Abstract
Aims
Atrial fibrillation (AF) is the most common sustained arrhythmia encountered in clinical practice. Patients presenting with AF are often admitted to hospital for rhythm or rate control, symptom management, and/or anticoagulation. We investigated temporal trends in AF hospitalizations in United States from 1996 to 2010.
Methods
Data were obtained from the National Hospital Discharge Survey (NHDS), a national probability sample survey of discharges conducted annually by National Center for Health Statistics. Because of the survey design, sampling weights were applied to the raw NHDS data to produce national estimates. Hospitalizations with a primary diagnosis of AF were identified using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) code of 427.31. Weighted least squares regression was used to test for linear trends in the number of AF admissions, length of stay, and inpatient mortality. We further stratified AF admissions based on patients' age, gender, and race.
Results
Admissions for a primary diagnosis of AF increased from approximately 286,000 in 1996 to about 410,000 in 2010 with a significant linear trend (β = 9470 additional admissions per year, p < 0.001). The trend of increased AF admissions was uniform across patient sub-groups. Overall, mean length of stay for AF admissions was 3.75 days, and this remained relatively stable over time (β = 0.002 days, p = 0.884). Inpatient mortality was 0.96% and also remained stable over time (β = 0.031%, p = 0.181).
Conclusion
Our data demonstrate an increase in the number of AF admissions but constant length of stay and mortality over time.
Keywords: Atrial fibrillation, Hospitalization, Length of stay, Mortality
1. Introduction
Atrial fibrillation (AF) is the most common sustained arrhythmia affecting about 1–2% of the general population [1]. Its prevalence in the United States (US) is projected to increase by 2.5 fold to reach about 7.5 Million by 2050, posing a public health and economic challenge [2] [3]. AF is associated with increased risk of stroke, congestive heart failure and all-cause mortality [4].
AF poses an increased economic burden on the health care system due to increasing cost of care driven in big part by hospitalizations [5]. The annual direct cost of AF management in the US is estimated at about $6–6.7 billion [6]. This economic burden is projected to increase further due to the increased prevalence of chronic heart diseases which usually lead to AF [7]. It is therefore important to examine the burden of inpatient care for AF patients and analyze its trends over time. To this end, we analyzed the National Hospital Discharge Survey Data (NHDS) database for temporal trends in AF hospitalizations over the past two decades.
2. Methods
Data were obtained from NHDS, an annual survey of inpatient discharges conducted by the National Center for Health Statistics since 1965. NHDS collects raw data on about 1% of hospital discharges and then weight each discharge to produce national estimates. Data collected included basic demographic variables, primary discharge diagnosis and several secondary discharge diagnoses. NHDS collects data from non-federal US hospitals that have more than six beds with average length of stay (LOS) of less than 30 days.
For the present analysis, data from 1996 through 2010 were included. A primary discharge diagnosis of AF was identified using the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) code of 427.31. Co-morbidities were ascertained through application of relevant ICD-9 codes to secondary diagnoses. NHDS also collects data on inpatient mortality and length of stay which were included in present study.
2.1. Statistical analysis
