Abstract
Information on surgical site infection (SSI) after surgical treatment of ankle fracture is limited and remains controversial. The purpose of the present study was to determine the incidence and risk factors for SSI after open reduction and internal fixation (ORIF) of ankle fracture. Patients who underwent ORIF for ankle fracture at 3 centers between January 2015 and December 2016 were included. The potential risk factors for SSI included demographic variables, including age, sex, body mass index (BMI), hypertension, diabetes mellitus, heart disease, smoking, and excessive alcohol intake; blood test variables including preoperative white blood cell count, neutrophil count, red blood cell count, hemoglobin, total protein, albumin and globulin; injury- and surgery-related variables, including duration of operation (minutes), intraoperative blood loss, surgeon level, fracture site, accompanied dislocation, use of a drainage tube, and antibiotic use. Factors related with SSI occurrence were investigated by univariate analysis, and then by multivariate analysis. During hospitalization, 4.37% (66/1511) of patients developed SSI, which was deep in 1.32% (20/1510) and superficial in 3.05% (46/1510). The most common causative agent was polymicrobial (causing approximately half of all SSIs), followed by methicillin-resistant Staphylococcus aureus (MRSA). Multivariate analysis revealed that the significant risk factors for SSI occurrence were open injury, advanced age, incision cleanliness II – IV, high-energy injury, more experienced surgeon level, greater BMI, chronic heart disease, history of allergy, and preoperative neutrophil count > 75%. Preoperative preventative measures should be taken in patients with these conditions to lower the incidence of SSI after ORIF of ankle fracture.
LEVEL OF EVIDENCE: Level III - Retrospective Comparative Study.
Keywords: ankle fracture, incidence and risk factors, open reduction and internal fixation, surgical site infection
1. Introduction
Ankle fractures are commonly seen in all age groups, accounting for approximately 50% of fractures of the tibia and fibula, and 7.6% of all fractures in adults.[1] With the aging population, the incidence and number of ankle fractures is increasing, trailing only hip and wrist fractures.[1,2] Although some ankle fracture types caused by simple injuries can achieve beneficial results via conservative treatments, the most prevalent treatment method for ankle fractures is surgical, especially open reduction and internal fixation (ORIF)[3–5]; there is substantial evidence to support the use of ORIF rather than conservative management.[6,7] However, surgical treatment of ankle fracture also has some disadvantages, including a high incidence of postoperative complications, and even ORIF itself carries an inherent risk of complications.
Of the complications associated with ORIF, surgical site infection (SSI) is the most common hospital-acquired infection. SSI negatively affects bony union and functional recovery of the ankle. Previous studies have identified some risk factors associated with SSI after surgical treatment of ankle fracture,[8–12] including advanced age, more severe injury type (open fracture, trimalleolar fracture, fracture with an accompanying dislocation, Weber type C fracture, higher grade soft tissue injury), delayed duration of operation (minutes), greater BMI, smoking, diabetes mellitus, and nursing home residence.[5,9,11,12] However, most of these studies were performed in a single institution, or were focused on a specific patient population,[10,13,14] which caused limitations due to small sample size and weak statistical power. In addition, the use of univariate analyses rather than multivariate analysis meant that the influence of some risk factors was reported as inconclusive, and their independent effects were not confirmed.[11,12] Furthermore, some variables with potential predictive value remain underreported or unreported, such as surgeon experience level, preoperative neutrophil count (NEUT), total protein (TP), and serum albumin concentration (ALB).[10,15]
We conducted this retrospective multicenter study with 3 aims: to investigate the incidence rate and characteristics of SSI after ORIF of ankle fracture during hospitalization; to test the hypothesis that some biochemical indicators [preoperative white blood cell count (WBC), NEUT%, TP, and ALB] were predictors of SSI occurrence, and to identify other risk factors, if any.
2. Materials and methods
2.1. Study design
We conducted this retrospective study at 3 level I institutions: the Third Hospital of Hebei Medical University, Handan branch of the Jizhong Energy Fengfeng Group General Hospital, and Xingtai People's Hospital. The institutional review boards from each of these 3 centers approved the present study before study commencement. The electronic medical records (EMRs) were searched to identify all adult patients (18 years and older) who had undergone ORIF to treat ankle fracture in the period from January 2015 to December 2016. The exclusion criteria were patient age < 18 years, pathological fractures, old fractures (>21 days after initial injury), and treatments rather than ORIF (external fixation, conservative treatments, manual reduction and internal fixation, traction).
