Abstract
The prevalence of end-stage renal disease is rising in the United States, which bears high financial and public health burden. The most common modality of renal replacement therapy (RRT) in the United States is in-center hemodialysis. Many patients report lack of comprehensive and timely education on their treatment options, which may preclude them from participating in home-based dialysis therapies and kidney transplantation evaluation. While RRT education has traditionally been provided in-person, the rise of telehealth has afforded new opportunities to improve upon the status quo. For example, technology-augmented RRT education has recently been implemented into telehealth nephrology clinics, informational websites and mobile applications maintained by professional organizations, patient-driven forums on social media, and multimodality programs. The benefits of technology in RRT education are increased access for geographically isolated and/or medically frail patients, versatility of content delivery, information repetition to enhance knowledge retention, and interpersonal connection for educational content and emotional support. Challenges center around privacy and accuracy of information sharing, in addition to differential access to technology based on age and socioeconomic status. Based on review of available scholarly and social media resources, technology-aided delivery of education on treatment options for end-stage renal disease provide an important alternative and/or supplemental resource for patients and families.
Keywords: telehealth, dialysis education, renal replacement therapy, technology
Introduction
Treatment of end-stage renal disease (ESRD) encompasses renal replacement therapies (RRT) and conservative management. RRT include in-center and home dialysis as well as living and deceased donor kidney transplantation. Patient autonomy is encouraged in the United States (U.S.) to choose a treatment modality to best fit individual lifestyle goals, as long as there are no medical or psychosocial contraindications or geographic inaccessibility. Pre-ESRD education aims at providing patients with the information needed to make a treatment decision. Current statistics related to education and RRT selection suggest that the nephrology community is falling short of this goal. This review will discuss existing educational strategies for RRT education/preparation as well as the opportunities to improve this area of nephrology education afforded by technology.
RRT prevalence and modalities in USA and international comparisons
There were approximately 680,000 prevalent cases of treated ESRD in the U.S. at the end of 2014, with a projected rise of 21,000 annually.1 Up to 38% of incident ESRD cases in 2014 were reported to have had little or no nephrology care prior to the initiation of treatment, thus precluding any pre-ESRD education.1 The groups with low rates of pre-ESRD nephrology care are African Americans, Native Americans, those with either unknown etiology of ESRD or ESRD due to hypertension, as well as those in the 22 – 44 year age group.1
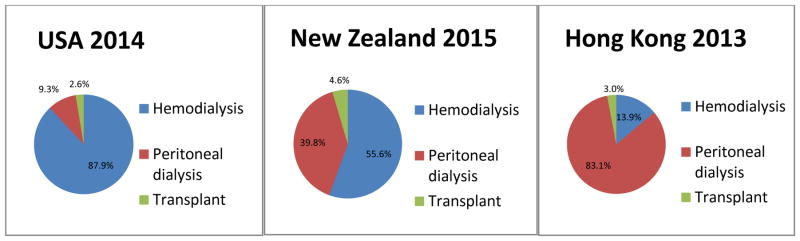
Of the incident cases in 2014, 87.9% of patients were treated with hemodialysis, 9.3% with peritoneal dialysis, and 2.6% with pre-emptive kidney transplant (Figure).1 Barring reporting bias and incomparable access to medical care internationally, many countries offer higher availability of home dialysis therapies compared to the U.S. For example, among incident ESRD cases, 83.1% and 39.8% were treated with peritoneal dialysis in Hong Kong and New Zealand, respectively (Figure).2,3 Focusing on prevalent hemodialysis cases, only 1.8% of U.S. patients are treated at home compared to 25.7% of patients in New Zealand. 1, 3
Figure.
