Abstract
The prevalence of food insecurity (FI) among food bank users in many European countries is unknown. The study aims to examine FI prevalence and associated population characteristics among this particular group of disadvantaged people in Germany. Food insecurity status was assessed among 1033 adult food bank users with a mean age of 53 years (57% female, 43% male) in Germany in 2015 using the food insecurity experience scale (FIES). About half of the participants (55.8%) were single with no children and born in Germany. Over 37% had a self-reported BMI of 30 kg/m2 or above and 37.4% indicated to smoke.
Over 70% of the food bank users can be described as food insecure. Of those, about 35% were considered mildly food insecure. Almost 30% were categorized as moderately food insecure while over 7% were categorized as severely food insecure. Significant associations with food insecurity were found for gender, age, subjective health status, smoking, duration of food bank use, school education and family type. Among this socially disadvantaged population, food insecurity is highly prevalent and public health efforts should be focusing on this vulnerable population taken into account the identified population and behavioral characteristics associated with food insecurity.
Keywords: Food insecurity, Food bank user, Low income
Highlights
-
•
Food insecurity (FI) is prevalent in highly developed countries.
-
•
Food bank users are a particular vulnerable group to FI.
-
•
The prevalence of FI among food bank users in Germany is high.
-
•
FI is associated with different behavioral and population characteristics.
1. Introduction
Food insecurity (FI) is described as the “limited or uncertain availability of nutritionally adequate and safe foods or limited or uncertain ability to acquire acceptable foods in socially acceptable ways” (Anderson, 1990). The rise of food insecurity is global, also affecting high-income countries such as the UK, Canada, the U.S. or Germany (FAO, 2016).
Research has shown that the path to FI often starts with the anxiety about not having enough food, followed by dietary changes to make limited food supply last longer and ending in decreased food intake (Coates et al. 2006; Radimer et al., 1990; Radimer et al., 1992;).
Thus, individuals suffering from FI do not necessarily differ in their energy intake from food secure individuals but research indicates that their consumption of fruits, vegetables and fish is lower (Bocquier et al., 2015). In general, FI seems to be correlated with poor diet quality which can be partly explained by lower daily diet costs (Bocquier et al., 2015). Food insecure individuals also appear to have a higher risk of poor health (Pruitt et al., 2016) including higher rates of obesity among women (Burns 2004; Dinour et al., 2007; Franklin et al., 2012), diabetes (Gucciardi et al., 2014), or mental disorders (Ramsey et al., 2012; Siefert et al., 2004; Vozoris and Tarasuk, 2003) than food secure individuals. Overall, FI is more prevalent among low income households (Coleman-Jensen et al., 2015; Martin-Fernandez et al., 2013; Vedovato et al., 2016) and people with low socio-economic status (Carter et al., 2012).
According to a new study comparing FI across 149 countries, 78.2% of people in North America can be described as food secure while 4.9% can be considered suffering from severe FI. In Europe, 74.3% of people are considered food secure while 3.5% are severely food insecure (6.3% with moderate FI and 16.0% with mild FI (Jones, 2017). The recent report by the Food and Agriculture Organization of the United Nations (FAO), publishing FI prevalence data for many different countries using nationally representative population samples, estimated that in Germany, 4.3% of the population are moderately and severely food insecure. However, as pointed out by the authors, this estimation was based on a sample size of <100 cases, which substantially reduces its informative value (FAO, 2016).
Foodbank data have been repeatedly used to measure FI among disadvantaged populations (Lindberg et al., 2015; Loopstra et al., 2016; Neter et al., 2014;). In the U.K., data by the Trussel Trusts's network of food banks reported that over 1.18 million people were given three-day emergency food supplies in the financial year 2016–2017 (Loopstra and Lalor, 2017). In Germany, the number of food banks has increased substantially over the last fifteen years, and it is estimated that 1.5 million people are currently benefiting from their food distribution (National Association of German Tafel, 2016).
Given the missing information on FI rates in Germany, the aim of this cross-sectional study was to examine FI prevalence among a large sample of food bank users. A second aim of the study was to determine the association of socio-demographic and health variables with FI.
2. Methods
2.1. Setting and participants
Food bank users in Germany can be described as a group of economically disadvantaged people with low- or no income, unemployment or low paid job, and a reliance on welfare assistance (Depa et al., 2015; Tinnemann et al., 2012). Adult food bank users were recruited at food banks in three different cities in Germany (Stuttgart, Berlin, Karlsruhe). To be included, food bank users had to be over the age of 18 years, be registered food bank users and be able to understand German, English, Russian or Arabic.
Depending on the type of food bank established in the according location, food bank stores and food redistribution points – also called food pantries – were visited several times between May and August of 2015 during opening hours (6–8 times at the four food bank stores in Stuttgart on varying weekdays and at different times during the month; 4 times at the redistribution point in Karlsruhe at different times during the month; 2–3 times at 8 representative redistribution points in Berlin at different times during the month). Visiting food bank users were approached by trained research personnel when entering or leaving the facilities. Research personnel introduced themselves and described their interest in studying eating behavior of food bank users. Interested users were invited to participate in the study by filling out a survey on site. Detailed written information of the study procedures as well as the university contact details were provided. Food bank users who had difficulties reading or understanding the questions were offered help filling out the questionnaire. On average, it took about 15 min to complete the self-reported questionnaire.