2.2. Data collection for variables of interest
EMRs were searched for variables of interest, including demographics, injury- and surgery-related characteristics, and biochemical indicators. Demographic characteristics included sex, age, profession, height, weight, BMI (kg/m2), smoking status, alcohol intake, comorbidities (hypertension, diabetes mellitus, chronic heart disease), previous history of surgery at any site, and allergy history. Injury-related variables included mechanism (low- or high-energy injury), fracture type (open or closed; uni-, bi-, or trimalleolar), and presence or absence of accompanying dislocation. We defined low-energy injuries as simple falls from standing height, and defined high-energy injuries as traffic accidents, falls from a substantial height, violent collisions, and sporting activity. Surgery-related variables included surgeon level (Chief Surgeon or Deputy Chief Surgeon), preoperative hospitalization (between initial injury and operation), incision cleanliness, anesthetic type, duration of operation(min), intraoperative blood loss, pre-, intra- and postoperative antibiotic use, postoperative drainage, and American Society of Anesthesiologists (ASA) grade. Generally, prophylactic preoperative antibiotics were given to patients 30 minutes before start of surgery, and these included cefalotin, cloxacillin, clindamycin, others, or combinations. If the duration of operation was longer than 3 hours, use of antibiotic prophylaxis was redosed, in accordance with our institution's surgical protocol. Biochemical indicators included preoperative levels of WBC, NEUT, lymphocytes, red blood cells (RBCs), hemoglobin, TP, ALB, globulin, and blood glucose.
2.3. Definition of surgical site infection
SSI was defined according to the Center for Disease Control guidelines.[16] EMR and microbiological records were reviewed for recorded signs, symptoms of SSI, and bacterial culture results.
Deep SSIs were defined as infections involving deep soft tissue, muscle, or fascia; persistent wound discharge or dehiscence; visible abscess or gangrene that required surgical debridement and implant exchange or removal. Any patient who commenced antibiotic treatment for wound problems (redness, swelling, heat, or pain), but did not meet the criteria for diagnosis of deep SSI was deemed to have a superficial SSI, irrespective of any microbiology results.
2.4. Statistical analysis
Univariate analysis of continuous variables was performed using the Mann–Whitney U test or the Student t test, depending on the normality of the data. Univariate Chi-squared or Fisher's exact testing was used to evaluate the differences in variables between the 2 groups. Finally, all variables were entered into a multivariable logistic regression model using the backward step-by-step method to identify the independent risk factors for SSI. The Hosmer–Lemeshow test was used to evaluate the goodness-of-fit of the final model; P < .05 indicated an acceptable result, and Nagelkerke R2 was used to quantify the goodness-of-fit. All statistical tests were performed using the SPSS 19.0 software package (SPSS Inc., Chicago, IL).
3. Results
3.1. Overall fracture characteristics
During the study period, a total of 1543 patients with ankle fractures treated by ORIF were initially screened, but 6 cases in which the patient died and 27 cases with incomplete data were excluded. Therefore, 1510 patients (843 males, 667 females) were included in the final analysis. SSI occurred in 34 of 843 males (4.03%), and 32 of 667 females (4.80%; P = .471). Table 1 summarizes the demographic characteristics. The overall mean patient age was 47.9 years (range, 18–86 years), and the mean age of patients with SSI was significantly greater than those without SSI (P = .022). Most patients were peasants, accounting for 70.0% of all patients, and peasants accounted for 65.1% (43/66) of all SSI cases. Nearly 71% of the ankle fractures were caused by low-energy injury (1070/1510), and 6.6% (100/1510) were open fractures. Regarding the fracture site, there were 653 cases (43.2%) of unimalleolar fractures, 472 (31.3%) bimalleolar fractures, and 385 (25.5%) trimalleolar fractures; 318 (21.1%) fractures were accompanied by dislocation. ORIF was performed a mean of 4.5 days after the injury, and 73.2% (1105/1510) underwent ORIF within 1 week after injury. Only 35.2% (558/1510) of patients had drainage via a tube, strip, or others. The mean total hospital stay were 16.2 days; the mean duration of hospitalization in the SSI group was significantly longer than that in the non-SSI group (P < .001).
