INTRODUCTION
Delirium is an acute, transient, usually reversible neuropsychiatric syndrome, seen in medical-surgical set-ups. It is considered to be a serious problem in acute care settings. Although delirium is encountered in all age groups, elderly are considered to be a high-risk group for development of delirium. It basically reflects decompensation of cerebral functions, as a result of one or more pathophysiological processes. Unfortunately, on many instances delirium is not detected or the detection is delayed. Delirium is known to be associated with varied negative outcomes like prolonged hospital stay, need for institutional care, poor functionality and high treatment costs. It has also been shown to be associated with high short-term and long-term mortality. Besides these, delirium has been shown to be associated with significant distress to the patient and the family. Due to all these negative consequences, it is very important to prevent the development of delirium in medically ill patients. It is also important to detect this entity at the earliest and manage the same to reduce the associated morbidity, mortality and distress among patients and their caregivers. Earlier it was thought that delirium is not associated with any long-term consequences, but now it is increasingly being recognised that in the long run, delirium is associated with cognitive decline and development of dementia.
Indian Psychiatric Society had published clinical practice guidelines (CPGs) for management of various psychiatric disorders amongst elderly for the first time in the year 2007. In the earlier version, management of delirium was included under the CPGs for management of Psychosis amongst elderly. This time it is felt that management of delirium involves a broader range of evaluations and interventions and hence, an effort is made to have separate CPGs for management of delirium. The new guidelines are an attempt to provide updated information on the subject and use the newer information in formulating the guidelines. Although these guidelines are published as part of CPGs for Geriatric Psychiatry, these guidelines can also be applied to patients of other age groups with delirium.
For these guidelines, Internet searches were carried out by using search engines of PUBMED, Embase and Google Scholar to find out the available evidence based literature both for non-pharmacological and pharmacological management. Available treatment guidelines on the topic by different organizations were also reviewed for formulation of the guidelines.
Epidemiology of delirium
Epidemiology of delirium has been evaluated across different treatment settings across the world and the incidence and prevalence is influenced by the treatment setting (Intensive care units, medical/surgical ward, post-operative patients, consultation-liaison psychiatry services), population assessed (elderly, pediatrics, adult, mixed age group) and method used for estimation (screening instrument, diagnostic instrument) of delirium. In general, data suggest an incidence rate of 3 to 42% in hospitalized patients and prevalence to vary from 5 to 44% amongst the hospitalized patients. Data also suggests that the incidence and prevalence of delirium is much higher among patients admitted to various intensive care units (ICUs) with prevalence reported to be as high as 82% with higher rates amongst those requiring mechanical ventilation. Studies evaluating patients in the emergency department, suggest that about 40% of patients have delirium. Studies from India, which have evaluated the incidence of delirium in various intensive care units, have reported prevalence rates to vary from 26.2% to 68.2% and the incidence rates to vary from 9.27 % to 59.6%. Studies, which have evaluated the course of delirium in ICU settings, suggest that the delirium usually starts after 2 (SD-1.7) days of admission to the ICU and lasts for 4.2 (SD-1.7) days.
Nosology
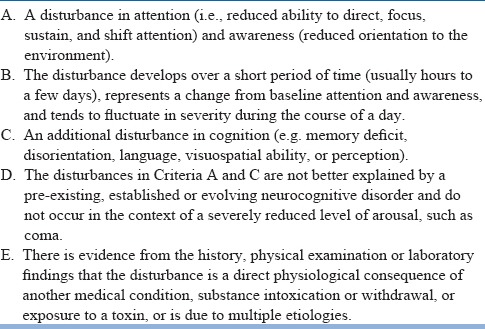
With each revision of the Diagnostic and Statistical Manual (DSM), American Psychiatric Association has made certain modifications in the diagnostic criteria of delirium. The DSM-III version gave importance to ‘clouding of consciousness with a reduced capacity to shift, focus and sustain attention’ as the core feature. Subsequent revision, i.e., DSM-III-R, shifted the emphasis from ‘clouding of consciousness’ to ‘reduced attentiveness’ and ‘disorganized thinking’. Each of these was defined as a major criterion and the term ‘clouding of consciousness’ was dropped. The DSM-IV took a reverse turn and again laid emphasis on ‘disturbance in consciousness and inattention’ as one of the major criteria. The most recent version, i.e., DSM-5 again lays importance on disturbance in attention (i.e., reduced ability to direct, focus, sustain, and shift attention) and awareness (reduced orientation to the environment) and do not consider clouding of consciousness in its clinical criteria of delirium (Table-1). Some of the researchers have questioned this change in emphasis and have shown that the interpretation of the criteria can influence the epidemiology of delirium.
Table 1.
DSM-5 criteria for Delirium
The World Health Organization's International Classification of Diseases (10th revision) defines delirium by disturbance in cognition manifested by both ‘impairment of immediate recall and recent memory’ and ‘disorientation to time, place and person.’ Additionally, criteria in ICD-10 include ‘disturbance in sleep wake cycle’, ‘psychomotor disturbances’, and ‘emotional disturbances’. ICD-10 also specifies the upper limit of 6 months for delirium. Some of the studies which have evaluated the concordance between DSM-IV and ICD-10 criteria suggest that DSM-IV is more sensitive than ICD-10 for the diagnosis of delirium.
Clinical features of delirium
The clinical features of delirium include a constellation of symptoms encompassing physical, biological and psychological disturbances. It is characterised by an acute onset of symptoms, with a fluctuating course. The symptoms of delirium are broadly divided into cognitive, non-cognitive and motoric symptoms. The cognitive symptoms include disturbances in attention, memory, orientation, comprehension, vigilance, visuo-spatial abilities and executive functioning. Of the various cognitive functions, inattention is considered to be the most consistent feature and accordingly is included as a diagnostic criterion. Disturbance in attention involves all aspects, i.e., ability to mobilize, shift and sustain attention. Impairments in memory can involve both short- and long-term memory with significant impairment in recent memory. Disorientation to time, place and person is also very common. Visuo-spatial disturbances and executive dysfunction when present impair the functionality of the patients. The non-cognitive symptoms of delirium include disturbances in the sleep wake cycle, speech and language disturbances, affective lability, perceptual abnormalities (hallucinations, illusions etc.) and delusions. Sleep-wake cycle disruptions can range from napping and nocturnal disruptions to asevere disintegration of the normal circadian rhythm. The motoric symptoms of delirium include an increase or decrease in the psychomotor activity. Based on the psychomotor activity, delirium is subtyped as hyperactive, hypoactive and mixed. The most common subtype of delirium varies from one treatment setting to the other. Studies based on referrals to the consultation-liaison psychiatry (CLP) teams suggest that hyperactive delirium is the most common subtype of delirium. On the other hand, studies involving ICU patients or studies that have reported data of inpatients screened for delirium suggest that hypoactive delirium is the most common subtype of delirium. Recognising the subtypes of delirium can have an important prognostic implication, as studies have shown that hypoactive subtype is associated with higher mortality rates.