Food bank officials gave their permission to recruit clients. Written informed consent was not obtained from food bank users to increase participation. Many people, particularly in this population group, have a general distrust of governmental agencies and academic institutions and are hesitant to give their informed consent because they perceive this act as relinquishing rather than protecting their rights (Yancey et al. 2006). Ethical approval was obtained from the University of Hohenheim ethics committee and agreed with the Helsinki Declaration.
2.2. Questionnaires
The self-administered questionnaire included sociodemographic variables including age, gender, country of birth, school education (no graduation, graduation at 10th grade or earlier, and graduation at 12th/13th grade) and household composition (single with no children, single-parent, couple with children, couple without children, other). Questions on self-rated health status using a 5-point Likert scale from “very good” to “very bad” (How do you rate your current health?), smoking (Do you currently smoke? Yes, no), as well as on food bank visiting patterns (For how long have you been visiting a food bank? <3 months to 3–6 months, 7–12 months, over 12 months; How often do you usually visit a food bank? > 4 times/month, 4 times/months, 2–3 times/month, 1 time or less/month) were also administered. Questions regarding health status were adapted from the DEGS (German health interview and examination survey for adults; Scheidt-Nave et al., 2012) which is a valid German survey. Height and weight were self-reported. The questionnaire has also been used in previous research studies among food bank users (Depa et al., 2015; Tinnemann et al., 2012).
FI was measured using the Food Insecurity Experience Scale (FIES) provided by the FAO (Ballard et al., 2013). The FIES captures the access dimension of food security including aspects from monetary restraint and availability to dietary quality. It also allows interpreting obtained data on different levels of severity. Using an experience-based metric for the severity of the food insecurity condition, the metric is calculated from data on people's direct responses to questions about their access to food of adequate quality and quantity over the last 12 months taking into account the definition of food security as “secure access at all times to sufficient food” (Maxwell and Smith, 1992). The FIES consists of eight questions (see Table 1) and is based on the U.S. Household food Security Survey Module (US HFSSM) and also took other experience-based food insecurity scales into consideration (e.g. Household Food Insecurity Access Scale - HFIAS and the Escala, Latinoamericana y Caribena de Seguridad Alimentaria -ELCSA) (FAO, 2016). Answer options included “yes, no, refused, don't know”. The FIES is a relatively new measuring instrument, but has been used numerous times assessing FI in many different countries (Frongillo et al., 2017; Jones, 2017).
Table 1.
Question of the FIES and affirmatively answered questions by the study sample (n = 1033).
| FIES Questions: During the last 12 months, was there a time when… |
n | % |
|---|---|---|
|
480 | 46.5 |
|
510 | 49.4 |
|
622 | 60.2 |
|
312 | 30.2 |
|
408 | 39.5 |
|
182 | 17.6 |
|
208 | 20.1 |
| … you went without eating for a whole day because of a lack of money? | 117 | 11.3 |
Survey conducted between May and August of 2015 among food bank users in Germany.
The questionnaire was provided in German, English, Russian and Arabic. All questionnaires were translated by native speakers using the existing versions of the FIES survey module and the guidelines for translation of the FIES provided by the FAO considering the intended target population. The adopted questionnaires were then validated using a small sample of food bank users in Stuttgart (n = 14) by asking them to rephrase the questions in their own words as if asking a friend (validation method: paraphrasing). One major change to the original questionnaire was the elimination of the words “or other resources (than lack of money)” because some food bank users did not know what was meant by it (they thought they were being asked about stealing food).
2.3. Statistical analysis
Severity levels of FI were calculated by the FAO (Nord, 2015) based on their statistical guidelines and depended on the number of questions a participant answered affirmatively. A person who negated all eight question was judged as food secure while someone who answered one up to three questions with “yes” was defined as mildly food insecure. Four up to seven affirmed questions indicated that a participant is moderately food insecure. To be categorized as severely food insecure, a person had to affirm all eight questions. Questionnaires (n = 212) with either one answer missing or with the answer options “don't know” and “refused” were not entered into the analyses. Participants living in Germany for less than one year (we did not want to know about food insecurity prior to their arrival in Germany, (n = 116), being first time food bank visitors (n = 14) and having language barriers or cognitive impairment (n = 5) were also excluded from the analyses. Therefore, for the prevalence calculation, data of 1033 individuals out of 1380 cases were used (see Fig. 1). Cronbach's alpha coefficient was 0.878 (based on 1033 participants), showing a very good internal reliability of the FIES.
Fig. 1.
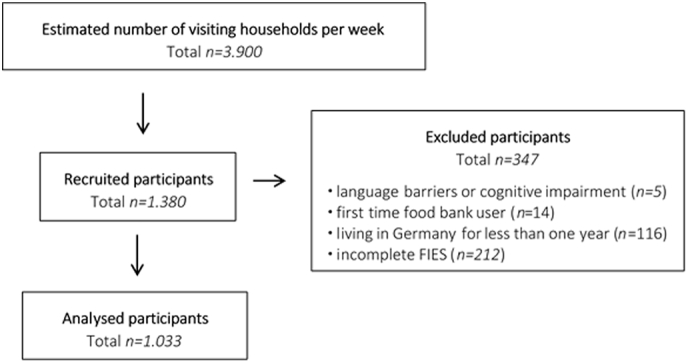
Recruited and excluded cases of food bank users in Germany.
