after implementation of a medical emergency team in study hospitals are compared. A significantly lower intercept or a more negative slope (lower odds ratio) after implementation would indicate that medical emergency teams reduced hospital mortality. Results are presented for the entire cohort and by hospital subgroups.
| Mortality Trend Before MET Intervention |
Mortality Trend After MET Intervention |
P | |
|---|---|---|---|
| Entire Cohort | |||
| Intercept (deaths per 1000 admits)* | 8.4 (7.8, 9.0) | 8.8 (8.3, 9.3) | 0.11 |
| Slope (Odds Ratios per year) | 0.94 (0.92, 0.96) | 0.94 (0.93, 0.95) | 0.98 |
|
| |||
| INTERACTION ANALYSES | |||
|
| |||
| By Bed Size | 0.69† | ||
| Intercept (deaths per 1000 admits)* | |||
| < 250 Hospital beds | 7.6 (6.4, 9.0) | 8.1 (7.2, 9.1) | |
| ≥ 250 Hospital beds | 8.6 (8.0, 9.3) | 9.0 (8.4, 9.6) | |
| Slope (Odds Ratios per year) | |||
| < 250 Hospital beds | 0.91 (0.86, 0.97) | 0.96 (0.93, 0.98) | |
| ≥ 250 Hospital beds | 0.94 (0.92, 0.97) | 0.94 (0.93, 0.95) | |
| By U.S. Census Region | 0.85† | ||
| Intercept (deaths per 1000 admits)* | |||
| Northeast | 7.3 (5.3, 10.2) | 8.1 (6.7, 9.9) | |
| Midwest | 8.4 (7.3, 9.6) | 8.6 (7.8, 9.6) | |
| South | 8.6 (7.8, 9.6) | 9.4 (8.4, 10.4) | |
| West | 8.8 (7.8, 9.9) | 8.6 (7.8, 9.5) | |
| Slope (Odds Ratios per year) | |||
| Northeast | 0.96 (0.85, 1.07) | 0.95 (0.93, 0.97) | |
| Midwest | 0.94 (0.89, 0.99) | 0.94 (0.93, 0.96) | |
| South | 0.94 (0.91, 0.97) | 0.94 (0.91, 0.96) | |
| West | 0.96 (0.92, 0.99) | 0.93 (0.91, 0.95) | |
Deaths per 1000 admissions at time of MET implementation
Overall p-value for interaction between hospital characteristic and MET implementation
To further clarify that our findings were not confounded by secular mortality trends, the adjusted mortality rates for each hospital by calendar year are displayed in Figure 2 and a comparison of aggregated risk-adjusted mortality for hospitals that had and had not yet implemented a medical emergency team for each calendar year are summarized in Table 4. Within each calendar year, there was no difference in aggregated risk-adjusted mortality between hospitals which had implemented a medical emergency team compared with those which had not yet already done so. When these individual calendar year comparisons were pooled, implementation of a medical emergency team was not associated with a reduction in hospital mortality (pooled odds ratio, 1.04 [95% CI: 0.96, 1.12] P=0.31), and the nonsignificantly higher odds ratio for hospital mortality after medical emergency team implementation mirrored the 5-year post-implementation predicted vs. observed mortality analyses above.