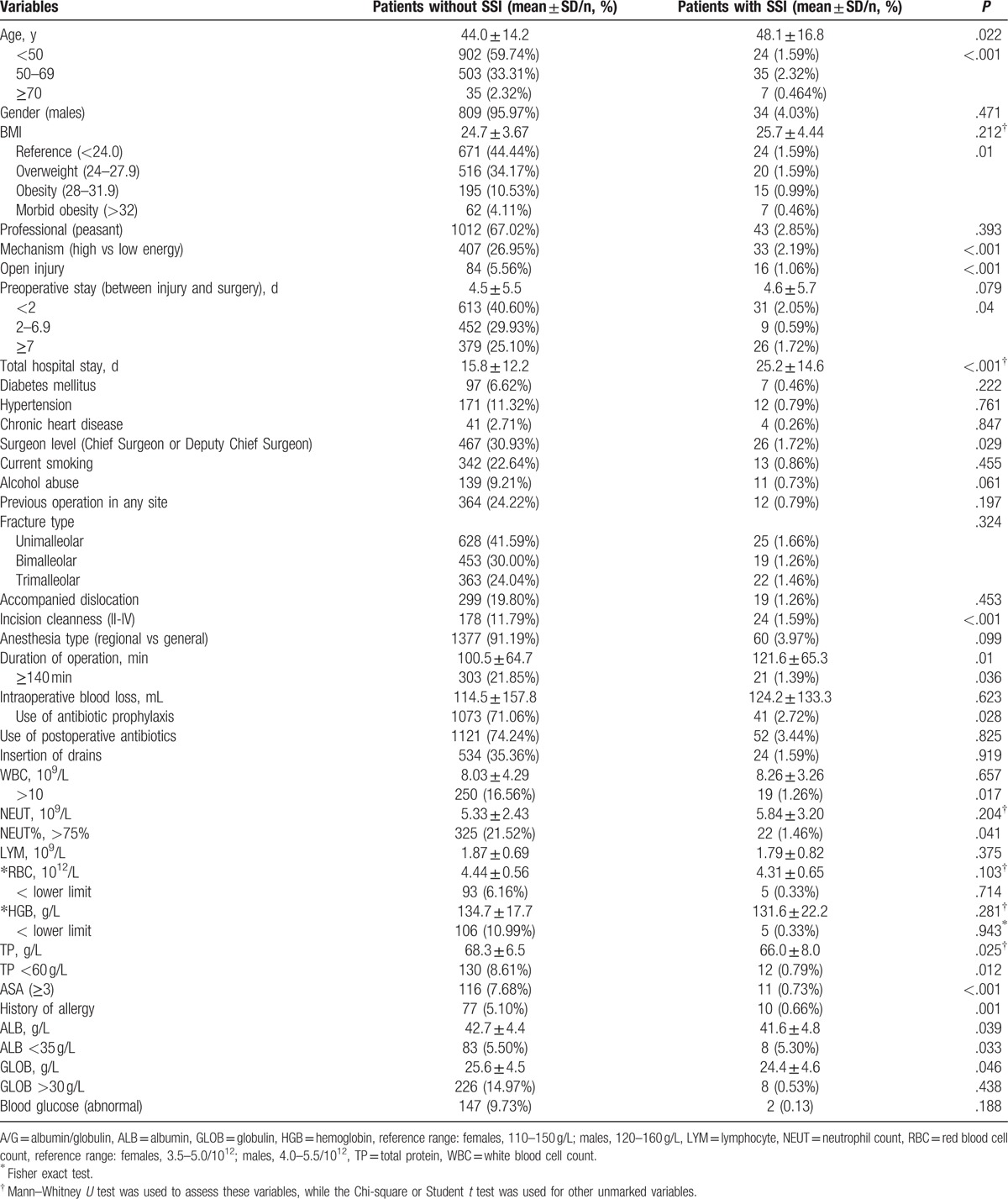
Table 1.
Univariate comparison of variables between ankle fracture patients with and without surgical site infection (SSI).
