INTRODUCTION
Depressive disorders are one of the common psychiatric ailments seen in elderly population. As per the World Health Organization (WHO) prevalence of depressive disorders among elderly is 10 to 20%. Data from India reveals a wide variation in the prevalence rate of depression. Prevalence in community-based studies have varied from 8.9% to 62.16% and clinic based studies have estimated the prevalence of depression to range from 42.4 to 72%. Unfortunately, depression among elderly is often considered as part and parcel of life and is under-recognised and under-diagnosed. Depression in elderly has been shown to be associated with significant negative consequences ranging from poor quality of life, difficulties with activities of daily living, physical comorbidities, premature mortality and cognitive impairments. Although the incidence of depression among elderly is similar to that reported in adult population, depression in elderly is associated with higher risk of suicide, more frequent hospitalization, higher number of consultations with the treatment agencies and family burden. Hence, it is very important to recognise depression among elderly and manage the same.
Timely recognition and adequate management of depression among elderly can lead to improvement in quality of life, maintaining optimal levels of function and independence, reduction in morbidity, reduction in mortality due to suicide, development of medical illnesses and treatment costs.
Indian Psychiatric Society (IPS) published Clinical Practice Guidelines (CPGs) for management of depression among elderly, for the first time in the year 2007. IPS also published revised CPGs for management of depression in adult patients in the year 2017. Current version of the CPGs is an update of the earlier version of CPGs for management of depression in elderly. The current version of the CPGs for depression in elderly must be read in conjunction with the previous version of CPGs for depression in elderly and revised CPGs for management of depression in adult population.
These guidelines provide a broad framework for assessment, management and follow-up of elderly patients presenting with depression. Most of the recommendations made as part of the guidelines are evidence based. However, these guidelines should not be considered as a sustitute for professional knowledge and clinical judgment. The recommendations made as part of these guidelines have to be tailored to address the clinical needs of the individual patient and treatment setting.
DIAGNOSTIC COMPLEXITIES OF DIAGNOSING DEPRESSIVE DISORDERS IN ELDERLY
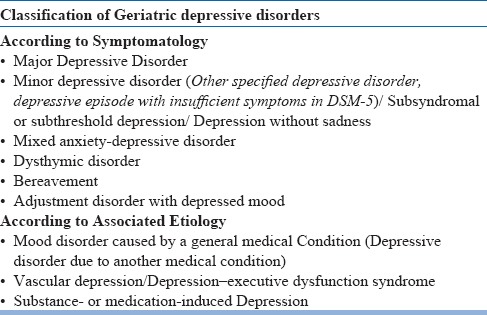
Depressive disorders in elderly can include a spectrum of disorders (Table-1). Depression in elderly is also known as late life depression, which is further understood as late onset depression and early onset depression. There is lack of consensus on the age cut-off used to define late onset depression, with some of the authors considering the age cut-off of 60 years, whereas others define it as experiencing first episode of depression ≥ 65 years of age). While assessing depression among elderly, it is important to remember that although many elderly have depressive symptoms, they do not fulfil the criteria of major depression. Presence of physical illness and atypical presentations further complicate the clinical picture. Hence it is postulated that although the presence of standard diagnostic criteria is a necessary for of depression in elderly, this is not sufficient condition for diagnosis of depression in elderly. Due to these intricacies, the concept of 'subthreshold’ depression, 'subclinical’ depression, ‘minor’ depression, ‘milder’ depression etc have been described. Accordingly, depression in elderly is often broadly classified as Major and Non-major Depression. The nonmajor category includes minor depression, dysthymia, adjustment disorder with depressed mood and mixed anxiety and depressive disorder.
Table 1.
Spectrum of Depressive Disorders in Elderly
In general it is suggested that prevalence of minor depression is more than that of major depression. Some of the studies suggest that with increasing age prevalence of major depression decreases and that of minor or sub-threshold depression increases. Minor depression in elderly is associated with significant number of disability days and concomitant anxiety disorder. Proper recognition of minor depression is of paramount importance because it is often the forerunner of the major depression among elderly subjects. The spectrum of depressive disorders among elderly also includes dysthymic disorder and adjustment disorder with depressed mood, which are also seen in 2% and 4% of the population respectively.
Minor depression is defined as presence of clinically significant depressive symptoms which do not meet the threshold duration criterion or the number of symptoms necessary for the diagnosis of Major depressive disorder (MDD) as per the current nosology. Some of the authors have further characterised minor or subsyndromal depression among elderly into 2 subtypes. According to some authors the first subtype of minor depression consists of syndromes qualitatively similar to major depression and dysthymia but it is characterised by presence of fewer symptoms or with less symptom continuity. The second type of subsyndromal depression is considered to be qualitatively different from MDD and is associated with lower suicidal thoughts and feelings of worthlessness or guilt but similar levels of worries about health and “weariness of living”. Judd et al described 2 subtypes of subsyndromal symptomatic depression (SDD) for minor depression as SDD with mood disturbance (minor depression) and SDD without mood disturbance.
Minor depression was described in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) as a condition requiring further research to determine both diagnostic utility and criteria refinement. In DSM-5, minor depression can be subsumed under the category of “Other specified depressive disorder, depressive episode with insufficient symptoms”, which is characterised by presence of depressed affect and at least one of the other eight symptoms of MDD, which is associated with clinically significant distress or impairment that persists for a duration of at least 2 weeks. It further requires that the person should never have met the criteria of any other depressive or bipolar disorder, does not currently meet active or residual criteria for any psychotic disorders and as well as does not meet the criteria for mixed anxiety and depressive disorder.
DSM-5 has a separate category for the depressive disorder due to another medical condition and describes it as medical disorder with depressive features (i.e., full criteria of MDD is not met), major depressive like and mixed-mood features.
Many elderly patients also present with late-onset dysthymia. Patients with late onset dysthymia are considered to differ from those with young onset dysthymia, in terms of absence of personality disorders and if present, these consist of obsessive–compulsive personality disorder and avoidant personality disorder. There is some evidence to suggest that clinical features of dysthymia in elderly differ from young onset in terms of higher prevalence of comorbid medical illness, presence of cognitive deterioration, and presence of frequent adverse life events and fewer “depressive cognitions” symptoms but similar neurovegetative and other somatic symptoms.
ASSESSMENT AND EVALUATION
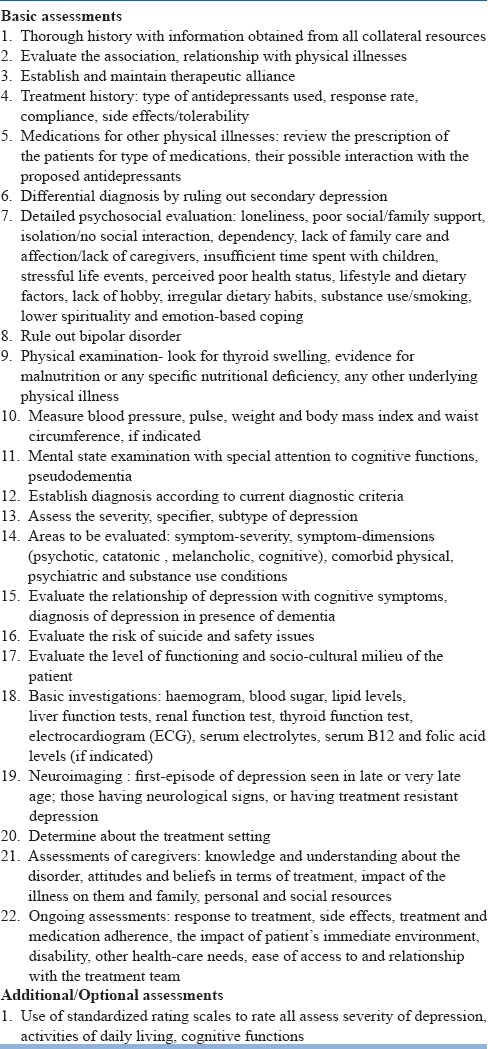
A comprehensive assessment of depression in elderly is of paramount importance to evaluate the risk factors, comorbidity and associated etiological factors, severity of depression, risk of self-harm and level of dysfunction. Additionally, assessment also involves establishing a good therapeutic alliance, deciding about treatment setting and patient's safety. It is important to remember that assessment is a continuous process and patient should be assessed regularly, as per the need and phase of the treatment.
