Abstract
Background
Rotavirus vaccination introduction in routine immunization is under consideration in Pakistan. Data on the baseline epidemiology of intussusception will inform surveillance strategies for intussusception after rotavirus vaccine introduction in Pakistan. We describe the epidemiology of intussusception-associated hospitalizations among children <2 years of age in Karachi, Pakistan.
Methods
We conducted a retrospective chart review for July 01, 2012 through June 30, 2015 at the National Institute of Child Health (NICH) and Aga Khan University Hospital (AKUH) Karachi. At AKUH, the International Classification of Disease, ninth revision, code 560.0 for intussusception was used to retrieve intussusception case records. At NICH, daily Operation Theater, Emergency Room, and surgical daycare log sheets and surgical ward census sheets were used to identify cases. Records of children who fulfilled eligibility criteria and the Brighton Collaboration level one case definition of intussusception were selected for data analysis. We used structured case report forms to extract data for the descriptive analysis.
Results
We identified 158 cases of confirmed intussusception; 30 cases (19%) were from AKUH. More than half (53%) of the cases occurred in children aged 6–12 months, followed by 35% among those aged <6 months. Two-thirds (106/158) of the cases were male. The most common presenting complaints were vomiting and bloody stool. At NICH, almost all (93%) were managed surgically, while at AKUH, ~57% of the cases were managed with enemas. Three deaths occurred, all from NICH. Cases occurred without any seasonality. At NICH, 4% (128/3618) of surgical admissions among children aged <2 years were attributed to intussusception, while that for AKUH was 2% (30/1702).
Conclusion
In this chart review, intussusception predominantly affected children 0–6 months of age and occurred more commonly in males. This information on the baseline epidemiology of intussusception will inform post-vaccine introduction adverse event monitoring related to intussusception in Pakistan.
Keywords: Intussusception, Rotavirus vaccine, Pakistan
1. Introduction
Intussusception (IS) is the most common cause of abdominal surgical emergencies in infants and children. It is characterized by a palpable abdominal mass, passage of bloody stool, vomiting and colicky abdominal pain, most commonly in children of 3 months to 5 years of age [1,2]. IS cases can resolve spontaneously; those that do not can be reduced by enema or surgery if treated immediately. However, delaying care can result in death [3]. Globally, the annual rates of naturally occurring intussusception are 74 per 100,000 infants, ranging from 9 to 328 per 100,000 [4], with higher rates reported in Asian countries such as Vietnam, Singapore, Japan, and Taiwan (71–302 cases per 100,000 infants) [3].
The exact mechanism that triggers IS remains unclear, but it is believed that a lesion in the bowel wall or irritant within the bowel lumen may cause a hyperactive peristaltic pattern resulting in invagination of one segment of bowel into an adjacent segment [5,6]. Data from different studies have shown an association of adenovirus infection with increased risk of IS, but no link with natural rotavirus infection has been established [7,8]. However, due to an association between a previously available oral rotavirus vaccine and intussusception, as well as a low-level association in post-marketing studies of the 2 currently widely used rotavirus vaccines (Rotarix, GSK, and RotaTeq, Merck) [9–12], there has been interest in understanding the epidemiology, etiology and pathophysiology of naturally occurring intussusception in infants in settings where rotavirus vaccine will soon be introduced [13].
Data on the epidemiology of intussusception-associated hospitalizations in Pakistan are limited. Given that the public health impact of rotavirus vaccination could be substantial in Pakistan, where diarrhea accounts for 16% of all child deaths [14], an assessment of the baseline epidemiology of intussusception will be useful for public health professionals and the Government of Pakistan in informing decisions related to rotavirus vaccine introduction.
The aim of this study is to describe the epidemiology of intussusception-associated hospitalizations among children <2 years of age at two tertiary care hospitals in Karachi, Pakistan.
