Abstract
Objective
To describe distressed and underprepared family caregiver’s use of and interest in formal support services (e.g., professional counseling, education, organizational assistance).
Methods
Cross-sectional mail survey conducted in communities of eight cancer centers in Tennessee, Alabama, and Florida (response rate: 42%). Family caregivers of Medicare beneficiaries with pancreatic, lung, brain, ovarian, head and neck, hematologic, and stage IV cancers reported support service use and completed validated measures of depression, anxiety, burden, preparedness, and health.
Results
Caregivers (n=294) were on average age 65 years and mostly female (73%), white (91%), and care recipients’ spouse/partner (60%); patients averaged 75 years, were majority male (54%) with lung cancer (39%). Thirty-two percent of caregivers reported accessing services while 28% were “mostly or “extremely” interested. Thirty-five percent of caregivers with high depressive symptoms (n=122), 33% with high anxiety symptoms (n=100) and 25% of those in the lowest quartile of preparedness (n=77) accessed services. Thirty-eight percent of those with high depressive symptoms, 47% with high anxiety symptoms, and 36% in the lowest quartile of preparedness were “mostly or “extremely” interested in receiving services. Being interested in support services was significantly associated with being a minority, shorter durations of caregiving, and with higher stress burden.
Conclusions
A large proportion of family caregivers, including those experiencing depression and anxiety symptoms and who were underprepared, are not using formal support services but have a strong interest in services. Strategies to increase service use may include targeting distressed caregivers early in their caregiving experience.
Keywords: cancer, family caregiver, support services, palliative care
Introduction
There are 2.8 million family members and friends serving as caregivers to adult persons with cancer in the US.1 Many experience significant stress2 in this role and might benefit from formal support services, such as professional or peer counseling, support groups, training workshops, and respite care. There is recent emphasis on the role and importance of family caregiving in serious illness, demonstrated by a landmark National Academies of Medicine report on family caregiving;3 concurrently, formal support for caregiving has become more common. National organizations, including the National Alliance for Caregiving,4 the Caregiver Action Network,5 and the American Association of Retired Persons,6 have made caregiving support a central focus of their mission. These organizations lobby at state and federal levels for caregiving policy and legislation (e.g., RAISE Family Caregivers Act) and facilitate linkages to state and local entities that offer education and counseling services to family caregivers. Many hospitals, hospices, Area Agencies on Aging, and Geriatric Education Centers, offer some form of educational or counseling support to family caregivers.3
In the few studies of support service use by cancer family caregivers, overall use is low. For example, rates of mental health service use among distressed caregivers7 and caregivers with diagnosable psychiatric disorders8 are reported as ~25%. This low use of services is striking given reported rates of depressive symptoms in the cancer caregiving population ranging from 16–32% and anxiety symptoms from 40–50%.9–11 Studies examining a range of formal support services (e.g., education, counseling, organizational assistance) in high-need cancer caregiver populations are lacking including whether or not people are interested in such services. Hence, to address this gap and begin developing interventions that are effectively marketed to and support cancer family caregivers, we assessed a high need caregiver population of Medicare beneficiaries with cancers known to be associated with high morbidity and mortality. Our aims were as follows: 1) describe rates of formal support service use and interest, including among those family caregivers who are distressed (surpassing clinical cut-offs for depression and anxiety symptoms) and underprepared; 2) describe rates and identify correlates of support service use; and 3) describe rates and identify correlates of support service interest. Our study was guided by the Andersen Model of Access,12 a commonly used conceptual model of factors affecting healthcare service access and use.7,13 These factors fall under three domains: 1) predisposing factors (e.g., age, gender, race, social relationships); 2) enabling factors (e.g., income, health insurance); and 3) need factors (e.g., poor physical health, psychological distress). These predisposing, enabling, and need factors were assessed as potential correlates to use of and interest in support services as has been similarly done in prior studies of cancer caregiving.7,14
Methods
Data for this analysis were collected as part of a cross-sectional mail survey study10 to ascertain the health and self-care of family caregivers of community-dwelling Medicare beneficiaries with cancer who were participating in a Centers for Medicaid and Medicare Innovation (CMMI) demonstration project to implement a lay healthcare navigator program (Patient Care Connect), described elsewhere.15 Institutional review board approval was obtained from all participating cancer centers (Protocol #X141103004). Consent was implied through a family caregiver’s voluntary completion and return of the survey. All participants received $10 for survey completion.