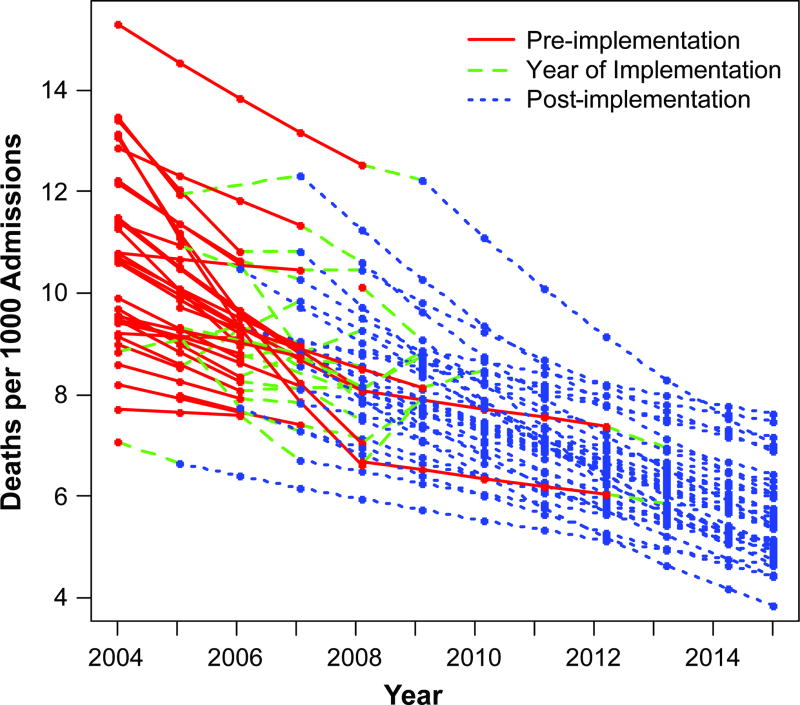
Figure 2. Risk-Adjusted Annual Mortality Rates for Each Hospital by Calendar Year.
Each hospital’s risk-adjusted mortality by calendar year are displayed, with red denoting the period before a hospital’s implementation of a MET team, green for the year of MET implementation, and blue for the period after MET implementation.
Abbreviations: MET, medical emergency team
TABLE 4. Yearly Comparisons of Risk-Adjusted Hospital Mortality Between Hospitals Before and After Medical Emergency Team Implementation.
When the individual calendar year comparisons were pooled, implementation of a medical emergency team was not associated with a reduction in hospital mortality (pooled odds ratio, 1.04 [95% CI: 0.96, 1.12], P=0.31),
| Year | Number of Hospitals | Aggregated Risk-Adjusted Mortality | ||||
|---|---|---|---|---|---|---|
| MET Not Yet in Place |
MET Begun This Year |
MET in Place |
MET Not Yet in Place |
MET in Place |
Odds Ratio for MET Implementation (95% CI) |
|
| 2004 | 38 | 10.6 | NA | |||
| 2005 | 35 | 3 | 9.8 | NA | ||
| 2006 | 29 | 6 | 3 | 9.1 | 9.3 | 1.03 (0.87, 1.21) |
| 2007 | 16 | 13 | 9 | 8.8 | 9.0 | 1.02 (0.91, 1.14) |
| 2008 | 6 | 10 | 22 | 7.3 | 8.3 | 1.14 (1.00, 1.29) |
| 2009 | 3 | 3 | 32 | 7.6 | 8.1 | 1.06 (0.91, 1.24) |
| 2010 | 2 | 1 | 35 | 6.9 | 7.5 | 1.09 (0.88, 1.34) |
| 2011 | 2 | 36 | 7.5 | 6.9 | 0.93 (0.76, 1.14) | |
| 2012 | 1 | 1 | 36 | 4.4 | 6.7 | 1.55 (1.00, 2.38) |
| 2013 | 1 | 37 | 6.3 | NA | ||
| 2014 | 38 | 6.0 | NA | |||
| 2015 | 38 | 5.1 | NA | |||
NA – For calendar years without at least one hospital with pre-implementation and post-implementation mortality data, odds ratios were not calculated.
Abbreviations: MET, medical emergency team
Moreover, within each of the 38 hospitals, a comparison of risk-adjusted mortality trends before and after medical emergency team implementation found that individual hospital mortality intercepts and slopes did not differ significantly for 36 (94.7%) of the hospitals (Supplementary Table 1). Two hospitals demonstrated significant differences pre- versus post-implementation, but in the opposite direction (a less negative slope over time leading to higher than expected mortality after medical emergency team implementation; Supplementary Figure 1). This suggests that implementation of a medical emergency team was not associated with a decrease in hospital mortality in any individual hospital beyond what would have been expected based on pre-implementation trends. Finally, we found no difference in the effect of implementation of a medical emergency team by hospital size or geographic region (interaction p-values 0.69 and 0.85 respectively; see Table 3).