Levels of food insecurity and participants' characteristics were examined by descriptive statistics, tables showing mean + SD and relative frequencies. Correlations between the FI levels and sociodemographic or health variables were assessed by calculating Cramer's V or Kendal's Tau b for each variable as a whole as well as across the single categories of the different variables (including Bonferroni corrections for multiple comparisons). IBM SPSS Statistics 24 was used for the analyses. Statistical significance was set at p < 0.05.
3. Results
3.1. Study sample
Fig. 1 presents the recruited and excluded cases of food bank users. With 1.380 recruited participants and an estimated 3.900 visiting households per week over all recruitment locations, the participation rate was estimated to be around 35%. Table 2 presents food bank users' demographic, health status information, and food bank use patterns. More than half of the participants were women (57%) and more than half were born in Germany (55.8%). Over one third of the participants had a school education that can be described as at or above the university entrance level (37.7%). Over 50% were single with no children. The prevalence of overweight and obesity was 68.4%. The majority of the participants rated their health as moderate or bad (65.9%). Also, the majority of the participants were weekly food bank users (68.0%) and visited food banks for more than one year (70.3%).
Table 2.
Food bank users' socio-demographic and health characteristics.
| Variable | Participants |
|---|---|
| Age in years (n = 1033, mean ± SD) | 53.1 ± 14.8 |
| Gender (n = 1033) | |
| Female | 589 (57.0%) |
| Male | 444 (43.0%) |
| Country of birth (n = 1032) | |
| Germany | 576 (55.8%) |
| Other | 456 (44.2%) |
| Highest completed education (n = 985) | |
| No graduation | 49 (5.0%) |
| Graduation at 10th grade or earlier | 565 (57.3%) |
| Graduation at 12th/13th grade (university entrance) | 371 (37.7%) |
| Household composition (n = 1002) | |
| Single, no children | 559 (55.8%) |
| Couple, no children | 142 (14.2%) |
| Couple, children | 135 (13.5%) |
| Single-parent | 82 (8.2%) |
| Other (e.g. shared living) | 84 (8.4%) |
| Body Mass Index (kg/m2, n = 887) | |
| Underweight or normal weight (BMI < 24.9) | 280 (31.6%) |
| Overweight (BMI 25–29.9) | 277 (31.2%) |
| Obesity (BMI ≥ 30) | 330 (37.2%) |
| Smoking status (n = 1028) | |
| No | 644 (62.6%) |
| Yes | 384 (37.4%) |
| Self-rated health status (n = 1026) | |
| Good/very good | 350 (34.1%) |
| Moderate | 464 (45.2%) |
| Bad/very bad | 212 (20.7%) |
| Food bank visits (n = 1023) | |
| <4×/month | 327 (32.0%) |
| 4×/month or more | 696 (68.0%) |
| Duration of food bank use (n = 1029) | |
| 12 months or less | 306 (29.7%) |
| >12 months | 723 (70.3%) |
Survey conducted between May and August of 2015 among food bank users in Germany.
3.2. FIES
The prevalence of FI status among the sample of food bank users was 70.2%. The prevalence of food insecurity status among food bank users divided by levels of food insecurity is presented in Fig. 2. About 34.8% were categorized as mildly food insecure, 27.8% as moderately food insecure and 7.6% as severely food insecure.
Fig. 2.
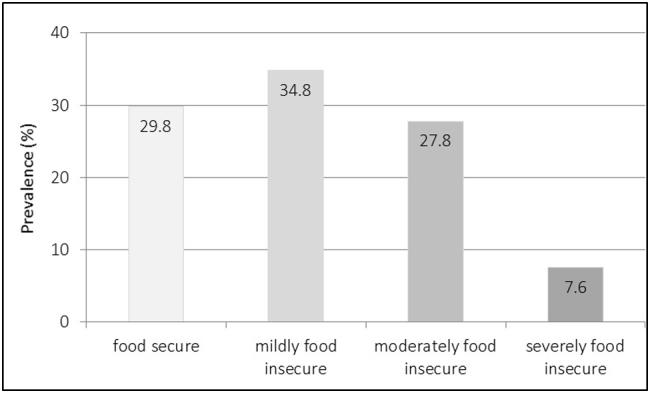
Prevalence of food insecurity status among food bank users in Germany (n = 1033).
When looking at each question of the FIES (Table 1), it was shown that the majority with 60.2% of the food bank users indicated to only have eaten a few kinds of foods during the last 12 months because of a lack of money. Almost half of the sample (49.5%) reported to have been unable to eat healthy and nutritious foods because of a lack of money. Some even went without eating for a whole day because of a lack of money (11.3%).
