Abstract
Introduction
Hospital emergency departments (EDs) around the country are being challenged by an ever-increasing volume of patients seeking psychiatric services. This manuscript describes a study performed to identify internal and external factors contributing to repeated psychiatric patient admissions to the hospital main ED.
Methods
Data from ED visits of patients who were admitted to the Parkland Memorial Hospital ED (the community hospital for Dallas County, TX, USA) with a psychiatric complaint more than once within a 30-day period were evaluated (n=202). A 50-item readmission survey was used to collect information on demographic and clinical factors associated with 30-day readmission, as well as to identify quality improvement opportunities by assessing related moderating factors. An analysis of acute readmission visits (occurring within 3 days of previous discharge) was also performed.
Results
Patients readmitted to the ED commonly present with a combination of acute psychiatric symptoms, substance use (especially in the case of acute readmission), and violent or suicidal behavior. The vast majority of cases reviewed found that readmitted patients had difficulties coordinating care outside the ED. A number of moderating factors were identified and targeted for quality improvement including additional support for filling prescriptions, transportation, communication with family and outside providers, drug and alcohol treatment, intensive case management, and housing.
Conclusion
Many of the resources necessary to reduce psychiatric patient visits to hospital EDs are available within the community. There is no formal method of integrating and insuring the continuity of community services that may reduce the demand for psychiatric and related services in the ED. While agreements between community service providers may be challenging and require considerable vigilance to maintain equitable agreements between parties, this route of improving efficiency may be the only available method, given the current and projected patient care needs.
Keywords: chronic mental illness, psychiatric readmission, emergency psychiatry, public mental health
Plain language summary
Over the last 20 years, there has been a steady increase in the number of patients being treated for mental health problems (including alcohol and drug use) in hospital emergency departments (EDs). This article describes a project undertaken at one of the busiest hospitals in the country to better understand the reasons patients keep returning to the ED at the hospital for acute mental health and substance treatment rather than receiving long-term treatment in the community. Records from 202 patients who had been admitted to the ED for a mental health or substance use problem and returned within 30 days were reviewed to find factors that may have been associated with the readmission. The results indicated that, while resources necessary to reduce psychiatric patient visits were often available within the community, patients had difficulties following through with treatment after they leave the ED. Finally, a number of steps to improve patients’ accessibility to care are outlined in the paper.
Introduction
Providing care for patients with mental health conditions is a global concern. In the USA alone, at any given time, a quarter of the population has a diagnosable mental health or substance use disorder, of which 60% are classified as moderate to serious in severity.1–5 By 2020, psychiatric disorders are projected to be the second leading cause of disability in both the years of potential life lost due to premature mortality and the years of productive life lost due to disability (disability adjusted life years).6–9
Changes in the health care infrastructure have resulted in a reduction in available long- and short-term mental health and substance use services. During the last 20 years, there has been a steady increase in the volume of patients seeking mental health services in hospital emergency departments (EDs), to the point that these patients represent the most rapidly growing component of ED treatment.10–14 EDs have become the first line of treatment for many patients seeking mental health services. It is estimated that >40% of patients in the ED have a diagnosable mental health or substance use disorder, and over 5% of all visits are for psychiatric reasons alone.15,16 Psychiatric patient visits to the Parkland Memorial Hospital (PMH) ED have reflected this trend and are currently at an historical high point.
In response to the considerable demand, diverse models of specialized emergency psychiatry services have evolved – ranging from solo consultants in medical EDs to large, comprehensive crisis mental health facilities. PMH relies on a combination of models to serve the psychiatric needs of the community, with a psychiatry emergency department (PED) that operates separately from the medical ED, psychiatric specialists consulting in the ED, and a consult–liaison service to provide support for all service lines in the hospital. Within the catchment area, Dallas County (TX, USA), PMH is the “safety net” public hospital and provides care to all those who present for treatment regardless of their insurance status and ability to pay for services. There are several other specialized facilities equipped to deal with patient in acute psychiatric distress, as well as limited residential psychiatric and drug treatment facilities available within the community. For a variety of reasons, PMH is often the first treatment facility visited by patients, care givers, and authorities, seeking psychiatric evaluation and treatment. While there is community outpatient psychiatric treatment available, some patients choose to visit the PMH ED for concerns that could be more effectively addressed in a nonacute care setting.
The PMH ED has ~15,000 psychiatric patient contacts per month. During the 12-month period, from September 2015 through August 2016, ~12% (1,800) of the psychiatric patient contacts were “readmission” visits, defined as ≥2 mental health–related admissions to the PMH ED (including those related to substance use) occurring within a 30-day period. In addition, the number of psychiatric contacts in the ED is steadily increasing, many of which will likely be avoidable readmission visits that could be managed more cost-effectively and appropriately at a less acute level of care in the community.
The goal of the project was to develop a better understanding of factors contributing to psychiatric patient readmissions in the ED, to identify those areas where improvements may be made, and to develop action plans to address those quality improvement opportunities.