Comprehensive assessment requires elicitation of detailed history including assessment for presence of physical comorbidity, physical examination and mental state examination. All efforts must be made to collect the history from multiple sources, especially from the family members.
The complete psychiatric evaluation involves reviewing history of the present episode and current symptoms, a psychiatric history including evaluation of symptoms of mania to rule out bipolar disorder, evaluation of treatment history in terms of current treatments and responses to previous treatments, history of medical illnesses, history of substance use disorders, personal history (e.g., psychological development, response to life transitions, and major life events), psychosocial history, review of current medications, thorough physical examination with review of all the systems, mental status examination and diagnostic tests as indicated (Table-2).
Table 2.
Components of assessment and evaluation
While assessing elderly for depression, it is important to remember that elderly patients often under-report their depressive symptoms and they may not acknowledge being sad, down or depressed. Common depressive symptoms (such as lack of enjoyment in normal activities, loss of interest in life, apprehension about future, poor sleep, recurrent thoughts of death, persistent unexplained pain, poor concentration or impaired memory) are often misattributed to old age, dementia or poor health. Due to this depression among elderly is often under-detected and untreated for a long time. Many elderly patients with depression often tend to report more somatic and cognitive symptoms than affective symptoms. It has been reported that women more often report mood-related symptoms when compared to men. Patients who do not acknowledge having depressed mood may report a lack of feeling or emotion or acknowledge a loss of interest and pleasure in activities. In view of the reporting of fewer depressive symptoms by elderly patients with depression, some of the authors have suggested the use of the term “depression without sadness”, which is considered as a variant of depression, which is specifically seen in primary care populations and comprises of symptoms of apathy, loss of interest, fatigue, difficulty sleeping, and other somatic symptoms, but not sad mood. However, it is unclear whether “depression without sadness” is an idiopathic depression, a depression secondary to medical illness, or a non-affective syndrome related to chronic medical disease.
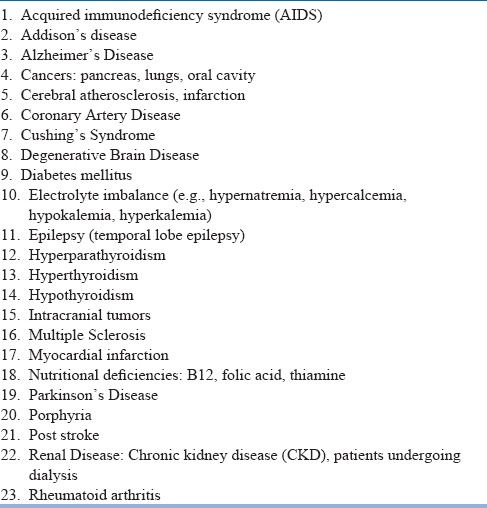
Other barriers to accurate diagnosis of depression among elderly include prevalent stigma and confounding effect of medical co-morbidity. Stigma often prevents effective health care seeking behavior and the accurate reporting of symptoms. Medical comorbidity among elderly patients with depression is a rule rather than an exception. Psychological stress of having an illness, ensuing functional disability, and life changes necessitated by chronic illness may precipitate depression in susceptible individuals. Many physical illnesses have been shown to have high prevalence of depression (Table-3). Accordingly, any elderly individual presenting with first episode depression in the late age must be properly evaluated for underlying physical illnesses. There is significant overlap of symptoms of depression and various medical illnesses and it is often difficult to segregate the attribution of symptoms. Symptoms such as weight loss, fatigue and insomnia may overlap with patients suffering from various physical illnesses. At times, evolution of depression may be indicated by appearance of new onset somatic symptoms, when the physical health was static. Efforts must be made to evaluate anhedonia and depressive ideations like self-deprecation, guilt, etc. The diagnosis of “depression due to a general medical condition” can be used for medical illnesses with a known etiologic link to depression. However, some of the authors consider this terminology to be irrelevant to significant proportion of the elderly patients in whom overall medical burden contributes to their depression. Various approaches have been used for diagnosing depression in medically ill subjects. These include exclusive approach, substitutive approach, best estimate approach and inclusive approach. The “exclusive approach” does not consider neurovegetative symptoms (e.g., changes in sleep, energy, appetite, and weight) to make a diagnosis of depression, whereas the “substitutive approach”, replaces the neurovegetative symptoms included in the nosological system by non-somatic cognitive symptoms (e.g., hopelessness) when defining a major depressive episode (MDD). The “best estimate approach” involves use of clinical judgment to consider whether the symptom is caused by a physical disorder or is part of a depressive syndrome. The “inclusive approach” presumes that all the symptoms contribute to the depressive episode, irrespective of the cause. In general it is suggested that, to overcome the under-recognition of depressive disorders among elderly, an inclusive approach to diagnosis may be preferable in older medically ill patients. However, it is also important to consider all the contributing factors towards the depressive symptoms (e.g., medical causes) to avoid use of unnecessary medications.
Table 3.
Some of the physical illnesses commonly associated with depression
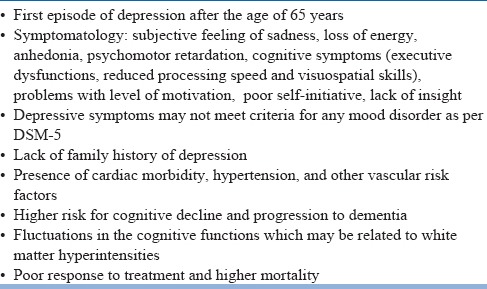
In terms of physical illnesses, it is important to remember that depression among elderly is often associated with presence of hypertension and accordingly vascular risk factors have received considerable attention in the research. This is known as “vascular depression” and newer studies based on magnetic resonance imaging (MRI) suggest that vascular depression accounts for upto 50% of depression in elderly. Patients with vascular depression are considered to have a distinct clinical and neuropsychological profile, which is linked to the presence of hypertension. The MRI findings in such patients include loss of brain volume and loss of white matter integrity. In general vascular depression has been shown to be associated with poor treatment outcomes, higher risk of development of cognitive impairments. Relationship of vascular depression with development of Alzheimer's disease is non-conclusive, with some reports suggesting that these patients have higher risk of progressing to Alzheimer's disease. A review provided the updated information on features of vascular depression and this include: onset of depression at ≥ 65 years of age, absence of family history of depression, presence of executive dysfunctions, loss of energy, subjective feeling of sadness, anhedonia, psychomotor retardation, motivational problems, reduced processing speed and visuospatial skills, deficits in self initiation and lack of insight; and may not meet the criteria for any mood disorder as per the DSM-5, presence of high cardiac illness burden, presence of increased rates of vascular risk factors (hypertension, etc.), fluctuating course of cognitive impairment due to progression of white matter hyperintensities, greater treatment resistance and poorer outcome, higher risk for cognitive decline and association with increased mortality (Table-4). However, it is important to remember that DSM-5 has not incorporated this entity in its classificatory system. Another entity related to vascular depression is depression-dysexecutive syndrome (DES) which is seen in patients with vascular risk factors and is associated with executive dysfunction due to dysfunction in the frontal-subcortical circuit.
Table 4.