2. Methods
2.1. Study design and setting
We conducted a retrospective hospital-based chart review of children <2 years of age presenting with intussusception to Aga Khan University Hospital (AKUH) and the National Institute of Child Health (NICH) in Karachi, Pakistan during July 2012 through June 2015. AKUH is a 630-bedded private tertiary care hospital located in Gulshan Town, Karachi. The hospital has 116 pediatric beds including 22 beds exclusively for pediatric surgery patients. The hospital predominantly attends to an upper and upper-middle class population. However, but due to the availability of charity in the form of Zakat, which is the Muslim practice of obligatory donations for those with assets above a certain threshold, as well as patient welfare funds, the hospital also receives patients from lower and lower-middle income families of Karachi and its surroundings. The hospital maintains electronic records of both outpatients and inpatients using the international classification of disease, ninth revision (ICD-9) coding system. All patients visiting AKUH are assigned a unique medical record number (MR #) which carries all the hospital records of that patient and is used on each subsequent visit. If a patient forgets his or her number, efforts are made to retrieve the number electronically using other identifiers.
NICH is one of the largest public sector children’s hospitals in the country. It is located in one of the most populated towns (Saddar town) of Karachi, Pakistan. It is the largest referral center for pediatric surgery in Sindh Province. NICH has 500 pediatric beds including 2 surgical units comprised of 80 beds. In addition, it has a surgical Intensive Care Unit (ICU) and Intensive Therapy Unit (ITU). NICH caters to all socioeconomic levels of the society, including the underprivileged majority. The hospital has a paper-based medical record system. Each patient admitted to the hospital receives a medical record number, and a medical record file carrying that particular number is open for the patient. All records including diagnostic reports are filed in this record which is submitted to the medical record department after patient discharge. Medical records are archived based on the ward, month, and year.
AKUH and NICH were selected for this study due to their high volume of pediatric surgeries, and their broad coverage of both the underprivileged and privileged classes of society.
2.2. Case definition and data abstraction
Charts of children with a confirmed diagnosis of intussusception based on level 1 Brighton Collaboration criteria [15] were reviewed for this study. This case definition for IS uses three main criteria: (1) surgical criteria: demonstration of invagination of intestine on surgery; (2) radiological criteria: demonstration of the invagination of intestine on air or liquid contrast enema or demonstration of an intra-abdominal mas on abdominal ultrasound with specific characteristics features (target sign or doughnut sign on transverse section and a pseudo kidney or sandwich sign on longitudinal section), that is proven to be reduced by hydrostatic enema on post-reduction ultrasound; or (3) autopsy criteria: demonstration of the invagination of the intestine on autopsy.
At AKUH, ICD-9 code 560.0 was used to identify patients admitted with intussusception. Diagnosis of congenital intussusception (code 751.5) and appendix (code 543.5) were excluded. Trained research associates retrieved records for each identified patient to confirm the diagnosis of intussusception using level 1 Brighton criteria. At NICH, a dedicated research associate identified potential cases of intussusception by reviewing the emergency room (ER), day care surgery, Operation theater (OT) registers and ward census sheets. Records were then retrieved from archives. The research associate reviewed all the selected medical record files to determine whether the case fulfilled the screening criteria and case definition for confirmed intussusception.
For each confirmed intussusception case, we used structured case report forms (CRFs) to abstract information on the child’s age, sex, transfer status from another hospital, clinical characteristics, diagnosis, and management of intussusception, complications, chronic medical conditions, and outcome at discharge.
The study was approved by the ethical review committee (ERC) of Aga khan University (AKU) and Institutional review board (IRB) of the NICH, Karachi, Pakistan.
2.3. Analysis plan
All data were entered into FoxPro. Data were simultaneously entered by two data entry operators and cross-checked for any errors or missing information. The analysis was conducted using STATA version 11.0. Frequencies with percentages were calculated for categorical data.
