Abstract
Background:
A validated questionnaire is needed to study a more holistic outcome assessment including postsurgical aesthetic satisfaction and psychosocial changes in orthognathic patients. The aim of this study was to determine the reliability and validity of 9 orthognathically relevant translated FACE-Q scales among Hong Kong Chinese orthognathic patients.
Methods:
Two hundred fifty adult Cantonese-speaking patients of 18 years or older who underwent orthognathic treatment were recruited in the Prince Philip Dental Hospital of Hong Kong. Nine of an overall of 40 independent FACE-Q scales were selected and translated into Hong Kong Chinese. The reliability, validity, and test–retest reliability were examined using Cronbach’s alpha, paired t test and Pearson’s correlation coefficients.
Results:
The Hong Kong Chinese version of the 9 FACE-Q scales was obtained by forward-backward translation. One hundred eight male (mean age, 25.57 ± 4.49) and 142 female (mean age, 24.61 ± 4.54) patients were recruited for the reliability and validation process. The internal consistency (0.89–0.97) and the test–retest reliability (0.73–0.90) were found to be high. The validity of the translated questionnaires was comparable with that of the original FACE-Q.
Conclusion:
The results presented here prove that the 9 translated FACE-Q scales are reliable and valid instruments for research and clinical purposes in Hong Kong Chinese orthognathic patients.
BACKGROUND
Orthognathic surgery represents the mainstay in the surgical treatment for patients with dentofacial deformities.1 Literature revealed that the main motives of patients who seek orthognathic treatment are improvements in self-confidence, appearance, and oral function.2 Even though it is important as functional and psychosocial outcomes, the scientific exploration of postsurgical aesthetic satisfaction in orthognathic patients still is meager. A more holistic assessment of orthognathic surgical outcomes should include the appraisals of postsurgical patients’ satisfaction with facial appearance, functional and psychosocial changes.
FACE-Q is a recently developed patient-reported outcome (PRO) instrument that encompasses a set of more than 40 independently functioning scales and checklists measuring concepts and symptoms important to facial aesthetics of patients in relation to different facial areas.3 These scales and checklists cover 4 different categories: appearance appraisal, quality of life, adverse effect, and patient’s experience.3 As these 4 categories together broadly cover the surgical outcome assessments in patients after orthognathic surgery, they are of utmost interest for research and clinical purposes. Each scale/checklist functions autonomously. Clinicians and researchers may select and apply particularly relevant scales to their patients. This turns FACE-Q into both a practical and unique instrument.
The original development and validation of the English FACE-Q scales have already been reported elsewhere.3–6 However, a validation exercise became necessary before applying the translated questionnaires in orthognathic patients in Hong Kong. Translations further provide the possibility to explore questionnaires’ utility across populations and languages, as well as their cross-cultural validity that allows international valid comparisons of results or findings.
This study aimed to translate and validate 9 FACE-Q scales into Hong Kong Chinese and examine their reliability and validity in the assessment of postsurgical satisfaction with the facial appearance, decision and outcome, and psychosocial changes in Cantonese-speaking patients after orthognathic surgery.
METHODOLOGY
The Institutional Review Board of The University of Hong Kong has granted the ethical approval for this cross-sectional study (IRB no: UW 16–240). The study was conducted at Prince Philip Dental Hospital, The University of Hong Kong, Hong Kong S.A.R..
Translation and Linguistic Validation
Nine FACE-Q scales and 1 FACE-Q checklist that are relevant to orthognathic surgery have been selected in this study (Table 1). The selected original FACE-Q scales and checklist were obtained from the authorities of MAPI Research Trust (https://eprovide.mapi-trust.org) with the permission of the developers. Two local native Cantonese-speaking dentists translated the selected scales and checklist into Hong Kong Chinese. Subsequently, an independent bilingual third local dentist performed the backward translation of these questionnaires. The translated version was compared with the original version, and minor discrepancies were revised based on a consensus after discussion among all involved parties. The translated scales and checklist have been tested in a pilot study on a convenient sample of 10 orthognathic patients attending the orthognathic review clinic at Oral and Maxillofacial Surgery outpatient station of the Prince Philip Dental Hospital in Hong Kong. The report on the forward–backward translation and pilot testing was subsequently submitted to the developer of the FACE-Q for approval. The flow chart in Figure 1 illustrates the translation process.
Table 1.