Features of Vascular Depression in Elderly
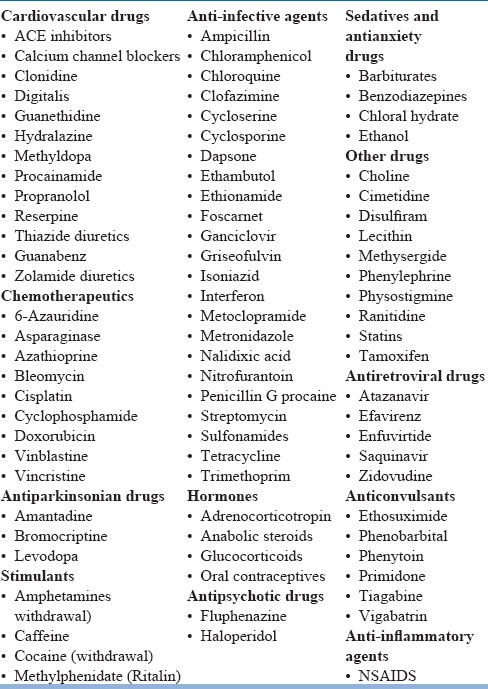
Depression is elderly is also often associated with use of certain medications (Table-5). Accordingly obtaining a detailed treatment history is of paramount importance. The treatment history may not be limited only to the prescription drugs, but should extend to evaluation of over the counter drugs and use of medicines from alternative schools of medicine. It is important to evaluate the temporal correlation of use of medications (starting of medications, escalation of dose of medication) and emergence of depressive symptoms to make any conclusion about the association. However, it is important to note that except for few drugs (e.g. corticosteroids, interferon), evidence for risk of development of depression with specific medications is inadequate and perhaps overstated.
Table 5.
Medications known to cause depression
While assessing depression among elderly it is important to remember that many elderly have atypical presentation of their depression. They may present with chronic unexplained physical symptoms, cognitive symptoms, change in behaviour, anxiety and worries, irritability and dysphoria, etc. However, development of a therapeutic alliance and proper assessment often reveals presence of depressive symptoms in these patients. While evaluating elderly patients, it must be remembered that when neurotic symptoms like hypochondriasis, obsessive compulsive features emerge for the first time in life in old age, than more often than not, these are associated with depression. Accordingly, in all such cases, depression must be ruled out properly. Elderly patients presenting with depression should also be properly evaluated for substance use disorders. At times, elderly patients with depression may present with alcohol dependence arising for the first time in the later life. A thorough history from the patient and an informant often provides clarity. Whenever required, appropriate tests like, urine or blood screens (with prior consent) may be used to confirm the existence of comorbid substance abuse/dependence.
Elderly patients with depression are at higher risk for self-harm and completed suicide when compared to young adults. Depression is the most common risk factor for suicide in elderly. Hence, every patient must be properly evaluated for suicidal behaviours. The risk factor for suicide among elderly and those with depression include older age, male gender, severe anxiety, panic attacks, living alone, severe depression, bereavement (especially in men) and presence of comorbid alcohol misuse, physical pain and history of suicide attempts in the past. Clinicians should directly enquire about the presence of suicidal ideations, planning and availability of means of suicide. If the patient has means to suicide then a judgment may be made concerning the lethality of those means. Family history of suicide also must be inquired into and taken into account while assessing the risk of future self-harm. Patients found to have suicidal or homicidal ideation, intention or plans need to be monitored closely and hospitalization should be considered for those at high risk of self-harm/suicide.
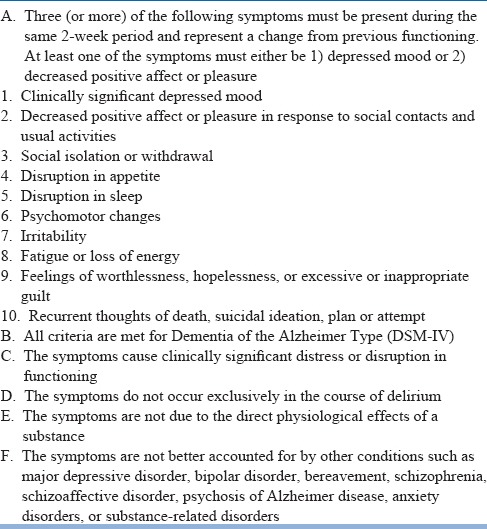
At times depression among elderly is often confused with dementia. Symptoms like apathy, loss of initiative, social withdrawal and cognitive dysfunction (poor attention and concentration) are present in both the disorders. Compared to dementia, depression often have more rapid onset, have evidence of mood change, diurnal variation with morning worsening of symptoms, intact orientation, fluctuating and inconsistent cognitive deficits, may give more ‘don't know’ answers, significant personal distress, disturbed sleep and appetite and suicidal ideations. However, it is important to remember that many patients with dementia also develop depression and it is often missed in such a scenario. Certain symptoms like psychomotor slowing, emotional lability, crying spells, insomnia, weight loss, inability to verbalize affective state and pessimism are seen in both depressed and non-depressed patients with dementia. Some of the studies suggest that patient's with Alzheimer's disease with depression display more self-pity, rejection sensitivity, anhedonia and fewer neurovegetative signs than non-demented depressed older patients. Specific scales like Cornell Scale for depression in dementia, which is considered to be the gold standard for assessing depressive symptoms among patients with dementia, may be used. Combining data from the patient interview, information obtained by caregivers and use of specific scale have been suggested to provide a reliable and valid assessment. The National Institute of Mental Health has developed criteria for diagnosis of depression in patients with Alzheimer's dementia. This includes a list of 10 symptoms, out of which 3 or more must be present during the same 2 week period and represent a change from previous functioning. Out of the 3 criteria fulfilled, at least one of these must be depressed mood or decreased positive affect or pleasure. Other features of the criteria include social isolation or withdrawal, disruption in appetite which is not related to another medical condition, disruption in sleep, psychomotor changes (agitation or slowed behavior), irritability, fatigue or loss of energy, feelings of worthlessness or hopelessness, or inappropriate or excessive guilt and recurrent thoughts of death, suicide plans or a suicide attempt. These symptoms must be present for at least 2 weeks for considering the diagnosis of depression among patients with definite diagnosis of Alzheimer's disease as per the DSM-IV criteria. The symptoms must be associated with clinically significant distress or disruption in function; symptoms are not part of delirium, are not related to physiological effect of substance and are not accounted by other psychiatric conditions (Table-6).
Table 6.
NIMH Provisional Diagnostic Criteria for Depression in Alzheimer Disease
An important aspect for evaluation of depression in elderly also involves evaluation for nutritional deficiencies which may be responsible for the depressive symptoms and correction of these may be sufficient to manage depressive symptoms.
Due attention must be given to psychosocial factors which may be associated with onset, continuation/maintenance of depression among elderly. Various psychosocial factors associated with depression among elderly include loneliness, poor social/family support, isolation/no social interaction, dependency, lack of family care and affection/lack of caregivers, insufficient time spent with children, stressful life events, perceived poor health status, lifestyle and dietary factors, lack of hobby, irregular dietary habits, substance use/smoking, lower spirituality and emotion-based coping.
Before considering the diagnosis of unipolar depressive disorders, it is important to ascertain that patient does not have bipolar disorder as use of antidepressants in patients with bipolar disorder can lead to antidepressant induced switch. Elderly patients presenting with depressive disorders often do not come up with history of previous hypomanic or manic episodes. Meticulous history from the patient, family members, review of treatment records often provide important clues and aid in confirming the diagnosis of bipolar disorder. At times use of standardized scales like mood disorder questionnaire can help in detecting bipolarity. Some of the clinical features which should alert a clinician about the possibility of bipolar disorder include presence of psychotic features, marked psychomotor retardation, reverse neurovegetative symptoms (excessive sleep and appetite), irritability of mood, anger and family history of bipolar disorder.
Evaluation of history should also take the longitudinal life course perspective to evaluate for previous episodes and presence of symptoms of depression amounting to dysthymia. History taking should look at the relationship of onset of depression with change in season (seasonal affective disorder) and relationship with menopause etc. Response to previous treatment should also be reviewed and whether the patient achieved full remission, partial remission and did not respond to treatment should be evaluated.
Elderly patients are at higher risk of completed suicide when compared with the young patients.
Depression is associated with marked dysfunction in the domains of interpersonal relationships, work, living conditions, activities of daily living, instrumental activities of daily living, and other medical or health-related needs. At baseline, these need to be noted and subsequently monitored. If feasible, standard scales may be used to record these dysfunctions. The areas of dysfunction must be addressed by encouraging the patient to set realistic, attainable goals for themselves in terms of desirable levels of functioning.