Treatment of incident end-stage renal disease by renal replacement modality
One of the proposed predictors for underutilization of home-based dialysis options and delayed referral for kidney transplantation evaluation in the U.S. is incomplete or late RRT education.4 In a survey of 427 incident dialysis patients in Southern California region in 2002, less than a third of patients were presented with options of peritoneal dialysis, home hemodialysis, transplant, or conservative care.5 Numerous international studies have demonstrated that pre-ESRD education leads to greater patient selection of home dialysis modalities.6 For example, a multicenter study from Spain during 2010 to 2012 period noted a prevalence of peritoneal dialysis therapy up to 47.8% among ESRD patients who received pre-ESRD education compared to 6.5% among patients who did not receive the same education.7 Analogously, preemptive kidney transplantation was 1.5% and 0% respectively. Similar results have been reported in Norway, where 55% of pre-ESRD patients who participated in a Pre Dialysis Education Program opted for a self-care dialysis modality.8 In Canada, 82% of patients randomized to a patient-centered pre-dialysis education intervention chose a self-care dialysis modality compared to 50% in the standard care group (p=0.02).9 In the U.S., data from the Kidney Early Evaluation Program and United States Renal Data System suggest that participation in a community pre-ESRD educational program was associated with higher rates of ESRD preparation and survival.10 Similarly, participation in a renal transplantation patient education intervention in Georgia (U.S.) was associated with a nearly 40% greater fold completion of transplant evaluation at one-year (risk ratio of participation vs. non-participation = 1.38, 95% CI 1.12–1.71).11
Current standards of practice for in-person RRT education
The Centers for Medicare & Medicaid Services Conditions for Coverage and clinical dialysis practice guidelines12 indicate that all patients with kidney failure should receive information about RRT options.13 Most often, patients learn about options from their treating nephrologist during a typical 20 – 30 minute ambulatory encounter.14 In these situations, the conversation about RRT options must fit alongside physical examination, review of laboratory findings, and treatment recommendations on pharmaceutical and dietary interventions to optimize health and wellbeing. The opportunity for patients to learn new information about RRT options and ask questions is very limited by time.
Some nephrology practices refer patients to attend longer educational sessions led by dialysis-experienced nurse educators and offered by dialysis providers (e.g. Fresenius Kidney Care15, DaVita Kidney Smart16, or Satellite Healthcare17) or large medical centers.18 These in-person classes are typically 1.5 to 4 hours long, and may include a tour of in-center dialysis facilities or home dialysis equipment. Patients may also receive paper-based decision aides that aim to reinforce differences among RRT options, such as the “Yorkshire Dialysis Decision Aid” and the “My Kidneys, My Choice” pamphlet.19,20 As patients are contemplating their treatment options they may encounter other comparable patients or patients already receiving renal replacement, though these peer-to-peer interactions are not typically arranged.
Many of these programs were developed or refined after passage of the Medicare Improvement for Patients and Providers Act of 2008, which provides a financial reimbursement mechanism for up to 6 individual or group educational sessions for Medicare beneficiaries with CKD stages 4 or 5.21 Despite these available resources, however, uptake has been poor22 and pre-ESRD education largely remains suboptimal, often too quick and too late. In an older 2002 survey of incident dialysis patients, nearly 65% of respondents reported less than one hour of total discussion time about their dialysis treatment options. Additionally, about one-half of patients who received RRT education noted that the presentation occurred either after or less than a month prior to their first dialysis treatment.5
More recent studies have confirmed ongoing poor satisfaction with RRT education, reporting unequal and insufficient presentation of all available RRT modalities,23,24 and insufficient facilitated communication with experienced patients, whose experiences are often as equally influential as nephrologists’ recommendations about modality choice.25 Studies have also demonstrated patient support for use of technology to optimize RRT education and augment existing provider-patient discussions, provided that there is a diversity of options that can be tailored to fit patients’ needs and preferences.26,27
Use of telehealth for chronic kidney disease education
The suboptimal status quo of in-person RRT education affords great opportunity for improvement pertaining to reach and availability as well as efficacy. Technology has been used to enhance health care delivery for years with the overarching goal of achieving the triple aim of better health care, improved health outcomes and lower costs.28 And while the field of nephrology has been a slow adopter, there has been a steady increase in the use of technology for patient education related to early chronic kidney disease.29 Notable examples include websites that provide basic information about kidney disease, its complications, and topics relevant to patient safety. Low literacy pamphlets are available for download/print in addition to patient-centered videos to explain challenging concepts (i.e., National Kidney Disease Education Program: www.nkdep.nih.gov; Veterans Affairs: ckd.vacloud.us; Safe Kidney Care: www.safekidneycare.org). Interactive voice response systems with and without accompanying mobile text messages have also been used to deliver CKD education,30,31 as have mobile health applications that focus on self-management.32,33
Examples of RRT education using telehealth
Given the importance of education about RRT options superimposed on examples of successful use of technology for CKD and healthcare education as well as patient enthusiasm for technology-aided decision support, it is intuitive to employ telehealth in this aspect of pre-ESRD care. Review of currently published literature is notable for rare examples of telehealth to specifically address RRT education, though adoption of technology in this area is burgeoning in the form of telehealth clinics, informational and advocacy websites, mobile applications, social media, and multi-modality programs (Table).