This report estimates the number of AF hospital admissions, mean LOS, and inpatient mortality for every year between 1996 and 2010. Weighted least squares regression was utilized to test for linear trends over time in the entire population. We also report number of AF admissions by age, gender, and racial subgroups. The results are presented as the estimated annual change (β), a 95% confidence interval for β, and p-value, which tested whether the annual change of each parameter differed significantly from zero. Due to the survey design, sampling weights provided in the NHDS data were applied to produce the national estimates [8]. Data analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC).
3. Results
Applying the weights to the raw data set converted 43,817 sampled hospitalizations to an estimated 5,826,067 total AF hospitalizations in the US from 1996 to 2010. The percentages of patients who were classified as having secondary diagnoses of selected ICD-9 codes representing comorbidities of interest are shown in Table 1.
Table 1.
Baseline characteristics and comorbidities by year.
| 1996 | 1997 | 1998 | 1999 | 2000 | |
|---|---|---|---|---|---|
| Age | 72.7 (63.1–80.9) | 73.5 (63.7–80.6) | 72.4 (62.2–80.3) | 72.5 (63.2–80.0) | 73.2 (63.7–80.7) |
| Age Group | |||||
| <50 | 28,168 (9.8%) | 29,148 (9.1%) | 23,906 (7.3%) | 31,010 (8.9%) | 32,567 (9.1%) |
| 50-59 | 26,345 (9.2%) | 25,368 (7.9%) | 39,109 (12.0%) | 35,571 (10.2%) | 33,644 (9.4%) |
| 60-69 | 60,941 (21.3%) | 61,158 (19.2%) | 65,524 (20.0%) | 64,352 (18.5%) | 69,997 (19.6%) |
| 70- 79 | 82,309 (28.7%) | 107,652 (33.7%) | 103,169 (31.5%) | 118,585 (34.2%) | 114,401 (32.1%) |
| >80 | 88,599 (30.9%) | 96,028 (30.1%) | 95,454 (29.2%) | 97,657 (28.1%) | 106,122 (29.7%) |
| Gender | |||||
| Male | 132,986 (46.4%) | 143,436 (44.9%) | 154,877 (47.3%) | 150,063 (43.2%) | 153,275 (43.0%) |
| Female | 153,376 (53.6%) | 175,918 (55.1%) | 172,285 (52.7%) | 197,112 (56.8%) | 203,456 (57.0%) |
| Race | |||||
| White | 210,621 (73.6%) | 237,744 (74.4%) | 242,030 (74.0%) | 246,635 (71.0%) | 242,741 (68.0%) |
| Black/African American | 13,625 (4.8%) | 20,366 (6.4%) | 19,055 (5.8%) | 22,217 (6.4%) | 19,890 (5.6%) |
| American Indian/Alaskan Native | 601 (0.2%) | 1,253 (0.4%) | 1,311 (0.4%) | 1,226 (0.4%) | 95 (0.0%) |
| Asian | 4,188 (1.5%) | 1,884 (0.6%) | 3,681 (1.1%) | 1,758 (0.5%) | 1,854 (0.5%) |
| Native Hawaiian/Pacific Islander | 2,827 (1.0%) | 3,997 (1.3%) | 4,308 (1.3%) | 4,124 (1.2%) | 305 (0.1%) |
| Other | 2,253 (0.6%) | ||||
| Multiple Races | 220 (0.1%) | ||||
| Not Stated | 54,500 (19.0%) | 54,110 (16.9%) | 56777 (17.4%) | 71215 (20.5%) | 89,373 (25.1%) |
| Marriage Status | |||||
| Married | 92,524 (32.3%) | 102,384 (32.1%) | 105,604 (32.3%) | 117,315 (33.8%) | 118,572 (33.2%) |
| Single | 20,083 (7.0%) | 23,549 (7.4%) | 25,810 (7.9%) | 19,576 (5.6%) | 28,332 (7.9%) |
| Widowed | 58,309 (20.4%) | 62,217 (19.5%) | 53,162 (16.2%) | 62,588 (18.0%) | 68,420 (19.2%) |
| Divorced | 7,559 (2.6%) | 9,887 (3.1%) | 8,945 (2.7%) | 11,699 (3.4%) | 8,646 (2.4%) |
| Separated | 1,136 (0.4%) | 1,938 (0.6%) | 1,251 (0.4%) | 1,264 (0.4%) | 3,735 (1.0%) |
| Not Stated | 106,751 (37.3%) | 119,379 (37.4%) | 132,390 (40.5%) | 134,733 (38.8%) | 129,026 (36.2%) |
| Region | |||||
| Northeast | 67,700 (23.6%) | 80,080 (25.1%) | 98,089 (30.0%) | 96,587 (27.8%) | 91,085 (25.5%) |
| Midwest | 71,540 (25.0%) | 79,176 (24.8%) | 80,823 (24.7%) | 88,474 (25.5%) | 95,047 (26.6%) |
| South | 102,217 (35.7%) | 111,960 (35.1%) | 108,629 (33.2%) | 110,853 (31.9%) | 125,328 (35.1%) |
| West | 44,905 (15.7%) | 48,138 (15.1%) | 39,621 (12.1%) | 51,261 (14.8%) | 45,271 (12.7%) |
| Ischemic heart disease | 80,039 (28.0%) | 71,959 (22.5%) | 88,463 (27.0%) | 91,635 (26.4%) | 92,326 (25.9%) |
| Ventricular arrhythmias | 9,194 (3.2%) | 10,523 (3.3%) | 9,944 (3.0%) | 7,669 (2.2%) | 10,233 (2.9%) |
| Left bundle branch block | 4,721 (1.6%) | 3,996 (1.3%) | 3,146 (1.0%) | 3,426 (1.0%) | 3,909 (1.1%) |