Participants and Procedures
Patients of potential caregiver participants were identified by a drop-down, codified field in the Patient Care Connect medical record system that designated a patient’s cancer as “high-risk” or “low-risk”. The “high-risk” category was selected in the medical record if patients had cancers defined by a CMMI demonstration project expert cancer clinician panel to have had historically high morbidity, mortality, distress, and healthcare utilization rates. These “high-risk” cancer types included pancreatic, lung, brain, ovarian, head and neck, hematologic, and any stage IV cancers. All “high-risk” patients served by eight participating cancer centers located in Alabama, Tennessee, and Florida were sent surveys between March 2015 and July 2015. Further details of the survey administration and data collection are described elsewhere.10 In brief, a modified Dillman survey approach16 was employed that consisted of a series of personalized mailings, including repeated mailings of the survey and measures, to encourage participation and survey completion. Mailings were addressed to patients but asked that a “family member or friend who knows you well and who helps you the most with your medical care” participate and complete the survey. Mailings stipulated that these should be unpaid family members or friends and that they did not have to live in the same household.
Measures
All measures below were self-reported by family caregiver participants in the survey.
Dependent variable: formal support service use and interest
Consistent with questions used in prior research,17 caregiver participants were asked three yes/no questions about whether or not they had received specific types of formal support services including “therapy or counseling,” “training and education,” and “assistance from national, state, or local organizations” at any time due to their caregiving role. These terms were used based on study-team clinical expertise with the family caregiver population and piloted with 5 older adult lay persons. If participants responded ‘no’ to any one of these questions, the survey directed them to respond to a follow-up question asking their level of interest in those particular services. The response options were: “Not at all interested,” “Mostly not interested,” “Neutral,” “Mostly interested,” and “Extremely interested.”
Independent variables
Predisposing factors
Variables included the caregiver’s and patient’s ages and genders, the patient’s cancer type, the caregiver’s race, marital status, employment status, the caregiver-patient relationship, and the number of months that the participant had been in the caregiving role.
Enabling factors
Variables included total household income, rural/urban residence, and home internet access (yes/no). Perceived difficulty for the caregiver in paying for their own medical care was assessed by the single item: “How hard is it to pay for your medical care?” Response options included “Very hard,” “Hard,” “Somewhat hard,” “Not very hard,” and “Don’t know.”
Need factors
Need variables included caregivers’ anxiety and depressive symptoms, caregivers’ physical health, caregiver burden, caregiver preparedness, and patient health. Anxiety and depressive symptoms were measured using the 14-item Hospital Anxiety and Depression Scale (HADS).18 This scale contains 7 items each for symptoms of depression and anxiety over the past 7 days. Subscale scores range from 0–21 with scores ≥8 indicating abnormally high symptoms. Caregivers’ physical health was measured using the physical health subscale of the SF-12 Health Survey Questionnaire (Version 2), with higher scores indicating better physical health over the past month (score range: 0–100).19 Caregiver burden was measured using the 14-item Montgomery-Borgatta Caregiver Burden Scale,20 which includes three subscales: objective (i.e., interference with the caregiver’s personal time and daily routine) (score range: 6–30), demand (i.e., perception that patients are being overly demanding of caregivers) (score range: 4–20), and stress burden (i.e., emotional impact from caregiving on caregiver’s mood and relationships) (score range: 4–20). Higher scores represent higher burden. Caregiver preparedness was measured using the 8-item Preparedness for Caregiving Scale (PCS).21 Items address confidence in providing emotional support, physical care, and care coordination. Higher scores indicate higher perceived preparedness (score range 0–4). Patient health was assessed with the single item taken and adapted from the SF-12, “In general, would you say your Care Recipient’s health is…” with 5 response options ranging from “Excellent” to “Poor.”
Statistical Analysis
Caregivers whose depression and anxiety scores were above the HADS cutoff for clinically high symptoms were considered in distress. Caregivers whose PCS scores were in the bottom quartile were considered underprepared as this cut off was found in our prior analysis to have theoretically valid associations (e.g., high depression and anxiety symptoms).10 Frequencies and percentages were tabulated for caregivers in these subsamples and in the overall sample who endorsed having received at least one of the formal support services (i.e., “therapy or counseling,” “training and education,” and/or “assistance from national, state, or local organizations”) and who were “mostly” or “strongly” interested in receiving at least one of these services. Of note, it was possible in this analysis for caregivers to both endorse using one service (e.g., “training and education”) and yet desiring another (e.g., “therapy or counseling”). Associations between predisposing, enabling, and need factors and the non-receipt of support services and whether the caregiver was “mostly” or “strongly” interested in receiving support services was explored using unadjusted bivariate logistic regression analyses. To pinpoint the set of predisposing, enabling, and need factors that captured the bulk of the associations with use of (Aim 2) and interest in (Aim 3) support services, we fit multivariate logistic models with factors selected in a stepwise manner via the Bayesian Information Criterion.22 To provide an assessment of generalizability of the resulting models, two overall fit statistics, Efron’s pseudo-R Squared and the C statistic (i.e., the area under the Receiver Operating Characteristic curve) were corrected for overfitting using a Bootstrap approach (200 resamples). The estimates of overfitting adjusted pseudo-R Squared and C statistic were corroborated with those from a Random Forest approach (2000 classification trees) computed with the Out-of-Bag predicted values (a type of cross-validated model-predicted values).23 The analyses were conducted using IBM SPSS Statistics 23 and R 3.3.2 (R Foundation for Statistical Computing, Vienna Austria) packages.