3.2. Characteristics of surgical site infections
During hospitalization (range, 4–109 days), 66 SSIs occurred, indicating an incidence of 4.37%; 20 (1.32%) were deep SSI, and 46 (3.05%) were superficial SSI. Secretion and swabs from all the deep SSI and from 17 superficial SSI were cultured for bacterial species and drug susceptibility. The culture results showed that the causative agent was polymicrobial in 17 SSI cases (45.9%), methicillin-resistant Staphylococcus aureus (MRSA) in 11 (29.7%), methicillin-susceptible S. aureus in 6 (16.2%), Bacillus cereus in 1 (2.7%), and Enterococcus faecalis in 2 (7.4%). The earliest diagnosis of SSI was on postoperative day 1, and the latest was on postoperative day 76, with a median time from surgery to SSI diagnosis of 4.5 days. Table 1 summarizes the results of the univariate analysis. Compared with the non-SSI group, the SSI group had a significantly greater mean age, longer duration of operation(min), lower preoperative TP, lower ALB, lower globulin, and longer duration of hospitalization. The other continuous variables were similar in the SSI and non-SSI groups.
3.3. Univariate and multivariate analysis
Univariate analysis revealed that the significant risk factors for development of SSI after ORIF of ankle fracture were older age, greater BMI, high-energy injury, open injury, delayed surgery, surgeon level of archiater or vice archiater, incision cleanliness grade 2–4, duration of operation (minutes) ≥ 140 minutes, preoperative WBC > 10∗109/L, NEUT > 75%, TP < 60 g/L, history of allergy, ASA grade ≥3, and ALB < 35 g/L. The other assessed variables were not significant risk factors for SSI occurrence, including sex, profession, underlying diseases such as diabetes mellitus, hypertension, chronic heart disease, current smoking, excessive alcohol intake, previous operation at any site, fracture type, accompanying dislocation, anesthetic type, preoperative antibiotic use, postoperative antibiotic use, drainage use, preoperative RBC, hemoglobin, and globulin. Use of intraoperative antibiotics significantly reduced the incidence of SSI (P = .028). The detailed information is presented in Table 1.
All the variables identified as significant risk factors for SSI occurrence after ORIF for ankle fracture in the univariate analysis were then entered into the multivariate logistic regression model. The multivariate analysis results are detailed in Table 2. After adjusting for confounding factors, the significant risk factors for SSI occurrence were open injury, older age, incision cleanliness grade 2 to 4, high-energy injury, surgeon level of archiater or vice archiater, greater BMI, chronic heart disease, history of allergy, and preoperative NEUT > 75%.
Table 2.
Multivariate analysis of factors associated with surgical site infection after open reduction and internal fixation of ankle fracture.
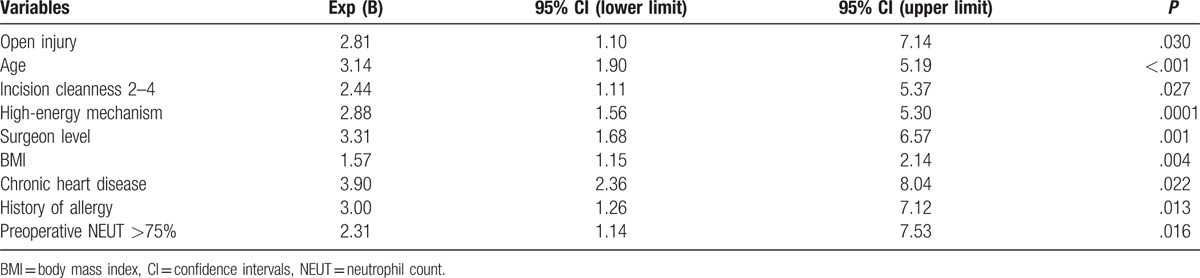
The Hosmer–Lemeshow test demonstrated adequate fitness of the final model (X2 = 4.535, P = .801; Nagelkerke R2 = 0.265).