Risk factors/etiology for delirium
Delirium is often multi-factorial in origin. Data on risk factors is mainly available from the hospital-based studies. Certain risk factors have been found to be consistent across various treatment settings, whereas other risk factors are specific to a particular treatment setting. The commonly identified risk factors are shown in Table-2. Among these factors, certain factors are considered to predispose or increase vulnerability to develop delirium while certain factors have been shown to be associated with development of delirium. Keeping this in mind, some authors categorise the factors associated with delirium as risk factors/predisposing factors and etiological/precipitating factors. Accordingly, predisposing factors are defined, as factors, which depict the vulnerability of an individual to develop delirium and these, are usually present prior to admission to the hospital and are considered to have a larger contribution than the precipitating factors for the onset of delirium. In contrast to these, precipitating factors are noxious insults or hospital-related factors, which contribute to the development of delirium and are often detected at the time of detection of delirium. However, this categorisation is arbitrary, as there is some overlap in these factors.
Table 2.
Risk factors for delirium
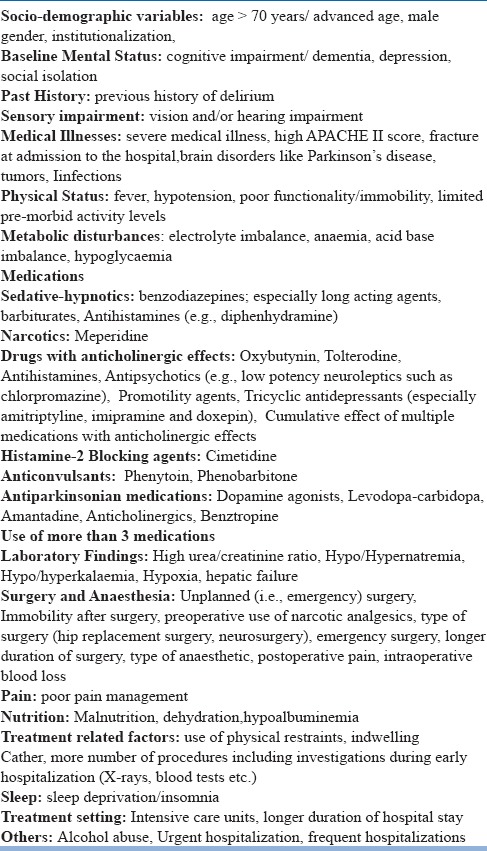
Of all the risk factors, higher age, presence of cognitive impairment, severe concomitant medical illnesses, and receiving medications are considered as ‘robust risk factors’. The commonly associated risk factors for delirium among elderly in acute hospital medical units include presence of dementia, older age (> 70 years), higher severity of medical illness, infection, use of ‘high-risk’ medications, reduction in activities of daily living, being immobile, sensory deprivation/impairment, presence of insitu urinary catheter, raised urea levels, electrolyte imbalance, malnutrition and longer duration of hospital stay.
Differential Diagnosis
The differential diagnosis of delirium includes dementia, depression and psychosis/schizophrenia. Dementia is a risk factor for delirium and is also a differential diagnosis for delirium. Careful history taking can help in distinguishing the two disorders. Delirium is characterised by an acute onset of illness; in contrast, dementia usually has an insidious onset. The cognitive symptoms in dementia manifest in the absence of an altered level of consciousness, whereas delirium is often characterized by an altered level of consciousness. Further, dementia usually follows a downhill course, whereas delirium is often reversible. However, it is important to remember that many patients may present with delirium superimposed on dementia and the symptom profile of patients with delirium with or without dementia do not differ much. Depression is also considered as a risk factor for delirium. History taking should focus on eliciting the history of persistent sadness of mood and morning worsening of symptoms. In contrast to this, delirium is often characterized by lability of mood and evening worsening of symptoms, which is also known as sun-downing effect. Primary psychiatric disorders are often characterized by presence of auditory hallucinations, whereas delirium is predominantly characterized by presence of visual and tactile hallucinations. Cognitive disturbances are present in patients with primary psychotic disorders though these are not as prominent as seen in patients with delirium.
Assessment Scales for Delirium
As delirium is commonly seen in medical-surgical settings, detection of the same requires a high index of suspicion on the part of the treating physician/surgeon. Various instruments have been designed to screen, diagnose and rate the severity of delirium. Separate screening and diagnostic instruments have been designed to assess delirium in different treatment settings,(for example, medical-surgical wards and ICUs). Additionally, instruments have also been designed for different age groups as well as to rate the motoric symptoms in delirium(Table-3).
Table 3.
Commonly Recommended Scales for Assessment of Delirium
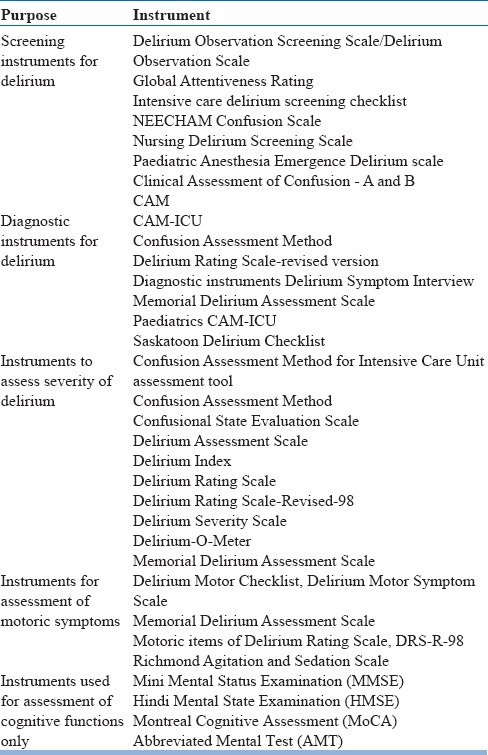
Screening instruments are recommended for non-mental health professionals. Amongst the various screening and diagnostic instruments, Confusion Assessment Method (CAM) is commonly used for both screening and diagnosing delirium by non-mental health professionals. It can be administered in a short span of time (usually 5 minutes) and has been shown to have good psychometric properties. Confusion Assessment Method for Intensive Care Unit (CAM-ICU) has been specifically designed to assess delirium in the ICU setting. It can be used in patients who cannot speak (for example those on mechanical ventilation). CAM-ICU can be used in patients who are arousable to verbal stimuli and can be completed within 1 to 2 minutes by a trained health care professional. CAM-ICU has been shown to have a higher sensitivity (95-100%) and specificity (93-98%), when compared with the diagnosis of delirium made by a mental health professional using DSM-IV criteria. CAM-ICU has also been shown to have high interrater reliability (0.79 to 0.95). For rating of severity of delirium, Delirium Rating Scale-Revised-98 (DRS-R-98) has been the most commonly used scale in recent times. Compared to the previous version, the revised version has a provision for evaluating cognitive symptoms, non-cognitive symptoms, and motoric symptoms and also has diagnostic items. DRS-R-98 has 16 items, out of which 3 items are of diagnostic importance. Patient's behaviour is rated on the basis of information available from all the sources including the mental status examination. Each severity item is rated from 0 (no impairment) to 3 (severe impairment), with a severity score > 15 and a total score of > 18 is indicative of delirium. Higher scores on the scale indicate a much more severe delirium. The DRS-R-98 total score is able to distinguish patients with delirium from those with other mental disorders like dementia, schizophrenia, and depression during blind rating, with a sensitivity ranging from 91% to 100% depending on the cut-off score chosen. It is also the one of the commonest scales used for evaluating the symptom profile or the phenomenology of delirium in various studies. The scale has also been used for monitoring the severity of delirium over a period of time and has been used as an outcome measure in different medication trials. However, it is important to remember that DRS-R-98 has not been validated in the ICU setting.