3. Results
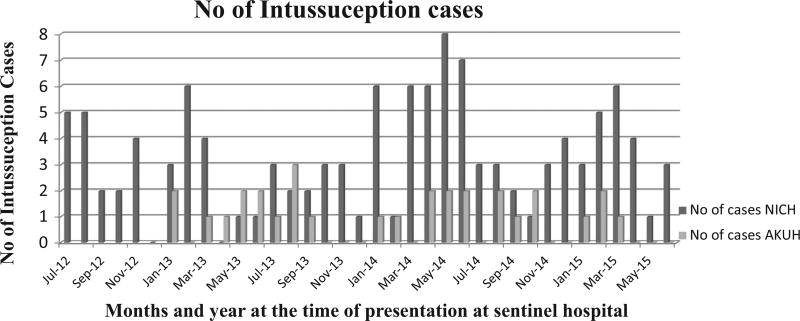
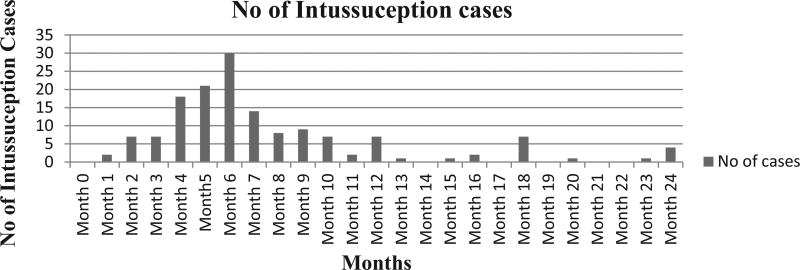
We identified 149 confirmed intussusception cases among children <2 years of age in the two sentinel hospitals of which 30/149 (20%) cases were from AKUH and the remaining cases were from NICH (Table 1). Fig. 1 shows the distribution of intussusception cases across the three-year study period. Intussusception hospitalizations occurred without any particular pattern or seasonality and occurred throughout the year in both sites (Fig. 1). Over half 77 (52%) of the intussusception cases occurred among children aged 6–12 months, followed by 55 (37%) among children <6 months of age, and 17 (11%) among children aged 12–24 months. (The number of intussusception-associated hospitalizations peaked among children aged 4–7 months (Fig. 2); there were only 16 cases (10%) among children aged 1–3 months of age as compared to 69 cases (46%) among children aged 4–6 months.) About two-thirds of the intussusception cases were male. None of the children had received rotavirus vaccine. Thirty-four (29%) cases were transferred to NICH from area hospitals, whereas none of the AKUH cases were transfers from other hospitals. Overall, the most common complaints at the time of presentation to hospital were vomiting in 103/120 (86%) children, bloody stools in 100/120 (83%), and abdominal pain in 79/104 (76%). At NICH, 87/100 (87%) of the patients presented with complaints of bloody stool compared to 13/20 (65%) at AKUH. Similarly at NICH, 85/97 (88%) of children presented with vomiting compared to 18/23 (78%) at AKUH.
Table 1.
Number of intussusception cases by year of children <2 years of age presented to the sentinel hospitals of Karachi, Pakistan (July 2012–June 2015).
| Annual cases | AKUH | NICH | Total |
|---|---|---|---|
| July 2012–June 2013 | 6 (20) | 36 (31) | 42 (28) |
| July 2013–June 2014 | 14 (47) | 48 (40) | 62 (42) |
| July 2014–June 2015 | 10 (33) | 35 (29) | 45 (30) |
Fig. 1.
Distribution of intussusception cases among children <2 years of age according to the month and year of presentation at sentinel hospitals, Karachi, Pakistan (July 2012–June 2015).
Fig. 2.
Distribution of intussusception cases among children <2 years of age, according to age in months at sentinel hospitals, Karachi, Pakistan (July 2012–June 2015).
At NICH, almost all (118/119) intussusception cases were diagnosed surgically while, at AKUH, two-thirds (19/30) of the cases were diagnosed radiologically (Table 3). No cases were identified using the autopsy criteria. Overall, 129/149 (87%) of the cases were treated surgically. At NICH, where radiological management is not routinely performed, 118/119 (99%) of cases were managed surgically; of those that were surgically treated, 22/118 (18%) required intestinal resection. In contrast, at AKUH, more than half of the cases 17/30 (57%) were treated by hydrostatic/pneumatic enema. For 12/30 (40%) of the patients, enema failed and surgical management was required. Of these, only 1/12 (8%) cases required intestinal resection. There were a total of 1702 surgical admissions among children <2 years of age at AKUH during the study period, making 2% (30/1702) proportion of intussusception associated admissions in the same age group. At NICH, there were total 3618 surgical admissions among children less than 2 years of age during the study period and the proportion of intussusception associated admissions was 4% (128/3618).
Table 3.