4. Discussion
The incidence rate of SSI following surgical treatment of ankle fracture reportedly varies from 1.1% to 40%,[9,12,17,18] mainly dependent on the study design, definition of SSI, comorbid medical conditions, and surgical methods. Although many studies have investigated the risk factors or predictors of SSI after ORIF of ankle fracture, very few have focused on the surgeon experience level and perioperative biochemical indicators. To address this issue, we performed the present retrospective multivariate study using data from 3 level I hospitals. The present results showed that the incidence rate of SSI during hospitalization after ORIF of ankle fracture was 4.37%, and that the independent risk factors for SSI occurrence were advanced age, open injury, incision cleanliness grade 2 to 4, high-energy mechanism of injury, surgeon level of archiater or vice archiater, greater BMI, chronic heart disease, and a history of allergy. Preoperative NEUT > 75% within 24 hours was a significant predictor of SSI, and the odds ratio in patients with NEUT > 75% was 2.31-fold greater than in those with normal NEUT. Nearly half of all SSI cases were caused by multiple microorganisms, while the second most common cause of SSI was MRSA. Patients with SSI had to remain hospitalized for significantly longer than those without SSI, approximately 9.4 days for each case. Identification of these SSI risk factors could be of great importance for clinicians to evaluate the postoperative risk of SSI in patients who are scheduled to undergo ORIF for ankle fracture.
The incidence of SSI is reportedly 1.1% to 6% for deep SSI, and 2.6% to 24% for superficial SSI.[5,9,10,12,13,19] This wide variation in the literature may reflect differences in the definition of SSI, study design, inclusion of participants, and hospital or surgeon levels. In the present study, we observed a relatively low rate of superficial (3.05%) and deep SSI (1.32%), which approached the lower limits of the ranges reported previously (1.1% for deep SSI; 2.6% for superficial SSI). We attributed this to the strict inclusion and exclusion criteria applied in the present study. A large-sample UK study that included 710 patients aged > 18 years with closed and open ankle fractures treated by ORIF reported similar results to the present study, with incidences of 1.1% for deep SSI and 2.9% for superficial SSI.[9] In addition, the SSI rate after open ankle fracture in the present study was 16% (16/100), which was in the range of previously reported data (6–40%).[17,18] It is not possible to make direct comparisons among studies with homogeneous participants, surgical techniques, and hospital or surgeon levels; however, these results from various studies could reflect overall trends, and provide important references for clinical surgeons.
Variables previously reported as significant risk factors for SSI after surgical treatment of ankle fracture include open injury, advanced age, poor skin condition (incision cleanliness grade 2–4), high-energy injury mechanism, and greater BMI.[8,10,12,20,21] The underlying mechanisms for SSI are summarized into several categories in the literature, such as poorer soft tissue and skin conditions (open injury and high-energy injury mechanism) and inferior systemic conditions (obesity, advanced age). In the present study, we used Chinese reference criteria to divide the patients into 4 subgroups according to BMI values: normal (≤23.9), overweight (24–27.9), obese (28–31.9), and morbidly obese (>32).[22] The present results showed that, with every 4 kg/m2 increase in BMI, the risk of SSI was significantly increased by 57%. Although the criteria used for BMI grouping in the present study were different from those applied in western countries, these results could be applicable and generalized to Asian persons. Both the univariate and multivariate analyses revealed that the presence of an ankle fracture with accompanying dislocation was not a risk factor for SSI occurrence, which was consistent with most previous studies[9,10,15,20,23]; only 2 previous studies reported accompanying dislocation as a significant risk factor for SSI,[11,12] and the results in both of these studies were obtained from univariate rather than multivariate analyses. Therefore, we infer that the relatively weak negative association of fracture dislocation with SSI was counteracted in a multivariate analysis by other more strongly associated variables such as the presence of an open fracture and high-energy injury mechanism.
An unexpected finding from the multivariate analysis was that an ankle fracture treated by an archiater or vice archiater was more likely to develop a SSI, with an incidence of 5.3%. This might be associated with the surgical classification management system used in these centers in which more severe fractures are treated by the most experienced surgeons. In the present study, an archiater or vice archiater treated 82.7% (67/81) of the open bimalleolar and trimalleolar fractures caused by high-energy injuries, compared with 56.7% of other less severe injuries.
Multivariate analysis also revealed that preoperative NEUT > 75% was a significant predictor of SSI in the present study, with an incidence rate of 6.34%. A few previous studies investigated the predictive value of some perioperative biochemical indicators (C-reactive protein values and blood leukocyte counts),[11,12,15] but none focused on the predictive value of NEUT. In the present study, 23.0% of patients had an increased NEUT within 24 hours preoperatively, and 22 of these cases developed SSI. Therefore, careful surveillance of preoperative NEUT is of clinical significance and should be considered.