All the elderly subjects with depressive disorders need to be investigated. The list of investigations is generally guided by the physical evaluation and history of medical illnesses. However, it is important to remember that if at all there is no historical evidence of medical illness and nothing significant is found in physical examination to warrant laboratory investigation then also the elderly patients should be subjected to a minimum battery comprising of haemogram, liver function tests, renal function tests, urine analysis, electrocardiography (ECG) and serum electrolytes. Some authors also advise to consider thyroid function tests, vitamin B12 and folate levels and serum levels of drugs received by the patient. Neuroimaging may be considered in those with in late or very late onset first episode depression, those having associated neurological signs and those experiencing treatment resistant depression.
Besides, obtaining information from the patients and caregivers, it is also important to evaluate their knowledge and understanding about the symptoms and the disorder, their attitudes and beliefs about the symptoms and treatment, the impact of the illness on them and their personal and social resources.
Many a times, elderly patients with depression present to the primary care to the physicians, who may require assistance of screening questionnaires to diagnose depression in elderly. The available questionnaires include Geriatric Depression Scale (GDS), Evans Liverpool Depression Rating Scale (ELDRS), Brief Assessment Schedule (BASDEC) and Patient Health Questionnaire (PHQ-9). However, it is important to note that these are screening questionnaires/scales, and detailed interview will be required for confirming the diagnosis. It also important to remember that level of cognitive impairment and visual deficits must be taken into account while asking the patients to complete these questionnaires or while administrating these questionnaires. Out of these 3 questionnaires, GDS is available in Hindi.
Scales can also be used to rate the severity of depression among elderly. The various scales which can be used include Hamilton Rating Scale for Depression (HAM-D), Zung Self-Rating Depression Scale (SDS), Geriatric Depression Scale (GDS), Beck Depression Inventgory (BDI), Montgomery-Asberg Depression Rating Scale (MADRS) and Cornell Scale for Depression in Dementia (CSDD). Among the various scales, GDS is the most well validated scale for use in elderly with intact cognitive functions.
Formulating a treatment plan
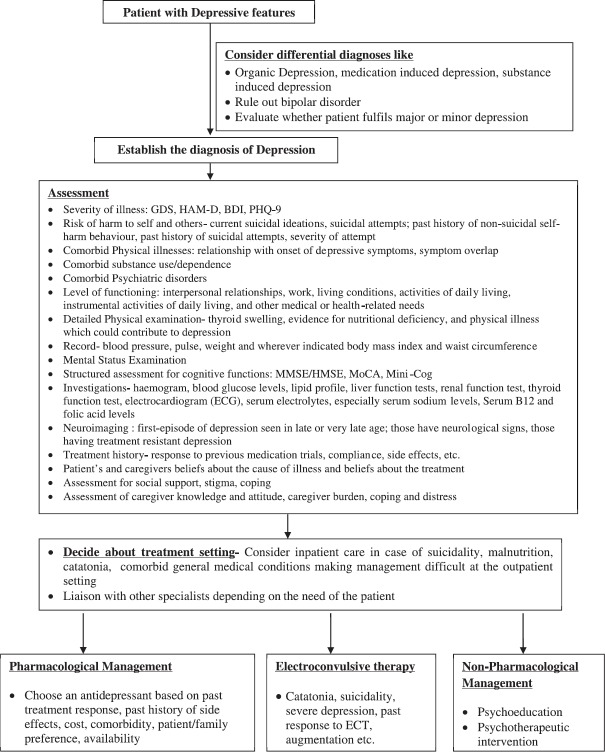
Formulation of treatment plan involves deciding about treatment setting, medications to be prescribed and psychological interventions to be used (Figure-1). Wherever possible, the patients may be involved in preparing the treatment plan. Caregivers must also be consulted in formulating a treatment plan. The role of caregivers becomes more important when the patient is not in a condition to participate in treatment decisions due to severity of the depression, lack of insight or marked cognitive impairment. The treatment plan needs to be practical, feasible and flexible to attend to the needs of the patients and caregivers. The treatment plan initially formulated need to be continuously re-evaluated and updated as per the clinical and psychosocial needs.
Figure 1.
Initial evaluation and management plan for Depression
DETERMINE A TREATMENT SETTING
Patients with depression can be managed on the outpatient basis. However, it is recommended that patients be managed in a setting which is most safe and effective. The decision about treatment setting must take into account symptom severity, comorbid physical and psychiatric conditions, suicidality, homicidal behaviour, level of functioning and available support system. It should also take into consideration the ability of a patient to adequately care for themselves, provide information about the health status to the clinician and cooperate with treatment. Further, this should be an ongoing process throughout the course of treatment. Some of the indications for inpatient care are given in Table-7.
Table 7.
Indications for admission in elderly patients with depression
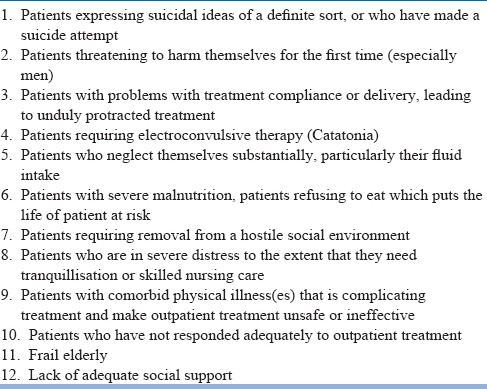
All inpatients should have accompanying family caregivers. In case inpatient care facilities are not available, then the patient and/or family must be informed about such a need and admission in nearest available inpatient facility can be facilitated.
ESTABLISH AND MAINTAIN A THERAPEUTIC ALLIANCE
Irrespective of the use of various treatment modalities, it is important for the clinicians to establish a therapeutic alliance with the patient. Depression often runs a chronic course and requires patients to actively participate and adhere to treatment for long periods. Another important aspect of successful treatment is tolerating the side effects of various treatment modalities. For these reasons, a strong treatment alliance is crucial. For clinicians, it is important to understand that paying attention to the concerns of patients and their families as well as their wishes for treatment enhances the therapeutic alliance.
MONITOR THE PATIENT'S PSYCHIATRIC STATUS AND SAFETY
Management of depression is an ongoing process, which requires continuous assessment of course of symptoms and acceptability of treatment. Accordingly, it is important to be on surveillance for emergence of destructive impulses towards self or others and hospitalization or more intensive treatment need to be considered for patients at higher risk. At times, patients may present with significant changes in psychiatric status or emergence of new symptoms, which may warrant a diagnostic re-evaluation of the patient.
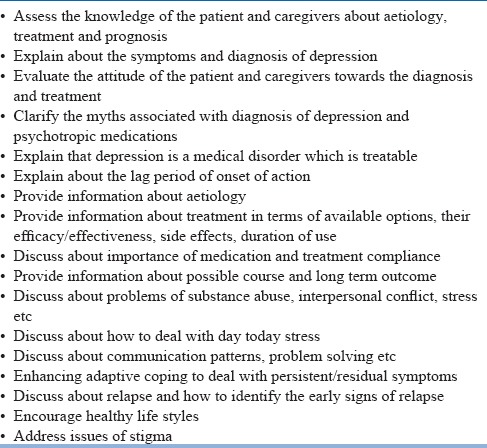
PROVIDE EDUCATION TO THE PATIENT AND, WHEN APPROPRIATE, TO THE FAMILY
All patients and their caregivers need to be educated about symptoms of depression, available treatment modality, course of disorder and time to response to treatment. Specific educational elements may be helpful in some circumstances, e.g. that depression is a real illness and that effective treatments are both necessary and available may be crucial for patients who attribute their illness to a moral defect, witch craft or harbour other supernatural causation for their depressive disorder. Education regarding available treatment options will help patients make informed decisions, anticipate side effects and adhere to treatments. Another important aspect of providing education is informing the patient and especially family about the lag period of onset of action of antidepressants.
ENHANCE TREATMENT ADHERENCE
Adequate management of depression requires adherence to treatment plans. Many elderly patients may attach stigma to depression and disagree with clinicians when informed about their diagnosis. Patients also often fear of becoming addicted to antidepressants and the impact of psychotropics on their medical disorders. Sometimes, patients who are overtly symptomatic may be poorly motivated and unduly pessimistic about their chances of improvement with treatment. On the other hand, many patients, who achieve clinical remission with treatment may underestimate the need for continued treatment and consider it as a burden. Some patients may not be able to take care of themselves due to cognitive deficits. Side effects are also well known to contribute to treatment non-adherence.