Methods
This manuscript details the result of a continuous quality improvement project designed and developed as a collaborative effort between the University of Texas Southwestern Medical Center (UTSW) and PMH. The project was approved by the UTSW Institutional Review Board and determined to be a performance improvement project, not requiring patient consent for chart review. The patient data used in the study were de-identified and securely stored in an independent database on the UTSW server. The purpose of the project was to provide PMH guidance in optimizing the benefit of patient care provided by gaining a better understanding of clinical, community, and patient issues related to psychiatric readmission visits in the ED. The plan–do–study–act (PDSA) cycle was used as a model to guide the quality improvement process.17 The first steps, as described in this manuscript, are as follows: 1) setting aims by identifying areas for improvement and identifying the target population; 2) measuring changes that may lead to improvement; and 3) identifying the changes mostly likely to result in improvement. The final step, implementing and testing changes, is currently underway and is designed to be an ongoing process of planning, implementing, observing (continued measurement), and adjusting actions based upon the knowledge gained.
Subjects
The study included patients who were admitted to the PMH ED with a psychiatric complaint ≥2 times within a 30-day period from September 2015 to August 2016 (patients who were admitted for a medical condition and later found to have a psychiatric complaint were also included in the sample). Patients who left the hospital against medical advice were not included in the study.
Materials
Based upon the current literature and the clinical experience of a collaborative multidisciplinary team of physicians, psychologists, nurses, social workers, and staff from UTSW and PMH created a chart review survey designed to capture relevant variables related to psychiatric patient readmission.18–30 The Parkland Readmission Survey (PRS) is a 50-item assessment designed to review readmission visits in the ED. The PRS captures demographic information (age, race, gender, ethnicity, employment and housing status, income source, and medical funding source), clinical features related to the readmission visit (medical and/or psychiatric complaint, specific psychiatric complaint and diagnosis from previous and current visit, and the presence/absence of an unresolved medical or psychiatric condition from previous visit), and treatment information (the number of times the patient was seen in any hospital in the last 30 days, the number of days since last admission for a psychiatric condition, and ability to follow medical and psychiatric treatment recommendations). In the final section of the PRS, using a fully anchored 4-point Likert scale (strongly agree, agree, disagree, and strongly disagree), reviewers rated 10 factors that were believed to be associated with the 30-day psychiatric patient readmission visits in the PMH ED. These factors were identified by consensus agreement among members of the multidisciplinary team developing the scale. A copy of the PRS is provided as Supplementary material.
Prior to deploying the PRS, standard assessment procedures were implemented. Specifically, the survey was beta-tested (3 trials over a 3-month period); during that time, the assessment was revised to improve performance. The objective items, such as demographics and clinical features, were revised to include instructions for the specific location of items within the medical record (eg, final diagnosis located in the discharge plan section of the chart). Raters were provided additional instruction in rating the subjective items (eg, rate based on all information contained in the chart, including social work and nursing specific notes). On the final trial, all objective items were in agreement, and there was no discordance between raters found in response to the subjective items (ie, differences in magnitude, but not in valence were present, meaning that differences such as strongly agree vs agree were present, but differences such as agree vs disagree were not found).
Procedures
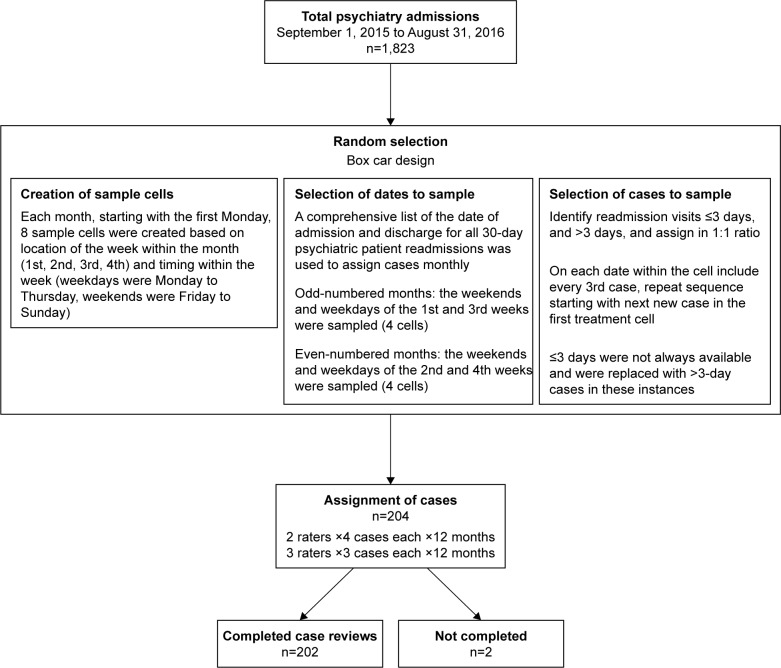
The PRS was put into the Research Electronic Data Capture system for the purpose of data entry and analyzed using the Statistical Package for the Social Sciences (IBM Corporation, Armonk, NY, USA).31,32 After 3 months of beta-testing, the assessment was finalized. The raters were 5 UTSW psychiatrists working at PMH as full-time or part-time providers in the PED who completed the PRS during protected administrative time. The raters were not directly involved in care provided during visits under review (although they may have been involved in care during a different visit). Each month, cases, from the prior month, were randomly selected for inclusion in the study. Figure 1 details the flow of cases from random selection through assignment to reviewer.
