Abstract
Whether mindfulness training (MT) could improve healthy behaviors is unknown. This study sought to determine feasibility and acceptability of integrating MT into school-based health education (primary outcomes) and to explore its possible effects on healthy behaviors (exploratory outcomes). Two high schools in Massachusetts (2014–2015) were randomized to health education plus MT (HE-MT) (one session/week for 8 weeks) or to health education plus attention control (HE-AC). Dietary habits (24-h dietary recalls) and moderate-to-vigorous physical activity (MVPA/7-day recalls) were assessed at baseline, end of treatment (EOT), and 6 months thereafter. Quantile regression and linear mixed models were used, respectively, to estimate effects on MVPA and dietary outcomes adjusting for confounders. We recruited 53 9th graders (30 HEM, 23 HEAC; average age 14.5, 60% white, 59% female). Retention was 100% (EOT) and 96% (6 months); attendance was 96% (both conditions), with moderate-to-high satisfaction ratings. Among students with higher MVPA at baseline, MVPA was higher in HE-MT vs. HE-AC at both EOT (median difference = 81 min/week, p = 0.005) and at 6 months (p = 0.004). Among males, median MVPA was higher (median difference = 99 min/week) in HE-MT vs. HEAC at both EOT (p = 0.056) and at 6 months (p = 0.04). No differences were noted in dietary habits. In sum, integrating school-based MT into health education was feasible and acceptable and had promising effects on MVPA among male and more active adolescents. These findings suggest that MT may improve healthy behaviors in adolescents and deserve to be reproduced in larger, rigorous studies.
Keywords: School-based interventions, Adolescents, Mindfulness, Diet, Physical activity, Prevention
Highlights
-
•
Integrating mindfulness training into high school health education is feasible.
-
•
The program is scalable because health education is commonly taught in US schools.
-
•
Larger studies are needed to establish its efficacy on health behaviors.
1. Introduction
Unhealthy diets and physical inactivity are modifiable risk factors for the development of cardiovascular disease, the principal cause of death in the United States and worldwide (Benjamin et al., 2017). Both behaviors have been linked with the early development of atherosclerosis (Raitakari et al., 2003) and are highly prevalent among adolescents (Benjamin et al., 2017). Since developing healthy dietary and exercise habits in youth leads to significant health benefits in adulthood, it is of primary importance to develop programs aimed at establishing such behaviors early in life (Daniels et al., 2011). Endeavors in this direction, however, have been unsuccessful and have produced only modest and transitory effects (Gonzalez-Suarez et al., 2009). Typically, adolescents underestimate the long-term consequences of unhealthy behaviors (Whalen et al., 1994) and may be reluctant to engage in preventive behaviors for which they do not see any immediate benefit.
Mindfulness training (MT), a behavioral approach aiming at the cultivation of a particular way of paying attention (on purpose and non-judgmentally) (Kabat-Zinn, 1990) to the moment-to-moment experience of mental events and physical sensations, has great potential for improving healthy behaviors by increasing the capacity for attentional and emotional self-regulation (Shapiro et al., 2006; Carmody, 2009). Evidence from observational studies suggests, in fact, that individuals who are more mindful tend to have healthier dietary and exercise behaviors (Roberts and Danoff-Burg, 2011; Gilbert and Waltz, 2010) and that MT can improve healthy behaviors in adults (Loucks et al., 2015; Salmoirago-Blotcher et al., 2013). The role of MT in promoting healthy behaviors in adolescents, however, has never been explored.
The goals of this study were to determine the feasibility and acceptability of integrating MT into school-based health education (primary outcome) and to explore its possible effect on exercise and dietary behaviors (exploratory outcomes).
2. Materials and methods
This pilot study (Clinicaltrials.gov NCT01975896) was conducted in two high schools in central Massachusetts (2014–2015) offering health education as part of their 9th grade curriculum. To be enrolled, participants had to be 9th graders and English-speaking. They were excluded if they planned to move out of the area, were unable/unwilling to provide informed assent/consent, and had a history of psychiatric conditions or developmental delay.
To avoid contamination between interventions, schools (instead of individual students) were randomized to Health Education plus MT (HE-MT) or to Health Education plus Attention Control (HE-AC). Once student assent and parental consent were obtained and eligibility confirmed, students were enrolled in the study and followed the protocol for their school condition. Students received a $20 incentive at each assessment visit. The Institutional Review Board at the University of Massachusetts Medical School approved the study protocol (Docket H-00002904).