Accordingly, treatment adherence can be improved by informing the patients about when and how often to take medicine, lag period of onset of action (at least 3-4 weeks will be required for the beneficial effects to emerge), the need to take medication even after feeling better, the need to consultation prior to discontinuing medication, what is to be done in the face of side effects and what is to be done, in case of a problem. Medication adherence among elderly can also be improved by simplifying the treatment regimen and reducing the cost of treatment. If the patient has severe, persistent or recurrent non-adherence with treatment, than there may be a need to evaluate the psychological conflicts or psychopathology which may be contributing to the non-adherence. Appropriate measures must be taken to address these issues. Family members must be involved in all stages of treatment and all form of psychoeducation, as they can play an important role in enhancing treatment adherence.
ADDRESS THE ISSUE OF EARLY SIGNS OF RELAPSE
Patient and family members need to be informed about the chances of relapse after improvement. Information need to be provided in terms of recognising early signs and symptoms of new episodes, need for seeking treatment at the earliest to reduce the chance of development of full-blown relapse.
TREATMENT OPTIONS FOR MANAGEMENT FOR DEPRESSION
The available treatment options for management of depression can be broadly categorised into antidepressants, somatic treatments and psychosocial interventions. The various somatic treatments include electro-convulsive therapy (ECT) repetitive transcranial magnetic stimulation (rTMS), transcranial direct stimulation, vagal nerve stimulation and deep brain stimulation. Other some of the less commonly recommended treatments include light therapy and sleep deprivation. Besides these, benzodiazepines are often prescribed as adjunctive treatment during the initial phase of treatment. Patients who do not respond to the first line treatments may require use of lithium and thyroid supplements as augmenting agents.
Depression can be managed with a whole range of antidepressant medications (Table-8). Antidepressants are the usually preferred modality of treatment for mild, moderate, or severe depressive episode. Psychotherapeutic treatments are usually indicated for management of patients with minor depression and mild to moderate major depression. Clinical features that may guide the choice of use of psychotherapeutic treatments include the presence of significant psychosocial stressors, intrapsychic conflict, interpersonal difficulties, or axis II comorbidity. Many times, patients themselves may be averse to use of antidepressants and express desire for psychotherapeutic treatments as the initial treatment modality. In such a scenario, patient's preference must be respected. Combination of antidepressants and psychotherapeutic interventions may be useful initial treatment choice for patients with psychosocial stressors, intrapsychic conflict, interpersonal problems, or a comorbid axis II disorder together with moderate to severe major depressive disorder. Other indications for combined treatment with antidepressants and psychotherapy include partial response to adequate trials of antidepressants or psychotherapeutic interventions and patients who are poorly adherent to pharmacotherapy. Presence of psychotic symptoms may suggest combined use of antidepressant and antipsychotic medications or ECT. Other indications for ECT include presence of catatonic features not responding to benzodiazepines (e.g. lorazepam), high risk of suicidality, presence of comorbid general medical conditions precluding the use of antidepressant medications, patients refusing food and are nutritionally compromised and those who have a past history of positive response to ECT. The patient preference is another important consideration that may influence the decision to select ECT as a treatment modality. However, it is to be remembered that ECT is relatively contraindicated in patients with recent myocardial infarction, brain tumor, cerebral aneurysm, and uncontrolled heart failure.
Table 8.
Antidepressants Armamentarium
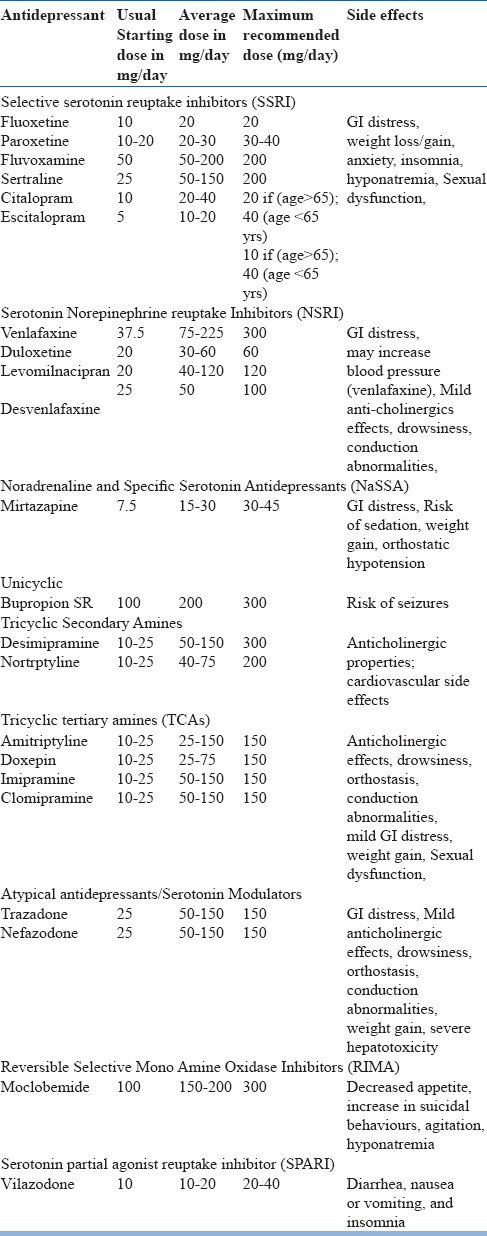
Selecting specific antidepressant: In general, there is no difference in the efficacy of various antidepressants in management of depression. A metanalysis, which included 51 randomised controlled trials (RCTs) comparing various antidepressants medications showed lack of significant difference in the efficacy of various antidepressant classes. Studies which have compared various antidepressants head-to-head show that there is lack of difference in the efficacy of escitalopram, citalopram, sertraline and paroxetine. Another meta-regression analysis, which included 34 RCTs showed lower response rate to various antidepressants in patients of male gender, older age and those having longer duration of current episode. Better response rate was seen in patients with higher baseline severity of depression and those experiencing first episode of depression.
Hence selection of antidepressant is guided by other features which can be broadly divided into patient specific and drug specific factors. The patient specific factors include patient preference, past history of response/tolerability to medication, family history of response to a particular antidepressant, comorbid medical illness, comorbid psychiatric disorder/symptoms, other medication being taken and intellectual and psychological capacities. The drug specific factors include the anticipated side effects, the safety or tolerability of these side effects for individual patients, cost, dosing schedule, type of formulations available and safety in overdose. Elderly people are generally more susceptible to anticholinergic effects, and the newer antidepressants should therefore be preferred. If a tricyclic antidepressant has to be used, drugs with pronounced anticholinergic effects, such as amitriptyline, should be avoided. Antidepressants associated with side effects like hypotension, and those with highly sedating properties must be avoided.