Table.
Existing telehealth applications and examples that deliver education about renal replacement therapy.
| Telehealth Application | Definition | Examples |
|---|---|---|
| Telehealth clinics | Use of electronic information and telecommunication technologies to support long-distance clinical health care. | Telenephrology clinic for Zuni and Navajo communities; Minneapolis Veterans Affairs telenephrology clinic |
| Informational websites | Static websites resulting from academic initiatives or advocacy groups that provide educational content in form of pamphlets, graphs, and videos. | EPOCH-RRT; Veterans Affairs e-Kidney Clinic; “Preparing for Kidney Failure” by NKDEP; “You Have Options” by AAKP |
| Mobile Applications | Wireless communication that provides individualized data to patients, delivered by a mobile device, most often a tablet or smart phone. | iChoose Kidney application |
| Social Media | Internet based social networks that focus on peer support and mentorship. | National Kidney Foundation Facebook page and Twitter feed |
| Multi-modality programs | Technology aided programs that combine educational content with peer and professional support. | Cricket Health, Inc. |
EPOCH-RRT=Empowering Patients on Choices for Renal Replacement Therapy; NKDEP=National Kidney Disease Education Program; AAKP=American Association of Kidney Patients
Telehealth clinics
There are several examples of telenephrology clinics that have successfully delivered pre-ESRD care and likely incorporate some amount of pre-ESRD education. For example, Narva and colleagues describe the successful 9-year implementation of a telenephrology clinic in rural New Mexico that provided almost 2 thousand patient visits in Pueblo Zuni and Navajo communities.34 Data from the Minneapolis Veterans Affairs Health Care System demonstrated equivalent clinical outcomes among patients who received CKD care in a telenephrology clinic (consisting of home virtual visits and a monitoring device) and a conventional clinic.35 In publications detailing both of these initiatives, there were no explicit descriptions of RRT education though they are presumed to have been incorporated in the overall telehealth interventions.
Informational websites
Several websites are used to deliver RRT education and provide decision aids for patients to select an RRT modality.36 For example, the Empowering Patients on Choices for Renal Replacement Therapy (EPOCH-RRT) decision aid (www.choosingidalysis.org) was developed based on data from semi-structured interviews with patients with advanced CKD/ESRD.24 It was created as an adjunct to regular RRT education to empower patients to choose a modality that is most congruent with their values. The web-based Veterans Affairs e-Kidney Clinic (http://ckd.vacloud.us/rooms/treatment/#ekidneyclinic) is another example of an RRT education website that includes written, graphical and video content about all RRT options, including conservative management.37 While created to enhance kidney education for Veterans, the website is available for all individuals with CKD and their caregivers with access to the Internet. Recent data suggest a tripling of the VA eKidney Clinic website traffic since its launch in 2013.