3.3. Association of FI with sociodemographic and health characteristics of food bank users
When looking at bivariate associations (Table 3), significant differences (V = 0.108, p = 0.008) were seen for gender with more men being categorized as severely food insecure (10.4% vs 5.4%, p < 0.05) while more women were categorized as mildly (36.7% vs 32.4%, n.s.) or moderately food insecure (29.4% vs 25.5%, n.s.). In addition, food insecurity declined with increasing age (rτ = −0.224, p < 0.000). Regarding the health characteristics, both self-rated health status and smoking were significantly related to FI. FI decreased with better self-rated health status (rτ = 0.129, p < 0.000), particularly in the severely food insecure category. Smokers across all food insecurity severity levels appeared to be more often food insecure than non-smokers (V = 0.219, p < 0.000). No significant associations for BMI were found.
Table 3.
Prevalence of FI severity levels by sociodemographic characteristics, health characteristics and food bank visiting patterns (n = 1033).
| Variable | N | Food secure (no “yes”) |
Mildly food insecure (1–3 times “yes”) |
Moderately food insecure (4–7 times “yes”) |
Severely food insecure (8 times ‘yes’) |
Correlations, p value |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |||
| Age | ||||||||||
| ≤40 Years | 234 | 51 | 21.8 a | 72 | 30.8 | 87 | 37.2 a | 24 | 10.3 a | rτ = −0.224 p < 0.000 |
| 41–50 Years | 206 | 41 | 19.9 a | 70 | 34.0 | 73 | 35.4 a | 22 | 10.7 a | |
| 51–65 Years | 368 | 110 | 29.9 a | 127 | 34.5 | 105 | 28.5 a | 26 | 7.1 a,b | |
| ≥66 Years | 225 | 106 | 47.1 b | 91 | 40.4 | 22 | 9.8 b | 6 | 2.7 b | |
| Gender | ||||||||||
| Female | 589 | 167 | 28.4 | 216 | 36.7 | 174 | 29.5 | 32 | 5.4 a | V = 0.108 p = 0.008 |
| Male | 444 | 141 | 31.8 | 144 | 32.4 | 113 | 25.5 | 46 | 10.4 b | |
| Country of birth | ||||||||||
| Germany | 576 | 164 | 28.5 | 179 | 31.1 a | 181 | 31.4 a | 52 | 9.0 a | V = 0.124 p = 0.001 |
| Other | 456 | 144 | 31.6 | 180 | 39.5 b | 106 | 23.2 b | 26 | 5.7 b | |
| Highest completed education | ||||||||||
| No graduation | 49 | 13 | 26.5 | 19 | 38.8 | 10 | 20.4 a,b | 7 | 14.3 | rτ = − 0.105 p = 0.004 |
| Graduation at 10th grade or earlier | 565 | 154 | 27.3 | 181 | 32.0 | 185 | 32.7 b | 45 | 8.0 | |
| Graduation at 12th/13th grade (university entrance) | 371 | 127 | 34.2 | 144 | 38.8 | 78 | 21.0 a | 22 | 5.9 | |
| Household composition | ||||||||||
| Single, no children | 559 | 156 | 27.9 a | 193 | 34.5 | 159 | 28.4 | 51 | 9.1 | V = 0.098 p = 0.004 |
| Couple, no children | 142 | 59 | 41.5 b | 50 | 35.2 | 26 | 18.3 | 7 | 4.9 | |
| Couple, children | 135 | 40 | 29.6 a,b | 51 | 37.8 | 38 | 28.1 | 6 | 4.4 | |
| Single-parent | 82 | 15 | 18.3 a | 35 | 42.7 | 26 | 31.7 | 6 | 7.3 | |
| Other (e.g. shared living) | 84 | 30 | 35.7 a,b | 22 | 26.2 | 29 | 34.5 | 3 | 3.6 | |
| Body mass index | ||||||||||
| Underweight or normal weight | 280 | 81 | 28.9 | 87 | 31.1 | 87 | 31.1 | 25 | 8.9 | V = −0.019 p = 0.520 |
| Overweight | 277 | 84 | 30.3 | 105 | 37.9 | 68 | 24.5 | 20 | 7.2 | |
| Obesity | 330 | 95 | 28.8 | 119 | 36.1 | 90 | 27.3 | 26 | 7.9 | |
| Smoking status | ||||||||||
| No | 644 | 212 | 32.9 a | 251 | 39.0 a | 154 | 23.9 a | 27 | 4.2 a | V = 0.219 p < 0.000 |
| Yes | 384 | 94 | 24.5 b | 108 | 28.1 b | 131 | 34.1 b | 51 | 13.3 b | |
| Self-rated health status | ||||||||||
| Good/very good | 350 | 128 | 36.6 a | 112 | 32.0 | 92 | 26.3 | 18 | 5.1 a | rτ = 0.129 p < 0.000 |
| Moderate | 464 | 144 | 31.0 a | 164 | 35.3 | 128 | 27.6 | 28 | 6.0 a | |
| Bad/very bad | 212 | 35 | 16.5 b | 82 | 38.7 | 66 | 31.1 | 29 | 13.7 b | |
| Food bank visits | ||||||||||
| <4×/Month | 327 | 103 | 31.5 | 107 | 32.7 | 90 | 27.5 | 27 | 8.3 | rτ = 0.001 p = 0.971 |
| 4×/Month or more | 696 | 204 | 29.3 | 252 | 36.2 | 192 | 27.6 | 48 | 6.9 | |
| Duration of food bank use | ||||||||||
| <1 Year | 306 | 78 | 25.5 a | 98 | 32.0 | 97 | 31.7 | 33 | 10.8 a | rτ = − 0.093 p = 0.001 |
| ≥1 Year | 723 | 229 | 31.7 b | 261 | 36.1 | 189 | 26.1 | 44 | 6.1 b | |
Different letters indicate statistically significant differences (p < 0.05, Bonferroni) per column within the variable category.