DISCUSSION
To reduce morbidity and improve hospital survival by proactively intervening in patients with clinical deterioration, many hospitals have implemented medical emergency teams. Whether the costs and efforts in training and staffing such teams have led to lower hospital mortality has not been clear, despite initial findings from single-centered studies. We found that implementation of a medical emergency team in 38 pediatric hospitals was not associated with lower hospital mortality than what would have been expected based on pre-implementation trends. This was the case overall, for each individual hospital, and regardless of hospital size or geography. Collectively, our results do not support the notion that medical emergency teams reduce hospital mortality.
Prior studies on the impact of medical emergency teams on mortality in pediatric hospitals have been limited. The few studies that exist have been single-center studies4, 5, 17, 18 (thus lacking generalizability) and may have been individually underpowered for an outcome such as hospital mortality, although a few of these studies did report significantly lower hospital mortality post-implementation. Additionally, most prior studies have simply compared aggregate pre-implementation vs. post-implementation hospital mortality rates. This approach ignores mortality trends before medical emergency team implementation and could lead to incorrect inferences regarding the effect of these teams on hospital mortality. This is particularly important to consider as efforts for earlier detection and treatment of sepsis and improved intensive unit care over the past decade have resulted in lower hospital mortality. Our study extends the findings of prior studies by examining the effect of medical emergency teams across 38 hospitals, thus increasing generalizability and statistical power. By controlling for pre-implementation hospital mortality trends (which were decreasing by a mean of 6.0% annually in our study sample), we found that hospital mortality rates were nearly identical to what would have been expected had a medical emergency team not been put into place. Moreover, by leveraging data involving over 6 million hospitalizations, we determined that our study had 80% power to detect even a small decrease of 2 deaths per 10,000 admissions annually with medical emergency team implementation.
The Institute of Healthcare Improvement has proposed implementation of medical emergency teams as 1 of 6 strategies to avoid preventable hospital deaths.1 Ideally, medical emergency teams are deployed to treat patients with acute physiological decline to prevent in-hospital cardiac arrest, which has a low survival rate of 20% to 25%.2 Reducing the morbidity and mortality of in-hospital cardiac arrest has been a focus of the American Heart Association and the Institute of Medicine, with the latter issuing a call to action in 2016 given the high prevalence and mortality associated with cardiac arrest events.19 In theory, by reducing the occurrence and morbidity associated with in-hospital cardiac arrest, medical emergency teams can also reduce hospital mortality and improve patient safety and outcomes.
Whether a hospital activates a medical emergency team in a consistent manner to respond to patients with acute physiological decline to realize these gains, however, is less clear. A recent study of 21,913 adult patients with in-hospital cardiac arrest from 274 hospitals found that only 1 in 6 patients had a medical emergency team evaluation prior to cardiac arrest, and, of those without an evaluation, 40% had evidence of severe vital sign derangement at least 1 hour prior to cardiac arrest that could have prompted evaluation by a medical emergency team but did not.20 Thus, the lack of significant benefit from medical emergency teams observed in this study may be due to their suboptimal implementation in routine practice, and it is possible that these teams could reduce hospital mortality if better protocols and implementation were developed. Given that our study is, to date, the largest to evaluate the effect of medical emergency team implementation on hospital mortality and exceeds the number of hospitals in the pediatric medical emergency team literature, it will be critical that future studies test specific designs of medical emergency team implementation, activation, and staff response to determine how best to realize the potential benefits of these teams.