RRT education is promoted on websites of many advocacy organizations as well. To enhance user engagement and relatability, the information is presented as answers to commonly asked questions and videos by patients and healthcare professionals. A few examples are “Preparing for Kidney Failure Treatment” by National Kidney Disease Education Program,38 “Choosing a Treatment for Kidney Failure” by National Kidney Foundation,39 and “You Have Options” by American Association of Kidney Patients.40 Taking on a narrower focus, National Kidney Foundation of Illinois maintains a bilingual (English and Spanish) website for the Hispanic/Latino community with ESRD, mainly focused on culturally sensitive education on living kidney donation but also briefly covers other treatment modalities.41 Informational content and visual design of this website were based on focus groups of patients, community members, and healthcare providers. Information is communicated by answers to commonly asked questions, videos of patient testimonials and interviews of community members, telenovelas, games, and links to research publications.
Mobile applications
Chronic disease education programs are increasingly adopting mobile health applications to support self-management practices, though little has been studied in the area of RRT education. One of the few examples in the literature is the “iChoose Kidney” electronic patient-provider decision aid that compares mortality on dialysis and kidney transplantation.42 This application aims to facilitate patient-provider discussions about the risks and benefits of transplantation versus dialysis. Its usability by patients and providers, efficacy at improving transplantation knowledge, and effectiveness at increasing selection of transplantation as a RRT modality are currently being evaluated in a randomized controlled trial.
Social media
Outside of scholarly publications, internet-based social networks provide consumers with educational content as well as peer support and mentorship. In fact, the National Kidney Foundation uses Facebook and Twitter for its outreach, with about 195,000 and 20,000 followers on each website respectively as of April 2017. Patients themselves can organize into information-sharing and support groups, although without oversight of credentialed professionals. Review of chat topics on Facebook43 or Kidney Patient Guide44 highlight patients’ desires to share emotions related to progression of CKD, experiences of undergoing a transplant evaluation, and self-care on dialysis.
Multimodality programs
Few technology-aided programs exist that combine educational materials, peer support, and professional oversight. Cricket™ Health Inc. recently launched a technology-enabled education program about ESRD treatment options, including conservative management, which is largely absent from the aforementioned programs. This multi-modality experience includes an online community of stakeholders, bringing together patients and caregivers with an experienced nephrology nurse and trained patient mentors undergoing various treatment modalities. Early feasibility data demonstrate that patients are able to utilize website to learn about their treatment options, engage with nurse and mentors to identify a treatment option that best fits their lifestyle, and in majority of cases, choose a home-based dialysis therapy.45
Potential benefits and challenges of RRT education via telehealth
The biggest benefit associated with telehealth for patient education lies in the incredible reach of mobile phone technology, which can be used for all aforementioned telehealth platforms. Recent estimates suggest that 90% of U.S. adults own a mobile device,46 and that nearly 60% of them access Internet with their phones.47 Additionally, studies suggest that African American and English-speaking Latinos are the most active users of the Mobile Web in the U.S.48 Because racial/ethnic minorities are disproportionately affected by ESRD,1 are less likely to dialyze using a home-based modality,49 and are less likely to be referred for transplant evaluation and waitlisted for transplantation,50 these statistics have direct relevance to RRT education. Availability of Internet-based technology can also increase the reach of telehealth education to pre-ESRD populations with limited mobility from physical disability or frailty, and to those patients who live in rural areas.
Compared to in-person RRT educational experiences, telehealth educational opportunities are also more flexible and adaptable to learner preferences. They can include both visual and auditory modalities of content delivery. Additionally, many applications, including virtual support groups (both live and asynchronous) and videos, offer more opportunity for engagement with the material and reinforcement of knowledge, for example, with knowledge assessment tests and games that emphasize educational concepts.51 They also encourage repetition and reinforcement. For example, patients and their caregivers can review a video multiple times or participate in different online educational group discussions within the comfort and privacy of their own home, without time constraints imposed by a health educator or a nephrology clinic. Importantly, all of these modalities occur outside the traditional health care encounter, allowing healthcare professionals the opportunity to reinforce key ideas and answer questions during a medical visit without requiring the time to fully explain different RRT options.