Diagnostic and Surgical characteristics of children less than 2 years of age with intussusception presenting to sentinel sites, Karachi Pakistan, (July 2012–June 2015).
| Characteristics | AKUH n = 30 (%) |
NICH n = 119 (%) |
Total N = 149 (%) |
|---|---|---|---|
| Diagnostic criteria (Brighton 1)b | |||
| Surgery | 11 (37) | 118 (99) | 129 (87) |
| Radiology | |||
| Demonstration of invagination of the intestine by either air or liquid contrast enema | 0 | 0 | 0 |
| Demonstration of an intra-abdominal mass by abdominal ultrasound | 19 (63) | 25 (21) | 44 (30) |
| Autopsy | 0 | 0 | 0 |
| Management of the intussusception | |||
| Hydrostatic/pneumatic enema | 17 (57) | 0 | 17 (11) |
| Surgery | 12 (40) | 118 (99) | 130 (87) |
| Intestinal resection among those who had surgery | 1 (3) | 22 (18) | 23 (15) |
| Surgical informationa | #cases/total with data available (%) | #cases/total with data available (%) | #cases/total with data available (%) |
|
| |||
| Location of the intussusception | |||
| Ileocolic | 23/30 (77) | 98/110 (89) | 121/140 (86) |
| Colocolic | 5/30 (17) | 0 | 5/140 (4) |
| Ileo-ileal | 2/30 (6) | 12/110 (11) | 14/140 (10) |
| Lead point identified | 0/15 (0) | 3/28 (11) | 3/43 (7) |
| Complications | |||
| Wound infection | 0/22 (0) | 2/117 (2) | 2/139 (1) |
| Wound dehiscence | 0/21 (0) | 2/118 (2) | 2/139 (1) |
| Peritonitis | 0/21 (0) | 0/118 (0) | 0/139 (0) |
| Secondary intestinal obstruction | 0/21 (0) | 1/118 (1) | 1/139 (1) |
| Other complication | 0/21 (0) | 1/119 (1) | 1/140 (1) |
AKUH = Aga Khan University Hospital, NICH = National Institute of Child Health.
Numbers may not sum up to the total because of unavailable data.
Multiple responses.
The intussusception foci were ileocolic in 121/140 children (86%), followed by ileo-ileal in 14/140 (10%) and colocolic in 5/140 (4%). There were no major complications reported among the children post operatively. Three out of the 119 intussusception cases at NICH (2%) died post-operatively, while no deaths occurred at AKUH (Table 2).
Table 2.
Demographic and clinical characteristics of children <2 years of age presented with intussusception to the sentinel hospitals of Karachi, Pakistan (July 2012–June 2015).
| Characteristics | AKUH n = 30 (%) | NICH n = 119 (%) | Total N = 149 (%) |
|---|---|---|---|
| Age in months | |||
| <6 months | 6 (20) | 49 (41) | 55 (37) |
| 6–12 months | 17 (57) | 60 (51) | 77 (52) |
| >12 & <24 months | 7 (23) | 10 (8) | 17 (11) |
| Sex | |||
| Male | 21 (70) | 79 (66) | 100 (67) |
| Female | 9 (30) | 40 (34) | 49 (33) |
| Transferred from another hospital | 0 | 34 (29) | 34 (23) |
| Received Rotavirus vaccine | 0 | 0 | 0 |
| Outcome at discharge | |||
| Died | 0 | 3 (2) | 3 (2) |
| Survived | 30 (100) | 115 (97) | 145 (97) |
| Transferred | 0 | 1 (1) | 1(1) |
| Clinical informationa | # Cases/total with data available (%) | # Cases/total with data available (%) | # Cases/total with data available (%) |
|
| |||
| Fever | 1/12 (8) | 30/64 (47) | 31/76 (41) |
| Vomiting | 18/23 (78) | 85/97 (88) | 103/120 (86) |
| Diarrhea | 6/15 (40) | 22/58 (38) | 28/73 (38) |
| Constipation | 1/11 (9) | 31/61 (51) | 32/72(44) |
| Bloody stools | 13/20 (65) | 87/100 (87) | 100/120 (83) |
| Abdominal pain | 13/19 (68) | 66/85 (78) | 79/104 (76) |
AKUH = Aga Khan University Hospital, NICH = National Institute of Child Health.