Selected FACE-Q Scales/Checklist
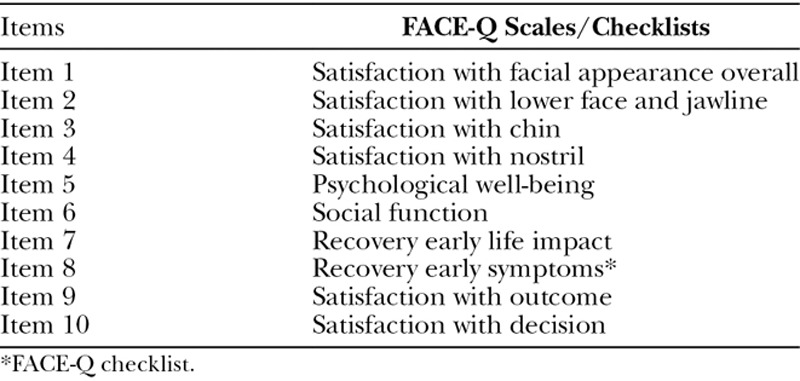
Fig. 1.
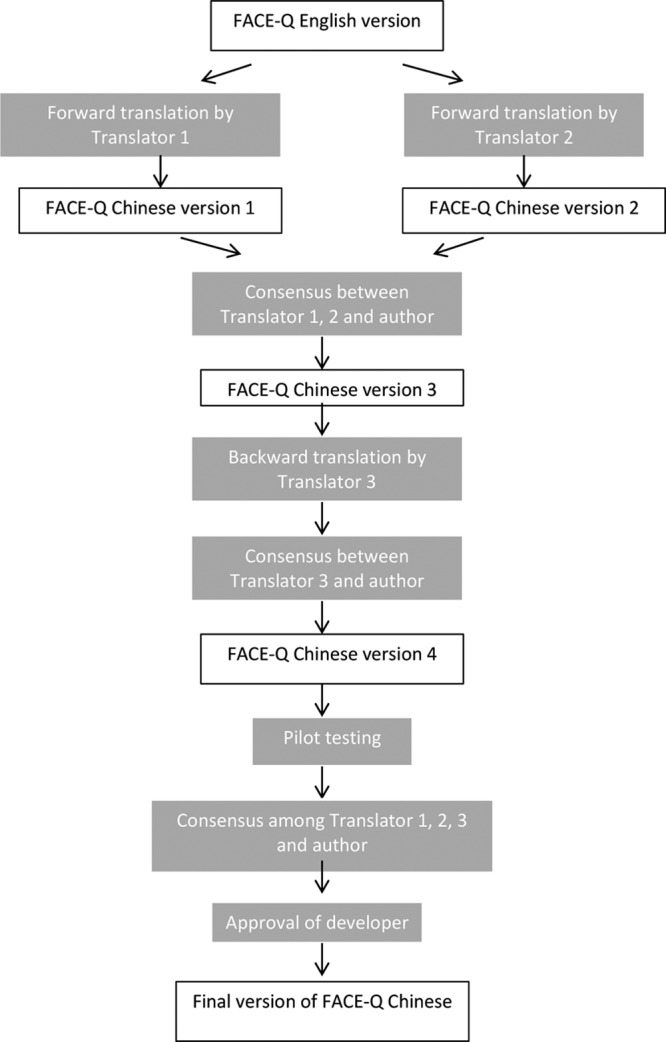
Flow chart of translation process.
Validity and Reliability
The cross-sectional study was conducted at the Department of Oral and Maxillofacial Surgery, Prince Philip Dental Hospital, The University of Hong Kong. All participants received an information sheet containing the study’s aim and describing its process. All participants agreed to participate voluntarily in the study and signed a written consent form. They previously were enlightened that they had the right to withdraw from the study anytime without providing any reason. Self-administered questionnaires of the translated final version of the Cantonese FACE-Q version were distributed to orthognathic patients aged 18 years old or older who have attended the orthognathic review clinic with the convenient sampling method. All patients completed the questionnaire unaided and independently. Additionally, 40 participants attending the long-term postsurgical review clinic received the same set of questionnaires, which they had to fill in 2 weeks later at home before returning them in self-addressed stamped envelopes.
Demographic variables of all subjects were recorded. Patients suffering from cleft lip and palate and those with syndromes were excluded from this study.
Data Analysis
The total score for each FACE-Q scales was calculated by adding the scores of the responses to each item of that particular questionnaire. Data analysis was performed using the software IBM SPSS Statistics for Windows, version 23.0.0.2 (IBM Corp., Armonk, New York, USA). Descriptive statistics were used to analyze socio-demographic characteristics and clinical data of all participants.