There are notable challenges associated with the use of telehealth for education, however, including those associated with data privacy/security, governance, and mistrust of clinical content delivered via telehealth applications. Additionally, matching patients with appropriate technologies for education is critical.52 A “digital divide” among persons with different ages, education levels, literacy, numeracy, and incomes has been described, which may be of particular relevance for RRT education.53 For example, ESRD prevalence is the highest among individuals 65 – 74 years old;1 many of these patients may not feel comfortable with technology and may prefer in-person education/discussions about their options. Comfort with telehealth may also be influenced by familiarity and prior access to technology.54 Data have suggested that low health literacy and limited formal education are quite prevalent among individuals with CKD55 and ESRD, potentially limiting the efficacy of telehealth for optimal RRT education.56
Conclusion
In conclusion, despite the challenges associated with technology-aided delivery of education, early data suggest that it can provide either an alternative, or more likely, an important supplemental resource for patients and families to learn about treatment options for ESRD. Timely and comprehensive teaching is likely to increase patient awareness of home-based dialysis treatments, conservative management, and kidney transplantation as feasible alternatives to the most predominant and costly in-center hemodialysis therapy. Convenience of remote and on-demand telehealth education compared to in-person education has the potential to reduce patient burden in terms of time and cost of travel, improve access for geographically isolated or frail patients, reduce provider costs in terms of personnel and facilities fees, and increase patient satisfaction and engagement with pre-ESRD and post-ESRD care. Finally, modern patients seek online communities both for educational content as well as emotional support. It is receptive and advantageous to the nephrology community to offer the delivery of pre-ESRD education through diverse technology-enabled media. While progress has been made in this field, it is clear that much work lies ahead. Only through intentional study can we improve the content and delivery of RRT education to maximally support our diverse patients.
Acknowledgments
Support: DST is supported by R01DK11041301 from the National Institute of Diabetes and Digestive and Kidney Diseases.
Footnotes
Disclosures: AM is Medical Director at Cricket Health, Inc. San Francisco, USA.
References
- 1.USRDS. Annual Date Report. [Accessed Feb 1 2017];Chapter 1: Incidence, Prevalence, Patient Characteristics, and Treatment Modalities. 2016 https://www.usrds.org/2016/view/v2_01.aspx.
- 2.Leung CB, Cheung WL, Li PK. Renal registry in Hong Kong-the first 20 years. Kidney Int Suppl (2011) 2015;5(1):33–38. doi: 10.1038/kisup.2015.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Australia & New Zealand Dialysis & Transplant Registry. [Accessed Feb 1 2017];The 39th Annual ANZDATA Report. 2016 http://www.anzdata.org.au/v1/report_2016.html.
- 4.Golper T. Patient education: can it maximize the success of therapy? Nephrol Dial Transplant. 2001;16(Suppl 7):20–24. doi: 10.1093/ndt/16.suppl_7.20. [DOI] [PubMed] [Google Scholar]
- 5.Mehrotra R, Marsh D, Vonesh E, Peters V, Nissenson A. Patient education and access of ESRD patients to renal replacement therapies beyond in-center hemodialysis. Kidney Int. 2005;68(1):378–390. doi: 10.1111/j.1523-1755.2005.00453.x. [DOI] [PubMed] [Google Scholar]
- 6.Key SM. Optimizing dialysis modality choices around the world: a review of literature concerning the role of enhanced early pre-ESRD education in choice of renal replacement therapy modality. Nephrol Nurs J. 2008;35(4):387–394. quiz 395. [PubMed] [Google Scholar]