| Complete AV block | 1,000 (0.3%) | 3,776 (1.2%) | 1,509 (0.5%) | 935 (0.3%) | 501 (0.1%) |
| Heart Failure | 62,204 (21.7%) | 67,396 (21.1%) | 70,400 (21.5%) | 71,955 (20.7%) | 67,705 (19.0%) |
| Peripheral vascular disease | 6,985 (2.4%) | 7,574 (2.4%) | 10,237 (3.1%) | 10,635 (3.1%) | 11,704 (3.3%) |
| Hypertension | 95,414 (33.3%) | 111,250 (34.8%) | 115,031 (35.2%) | 140,775 (40.5%) | 139,175 (39.0%) |
| Chronic pulmonary diseases | 36,084 (12.6%) | 53,631 (16.8%) | 48,156 (14.7%) | 55,944 (16.1%) | 51,179 (14.3%) |
| Diabetes | 42,336 (14.8%) | 49,206 (15.4%) | 52,697 (16.1%) | 52,284 (15.1%) | 54,732 (15.3%) |
| Chronic kidney disease | 3,564 (1.2%) | 5,383 (1.7%) | 4,813 (1.5%) | 6,389 (1.8%) | 8,196 (2.3%) |
| Anemia | 10,488 (3.7%) | 14,384 (4.5%) | 16,142 (4.9%) | 13,062 (3.8%) | 16,618 (4.7%) |
| Pulmonary circulation disorders | 4,782 (1.7%) | 6,628 (2.1%) | 6,610 (2.0%) | 6,377 (1.8%) | 9,044 (2.5%) |
| Paralysis | 6,827 (2.4%) | 5,957 (1.9%) | 3,669 (1.1%) | 3,537 (1.0%) | 4,119 (1.2%) |
| Valvular diseases | 43,549 (15.2%) | 49,011 (15.3%) | 55,225 (16.9%) | 58,471 (16.8%) | 60,485 (17.0%) |
| Other neurologic disorders | 5,992 (2.1%) | 12,481 (3.9%) | 13,569 (4.1%) | 10,502 (3.0%) | 12,314 (3.5%) |
| Hypothyroidism | 19,552 (6.8%) | 18,621 (5.8%) | 19,932 (6.1%) | 26,206 (7.5%) | 34,374 (9.6%) |
| Liver disease | 1,249 (0.4%) | 2,586 (0.8%) | 1,023 (0.3%) | 1,956 (0.6%) | 1,439 (0.4%) |
| PUD | 4,077 (1.4%) | 3,627 (1.1%) | 4,779 (1.5%) | 4,714 (1.4%) | 2,619 (0.7%) |
| AIDS | 40 (0.0%) | 122 (0.0%) | |||
| Lymphoma | 1,168 (0.4%) | 1,504 (0.5%) | 969 (0.3%) | 2,477 (0.7%) | 854 (0.2%) |
| Metastatic cancer | 945 (0.3%) | 2,826 (0.9%) | 5,817 (1.8%) | 4,307 (1.2%) | 5,670 (1.6%) |
| Solid tumor without mets | 18,352 (6.4%) | 19,885 (6.2%) | 21,116 (6.5%) | 20,420 (5.9%) | 24,022 (6.7%) |
| Collagen vascular diseases | 3,201 (1.1%) | 6,215 (1.9%) | 3,612 (1.1%) | 6,427 (1.9%) | 7,849 (2.2%) |
| Coagulopathy | 2,062 (0.7%) | 5,791 (1.8%) | 4,387 (1.3%) | 2,724 (0.8%) | 6,732 (1.9%) |
| Obesity | 7,465 (2.6%) | 6,709 (2.1%) | 13,359 (4.1%) | 14,535 (4.2%) | 11,107 (3.1%) |
| Weight loss | 727 (0.3%) | 3,442 (1.1%) | 1,551 (0.5%) | 1,737 (0.5%) | 3,712 (1.0%) |
| Fluid and electrolyte disorders | 23,202 (8.1%) | 34,518 (10.8%) | 27,156 (8.3%) | 27,553 (7.9%) | 32,556 (9.1%) |
| Alcohol abuse | 4,240 (1.5%) | 7,602 (2.4%) | 7,446 (2.3%) | 8,238 (2.4%) | 5,746 (1.6%) |
| Drug abuse | 1,407 (0.5%) | 883 (0.3%) | 1,359 (0.4%) | 2,370 (0.7%) | 737 (0.2%) |
| Depression | 4,145 (1.4%) | 3,882 (1.2%) | 9,730 (3.0%) | 9,428 (2.7%) | 19,677 (5.5%) |
| Psychosis | 1,712 (0.6%) | 2,824 (0.9%) | 2,154 (0.7%) | 2,496 (0.7%) | 4,302 (1.2%) |
| Smoking (other tobacco use) | 5,157 (1.8%) | 9,277 (2.9%) | 13,557 (4.1%) | 19,479 (5.6%) | 18,153 (5.1%) |
| 2001 | 2002 | 2003 | 2004 | 2005 | |
|---|---|---|---|---|---|
| Age | 72.9 (64.4–80.7) | 74.0 (64.5–81.2) | 73.0 (61.9–80.6) | 72.9 (61.7–81.7) | 73.9 (63.1–82.3) |
| Age Group | |||||
| <50 | 28,969 (7.5%) | 27,895 (6.7%) | 34,673 (8.1%) | 37,188 (9.2%) | 34,057 (8.3%) |
| 50-59 | 38,505 (10.0%) | 43,377 (10.4%) | 51,590 (12.0%) | 44,755 (11.1%) | 39,057 (9.5%) |
| 60-69 | 77,476 (20.1%) | 68,905 (16.5%) | 79,985 (18.7%) | 80,072 (19.9%) | 79,418 (19.3%) |
| 70- 79 | 122,794 (31.9%) | 144,374 (34.5%) | 136,604 (31.9%) | 101,018 (25.1%) | 117,663 (28.6%) |
| >80 | 117,265 (30.5%) | 133,350 (31.9%) | 125,899 (29.4%) | 140,133 (34.8%) | 140,865 (34.3%) |
| Gender | |||||
| Male | 171,195 (44.5%) | 185,964 (44.5%) | 186,901 (43.6%) | 180,381 (44.7%) | 177,694 (43.2%) |
| Female | 213,814 (55.5%) | 231,937 (55.5%) | 241,850 (56.4%) | 222,785 (55.3%) | 233,366 (56.8%) |
| Race | |||||
| White | 266,424 (69.2%) | 297,212 (71.1%) | 301,868 (70.4%) | 275,647 (68.4%) | 276,423 (67.2%) |