Survey conducted between May and August of 2015 among food bank users in Germany.
Being born in Germany was associated with moderate (31.4 vs. 23.2%) and severe FI (9.0 vs. 5.7%) compared to being born in another country (V = 0.124, p = 0.001). Higher school education was negatively associated with FI (rτ = −0.105, p = 0.004). FI level also differed by family status (V = 0.103, p = 0.014). Singles (living without children) seemed to be affected by FI more often than couples without children (severe FI: 9.1% vs 4.9%, moderate FI: 28.4 vs 18.3) while being a single parent appeared to increase FI. Only 18.3% of single parents did not experience FI during the last 12 months (couples with children: 29.6%, couples without children: 41.5%).
At last, looking at the duration of using a food bank, users visiting food banks for <12 months were less often food secure (25.5%) and nearly twice as often severely food insecure (10.8%) compared to users visiting food banks for >12 months (31.7% and 6.1%, overall rτ = −0.093, p = 0.001).
4. Discussion
United Nations survey data suggested that 4.3% of the population in Germany are food insecure (FAO, 2016). Our findings indicate that a larger percentage of people in Germany are likely to be food insecure given that the sample in the United Nations survey was small and included all income level households. Both people receiving benefits as well as people visiting food banks suffer more often from FI - e.g. in UK (Power et al., 2017) than the general population. Since 6 million people in Germany are receiving social benefits (Federal Ministry of Labour and Social Affairs, 2017) and at least 15 million people are considered eligible to visit a food bank (National Association of German Tafel, 2016), given our prevalence results, the percentage of food insecure individuals in the German population can be expected to be higher than 4%.
Thus, as also discussed elsewhere (Power et al., 2017), our data supports the body of evidence that the majority of the people using food banks can be considered food insecure. The results add to the limited evidence that FI is also highly prevalent in affluent European countries (Neter et al., 2014, Power et al., 2017). A comparison with FI prevalence rates of food bank users in other countries showed lower rates among food bank users in Germany compared to food bank users in the Netherlands (Neter et al., 2014), France (Castetbon et al., 2016), the U.S. or Canada (Tarasuk and Beaton, 1999; Robaina and Martin, 2013; Leung et al., 2015). Both Dutch and French food banks provide food parcels that supplement the participants' diet while German food banks allow food bank users to choose available, mainly fresh foods. In addition, both studies (Castetbon et al., 2016; Neter et al., 2014) included a higher proportion of households with children, including single parent households (in the Dutch study) compared to our sample. These factors could have contributed to the difference in prevalence rates.
A potential explanation for the lower prevalence rate in our study compared to the studies in the U.S. and Canada could be the difference in social welfare systems across the countries. Another important factor to consider is the difference in measurement instruments used. When looking at associated factors, increasing age appears to be related to food security with fewer older people being affected by FI, which has also been reported elsewhere (Robaina and Martin, 2013). It is possible that, with age, people get better at organizing and managing their daily expenses or lack thereof, which can positively influence their food intake.
Gender differences were also detected. More women were mildly food insecure, which could be because women often prioritize and focus on their family and children's diet while neglecting their own (McIntyre et al., 2007). Single parents, which were more often women (86.6%), were very often affected by FI, a fact also found in other studies (Martin-Fernandez et al., 2013; Nnakwe, 2008). Interestingly, more men were observed to be severely food insecure, which might have been because men tend to have less dietary and health knowledge and fewer cooking skills (Hartmann et al., 2013; Westenhoefer, 2005).
In this study, education appeared to slightly protect from FI, maybe due to better food preparation and financial skills necessary to manage the household food supply with less money but results from other studies examining e.g. emergency assistance users are controversial (Basiotis et al., 1987; Olson et al., 2004). Thus, more research in this area would help to gain insight into the relationship between education and FI among food bank users.
Smoking was associated with FI. While the direction of this relationship cannot be determined in this study, some studies point towards the possibility that smoking limits available financial resources to be spent on food (Widome et al., 2015). However, it is of course also possible that being food insecure increases the likelihood of smoking since it might be used as a coping strategy against financial stress and concerns regarding the purchase of food (Armour et al., 2008; Siahpush et al., 2003). But there are compelling arguments that the relationship between smoking and financial stress is likely not entirely unidirectional (Widome et al., 2015). As found in previous research, self-rated health status was also associated with a higher FI prevalence (Ramsey et al., 2012).
In contrast to the literature, the longer people were visiting food banks, the less likely they seemed to be food insecure. One potential reason that needs to be examined further could be that food banks help to support a life with little money by offering foods since food banks are often used as a coping strategy after having exhausted other forms of support (Lambie-Mumford et al.; 2014; Loopstra and Tarasuk, 2012).