- 7.Prieto-Velasco M, Quiros P, Remon C Spanish Group for the Implementation of a Shared Decision Making Process for RRTCwPDAT. The Concordance between Patients’ Renal Replacement Therapy Choice and Definitive Modality: Is It a Utopia? PLoS One. 2015;10(10):e0138811. doi: 10.1371/journal.pone.0138811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goovaerts T, Jadoul M, Goffin E. Influence of a pre-dialysis education programme (PDEP) on the mode of renal replacement therapy. Nephrol Dial Transplant. 2005;20(9):1842–1847. doi: 10.1093/ndt/gfh905. [DOI] [PubMed] [Google Scholar]
- 9.Manns BJ, Taub K, Vanderstraeten C, et al. The impact of education on chronic kidney disease patients’ plans to initiate dialysis with self-care dialysis: a randomized trial. Kidney Int. 2005;68(4):1777–1783. doi: 10.1111/j.1523-1755.2005.00594.x. [DOI] [PubMed] [Google Scholar]
- 10.Kurella Tamura M, Li S, Chen SC, et al. Educational programs improve the preparation for dialysis and survival of patients with chronic kidney disease. Kidney Int. 2014;85(3):686–692. doi: 10.1038/ki.2013.369. [DOI] [PubMed] [Google Scholar]
- 11.Patzer RE, Perryman JP, Pastan S, et al. Impact of a patient education program on disparities in kidney transplant evaluation. Clin J Am Soc Nephrol. 2012;7(4):648–655. doi: 10.2215/CJN.10071011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moss AH. Revised dialysis clinical practice guideline promotes more informed decision-making. Clin J Am Soc Nephrol. 2010;5(12):2380–2383. doi: 10.2215/CJN.07170810. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Medicare & Medicaid Services (CMS) H. Conditions for coverage for end-stage renal disease facilities; Final Rule. Fed Regist. 2008;(73):20369–29484. https://www.cms.gov/Regulations-and-Guidance/Legislation/CFCsAndCoPs/downloads/esrdfinalrule0415.pdf. [PubMed]
- 14.Morton RL, Howard K, Webster AC, Snelling P. Patient INformation about Options for Treatment (PINOT): a prospective national study of information given to incident CKD Stage 5 patients. Nephrol Dial Transplant. 2011;26(4):1266–1274. doi: 10.1093/ndt/gfq555. [DOI] [PubMed] [Google Scholar]
- 15.Fresenius Kidney Care. [Accessed Feb 1 2017];Treatment Options Class. https://www.freseniuskidneycare.com/ckd-treatment/dialysis-treatment-options-program.
- 16.DaVita. [Accessed Feb 1 2017];Kidney Smart Class. https://www.davita.com/services/find-a-kidney-education-class/index.cfm?gclid=CJ7duNS61NICFRB2fgodYJkAOA.
- 17.Satellite Healthcare. [Accessed Feb 1 2017];Dialysis Treatment Options. http://www.satellitehealth.com/for-patients-families/what-to-expect-on-your-first-day/options.
- 18.Greer RC, Ameling JM, Cavanaugh KL, et al. Specialist and primary care physicians’ views on barriers to adequate preparation of patients for renal replacement therapy: a qualitative study. BMC Nephrol. 2015;16:37. doi: 10.1186/s12882-015-0020-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Winterbottom AE, Gavaruzzi T, Mooney A, et al. Patient Acceptability of the Yorkshire Dialysis Decision Aid (YoDDA) Booklet: A Prospective Non-Randomized Comparison Study Across 6 Predialysis Services. Perit Dial Int. 2016;36(4):374–381. doi: 10.3747/pdi.2014.00274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fortnum D, Grennan K, Smolonogov T. End-stage kidney disease patient evaluation of the Australian ‘My Kidneys, My Choice’ decision aid. Clin Kidney J. 2015;8(4):469–475. doi: 10.1093/ckj/sfv050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Young HN, Chan MR, Yevzlin AS, Becker BN. The rationale, implementation, and effect of the Medicare CKD education benefit. Am J Kidney Dis. 2011;57(3):381–386. doi: 10.1053/j.ajkd.2010.10.056. [DOI] [PubMed] [Google Scholar]