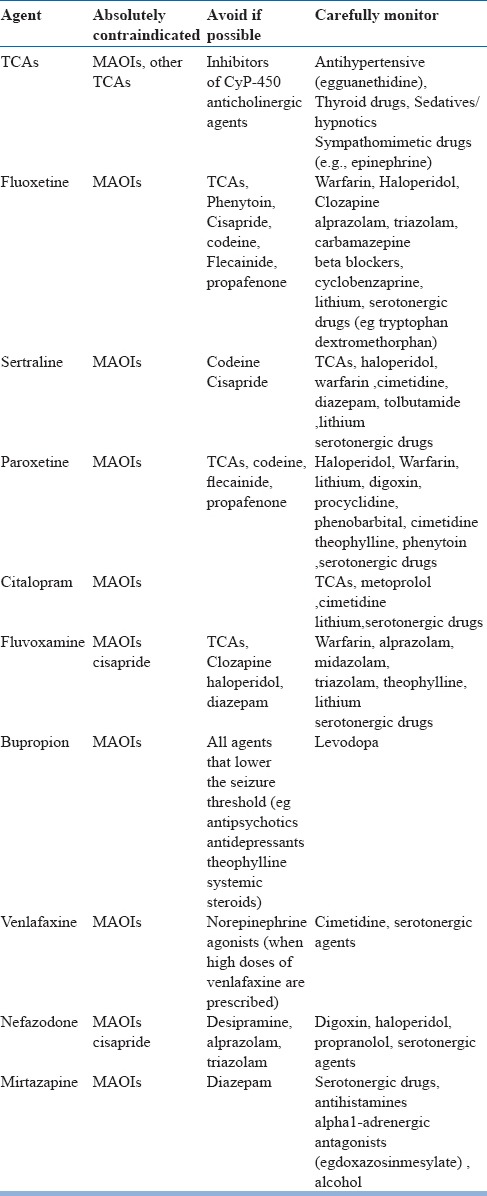
Among the cyclic compounds, desipramine is less sedating and can be taken during the day, and nortriptyline is less likely to cause orthostatic hypotension than amitriptyline or imipramine. Although MAOIs are thought to be dangerous and difficult to use, drugs such as phenelzine are relatively safe and effective in older patients. However, it is important to remember that MAO inhibitors are associated with development of hypotension, hypertension, and food-drug interactions. Moclobemide is well tolerated by older people. Although a special diet is not required, patients should be aware of the drug interactions with painkillers and other antidepressants. Blood pressure monitoring is necessary with venlafaxine in patients with pre-existing cardiovascular disease and patients taking relatively high dosages. Nefazodone works well in patients with anxiety and depression. Gastrointestinal symptoms side effects with SSRIs are well known. Among the SSRIs sertraline and citalopram have the least potential for drug interactions. For clinicians it is important to remember that the antidepressant effect may be more delayed in elderly people than in younger subjects, and treatment may need to be continued for longer than six months. A small proportion of elderly patients who are prescribed antidepressants may go on to develop hyponatremia. Hyponatremia is usually seen during the initial phase of treament. The various risk factors for development of hyponatremia include older age, female gender, low body weight, presence of comorbid physical illnesses (i.e., diabetes mellitus, hypertension, hypothyroidism, chronic obstructive pulmonary disease, cardiac failure, head Injury, stroke, cirrhosis of liver and presence of malignancies), concomitant use of other medications (i.e., diuretics, antihypertensives, antidepressants, cytochrome P450 inhibitors), past history of hyponatremia, low baseline serum sodium levels, summer season and initial phase of antidepressant therapy. Accordingly, some of the authors suggest evaluating the baseline serum sodium levels in all elderly patients prior to initiation of antidepressants and monitoring the same during the initial phase of treatment. Other rare but life-threatening side effects of antidepressants include upper gastro-intestinal (GI) bleeding. It is in general suggested to be more common in elderly compared to young adult patients. Antidepressants, specifically those which act on serotonergic system, decrease platelet aggregation and increase the risk of bleeding. Risk of serotonergic antidepressants associated GI bleed is high in elderly, those with history of peptic ulcers, gastritis, oesophageal varices, gastric or colorectal cancers, chronic alcohol use, liver disease, coagulopathies and concomitant use of other medications (i.e., corticosteroids, warfarin, clopidogrel, aspirin and other non-steroidal anti-inflammatory agents, calcium channel blockers, concomitant use of more than one antidepressant). Accordingly, if required antidepressants are to be used, these must be used under the cover of proton pump blockers, to reduce the risk of GI bleeding. Possibility of drug interactions must always be kept in mind while selecting an antidepressant and certain combinations must be avoided (Table-9). The most clinically significant drug interactions usually involve inhibition or induction of CYP450 enzymes. Accordingly, the clinicians can use ready reckoner or online drug interaction calculators to evaluate for the possible drug interactions.
Table 9.
Monitor or avoid following combinations in elderly
In general, SSRIs are considered to be the first line antidepressants because of the side effect and safety profile. Other alternatives include tricyclic antidepressants, mirtazapine, bupropion, and venlafaxine.
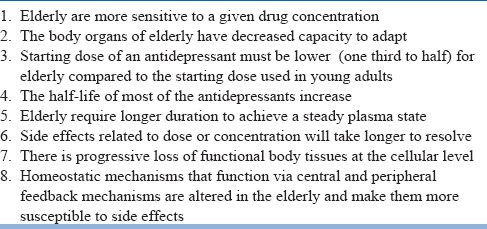
Institution of antidepressant therapy: While using antidepressants among elderly, it is important to take age related pharmacokinetic and pharmacodynamic changes into consideration (Table-10). Accordingly, it is suggested that antidepressants must be started in lower doses and the general principle of “start low and go slow” need to be followed. Usually the medication must be started in the lower doses and the doses must be titrated upwards, depending on the response and the side effects experienced. Patients started on antidepressants need to be monitored carefully to assess the response to pharmacotherapy as well as the emergence of side effects and safety. Factors which influence the frequency of monitoring include severity of illness, patient's co-operation with treatment, the availability of social support and the presence of comorbid general medical problems. The dose of antidepressants can be titrated to the full therapeutic doses over the initial weeks of treatment, but it is usually guided by the development of side effects and the presence of comorbid conditions. Patients need to be monitored closely for response to pharmacotherapy as well as the emergence of side effects, clinical condition, and safety. Visits should be frequent enough to monitor and address suicidality and to promote treatment adherence. The frequency of monitoring during the acute phase of pharmacotherapy can vary from once a week in routine cases to multiple times per week in more complex cases. Clinicians should also reassure patients that they may feel worse before they start to feel better.
Table 10.
Points to remember for prescription of antidepressants in elderly
The dose of antidepressants can be increased if patient compliance is good and there is no response during the initial 3 weeks of treatment. If partial response to treatment is noted that, clinician can wait for another 2 weeks before escalating the dose. Improvement with pharmacotherapy can be observed after 4-6 weeks of treatment. If at least a moderate improvement is not observed in 4-6 weeks, reappraisal and adjustment of the pharmacotherapy should be considered.
Although there is lack of consensus, but most experts agree that elderly patients require longer time than young adults to perceive any improvement and moderate improvement with pharmacotherapy is seen after 4–8 weeks of treatment, but 2 to 3 months of therapy are necessary to achieve the full benefit of treatment. The delayed clinical response to antidepressants makes it difficult to establish the optimal dose quickly. The individual dose is usually decided by trial and error. The patient is usually the last to notice a change, and others often will tell the person that he/she looks better than before.
At least 30% of elderly patients with depression do not respond to first-line treatment with an antidepressant. If at least moderate improvement is not observed following 4–8 weeks of pharmacotherapy, a thorough review must be done for re-evaluation of diagnosis, treatment adherence and pharmacokinetic/pharmacodynamic factors which may be affecting treatment. Treatment plan must be revised by implementing one of several therapeutic options, including maximizing the initial medication treatment, switching to another antidepressant medication, augmenting antidepressant medications with other agents, psychotherapy, or ECT. Maximizing the initial treatment regimen is perhaps the most conservative strategy. Patients who show partial response, particularly those with features of personality disorders, antidepressant medication trial should be extended as it may allow some patients to respond more fully. Use of higher antidepressant doses may be helpful for patients who have received only modest doses. Patients who have had their dose increased, should be monitored for an increase in the severity of side effects or emergence of newer side effects.
Switching to a different antidepressant medication is a common strategy for treatment-refractory patients, especially those who have not shown at least partial response to the initial medication regimen. There is no consensus about switching and patients can be switched to an antidepressant medication from the same pharmacologic class (e.g., from an SSRI to another SSRI) or to one from a different pharmacologic class (e.g., from an SSRI to a tricyclic antidepressant). Some expert suggests that while switching, a drug with a different or broader mechanism of action should preferably be chosen. While switching to a second antidepressant, clinicians should remember that there is some evidence to suggest that venlafaxine may be useful in patients, who don't respond to initial pharmacotherapy.