Results
A total of 911 surveys were mailed to patients. After accounting for surveys that would not have had a potential family caregiver response (e.g., patient reports no caregiver, invalid address), there were 695 possible survey responses. Of 695 possible surveys, 294 were completed (response rate=42.3%) (Table 1).
Table 1.
Survey Outcome Summary
| Total surveys mailed | 911 |
| Patient reports no caregiver | 86 |
| Patient not willing | 21 |
| Patient already deceased | 57 |
| Invalid address | 30 |
| Total other (e.g. survey returned blank, patient states does not have advanced cancer) | 22 |
| Total possible survey responses | 695 |
| Surveys completed | 294 |
| Survey non-responders | 401 |
|
| |
| Response rate | 42.3% |
On average, caregivers were 65.5 years old and mostly female, white, and married, with most caregivers being the spouse or partner of the patient and had been providing care for an average of 33.5 months (Table 2). The largest proportion had total household incomes between $50,000–$100,000 (36.4%) followed next by those making <$30,000 (29.3%). Most caregiver participants were Protestant (76.2%), retired (54.4%), and self-defined urban/suburban dwelling (53.1%). Large proportions of the caregiver sample also evidenced depression (41.5%) and anxiety symptoms (34.0%). Care recipients were on average 75.3 years old and mostly male with lung (38.8%) and head and neck cancer (21.1%). Forty-three percent were in “poor” or “fair” health.
Table 2.
Family caregiver (n=294) characteristics
| Characteristic | No. | % |
|---|---|---|
| Age, Mean (SD) | 65.5 (12.7) | |
|
| ||
| Female gender | 214 | 72.8 |
|
| ||
| Race | ||
| White | 268 | 91.2 |
| African-American/Black | 23 | 7.8 |
| Other | 3 | 1.0 |
|
| ||
| Marital Status | ||
| Married or living with partner | 243 | 82.6 |
| Divorced or separated | 21 | 7.1 |
| Single | 20 | 6.8 |
| Widowed | 10 | 3.4 |
|
| ||
| Socioeconomic Status (Total Household Income) | ||
| <$30,000 | 86 | 29.3 |
| $30,000–$49,999 | 72 | 24.5 |
| $50,000–$100,000 | 107 | 36.4 |
| >$100,000 | 29 | 9.9 |
|
| ||
| Religion | ||
| Protestant | 224 | 76.2 |
| Catholic | 25 | 8.5 |
| No religious affiliation | 19 | 6.5 |
| Other | 26 | 8.8 |
|
| ||
| Employment Status | ||
| Employed full or part time | 67 | 22.8 |
| Retired | 160 | 54.4 |
| Unemployed | 27 | 9.2 |
| Other | 40 | 13.6 |
|
| ||
| Residence type | ||
| Urban/suburban | 156 | 53.1 |
| Rural | 138 | 46.9 |
|
| ||
| Relationship to patient (This person is my…) | ||
| Spouse/partner | 177 | 60.2 |
| Parent | 47 | 16.0 |
| Child | 31 | 10.5 |
| Other family member | 16 | 5.4 |
| Sibling | 9 | 3.1 |
| Friend | 9 | 3.1 |
|
| ||
| Months as a caregiver, Mean (SD) | 33.5 (40.3) | |
|
| ||
| Care recipient age, Mean (SD) | 75.3 (6.6) | |
|
| ||
| Care recipient male gender | 160 | 54.4 |
|
| ||
| Care recipient cancer diagnosis | ||
| Lung | 114 | 38.8 |
| Head and neck | 62 | 21.1 |
| Leukemia/Non-Hodgkin lymphoma | 30 | 10.2 |
| Ovarian | 28 | 9.5 |
| Pancreatic | 13 | 4.4 |
| Bladder and/or Kidney | 11 | 3.7 |
| Other | 36 | 12.6 |
|
| ||
| Proportion of caregivers with… | ||
| High depressive symptoms | 122 | 41.5 |
| High anxiety symptoms | 100 | 34.0 |
|
| ||
| My care recipient’s health is… | ||
| Poor or fair | 127 | 43 |
| Good | 116 | 40 |
| Very good or excellent | 51 | 17 |
Comparisons of responders and nonresponders revealed that fewer caregivers of minority (p<.01) and unmarried care recipients (p<.01) responded to the survey. There were no differences by age, gender, and cancer-type.