- 22.Davis JS, Zuber K. Implementing patient education in the CKD clinic. Adv Chronic Kidney Dis. 2013;20(4):320–325. doi: 10.1053/j.ackd.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 23.Fadem SZ, Walker DR, Abbott G, et al. Satisfaction with renal replacement therapy and education: the American Association of Kidney Patients survey. Clin J Am Soc Nephrol. 2011;6(3):605–612. doi: 10.2215/CJN.06970810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dahlerus C, Quinn M, Messersmith E, et al. Patient Perspectives on the Choice of Dialysis Modality: Results From the Empowering Patients on Choices for Renal Replacement Therapy (EPOCH-RRT) Study. Am J Kidney Dis. 2016;68(6):901–910. doi: 10.1053/j.ajkd.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 25.Rygh E, Arild E, Johnsen E, Rumpsfeld M. Choosing to live with home dialysis-patients’ experiences and potential for telemedicine support: a qualitative study. BMC Nephrol. 2012;13:13. doi: 10.1186/1471-2369-13-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sieverdes JC, Nemeth LS, Magwood GS, et al. Patient-Centered mHealth Living Donor Transplant Education Program for African Americans: Development and Analysis. JMIR Res Protoc. 2015;4(3):e84. doi: 10.2196/resprot.3715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vassilev I, Rowsell A, Pope C, et al. Assessing the implementability of telehealth interventions for self-management support: a realist review. Implement Sci. 2015;10:59. doi: 10.1186/s13012-015-0238-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Soman SS, Yee J. Nephrology and Telehealth: Now? or Now! Adv Chronic Kidney Dis. 2017;24(1):1–3. doi: 10.1053/j.ackd.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 29.Tuot DS, Boulware LE. Telehealth Applications to Enhance CKD Knowledge and Awareness Among Patients and Providers. Adv Chronic Kidney Dis. 2017;24(1):39–45. doi: 10.1053/j.ackd.2016.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tuot DS, Velasquez A, McCulloch CE, et al. The Kidney Awareness Registry and Education (KARE) study: protocol of a randomized controlled trial to enhance provider and patient engagement with chronic kidney disease. BMC Nephrol. 2015;16:166. doi: 10.1186/s12882-015-0168-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fink JC, Doerfler RM, Yoffe MR, et al. Patient-Reported Safety Events in Chronic Kidney Disease Recorded With an Interactive Voice-Inquiry Dial-Response System: Monthly Report Analysis. J Med Internet Res. 2016;18(5):e125. doi: 10.2196/jmir.5203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ong SW, Jassal SV, Porter E, Logan AG, Miller JA. Using an electronic self-management tool to support patients with chronic kidney disease (CKD): a CKD clinic self-care model. Semin Dial. 2013;26(2):195–202. doi: 10.1111/sdi.12054. [DOI] [PubMed] [Google Scholar]
- 33.McManus RJ, Mant J, Haque MS, et al. Effect of self-monitoring and medication self-titration on systolic blood pressure in hypertensive patients at high risk of cardiovascular disease: the TASMIN-SR randomized clinical trial. JAMA. 2014;312(8):799–808. doi: 10.1001/jama.2014.10057. [DOI] [PubMed] [Google Scholar]
- 34.Narva AS, Romancito G, Faber T, Steele ME, Kempner KM. Managing CKD by Telemedicine: The Zuni Telenephrology Clinic. Adv Chronic Kidney Dis. 2017;24(1):6–11. doi: 10.1053/j.ackd.2016.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ishani A, Christopher J, Palmer D, et al. Telehealth by an Interprofessional Team in Patients With CKD: A Randomized Controlled Trial. Am J Kidney Dis. 2016;68(1):41–49. doi: 10.1053/j.ajkd.2016.01.018. [DOI] [PubMed] [Google Scholar]
- 36.Green JA, Boulware LE. Patient Education and Support During CKD Transitions: When the Possible Becomes Probable. Adv Chronic Kidney Dis. 2016;23(4):231–239. doi: 10.1053/j.ackd.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 37.Crowley ST, Belcher J, Choudhury D, et al. Targeting Access to Kidney Care Via Telehealth: The VA Experience. Adv Chronic Kidney Dis. 2017;24(1):22–30. doi: 10.1053/j.ackd.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 38.National Kidney Disease Education Program. [Accessed Feb 1 2017];Preparing for Kidney Failure Treatment. https://www.niddk.nih.gov/health-information/health-communication-programs/nkdep/learn/living/kidney-failure/prepare-for-treatment/Pages/prepare-for-treatment.aspx.