Mini Mental Status Examination (MMSE) is also used for evaluating the cognitive impairment in patients with delirium. However, it is important to remember that MMSE can evaluate only the cognitive dysfunction.
Management of Delirium
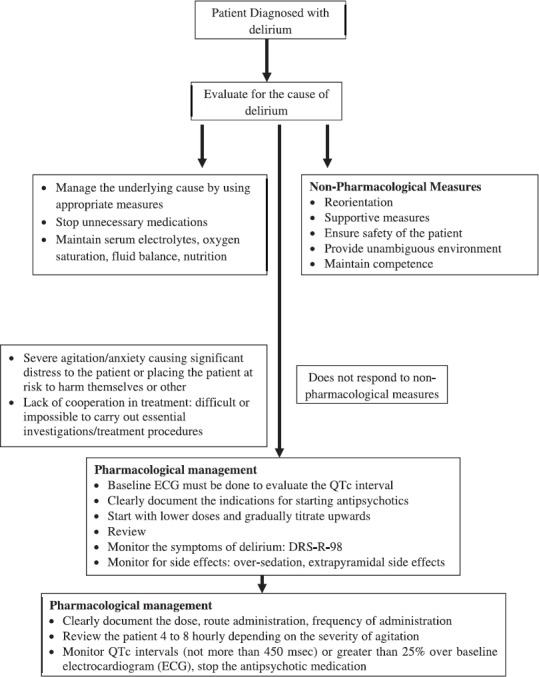
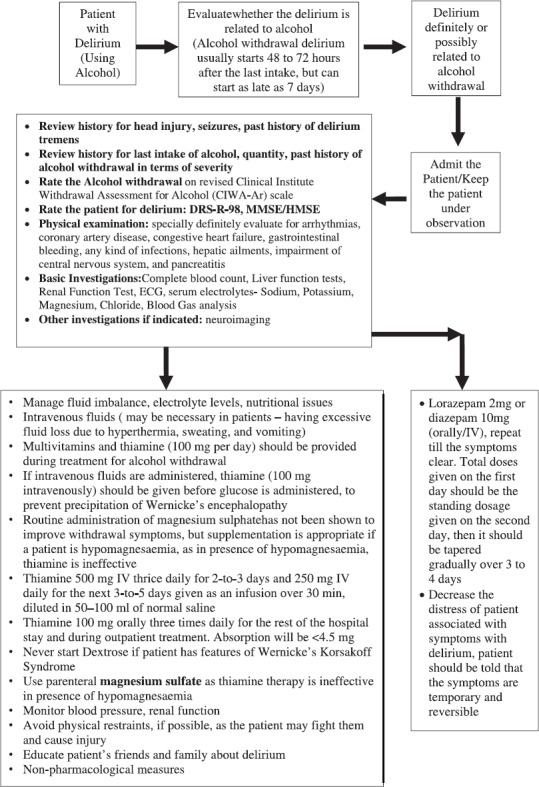
Delirium is a psychiatric emergency, management of which requires proper detection, identification of the cause and treatment of symptoms (Figure-1 & 2). First and foremost, it involves making a correct diagnosis. Diagnosis should be based on any standard nosological system as appropriate rating scales must be used to rate the severity of the symptoms and subtyping delirium. In case patient has alcohol withdrawal delirium then appropriate scales like revised Clinical Institute Withdrawal Assessment for Alcohol Scale (CIWA-Ar) can be used to quantify the severity of alcohol withdrawal syndrome at the baseline and for monitoring the symptoms over time.
Figure 1.
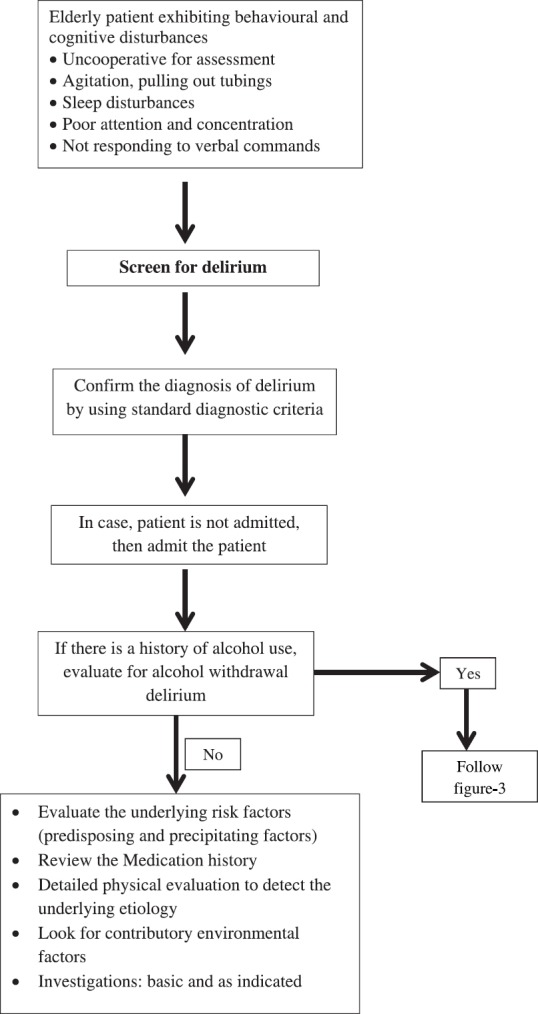
Assessment of patients with Delirium
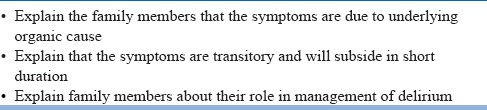
Figure 2.
