Supplemental Digital Content is available in the text
Keywords: coronary artery bypass graft, drug-eluting stent, percutaneous coronary intervention, unprotected left main coronary artery disease
Abstract
Background:
Results on the safety and long-term efficacy of drug-eluting stent placement in unprotected left main coronary artery disease (ULMCAD) compared with those of coronary artery bypass surgery (CABG) remain inconsistent across randomized clinical trials and recent meta-analysis studies. We aimed to compare the clinical outcomes and safety over short- and long-term follow-ups by conducting a meta-analysis of large pooled data from randomized controlled trials and up-to-date observational studies.
Methods:
A systematic review of PubMed, Google Scholar, Medline, and reference lists of related articles was performed for studies conducted in the drug-eluting stent era, to compare percutaneous coronary intervention (PCI) with CABG in ULMCAD. The primary outcome was major adverse cardiovascular and cerebrovascular events (MACCE), myocardial infarction (MI), stroke, all-cause mortality, and revascularization after at least 1-year follow-up. In-hospital and 30-day clinical outcomes were considered secondary outcomes. Furthermore, a subgroup analysis of studies with ≥5 years follow-up was performed to test the sustainability of clinical outcomes.
Results:
A total of 29 studies were extracted with 21,832 patients (10,424 in PCI vs 11,408 in CABG). Pooled analysis demonstrated remarkable differences in long-term follow-up (≥1 year) MACCE (odds ratio [OR] 1.42, 95% CI 1.27–1.59), P < .00001), repeat revascularization (OR 3.00, 95% CI 2.41–3.73, P < .00001), and MI (OR 1.32, 95% CI 1.14–1.53, P = .0002), favoring CABG over PCI. However, stroke risk was significantly lower in the PCI group. Subgroup analysis of studies with ≥5 years follow-up showed similar outcomes except for the noninferiority outcome of MACCE in the PCI arm. However, the PCI group proved good safety profile after a minimum of 30-day follow-up with lower MACCE outcome.
Conclusion:
PCI for ULMCAD can be applied with attentiveness in carefully selected patients. MI and the need for revascularization remain drawbacks and areas of concern among previous studies. Nonetheless, it has been proven safe during short-term follow-up.
1. Introduction
Left main coronary artery disease is found in about 6% of patients undergoing coronary angiography.[1] Unless being protected by collaterals or a patent graft, it has major cardiovascular mortality and morbidity among patients who present with acute cardiovascular events. Traditionally, coronary artery bypass surgery (CABG) is recommended as the sole treatment option, given its safety and efficacy compared with medical therapy, with significant improvement in the patient survival rate.[2] However, nonsurgical candidates presented a challenge in treatment and led to the implementation of percutaneous coronary intervention (PCI) rescue with bare metal stents.[3–5] Unfortunately, the mortality and revascularization rates were inferior to those of CABG, and the American College of Cardiology/American Heart Association guidelines, 2011, remained firm in stating that CABG is recommended for significant left main coronary artery stenosis, class 1 recommendation. However, the PCI approach is considered reasonable, class IIa recommendation, in favorable anatomical lesions or low SYNTAX score. The emergence of drug-eluting stents (DESs) has caused a major shift in interventional cardiology, and the issue of PCI versus CABG has become a topic of debate between interventional cardiologists and cardiac surgeons during the last 20 years. Randomized and nonrandomized trials in the DES era showed conflicting results with different follow-up durations. Small meta-analysis studies[6,7] that mainly recruited randomized trials were conducted in the past; however, the outcomes have been variable. We therefore conducted this large, updated meta-analysis study involving randomized and up-to-date published data to review the clinical outcomes between the 2 treatment modalities.
2. Methods
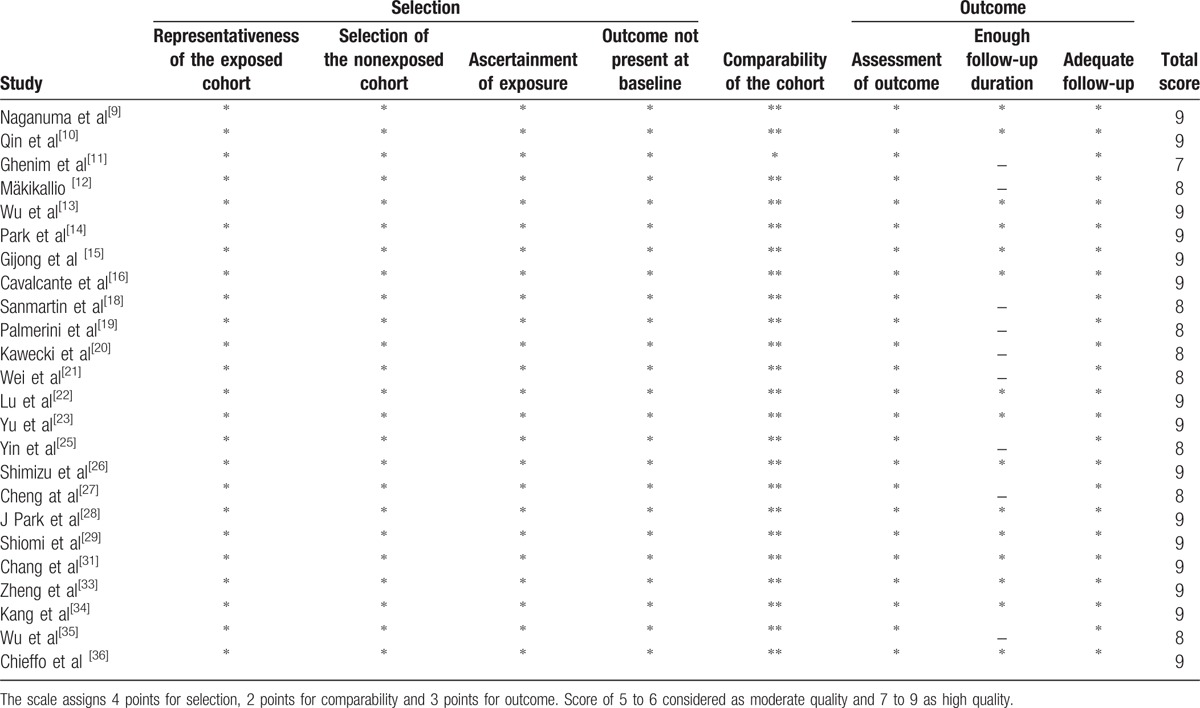
The flow diagram for the meta-analysis is shown in Fig. 1. The study was based on previous published articles; therefore, no ethical approval or patient consent is needed. We used 4 databases for our research to collect appropriate studies (Table 1).[8–36] PubMed, Google Scholar, reference lists of relevant articles, and Medline were the primary tools used in our study. A total of 2 investigators including the author were involved in identifying the required studies up to September 2017. Steps were taken to prevent duplication. The following terms were used in our search: “left main PCI versus CABG,” “drug-eluting stents, ” “bypass surgery, ” and “left main stenting. ” Furthermore, the reference lists of all relevant studies were scrutinized to obtain more qualified studies. The same investigators independently extracted the data and clinical outcomes from the relevant studies to minimize errors or missing data. Studies were included if they compared PCI (strictly DESs) with CABG, had at least 1-year clinical follow-up, and were randomized and nonrandomized trials. Studies were excluded if they compared bare metal stents with CABG, targeted certain patients with chronic diseases, had unclear or difficult-to-extract outcomes, did not compare PCI with CABG, and assessed the outcome in patients who presented with acute coronary syndrome. The risk of bias for all included studies was assessed using the components proposed by the Cochrane Collaboration, which are random sequence generation, allocation concealment, blinding of outcome assessors, incomplete outcome data; and selective outcome reporting.[37] The quality of randomized studies was assessed by the Jadad Score, which ranges from 0 to 5[38]. The randomized trials had score of 2 for lack of double-blind effect (Table 2).[8,17,24,30,32] On the other hand, the quality of observation studies was evaluated based on the Newcastle–Ottawa Scale form.[39] A minimum score of 7 was considered high quality study (Table 3).[9–16,18–23,25–29,31,33–36] We calculated some of the clinical outcomes if reported with percentage numbers. Propensity score analysis data were included if available. The pooled data were analyzed with Review Manager Version 5.3 (RevMan software, available from http://tech.cochrane.org/revman). The primary outcomes were major adverse cardiovascular and cerebrovascular events (MACCE), stroke, all-cause mortality, myocardial infarction (MI), and revascularization after at least 1 year of follow-up. The definition of MACCE was reviewed carefully in each individual study, and it included revascularization in our analysis. Subgroup analysis for the same outcomes after at least 5 years of follow-up was also performed. The secondary outcomes of MACCE, stroke, all-cause mortality, MI, and revascularization during the hospital stay and at the 30-day period were analyzed. We used the Mantel–Haenszel statistical method with random effects. Effect size for individual clinical outcomes was estimated using odds ratios (ORs) and confidence intervals (CIs). The heterogeneity across studies was examined by using the Q test and quantified with the I2 test. A value of >50% and a P value of <.1 were considered significant. We conducted a sensitivity/meta-regression analysis and a leave-one-out study when appropriate to explain significant heterogeneity.