Figure 1.
Patient flow.
Note: Admissions to the emergency department of the Parkland Memorial Hospital with a psychiatric complaint ≥2 times within a 30-day period from September 2015 to August 2016.
Analysis
A descriptive analysis provides details regarding the total sample across 3 domains: demographics, treatment factors, and identifiable problems, as well as information regarding the reviewer’s impression of strategies that may help prevent future readmissions. In addition, a more granular secondary analysis was undertaken to identify independent factors that may be associated with acute readmission (≤3 days, ≤72 hours). The aim of the secondary analysis was to determine whether rapid returns to the ED (<3 days) were associated with different clinical and patient factors than the less acute readmissions (4–30 days). In order to obtain an adequate sample of acute readmissions (≤3 days), the sample was stratified at a ratio of 1:1 based upon time from last admission (≤3 days, >3 days). Between-group differences (≤3 day, 4–30 days) were evaluated by using a Yates corrected χ2 analyses for nonparametric variables, and the analysis of variance was used to examine the parametric data (p<0.05). The selection of sample size was pragmatic in that 200 cases provided adequate power for limited clinical, demographic, treatment subgroup analysis and was large enough to be representative of the total population.
Results
Demographics
The sample consisted of 202 patients with 30-day readmission visits and data were collected over a 12-month period from September 2015 to August 2016. The average age of patients with the ED readmission was 40 years, and the patients had 11 years of formal education. The sample was 80% male, was 10% Hispanic, and predominately composed of patients self-identified as African American (45%) or Caucasian (43%). The majority of patients included in the evaluation were homeless (63%) and not employed (87%) with limited (35% received disability benefits) or no source of income (46%). The secondary analysis found no statistically significant differences in demographic factors between patients who were readmitted within 3 days and those who were readmitted after 3 days (see Table 1 for complete demographic information).
Table 1.
Demographics
| Days between admissions
|
|||
|---|---|---|---|
| Total (n=202) |
≤3 (n=93) |
>3 (n=109) |
|
| Age, years (mean ± SD) | 40.0 (11.9) | 38.7 (10.3) | 40.4 (12.9) |
| Education, years (mean ± SD) | 11.1 (2.4) | 11.0 (2.5) | 11.3 (2.3) |
| Gender (male) | 162 (80%) | 76 (82%) | 86 (79%) |
| Race | |||
| American Indian or Native Alaskan | 14 (7%) | 9 (10%) | 5 (5%) |
| Asian | 1 (1%) | 0 (0%) | 1 (1%) |
| Black or African American | 91 (45%) | 40 (43%) | 51 (47%) |
| Native Hawaiian or other Pacific Islander | 0 (0%) | 0 (0%) | 0 (0%) |
| White | 87 (43%) | 41 (44%) | 46 (42%) |
| Other | 8 (4%) | 3 (3%) | 5 (5%) |
| Ethnicity | |||
| Hispanic | 20 (10%) | 9 (10%) | 11 (10%) |
| Non-Hispanic | 182 (90%) | 84 (90%) | 98 (90%) |
| Employment status | |||
| Not employed | 175 (87%) | 81 (87%) | 94 (86%) |
| Full-time employment | 1 (1%) | 0 (0%) | 1 (1%) |
| Part-time employment | 16 (8%) | 6 (6%) | 10 (9%) |
| Income source | |||
| No income source | 93 (46%) | 48 (52%) | 45 (41%) |
| SSI/SSDI and other disability | 72 (35%) | 32 (34%) | 40 (37%) |
| Family support | 9 (4%) | 2 (2%) | 7 (6%) |
| Other | 21 (10%) | 7 (8%) | 14 (13%) |
Notes: Random sample of 30-day psychiatric patient readmissions in the emergency department over a 12-month period, September 2015 to August 2016. Patients may have multiple listings for race and income source. Employment status was not released by all the patients.
Abbreviations: SSDI, Social Security Disability Insurance; SSI, Supplemental Security Income.
The results indicate that the majority of the patients (72%) were readmitted for the same problem seen in the previous visit and that these patients had difficulty following the treatment recommendations and difficulty accessing community resources. The secondary analysis found no statistically significant between-group differences in evidence (see Table 2 to review treatment factors).
Table 2.