| Black/African American | 17,561 (4.6%) | 21,796 (5.2%) | 24,868 (5.8%) | 24,964 (6.2%) | 25,916 (6.3%) |
| American Indian/Alaskan Native | 509 (0.1%) | 1,042 (0.2%) | 727 (0.2%) | 521 (0.1%) | 669 (0.2%) |
| Asian | 2,767 (0.7%) | 1,781 (0.4%) | 2,308 (0.5%) | 3,841 (1.0%) | 6,418 (1.6%) |
| Native Hawaiian/Pacific Islander | 1,001 (0.3%) | 645 (0.2%) | 1,011 (0.2%) | 817 (0.2%) | 849 (0.2%) |
| Other | 2,737 (0.7%) | 2,504 (0.6%) | 3,832 (0.9%) | 3,948 (1.0%) | 2,619 (0.6%) |
| Multiple Races | 1,858 (0.4%) | ||||
| Not Stated | 94,010 (24.4%) | 92,921 (22.2%) | 92,279 (21.5%) | 93,428 (23.2%) | 98,166 (23.9%) |
| Marriage Status | |||||
| Married | 122,554 (31.8%) | 136,338 (32.6%) | 150,371 (35.1%) | 122,717 (30.4%) | 112,260 (27.3%) |
| Single | 29,703 (7.7%) | 32,238 (7.7%) | 29,207 (6.8%) | 25,276 (6.3%) | 36,049 (8.8%) |
| Widowed | 65,496 (17.0%) | 83,398 (20.0%) | 81,540 (19.0%) | 71,521 (17.7%) | 70,304 (17.1%) |
| Divorced | 13,820 (3.6%) | 12,669 (3.0%) | 13,563 (3.2%) | 20,813 (5.2%) | 21,544 (5.2%) |
| Separated | 2,034 (0.5%) | 1,561 (0.4%) | 1,045 (0.2%) | 2,376 (0.6%) | 451 (0.1%) |
| Not Stated | 151,402 (39.3%) | 151,697 (36.3%) | 153,025 (35.7%) | 160,463 (39.8%) | 170,452 (41.5%) |
| Region | |||||
| Northeast | 111,299 (28.9%) | 108,740 (26.0%) | 108,299 (25.3%) | 102,661 (25.5%) | 96,968 (23.6%) |
| Midwest | 100,599 (26.1%) | 109,692 (26.2%) | 104,426 (24.4%) | 105,317 (26.1%) | 106,213 (25.8%) |
| South | 119,959 (31.2%) | 140,089 (33.5%) | 153,475 (35.8%) | 138,485 (34.3%) | 133,930 (32.6%) |
| West | 53,152 (13.8%) | 59,380 (14.2%) | 62,551 (14.6%) | 56,703 (14.1%) | 73,949 (18.0%) |
| Ischemic heart disease | 101,927 (26.5%) | 100,821 (24.1%) | 110,532 (25.8%) | 111,810 (27.7%) | 98,838 (24.0%) |
| Ventricular arrhythmias | 10,805 (2.8%) | 8,210 (2.0%) | 13,628 (3.2%) | 10,349 (2.6%) | 10,242 (2.5%) |
| Left bundle branch block | 2,570 (0.7%) | 5,247 (1.3%) | 5,901 (1.4%) | 2,936 (0.7%) | 5,415 (1.3%) |
| Complete AV block | 1,781 (0.5%) | 801 (0.2%) | 1,792 (0.4%) | 836 (0.2%) | 3,231 (0.8%) |
| Heart Failure | 84,181 (21.9%) | 98,307 (23.5%) | 90,742 (21.2%) | 86,217 (21.4%) | 91,698 (22.3%) |
| Peripheral vascular disease | 11,976 (3.1%) | 10,645 (2.5%) | 13,505 (3.1%) | 14,449 (3.6%) | 15,380 (3.7%) |
| Hypertension | 160,549 (41.7%) | 174,329 (41.7%) | 183,173 (42.7%) | 197,710 (49.0%) | 192,070 (46.7%) |
| Chronic pulmonary diseases | 63,562 (16.5%) | 66,993 (16.0%) | 78,923 (18.4%) | 61,363 (15.2%) | 62,216 (15.1%) |
| Diabetes | 63,273 (16.4%) | 72,850 (17.4%) | 68,111 (15.9%) | 73,862 (18.3%) | 73,210 (17.8%) |
| Chronic kidney disease | 7,096 (1.8%) | 10,562 (2.5%) | 5,449 (1.3%) | 10,750 (2.7%) | 15,284 (3.7%) |
| Anemia | 21,165 (5.5%) | 18,285 (4.4%) | 24,117 (5.6%) | 23,842 (5.9%) | 21,731 (5.3%) |
| Pulmonary circulation disorders | 8,672 (2.3%) | 7,378 (1.8%) | 10,804 (2.5%) | 6,256 (1.6%) | 9,803 (2.4%) |
| Paralysis | 3,471 (0.9%) | 5,219 (1.2%) | 6,190 (1.4%) | 3,881 (1.0%) | 3,584 (0.9%) |
| Valvular diseases | 63,069 (16.4%) | 59,957 (14.3%) | 63,513 (14.8%) | 55,427 (13.7%) | 63,629 (15.5%) |
| Other neurologic disorders | 13,031 (3.4%) | 14,734 (3.5%) | 15,309 (3.6%) | 15,518 (3.8%) | 16,225 (3.9%) |
| Hypothyroidism | 31,350 (8.1%) | 41,086 (9.8%) | 36,145 (8.4%) | 42,375 (10.5%) | 41,275 (10.0%) |
| Liver disease | 1,868 (0.5%) | 2,307 (0.6%) | 2,705 (0.6%) | 3,379 (0.8%) | 4,823 (1.2%) |
| PUD | 3,162 (0.8%) | 4,940 (1.2%) | 2,992 (0.7%) | 4,408 (1.1%) | 3,513 (0.9%) |
| AIDS | 85 (0.0%) | 255 (0.1%) | 57 (0.0%) | ||
| Lymphoma | 2,381 (0.6%) | 1,811 (0.4%) | 3,665 (0.9%) | 2,785 (0.7%) | 3,386 (0.8%) |
| Metastatic cancer | 3,079 (0.8%) | 9,711 (2.3%) | 4,801 (1.1%) | 3,150 (0.8%) | 5,287 (1.3%) |
| Solid tumor without mets | 21,367 (5.5%) | 31,566 (7.6%) | 30,442 (7.1%) | 22,497 (5.6%) | 22,671 (5.5%) |
| Collagen vascular diseases | 7,962 (2.1%) | 6,947 (1.7%) | 12,279 (2.9%) | 8,229 (2.0%) | 9,445 (2.3%) |