Figure 1.
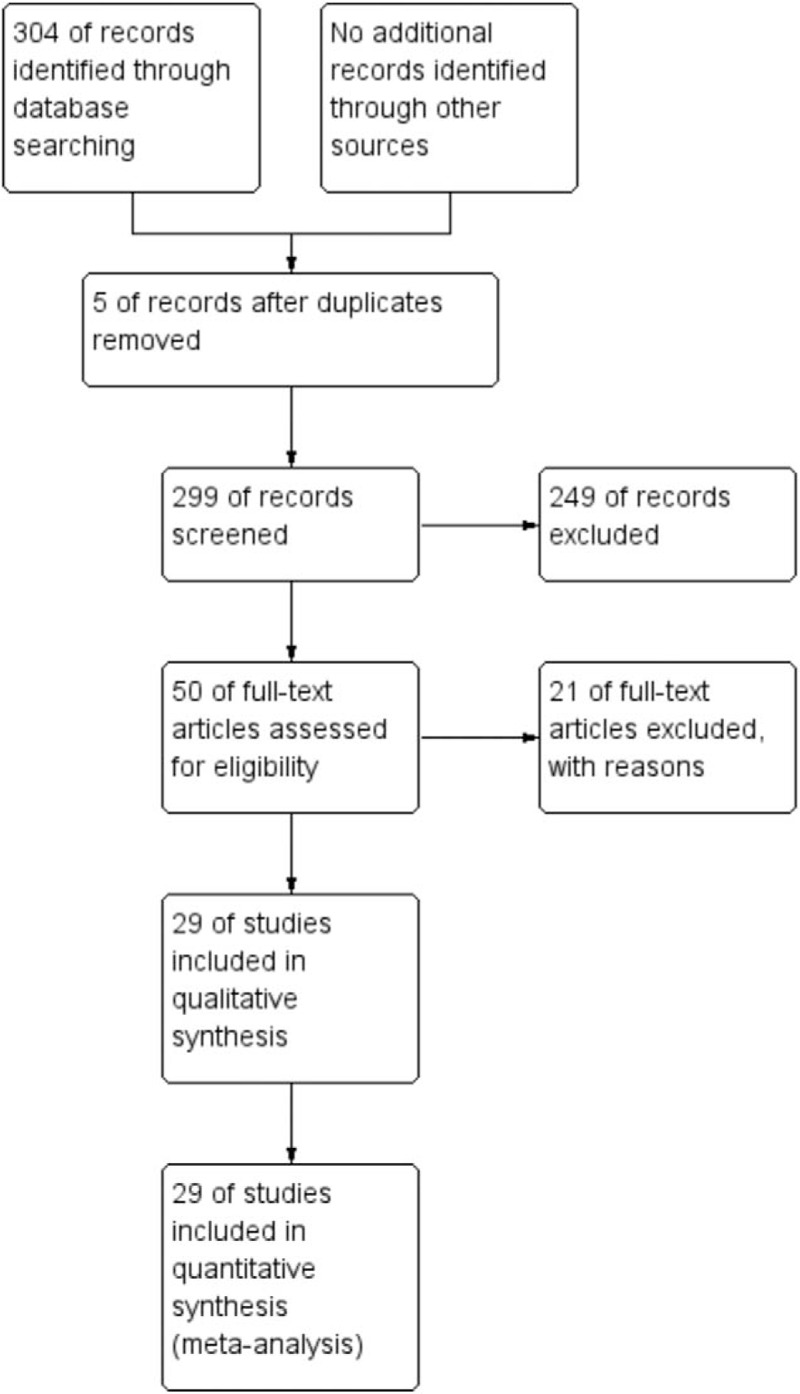
The study flow diagram.
Table 1.
Selected baseline characteristics of randomized trials and observational studies.
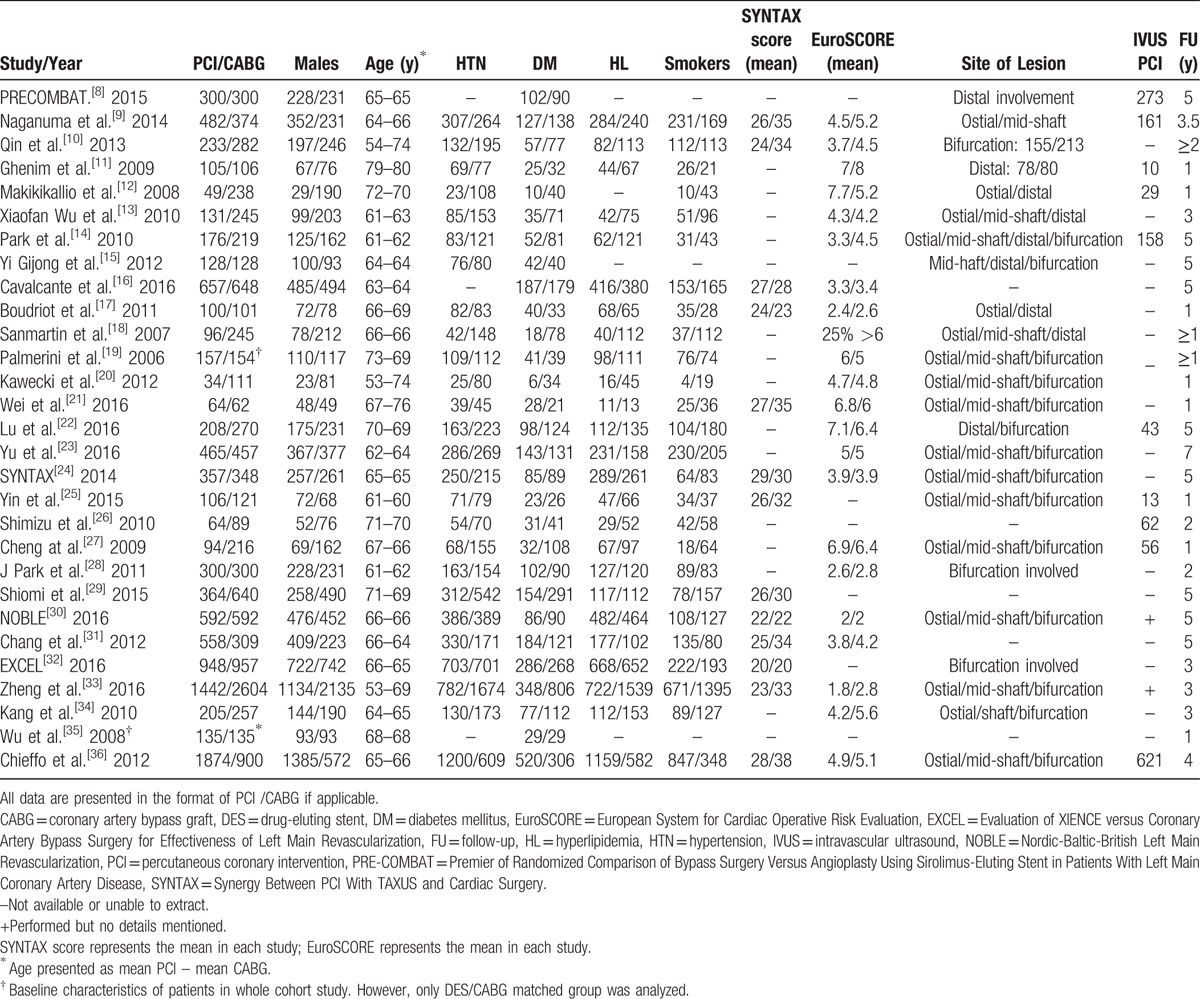
Table 2.