Although studies have reported a decrease in cardiac arrest rates after implementation of a medical emergency team,5, 17, 18 the discordance between a reduction in cardiac arrest rates in prior studies and hospital mortality in this study may be due to 4 reasons. First, most prior studies evaluating the effect of medical emergency teams on rates of in-hospital cardiac arrest have not accounted for pre-implementation trends, thus overestimating the benefit of these teams on lowering cardiac arrest rates. Second, because medical emergency teams transfer patients with acute physiological decline to the intensive care unit (ICU), and as most prior studies have only reported rates of non-ICU cardiac arrests (rather than hospital-wide rates), findings from these studies are subject to high levels of reporting bias since a patient transferred to the ICU by the medical emergency team with a subsequent in-hospital cardiac arrest would not have been counted in these studies’ results.21 Third, as one of the potential actions of medical emergency teams is to establish do-not-resuscitate (DNR) orders in appropriate patients, higher rates of DNR orders after medical emergency team implementation could lead to lower rates of in-hospital cardiac arrest but would not be expected to affect overall hospital mortality. Finally, even if a medical emergency team is successful in preventing an in-hospital cardiac arrest short-term, this may not be sufficient to alter overall mortality risk in critically ill patients throughout their hospitalization. These considerations highlight the importance for future studies to use rigorous methodology to adjust for pre-implementation trends and demonstrate that medical emergency teams not only decrease rates of in-hospital cardiac arrest but also hospital mortality.
Our study should be interpreted in the context of the following limitations. The PHIS database does not collect information on in-hospital cardiac arrest, and only 3 of this study’s 38 hospitals participate in the national Get With The Guidelines-Resuscitation registry for in-hospital cardiac arrest.22 Therefore, we were unable to examine the effect of medical emergency teams on rates of in-hospital cardiac arrest across the study sample. Nonetheless, our study’s mortality findings raise questions as to whether just showing lower cardiac arrest rates would be meaningful, as the latter is an “intermediate” outcome as compared with hospital mortality. Second, the PHIS database does not contain information on cause of death; therefore, we were unable to assess the impact of medical emergency teams on rates of cardiovascular mortality. Third, our study assumed that pre-implementation mortality trends would continue post-implementation. This assumption is less problematic, however, since study hospitals did not implement their medical emergency teams during the same calendar year, and it is unlikely that an external confounder was present for different years for each hospital and coincidental only during each hospital’s pre-implementation period. This is also supported by the fact that, for each calendar year, we found that the mortality rate of hospitals which had implemented their medical emergency team was not lower than hospitals which had not yet implemented their medical emergency team. Fourth, our study was unable to assess other outcomes, such as nursing satisfaction, establishment of DNR orders, and prevention of in-hospital complications. We acknowledge that there has been a significant change in hospital culture over the past decade, wherein resuscitation care is no longer perceived as futile. As such, medical emergency teams may provide important support and value for nursing staff even if they are not associated with lower hospital mortality. Fifth, we did not have detailed data on medical emergency team composition or implementation strategy at each hospital. Such information could have been used to identify medical emergency team characteristics associated with lower hospital mortality; however, since we did not detect evidence for improvement in hospital mortality in the overall study sample or in any individual hospital, this information would not have been useful in discriminating which medical emergency team designs are most effective. Sixth, all but one of the study hospitals were academic hospitals. Nonetheless, as nearly all children’s hospitals in the U.S. are academic hospitals, our findings are likely representative of pediatric centers. Finally, our study examined the effect of medical emergency teams on pediatric hospital mortality; therefore, our findings may not be generalizable to adults.
Conclusion
Across a broad range of unselected pediatric hospitals in the U.S., implementation of medical emergency teams was not associated with a reduction in hospital mortality beyond what would have been expected based on pre-implementation mortality trends.
Supplementary Material
CLINCAL PERSPECTIVE.
I. What is New?
Although most U.S. hospitals have implemented medical emergency teams to reduce hospital mortality in response to the Institute for Healthcare Improvement’s Five Million Lives Campaign, whether these teams have resulted in a reduction in hospital mortality beyond temporal trends is unclear.