Numbers may not sum up to the total because of unavailable data.
4. Discussion
This is the first study reporting the frequencies and epidemiology of confirmed cases of intussusception from a large tertiary care private hospital and the largest public sector pediatric hospital in Karachi, Pakistan. This study found that intussusception was most common during first year of life, with a higher proportion of cases occurring during 6–12 months of age. There was a steep rise in the number of cases after 3 months of age peaking at 6 months and then gradually decreasing. Some studies have reported similar age trends as that seen in our analysis [16,17], while others have found different trends. One retrospective review of intussusception associated hospitalization among children <2 years of age in Matlab area of Bangladesh reported a higher proportion of intussusception occurring in children aged 0–5 months, followed by those aged 6–11 months [18]. This difference in age at onset of intussusception in Bangladesh could be attributed to the difference in case definition for identifying intussusception cases. While this study used the level 1 Brighton criteria for definite diagnosis of intussusception, the study in Bangladesh also included probable and possible Brighton Collaboration criteria case definitions, which resulted in the identification of 4 probable and 19 possible intussusception cases. The clinical criteria for diagnosing probable or possible intussusception are sensitive but not specific, and hence it might identify mild or transient cases of intussusception earlier in life. Interestingly, a study from Hanoi, Vietnam which used the ICD-10 coding system and diagnostic criteria by the Japanese Society of Emergency Paediatrics for the identification of intussusception cases, reported a higher number of cases during 2nd year of age. The diagnosis was based on the classical triad of intussusception (i.e., vomiting, abdominal pain, bloody stools) which was present only in 26 patients (13.9%) as compared to 122 patients (65.2%) who showed a combination of vomiting, abdominal pain and abdominal mass. Air enema was successfully used for the treatment of 185 (99%) patients with intussusception and only two (1%) out of 187 patients required surgery patients while in our study 82% of the cases were resolved by surgery. The relatively low proportion of bloody stools (17%) observed in the Vietnam study was probably related to the short duration of time before presentation at the hospital (a median of 5 h). Moreover, they found increasing trend of intussusception with a peak at 11 and 12 months of age following by a persistent higher number of cases till 23 months of age and then a gradual decline until 3 years of life and beyond. The study in Vietnam also observed higher number of intussusception even after 2 years of age [19].
Like other studies, we found the predominance of intussusception among the male population. This finding is very consistent with the available literature globally [20], however the exact mechanism of male preponderance for intussusception is not well understood. Similarly, we found the occurrence of intussusception throughout the year without any observed seasonality. Earlier studies in the region has also found similar pattern of intussusception without any obvious variation during the year [18–21].
Regarding clinical management of intussusception, we found that a substantial number of intussusception cases (40% at AKUH and 99% at NICH) were managed surgically. The wide difference between management techniques between the two sentinel sites may be due to the following reasons: first, radiographic management is not routinely performed at NICH, and second, delayed presentation of the cases to NICH may have led to a need for surgical management. Also, about 29% of the intussusception cases were referred from other hospitals to NICH, suggesting higher severity of cases. In contrast, none of the children at AKUH were transferred from another hospital. A systematic review of intussusception reported highest rates of surgical management from Africa (77%), and central and South America (86%) as compared to the other regions (13–29%) [20]. Our surgery rates are higher than that reported for the Eastern Mediterranean region, however, it is lower than Africa and South America [17]. Similarly, the case fatality in our study was about 2%, slightly higher than the region (<1%) and lower than African region (9%).
We observed only few cases during the first three months of life. This finding is consistent with earlier studies in Bangladesh [18] and Vietnam [19] which also reported either very few cases or no cases at all during the first 3 months of age. This finding is crucial from a programmatic point of view. The World Health Organization currently recommends that the first and second doses of rotavirus vaccines be administered early in life at ages 6 and 10 weeks [22], when the incidence of naturally occurring intussusception is very low [20]. This study demonstrated that the background number of intussusception is very low in the age group that would receive the first dose of the rotavirus vaccine. Moreover, this age group is outside the risk period where the incidence of intussusception sharply increased. Nevertheless, the completion of subsequent doses of rotavirus vaccine would occur toward the age period when a sharp increase in the intussusception cases occurred. Therefore, it is highly recommended to complete the full dose of rotavirus vaccination earlier in life to avoid the occurrence of intussusception by chance alone post vaccination [19,20].