Randomized studies quality assessment using Oxford Quality Scoring System.
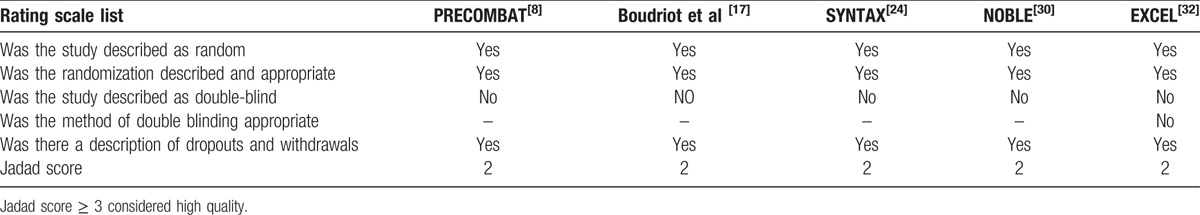
Table 3.
Newcastle–Ottawa scale (NOS) for assessing quality of observational studies.
3. Results
A total of 21,832 patients were included in our study, with 10,424 in the PCI/DES group versus 11,408 in the CABG group. We identified 5 randomized controlled trials and 24 observational studies of PCI/DES versus CABG for ULMCAD with at least 1 year of follow-up. The randomized controlled trials included the EXCEL trial (Everolimus-Eluting Stents or Bypass Surgery for Left Main Coronary Artery Disease), Nordic-Baltic-British Left Main Revascularization (NOBLE) trial (Percutaneous Coronary Angioplasty versus Coronary Artery Bypass Grafting in Treatment of Unprotected Left Main Stenosis), PRE-COMBAT trial—5 years (Bypass Surgery versus Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease), SYNTAX trial (Synergy between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery), and the trial by Boudriot et al (Randomized Comparison of Percutaneous Coronary Intervention With Sirolimus-Eluting Stents Versus Coronary Artery Bypass Grafting in Unprotected Left Main Stem Stenosis). The baseline characteristics and follow-up duration of all included studies are summarized in Table 1. We omitted the CUSTOMIZE trial (Appraise a Customized Strategy for Left Main Revascularization) because 10% of its patients did not receive DESs. The risk of bias of all included studies was summarized in Figs. 2 and 3. Observational studies carried an expected risk of bias. However, they had high quality in their clinical design and data outcome (Table 3).
Figure 2.
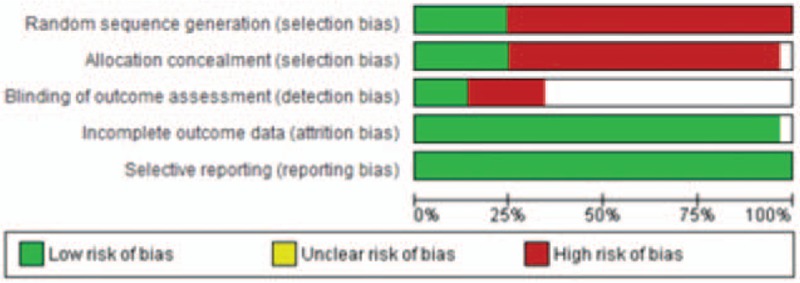
Risk of bias graph: review authors’ judgements about each risk of bias item presented as percentages across all included studies.
Figure 3.
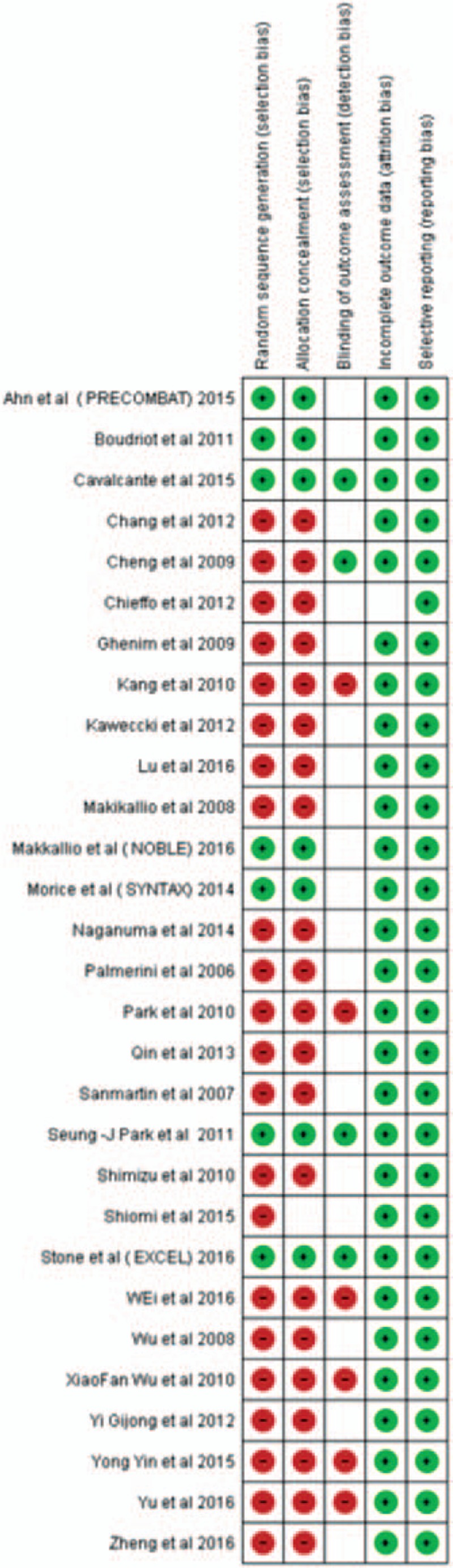
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study.