Each FACE-Q scale was examined for its internal reliability using Cronbach’s alpha test; the test–retest reliability was assessed using Pearson’s correlation. A Cronbach’s alpha of > 0.70 and item-total correlation coefficients of > 0.20 were regarded as good. The level of significance was set at 0.05 for all statistical tests. The validity was assessed in the following aspects:
Presurgical and postsurgical scores for scales 1–6* were compared to examine the contrast validity with paired t test with 95% CI. Postsurgical scores were predicted to be significantly higher, as it was assumed that patients after orthognathic surgery were more satisfied with their appearance and showed a better psychosocial status.
Scores for the scales 1–6* and 9–10* were correlated to determine the extent they measure separate but related constructs.3 These intercorrelations were hypothesized to be moderate, ranging between r = 0.30 to r = 0.70, as these scales were developed to measure distinct but related clinical variables.3
Scores for the scales/checklist 1–10* were correlated with patients’ characteristics (ie, age and sex) to determine the extent to which a scale may be susceptible to bias due to these sociodemographic variables.3 The correlations were predicted to be low (< 0.30).3
-
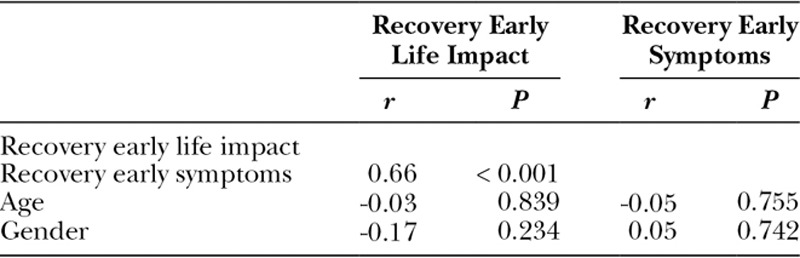
The Early Life Impact of Treatment scale score (scale 7*) was correlated with the Recovery Early Symptom checklist (checklist 8). It was hypothesized that a higher Early Life Impact of Treatment score, that is, worse health-related quality of life during the recovery phase, would correlate with more symptoms.3
(*Scales numbering referring to Table 1.)
RESULTS
Participants
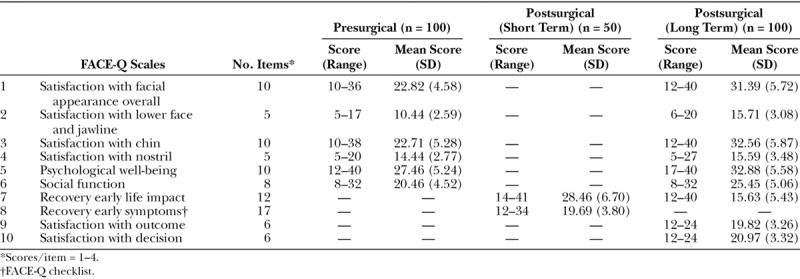
A total of 250 orthognathic patients, 142 women and 108 men, were recruited for validity and reliability testing of translated Hong Kong Chinese FACE-Q questionnaires. The mean age between males (25.57 ± 4.49) and females (24.61 ± 4.54) did not differ significantly. Only 22 of the 40 test–retest participants have returned the second set of the questionnaires by mail, resulting in a response rate of 55%. All subjects were local Hong Kong Chinese. The characteristics of the participants are summarized in Table 2. The scores for each FACE-Q scale are highlighted in Table 3.
Table 2.
Demographic Characteristics of Recruited Participants
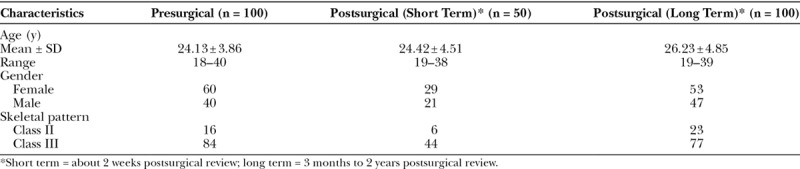
Table 3.