Augmentation of antidepressant may be considered in patients who show partial response to initial antidepressant monotherapy. Options include adding a second antidepressant medication from a different pharmacologic class, or adding another adjunctive medication such as lithium, psychostimulants, modafinil, thyroid hormone, an anticonvulsant etc. Adding, changing, or increasing the intensity of psychotherapy should be considered for patients with MDD who do not respond to medication treatment. Following any change in treatment, the patient needs to be closely monitored. If at least moderate level of improvement is not seen after an additional 4–8 weeks of treatment, the psychiatrist another thorough review need to be carried out. This reappraisal should include verifying the patient's diagnosis and adherence; uncovering and addressing clinical factors that may be preventing improvement, such as the presence of comorbid general medical conditions or psychiatric conditions (e.g., alcohol or substance abuse); and uncovering and addressing psychosocial issues that may be impeding recovery. If no new information is uncovered to explain the patient's lack of adequate response, ECT should be considered.
Psychotherapeutic interventions
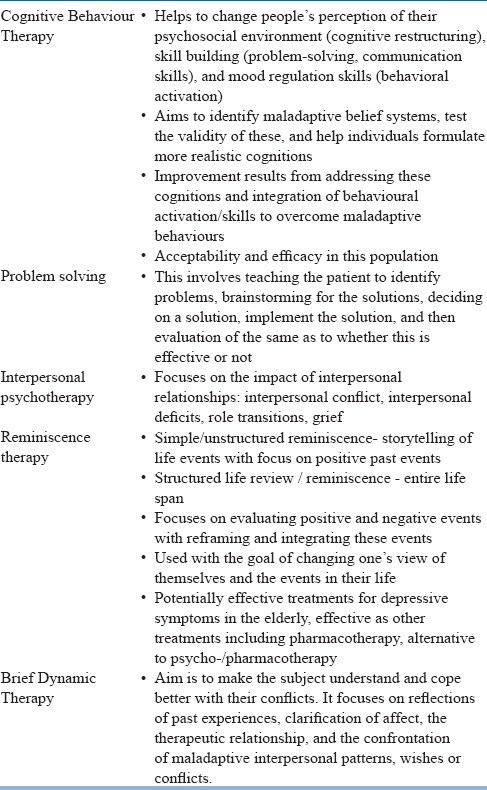
Out of the various psychotherapeutic models used in elderly, cognitive behavior therapy (CBT)/Problem solving techniques, interpersonal psychotherapy (IPT), Brief dynamic therapy and reminiscence therapy have been found to have some evidence (Table-11). Use of psychotherapy is often guided by the patient preference and the availability of clinicians with appropriate training and expertise in specific psychotherapeutic approaches.
Table 11.
Psychotherapeutic interventions for elderly patients with depression
Medications plus psychotherapy
As in adults, there is some data to suggest that combination of pharmacotherapy and psychotherapy is better than monotherapies in the treatment of late-life depression.
Psychoeducation to the patient and, when appropriate, to the family
Psychoeducation of patients and family members must be integral part of all treatment packages. Psychoeducation need to address the issues of knowledge about the illness, available treatment options, time to response, side effects with medications, need for medication and treatment adherence, providing information about the course and outcome, impact of stressors on the course of illness, improving adaptive coping skills, risk of relapse and identification of early signs of relapse, address stigma and encourage maintenance of healthy life style. Important components of psychoeducation are given in table-12.
Table 12.
Basic components of Psychoeducation
ECT in Elderly:
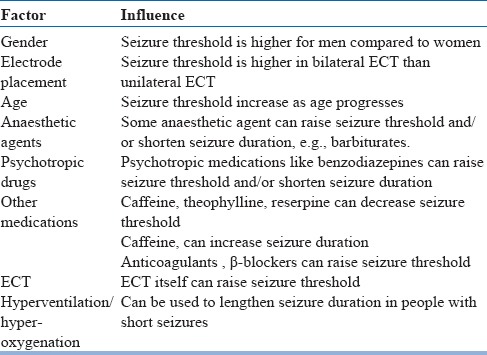
Available data suggests that ECT is as effective in management of depression in elderly as in adults. Data also suggest that ECT is well tolerated in patients of old age depression even by subject aged more than 80 years of age. Studies which have compared ECT with antidepressants suggest that it is more effective than antidepressants. Over the years it is increasingly understood that there is no absolute contraindication for ECT. The potential risk and benefit should be weighed on case to case basis and where ever warranted the medical treatment should be optimized before ECT. Data suggests that the risk of complications in elderly is more among those receiving more number of medications, especially those who are on more number of cardiovascular medications. However, studies have shown that cardiovascular complications arising during ECT are transient and don't prevent successful completion of treatment course. The commonly reported side effects of ECT include an increased risk of falls, post-ECT delirium or dementia. Data suggests that elderly patients with compromised medical status are at highest risk for prolonged confusion. Occasional study has also evaluated the effectiveness of ECT in the continuation/maintenance phase of treatment and this suggests that the risk of relapse/recurrence with ECT plus nortriptyline is significantly lower than nortriptyline alone. However, while using ECT among elderly, certain facts, which can influence the seizure threshold and seizure duration must be kept in mind (Table-13). In general, it is important to remember that seizure threshold increases with age. Elderly patients also require modifications of doses of anticholinergic, anesthetic, and relaxant agents in view of the physiological changes associated with aging. Patients receiving ECT should be closely monitored for emergence of cognitive side effects. Patients with pre-existing cognitive deficits are more vulnerable to the development of cognitive side-effects during the course of ECT and are at risk of having longer lasting cognitive side-effects. Cognitive side effects can be minimized by use of high-dose right unilateral ECT in place of the bilateral ECT.
Table 13.
Factors influencing seizure threshold and/or seizure duration
Repetitive Transcranial Magnetic Stimulation (rTMS):
rTMS has been used in the management of depression. It is usually not the first line treatment. Repetitive TMS applied to the left dorsolateral prefrontal cortex (DLPFC) has been shown to have beneficial effect. However, still there is lack of consensus about the exact brain localization for individual coil placement. RCTs which have evaluated the role of rTMS in management of depression in elderly, suggest that rTMS does not have any beneficial effect at 2 weeks. However, few RCT reported positive outcome in patients with refractory depression /treatment resistant depression. Recent data from RCTs suggest that rTMS is equally effective in young and older (>60years) patients.
PHASES OF ILLNESS/TREATMENT
Management of depression is divided into three phases, i.e., acute phase, continuation phase and maintenance phase. Maintenance phase of treatment is usually considered when patient has recurrent depressive disorder (RDD).
ACUTE PHASE TREATMENT
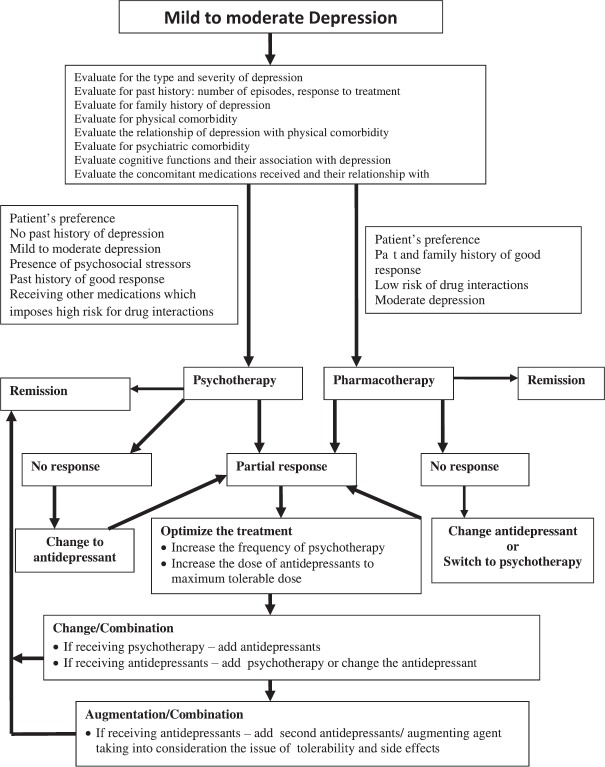
Acute phase treatment must aim to achieve remission. The various components of acute phase treatment are shown in Table-14. Selection of initial treatment depends on severity of depression and patients preferences. The first and foremost thing for starting treatment is thorough evaluation (Figure 2 and 3) and deciding about treatment strategies after considering the severity of the symptoms.
Table 14.