| Coagulopathy | 5,722 (1.5%) | 5,567 (1.3%) | 7,433 (1.7%) | 7,500 (1.9%) | 8,635 (2.1%) |
| Obesity | 14,487 (3.8%) | 16,346 (3.9%) | 20,347 (4.7%) | 19,471 (4.8%) | 20,732 (5.0%) |
| Weight loss | 2,920 (0.8%) | 1,495 (0.4%) | 3,077 (0.7%) | 1,629 (0.4%) | 2,513 (0.6%) |
| Fluid and electrolyte disorders | 37,699 (9.8%) | 42,724 (10.2%) | 45,981 (10.7%) | 43,905 (10.9%) | 50,037 (12.2%) |
| Alcohol abuse | 5,972 (1.6%) | 7,034 (1.7%) | 9,993 (2.3%) | 7,569 (1.9%) | 11,900 (2.9%) |
| Drug abuse | 195 (0.1%) | 729 (0.2%) | 1,873 (0.4%) | 2,261 (0.6%) | 2,572 (0.6%) |
| Depression | 12,274 (3.2%) | 10,340 (2.5%) | 11,677 (2.7%) | 13,325 (3.3%) | 19,173 (4.7%) |
| Psychosis | 3,554 (0.9%) | 2,449 (0.6%) | 3,776 (0.9%) | 3,183 (0.8%) | 6,320 (1.5%) |
| Smoking (other tobacco use) | 14,619 (3.8%) | 22,915 (5.5%) | 22,211 (5.2%) | 17,453 (4.3%) | 28,184 (6.9%) |
| 2006 | 2007 | 2008 | 2009 | 2010 | p-value | |
|---|---|---|---|---|---|---|
| Age | 72.7 (61.6–81.1) | 73.3 (62.0–81.3) | 70.9 (60.5–80.1) | 73.2 (61.6–80.9) | 70.7 (58.7–80.8) | 0.001 |
| Age Group | <0.001 | |||||
| <50 | 36,465 (8.7%) | 32,521 (6.8%) | 43,973 (10.2%) | 32,281 (7.9%) | 41,924 (10.2%) | |
| 50-59 | 45,752 (11.0%) | 60,369 (12.6%) | 53,185 (12.4%) | 48,360 (11.9%) | 62,166 (15.1%) | |
| 60-69 | 92,688 (22.2%) | 99,522 (20.8%) | 93,195 (21.7%) | 82,552 (20.3%) | 84,945 (20.7%) | |
| 70- 79 | 110,667 (26.5%) | 131,076 (27.3%) | 119,986 (27.9%) | 110,187 (27.1%) | 100,455 (24.5%) | |
| >80 | 132,091 (31.6%) | 156,064 (32.5%) | 118,961 (27.7%) | 132,808 (32.7%) | 121,203 (29.5%) | |
| Gender | 0.001 | |||||
| Male | 196,760 (47.1%) | 234,189 (48.8%) | 216,569 (50.4%) | 206,657 (50.9%) | 199,191 (48.5%) | |
| Female | 220,903 (52.9%) | 245,363 (51.2%) | 212,731 (49.6%) | 199,531 (49.1%) | 211,502 (51.5%) | |
| Race | ||||||
| White | 275,893 (66.1%) | 331,997 (69.2%) | 299,218 (69.7%) | 306,890 (75.6%) | 331,392 (80.7%) | |
| Black/African American | 24,405 (5.8%) | 26,635 (5.6%) | 24,129 (5.6%) | 37,294 (9.2%) | 25,577 (6.2%) | |
| American Indian/Alaskan Native | 409 (0.1%) | 1,054 (0.2%) | 1,750 (0.4%) | 539 (0.1%) | 1,300 (0.3%) | |
| Asian | 4,898 (1.2%) | 5,609 (1.2%) | 2,681 (0.6%) | 4,654 (1.1%) | 1,941 (0.5%) | |
| Native Hawaiian/Pacific Islander | 106 (0.0%) | 479 (0.1%) | 862 (0.2%) | 2,540 (0.6%) | ||
| Other | 3,293 (0.8%) | 4,849 (1.0%) | 6,468 (1.5%) | 8,447 (2.1%) | 7,123 (1.7%) | |
| Multiple Races | 228 (0.1%) | 412 (0.1%) | 315 (0.1%) | 321 (0.1%) | ||
| Not Stated | 108,431 (26.0%) | 108,929 (22.7%) | 93,780 (21.8%) | 48,049 (11.8%) | 40,499 (9.9%) | |
| Marriage Status | <0.001 | |||||
| Married | 129,715 (31.1%) | 170,658 (35.6%) | 133,682 (31.1%) | 121,761 (30.0%) | 131,023 (31.9%) | |
| Single | 27,411 (6.6%) | 41,705 (8.7%) | 24,644 (5.7%) | 27,824 (6.9%) | 27,561 (6.7%) | |
| Widowed | 67,684 (16.2%) | 76,988 (16.1%) | 62,128 (14.5%) | 55,509 (13.7%) | 52,675 (12.8%) | |
| Divorced | 16,386 (3.9%) | 23,693 (4.9%) | 18,313 (4.3%) | 17,079 (4.2%) | 19,279 (4.7%) | |
| Separated | 3,314 (0.8%) | 2,373 (0.5%) | 2,679 (0.6%) | 4,049 (1.0%) | 2,607 (0.6%) | |
| Not Stated | 173,153 (41.5%) | 164,135 (34.2%) | 187,854 (43.8%) | 179,966 (44.3%) | 177,548 (43.2%) | |
| Region | <0.001 | |||||
| Northeast | 102,215 (24.5%) | 118,799 (24.8%) | 112,595 (26.2%) | 127,094 (31.3%) | 96,654 (23.5%) | |
| Midwest | 110,997 (26.6%) | 118,194 (24.6%) | 90,604 (21.1%) | 77,054 (19.0%) | 96,314 (23.5%) | |
| South | 140,513 (33.6%) | 144,869 (30.2%) | 156,072 (36.4%) | 152,000 (37.4%) | 165,745 (40.4%) | |
| West | 63,938 (15.3%) | 97,690 (20.4%) | 70,029 (16.3%) | 50,040 (12.3%) | 51,980 (12.7%) | |
| Ischemic heart disease | 105,839 (25.3%) | 122,870 (25.6%) | 109,629 (25.5%) | 88,869 (21.9%) | 112,444 (27.4%) | 0.119 |