Management of Delirium
Once a patient is diagnosed with delirium, management should involve identification of possible causes, correction/removal of the etiological factors, and management of symptoms of delirium by using both pharmacological and non-pharmacological treatment. In addition, the clinician should play a role in prevention of any complications and provide adequate information to the family (Table-4).
Table 4.
General Principles of Management of Delirium
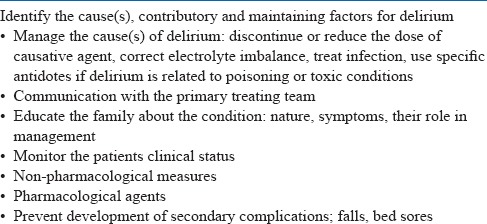
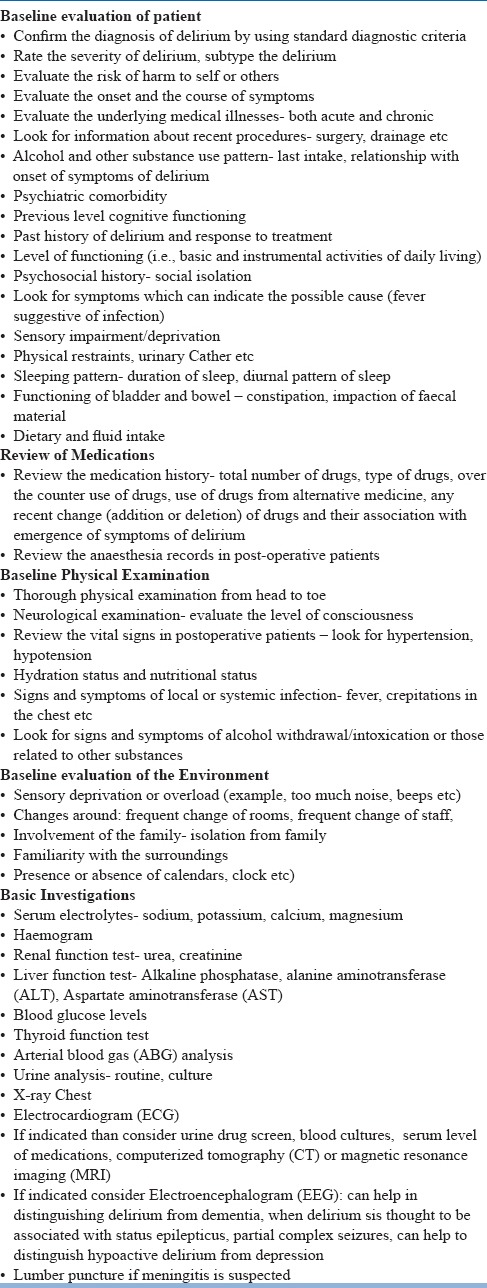
General Principles of Assessment of underlying cause(s), contributory and maintaining factors for delirium
Once the diagnosis of delirium is established with certainty then all efforts must be made to identify the underlying cause for delirium (Table-5). Elderly patients are often not able to provide proper history and in such a scenario efforts must be made to collect the information from all the collateral resources. A thorough review must be done for medications received including the prescription and over the counter medications. Due attention must be paid to addition of any new drug or an increase in dosage of medication (s). If there is a close link between onset of delirium and change in the dosage or starting of a medication then it can be considered as a possible offending agent. Detailed physical examination needs to be done to evaluate all the possible causes of delirium. In terms of investigations, neuroimaging is not indicated routinely and must be considered in persons having suspicion of intracranial lesions, i.e., patients having focal neurological signs, history of head injury/trauma just prior to onset of symptoms, presence of papilloedema indicating raised intracranial pressure. Similarly electroencephalogram should not be done routinely.
Table 5.
General Principles for Assessment of cause of delirium
Management for the underlying cause(s) of delirium
Once a cause is identified it should be treated with adequate measures. It is important to remember that on many occasions, more than one factor lead to delirium, i.e., there may be just one offending agent but multiple contributory factors. In case the delirium is attributed to a medication, the offending agent must be removed in consultation with the primary treating team. Additionally all non-required medications need to be stopped in liaison with the primary treating team (Table-6).
Table 6.
Management of Underlying Cause(s)
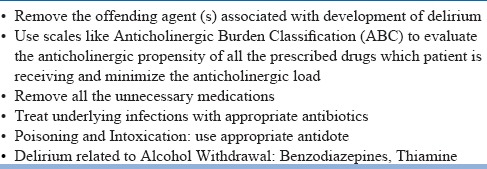
At times delirium may not be attributed to one specific medication, but it may be due to cumulative anticholinergic properties of various medications received. This can be done by using available charts like Anticholinergic Burden Classification (ABC), Anticholinergic Drug Scale (ADS), Anticholinergic Risk Scale (ARS), Anticholinergic Cognitive Burden Scale (ACB), Clinician-rated Anticholinergic Score, Anticholinergic Activity Scale (AAS) and Anticholinergic Loading Scale (ACL). Among these instruments, ABC is the most commonly used scale. The ABC provides a list of medications along with their anticholinergic propensities. The drugs are rated from 1 to 3 depending on the anticholinergic properties. This can help in understanding the anticholinergic load and identifying the agents, which need to be stopped. If delirium is related to an infection, appropriate measures must be taken treat the infection. Appropriate antidote must be used in case delirium is related to a poisoning or intoxication. If delirium is related to alcohol withdrawal, then benzodiazepines must be considered. Additionally, measures like use of high doses of thiamine must be carried out. Many elderly patients are prone to have nutritional deficiencies and if these are suspected then use of multivitamins may be considered.
Communication with the primary treating team
As delirium is most often encountered in the consultation-liaison psychiatry set-up, communication with the primary treating team forms an important aspect of the management. Often the physicians and surgeons equate delirium with other psychiatric disorder, which do not have underlying physical causes and request to shift the patient to the psychiatric unit. In such situations, it is important to explain to the primary team members that although the patient is having symptoms similar to some of the other psychiatric disorders like psychosis, but delirium is a result of an underlying medical-surgical aetiology and is reversible. Emphasis must be laid upon the fact that correction of underlying cause can reverse the process. Besides this, the primary treating team must be explained about the role of non-pharmacological and supportive measures and the use of psychotropics to manage delirium.