Treatment factors
| Days between admissions
|
|||
|---|---|---|---|
| Total (n=202) |
≤3 (n=93) |
>3 (n=109) |
|
| aDays since last admission (mean ± SD) | 8.2±8.6 | 1.5±0.8 | 13.9±8.1 |
| Hospital visits in last 30 days (mean ± SD) | 4.4±4.8 | 5.8±5.9 | 2.9±2.5 |
| Readmission visit related to/or a continuation of an unresolved issue from the previous visit | |||
| Identical or very similar to previous visit | 145 (72%) | 67 (72%) | 78 (72%) |
| Related but not identical | 44 (22%) | 21 (23%) | 23 (21%) |
| Not related but could have been addressed | 1 (1%) | 1 (1%) | 0 (0%) |
| Totally unrelated | 8 (4%) | 3 (3%) | 5 (5%) |
| bContinuity of care: treatment recommendations provided at the previous visit followed | |||
| Fully | 12 (6%) | 4 (4%) | 8 (7%) |
| Partially | 72 (36%) | 28 (30%) | 44 (40%) |
| Not at all | 115 (58%) | 58 (62%) | 57 (52%) |
| cContinuity of care: resources provided at the previous visit utilized | |||
| Fully | 11 (5%) | 5 (5%) | 6 (6%) |
| Partially | 72 (36%) | 26 (28%) | 46 (42%) |
| Not at all | 118 (58%) | 62 (67%) | 56 (51%) |
Notes: Random sample of 30-day psychiatric patient readmissions over a 12-month period, September 2015 to August 2016.
Included for descriptive purposes. Information in the chart review indicated a problem in the continuity of care:
treatment recommendations provided at discharge were not able to be followed;
referrals and appointments for psychiatric and/or medical treatment were not able to be completed.
The reviews identified a number of factors that may have contributed to the readmission visit. For a variety of reasons, many patients experienced a breakdown in the continuity of care after leaving the hospital, specifically with outpatient follow-up care (43%), using referrals (56%), and obtaining and taking prescribed medication (41%). Problems related to housing (63%) and transportation (14%) were also found. No statistically significant between-group differences were found in the secondary analysis (Table 3).
Table 3.
Factors contributing to readmission
| Days between admissions
|
|||
|---|---|---|---|
| Total (n=202) |
≤3 (n=93) |
>3 (n=109) |
|
| Outpatient follow-up | 43% | 41% | 46% |
| Missed appointment | 56 (26%) | 23 (25%) | 33 (30%) |
| Did not understand follow-up instructions | 3 (1%) | 1 (1%) | 1 (2%) |
| Clinic unable to provide services | 1 (1%) | 1 (1%) | 0 (0%) |
| Other problem | 33 (16%) | 18 (19%) | 14 (13%) |
| Referrals | 56% | 63% | 48% |
| Did not use referral | 95 (46%) | 51 (55%) | 44 (40%) |
| Facility unable to provide services | 4 (2%) | 4 (4%) | 0 (0%) |
| Referral not given | 1 (1%) | 1 (1%) | 0 (0%) |
| Other problem | 16 (8%) | 8 (9%) | 8 (7%) |
| Transportation | 14% | 13% | 14% |
| Transportation not available for medical appointment | 2 (1%) | 0 (0%) | 2 (2%) |
| Transportation not available for psychiatric appointment | 5 (2%) | 3 (3%) | 2 (2%) |
| Transportation not available for substance treatment | 4 (2%) | 3 (3%) | 1 (1%) |
| Other problem | 17 (9%) | 10 (11%) | 7 (6%) |
| Housing | 63% | 72% | 58% |
| Homeless | 127 (63%) | 64 (69%) | 63 (58%) |
| Could not get into shelter | 1 (1%) | 1 (1%) | 0 (0%) |
| Banned from shelter | 1 (1%) | 1 (1%) | 0 (0%) |
| Asked to leave current housing | 1 (1%) | 1 (1%) | 0 (0%) |
| No identification – required for shelter | 4 (2%) | 3 (3%) | 1 (1%) |
| Does not want to return to current housing | 1 (1%) | 1 (1%) | 0 (0%) |
| Other problem | 4 (2%) | 2 (2%) | 2 (2%) |
| Medications | 41% | 40% | 42% |
| Unable to fill prescription | 9 (4%) | 3 (3%) | 6 (6%) |
| Did not go to pharmacy | 38 (18%) | 22 (24%) | 16 (15%) |
| Declined by pharmacy | 1 (1%) | 1 (1%) | 0 (0%) |
| Unable to afford prescription medications | 1 (1%) | 0 (0%) | 1 (1%) |
| Lost prescription | 9 (4%) | 3 (3%) | 6 (6%) |
| Unable to tolerate (side effects) medication | 4 (2%) | 1 (1%) | 3 (3%) |
| Refused to take prescription medications | 8 (4%) | 4 (4%) | 4 (4%) |
| Did not understand the need to take medications | 1 (1%) | 0 (0%) | 1 (1%) |
| Forgot to take medication | 1 (1%) | 1 (1%) | 0 (0%) |
| Afraid of medication | 0 (0%) | 0 (0%) | 0 (0%) |
| Confused about how to take medication | 2 (1%) | 0 (0%) | 2 (2%) |
| Other problem | 21 (10%) | 5 (5%) | 16 (15%) |
Notes: Random sample of 30-day psychiatric patient readmissions over a 12-month period, September 2015 to August 2016; includes homelessness as well as other concerns such as does not like, or cannot tolerate, current housing, could not get into shelter, banned from shelter, and asked to leave current housing.