| Ventricular arrhythmias | 11,926 (2.9%) | 11,382 (2.4%) | 11,595 (2.7%) | 9,928 (2.4%) | 10,842 (2.6%) | 0.962 |
| Left bundle branch block | 7,080 (1.7%) | 6,912 (1.4%) | 6,382 (1.5%) | 4,662 (1.1%) | 9,364 (2.3%) | 0.133 |
| Complete AV block | 1,263 (0.3%) | 1,795 (0.4%) | 1,512 (0.4%) | 261 (0.1%) | 661 (0.2%) | 0.065 |
| Heart Failure | 88,285 (21.1%) | 98,665 (20.6%) | 101,429 (23.6%) | 95,091 (23.4%) | 107,955 (26.3%) | 0.076 |
| Peripheral vascular disease | 13,445 (3.2%) | 16,169 (3.4%) | 16,234 (3.8%) | 15,593 (3.8%) | 16,907 (4.1%) | 0.732 |
| Hypertension | 201,879 (48.3%) | 228,497 (47.6%) | 184,988 (43.1%) | 177,376 (43.7%) | 202,625 (49.3%) | <0.001 |
| Chronic pulmonary diseases | 71,677 (17.2%) | 74,168 (15.5%) | 59,294 (13.8%) | 57,324 (14.1%) | 77,870 (19.0%) | 0.012 |
| Diabetes | 67,310 (16.1%) | 90,092 (18.8%) | 71,953 (16.8%) | 75,602 (18.6%) | 80,427 (19.6%) | 0.120 |
| Chronic kidney disease | 21,434 (5.1%) | 10,214 (2.1%) | 9,461 (2.2%) | 10,063 (2.5%) | 13,297 (3.2%) | <0.001 |
| Anemia | 23,809 (5.7%) | 24,379 (5.1%) | 21,801 (5.1%) | 20,608 (5.1%) | 41,857 (10.2%) | <0.001 |
| Pulmonary circulation disorders | 7,837 (1.9%) | 11,262 (2.3%) | 11,291 (2.6%) | 13,571 (3.3%) | 20,436 (5.0%) | <0.001 |
| Paralysis | 5,821 (1.4%) | 6,854 (1.4%) | 3,707 (0.9%) | 4,431 (1.1%) | 7,113 (1.7%) | 0.467 |
| Valvular diseases | 73,627 (17.6%) | 67,825 (14.1%) | 52,666 (12.3%) | 43,172 (10.6%) | 72,117 (17.6%) | <0.001 |
| Other neurologic disorders | 15,420 (3.7%) | 19,009 (4.0%) | 14,958 (3.5%) | 12,023 (3.0%) | 20,615 (5.0%) | 0.360 |
| Hypothyroidism | 35,428 (8.5%) | 49,198 (10.3%) | 44,580 (10.4%) | 37,443 (9.2%) | 46,300 (11.3%) | <0.001 |
| Liver disease | 2,668 (0.6%) | 2,804 (0.6%) | 3,245 (0.8%) | 2,972 (0.7%) | 3,039 (0.7%) | 0.721 |
| PUD | 4,445 (1.1%) | 4,592 (1.0%) | 1,194 (0.3%) | 851 (0.2%) | 6,700 (1.6%) | 0.058 |
| AIDS | 23 (0.0%) | 722 (0.2%) | 212 (0.0%) | |||
| Lymphoma | 2,875 (0.7%) | 1,704 (0.4%) | 2,261 (0.5%) | 1,244 (0.3%) | 8,271 (2.0%) | 0.001 |
| Metastatic cancer | 4,888 (1.2%) | 4,369 (0.9%) | 6,229 (1.5%) | 2,035 (0.5%) | 4,339 (1.1%) | 0.048 |
| Solid tumor without mets | 21,401 (5.1%) | 31,180 (6.5%) | 27,538 (6.4%) | 17,502 (4.3%) | 38,954 (9.5%) | 0.002 |
| Collagen vascular diseases | 5,898 (1.4%) | 8,127 (1.7%) | 5,302 (1.2%) | 4,997 (1.2%) | 7,035 (1.7%) | 0.367 |
| Coagulopathy | 9,463 (2.3%) | 10,435 (2.2%) | 6,529 (1.5%) | 11,380 (2.8%) | 13,045 (3.2%) | 0.014 |
| Obesity | 28,898 (6.9%) | 22,816 (4.8%) | 24,615 (5.7%) | 19,607 (4.8%) | 39,063 (9.5%) | <0.001 |
| Weight loss | 2,339 (0.6%) | 3,143 (0.7%) | 4,166 (1.0%) | 2,258 (0.6%) | 4,060 (1.0%) | 0.520 |
| Fluid and electrolyte disorders | 51,793 (12.4%) | 57,011 (11.9%) | 51,297 (11.9%) | 50,009 (12.3%) | 74,275 (18.1%) | <0.001 |
| Alcohol abuse | 15,637 (3.7%) | 12,864 (2.7%) | 14,500 (3.4%) | 11,342 (2.8%) | 15,230 (3.7%) | 0.007 |
| Drug abuse | 2,235 (0.5%) | 3,377 (0.7%) | 1,344 (0.3%) | 1,785 (0.4%) | 4,485 (1.1%) | 0.138 |
| Depression | 15,725 (3.8%) | 19,884 (4.1%) | 16,654 (3.9%) | 11,200 (2.8%) | 27,399 (6.7%) | <0.001 |
| Psychosis | 5,304 (1.3%) | 6,449 (1.3%) | 4,222 (1.0%) | 2,966 (0.7%) | 5,670 (1.4%) | 0.515 |
| Smoking (other tobacco use) | 27,183 (6.5%) | 32,694 (6.8%) | 34,151 (8.0%) | 29,009 (7.1%) | 70,264 (17.1%) | <0.001 |
3.1. Number of AF hospitalizations
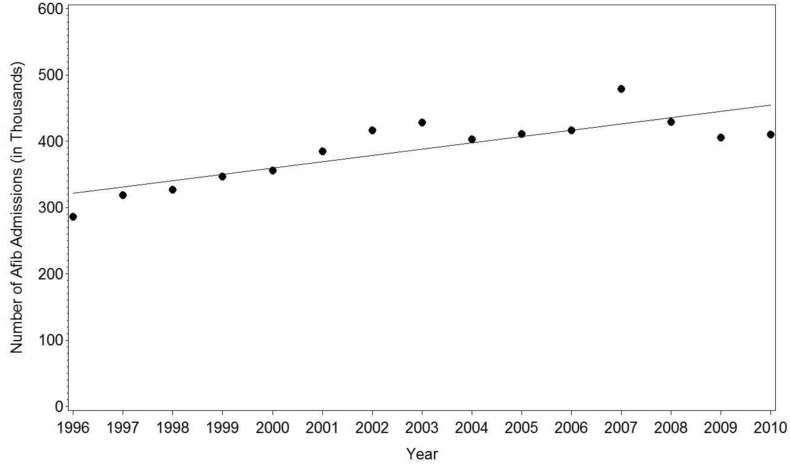
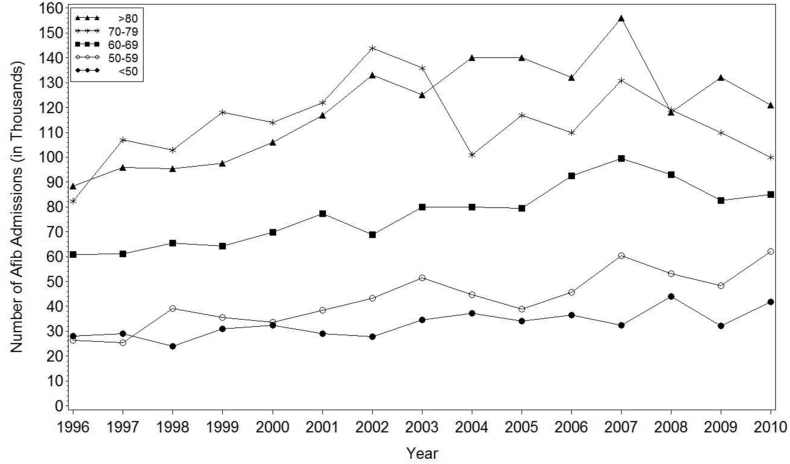
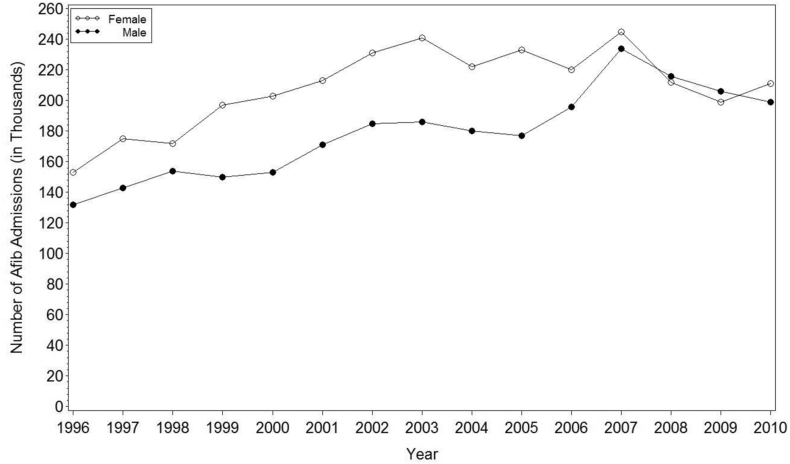
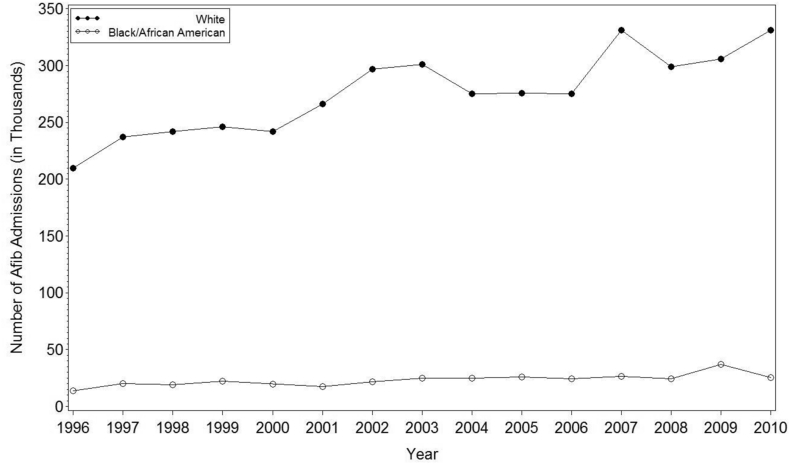
The total number of hospitalizations due to AF steadily increased from 286,362 in 1996 to a peak of 479,552 in 2007, before decreasing to 410,693 in 2010. These numbers reflect a trend of increase in the number of hospitalizations with primary diagnosis of AF over time (β = 9470 hospitalizations per year, 95% CI (5,645, 13,296), p < 0.001; see Fig. 1). This is generally reflective of an increase in AF hospitalization across all age groups (Fig. 2), both genders (Fig. 3), and various racial groups (Fig. 4).