Mean Scores for FACE-Q Scales/Checklist
Reliability
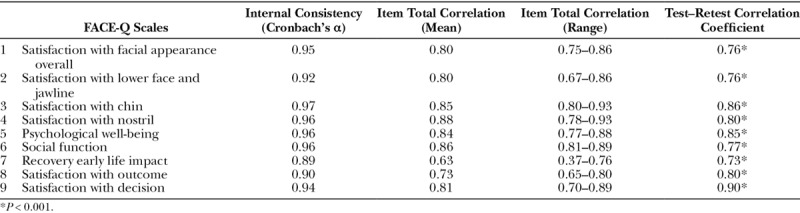
The reliability tests were performed on postsurgical data (Table 4). In brief, all FACE-Q scales showed high Cronbach’s alpha coefficients scores, displaying a good internal consistency. All Item Total Correlation values were found to be good, and the test–retest correlation coefficients were high.
Table 4.
Reliability Tests for FACE-Q Scales
Validity
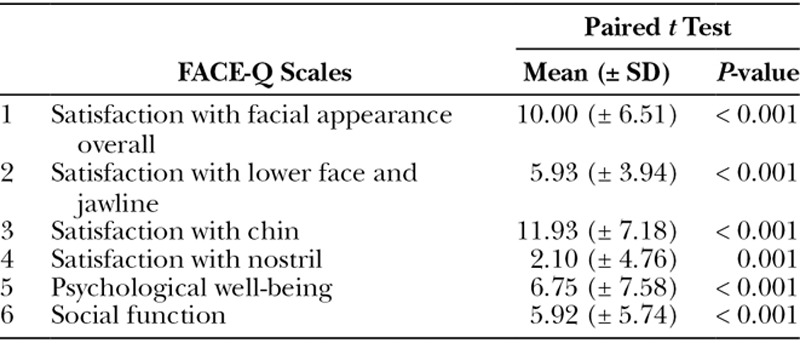
Sixty-one pairs of pre- and postsurgical long-term patients were matched based on gender, age, and skeletal pattern. Paired t tests were performed on 6 FACE-Q scales (Table 5). All scales showed significantly increased (P < 0.001) mean postsurgical compared with presurgical scores, as predicted.
Table 5.
Validity Tests for FACE-Q Scales
The correlations of 6 FACE-Q scales pertaining to satisfaction of facial appearance and psychosocial status were analyzed (Table 6). The correlations ranged from 0.37 to 0.57. The correlation of 2 other scales related to satisfaction to outcome and decision displayed an r = 0.70 (Table 7). These findings suggest that these scales measure distinct but related clinical variables. A strong correlation, r = 0.66, exists between the Early Recovery Symptoms and the Recovery Early Life Impact scores in early postsurgical patients (Table 8), whereas correlations between all FACE-Q scales relate to age and gender displayed a value < 0.30. All correlations were found to fall within the range of hypothesized values.
Table 6.
Correlation of FACE-Q Scales Related to Satisfaction to Facial Appearance and Psychosocial Status
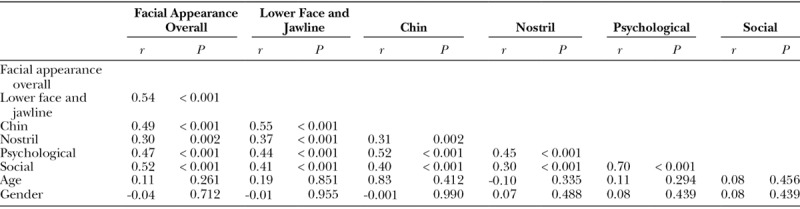
Table 7.
Correlation of FACE-Q Scales Related to Satisfaction to Outcome and Decision
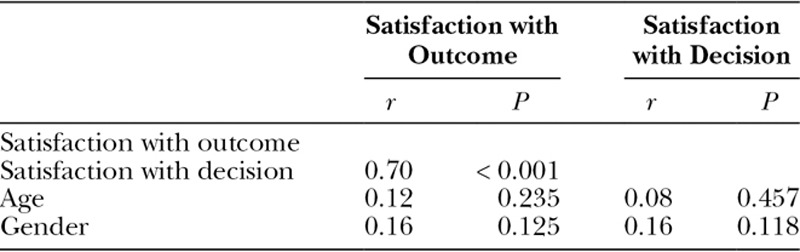
Table 8.
Correlation of FACE-Q Scales/Checklist Related to Recovery Early Life Impact and Symptoms
DISCUSSION
The 9 translated FACE-Q scales presented here are reliable and valid instruments to assess appearance appraisal, quality of life, adverse effect, and patient’s experience in native Cantonese-speaking orthognathic patients in Hong Kong. FACE-Q is currently the only PRO instrument including scales that measure facial appearance.7 The 9 translated FACE-Q scales are valuable PRO instruments to assess orthognathic patients’ domains, such as satisfaction to facial appearance, psychosocial status, and satisfaction with decision and outcome using simple and easy self-administered questionnaires.