Treatment factors
Initial complaints in patients were identified in the 202 visits reviewed. Three major areas were found to be present in half of the sample (psychiatric symptoms, substance use, and violent/suicidal behavior). An additional 13% presented for a medical complaint and were later found to have a comorbid psychiatric issue that needed to be addressed. Six percent of the visits were found to be unnecessary, meaning that the visit was to meet a physical need (eg, housing and transportation) in the absence of an acute psychiatric condition that required treatment. The secondary analysis found statistically significant differences between patients who were readmitted within 3 days and those who were readmitted after 3 days, with the former reporting significantly higher rates of substance use (Yates corrected χ2=6.06, p=0.014; see Table 4).
Table 4.
Presenting complaint
| Days between admissions
|
|||
|---|---|---|---|
| Total (n=202) |
≤3 (n=93) |
>3 (n=109) |
|
| Psychiatric symptoms (% of patients) | 52% | 49% | 53% |
| Symptoms of anxiety | 13 | 5 | 8 |
| Symptoms of confusion (delirium and dementia) | 2 | 1 | 1 |
| Symptoms of mania/hypomania | 8 | 3 | 5 |
| Symptoms of depression | 34 | 18 | 16 |
| Symptoms of psychosis (ie, paranoia, disorganized thought process, and hallucinations) | 47 | 19 | 28 |
| Substance use* | 36% | 45% | 28% |
| Substance use issue (withdrawal/requesting referral) | 55 | 31 | 24 |
| Intoxication primary issue (violent or disorganized behavior included if secondary to intoxication) | 17 | 11 | 6 |
| Violent/suicidal ideation and behavior | 52% | 48% | 55% |
| Violence: self-directed (suicidal ideation, behavior, and post-suicide attempt) | 84 | 34 | 50 |
| Violence: directed toward others (homicidal, aggressive, assaultive, and intending to harm others) | 21 | 11 | 10 |
| aPrimary medical complaint* | 13% | 10% | 16% |
| bNonacute psychiatric complaint | 6% | 6% | 6% |
| Social factors leading to psychosocial stress (ie, shelter, food, and respite) | 2 | 0 | 2 |
| Psychiatric medications refill | 11 | 6 | 5 |
Notes: Random sample of 30-day psychiatric patient readmissions in the emergency department over a 12-month period, September 2015 to August 2016. Patients may have presented with multiple psychiatric complaints (psychiatric symptoms, substance use disorders, and violent/suicidal ideation and behavior).
Patients who presented for the treatment of a medical condition and were later found to have a comorbid psychiatric complaint.
Patients who did not present for or require acute psychiatric care.
p<0.05 (Yates corrected χ2=6.06, p=0.014).
The largest diagnostic pools found in the sample were substance use disorders (51%), mood disorders (36%), and psychotic disorders (26%). Anxiety disorders (2%) and other disorders (17%) were also present. Patients with multiple diagnoses were included in the sample. The secondary analysis found no statistically significant between-group differences (Table 5).
Table 5.
Diagnosis
| Days between admissions
|
|||
|---|---|---|---|
| Total (n=202) |
≤3 n=93 |
>3 (n=109) |
|
| No diagnosis | 0% | 0% | 0% |
| Anxiety disorders | 2% | 2% | 1% |
| Mood disorders | 36% | 32% | 39% |
| Bipolar disorder | 24 | 7 | 18 |
| Depressive disorder | 48 | 23 | 25 |
| Psychotic disorders | 26% | 26% | 25% |
| Schizophrenia/schizoaffective | 40 | 19 | 21 |
| Psychosis disorder other or unspecified | 13 | 5 | 8 |
| Substance use disorders (including withdrawal) | 51% | 57% | 45% |
| Other disorders | 17% | 20% | 16% |
Notes: Random sample of 30-day psychiatric patient readmissions over a 12-month period, September 2015 to August 2016. Anxiety disorders include panic disorder, obsessive–compulsive disorder, posttraumatic stress disorder, anxiety disorder not otherwise specified, and anxiety disorder.