We found that routine implementation of a medical emergency team in 38 freestanding pediatric hospitals was not associated with lower hospital mortality than what would have been expected based on pre-implementation trends, both overall and within each hospital.
Our study is the largest, to date, to examine the association of medical emergency team implementation on hospital mortality.
II. What Are the Clinical Implications?
Although the theoretical foundation for medical emergency teams has merit, prior studies have found that medical emergency teams are not always deployed to patients with acute physiological decline who may benefit from them.
Our study’s null findings on hospital mortality suggest that either medical emergency teams have no effect on hospital mortality, or are poorly implemented in the real-world. Further study is required to establish the effectiveness of medical emergency teams in reducing hospital mortality and whether there are specific team designs (composition, activation, and therapeutic interventions) that are effective.
Acknowledgments
Funding Sources:
Dr. Kutty is supported by funding (R41HD089823-01) from the National Institute of Child Health and Development. Dr. Chan is supported by funding (R01HL123980) from the National Heart Lung and Blood Institute.
Footnotes
- Dr. Chan has served as a consultant for the American Heart Association and Optum Rx. None of the other authors has any conflicts of interest or financial interests to disclose.
Authorship: Dr. Chan had full access to all of the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study Concept and design: Kutty, Chan
Acquisition of Data: Kutty, Karels, Joseph
Statistical Analysis: Jones, Karels
Analysis and interpretation of data: Kutty, Jones, Karels, Joseph, Spertus, Chan
Drafting of the manuscript: Kutty, Chan
Critical revision of the manuscript for important intellectual content: Kutty, Jones, Karels, Jospeph, Spertus, Chan
Study Supervision: Chan
References
- 1.Institute for Healthcare Improvement. Protecting 5 Million Lives From Harm. [Accessed February 27, 2017]; http://www.ihi.org/Engage/Initiatives/Completed/5MillionLivesCampaign/Pages/default.aspx.
- 2.Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012;367:1912–1920. doi: 10.1056/NEJMoa1109148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Devita MA, Bellomo R, Hillman K, Kellum J, Rotondi A, Teres D, Auerbach A, Chen WJ, Duncan K, Kenward G, Bell M, Buist M, Chen J, Bion J, Kirby A, Lighthall G, Ovreveit J, Braithwaite RS, Gosbee J, Milbrandt E, Peberdy M, Savitz L, Young L, Harvey M, Galhotra S. Findings of the first consensus conference on medical emergency teams. Crit Care Med. 2006;34:2463–2478. doi: 10.1097/01.CCM.0000235743.38172.6E. [DOI] [PubMed] [Google Scholar]
- 4.Tibballs J, Kinney S. Reduction of hospital mortality and of preventable cardiac arrest and death on introduction of a pediatric medical emergency team. Pediatr Crit Care Med. 2009;10:306–312. doi: 10.1097/PCC.0b013e318198b02c. [DOI] [PubMed] [Google Scholar]
- 5.Sharek PJ, Parast LM, Leong K, Coombs J, Earnest K, Sullivan J, Frankel LR, Roth SJ. Effect of a rapid response team on hospital-wide mortality and code rates outside the ICU in a Children's Hospital. JAMA. 2007;298:2267–2274. doi: 10.1001/jama.298.19.2267. [DOI] [PubMed] [Google Scholar]