2.1. Interventions
Interventions were delivered during the health education period at both schools. To avoid singling out, all students received study interventions but only those who provided assent/consent completed study assessments.
2.1.1. Health education (both schools)
Students received one health education session for four days/week for two consecutive weeks delivered by health education teachers at each school. The curriculum (identical for both schools) was based on the standard health education curriculum adopted in high schools in Massachusetts integrated with materials from the Diabetes Prevention Project and the American Heart Association (AHA) (Salmoirago-Blotcher et al., n.d.) and focused on increasing the intake of healthy food and reducing that of unhealthy food, eating breakfast, portion sizes, engaging in at least 1 h of moderate-to-vigorous physical activity (MVPA) every day, and reducing sedentary behavior.
2.1.2. Mindfulness training (HE-MT school)
Students received one 45-min session of MT per week for 8 weeks, led by a certified mindfulness instructor. The curriculum was based on the widely known Mindfulness-Based Stress Reduction program, modified to meet the needs of adolescents (Prince et al., 2011). Students were trained to cultivate attention to bodily and breathing sensations, sounds, visual objects, thoughts, and emotions; to learn noticing which events the attention was spontaneously drawn to from moment to moment; and to practice mindful movement exercises (walking and standing yoga). Students also listened to a 15-min digitally recorded guided mindfulness practice in class every day during non-session days and were encouraged to listen to the recording on their own at least once daily throughout the duration of the intervention.
2.1.3. Attention control (HE-AC school)
Students received one “attention control” session/week for 8 weeks. The curriculum focused on topics such as wellness, health risk factors, mental and emotional health, self-esteem, and resiliency.
2.2. Intervention Fidelity
Mindfulness instructors digitally recorded each session and 10% of recordings were randomly audited. A checklist was used by health education teachers to ensure all planned topics were discussed (Bellg et al., 2004).
2.3. Study assessments
Assessments were performed at baseline, end of treatment (EOT) and 6-month thereafter (end of the academic year). With the exception of diet and physical activity, assessments were conducted at school using Research Electronic Data capture (REDCap) technology. Data management and analysis personnel were blinded to school allocation; the research assistant was blinded to the study outcomes.
2.3.1. Primary outcomes
Feasibility metrics included retention rates, class attendance, and intervention adherence (number of times/week participants listened to the study recording, assessed via a self-reported mindfulness log). Acceptability was assessed using a program satisfaction survey (ratings ranged from 1-not at all to 5-very much).
2.3.2. Exploratory outcomes
The 7 day physical activity recall (PAR), (Blair et al., 1985) conducted by trained personnel via phone interviews, was used to measure MVPA in minutes/week. Dietary measures included key components of AHA dietary recommendations such as intake of fruits and vegetables, sodium, fish, and sugar-sweetened beverages (Gidding et al., 2005) assessed via 24-h phone dietary recall (Interactive Nutrition Data System, University of Minnesota, Minneapolis, MN) conducted by trained assessors on a randomly selected day of the week.
2.3.3. Covariates
Age, gender, ethnicity, and socio-economic status were self-reported at baseline. Body mass index (BMI - weight (kg)/height squared (meters)) was calculated from direct measurements of weight and height; BMI percentiles for age/sex were determined using CDC growth charts. Perceived parental control on dietary habits, healthy food availability, and PA was assessed using a questionnaire based on the Parental Control Index (Johnson and Birch, 1994). Depression was measured using a validated 6-item measure of depressive mood with scores ranging from 10 to 30 (Kandel and Davies, n.d.).
2.4. Sample size
Sample size was estimated based on retention rates, a key aspect of feasibility. Based on estimates from previous studies, the design effect is 1 + (0.027 × 1.5 × (20−1) = 1.77. For a minimum nominal per-school sample size of 23 – corresponding to an effective per-school sample size of 23/1.77 = 13 – and an anticipated 95% retention rate based on our prior studies, a conservative projected 95% confidence interval for per-condition (school) retention rate was (67.6%, 100%).
2.5. Statistical analysis
Analyses were performed according to the intention to treat approach. Retention, attendance, adherence as well as acceptability scores at EOT and 6 months of follow-up were calculated separately for each condition. For exploratory outcomes, interest was in obtaining estimates of effect rather than in hypothesis testing. As physical activity outcomes are subject to high variability, particularly in small samples, quantile regression (which models the median outcome at follow-up in lieu of the mean) was used, controlling for baseline values of MVPA and potential confounders (gender, parental control, depressive symptoms, race, and socio-economic status). One significant outlier with respect to baseline MVPA was removed from subsequent analyses. As there was substantial variability in baseline MVPA models also included interactions between group and baseline activity. Finally, we explored potential moderating effects of gender on MVPA, using a similar approach.