Factors identified to prevent readmission
Reviewers identified factors that could ameliorate psychiatric patient readmission visits. These include facilitation of bidirectional communication with follow-up providers (50%) and/or family members and other caretakers (46%). Sixty-five percent of patients need to be assigned an intensive case manager or be reconnected with their existing intensive case manager (38%). Other factors that may help reduce readmission are as follows: support in managing psychotropic medication prescriptions (50%), increased access to drug and alcohol counseling (65%, both within and outside PMH), and assistance with resolving housing issues (short term, 39%; long term, 50%). No secondary analyses were performed for these factors (Table 6).
Table 6.
Quality improvement opportunities
| Days between admissions
|
|||
|---|---|---|---|
| Total (n=202) |
≤3 (n=93) |
>3 (n=109) |
|
| Support and education for filling prescriptions | 37% | 30% | 43% |
| Assistance with transportation | 26% | 29% | 31% |
| Increased communication with follow-up providers | 50% | 40% | 58% |
| Increased communication with family or other caretaker such as case worker | 46% | 38% | 53% |
| Increased drugs/ETOH resources within PMH | 65% | 65% | 63% |
| Increased drugs/ETOH resources outside PMH | 65% | 67% | 62% |
| Establishing intensive case management | 65% | 62% | 65% |
| Connecting with existing intensive case management | 38% | 33% | 41% |
| Short-term housing solutions (overnight stay) | 39% | 43% | 35% |
| Long-term housing solutions | 50% | 53% | 45% |
Note: Random sample of 30-day psychiatric patient readmissions over a 12-month period, September 2015 to August 2016.
Abbreviations: ETOH, ethyl alcohol; PMH, Parkland Memorial Hospital.
Discussion
Hospitals across the country are struggling to meet the increased demand for psychiatric services in the ED. The findings from this project, while not comprehensive, suggest that, in many cases, lack of continuity of care may be a significant factor contributing to readmission. The problem may be reduced to the absence of the patient at a facility that provides community care (medications, housing, inpatient, outpatient, etc.) after discharge from the ED. This can be further broken down: 1) Why did the patient not receive the recommended care and 2) was there appropriate treatment available at the time of discharge?
Upon review, many of these ED visits appear to have been avoidable. In many instances, acute care is not necessary, more often may have been avoided, and had linkage to community treatment occurred. Many of these patients are seen repeatedly for the same psychiatric problem and report difficulty in managing care outside the ED. A number of factors appear to be negatively affecting patients’ ability to continue receiving treatment after leaving the ED and subsequently leading to ED readmissions for the same unresolved problem. The primary area identified for improvement was in the area of transition of care from PMH to caregivers and providers in the community. The evaluation suggested that there is a problem with the linkage of care, specifically upon exiting the hospital; patients often do not continue treatment in the community, leading to treatment being repeatedly sought for in the hospital ED.
While factors leading to psychiatric patient readmission in the hospital EDs are complex, it appears that a large number of these visits are related to substance use and may reflect the presence of a subset of patients with unique needs. It may be beneficial to have dedicated space for these patients to be observed as they are being evaluated, followed by community-based detoxification and residential treatment available. In general, additional inpatient and outpatient services are needed for patients with substance use disorders, with and without other comorbid psychiatric and medical conditions.
Given the chronic nature of psychiatric illnesses and the associated impairment in social and occupational functioning that increases with symptom severity, it would be expected that patients with unresolved psychiatric conditions that remain untreated will have acute exacerbations of the disease and would then present for care in a familiar environment such as the ED. As noted, the presenting complaints share the common theme of unresolved psychiatric issues. In the study sample, 90% of readmitted patients came in to receive services for the exact or a related complaint as in the previous visit. The issue becomes how to improve the accessibility and utilization of community resources by this vulnerable population of psychiatric patients.
Within the PMH catchment area, there are community resources available to manage and treat mental health and substance use, as well as to support in meeting housing and funding needs. Unfortunately, the services are, at best, limited and, even when they exist, are fragmented, with multiple individual service providers independently handling patient needs. Vulnerable patients living in the community are not always able to effectively access the resources needed to prevent an acute exacerbation of their psychiatric illness. Patients in this subpopulation are frequently high utilizers of ED services. In these situations, PMH has 2 primary roles: 1) providing the best possible level of care based on a level of acuity and 2) (re)establishing the patient’s linkages to appropriate community resources. While it is understood that subpopulation of patients may continue to use the ED as the primary source of psychiatric care, a large number of unnecessary visits may be reduced through improved connection to and collaboration with appropriate community service providers.
A number of opportunities for quality improvement were identified and action plans were developed. Several of the initiatives have begun to be implemented; others are still in the planning stages, while others remain under consideration.