Several limitations need to be stated. The study was cross-sectional and therefore failed to reveal cause-effect-relationships. In addition, in an effort to reach German and non-German users, the questionnaires were provided in four languages. However, the questionnaire was not available e.g. in Turkish, which possibly leads to an underrepresentation of a widely prevalent group of food bank users in Germany. In general, a representative sample of food bank users in Germany was not obtained, which could have caused a selection bias.
A further limitation is the use of self-reports for the variables height and weight (Merrill and Richardson, 2009). It is possible that results among food insecure individuals are skewed since they, especially women, overestimate their weight and height when using self-reports compared to food secure households (Lyons et al., 2008).
At last, different other potential risk factors, e.g. general health (Ramsey et al., 2012; Siefert et al., 2004; Vozoris and Tarasuk, 2003), and protective factors, e.g. self-efficacy of eating healthy (Neter et al., 2014), can influence food insecurity but were not investigated in this study and therefore limit the observed associations between FI and several risk factors.
However, this study is its first in Germany and one of only a few studies examining FI in European countries (Castetbon et al., 2016; Neter et al., 2014; Power et al., 2017). Another strength of this study is the large number of participants from three different German cities.
In conclusion, FI appears to be highly prevalent among food bank users in Germany. The result add to the literature that even high-income countries with a good social welfare system cannot fully or adequately prevent low income people to become food insecure. The study could also identify age and smoking status as the two factors with the strongest association. Besides more research on underlying determinants of FI, causes for differences in prevalence rates across countries need to be investigated. In addition, public health entities should consider the potential of using food banks as a mean to improve nutrition and alleviate FI (Byker Shanks, 2017; Bazerghi et al. 2016) while paying particular attention to health-related characteristics of this population (e.g. considering the high smoking rate and its relationship with FI; Perkett et al., 2017).
Conflict of interest
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgments
The authors would like to thank the food bank users for their participation and the food bank officials for their collaboration.
References
- Anderson S.A. Core indicators of nutritional state for difficult to sample populations. J. Nutr. 1990;120:1557–1600. doi: 10.1093/jn/120.suppl_11.1555. [DOI] [PubMed] [Google Scholar]
- Armour B.S., Pitts M.M., Lee C.-W. Cigarette smoking and food insecurity among low-income families in the United States, 2001. Am. J. Health Promot. 2008;22:386–392. doi: 10.4278/ajhp.22.6.386. [DOI] [PubMed] [Google Scholar]
- Ballard T.J., Kepple A.W., Cafiero C. FAO; Rome: 2013. The Food Insecurity Experience Scale: Development of a Global Standard for Monitoring Hunger Worldwide. [Google Scholar]
- Basiotis P., Johnson S.R., Morgan K.J., Chen J.-S.A. Food stamps, food costs, nutrient availbility, and nutrient intake. J. Policy Model. 1987;9:383–404. [Google Scholar]
- Bazerghi C., McKay F.H., Dunn M. The role of food banks in addressing food insecurity: a systematic review. J. Community Health. 2016;41:732–740. doi: 10.1007/s10900-015-0147-5. [DOI] [PubMed] [Google Scholar]
- Bocquier A., Vieux F., Lioret S., Dubuisson C., Caillavet F., Darmon N. Socio-economic characteristics, living conditions and diet quality are associated with food insecurity in France. Public Health Nutr. 2015;18:2952–2961. doi: 10.1017/S1368980014002912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns C. VicHealth; Melbourne: 2004. A Review of the Literature Describing the Link between Poverty, Food Insecurity and Obesity with Specific Reference to Australia. [Google Scholar]
- Byker Shanks C. Promoting food pantry environments that encourage nutritious eating behaviors. J. Acad. Natur. Diet. 2017;117:523–525. doi: 10.1016/j.jand.2016.12.020. [DOI] [PubMed] [Google Scholar]
- Carter M.A., Dubois L., Tremblay M.S., Taljaard M. Local social environmental factors are associated with household food insecurity in a longitudinal study of children. BMC Public Health. 2012;12(1038) doi: 10.1186/1471-2458-12-1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castetbon K., Grange D., Guibert G., Vernay M., Escalon H., Vincelet C. Recent changes in sociodemographic characteristics, dietary behaviors and clinical parameters of adults receiving food assistance in France. BMC Public Health. 2016;16(779) doi: 10.1186/s12889-016-3443-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coates J., Frongillo E.A., Rogers B.L., Webb P., Wilde P.E., Houser R. Commonalities in the experience of household food insecurity across cultures: what are measures missing? J. Nutr. 2006;136:1438–1448. doi: 10.1093/jn/136.5.1438S. [DOI] [PubMed] [Google Scholar]