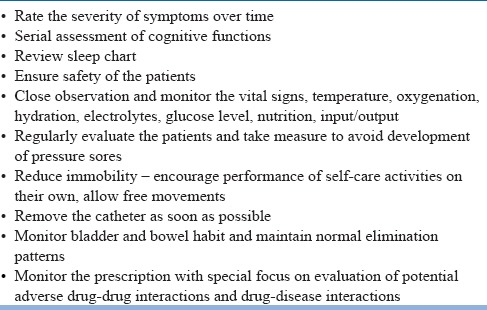
Figure 3.
Management of Alcohol Withdrawal Delirium
Educate the family about delirium
Family members often experience significant distress on seeing the clinical manifestation of delirium. They are also often ignorant about their role in management of delirium. Hence, it is of utmost importance to address the family members as they can be an important integral part of the management. They should be provided adequate information about the nature of the syndrome, symptoms and their role in management (Table-7).
Table 7.
Educate the family members about delirium
Monitoring of the patient
All patients with delirium require close monitoring till the symptoms subside. Monitoring over a period of time must be done to avoid emergence of newer factors, which can worsen the delirium and can lead to continuation of symptoms of delirium. Other important aspects of monitoring include ensuring safety of the patient, ensuring adequate sleep, avoiding development of complications like bed sores and falls (Table-8). In general physical restraints must be avoided as far as possible. Physical restraints may be considered when there is a serious risk for bodily harm to self or other, other measures to control (i.e., pharmacotherapy have failed) and the potential benefits outweigh the risks of using restraints. When required, least restrictive physical restraints be used and for the shortest possible duration and must be removed when the potential harm threatening behaviours have subsided or if the patient develops physical complications due to the use of restraints.
Table 8.
Monitoring of patients with delirium
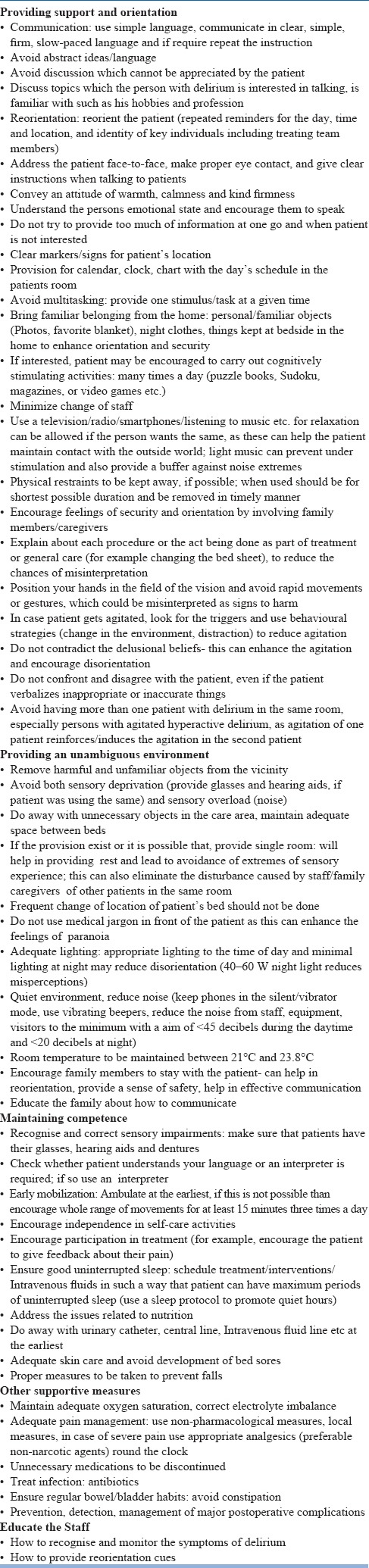
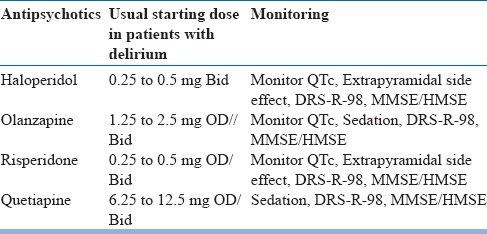
Non-Pharmacological Management
Non-Pharmacological treatment involves providing unambiguous, supportive environment to improve the orientation and maintain the competence of the patients. The components of this can be divided into providing support and orientation, providing unambiguous environment, measures at maintaining competence and providing other supportive measures (Table-9). Many studies have evaluated the various components of the non-pharmacological interventions in delirium. However, there are limited numbers of randomised control trials (RCTs), which have evaluated non-pharmacological interventions. Findings from various RCTs suggest that systematic detection and multidisciplinary care do not appear to be superior than usual care provided to elderly patients admitted to medical services. However these studies have been criticised for the limitations in the form of a contamination effect, i.e., patients in both the intervention arms were managed in the same units by the same staff.
Table 9.
Non-pharmacological measures for delirium
Pharmacological treatment for delirium
A wide range of pharmacological agents has been evaluated for the management of delirium (Table-10). Factors, which influence the medication selection, include the treatment setting (medical-surgical ward/ICU/Palliative care), treating agency (Intensive care interventionist versus CL Psychiatrist) and the clinical demand (hyperactive/hypoactive delirium).
Table 10.
Pharmacological management of Delirium
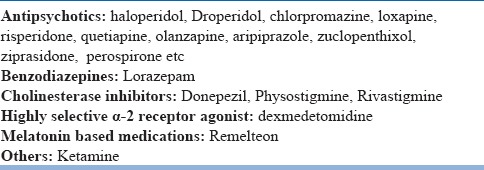
Use of pharmacological agents must be weighed against the possible side effects. Pharmacological management is not indicated in all the patients. It is suggested that pharmacotherapy be considered when non-pharmacological measures have failed to manage the patient in ease or there are specific indications for its use. The most common indication for pharmacological management includes severe agitation or severe anxiety causing significant distress to the patient or placing the patient at risk to harm themselves or others. Other indications for pharmacotherapy include a lack of cooperation in treatment to the extent that it is difficult or impossible to carry out essential investigations or treatment procedures. Further, despite the best attempts at carrying out non-pharmacological treatment, symptoms of delirium are persisting.
Antipsychotics: In general, antipsychotics are considered as the medication of choice in the management of delirium. Studies have evaluated various antipsychotics in the management of delirium. However, there are a very few double blinded randomised placebo controlled trials which have evaluated the efficacy of antipsychotics in patients with delirium. Available trials are also limited by a small sample size and heterogeneity in the treatment setting, in which the studies have been carried out. Despite these limitations most of the experts agree on the use of antipsychotics for a short duration in the management of delirium.