Limitations and future directions
This study is a naturalistic observation, and as such, there is no experimental control (eg, open-label treatment, observational data, retrospective data analysis, and unblinded raters), leading to any number of inferential concerns. Specifically, raters were providers in the PED and as such familiar with the operations, but were not directly involved in the cases assigned and relied upon the detail and completeness of the chart note. While the quality of chart notes is monitored and regulated, much of the information used to make ratings was extracted from the additional detail contained within the note, which may vary from case to case. Another limitation that needs to be considered when interpreting the data is that the PRS was constructed specifically for this study, and the content of these final questions was designed for use at PMH and may be limited in scope. This is reflected in the high prevalence rates found across problem areas. Future studies may consider expanding this section to include more speculative sources of readmission. All sections of the PRS, the final section in particular, would require modification to meet the specific needs of the setting under study, and items were reevaluated for validity and reliability. A study such as this has significant strengths in that it is replicable in most settings; however, this ease of replication also poses a concern due to the lack of experimental control. Another strength of the study is the location (large metropolitan area) and population (public hospital), which aid in the generalization of the findings to other public and, perhaps to a lesser degree, private metal health facilities. While the process is iterative and ongoing, global outcomes are obtainable.17 The next step is to evaluate the outcomes of specific action plans and to identify those that most effectively address the concern of chronic psychiatric patient readmission in the ED.
Conclusion
This study described a continuous quality improvement project, using a well-established technique (the PDSA cycle), to address a critical ongoing concern shared by public hospitals around the country: how to improve psychiatric patient care in the ED, in the presence of increased volume and in the absence of additional resources. In the case of PMH, as would be expected of any institution, quality improvement opportunities are found internally, as well as outside the organization. Holistically, the findings point in one direction; specifically, it appears that it will require a unified effort, with all community resource providers acting in symphony, to ebb the rising tide of requests for psychiatric services in the hospital EDs across the country. While, on the face of it, this seems a naïve proposition, the economic force generated by the increased burden of maintaining fragmented services may be sufficient to drive change out of sheer necessity. It appears that, in this case, “A house divided will not stand.” The process at PMH has only begun, but thus far, the community resource providers we have encountered have been eager and willing to collaborate on the acute and long-term solutions.
Acknowledgments
This publication was supported by National Institutes of Health (NIH)/National Center for Research Resources Clinical and Translational Science Institute Grant Number UL1 RR025780. Its contents are the authors’ sole responsibility and do not necessarily represent official NIH views. The authors would like to thank A John Rush (the UTSW, Dallas, TX, USA), for his assistance in the preparation of this manuscript.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Center for Health Statistics . Health, United States 2010: With Special Feature on Death and Dying. Hyattsville, MD: National Center for Health Statistics; 2011. [PubMed] [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration Mental and substance use disorders [Updated October 9, 2014] [Accessed July 10, 2017]. Available from: http://www.samhsa.gov/disorders.
- 4.Agency for Healthcare Research and Quality [homepage on the Internet] [Accessed July 10, 2017]. Available from: http://hcupnet.ahrq.gov.
- 5.Heslin KC, Weiss AJ. Hospital Readmissions Involving Psychiatric Disorders, 2012. Rockville, MD: Agency for Healthcare Research and Quality; 2015. [Accessed February 19, 2018]. (HCUP Statistical Brief #189). Available from: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb189-Hospital-Readmissions-PsychiatricDisorders-2012.pdf. [PubMed] [Google Scholar]
- 6.Kessler RC, Aguilar-Gaxiola S, Alonso J, et al. The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiol Psychiatr Soc. 2009;18(1):23–33. doi: 10.1017/s1121189x00001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 8.Whiteford HA, Ferrari AJ, Degenhardt L, Feigin V, Vos T. The global burden of mental, neurological and substance use disorders: an analysis from the Global Burden of Disease Study 2010. PLoS One. 2015;10(2):e0116820. doi: 10.1371/journal.pone.0116820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3(2):171–178. doi: 10.1016/S2215-0366(15)00505-2. [DOI] [PubMed] [Google Scholar]
- 10.Weiss AJ, Barrett ML, Steiner C. Trends and projections in inpatient hospital costs and utilization, 2003–2013. Rockville, MD: Agency for Healthcare Research and Quality; 2014. [Accessed March 13, 2015]. (HCUP Statistical Brief #175). Available from: http://www.hcupus.ahrq.gov/reports/statbriefs/sb175-Hospital-Cost-Utilization-Projections-2013.pdf. [PubMed] [Google Scholar]
- 11.Larkin GL, Claassen CA, Emond JA, Pelletier AJ, Camargo CA. Trends in U.S. emergency department visits for mental health conditions, 1992 to 2001. Psychiatr Serv. 2005;56(6):671–677. doi: 10.1176/appi.ps.56.6.671. [DOI] [PubMed] [Google Scholar]
- 12.Fields WW, Asplin BR, Larkin GL, et al. The Emergency Medical Treatment and Labor Act as a federal health care safety net program. Acad Emerg Med. 2001;8(11):1064–1069. doi: 10.1111/j.1553-2712.2001.tb01116.x. [DOI] [PubMed] [Google Scholar]
- 13.Hazlett SB, McCarthy ML, Londner MS, Onyike CU. Epidemiology of adult psychiatric visits to US emergency departments. Acad Emerg Med. 2004;11(2):193–195. [PubMed] [Google Scholar]
- 14.Larkin GL, Smith RP, Beautrais AL. Trends in US emergency department visits for suicide attempts, 1992–2001. Crisis. 2008;29(2):73–80. doi: 10.1027/0227-5910.29.2.73. [DOI] [PubMed] [Google Scholar]
- 15.Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK. The de facto US mental and addictive disorders service system. Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry. 1993;50(2):85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- 16.Merrick EL, Perloff J, Tompkins CP. Emergency department utilization patterns for Medicare beneficiaries with serious mental disorders. Psychiatr Serv. 2010;61(6):628–631. doi: 10.1176/ps.2010.61.6.628. [DOI] [PubMed] [Google Scholar]
- 17.Health Resources and Services Administration Quality Improvement. [Accessed February 19, 2018]. Available from: https://www.hrsa.gov/quality/toolbox/methodology/qualityimprovement/part3.html.