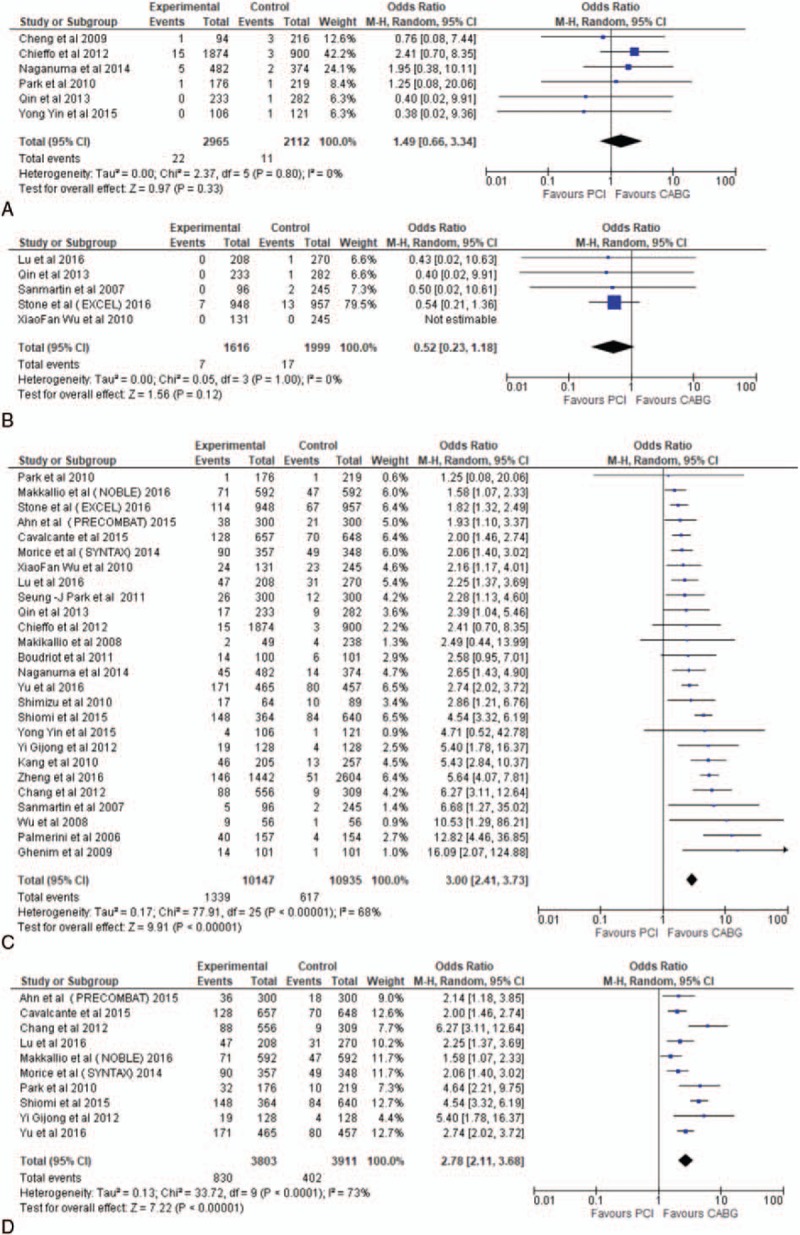
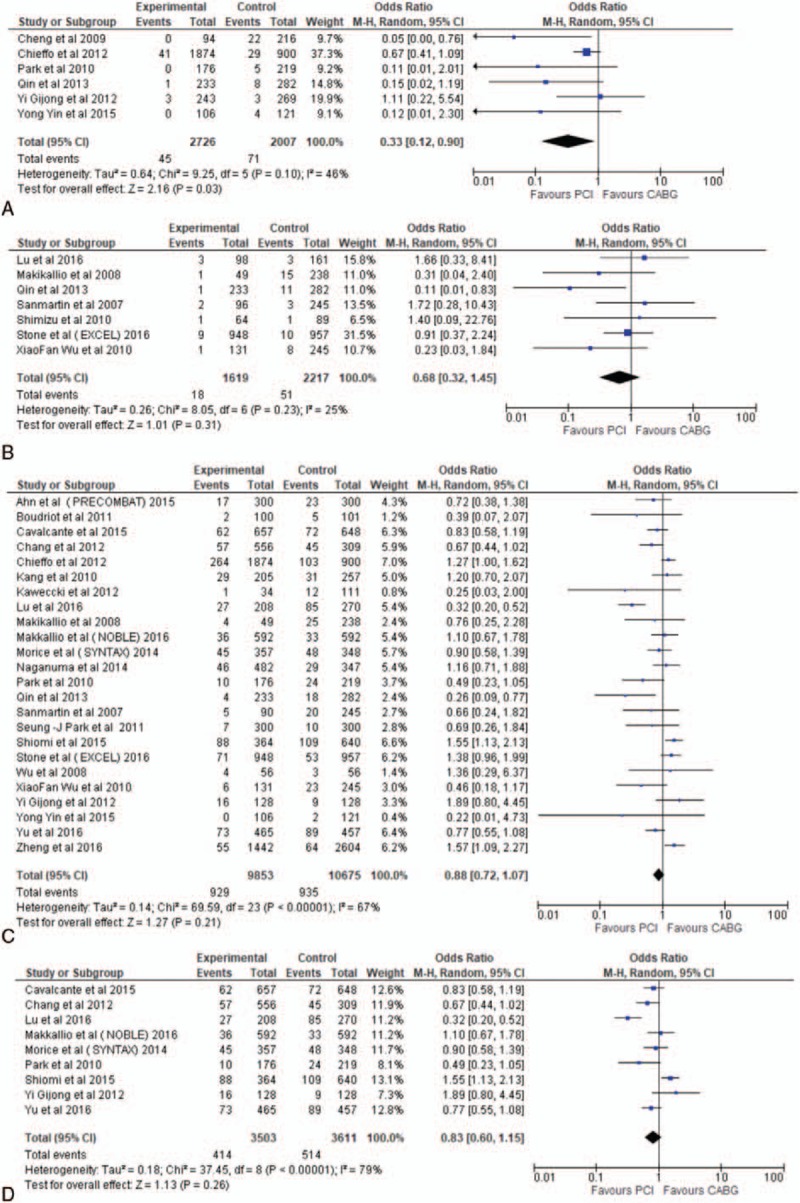
There were no significant differences between the 2 groups in hospital MACCE (OR 0.42, 95% CI 0.14–1.23, P = .11), MI (OR 0.62, 95% CI 0.20–1.96, P = .42), and revascularization (OR 1.49, 95% CI 0.66–3.34, P = .33). However, PCI was found superior to CABG in terms of mortality (OR 0.33, 95% CI 0.12–0.90, P = .03) and stroke (OR 0.28, 95% CI 0.13–0.58, P = .0006) (Figs. 4–8). The 30-day follow-up outcomes revealed a shift favoring PCI for MACCE (OR 0.52, 95% CI 0.38–0.72, P < .0001), and MI (OR 0.65, 95% CI 0.43–0.99, P = .04) whereas the difference remained not significant for revascularization (OR 0.52, 95% CI 0.23–1.18, P = .12), and mortality (OR 0.68, 95% CI 0.32–1.45, P = .31) (Figs. 4–8). A minimum of 1-year follow-up showed favorable outcomes for CABG in terms of MACCE (OR 1.42, 95% CI 1.27–1.59, P < .00001), revascularization (OR 3.00, 95% CI 2.41–3.73, P < .00001), and MI (OR 1.32, 95% CI 1.14–1.53, P = .0002), whereas the risk of stroke favored PCI (OR 0.52, 95% CI 0.37–0.72, P < .0001) over CABG. Nonetheless, long-term mortality remained not significant between the 2 groups (OR 1.24, 95% CI 0.88–1.07, P = .21) (Figs. 4–8).
Figure 4.
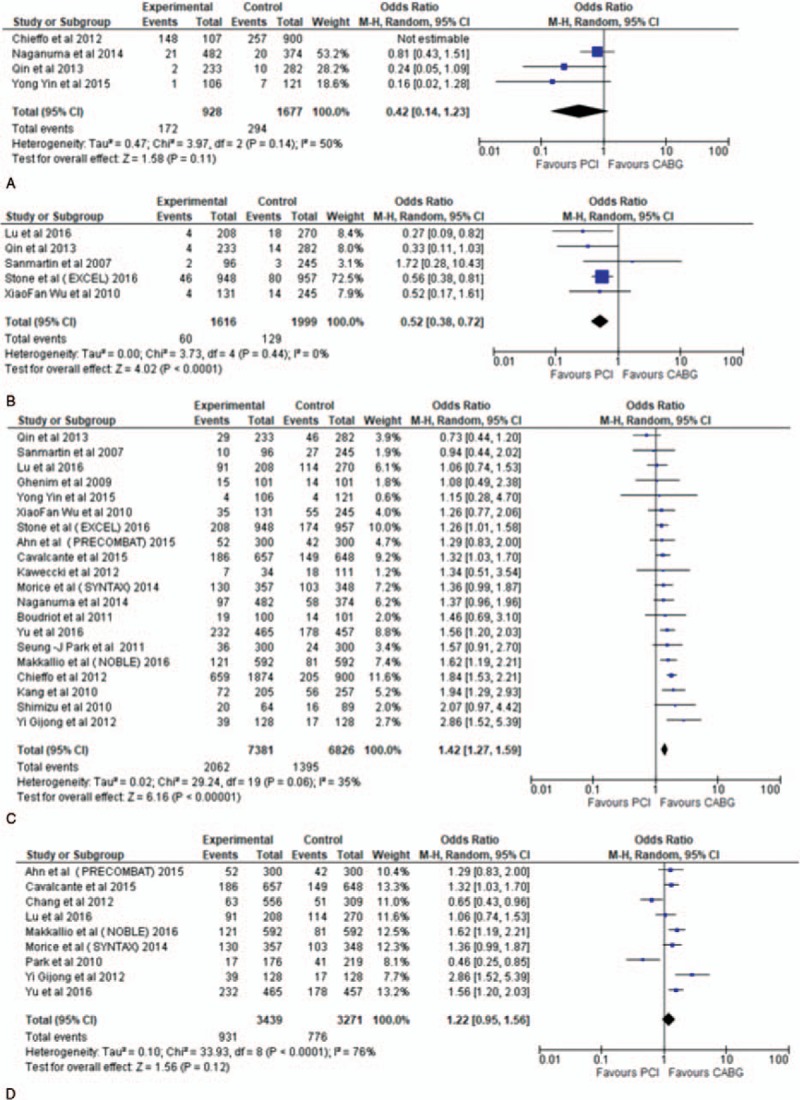
Forest plot of major cardiovascular and cerebrovascular events (MACCE) outcome in percutaneous coronary intervention (PCI) versus coronary artery bypass surgery (CABG) for unprotected left main coronary artery disease (ULMCAD). Forest plot shows the odd ratio (OR) of MACCE in PCI versus CABG during in hospital follow-up (A), 30-day follow-up (B), long-term follow-up ≥ 1 year (C), and subgroup ≥ 5 years follow-up (D).