- 39.National Kidney Foundation. [Accessed Feb 1, 2017];Choosing A Treatment For Kidney Failure. https://www.kidney.org/sites/default/files/docs/choosing_treat.pdf.
- 40.American Association of Kidney Patients. [Accessed Feb 1, 2017];You Have Options. https://aakp.org/dialysis/you-have-options/
- 41.NKF Illinois. [Accessed Feb 1 2017];Inform Yourself About Living Kidney Donation for Hispanics/Latinos. http://informate.org/english/
- 42.Patzer RE, Basu M, Mohan S, et al. A Randomized Controlled Trial of a Mobile Clinical Decision Aid to Improve Access to Kidney Transplantation: iChoose Kidney. Kidney Int Rep. 2016;1(1):34–42. doi: 10.1016/j.ekir.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Facebook. [Accessed March 1, 2017];Renal Support Network. https://www.facebook.com/RenalSupportNetwork/
- 44.Kidney Patient Guide. [Accessed March 1 2017];The Treatment of Kidney Failure. http://www.kidneypatientguide.org.uk/dialysis.php.
- 45.Malkina ABB, Rajan A, et al. Technology-Enabled Education on ESRD Treatment Options via Integrated Patient and Provider Online Community. National Kidney Foundation Spring Clinical Meeting; Orlando, FL. April 2017. [Google Scholar]
- 46.Pew Research Center. [Accessed June 15 2016]; Available at: http://www.pewinternet.org/data-trend/mobile/cell-phone-and-smartphone-ownership-demographics/
- 47.Pew Research Center. [Accessed June 15 2016]; Available at: http://www.pewinternet.org/data-trend/mobile/cell-phone-activities/
- 48.Pew Research Center. [Accessed June 15 2016]; Available at: http://www.pewinternet.org/data-trend/mobile/cell-phone-and-smartphone-ownership-demographics/
- 49.Wallace EL, Lea J, Chaudhary NS, et al. Home Dialysis Utilization Among Racial and Ethnic Minorities in the United States at the National, Regional, and State Level. Perit Dial Int. 2017;37(1):21–29. doi: 10.3747/pdi.2016.00025. [DOI] [PubMed] [Google Scholar]
- 50.Patzer RE, Perryman JP, Schrager JD, et al. The role of race and poverty on steps to kidney transplantation in the Southeastern United States. Am J Transplant. 2012;12(2):358–368. doi: 10.1111/j.1600-6143.2011.03927.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shneerson C, Windle R, Cox K. Innovating information-delivery for potential clinical trials participants. What do patients want from multi-media resources? Patient Educ Couns. 2013;90(1):111–117. doi: 10.1016/j.pec.2012.06.031. [DOI] [PubMed] [Google Scholar]
- 52.Weiner S, Fink JC. Telemedicine to Promote Patient Safety: Use of Phone-Based Interactive Voice-Response System to Reduce Adverse Safety Events in Pre-dialysis CKD. Adv Chronic Kidney Dis. 2017;24(1):31–38. doi: 10.1053/j.ackd.2016.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sarkar U, Karter AJ, Liu JY, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc. 2011;18(3):318–321. doi: 10.1136/jamia.2010.006015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Diamantidis CJ, Becker S. Health information technology (IT) to improve the care of patients with chronic kidney disease (CKD) BMC Nephrol. 2014;15:7. doi: 10.1186/1471-2369-15-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Devraj R, Borrego M, Vilay AM, Gordon EJ, Pailden J, Horowitz B. Relationship between Health Literacy and Kidney Function. Nephrology (Carlton) 2015;20(5):360–367. doi: 10.1111/nep.12425. [DOI] [PubMed] [Google Scholar]
- 56.Cavanaugh KL, Wingard RL, Hakim RM, et al. Low health literacy associates with increased mortality in ESRD. J Am Soc Nephrol. 2010;21(11):1979–1985. doi: 10.1681/ASN.2009111163. [DOI] [PMC free article] [PubMed] [Google Scholar]