Formal Support Service Use and Interest Due to the Caregiving Role (Aim 1)
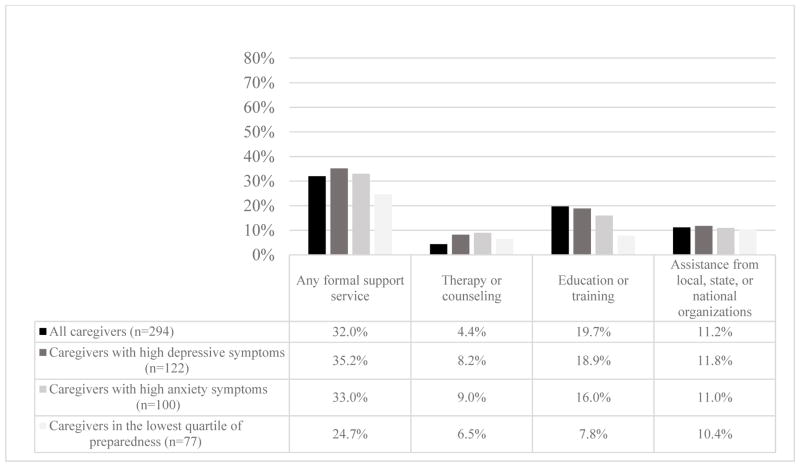
Of 294 caregivers, 32% (n=94) used formal support services, 4.4% used therapy or counseling, 19.7% received education and training, and 11.2% received assistance from local, state, or national organizations (Figure 1). Thirty-five percent (n=122) of caregivers with high depressive symptoms, 33% (n=100) with high anxiety symptoms and 25% (n=77) of those in the lowest quartile of preparedness used services. Caregivers with high depression and anxiety symptoms appeared to have similar utilization rates of therapy and counseling services (8.2% vs. 9.0%); caregivers in the lowest quartile of preparedness showed lower rates of use of education and training services (7.8%).
Figure 1.
Percentage of Caregivers Reporting Use of Formal Support Services
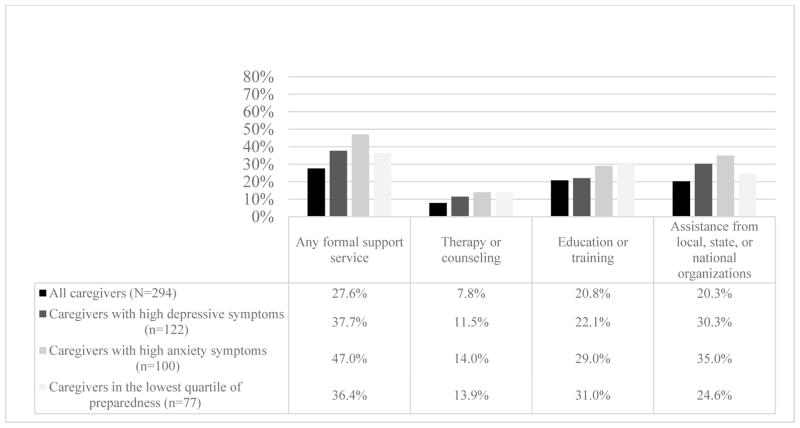
Nearly 28% (n=82) of all caregivers reported interest in some type of support service with the highest percentage of interest shown for education and training services (20.8%) and assistance from local, state, or national organizations (Figure 2). Over a third (37.7%) of individuals with high depressive symptoms and just under half (47.0%) with anxiety symptoms were interested in some type of support services, with the most interest shown for assistance for local, state, or national organization assistance; these percentages were notably higher than reported in the entire sample. Thirty-six percent (n=28) of those in the lowest quartile of preparedness were “mostly” or “extremely” interested in support services.
Figure 2.
Percentage of Family Caregivers “Mostly” or “Extremely” Interested in Formal Support Services
When considering the total denominator of those who used a service (n=94) combined with those interested in a service (that they were not using) (n=82), approximately half (47%) of caregivers with an interest in a support service were not using it ( or 47%).
Use of Formal Support Services (Aim 2)
Bivariate logistic regression analyses of predisposing, enabling, and need factors and use of formal support service (Supplemental Table 1) revealed that support service use was significantly associated with being unmarried (OR=1.99, p<.05), being a non-spouse of the care recipient (OR=2.03, p<.01), having lower levels of objective burden (OR=.69, p<.01), and being more prepared as a caregiver (OR=1.54, p<.01).
The multivariate approach identified being a non-spouse of the care recipient (b=.90, OR=2.52), having lower levels of objective burden (b=.39, OR=.67), and being more prepared as a caregiver (b=.45, OR=1.57) as salient predictors of support service use. This multivariate model fit fairly well with our data (Efron’s pseudo-R Squared [fitted model]=0.12, C Statistic [fitted model]: .70); however, the overfitting adjusted results indicate uncertainty of its generalizability to other samples (Efron’s pseudo-R Squared [overfitting adjusted]=.04, C Statistic [overfitting adjusted]: .64). These fit results were corroborated by a random forest ensemble (Efron’s pseudo-R Squared =.02, C Statistic =.59).