Figure 8.
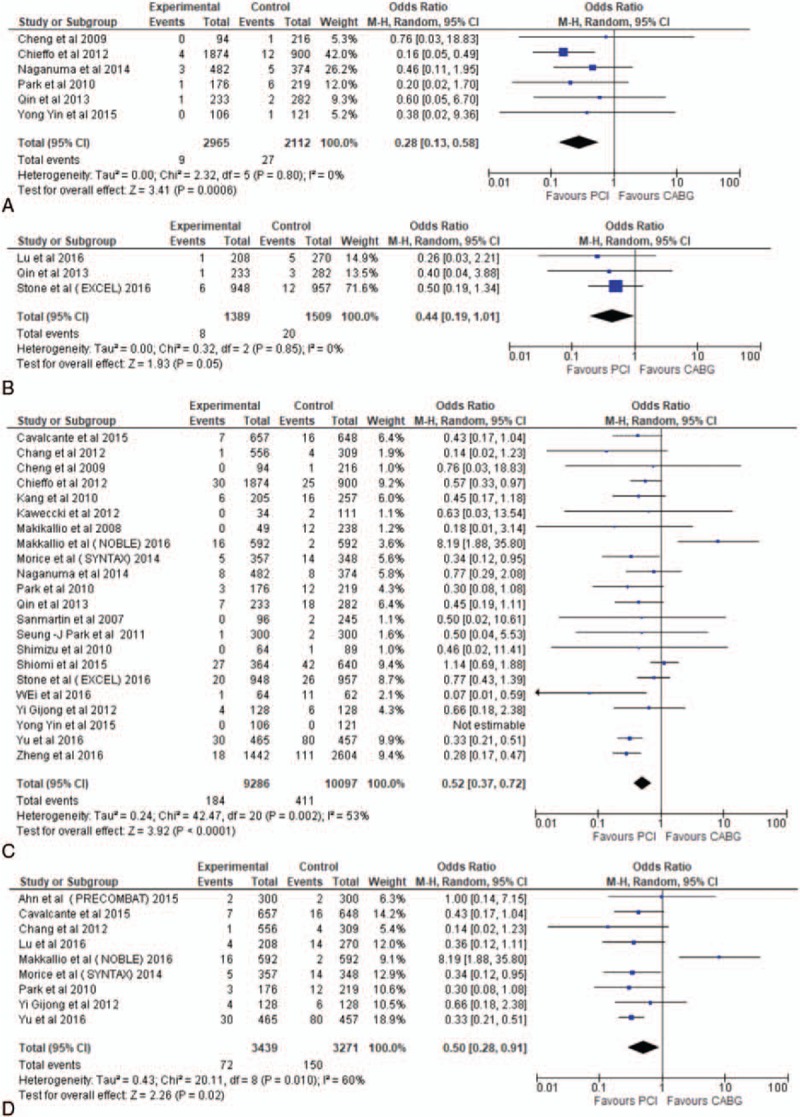
Forest plot of stroke outcome in percutaneous coronary intervention (PCI) versus coronary artery bypass surgery (CABG) for unprotected left main coronary artery disease (ULMCAD). Forest plot shows the odd ratio (OR) of stroke in PCI versus CABG during in hospital follow-up (A), 30-day follow-up (B), long-term follow-up ≥1 year (C), and subgroup ≥ 5 years follow-up (D).
Pooled analysis of studies conducted for at least 5 years was then performed as a subgroup analysis to test the consistency of the primary outcome results beyond 1 year of follow-up and to increase the power of the study design. We found that CABG remained favorable over PCI in terms of revascularization (OR 2.86, 95% CI 2.19–3.74, P < .00001) and MI (OR 1.42, 95% CI 1.0–2.01, P = .05). There was no difference in mortality (OR 0.83, 95% CI 0.60–1.15, P = .26) and MACCE (OR 1.22, 95% CI 0.95–1.56, P = .12). The risk of stroke remained low in the PCI group (OR 0.55, 95% CI 0.31–0.96, P = .03) (Figs. 4–8).
A significant heterogeneity was noted in long-term (≥ 1 year) revascularization and stroke. For stroke, leave-one-out sensitivity analysis showed that the NOBLE trial played a major role in the high heterogeneity effect. On the other hand, no similar influence was found in the revascularization outcome; hence, meta-regression analysis was performed.
In the meta-regression analysis, a total of 5 baseline characteristics—number of male subjects, diabetes mellitus, hypertension, left ventricular ejection fraction, and SYNTAX score—were included in the analysis. The mean of SYNTAX score and left ventricular ejection fraction was calculated for each individual study in the long-term follow-up (≥ 1 year) group and the 5-year group (Supplemental Figures). SYNTAX score was the only covariant with a size effect between both groups. The long-term follow-up (≥ 1 year) group showed a regression coefficient of 0.067 (P = .005), and the 5-year follow-up group had a regression coefficient of 0.109 (P = .010). In other words, the lower the SYNTAX score, the lower relative risk of revascularization.
4. Discussion
The advancements in medical technology have shifted the practice of cardiology to less invasive surgical interventions. The safety of PCI for ULMCAD has remained an issue of debate between cardiac surgeons and interventional cardiologists. To date, many observational studies and a few randomized trials have been conducted, with conflicting results. We conducted this meta-analysis of 29 studies including randomized trials, with the aim of addressing the safety and feasibility of PCI/DES in ULMCAD. Our review of 29 studies and 21,832 patients is, to our knowledge, the largest meta-analysis to address short-term (in-hospital and 30-day) and long-term follow-ups. Our findings clearly showed that PCI is safe and feasible during in-hospital and short-term follow-ups; however, it loses its potentiality after a minimum of 1 year of follow-up with more need for revascularization and increased numbers of MI events (Figure 5C, 7C). We noted a dramatic shift in clinical outcomes during the long-term follow-ups compared with the early phase, in-hospital, and 30-day follow-up periods. In the early phase, patients who underwent PCI tended to experience less stroke and MACCE (Figure 4B, 8B). These findings were supported by the EXCEL randomized trial (Table 1), in which patients with CABG had high MACCE during the 30-day follow-up (HR 0.57, 95% CI 0.4–0.82, P = .002). Contrary to the EXCEL trial, our meta-analysis revealed that stroke and MI led to a high MACCE clinical outcome (Fig. 8), whereas MI (HR 0.63, 95% CI 0.42–0.95, P = .02) played a major role in the EXCEL trial. Of note, our early phase results were heavily based on the EXCEL trial which accounted for 70% to 90% of the analysis. Unfortunately, this short-term noninferiority of PCI to CABG started to lose its potentiality after 1 year of follow-up with more need for revascularization (Fig. 5). Boudriot et al (Table 1) conducted a 1-year randomized trial in which repeat revascularization in the PCI group was inferior to CABG. However, it might be fair to point out that routine angiographic follow-up was 15% more frequently conducted in patients who underwent PCI, and this might have led to the more revascularization observed in the study. Additionally, about two-thirds of the reported lesions were in the distal segment of the ULMCAD. Anatomically, the left main coronary artery is divided into 3 segments: ostial, mid-shaft, and distal bifurcation with a smaller diameter than the proximal segment. Thus, the proximal segment allows interventional cardiologists to use larger-diameter stents with a low rate of restenosis. Furthermore, the treatment of the distal left main bifurcation diseases implies the need for more complex and technically demanding bifurcation techniques. In particular, the need for 2- stent approach has shown a higher incidence of procedure- related complications and unfavorable outcomes.[40] A meta-analysis of 16 trials involving PCI for ULMCAD identified distal lesions as the most significant predictor of repeated revascularization and overall MACCE outcomes.[41] Moreover, previous studies have reported better outcomes for proximal segment stenting in ULMCAD.[42,43] It is noteworthy to mention that about 80% of the analyzed studies (PCI group) included distal bifurcation lesions, which, in other words, may explain this unfavorable outcome in the PCI group.