- 18.Sullivan G, Wells KB, Morgenstern H, Leake B. Identifying modifiable risk factors for rehospitalization: a case-control study of seriously mentally ill persons in Mississippi. Am J Psychiatry. 1995;152(12):1749–1756. doi: 10.1176/ajp.152.12.1749. [DOI] [PubMed] [Google Scholar]
- 19.Walker R, Minor-Schork D, Bloch R, Esinhart J. High risk factors for rehospitalization within six months. Psychiatr Q. 1996;67(3):235–243. doi: 10.1007/BF02238954. [DOI] [PubMed] [Google Scholar]
- 20.Boyer CA, McAlpine DD, Pottick KJ, Olfson M. Identifying risk factors and key strategies in linkage to outpatient psychiatric care. Am J Psychiatry. 2000;157(10):1592–1598. doi: 10.1176/appi.ajp.157.10.1592. [DOI] [PubMed] [Google Scholar]
- 21.Nelson EA, Maruish ME, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv. 2000;51(7):885–889. doi: 10.1176/appi.ps.51.7.885. [DOI] [PubMed] [Google Scholar]
- 22.Oiesvold T, Saarento O, Sytema S, et al. Predictors for readmission risk of new patients: the Nordic Comparative Study on Sectorized Psychiatry. Acta Psychiatr Scand. 2000;101(5):367–373. doi: 10.1034/j.1600-0447.2000.101005367.x. [DOI] [PubMed] [Google Scholar]
- 23.Shaw H, Mackie CA, Sharkie I. Evaluation of pharmacy discharge planning on medication problems experienced by discharged acute admission mental health patients. Int J Pharm Pract. 2000;8(2):144–153. [Google Scholar]
- 24.Cuffel BJ, Held M, Goldman W. Predictive models and the effectiveness of strategies for improving outpatient follow-up under managed care. Psychiatr Serv. 2002;53(11):1438–1443. doi: 10.1176/appi.ps.53.11.1438. [DOI] [PubMed] [Google Scholar]
- 25.Durbin J, Lin E, Layne C, Teed M. Is readmission a valid indicator of the quality of inpatient psychiatric care? J Behav Health Serv Res. 2007;34(2):137–150. doi: 10.1007/s11414-007-9055-5. [DOI] [PubMed] [Google Scholar]
- 26.Dixon L, Goldberg R, Iannone V, et al. Use of a critical time intervention to promote continuity of care after psychiatric inpatient hospitalization. Psychiatr Serv. 2009;60(4):451–458. doi: 10.1176/ps.2009.60.4.451. [DOI] [PubMed] [Google Scholar]
- 27.Joynt KE, Jha AK. Thirty-day readmissions – truth and consequences. N Engl J Med. 2012;366(15):1366–1369. doi: 10.1056/NEJMp1201598. [DOI] [PubMed] [Google Scholar]
- 28.Vigod SN, Kurdyak PA, Dennis CL, et al. Transitional interventions to reduce early psychiatric readmissions in adults: systematic review. Br J Psychiatry. 2013;202(3):187–194. doi: 10.1192/bjp.bp.112.115030. [DOI] [PubMed] [Google Scholar]
- 29.Shaffer SL, Hutchison SL, Ayers AM, et al. Brief critical time intervention to reduce psychiatric rehospitalization. Psychiatr Serv. 2015;66(11):1155–1161. doi: 10.1176/appi.ps.201400362. [DOI] [PubMed] [Google Scholar]
- 30.Smith TE, Abraham M, Bolotnikova NV, et al. Psychiatric inpatient discharge planning practices and attendance at aftercare appointments. Psychiatr Serv. 2017;68(1):92–95. doi: 10.1176/appi.ps.201500552. [DOI] [PubMed] [Google Scholar]
- 31.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Corp IBM. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp; 2013. [Google Scholar]