Fig. 1.
Total Number of Hospital Admissions with a Primary Diagnosis of AF from 1996 to 2010.
Weighted Least Squares Regression:
(in Thousands) Slope, (in Thousands) Slope: 9.46, 95% CI: (5.65, 13.27), p-value: 0.0001.
(Total) Slope, (Total) Slope: 9, 470, 95% CI: (5,645, 13,296), p-value: 0.0001.
Fig. 2.
Number of hospital admissions with a primary diagnosis of AF by age groups from 1996 to 2010.
Fig. 3.
Number of hospital admissions with a primary diagnosis of AF by sex from 1996 to 2010.
Fig. 4.
Number of hospital admissions with a primary diagnosis of AF by race from 1996 to 2010.
3.2. Length of stay and inpatient mortality during AF hospitalizations
Between 1996 and 2010, the mean length of stay for hospitalizations with a primary diagnosis of AF was relatively stable (β = 0.002 days per year, 95% CI (−0.033, 0.037), p = 0.884. The mean length of stay was 3.66 days in 1996 and 3.82 days in 2010, with a peak of 4.48 days in 1997.
Over the same sampling period, the inpatient mortality rate for patients with a primary diagnosis of AF was also stable (β = 0.031% per year, 95% CI (−0.02, 0.08), p = 0.181. The inpatient mortality rate was 0.86% in 1996 and 1.64% in 2010, with a peak of 1.81% in 2004.
4. Discussion
Our data demonstrate a significant increase in AF admissions from 1996 to 2010 across all patient demographics. AF LOS and inpatient mortality were, however, relatively stable. Our findings are consistent with some earlier studies that have shown similar trend of increased AF admissions over time [5] [9]. Using data from Nationwide Inpatient Survey, Patel et al. found that AF hospitalizations increased by 23% from 2000 to 2010, albeit in that study, the increased rates were primarily seen in patients older than 65 years of age [5]. This is in contrast to our study which has shown uniform increase in AF hospitalizations across all age groups. In a previous study published on national US data by Arowolaju et al. there was a trend towards reduced AF admissions and increased inpatient mortality in patients admitted with AF [10]. It is pertinent to point out that Arowolaju et al. included patients with both primary and secondary diagnosis of AF whereas our analysis was strictly limited to primary AF hospitalizations. By including only primary AF hospitalizations, our study has focused on resource utilizations that could only be attributed to AF rather than to other diagnoses.
Recent advances in minimally invasive AF related procedures such as AF ablation, atrio-ventricular nodal ablation with pacemaker implantation etc., which have shown to benefit patients across various demographics [11] [12] [13], may have led to increased rates of AF related hospitalization. Moreover, many patients with AF require anti-coagulation to prevent thromboembolic events. Till 2010, the only option for oral anticoagulation in the US was warfarin, which often required inpatient hospital admission especially when bridging with heparin is required, thus potentially contributing to higher rates of AF hospitalizations. With the introduction of new oral anti-coagulation agents in the US market which often do not require heparin bridging, these trends may change over time.
In the present analysis, we report a significantly low incidence of AF admissions in African-American patients compared to other racial and ethnic groups, which is consistent with earlier studies [14] [15] [16]. This could be reflective of a true low incidence of AF in this sub-group or may also be indicative of a lower ability to detect AF in African-Americans due to reduced access to health care [17]. Unfortunately this is entirely speculative and cannot be assessed with present dataset.