Interest in Formal Support Services (Aim 3)
Bivariate logistic regression analyses (Supplemental Table 2) revealed that having a strong interest in services was significantly associated with minority status (OR=4.95, p<.01), shorter durations of caregiving (OR=.38, p<.01), higher depression (OR=1.77, p<.01) and anxiety symptoms (OR=1.99, p<.001), being physically healthier (OR=2.16, p<.05), being less objectively burdened (OR=.66, p<.05), experiencing more demand (OR=1.56, p<.05) and stress burden (OR=2.75, p<.001), being less prepared for caregiving (OR=.71, p<.05), and perceiving the care recipient to be in worse health (OR=.60, p<.01).
In the multivariate analysis, being a minority (b=2.22, OR=9.20), having shorter durations of caregiving (b=1.05, OR=.35), and having a high degree of stress burden (b=1.17, OR=3.23) were selected as salient predictors of being “Extremely” or “Mostly” interested in receiving support services. This multivariate model fit well with our sample of data (Efron’s pseudo-R Squared [fitted model].25, C Statistic [fitted model]: .80); after overfitting adjustment, the results suggested fair generalizability to other samples (Efron’s pseudo-R Squared [overfitting adjusted]=.11, C Statistic [overfitting adjusted]: .74). These fit results were corroborated by a random forest ensemble (Efron’s pseudo-R Squared=.11, C Statistic: .71).
Discussion
This is the first study to describe use and interest in formal support services among caregivers of older adults with high-burden cancers in the Southeastern U.S.. When considering all those caregivers who used a service (n=94) in combination with those who had interest in service (but were not using it) (n=82), nearly half of caregivers were not using a formal support service that they were interested in. Similar trends were observed among those with high depression and anxiety symptoms and who were underprepared, all of whom would seemingly benefit greatly from such services. These results reinforce and extend other cancer caregiving research,1,7,8,17,24,25 documenting a wide gap between caregiver support service use and interest.
Support service use was associated with being a nonspousal caregiver, feeling prepared for the role and having a low degree of feeling that one’s life is being infringed and disrupted (objective burden). While statements of directionality are speculative in this type of cross-sectional study, the latter two associations raise the question of whether participation in support services leads to better role preparation and lessens the perception that caregiving tasks interfere with one’s day-to-day routine. It is possible that highly-prepared caregivers may be more efficient at accomplishing and coordinating tasks such that it takes less time from their day resulting in lower burden. Alternatively, it may also be the case that those caregivers with less objective burden may simply have more time to devote to accessing support services. Longitudinal observations would ultimately be needed to fully substantiate the nature of the relationship between support service utilization and caregiver preparedness.
Though research is sparse, there are several potential explanations for the association between nonspousal caregiving and support service use. Spousal caregivers may perceive the caregiving role as an expected part of the marital relationship.26 Many of the nonmedical tasks may have already been part of the normal give-and-take in the relationship (e.g., cooking, household chores), thus potentially resulting in less distress in assuming the caregiving role, which may result in lower interest for support. Conversely, nonspousal caregivers, such as adult children, may have more unmet needs as a result of taking on unanticipated medical and nonmedical tasks while also juggling a full-time job and young children,27 contributing to their interest in and use of support.
Factors strongly associated with interest in support services included being a minority, shorter durations of caregiving, and experiencing higher stress burden. Because our minority sample size was small, we are cautious in interpreting this result, even though it is consistent with the literature that minority caregivers demonstrate higher levels of burden and unmet needs compared to Whites.28,29 Caregiver distress and the need for knowledge about cancer and treatments and care coordination demands has been shown to be highest at diagnosis when a family member starts the stressful process of rearranging daily life to accommodate the caregiving role;30–32 hence, it is understandable that shorter durations of caregiving and high stress burden were associated with interest in support services. Additionally, the fact that this study’s patient population had cancers that have historically had high rates of morbidity, mortality, distress, and healthcare utilization rates may have exacerbated the pressing urgency for support. Interestingly, caregivers with longer durations in their role were not more likely to have used support services. It could be the case that over time family caregivers in this sample were having their needs for support services met by lay patient navigators who were assigned to all patients as part of the CMMI Patient Care Connect project. The point of diagnosis of such cancers when patient navigation is initiated might present the ripest opportunity to screen and identify caregivers who might be most interested in and be most likely to benefit from formal support.33 As the availability of palliative and supportive care providers are expected to decline in the coming decades relative to the growing need for services,34 it is critical that screening processes are integrated into the routine clinical care of patients and sensitive enough to identify caregivers most in need of formal support. Interventions should be developed that target increased support service utilization by family caregivers, especially for those who are distressed and underprepared.