Chronic heart disease and a history of allergy have not been identified as risk factors for SSI in previous studies; however, in the present study, these were 2 of the strongest associations in the multivariate analysis. We consider that susceptible physical conditions that cause hypoimmunity, such as irritable physique (history of allergy) and weak blood supply status (chronic heart disease), may have partially contributed to the occurrence of SSI. In addition, patients with chronic heart diseases (especially congestive heart failure) may have weaker venous blood flow, especially in the lower limbs and ankle joints, which could influence blood circulation and cause edema. All of these factors would negatively impact wound healing, inducing SSI occurrence. Another interesting phenomenon was that although chronic heart disease was not identified as a significant risk factor in univariate analysis, it was identified as a significant risk factor for SSI in multivariate regression analysis. This might be due to the elimination of the confounding effects of variables in the multivariate analysis. The detailed mechanism by which chronic heart or history of allergy affects SSI occurrence after ORIF of an ankle fracture remains unclear. Further study is required to determine whether commonly prescribed medications in patients with these medical conditions are associated with SSI occurrence.
It is impossible to avoid the occurrence of SSI, as almost all of the identified risk factors were not alterable. However, given that SSI causes a great economic burden and adverse consequences on functional recovery, it is of paramount importance that we make use of all available resources to reduce its incidence. Therefore, the injury characteristics, patient lifestyle habits, comorbidities, and preoperative laboratory results should be comprehensively and carefully evaluated to aid in stratifying the patients according to SSI risk and enable the implementation of appropriate preventive measures.
The limitations of our study are predominantly due to the retrospective design and the method of data collection. Sole reliance upon EMR may have compromised the reliability of the results due to potentially inaccurate data recording. Postoperative parameters such as fracture reduction quality, materials and number of implants, biomechanical laboratory indicators, and rehabilitation exercise onset and persistence were not recorded and analyzed, which might have affected the identification of other potential risk factors. Moreover, some SSI cases were recognized on the basis of the signs and symptoms recorded in the EMR rather than on bacterial culture results. Therefore, it is feasible that the incidence of SSI might have been overestimated.
In summary, the present retrospective multicenter study found a relatively low SSI incidence rate (4.37%) following ORIF of ankle fracture, with incidences of 3.05% for superficial and 1.32% for deep SSI. The most common causative agents were polymicrobial, followed by MRSA and others. The significant risk factors or predictors for SSI occurrence were open injury, older age, incision cleanliness grade 2 to 4, high-energy injury, surgeon level of archiater or vice archiater, greater BMI, chronic heart disease, history of allergy, and preoperative NEUT > 75%. Identification of these risk factors could be of great importance in risk–benefit analysis of prophylaxis before surgery, and in implementing appropriate preventive measures. Moreover, the results could be used during counseling of patients and their families during the consent process.
Acknowledgment
We thank Dr Kelly Zammit, BVSc, from Liwen Bianji, Edanz Group China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Footnotes
Abbreviations: ALB = serum albumin concentration, ASA = American Society of Anesthesiologists, BMI = body mass index, EMR = electronic medical records, NEUT = neutrophil count, ORIF = open reduction and internal fixation, RBC = red blood cells, SSI = Information on surgical site infection, TP = total protein, WBC = white blood cell.
Both YS and HW authors contributed equally to this work.
All the authors declare that they have no conflict of interest.