Figure 5.
Forest plot of revascularization outcome in percutaneous coronary intervention (PCI) versus coronary artery bypass surgery (CABG) for unprotected left main coronary artery disease (ULMCAD). Forest plot shows the odd ratio (OR) of revascularization in PCI versus CABG during in hospital follow-up (A), 30-day follow-up (B), long-term follow-up ≥ 1 year (C), and subgroup ≥ 5 years follow-up (D).
Figure 7.
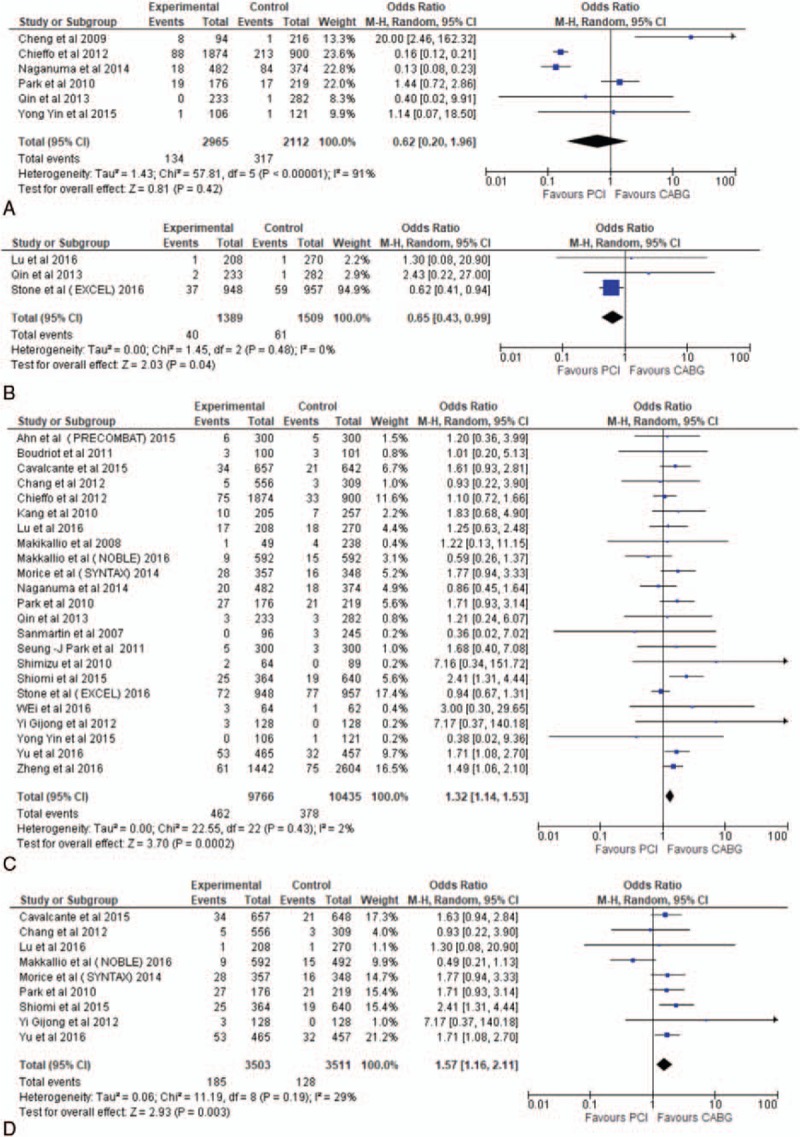
Forest plot of MI outcome in percutaneous coronary intervention (PCI) versus coronary artery bypass surgery (CABG) for unprotected left main coronary artery disease (ULMCAD). Forest plot shows the odd ratio (OR) of myocardial infarction (MI) in PCI versus CABG during in hospital follow-up (A), 30-day follow-up (B), long-term follow-up ≥ 1 year (C), and subgroup ≥ 5 years follow-up (D).
Moreover, we noted an increased incidence of MI after long-term follow-up in the PCI group compared with the CABG group (OR 1.32, 95% CI 1.14–1.53, P = .0002) (Fig. 7C) which, in turn, may represent the high revascularization demand possibly related to true angina symptoms. The MI outcome was also sustained after subgroup analysis of studies with ≥5 years of follow-up. Our finding is similar to that of the NOBLE trial (Table 1) (HR 2.88, 95% CI 1.40–5.90, P = .004). This advantage of CABG might be achieved by detouring blood supply over the long lesion segment, which, to some extent, protects against target-lesion and de novo lesion MIs. However, no significant difference in MI was found in the EXCEL (HR 0.93, 95% CI 0.67–1.28, P = .64) and SYNTAX (HR 1.67, 95% CI 0.91–3.10, P = .10) trials, with a noninferiority outcome between the 2 groups (Table 1). This discrepancy between trials is difficult to explain; however, the definition of MI is not universal owing its own limitations when applied to clinical outcome.
Numerous previous studies found no statistical difference in the long-term mortality between the 2 groups. This observation is supported by the EXCEL (HR 1.34, 95% CI 0.94–1.91, P = .11), SYNTAX (HR 0.88, 95% CI 0.58–1.32, P = .53), and NOBLE (HR 1.04, 95% CI 0.65–1.67, P = .86) trials (Table 1). Our study agrees with previous trials, although the mortality rate was high among the CABG population during in-hospital stay (Fig. 6A and C). A number of preoperative and intraoperative factors have been demonstrated to influence the operative mortality in CABG per se, including comorbid conditions. In the United States, the mortality rate after CABG between 1997 and 2001 averaged about 2% to 5% in general.[44,45] However, after a minimum of 30 days of follow-up, both groups tended to have the same mortality rate even after 5 years of follow-up (Fig. 6D). In a real-world comparison, Yi et al (Table 1) conducted a prospective study with a matching patient cohort, comparing off-pump bypass procedures versus DES in ULMCAD. Again, the authors found no difference in mortality between the 2 groups during 5 years of follow-up. On the contrary, Qin et al (Table 1) reported a different result with a higher mortality rate among the CABG group, resulting from the high cardiac death after long-term follow-up (1.7% PCI vs 6.4% CABG, P = .01). Nevertheless, we noted that the left internal mammary artery was used below the usual percentile, which might be a factor in the different clinical outcomes.
Figure 6.
Forest Plot of mortality outcome in percutaneous coronary intervention (PCI) versus coronary artery bypass surgery (CABG) for unprotected left main coronary artery disease (ULMCAD). Forest plot shows the odd ratio (OR) of mortality in PCI versus CABG during in hospital follow-up (A), 30-day follow-up (B), long-term follow-up ≥1 year (C), and subgroup ≥ 5 years follow-up (D).
The risk of stroke, as one of the most devastating complications, remained high in the CABG group even after long-term follow-up. However, including the NOBLE trial, the heterogeneity effect increased among the compared studies, secondary with the increase in stroke in the PCI group. Although no clear reasons were found, it was noted that most strokes occurred mainly after 1 year, coinciding with the discontinuation of dual antiplatelet therapy. Similar to our finding, a meta-analysis study by Athappan et al[46] found that PCI is superior to CABG in terms of stroke outcome even after 5 years of follow-up (OR 0.27, 95% CI 0.13–0.55, P = .00). Moreover, many nonrandomized trials showed noninferiority or even superiority of PCI over CABG when the risk of stroke was considered. Two variables are believed to play a major role in the stroke incidence after bypass surgery: cerebral embolism due to the manipulation of aortic atherosclerotic plaques during surgery[47,48] and cerebral hypoperfusion during surgery.[49,50] Therefore, the prevalence of atherosclerotic disease among patients with ULMCAD highlights the importance of identifying vulnerable patients and is crucial in weighing the benefits of performing PCI during decision making.