Although approximately one-third of caregivers with high depression symptoms and who were underprepared and a nearly a half of those with anxiety symptoms reported that they were interested in receiving support services, approximately three-quarters to a half did not express interest. This discrepancy between apparent need and interest in services was especially pronounced relative to receipt of “counseling and therapy.” This is likely in part due to several issues including a well-documented stigma against mental health services,35 including among cancer family caregivers.36 Second, caregivers may feel guilty about focusing on their own needs believing that it is at the expense of patients’ needs.37 Third, distressed caregivers may be unaware or unconcerned that their distress is high8 or may believe based on cultural upbringing that mental and emotional concerns are to be self-managed without assistance from others.36 Future research should explore this relationship between caregiver distress awareness and health seeking behaviors.
Limitations
This study has several limitations. First, our response rate of 42.3% is lower than the “gold standard” of 60% espoused by Dillman,16 hence this study is at greater risk of selection bias, as indicated by the differential response rates by family caregivers of Black/African-American and unmarried patients. Response rates may have been impacted by the request for participants to complete a university-mandated W-9 form that asked for sensitive information (e.g., social security number) in order to receive the $10 incentive. Also, some patients may not have had a family caregiver and simply not returned the survey for that reason.
Second, we are uncertain how respondents interpreted the terms for formal support services, including “therapy and counseling,” “training and education,” and “assistance of any kind from national, state, or local organizations.” No further detail was stated in the survey about what these terms meant or what specific services they could have included. Indeed, percentages ranging between 20–30% of highly distressed and underprepared caregivers endorsed the “neutral” response option regarding their interest in the formal support services. This could indicate that these caregivers might have been interested in these services if they had more information about them.
Third, our survey prompted participants to respond about their use and interest in formal support services “related to their caregiving role” and thus might not have captured their use of or interest in these services for reasons unrelated to their caregiving role. Future research should account for use of and interest in formal support services both related and unrelated to the caregiving role.
Fourth, we did not account for differences among the 8 cancer centers and their communities in the services that may have been available for family caregivers. Because we were focused on individual-level factors consistent with the Andersen Model of Access, we did not include any provider or site characteristics in the analysis. Furthermore, our sample size was insufficient to add additional site variables to the variables already examined in these analyses. Future studies examining support services for family caregivers across different sites would be strengthened by exploring or controlling for site-level characteristics.
Finally, this sample of caregivers was taken from a Medicare population of patients in the Southeastern U.S. that was receiving lay patient navigation services. Also, while we used the best indicator available in the CMMI medical to identify high-burden cancers, the cancer staging and curability of our caregiver sample’s patients is unknown. This consideration is important when evaluating the generalizability of the findings to other populations.
Implications
In conclusion, our results warrant several implications for clinicians and future research. This 3-state survey of 294 family caregivers of high-burden cancer patients found that around half of distressed and underprepared caregivers had a strong interest in formal support services, yet only a small proportion accessed these services. Based on our findings, strategies to increase service use should be designed to target caregivers early in their caregiving experience and who report high distress. Part of the challenge going forward will be the development of marketing, outreach, and awareness interventions that compel caregivers to avail themselves of these support services, many of which already exist. The coming decades will see marked increases in the number of older persons living with serious cancers in the community;38,39 it is thus imperative that support be given to families who are increasingly performing as the frontline healthcare workforce.
Supplementary Material
Acknowledgments
This study was funded by a UAB Center for Palliative and Supportive Care PREP Grant (PI: Dionne-Odom) and was conducted under the auspices of a Centers for Medicare and Medicaid Services Health Care Innovation Challenge demonstration project (PI: Partridge). Over the course of this study, Dr. Dionne-Odom has been supported by the NIH/NINR (1K99NR015903), the National Cancer Institute (2R25CA047888-24), the National Palliative Care Research Center, and the American Cancer Society (RSG PCSM – 124668). Dr. Demark-Wahnefried receives support from the NIH/NCI UAB Cancer Center Core Grant (5P30CA13148). Dr. Rocque is funded by a Frommeyer Fellowship in Investigative Medicine. Dr. Bakitas is funded by the NIH/NINR (R01NR013665) and the American Cancer Society (RSG PCSM-124668). The authors would like to thank Ms. Julie Schach, Program Manager and staff of the UAB Recruitment and Retention Shared Facility for administration and oversight of the survey study. The authors would also like to acknowledge all participating Patient Care Connect medical centers including: the UAB Comprehensive Cancer Center (Birmingham, AL), Marshall Medical Center (Albertville, AL), Memorial Hospital (Chattanooga, TN), Fort Walton Beach Medical Center (Fort Walton Beach, FL), Gulf Coast Regional Medical Center (Panama City, FL), Southeast Alabama Medical Center (Dothan, AL), Northeast Alabama Regional Medical Center (Anniston, AL), and Mitchell Cancer Institute (Mobile, AL).