- Coleman-Jensen A., Matthew P.R., Christian G., Singh A. U.S. Department of Agriculture, Economic Research Service; 2015. Household Food Security in the United States in 2014, ERR-194. USA. [Google Scholar]
- Depa J., Hilzendegen C., Tinnemann P., Stroebele-Benschop N. An explorative cross-sectional study examining self-reported health and nutritional status of disadvantaged people using food banks in Germany. Int. J. Equity Health. 2015;14(385) doi: 10.1186/s12939-015-0276-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinour L.M., Bergen D., Yeh M.C. The food insecurity–obesity paradox: a review of the literature and the role food stamps may play. J. Am. Diet. Assoc. 2007;107:1952–1961. doi: 10.1016/j.jada.2007.08.006. [DOI] [PubMed] [Google Scholar]
- FAO . Technical Report. FAO; Rome: 2016. Voices of the Hungry. Methods for estimating comparable prevalence rates of food insecurity experienced by adults throughout the world. [Google Scholar]
- Federal Ministry of Labour and Social Affairs . 2017. Der fünfte Armuts- und Reichtumsbericht der Bundesregierung. Lebenslagen in Deutschland. [The fifth poverty and wealth report of the federal government. Living circumstances in Germany]. Federal Ministry of Labour and Social Affairs, Bonn. [Google Scholar]
- Franklin B., Jones A., Love D., Puckett S., Macklin J., White-Means S. Exploring mediators of food insecurity and obesity: a review of recent literature. J. Community Health. 2012;37:253–264. doi: 10.1007/s10900-011-9420-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frongillo E.A., Nguyen H.T., Smith M.D., Coleman-Jensen A. Food insecurity is associated with subjective well-being among individuals from 138 countries in the 2014 Gallup world poll. J. Nutr. 2017;147:680–687. doi: 10.3945/jn.116.243642. [DOI] [PubMed] [Google Scholar]
- Gucciardi E., Vahabi M., Norris N., Del Monte J.P., Farnum C. The intersection between food insecurity and diabetes: a review. Curr. Nutr. Rep. 2014;3:324–332. doi: 10.1007/s13668-014-0104-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann C., Dohle S., Siegrist M. Importance of cooking skills for balanced food choices. Appetite. 2013;65:125–131. doi: 10.1016/j.appet.2013.01.016. [DOI] [PubMed] [Google Scholar]
- Jones A.D. Food insecurity and mental health status: a global analysis of 149 countries. Am. J. Prev. Med. 2017;53:264–273. doi: 10.1016/j.amepre.2017.04.008. [DOI] [PubMed] [Google Scholar]
- Lambie-Mumford H., Crossley D., Jensen E., Verbeke M., Dowler E. The University of Warwick; Food Ethics Council: 2014. Household Food Security in the UK: A Review of Food Aid Final Report: Final Report. [Google Scholar]
- Leung C.W., Epel E.S., Willett W.C., Rimm E.B., Laraia B.A. Household food insecurity is positively associated with depression among low-income supplemental nutrition assistance program participants and income-eligible nonparticipants. J. Nutr. 2015;145:622–627. doi: 10.3945/jn.114.199414. [DOI] [PubMed] [Google Scholar]
- Lindberg R., Whelan J., Lawrence M., Gold L., Friel S. Still serving hot soup? Two hundred years of a charitable food sector in Australia: a narrative review. Aust. N. Z. J. Public Health. 2015;39:358–365. doi: 10.1111/1753-6405.12311. [DOI] [PubMed] [Google Scholar]
- Loopstra R., Lalor D. University of Oxford's Economic and Social Research Council; 2017. Financial insecurity, food insecurity, and disability: The profile of people receiving emergency food assistance from The Trussel Trust Foodbank Network in Britain. (June) [Google Scholar]
- Loopstra R., Tarasuk V. The relationship between food banks and household food insecurity among low-income Toronto families. Canadian Public Policy. 2012;38:497–514. [Google Scholar]
- Loopstra R., Fledderjohann J., Reeves A., Stuckler D. University of Oxford; Sociology Working Papers: 2016. The Impact of Benefit Sanctioning on Food Insecurity: A Dynamic Cross-area Study of Food Bank Usage in the UK. [Google Scholar]
- Lyons A.A., Park J., Nelson C.H. Food insecurity and obesity: a comparison of self-reported and measured height and weight. Am. J. Public Health. 2008;98:751–757. doi: 10.2105/AJPH.2006.093211. (10r.2105/AJPH.2006.093211) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin-Fernandez J., Grillo F., Parizot I., Caillavet F., Chauvin P. Prevalence and socioeconomic and geographical inequalities of household food insecurity in the Paris region, France, 2010. BMC Public Health. 2013;13(486) doi: 10.1186/1471-2458-13-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell S., Smith M. Household food security: A conceptual review. In: Maxwell S., Frankenberger T.R., editors. Household Food Security: Concepts, Indicators, Measurements. A Technical Review. UNICEF, IFAD; 1992. pp. 1–72. [Google Scholar]
- McIntyre L., Tarasuk V., Jinguang Li T. Improving the nutritional status of food-insecure women: first, let them eat what they like. Public Health Nutr. 2007;10:1288–1298. doi: 10.1017/S1368980007702902. [DOI] [PubMed] [Google Scholar]
- Merrill R.M., Richardson J.S. Validity of self-reported height, weight, and body mass index: findings from the National Health and Nutrition Examination Survey, 2001–2006. Prev. Chronic Dis. 2009;6:121. [PMC free article] [PubMed] [Google Scholar]