4.1. Limitations
This retrospective chart review has certain limitations that may affect the interpretation of our findings. First, at AKUH, we may have missed cases which were not correctly coded as intussusception, though the probability of such error is quite rare as the staff are well-trained in the ICD-9 and ICD-10 coding systems and random quality checks are performed routinely. Along the same lines, although we have used various hospital registers to identify the medical record numbers of the suspected intussusception cases at NICH, there is a slight possibility that few cases of intussusception might have been admitted with a diagnosis for some other condition at the time of presentation and hence missed during our review. Second, the number of deaths at NICH during three years period was unexpectedly very low. We examined the rate of surgical management and intestinal resection for intussusception and believe that the true number of intussusception-associated mortality would be higher than the existing numbers. We have initiated prospective surveillance of intussusception among children <2 years of age at both the sentinel sites from July 2015 onwards using the same level 1 Brighton Collaboration case definition and eligibility criteria. This prospective surveillance identified 10 deaths in intussusception cases at NICH in the first year of enrolment, supporting our point that the deaths reported in this paper might be an underestimation of the actual mortality rate (unpublished data). Finally, the unavailability of an accurate population estimate for the catchment areas for either of the hospitals did not allow for intussusception hospitalization incidence rate calculations. Despite these limitations, this is the first study reporting intussusception burden from the two large tertiary care hospitals from Pakistan. Also, the study used a standard case definition for the identification of only confirmed cases of intussusception avoiding any potential misclassification.
5. Conclusion
This study provides important data on the baseline epidemiology of intussusception that will inform post-vaccine introduction adverse event monitoring related to intussusception in Pakistan.
Footnotes
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention (CDC).
References
- 1.Parashar UD, Holman RC, Cummings KC, et al. Trends in intussusception-associated hospitalizations and deaths among US infants. Pediatrics. 2000;106:1413–21. doi: 10.1542/peds.106.6.1413. [DOI] [PubMed] [Google Scholar]
- 2.Nakagomi T, Takahashi Y, Arisawa K, Nakagomi O. A high incidence of intussusception in Japan as studied in a sentinel hospital over a 25-year period (1978–2002) Epidemiol Infect J. 2006;134:57–61. doi: 10.1017/S0950268805004644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giak CL, Singh HS, Nallusamy R, Leong TY, Ng TL, Bock HL. Epidemiology of intussusception in Malaysia: a three-year review. [PubMed] [Google Scholar]
- 4.Patel MM, Clark AD, Sanderson CF, Tate J, Parashar UD. Removing the age restrictions for rotavirus vaccination: a benefit-risk modeling analysis. PLoS Med. 2012;9(10):e1001330. doi: 10.1371/journal.pmed.1001330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Takeuchi K, Tsuzuki Y, Ando T, Sekihara M, Hara T, Kori T, et al. The diagnosis and treatment of adult intussusceptions. J Clin Gastrenterol. 2003;36:18–21. doi: 10.1097/00004836-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Begos DS, Sandor A, Modlin IM. The diagnosis and management of adult intussusceptions. Am J Surg. 1997;173:88–94. doi: 10.1016/S0002-9610(96)00419-9. Comment Am J Surg 177 1999 442. [DOI] [PubMed] [Google Scholar]