The definition of MACCE was somehow variable among the different studies. We analyzed data from studies that defined MACCE strictly as a composite of MI, stroke, all-cause mortality, and revascularization. In our study, MACCE yielded different results after each period of follow-up. It seems that PCI is not inferior to CABG during in-hospital stay, and even achieved superiority after a minimum of 30-day follow-up (OR 0.52, 95% CI 0.38–0.72, P < .0001). Nevertheless, this potential benefit shifted to CABG after long-term follow-up (OR 1.42, 95% CI 1.27–1.59, P < .00001) (Fig. 4). In a retrospective study conducted by Shimizu et al (Table 1), the MACCE-free survival rate was better (P = .033) in the CABG group (CABG 82.2% vs DES 62.6%) at 2 years. However, analysis of data extracted from studies of ≥5 years follow-up yielded different outcomes, and no statistical difference was found between the 2 groups (OR 1.22, 95% CI 0.95–1.56, P = .12) (Fig. 4D). The latter finding is in agreement with the SYNTAX trial (HR 1.23, 95% CI 0.95–1.59, P = .12). Contrary to our finding, MACCE remained favorable in the PCI group in a 5-year meta-analysis study conducted by Athappan et al[46] (OR 0.64, 95% CI 051–0.8, P = .00). However, more articles were included in our analysis, which increased the study power effect. Overall, and given the inconsistent results among different studies, we can conclude that PCI remained at least noninferior to CABG in terms of MACCE after long-term monitoring. The strict definition of MACCE in our study improved the reliability and enhanced the interpretation of the MACCE outcome.
Our study has some limitations. First, the inclusion and exclusion criteria used may have created unintentional bias. Second, the observational studies carried inevitable high risk selection bias. Third, searches of the current databases still may not include all published studies with more negative results. Fourth, the in-hospital and 30-day follow-up outcomes were not reported by many studies, thus minimizing the analytical power of results. Fifth, although the significant heterogeneity noted in revascularization outcome was further explored, other underlying clinical variables may have been overlooked. Sixth, the definition of MI tended to vary among studies and thereby has its own limitations in clinical interpretation. Seventh, data of intravascular ultrasound practice were absent among a large proportion of the studies, making data analysis inaccurate, as they were not included in our meta-regression analysis.
In conclusion, compared with CABG, PCI/DES in ULMCAD was associated with increases in revascularization and MI during long-term follow-up; however, it showed a good safety profile during the short-term follow-up. It is reasonable to use the SYNTAX score to help guide decision making.
Supplementary Material
Footnotes
Abbreviations: CABG = coronary artery bypass graft, DES = drug-eluting stent, DM = diabetes mellitus, EuroSCORE = European System for Cardiac Operative Risk Evaluation, EXCEL = Evaluation of XIENCE versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization, FU = follow-up, HL = hyperlipidemia, HTN = hypertension, IVUS = intravascular ultrasound, MACCE = major adverse cardiovascular and cerebrovascular events, MI = myocardial infarction, NOBLE = Nordic-Baltic-British Left Main Revascularization, PCI = percutaneous coronary intervention, PRE-COMBAT = Premier of Randomized Comparison of Bypass Surgery Versus Angioplasty Using Sirolimus-Eluting Stent in Patients With Left Main Coronary Artery Disease, SYNTAX = Synergy Between PCI With TAXUS and Cardiac Surgery, ULMCAD = unprotected left main coronary artery disease.
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Ragosta M, Dee S, Sarembock IJ, et al. Prevalence of unfavorable angiographic characteristics for percutaneous intervention in patients with unprotected left main coronary artery disease. Catheter Cardiovasc Interv 2006;68:357–62. [DOI] [PubMed] [Google Scholar]
- [2].Chaitman BR, Fisher LD, Bourassa MG, et al. Effect of coronary bypass surgery on survival patterns in subsets of patients with left main coronary artery disease. Report of the Collaborative Study in Coronary Artery Surgery (CASS). Am J Cardiol 1981;48:765–77. [DOI] [PubMed] [Google Scholar]
- [3].Tan WA, Tamai H, Park SJ, et al. Long-term clinical outcomes after unprotected left main trunk percutaneous revascularization in 279 patients. Circulation 2001;104:1609–14. [DOI] [PubMed] [Google Scholar]
- [4].Park SJ, Park SW, Hong MK, et al. Long-term (three-year) outcomes after stenting of unprotected left main coronary artery stenosis in patients with normal left ventricular function. Am J Cardiol 2003;91:12–6. [DOI] [PubMed] [Google Scholar]
- [5].Park SJ, Hong MK, Lee CW, et al. Elective stenting of unprotected left main coronary artery stenosis: effect of debulking before stenting and intravascular ultrasound guidance. J Am Coll Cardiol 2001;38:1054–60. [DOI] [PubMed] [Google Scholar]
- [6].Qian C, Feng H, Cao J, et al. Meta-analysis of randomized control trials comparing drug-eluting stents versus coronary artery bypass grafting for significant left main coronary narrowing. Am J Cardiol 2017;119:1338–43. [DOI] [PubMed] [Google Scholar]
- [7].Sá MP, Ferraz PE, Escobar RR, et al. Five-year outcomes following PCI with DES versus CABG for unprotected LM coronary lesions: meta-analysis and meta-regression of 2914 patients. Rev Bras Circ Cardiovasc 2013;28:83–92. [DOI] [PubMed] [Google Scholar]
- [8].Ahn JM, Roh JH, Kim YH, et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease: 5-year outcomes of the PRECOMBAT study. J Am Coll Cardiol 2015;65:2198–206. [DOI] [PubMed] [Google Scholar]
- [9].Naganuma T, Chieffo A, Meliga E, et al. Long-term clinical outcomes after percutaneous coronary intervention versus coronary artery bypass grafting for ostial/midshaft lesions in unprotected left main coronary artery from the DELTA registry: a multicenter registry evaluating percutaneous coronary intervention versus coronary artery bypass grafting for left main treatment. JACC Cardiovasc Interv 2014;7:354–61. [DOI] [PubMed] [Google Scholar]
- [10].Qin Q, Qian J, Wu X, et al. A comparison between coronary artery bypass grafting surgery and percutaneous coronary intervention for the treatment of unprotected left main coronary artery disease. Clin Cardiol 2013;36:54–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ghenim R, Roncalli J, Tidjane AM, et al. One-year follow-up of nonrandomized comparison between coronary artery bypass grafting surgery and drug-eluting stent for the treatment of unprotected left main coronary artery disease in elderly patients (aged > or = 75 years). J Interv Cardiol 2009;22:520–6. [DOI] [PubMed] [Google Scholar]
- [12].Mäkikallio TH, Niemelä M, Kervinen K, et al. Coronary angioplasty in drug eluting stent era for the treatment of unprotected left main stenosis compared to coronary artery bypass grafting. Ann Med 2008;40:437–43. [DOI] [PubMed] [Google Scholar]
- [13].Wu X, Chen Y, Kubo T, et al. Long-term (4-year) outcomes and predictors of adverse cardiac events after sirolimus-eluting stent implantation in unprotected left main coronary artery. Int Heart J 2010;51:377–82. [DOI] [PubMed] [Google Scholar]
- [14].Park DW, Kim YH, Yun SC, et al. Long-term outcomes after stenting versus coronary artery bypass grafting for unprotected left main coronary artery disease: 10-year results of bare-metal stents and 5-year results of drug-eluting stents from the ASAN-MAIN (ASAN Medical Center-Left MAIN Revascularization) Registry. J Am Coll Cardiol 2010;56:1366–75. [DOI] [PubMed] [Google Scholar]
- [15].Yi G, Youn YN, Hong S, et al. Midterm outcome of off-pump bypass procedures versus drug-eluting stent for unprotected left main coronary artery disease. Ann Thorac Surg 2012;94:15–22. [DOI] [PubMed] [Google Scholar]
- [16].Cavalcante R, Sotomi Y, Lee CW, et al. Outcomes after percutaneous coronary intervention or bypass surgery in patients with unprotected left main disease. J Am Coll Cardiol 2016;68:999–1009. [DOI] [PubMed] [Google Scholar]