4.1. Limitations
The NHDS is a large administrate claims based database which utilizes ICD-9 codes to identify diseases and comorbid conditions. These codes are susceptible to error during the coding process. The hard clinical points such as death and LOS, however, are less prone to error. Individual patient entry is represented as a separate patient data with no data for readmission and disease progression in the same patient. Also, the dataset lacks details regarding the type, severity and duration of AF. AF is often associated with other cardiovascular events such as stroke and heart failure and there is no relevant clinical information available in NHDS that could differentiate between these disease processes. Thus, coders may use these co-existing conditions as primary diagnosis, which could result in underestimation of AF from this dataset. NHDS is a population-based survey which was designed to analyze prevalence and trends of various disease processes necessitating inpatient care. The dataset does not collect information on treatment given in a particular inpatient admission which is another limitation. Furthermore, important echocardiographic parameters such as left atrial and ventricular dimensions and ejection fraction which predict AF recurrence and subsequent inpatient care cannot unfortuntely be examined through present dataset.
5. Conclusion
Our data suggest increased temporal trend in AF hospitalizations. Efforts to reduce the economic burden of AF should be directed towards reducing the number of hospitalizations and readmissions especially in patients with less severe AF and at the same time decreasing the LOS in those patients in whom hospitalization cannot be avoided.
Source of funding
None.
Disclosures
None.
Footnotes
Peer review under responsibility of Indian Heart Rhythm Society.
References
- 1.Stewart S., Hart C.L., Hole D.J., McMurray J.J. Population prevalence, incidence, and predictors of atrial fibrillation in the Renfrew/Paisley study. Heart. 2001;86:516–521. doi: 10.1136/heart.86.5.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilke T., Groth A., Mueller S. Incidence and prevalence of atrial fibrillation: an analysis based on 8.3 million patients. Europace. 2013;15:486–493. doi: 10.1093/europace/eus333. [DOI] [PubMed] [Google Scholar]
- 3.Naccarelli G.V., Varker H., Lin J., Schulman K.L. Increasing prevalence of atrial fibrillation and flutter in the United States. Am J Cardiol. 2009;1:1534–1539. doi: 10.1016/j.amjcard.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 4.Chugh S.S., Blackshear J.L., Shen W.K., Hammill S.C., Gersh B.J. Epidemiology and natural history of atrial fibrillation: clinical implications. J Am Coll Cardiol. 2001;37:371–378. doi: 10.1016/s0735-1097(00)01107-4. [DOI] [PubMed] [Google Scholar]
- 5.Patel N.J., Deshmukh A., Pant S. Contemporary trends of hospitalization for atrial fibrillation in the United States, 2000 through 2010: implications for healthcare planning. Circulation. 2014;10(129):2371–2379. doi: 10.1161/CIRCULATIONAHA.114.008201. [DOI] [PubMed] [Google Scholar]
- 6.Coyne K.S., Paramore C., Grandy S., Mercader M., Reynolds M., Zimetbaum P. Assessing the direct costs of treating nonvalvular atrial fibrillation in the United States. Value Health. 2006;9:348–356. doi: 10.1111/j.1524-4733.2006.00124.x. [DOI] [PubMed] [Google Scholar]
- 7.Ford E.S., Roger V.L., Dunlay S.M., Go A.S., Rosamond W.D. Challenges of ascertaining national trends in the incidence of coronary heart disease in the United States. J Am Heart Assoc. 2014;3:e001097. doi: 10.1161/JAHA.114.001097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dennison C., Pokras R. Design and operation of the national hospital discharge survey: 1988 redesign. Vital Health Stat. 2000;1:39. [PubMed] [Google Scholar]
- 9.Wattigney W.A., Mensah G.A., Croft J.B. Increasing trends in hospitalization for atrial fibrillation in the United States, 1985 through 1999. Circulation. 2003;108:711–716. doi: 10.1161/01.CIR.0000083722.42033.0A. [DOI] [PubMed] [Google Scholar]
- 10.Arowolaju A., 2nd, Gillum R.F. A new decline in hospitalization with atrial fibrillation among the elderly. Am J Med. 2013;126:455–457. doi: 10.1016/j.amjmed.2012.10.023. [DOI] [PubMed] [Google Scholar]
- 11.Kneeland P.P., Fang M.C. Trends in catheter ablation for atrial fibrillation in the United States. J Hosp Med. 2009;4:E1–E5. doi: 10.1002/jhm.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ellis E.R., Culler S.D., Simon A.W., Reynolds M.R. Trends in utilization and complications of catheter ablation for atrial fibrillation in Medicare beneficiaries. Heart Rhythm. 2009;6:1267–1273. doi: 10.1016/j.hrthm.2009.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deshmukh A., Patel N.J., Pant S. In-hospital complications associated with catheter ablation of atrial fibrillation in the United States between 2000 and 2010: analysis of 93 801 procedures. Circulation. 2013;5:2104–2112. doi: 10.1161/CIRCULATIONAHA.113.003862. [DOI] [PubMed] [Google Scholar]
- 14.Alonso A., Agarwal S.K., Soliman E.Z. Incidence of atrial fibrillation in whites and African-Americans: the atherosclerosis risk in communities (ARIC) study. Am Heart J. 2009;158:111–117. doi: 10.1016/j.ahj.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khairallah F., Ezzedine R., Ganz L.I., London B., Saba S. Epidemiology and determinants of outcome of admissions for atrial fibrillation in the United States from 1996 to 2001. Am J Cardiol. 2004;94:500–504. doi: 10.1016/j.amjcard.2004.04.068. [DOI] [PubMed] [Google Scholar]
- 16.Upshaw C.B., Jr. Reduced prevalence of atrial fibrillation in black patients compared with white patients attending an urban hospital: an electrocardiographic study. J Natl Med Assoc. 2002;94:204–208. [PMC free article] [PubMed] [Google Scholar]
- 17.Garrido T., Kanter M., Meng D. Race/ethnicity, personal health record access, and quality of care. Am J Manag Care. 2015;21:e103–e113. [PubMed] [Google Scholar]