Footnotes
Conflict of Interest Disclosure
The authors have no relevant conflict of interests to disclose.
References
- 1.National Alliance for Caregiving. Cancer Caregiving in the US: An Intense, Episodic, and Challenging Care Experience. Bethesda, MD: National Alliance for Caregiving; 2016. [Google Scholar]
- 2.Goren A, Gilloteau I, Lees M, DaCosta Dibonaventura M. Quantifying the burden of informal caregiving for patients with cancer in Europe. Support Care Cancer. 2014;22(6):1637–1646. doi: 10.1007/s00520-014-2122-6. [DOI] [PubMed] [Google Scholar]
- 3.National Academies of Science, Engineering, and Medicine. Families Caring for an Aging America. Washington, DC: The National Academies Press; 2016. [PubMed] [Google Scholar]
- 4.National Alliance for Caregiving. [Accessed October 20, 2017];About the Alliance. 2017 http://www.caregiving.org/about/about-the-alliance/
- 5.Caregiver Action Network. [Accessed October 31, 2017];About Caregiver Action Network. 2017 http://caregiveraction.org/about.
- 6.AARP. [Accessed October 31, 2017];Home and Family Caregiving. 2017 https://www.aarp.org/home-family/caregiving/
- 7.Mosher CE, Champion VL, Hanna N, et al. Support service use and interest in support services among distressed family caregivers of lung cancer patients. Psychooncology. 2013;22(7):1549–1556. doi: 10.1002/pon.3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vanderwerker LC, Laff RE, Kadan-Lottick NS, McColl S, Prigerson HG. Psychiatric disorders and mental health service use among caregivers of advanced cancer patients. J Clin Oncol. 2005;23(28):6899–6907. doi: 10.1200/JCO.2005.01.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nielsen MK, Neergaard MA, Jensen AB, Bro F, Guldin MB. Psychological distress, health, and socio-economic factors in caregivers of terminally ill patients: a nationwide population-based cohort study. Support Care Cancer. 2016;24(7):3057–3067. doi: 10.1007/s00520-016-3120-7. [DOI] [PubMed] [Google Scholar]
- 10.Dionne-Odom JN, Demark-Wahnefried W, Taylor RA, et al. The self-care practices of family caregivers of persons with poor prognosis cancer: differences by varying levels of caregiver well-being and preparedness. Support Care Cancer. 2017 doi: 10.1007/s00520-017-3650-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hudson PL, Thomas K, Trauer T, Remedios C, Clarke D. Psychological and social profile of family caregivers on commencement of palliative care. J Pain Symptom Manage. 2011;41(3):522–534. doi: 10.1016/j.jpainsymman.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 12.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 13.Ricketts TC, Goldsmith LJ. Access in health services research: the battle of the frameworks. Nurs Outlook. 2005;53(6):274–280. doi: 10.1016/j.outlook.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 14.Martindale-Adams J, Nichols LO, Zuber J, Burns R, Graney MJ. Dementia Caregivers’ Use of Services for Themselves. Gerontologist. 2016;56(6):1053–1061. doi: 10.1093/geront/gnv121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rocque GB, Partridge EE, Pisu M, et al. The Patient Care Connect Program: Transforming Health Care Through Lay Navigation. J Oncol Pract. 2016 doi: 10.1200/JOP.2015.008896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dillman D, Smyth J, Christian L. Internet, Mail, and Mixed-Mode Surveys: The Tailored Design Method. 3. Hoboken, NJ: John Wiley & Sons, Inc; 2009. [Google Scholar]
- 17.Applebaum AJ, Farran CJ, Marziliano AM, Pasternak AR, Breitbart W. Preliminary study of themes of meaning and psychosocial service use among informal cancer caregivers. Palliat Support Care. 2014;12(2):139–148. doi: 10.1017/S1478951513000084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: An updated literature review. Journal of Psychosomatic Research. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 19.Cheak-Zamora NC, Wyrwich KW, McBride TD. Reliability and validity of the SF-12v2 in the medical expenditure panel survey. Qual Life Res. 2009;18(6):727–735. doi: 10.1007/s11136-009-9483-1. [DOI] [PubMed] [Google Scholar]
- 20.Montgomery R, Gonyea J, Hooyman N. Caregiving and the Experience of Subjective and Objective Burden. Family Relations. 1985;34:19–26. [Google Scholar]
- 21.Archbold PG, Stewart BJ, Greenlick MR, Harvath T. Mutuality and preparedness as predictors of caregiver role strain. Res Nurs Health. 1990;13(6):375–384. doi: 10.1002/nur.4770130605. [DOI] [PubMed] [Google Scholar]