Antipsychotics have been reported to reduce the agitation, anxiety, associated psychotic symptoms, have a sedative effect and have also been shown to improve the cognitive symptoms of delirium. Decision to start antipsychotics must be taken in liaison with the family/caregivers and members of the primary treating team.
The important thing to remember is that, the mean doses required to control the symptoms of delirium are significantly less than the dose usually used in the management of other psychiatric disorders. Hence, whenever antipsychotics are used, these must be started in lower doses and slowly titrated upwards (Table-11 and 12).
Table 11.
General Principles of use of antipsychotics in Delirium
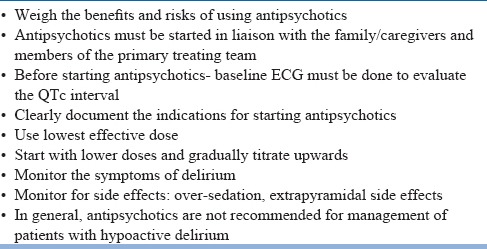
Table 12.
Antipsychotics with recommended doses
In terms of selection of an antipsychotic medication, haloperidol is the most preferred agent. It is one of the oldest molecules used in the management of delirium. In fact, all the newer antipsychotics, which have been evaluated in the management of delirium, have been compared against haloperidol. Haloperidol has certain advantages over other antipsychotics. It is available in different formulations (oral, intramuscular and intravenous routes) and reported to be associated with a lower risk of sedation and hypotension. It is usually started in low doses, i.e., in the dose range of 0.25–0.50 mg 4 hourly for elderly. Doses are titrated as per the need. As haloperidol is thought to be associated with a high incidence of cardiac conduction problems such as prolongation of the QT interval and arrhythmias, which can lead to torsades de pointes and ventricular fibrillation, electrocardiogram (ECG) must be closely monitored. In terms of efficacy, most of the recent trials which have compared haloperidol with various other antipsychotics suggest that it is as efficacious/effective as other antipsychotics. However, occasional studies, which have evaluated haloperidol against placebo in palliative care settings, have reported it to be inferior to placebo in reducing symptoms of delirium. A recent review of data on haloperidol suggests that it is associated with reduction in severity of symptoms in delirium. Regarding the side effects of haloperidol, the authors concluded that although side effects do not limit its use in delirium, but at the same time cautioned, that only a few studies have systematically assessed the adverse events.
In the last decade or so, some data has been generated for the efficacy/effectiveness of other antipsychotics like risperidone, quetiapine, olanzapine, aripiprazole, zuclopenthixol, ziprasidone and perospirone in the management of delirium. These studies suggest that atypical antipsychotics like olanzapine, risperidone and quetiapine are as efficacious as haloperidol in reducing the severity of delirium. Alongside, they also improve the cognitive functions and are associated with lower incidence of side effects as compared to haloperidol. A double blind placebo controlled trial, which compared quetiapine with placebo showed that quetiapine leads to reduction in the severity of non-cognitive symptoms of delirium at a faster rate than placebo. Although haloperidol is considered as the most preferred agent in the management of delirium, but if elderly patients with Parkinson's disease or Lewy Body Dementia, develop delirium, atypical antipsychotics are considered as the preferred agents by a few authors. Regarding the duration of treatment, there is no consensus. Some authors suggest that antipsychotics should be discontinued immediately after the resolution of delirium, whereas others recommend tapering off of antipsychotics after a 1-week of asymptom free period.
Benzodiazepines: Benzodiazepines can worsen the cognitive functions and lead to excessive sedation. Hence, benzodiazepines are not considered as the first line agent forthe management of delirium. Benzodiazepines may be used when the delirium is caused by sedatives or as a result of alcohol withdrawal or it is associated with seizures. If benzodiazepines are considered in the management of alcohol withdrawal delirium then, lorazepam is the preferred agent, because of its short-half life, lack of major active metabolites and a relatively predictable bioavailability when given intramuscularly. When used, benzodiazepines must be initiated in low doses, especially amongst the elderly, those with respiratory or hepatic impairment and in patients receiving medications, which undergo extensive hepatic oxidative metabolism. It is important to remember that in general, benzodiazepines are contraindicated in delirium associated with hepatic encephalopathy as in this condition there is accumulation of glutamine, which is chemically related to γ-aminobutyric acid (GABA). If benzodiazepines are to be used in patients with hepatic insufficiency or those receiving other medications metabolized by the cytochrome P450 system, benzodiazepines that get primarily metabolized by glucuronidation (lorazepam, oxazepam, and temazepam) should be preferred. In patients with respiratory insufficiency, benzodiazepines need to be used with caution. When used, benzodiazepines should not be stopped abruptly; rather, these must be tapered off.
If delirium in patients with alcohol withdrawal does not respond to benzodiazepines alone, then use of antipsychotics may be warranted. However, it is important to remember that in such a scenario antipsychotics should be used along with benzodiazepines. Antipsychotics may be considered when agitation, perceptual disturbances, or disturbed thinking are not controlled adequately with the use of benzodiazepines alone.
Data on combined use of antipsychotics and benzodiazepines in patients with delirium not related to alcohol withdrawal is limited. Limited existent data suggest that use of combination may decrease the emergent side effects and may improve the clinical effectiveness (shorter duration of delirium, less extrapyramidal symptoms) in special population, like those with severely ill cancer and AIDS.
In view of role of excess of acetylcholine in pathogenesis of delirium, some of the studies have evaluated the efficacy/effectiveness of cholinergic medications in delirium. The most commonly studied cholinesterase inhibitor is physostigmine. Other molecules, which have been evaluated, include tacrine and donepezil. Overall, there is very limited data for this class of medications.
Effectiveness of highly selective α-2 receptor agonist, dexmedetomidine, has also been evaluated mainly in the ICU patients. It has sedating properties (which is independent of γ-aminobutyric acid receptors), anxiolytic properties and modest analgesic properties. Further, it has a very low propensity to cause respiratory depression. Due to this unique profile, the molecule has been evaluated in ICU patients with delirium. A review of available studies, which included 8 clinical trials, of which 5 were Double Blind Randomized Controlled Trials (DBRCTs), concluded that dexmedetomidine might be useful in treatment of delirium.
Over the years, melatonin has also been implicated in the etiopathogenesis of delirium. In view of this some of the studies have evaluated the role of ramelteon in management of delirium. Preliminary evidence suggests that ramelteon may be useful in management of delirium.