- 6.Maharaj R, Raffaele I, Wendon J. Rapid response systems: a systematic review and meta-analysis. Crit Care. 2015;19:254. doi: 10.1186/s13054-015-0973-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS American Heart Association Get with the Guidelines-Resuscitation I. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012;367:1912–1920. doi: 10.1056/NEJMoa1109148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson ML, Nichol G, Dai D, Chan PS, Thomas L, Al-Khatib SM, Berg RA, Bradley SM, Peterson ED American Heart Association's Get With the Guidelines-Resuscitation I. Association Between Hospital Process Composite Performance and Patient Outcomes After In-Hospital Cardiac Arrest Care. JAMA Cardiol. 2016;1:37–45. doi: 10.1001/jamacardio.2015.0275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369:840–851. doi: 10.1056/NEJMra1208623. [DOI] [PubMed] [Google Scholar]
- 10.Kumar G, Kumar N, Taneja A, Kaleekal T, Tarima S, McGinley E, Jimenez E, Mohan A, Khan RA, Whittle J, Jacobs E, Nanchal R Milwaukee Initiative in Critical Care Outcomes Research Group of I. Nationwide trends of severe sepsis in the 21st century (2000–2007) Chest. 2011;140:1223–1231. doi: 10.1378/chest.11-0352. [DOI] [PubMed] [Google Scholar]
- 11.Zimmerman JE, Kramer AA, Knaus WA. Changes in hospital mortality for United States intensive care unit admissions from 1988 to 2012. Crit Care. 2013;17:R81. doi: 10.1186/cc12695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Danford DA, Karels Q, Kulkarni A, Hussain A, Xiao Y, Kutty S. Mortality-related resource utilization in the inpatient care of hypoplastic left heart syndrome. Orphanet J Rare Dis. 2015;10:137. doi: 10.1186/s13023-015-0355-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Averill RF, McCullough EC, Goldfield N, Hughes JS, Bonazelli J, Bentley L, Muldoon J, Turner L. 3M APR DRG Classification System. 31. Wallingford, CT: Agency for Healthcare Research and Quality; 2013. pp. 1–98. Report No.: GRP-041. [Google Scholar]
- 14.Parker MW, Shah SS, Hall M, Fieldston ES, Coley BD, Morse RB. Computed Tomography and Shifts to Alternate Imaging Modalities in Hospitalized Children. Pediatrics. 2015;136:e573–581. doi: 10.1542/peds.2015-0995. [DOI] [PubMed] [Google Scholar]
- 15.Jones HE, Ohlssen DI, Spiegelhalter DJ. Use of the false discovery rate when comparing multiple health care providers. J Clin Epidemiol. 2008;61:232–240. doi: 10.1016/j.jclinepi.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 16.Team RDC. R: A language and environment for statistical computing. R Foundation for Statistical Computing V; Austria: 2008. URL http://www.R-project.org. [Google Scholar]
- 17.Zenker P, Schlesinger A, Hauck M, Spencer S, Hellmich T, Finkelstein M, Thygeson MV, Billman G. Implementation and impact of a rapid response team in a children's hospital. Joint Commission journal on quality and patient safety / Joint Commission Resources. 2007;33:418–425. doi: 10.1016/s1553-7250(07)33048-1. [DOI] [PubMed] [Google Scholar]
- 18.Brilli RJ, Gibson R, Luria JW, Wheeler TA, Shaw J, Linam M, Kheir J, McLain P, Lingsch T, Hall-Haering A, McBride M. Implementation of a medical emergency team in a large pediatric teaching hospital prevents respiratory and cardiopulmonary arrests outside the intensive care unit. Pediatr Crit Care Med. 2007;8:236–246. doi: 10.1097/01.PCC.0000262947.72442.EA. [DOI] [PubMed] [Google Scholar]
- 19.Strategies to Improve Cardiac Arrest Survivial: A Time to Act. Institute of Medicine; Washington, D.C.: 2015. [Google Scholar]
- 20.Chan ML, Spertus JA, Tang F, Jayaram N, Chan PS. Missed opportunities in use of medical emergency teams prior to in-hospital cardiac arrest. Am Heart J. 2016;177:87–95. doi: 10.1016/j.ahj.2016.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid Response Teams: A Systematic Review and Meta-analysis. Arch Intern Med. 2010;170:18–26. doi: 10.1001/archinternmed.2009.424. [DOI] [PubMed] [Google Scholar]
- 22.Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, Berg RA, Nichol G, Lane-Trultt T. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.