Linear mixed models were used to estimate effects on dietary outcome Models included random effect for class and adjusted for baseline value of the outcome and the same potential confounders as mentioned above.
3. Results
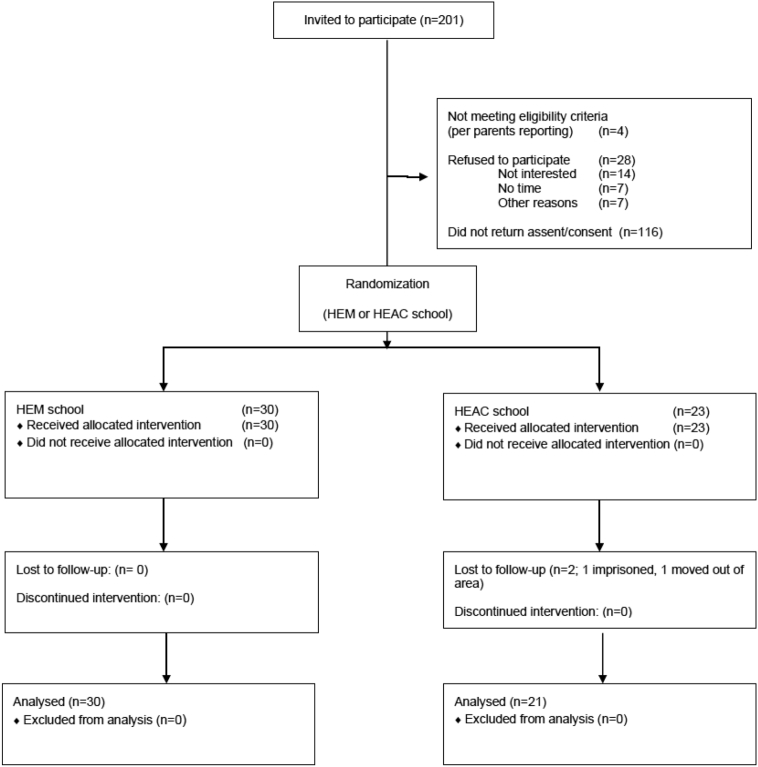
Among 201 students invited to participate, 53 (26.4%) provided assent/consent and were enrolled in the study (30 HE-MT, 23 HE-AC) (Fig. 1). Baseline characteristics were similar between groups (Table 1). Overall, <40% of study participants met AHA recommendations for adolescent physical activity (≥ 60 min of MVPA/day) and only one adolescent met AHA dietary recommendations.
Fig. 1.
CONSORT flow diagram.
HE-MT = Health Education + Mindfulness Training.
HE-AC = Health Education + Attention Control.
Central Massachusetts, 2014–2015.
Table 1.
Baseline characteristics by school allocationa.
| HE-MT school n = 30 |
HE-AC school n = 23 |
|
|---|---|---|
| Age (mean (SD)) | 14.6 (0.3) | 14.5 (0.4) |
| Female | 21 (70%) | 10 (43.5%) |
| Hispanic | 9 (30%) | 11 (47.8%) |
| White | 20 (66.7%) | 12 (52.2%) |
| Black/African American | 1 (3.3%) | 0 (0%) |
| American Indian/Alaskan Native | 1 (3.3%) | 0 (0%) |
| Other | 4 (13.3%) | 5 (21.7%) |
| Multiple races | 4 (13.3%) | 6 (26.1%) |
| BMI for age percentile (mean (SD)) | 66.5 (30.8) | 69.4 (31.3) |
| Meeting AHA MVPA recommendationsb | 13 (43.3%) | 8 (34.8%) |
| Meeting AHA dietary recommendationsc | 1 (3.3%) | 0 (0%) |
| Children depression inventory (mean (SD)) | 23.9 (3.9) | 23.1 (3.9) |
Central Massachusetts, 2014–2015.
BMI = Body Mass Index.
MVPA = Moderate-to-vigorous physical activity.
AHA = American Heart Association
HE-AC = Health education + attention control.
HE-MT = Health education + mindfulness training.
Values are n (%) unless otherwise indicated.
≥60 min of MVPA/day.