Studies have also evaluated the role of paralytic agents in conjunction with use of mechanical ventilation for the management of delirium in ICU settings. It is recommended when patient does not respond to conventional treatment for delirium in the ICU setting. This has mostly been tried for patients with hyperactive delirium, which due to overexertion and fatigue leads to a hypercatabolic state, which can exacerbate hypoxia and metabolic abnormalities. Use of heavy sedation along with morphine improves oxygenation and reduces skeletal muscle exertion. Use of morphine and other opioids is also useful in patients of delirium where pain is a precipitating or acontributory factor. However, it is important to note that opiates can worsen or cause delirium, especially those with high anticholinergic properties.
Electroconvulsive therapy is also rarely being used for themanagement of delirium. The data is limited toa few case reports and it can be said that ECT cannot be used as a substitute for other conventional treatments. Use of ECT is recommended only in cases of delirium, associated with neuroleptic malignant syndrome or to patients who have not responded to all the pharmacological agents.
Discharge from the Hospital and Follow-up
Ideally patients with delirium must be kept in the hospital until the delirium resolves. Prior to discharge, family needs to be explained about the any further management issues and the required monitoring. As patients with delirium are at a risk of developing dementia, their cognitive functions must be monitored from time to time. Past history of delirium also increases the risk of future episodes of delirium. Accordingly, the family members must be explained about the symptoms of impending delirium and what is to be done in such a situation. Many patients experience significant distress by recollecting their experience of delirium. They should be provided with supportive psychotherapeutic intervention to allay their distress. Even after discharge, patient and family members must be advised to follow-up with the psychiatric services for further re-evaluations and required interventions. In case, such patients are being managed on outpatient basis, the aim of the clinician should be to monitor the symptoms in each follow up by using measurement based care. Alongside, a close liaison with the primary treating physician/surgeon must be maintained to promote a joint decision-making and minimising the confusion.
Prevention of complications of delirium
Delirium can often be associated with secondary complications like falls, development of bedsores, hospital acquired infections, functional impairment, problems with bladder and bowel control and over sedation. Falls can be prevented by providing care on lower beds or placing the mattress of the patient on the floor. Wherever possible, use of physical restraints should be avoided. Because of prolonged lying down position, especially amongst those admitted to ICUs, the risk of developing pressure sores and secondary infections is particularly high in patients with delirium. Accordingly, patients must be repositioned from time to time and regularly evaluated for possible bedsores. Wherever possible, provision of special mattresses like (water beds) must be considered. To reduce the functional impairment, patient must be mobilized at the earliest and in case this is not possible, adequate mobility must be maintained with the help of a physiotherapist. As use of catheter for a long duration can be associated with infections, catheters must be removed at the earliest and a regular toileting must be encouraged. Similarly, bowel movement must be monitored to avoid and constipation.
Prevention of delirium
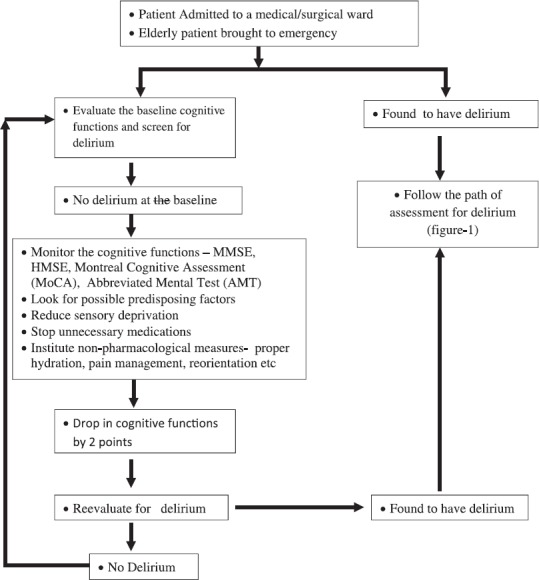
Considering the fact that delirium is associated with significant negative health related outcomes, efforts must be made to prevent the same. The basic algorithm to be followed for prevention of delirium is given in the figure-2. All elderly patients or patients of other age group admitted to medical-surgical ward must be evaluated for their baseline cognitive functions by using standard instruments like MMSE, Hindi Mental State Examination (HMSE), Montreal Cognitive Assessment (MoCA), Abbreviated Mental Test (AMT) etc. Additionally, the baseline assessment should involve an evaluation of risk factors, which make the person vulnerable to develop delirium, in the face of further insult. It is of paramount importance to review the treatment of the patient and all the unnecessary medications need to be stopped. Other measures include an adequate pain management, ensuring an adequate sleep, appropriate hydration and nutrition, a provision of adequate cognitive stimulation, and minimizing sensory deprivation by correction of sensory deficits (Table-13). There is some evidence to support the role of preoperative consultation and regular daily visits, throughout the period of hospitalization, by mental health professionals in non-delirious elderly patients and targeted recommendations based on a structured protocol to reduce the incidence of delirium.
Table 13.
Prevention of Delirium
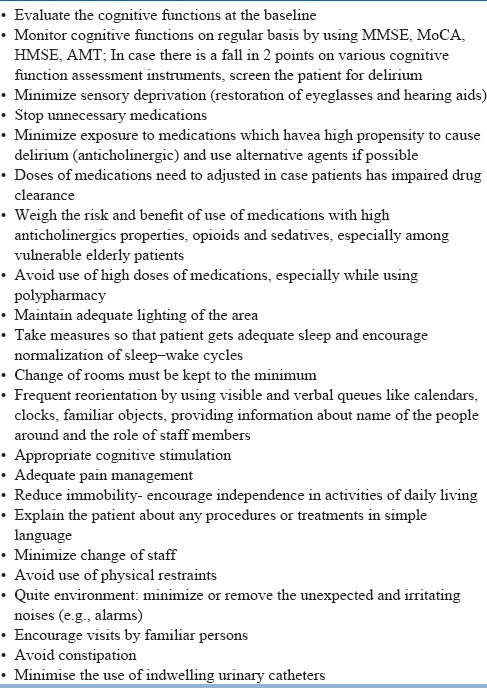
Various pharmacological agents used for the management of delirium (i.e., haloperidol, cholinesterase inhibitors- donepezil, benzodiazepines, dexmedetomidine etc) have also been studied for their role in prevention of delirium, especially in patients undergoing surgical procedures. The available evidence is inconclusive with respect to the role of pharmacological agents in prevention of delirium. A systematic review and metanalysis suggests that antipsychotics reduce the incidence of post-operative delirium, mainly in persons undergoing orthopaedic surgery and those who are at a higher risk for delirium. The authors also suggested that there is lot of heterogeneity in the data. There is some data to support the role of melatonin in reducing the incidence of delirium among elderly patients admitted to various medical wards. A recent Cochrane review, reviewed the available data for prevention of delirium in patients admitted in non-ICU set-ups. It concluded that there is no role of of antipsychotics, melatonin and cholinesterase inhibitors in prevention of delirium. However, the authors concluded that there is a strong evidence for the role of supportive multi-component interventions in prevention of delirium. Currently available guidelines for management of delirium from various professional organisations do not recommend use of antipsychotics or other pharmacological agents for prevention of delirium.