- 7.Bines JE, Liem NT, Justice FA, et al. Intussusception Study Group. Risk factors for intussusception in infants in Vietnam and Australia: adenovirus implicated, but not rotavirus. J Pediatr. 2006;149:452–60. doi: 10.1016/j.jpeds.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 8.Bahl R, Saxena M, Bhandari N, et al. Delhi Intussusception Study Hospital Group. Population-based incidence of intussusception and a case-control study to examine the association of intussusception with natural rotavirus infection among Indian children. J Infect Dis. 2009;200(suppl 1):S277–81. doi: 10.1086/605045. [DOI] [PubMed] [Google Scholar]
- 9.Buttery JP, Danchin MH, Lee KJ, Carlin JB, McIntyre PB, Elliott EJ, et al. Intussusception following rotavirus vaccine administration: post-marketing surveillance in the National Immunization Program in Australia. Vaccine. 2011;29(16):3061–6. doi: 10.1016/j.vaccine.2011.01.088. [DOI] [PubMed] [Google Scholar]
- 10.Patel MM, Lopez-Collada VR, Bulhoes MM, De Oliveira LH, Bautista Marquez A, Flannery B, et al. New Engl J Med. 2011;364(24):2283–92. doi: 10.1056/NEJMoa1012952. Epub 2011/06/17.eng.. [DOI] [PubMed] [Google Scholar]
- 11.Weintraub ES, Baggs J, Duffy J, Vellozzi C, Belongia EA, Irving S, et al. Risk of intussusception after monovalent rotavirus vaccination. New Engl J Med. 2014;370(6):513–9. doi: 10.1056/NEJMoa1311738. [DOI] [PubMed] [Google Scholar]
- 12.Yih WK, Lieu TA, Kulldorff M, Martin D, McMahill-Walraven CN, Platt R, et al. Intussusception risk after rotavirus vaccination in U.S. infants. New Engl J Med. 2014;370(6):503–12. doi: 10.1056/NEJMoa1303164. [DOI] [PubMed] [Google Scholar]
- 13.Ngendahayo E, Bonane A, Ntakiyiruta G, Munyanshongore A, Muganga N, Bikoroti J, Mwenda JM, Tate JE, Ngabo F. Preparing for safety monitoring after rotavirus vaccine implementation: a retrospective review of intussusception cases among children at a large teaching hospital in Rwanda, 2009–2012. Pediat Infect Dis J. 2014;1(33):S99–S103. doi: 10.1097/INF.0000000000000093. [DOI] [PubMed] [Google Scholar]
- 14.Quadri F, Nasrin D, Khan A, Bokhari T, Tikmani SS, Nisar MI, Bhatti Z, Kotloff K, Levine MM, Zaidi AK. Health care use patterns for diarrhea in children in low-income periurban communities of Karachi, Pakistan. Am J Trop Med Hygiene. 2013;89(1 Suppl):49–55. doi: 10.4269/ajtmh.12-0757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bines JE, Liem NT, Justice F, Son TN, Carlin JB, de Campo M, et al. Validation of clinical case definition of acute intussusception in infants in Viet Nam and Australia. Bull World Health Organ. 2006;84(7):569–75. doi: 10.2471/blt.05.025445. Epub 2006/08/01.Eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tate JE, Simonsen L, Viboud C, et al. Trends in intussusception hopsitalization among US infants 1993–2004: implications for monitoring the safety of new rotavirus vaccination program. Pediatrics. 2008;121:e1125–32. doi: 10.1542/peds.2007-1590. http://dx.doi.org/10.1542/peds.2007-1590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jiang J, Jiang B, Parashar U, Nguyen T, Bines J, Patel MM. Childhod Intussusception: a literature review. Plos One. 2013;8(7):e68482. doi: 10.1371/journal.pone.0068482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zaman K, Breiman RF, Yunas Md, et al. Intussusception surveillance in rural demographic surveillance area in Bangladesh. J Infect Dis. 2009;200:S271–6. doi: 10.1086/605047. [DOI] [PubMed] [Google Scholar]
- 19.Tran LAT, Yoshida LM, Nakagomi T, et al. A high incidence of intussusception revealed by a retrospective hospital-based study in Nha Trang, Vietnam between 2009 and 2011. Trop Med Health. 2013;41(3):121–7. doi: 10.2149/tmh.2013-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rotavirus vaccines WHO position paper-January 2013. Wkly Epidemiol Rec. 2013;88:49–64. [PubMed] [Google Scholar]
- 21.Trang NV, Nguyen NTL, Dao HT, et al. Incidence and epidemiology of intussusception among infants in Ho Chi Minh City Vietnam. J Pediatr. 2013 doi: 10.1016/j.jpeds.2013.10.006. http://dx.doi.org/10.1016/j.jpeds.2013.10.006 [DOI] [PubMed]
- 22.Centers for Disease control and prevention. Vaccination. 2016 available from < https://www.cdc.gov/rotavirus/vaccination.html>.