Translation and validation of PRO instruments are mandatory steps to ensure their cross-cultural adaptive capacity for comparative international research trials and clinical applications. The results of this study revealed that the Hong Kong Chinese version of the translated FACE-Q scales is equivalent to the original English FACE-Q parts, showing similar reliability and validity values. This translated version, hence, is both reliable and valid without any structural change, maintaining all original items.
The reliability of the FACE-Q was tested with Cronbach’s alpha. A good internal consistency corresponds to values of > 0.70.8 Therefore, all 9 tested FACE-Q scales have demonstrated a very high internal reliability, comparable with those values of the original internal reliability testing.5,9,10
The following study limitations are worth mentioning. First, the different patient samples for the pre- and postsurgical groups. Orthognathic surgical treatment represents a long process that easily can take years from the patients’ first clinical examination to the eventual orthognathic surgery with postsurgical orthodontic refinement. Therefore, a cross-sectional study design was chosen to more swiftly collect the data, even though this resulted in a consequently partial subject matching for data analysis. Second, it might be considered as a shortcoming to have recruited mainly orthognathic patients with skeletal class III pattern. However, unfortunately there is not much one can do about it, as this dentoalveolar growth pattern represents the usual clinical patient sample referred for orthognathic surgery in Hong Kong.
CONCLUSIONS
The Hong Kong Chinese versions of FACE-Q scales presented here are reliable and valid instruments to assess the satisfaction and psychosocial status of Hong Kong Chinese orthognathic patients in research trials as well as daily clinical applications.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Soh CL, Narayanan V. Quality of life assessment in patients with dentofacial deformity undergoing orthognathic surgery—a systematic review. Int J Oral Maxillofac Surg. 2013;42:974–980.. [DOI] [PubMed] [Google Scholar]
- 2.Alanko OM, Svedström-Oristo AL, Tuomisto MT. Patients’ perceptions of orthognathic treatment, well-being, and psychological or psychiatric status: a systematic review. Acta Odontol Scand. 2010;68:249–260.. [DOI] [PubMed] [Google Scholar]
- 3.Klassen AF, Cano SJ, Schwitzer JA, et al. FACE-Q scales for health-related quality of life, early life impact, satisfaction with outcomes, and decision to have treatment: development and validation. Plast Reconstr Surg. 2015;135:375–386.. [DOI] [PubMed] [Google Scholar]
- 4.Klassen AF, Cano SJ, Scott A, et al. Measuring patient-reported outcomes in facial aesthetic patients: development of the FACE-Q. Facial Plast Surg. 2010;26:303–309.. [DOI] [PubMed] [Google Scholar]
- 5.Pusic AL, Klassen AF, Scott AM, et al. Development and psychometric evaluation of the FACE-Q satisfaction with appearance scale: a new patient-reported outcome instrument for facial aesthetics patients. Clin Plast Surg. 2013;40:249–260.. [DOI] [PubMed] [Google Scholar]
- 6.Sinno S, Schwitzer JA, Anzai L, et al. Facelift satisfaction using the FACE-Q. Plast Reconstr Surg. 2015;136:144. [DOI] [PubMed] [Google Scholar]
- 7.Klassen AF, Cano SJ, Schwitzer JA, et al. Development and psychometric validation of the FACE-Q skin, lips, and facial rhytids appearance scales and adverse effects checklists for cosmetic procedures. JAMA Dermatol. 2016;152:443–451.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.LJ C. Coefficient alpha and the internal structure of tests. Psychometrika 1951;16:297–334.. [Google Scholar]
- 9.Klassen AF, Cano SJ, Scott AM, et al. Measuring outcomes that matter to face-lift patients: development and validation of FACE-Q appearance appraisal scales and adverse effects checklist for the lower face and neck. Plast Reconstr Surg. 2014;133:21–30.. [DOI] [PubMed] [Google Scholar]
- 10.Klassen AF, Cano SJ, East CA, et al. Development and psychometric evaluation of the FACE-Q scales for patients undergoing rhinoplasty. JAMA Facial Plast Surg. 2016;18:27–35.. [DOI] [PMC free article] [PubMed] [Google Scholar]