AHA dietary scores >3. Ideal = scores 4–5; intermediate = 2–3; poor = 0–1.
3.1. Primary outcomes
Retention at intervention completion and at 6 months of follow-up was 100% and 98%, respectively. Class attendance was 96% in both conditions. HE-MT students reported listening to the recording on their own 5 (SD 2.9) times/week. >90% of students were “somewhat to very satisfied” with the health education intervention and 77% were ‘somewhat to very satisfied’ with the mindfulness program. No adverse effects were reported during the study.
3.2. Exploratory outcomes
Baseline median MVPA in the overall population was 283 min/week (range, 0 to 1265 min), with no differences between groups (p = 0.43). Among those with higher baseline MVPA, median MVPA at EOT was higher in the HE-MT compared to the HE-AC condition (difference in median MVPA at EOT of 81 min, p = 0.005). This effect was maintained at 6 months of follow-up (p = 0.004). Exploratory analyses by gender suggested that among males, median MVPA for HE-MT was higher at EOT compared to controls, particularly among those with higher levels of baseline MVPA (p = 0.056). These associations were maintained 6 months after EOT (p = 0.04), with a difference in median MVPA of 99 min/week in favor of HE-MT.
We did not observe differences in the intake of fruit and vegetables, sodium, and sweetened beverages at EOT (p = 0.72, 0.88, and 0.29, respectively) and at 6 months of follow-up (p = 0.19, 0.97, and 0.42, respectively). Only one participant reported to eat fish during the study and analyses for this nutrient were not conducted.
4. Discussion
This is the first study examining the feasibility and possible effect of a MT program integrated into health education on healthy behaviors in adolescents. This approach was feasible and acceptable to a large majority of students. MT also improved MVPA at EOT especially among male and more active adolescents, which was maintained at 6 months of follow-up, while no significant differences were observed in dietary behaviors.
Findings on MVPA are promising and even more relevant if we consider that all students (and not only physically inactive ones) were included in the study, likely producing a ceiling effect. It is noteworthy that effects were more pronounced among more active adolescents and among males. This finding is perhaps not surprising given that PA improves proprioception, which is also one of the focuses of MT (i.e., via practices directing attention to body sensations and to the entire body). More active adolescents may be more aware of their bodies and somewhat “primed” to mindfulness practice.
The lack of effect on dietary habits could be explained by a number of factors. First, due to budgetary constraints, we were able to conduct only one 24-h dietary recall (vs. the recommended three) at each time-point, which likely did not adequately capture dietary habits. In addition, the study was conducted in winter when fruits and vegetables prices are higher, a fact that might have limited the availability of fruits and vegetables among our low-income students.
Notable strengths of this study include its ethnically diverse population, the use of an attention control condition, and the integration of MT into school health education classes with the advantage of not imposing transportation burdens on students and their families to receive MT outside of regular school hours. We also acknowledge a number of limitations of this study, including its small sample size, the involvement of only two schools, and the use of self-reported assessments of MVPA.
Findings from this study need to be reproduced in larger studies involving schools from different geographic areas. Such studies should also use objective assessments of physical activity (e.g., accelerometry) and employ alternative strategies (e.g., on-line dietary recalls, which can be easily administered via computer interface) to improve the collection of dietary information.
In conclusion, integrating MT into existing health education classes was feasible and acceptable and showed promising effects on exercise behaviors. Because health education is taught in >60% of high schools in the US, (Brener et al., 2011) this approach – if proven effective – could be easily disseminated across schools. The availability of qualified MT instructors is increasing nationwide (see, for example, http://www.mindfulschools.org/resources/directory/) and thus access to MT will likely become easier and cheaper in the future. Alternatively, if this approach is proven effective, health education teachers could be trained to deliver MT to students.
Funding
This project was funded by a grant (R21HL119665) from the National Heart, Lung, and Blood Institute (NHLBI) to Drs. Pbert and Salmoirago-Blotcher. The funding source had no involvement in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Conflict of interest
Drs. Pbert and Salmoirago-Blotcher report grants (R21HL119665) from the National Heart, Lung, and Blood Institute, National Institutes of Health, during the conduct of the study; SD, FFM, CF, and SC have no competing interests to declare.
Acknowledgments
The authors wish to thank the health educators at each school and the mindfulness instructor, Ms. Leslie Smith Frank, for their collaboration on this study.