- 22.Efron B, Hastie T. Computer Age Statistical Inference: Algorithms, Evidence and Data Science. New York, NY: Cambridge University Press; 2016. [Google Scholar]
- 23.Harrell F. Regression Modeling Strategies with Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. 2. New York, NY: Springer; 2015. [Google Scholar]
- 24.Merckaert I, Libert Y, Lieutenant F, et al. Desire for formal psychological support among caregivers of patients with cancer: prevalence and implications for screening their needs. Psychooncology. 2013;22(6):1389–1395. doi: 10.1002/pon.3153. [DOI] [PubMed] [Google Scholar]
- 25.Wolff JL, Spillman BC, Freedman VA, Kasper JD. A National Profile of Family and Unpaid Caregivers Who Assist Older Adults With Health Care Activities. JAMA Intern Med. 2016;176(3):372–379. doi: 10.1001/jamainternmed.2015.7664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McLean LM, Jones JM. A review of distress and its management in couples facing end-of-life cancer. Psychooncology. 2007;16(7):603–616. doi: 10.1002/pon.1196. [DOI] [PubMed] [Google Scholar]
- 27.Lambert SD, Harrison JD, Smith E, et al. The unmet needs of partners and caregivers of adults diagnosed with cancer: a systematic review. BMJ Support Palliat Care. 2012;2(3):224–230. doi: 10.1136/bmjspcare-2012-000226. [DOI] [PubMed] [Google Scholar]
- 28.Scharlach AE, Kellam R, Ong N, Baskin A, Goldstein C, Fox PJ. Cultural attitudes and caregiver service use: lessons from focus groups with racially and ethnically diverse family caregivers. J Gerontol Soc Work. 2006;47(1–2):133–156. doi: 10.1300/J083v47n01_09. [DOI] [PubMed] [Google Scholar]
- 29.Martin MY, Sanders S, Griffin JM, et al. Racial variation in the cancer caregiving experience: a multisite study of colorectal and lung cancer caregivers. Cancer Nurs. 2012;35(4):249–256. doi: 10.1097/NCC.0b013e3182330850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hodges LJ, Humphris GM, Macfarlane G. A meta-analytic investigation of the relationship between the psychological distress of cancer patients and their carers. Soc Sci Med. 2005;60(1):1–12. doi: 10.1016/j.socscimed.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 31.Lambert SD, Girgis A, Lecathelinais C, Stacey F. Walking a mile in their shoes: anxiety and depression among partners and caregivers of cancer survivors at 6 and 12 months post-diagnosis. Support Care Cancer. 2013;21(1):75–85. doi: 10.1007/s00520-012-1495-7. [DOI] [PubMed] [Google Scholar]
- 32.Girgis A, Lambert SD, McElduff P, et al. Some things change, some things stay the same: a longitudinal analysis of cancer caregivers’ unmet supportive care needs. Psychooncology. 2013;22(7):1557–1564. doi: 10.1002/pon.3166. [DOI] [PubMed] [Google Scholar]
- 33.Dionne-Odom J, Azuero A, Lyons K, et al. Benefits of immediate versus delayed palliative care to informal family caregivers of persons with advanced cancer: Outcomes from the ENABLE III randomized clinical trial. American Society of Clinical Oncology; Chicago, IL: 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kamal AH, Bull JH, Swetz KM, Wolf SP, Shanafelt TD, Myers ER. Future of the Palliative Care Workforce: Preview to an Impending Crisis. Am J Med. 2017;130(2):113–114. doi: 10.1016/j.amjmed.2016.08.046. [DOI] [PubMed] [Google Scholar]
- 35.Schnyder N, Panczak R, Groth N, Schultze-Lutter F. Association between mental health-related stigma and active help-seeking: systematic review and meta-analysis. Br J Psychiatry. 2017;210(4):261–268. doi: 10.1192/bjp.bp.116.189464. [DOI] [PubMed] [Google Scholar]
- 36.Mosher CE, Given BA, Ostroff JS. Barriers to mental health service use among distressed family caregivers of lung cancer patients. Eur J Cancer Care (Engl) 2015;24(1):50–59. doi: 10.1111/ecc.12203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Palos GR, Hare M. Patients, family caregivers, and patient navigators: a partnership approach. Cancer. 2011;117(15 Suppl):3592–3602. doi: 10.1002/cncr.26263. [DOI] [PubMed] [Google Scholar]
- 38.Kent EE, Malinoff R, Rozjabek HM, et al. Revisiting the Surveillance Epidemiology and End Results Cancer Registry and Medicare Health Outcomes Survey (SEER-MHOS) Linked Data Resource for Patient-Reported Outcomes Research in Older Adults with Cancer. J Am Geriatr Soc. 2016;64(1):186–192. doi: 10.1111/jgs.13888. [DOI] [PubMed] [Google Scholar]
- 39.Miller KD, Siegel RL, Lin CC, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. 2016;66(4):271–289. doi: 10.3322/caac.21349. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.