- [17].Boudriot E, Thiele H, Walther T, et al. Randomized comparison of percutaneous coronary intervention with sirolimus-eluting stents versus coronary artery bypass grafting in unprotected left main stem stenosis. J Am Coll Cardiol 2011;57:538–45. [DOI] [PubMed] [Google Scholar]
- [18].Sanmartin M, Baz JA, Claro R, et al. Comparison of drug-eluting stents versus surgery for unprotected left main coronary artery disease. Am J Cardiol 2007;100:970–3. [DOI] [PubMed] [Google Scholar]
- [19].Palmerini T, Marzocchi A, Marrozzini C. Comparison between coronary angioplasty and coronary artery bypass surgery for the treatment of unprotected left main coronary artery stenosis (the Bologna Registry). Am J Cardiol 2006;98:54–9. [DOI] [PubMed] [Google Scholar]
- [20].Kawecki D, Morawiec B, Fudal M, et al. Comparison of coronary artery bypass grafting with percutaneous coronary intervention for unprotected left main coronary artery disease. Yonsei Med J 2012;53:58–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Wei Z, Xie J, Wang K, et al. Comparison of percutaneous coronary intervention versus coronary artery bypass graft in aged patients with unprotected left main artery lesions. Int Heart J 2016;57:682–8. [DOI] [PubMed] [Google Scholar]
- [22].Lu TM, Lee WL, Hsu PF, et al. Long-term results of stenting versus coronary artery bypass surgery for left main coronary artery disease—a single-center experience. J Chin Med Assoc 2016;79:356–62. [DOI] [PubMed] [Google Scholar]
- [23].Yu XP, Wu CY, Ren XJ, et al. Very long-term outcomes and predictors of percutaneous coronary intervention with drug-eluting stents versus coronary artery bypass grafting for patients with unprotected left main coronary artery disease. Chin Med J (Engl) 2016;129:763–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Morice MC, Serruys PW, Kappetein AP, et al. Five-year outcomes in patients with left main disease treated with either percutaneous coronary intervention or coronary artery bypass grafting in the synergy between percutaneous coronary intervention with taxus and cardiac surgery trial. Circulation 2014;129:2388–94. [DOI] [PubMed] [Google Scholar]
- [25].Yin Y, Xin X, Geng T, et al. Clinical comparison of percutaneous coronary intervention with domestic drug-eluting stents versus off pump coronary artery bypass grafting in unprotected left main coronary artery disease. Int J Clin Exp Med 2015;8:14376–82. [PMC free article] [PubMed] [Google Scholar]
- [26].Shimizu T, Ohno T, Ando J, et al. Mid-term results and costs of coronary artery bypass vs drug-eluting stents for unprotected left main coronary artery disease. Circ J 2010;74:449–55. [DOI] [PubMed] [Google Scholar]
- [27].Cheng CI, Lee FY, Chang JP, et al. Long-term outcomes of intervention for unprotected left main coronary artery stenosis: coronary stenting vs coronary artery bypass grafting. Circ J 2009;73:705–12. [DOI] [PubMed] [Google Scholar]
- [28].Park SJ, Kim YH, Park DW, et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease. N Engl J Med 2011;364:1718–27. [DOI] [PubMed] [Google Scholar]
- [29].Shiomi H, Morimoto T, Furukawa Y, et al. Comparison of percutaneous coronary intervention with coronary artery bypass grafting in unprotected left main coronary artery disease—5-year outcome from CREDO-Kyoto PCI/CABG Registry Cohort-2. Circ J 2015;79:1282–9. [DOI] [PubMed] [Google Scholar]
- [30].Makikallio T, Holm NR, Lindsay M, et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. Lancet 2016;388:2743–52. [DOI] [PubMed] [Google Scholar]
- [31].Chang K, Koh YS, Jeong SH, et al. Long-term outcomes of percutaneous coronary intervention versus coronary artery bypass grafting for unprotected left main coronary bifurcation disease in the drug-eluting stent era. Heart 2012;98:799–805. [DOI] [PubMed] [Google Scholar]
- [32].Stone GW, Sabik JF, Serruys PW, et al. Everolimus-eluting stents or bypass surgery for left main coronary artery disease. N Engl J Med 2016;375:2223–35. [DOI] [PubMed] [Google Scholar]
- [33].Zheng Z, Xu B, Zhang H, et al. Coronary artery bypass graft surgery and percutaneous coronary interventions in patients with unprotected left main coronary artery disease. JACC Cardiovasc Interv 2016;9:1102–11. [DOI] [PubMed] [Google Scholar]
- [34].Kang SH, Park KH, Choi DJ, et al. Coronary artery bypass grafting versus drug-eluting stent implantation for left main coronary artery disease (from a two-center registry). Am J Cardiol 2010;105:343–51. [DOI] [PubMed] [Google Scholar]
- [35].Wu C, Hannan EL, Walford G, et al. Utilization and outcomes of unprotected left main coronary artery stenting and coronary artery bypass graft surgery. Ann Thorac Surg 2008;86:1153–9. [DOI] [PubMed] [Google Scholar]
- [36].Chieffo A, Meliga E, Latib A, et al. Drug-eluting stent for left main coronary artery disease. The DELTA registry: a multicenter registry evaluating percutaneous coronary intervention versus coronary artery bypass grafting for left main treatment. JACC Cardiovasc Interv 2012;5:718–27. [DOI] [PubMed] [Google Scholar]
- [37].Turner L, Boutron I, Hróbjartsson A, et al. The evolution of assessing bias in Cochrane systematic reviews of interventions: celebrating methodological contributions of the Cochrane Collaboration. Syst Rev 2013;2:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1–2. [DOI] [PubMed] [Google Scholar]
- [39].Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5. [DOI] [PubMed] [Google Scholar]
- [40].Ahn JM, Lee PH, Park SJ. Practical based approach to left main bifurcation stenting. BMC Cardiovasc Disord 2016;16:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Biondi-Zoccai GG, Lotrionte M, Moretti C, et al. A collaborative systematic review and meta-analysis on 1278 patients undergoing percutaneous drug-eluting stenting for unprotected left main coronary artery disease. Am Heart J 2008;155:274–83. [DOI] [PubMed] [Google Scholar]
- [42].Chieffo A, Park SJ, Valgimigli M, et al. Favorable long-term outcome after drug-eluting stent implantation in nonbifurcation lesions that involve unprotected left main coronary artery: a multicenter registry. Circulation 2007;116:158–62. [DOI] [PubMed] [Google Scholar]
- [43].Chieffo A, Park SJ, Valgimigli M, et al. Ostial and midshaft lesions vs. bifurcation lesions in 1111 patients with unprotected left main coronary artery stenosis treated with drug-eluting stents: results of the survey from the Italian Society of Invasive Cardiology. Eur Heart J 2009;30:2087–94. [DOI] [PubMed] [Google Scholar]
- [44].Reames BN, Ghaferi AA, Birkmeyer JD, et al. Hospital volume and operative mortality in the modern era. Ann Surg 2014;260:244–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Peterson ED, Coombs LP, DeLong ER, et al. Procedural volume as a marker of quality for CABG surgery. JAMA 2004;291:195–201. [DOI] [PubMed] [Google Scholar]
- [46].Athappan G, Patvardhan E, Tuzcu ME, et al. Left main coronary artery stenosis: a meta-analysis of drug-eluting stents versus coronary artery bypass grafting. JACC Cardiovasc Interv 2013;6:1219–30. [DOI] [PubMed] [Google Scholar]
- [47].Palmerini T, Biondi-Zoccai G, Reggiani LB, et al. Risk of stroke with coronary artery bypass graft surgery compared with percutaneous coronary intervention. J Am Coll Cardiol 2012;60:798–805. [DOI] [PubMed] [Google Scholar]
- [48].Roach GW, Kanchuger M, Mangano CM, et al. Adverse cerebral outcomes after coronary bypass surgery. Multicenter Study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators. N Engl J Med 1996;335:1857–63. [DOI] [PubMed] [Google Scholar]
- [49].Dávila-Román VG, Murphy SF, Nickerson NJ, et al. Atherosclerosis of the ascending aorta is an independent predictor of long-term neurologic events and mortality. J Am Coll Cardiol 1999;33:1308–16. [DOI] [PubMed] [Google Scholar]
- [50].Bergman P, van der Linden J. Atherosclerosis of the ascending aorta as a major determinant of the outcome of cardiac surgery. Nat Clin Pract Cardiovasc Med 2005;2:246–51. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