References
- Bellg A., Borrelli B., Resnick B. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH behavior change consortium. Health Psychol. 2004;23:443–451. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- Benjamin E.J., Blaha M.J., Chiuve S.E. Heart disease and stroke Statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135:e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair S.N., Haskell W.L., Ho P. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am. J. Epidemiol. 1985;122 doi: 10.1093/oxfordjournals.aje.a114163. (794-04) [DOI] [PubMed] [Google Scholar]
- Brener N., Demissie Z., Foti K. Atlanta: Centers for Disease Control and Prevention; 2011. School Health Profiles 2010: Characteristics of Health Programs Among Secondary Schools. [Google Scholar]
- Carmody J. Evolving conceptions of mindfulness in clinical settings. J. Cogn. Psychother. 2009;23:270–280. [Google Scholar]
- Daniels S.R., Pratt C.A., Hayman L.L. Reduction of risk for cardiovascular disease in children and adolescents. Circulation. 2011;124:1673–1686. doi: 10.1161/CIRCULATIONAHA.110.016170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gidding S.S., Dennison B.A., Birch L.L. Dietary recommendations for children and adolescents: a guide for practitioners: consensus statement from the American Heart Association. Circulation. 2005;112:2061–2075. doi: 10.1161/CIRCULATIONAHA.105.169251. [DOI] [PubMed] [Google Scholar]
- Gilbert D., Waltz J. Mindfulness and health behaviors. Mindfulness. 2010;1:227–234. [Google Scholar]
- Gonzalez-Suarez C., Worley A., Grimmer-Somers K., Dones V. School-based interventions on childhood obesity: a meta-analysis. Am. J. Prev. Med. 2009;37:418–427. doi: 10.1016/j.amepre.2009.07.012. [DOI] [PubMed] [Google Scholar]
- Johnson S.L., Birch L.L. Parents' and children's adiposity and eating style. Pediatrics. 1994;94:653–661. [PubMed] [Google Scholar]
- Kabat-Zinn J. Dell Publishing; New York: 1990. Full Catastrophe Living: Using the Wisdom of your Body and Mind to Face Stress, Pain, and Illness. [Google Scholar]
- Kandel DB, Davies M. Epidemiology of depressive mood in adolescents: an empirical study. Arch. Gen. Psychiatry 39: 1205–12. [DOI] [PubMed]
- Loucks E.B., Britton W.B., Howe C.J., Eaton C.B., Buka S.L. Positive associations of dispositional mindfulness with cardiovascular health: the New England family study. Int. J. Behav. Med. 2015;22:540–550. doi: 10.1007/s12529-014-9448-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince J., Roberts M., Howland J., Thomson I., Meleo-Meyer F. 9th Annual International Mindfulness Conference of the Center for Mindfulness in Medicine, Health Care, and Society. Norwood, MA. 2011. A pilot investigation of Cool Minds: A mindfulness based stress reduction program for teens. [Google Scholar]
- Raitakari O., Juonala M., Khn M. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the cardiovascular risk in young finns study. JAMA. 2003;290:2277–2283. doi: 10.1001/jama.290.17.2277. [DOI] [PubMed] [Google Scholar]
- Roberts K.C., Danoff-Burg S. Mindfulness and health behaviors: is paying attention good for you? J. Am. Coll. Heal. 2011;59:165–173. doi: 10.1080/07448481.2010.484452. [DOI] [PubMed] [Google Scholar]
- Salmoirago-Blotcher E., Hunsinger M., Morgan L., Fischer D., Carmody J. Mindfulness-based stress reduction and change in health-related behaviors. J. Evid. Based Complement. Alternat. Med. 2013;18:243–247. [Google Scholar]
- Salmoirago-Blotcher E, Druker S, Meyer F, Bock B, Crawford S, Pbert L. Design and methods for "Commit to Get Fit" - A pilot study of a school-based mindfulness intervention to promote healthy diet and physical activity among adolescents. Contemp. Clin. Trials 41: 248–58. [DOI] [PMC free article] [PubMed]
- Shapiro S.L., Carlson L.E., Astin J.A., Freedman B. Mechanisms of mindfulness. J. Clin. Psychol. 2006;62:373–386. doi: 10.1002/jclp.20237. [DOI] [PubMed] [Google Scholar]
- Whalen C.K., Henker B., O'Neil R., Hollingshead J., Holman A., Moore B. Optimism in children's judgments of health and environmental risks. Health Psychol. 1994;13:319–325. doi: 10.1037//0278-6133.13.4.319. [DOI] [PubMed] [Google Scholar]