References
- [1].Zhang Y, Su Y, Hao J, Punsoni M. Clinical Epidemiology of Orthopedic Trauma. Thieme; 2012. [Google Scholar]
- [2].Sporer SM, Weinstein JN, Koval KJ. The geographic incidence and treatment variation of common fractures of elderly patients. J Am Acad Orthop Surg 2006;14:246–55. [DOI] [PubMed] [Google Scholar]
- [3].Davidovitch RI, Walsh M, Spitzer A, et al. Functional outcome after operatively treated ankle fractures in the elderly. Foot Ankle Int 2009;30:728–33. [DOI] [PubMed] [Google Scholar]
- [4].Koval KJ, Zhou W, Sparks MJ, et al. Complications after ankle fracture in elderly patients. Foot Ankle Int 2007;28:1249–55. [DOI] [PubMed] [Google Scholar]
- [5].Thangarajah T, Prasad PS, Narayan B. Surgical site infections following open reduction and internal fixation of ankle fractures. Open Orthop J 2009;3:56–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Vioreanu M, Dudeney S, Brophy S, et al. Displaced ankle fractures in the geriatric population: operative or non-operative treatment. Foot Ankle Surg 2007;13:10–4. [Google Scholar]
- [7].Jain S, Haughton BA, Brew C. Intramedullary fixation of distal fibular fractures: a systematic review of clinical and functional outcomes. J Orthop Traumatol 2014;15:245–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Chaudhary SB, Liporace FA, Gandhi A, et al. Complications of ankle fracture in patients with diabetes. J Am Acad Orthop Surg 2008;16:159–70. [DOI] [PubMed] [Google Scholar]
- [9].Korim MT, Payne R, Bhatia MA. case-control study of surgical site infection following operative fixation of fractures of the ankle in a large U.K. trauma unit. Bone Joint J 2014;96-B:636–40. [DOI] [PubMed] [Google Scholar]
- [10].Miller AG, Margules A, Raikin SM. Risk factors for wound complications after ankle fracture surgery. J Bone Joint Surg Am 2012;94:2047–52. [DOI] [PubMed] [Google Scholar]
- [11].Ovaska M. Complications in ankle fracture surgery. Acta Orthop 2015;86:1–32. [DOI] [PubMed] [Google Scholar]
- [12].Ovaska MT, Mäkinen TJ, Madanat R, et al. Risk factors for deep surgical site infection following operative treatment of ankle fractures. J Bone Joint Surg Am 2013;95:348–53. [DOI] [PubMed] [Google Scholar]
- [13].Srinivasan C, Moran CG. Internal fixation of ankle fractures in the very elderly. Injury 2001;32:559–63. [DOI] [PubMed] [Google Scholar]
- [14].Shivarathre DG, Chandran P, Platt SR. Operative fixation of unstable ankle fractures in patients aged over 80 years. Foot Ankle Int 2011;32:599–602. [DOI] [PubMed] [Google Scholar]
- [15].Ovaska MT, Mäkinen TJ, Madanat R, et al. Predictors of poor outcomes following deep infection after internal fixation of ankle fractures. Injury 2013;44:1002–6. [DOI] [PubMed] [Google Scholar]
- [16].Todd B. New CDC guideline for the prevention of surgical site infection. Am J Nurs 2017;117:17. [DOI] [PubMed] [Google Scholar]
- [17].Acello AN, Wallace GF, Pachuda NM. Treatment of open fractures of the foot and ankle: a preliminary report. J Foot Ankle Surg 1995;34:329–46. [DOI] [PubMed] [Google Scholar]
- [18].Tho KS, Chiu PL, Krishnamoorthy S. Grade III open ankle fractures: a review of the outcome of treatment. Singapore Med J 1994;35:57–8. [PubMed] [Google Scholar]
- [19].Kelly EG, Cashman JP, Groarke PJ, et al. Risk factors for surgical site infection following operative ankle fracture fixation. Ir J Med Sci 2013;182:453–6. [DOI] [PubMed] [Google Scholar]
- [20].Nåsell H, Ottosson C, Törnqvist H, et al. The impact of smoking on complications after operatively treated ankle fractures: a follow-up study of 906 patients. J Orthop Trauma 2011;25:748–55. [DOI] [PubMed] [Google Scholar]
- [21].Soohoo NF, Krenek L, Eagan MJ, et al. Complication rates following open reduction and internal fixation of ankle fractures. J Bone Joint Surg 2009;91:1042–9. [DOI] [PubMed] [Google Scholar]
- [22].Zhu Y, Liu S, Zhang X, et al. Incidence and risks for surgical site infection after adult tibial plateau fractures treated by ORIF: a prospective multicentre study. Int Wound J 2017;14:982–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Schepers T, Vries MRD, Lieshout EMMV, et al. The timing of ankle fracture surgery and the effect on infectious complications; A case series and systematic review of the literature. Int Orthop 2013;37:489–94. [DOI] [PMC free article] [PubMed] [Google Scholar]