Figure 4.
Algorithm for prevention of delirium
SUGGESTED READING
- 1.Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49:516–22. doi: 10.1046/j.1532-5415.2001.49108.x. [DOI] [PubMed] [Google Scholar]
- 2.Fok MC, Sepehry AA, Frisch L, Sztramko R, Borger van der Burg BL, Vochteloo AJ, Chan P. Do antipsychotics prevent postoperative delirium? A systematic review and meta-analysis. Int J Geriatr Psychiatry. 2015;30:333–44. doi: 10.1002/gps.4240. [DOI] [PubMed] [Google Scholar]
- 3.Chen S, Shi L, Liang F, Xu L, Desislava D, Wu Q, Zhang J. Exogenous Melatonin for Delirium Prevention: a Meta-analysis of Randomized Controlled Trials. Mol Neurobiol. 2016;53:4046–53. doi: 10.1007/s12035-015-9350-8. [DOI] [PubMed] [Google Scholar]
- 4.Siddiqi N, Harrison JK, Clegg A, Teale EA, Young J, Taylor J, Simpkins SA. Interventions for preventing delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev. 2016;3:CD005563. doi: 10.1002/14651858.CD005563.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mo Y, Zimmermann AE. Role of dexmedetomidine for the prevention and treatment of delirium in intensive care unit patients. Ann Pharmacother. 2013;47:869–76. doi: 10.1345/aph.1AR708. [DOI] [PubMed] [Google Scholar]
- 6.Miura S, Furuya M, Yasuda H, Miyaoka T, Horiguchi J. Novel Therapy With Ramelteon for Hypoactive Delirium: A Case Report. J Clin Psychopharmacol. 2015 t;35:616–8. doi: 10.1097/JCP.0000000000000370. [DOI] [PubMed] [Google Scholar]
- 7.Tsuda A, Nishimura K, Naganawa E, Otsubo T, Ishigooka J. Ramelteon for the treatment of delirium in elderly patients: a consecutive case series study. Int J Psychiatry Med. 2014;47:97–104. doi: 10.2190/PM.47.2.a. [DOI] [PubMed] [Google Scholar]
- 8.Kimura R, Mori K, Kumazaki H, Yanagida M, Taguchi S, Matsunaga H. Treatment of delirium with ramelteon: initial experience in three patients. Gen Hosp Psychiatry. 2011;33:407–9. doi: 10.1016/j.genhosppsych.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 9.Meagher D, Leonard M. The active management of delirium: improving detection and treatment. Adv Psychiatric Treat. 2008;14:292–301. [Google Scholar]
- 10.Grover S, Mattoo SK, Gupta N. Usefulness of atypical antipsychotics and Choline esterase inhibitors in delirium: A review. Pharmacopsychiatry. 2011;44:43–54. doi: 10.1055/s-0031-1273759. [DOI] [PubMed] [Google Scholar]
- 11.Grover S, Kumar V, Chakrabarti S. Comparative efficacy study of Haloperidol, Olanzapine and Risperidone in delirium. J Psychosomatic Res. 2011;71:277–81. doi: 10.1016/j.jpsychores.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 12.Grover S, Mahajan S, Chakrabarti S, Avasthi A. Comparative effectiveness of quetiapine and haloperidol in delirium: A single blind randomized controlled study. World J Psychiatry. 2016;6:365–71. doi: 10.5498/wjp.v6.i3.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tahir TA, Eeles E, Karapareddy V, Muthuvelu P, Chapple S, Phillips B, Adyemo T, Farewell D, Bisson JI. A randomized controlled trial of quetiapine versus placebo in the treatment of delirium. J Psychosom Res. 2010;69:485–90. doi: 10.1016/j.jpsychores.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 14.Schrijver EJ, de Graaf K, de Vries OJ, Maier AB, Nanayakkara PW. Efficacy and safety of haloperidol for in-hospital delirium prevention and treatment: A systematic review of current evidence. Eur J Intern Med. 2016;27:14–23. doi: 10.1016/j.ejim.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 15.Agar MR, Lawlor PG, Quinn S, Draper B, Caplan GA, Rowett D, Sanderson C, Hardy J, Le B, Eckermann S, McCaffrey N, Devilee L, Fazekas B, Hill M, Currow DC. Efficacy of Oral Risperidone, Haloperidol, or Placebo for Symptoms of DeliriumAmong Patients in Palliative Care: A Randomized Clinical Trial. JAMA Intern Med. 2017;177:34–42. doi: 10.1001/jamainternmed.2016.7491. [DOI] [PubMed] [Google Scholar]
- 16.Clinical Practice Guidelinesfor the Managementof Delirium in Older People. Developed by the Clinical Epidemiology and Health Service Evaluation Unit, MelbourneHealth in collaboration with the Delirium Clinical Guidelines Expert Working Group. Commissioned on behalf of the Australian Health Ministers’ Advisory Council (AHMAC), by the AHMAC Health Care of Older Australians Standing Committee (HCOASC) 2006 Oct [Google Scholar]
- 17.Bush SH, Bruera E, Lawlor PG, Kanji S, Davis DH, Agar M, Wright DK, Hartwick M, Currow DC, Gagnon B, Simon J, Pereira JL. Clinical practice guidelines for delirium management: potential application in palliative care. J Pain Symptom Manage. 2014;48:249–58. doi: 10.1016/j.jpainsymman.2013.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cole MG, Primeau FJ, Bailey RF, Bonnycastle MJ, Masciarelli F, Engelsmann F, Pepin MJ, Ducic D. Systematic intervention for elderly inpatients with delirium: a randomized trial. CMAJ. 1994;151:965–70. [PMC free article] [PubMed] [Google Scholar]
- 19.Cole MG, McCusker J, Bellavance F, Primeau FJ, Bailey RF, Bonnycastle MJ, Laplante J. Systematic detection and multidisciplinary care of delirium in older medical inpatients: a randomized trial. CMAJ. 2002;167:753–9. [PMC free article] [PubMed] [Google Scholar]
- 20.Canadian Coalition for Seniors’ Mental Health (CCSMH) National Guidelines for Seniors’ Mental Health - The Assessment and Treatment of Delirium. Canadian Coalition for Seniors’ Mental Health, Toronto. 2006 [Google Scholar]