- National Association of German Tafel Tafel – Meeting places. Volunteers bridging, food rescue, and social commitment. Bundesverband Deutsche Tafel e.V. [National Association of German Tafel], Berlin. 2016. https://www.tafel.de/fileadmin/media/Englische_Informationen/EN_Tafel_Imagebroschuere.pdf (accessed 08-01-2017)
- Neter J.E., Dijkstra S.C., Visser M., Brouwer I.A. Food insecurity among Dutch food bank recipients: a cross-sectional study. BMJ Open. 2014;4 doi: 10.1136/bmjopen-2013-004657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nnakwe N.E. Dietary patterns and prevalence of food insecurity among low-income families participating in community food assistance programs in a midwest town. Fam. Consum. Sci. Res. J. 2008;36:229–242. [Google Scholar]
- Nord M. Unpublished Technical Report to the conducted study. Voices of the Hungry (VoH), FAO. 2015. Food Security Data in German Foodbanks Survey, 2015. [Google Scholar]
- Olson C., Anderson K., Kiss E., Lawrence F.C., Seiling S.B. Factors protecting against and contributing to food insecurity among rural families. Fam. Econ. Nutr. Rev. 2004;16:12–20. [Google Scholar]
- Perkett M., Robson S.M., Kripalu V. Characterizing cardiovascular health and evaluating a low-intensity intervention to promote smoking cessation in a food-assistance population. J. Community Health. 2017;42:605–611. doi: 10.1007/s10900-016-0295-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power M., Uphoff E.P., Stewart-Knox B., Small N., Doherty B., Pickett K.E. Food insecurity and socio-demographic characteristics in two UK ethnic groups: an analysis of women in the born in Bradford cohort. Aust. J. Public Health. 2017;25:1–9. doi: 10.1093/pubmed/fdx029. [DOI] [PubMed] [Google Scholar]
- Pruitt S.L., Leonard T., Xuan C. Who is food insecure? Implications for targeted recruitment and outreach, National Health and Nutrition Examination Survey, 2005–2010. Prev. Chronic Dis. 2016;13 doi: 10.5888/pcd13.160103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radimer K.L., Olson C.M., Campbell C.C. Development of indicators to assess hunger. J. Nutr. 1990;120(Suppl. 11):1544–1548. doi: 10.1093/jn/120.suppl_11.1544. [DOI] [PubMed] [Google Scholar]
- Radimer K.L., Olson C.M., Greene J.C., Campbell C.C., Habicht J.-P. Understanding hunger and developing indicators to assess it in women and children. J. Nutr. Educ. 1992;24:36–44. [Google Scholar]
- Ramsey R., Giskes K., Turrell G., Gallegos D. Food insecurity among adults residing in disadvantaged urban areas: potential health and dietary consequences. Public Health Nutr. 2012;15:227–237. doi: 10.1017/S1368980011001996. [DOI] [PubMed] [Google Scholar]
- Robaina K.A., Martin K.S. Food insecurity, poor diet quality, and obesity among food pantry participants in Hartford, CT. J. Nutr. Educ. Behav. 2013;45:159–164. doi: 10.1016/j.jneb.2012.07.001. [DOI] [PubMed] [Google Scholar]
- Scheidt-Nave C., Kamtsiuris P., Gößwald A. German health interview and examination survey for adults (DEGS) – design, objectives and implementation of the first data collection wave. BMC Public Health. 2012;12(730) doi: 10.1186/1471-2458-12-730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siahpush M., Borland R., Scollo M. Smoking and financial stress. Tob. Control. 2003;12:60–66. doi: 10.1136/tc.12.1.60. https://doi.org/10.1136/tc.12.1.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siefert K., Heflin C.M., Corcoran M.E., Williams D.R. Food insufficiency and physical and mental health in a longitudinal survey of welfare recipients. J. Health Soc. Behav. 2004;45:171–186. doi: 10.1177/002214650404500204. [DOI] [PubMed] [Google Scholar]
- Tarasuk V.S., Beaton G.H. Household food insecurity and hunger among families using food banks. Can. J. Public Health. 1999;90:109–113. doi: 10.1007/BF03404112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinnemann P., Pastatter R., Willich S.N., Stroebele N. Healthy action against poverty: a descriptive analysis of food redistribution charity clients in berlin, Germany. Eur. J. Pub. Health. 2012;22:721–726. doi: 10.1093/eurpub/ckr095. [DOI] [PubMed] [Google Scholar]
- Vedovato G.M., Surkan P.J., Jones-Smith J. Food insecurity, overweight and obesity among low-income African-American families in Baltimore City: associations with food-related perceptions. Public Health Nutr. 2016;19:1405–1416. doi: 10.1017/S1368980015002888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vozoris N.T., Tarasuk V.S. Household food insufficiency is associated with poorer health. J. Nutr. 2003;133:120–126. doi: 10.1093/jn/133.1.120. [DOI] [PubMed] [Google Scholar]
- Westenhoefer J. Age and gender dependent profile of food choice. Forum Nutr. 2005;57:44–51. doi: 10.1159/000083753. [DOI] [PubMed] [Google Scholar]
- Widome R., Joseph A.M., Hammett P. Associations between smoking behaviors and financial stress among low-income smokers. Prev Med Rep. 2015;2:911–915. doi: 10.1016/j.pmedr.2015.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancey A.K., Ortega A.N., Kumanyika S.K. Effective recruitment and retention of minority research participants. Annu. Rev. Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]