Management in the Acute Phase
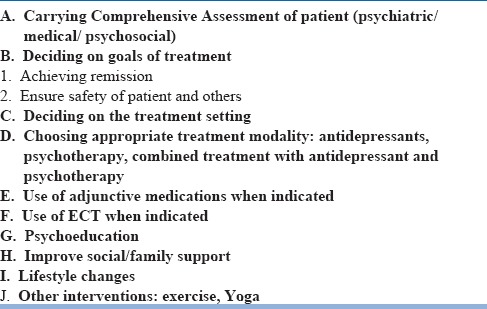
Figure 2.
Treatment algorithm of mild to moderate Depression in elderly
Figure 3.
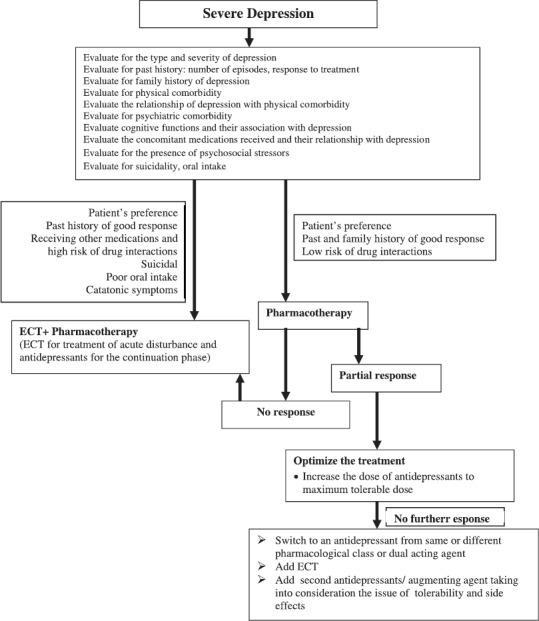
Treatment algorithm of Severe Depression in elderly
Antidepressant medications may be used as initial treatment modality for patients with any level of severity (mild, moderate, or severe). Features that suggest that medications may be the preferred treatment modality include history of previous response to antidepressants, severity of symptoms, presence of marked sleep and appetite disturbances or agitation, or anticipation of the need for maintenance therapy. Combination of antidepressant and antipsychotic medication and/or ECT may be preferred for patients with severe depression with psychotic features. Selection of specific antidepressant is usually guided by the comorbid physical illnesses, possible side effects, the tolerability of these side effects for individual patients, patient preference, and concomitant pharmacotherapy. Usually, SSRIs are considered as the first line treatment of choice. Among the various SSRIs, escitalopram and sertraline are considered to have minimal drug interactions and are considered to be safe in presence of wide range of physical illnesses. In addition to the use of antidepressants, depending on the symptom severity and type of symptoms, such as presence of insomnia or anxiety, benzodiazepines or other hypnotics may be used for short duration. When used, these must be used for shortest possible duration and the patients and the caregivers must be informed about the anticipated side effects and risks of over-sedation. Improvement with pharmacotherapy can be observed after 4-6 weeks of treatment. Additionally, depending on the concomitant medications, proton pump blockers may be used to minimize the GI side effects and to reduce the risk of GI bleeding. During the initial phase of treatment serum sodium levels may also be monitored, depending upon the presence of risk factors. The principle of “start low and go slow”, must be adhered to and it must be remembered that elderly usually require lower doses of antidepressants than the adults. The usual starting dose which is recommended is half of the adult dose. In presence of comorbid physical illnesses, the usual starting dose in an elderly may be one-fourth of the adult dose.
If some improvement (>25%) is not apparent after continuing antidepressants for 6 weeks, the treatment should be reviewed and a change of antidepressant needs to be considered. When patient shows 25-50% improvement after the initial 4-6 weeks of antidepressant trial, the dose must be increased to the maximum tolerable dose. If there is less than 50% improvement with 6-8 weeks of maximum tolerable dose and the medication compliance is good, a change in antidepressant may be considered.
If moderate improvement is not evident even after 4-8 weeks of pharmacotherapy, then a thorough review with review of the diagnosis, complicating conditions and issues, and treatment plan need to be carried out (Figure-4). Reappraisal of the treatment regimen also includes evaluation of patient adherence and pharmacokinetic/pharmacodynamic factors. After the review, the treatment plan can be redesigned by implementing one of several therapeutic options, including maximizing the initial medication treatment, switching to another antidepressant medication and augmenting antidepressant medications with other agents/psychotherapy/ECT. Maximizing the initial treatment regimen is possibly the most conservative strategy. It is important to note that, while using the higher therapeutic doses, it is important to closely monitor the patient for an increase in the severity of side effects or emergence of newer side effects.
Figure 4.
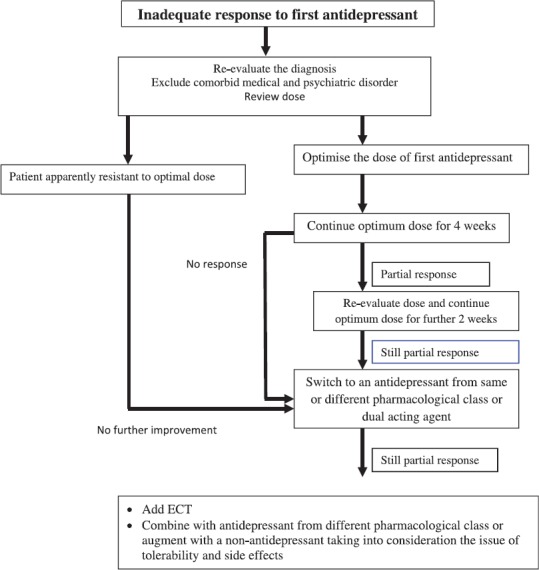
Treatment algorithm for inadequate response to first antidepressant therapy in elderly
For treatment-refractory patients, switching to a different antidepressant medication, especially those who have not shown at least partial response to the initial medication regimen is a common strategy. There is lack of consensus about switching and a patient can be switched to an antidepressant medication from the same pharmacologic class (e.g., from an SSRI to another SSRI) or a different pharmacologic class (e.g., from an SSRI to a tricyclic antidepressant). In general it is suggested that while switching, a drug with a different or broader mechanism of action may be chosen.
Among patients who show partial response to initial antidepressant monotherapy, augmentation with another agent may be considered. Augmentation can be done with a second antidepressant medication from a different pharmacologic class, or adding agents like lithium, psychostimulants, modafinil, thyroid hormone, an anticonvulsant etc. Adding, changing, or increasing the intensity of psychotherapy may be considered for patients who do not respond to medication treatment. Close monitoring of patient need to be done at the time of change and after the change. If change of treatment strategy do not yield at least a moderate level of improvement after an additional 4–8 weeks of treatment, than another thorough review need to be carried out. This reappraisal may include reviewing the diagnosis and patient's medication adherence; looking for and addressing clinical factors that may be impeding improvement, such as the presence of comorbid general medical conditions or psychiatric conditions (e.g., alcohol or substance abuse); and identifying and addressing psychosocial issues that may be preventing recovery. If no new information emerges which can explain the patient's inadequate response, depending on the severity of depression, ECT may be considered.
Psychotherapeutic interventions: The importance of psychotherapeutic interventions does not diminish with increasing age. Available data suggest that in elderly patients with mild to moderate depression, psychotherapeutic interventions are as effective as antidepressants. Some of the studies also suggest that elderly often have better treatment compliance, lower dropout rates, and more positive responses to psychotherapy than younger patients. Cognitive behavior therapy (CBT) and interpersonal psychotherapy (IPT) have been found to have sufficient evidence for management of depression in elderly. However, it is important to note that studies which have evaluated the effectiveness of psychotherapy in elderly with depression have done so in cognitively intact and medically stable patients and effectiveness outside this patient group is not fully established. Small studies and case reports suggest that CBT can be adapted for physically frail patients and those with mild cognitive impairment, but further research is needed. Use of psychotherapy is often guided by the patient preference and the availability of clinicians with appropriate training and expertise in specific psychotherapeutic approaches. In terms of clinical factors, psychotherapy is usually recommended for elderly patients with mild to moderate depression who have evidence of stressful life events, family conflicts, and the reduction or absence of social support. In a country like India, where there is scarcity of trained psychotherapists, clinicians can also use psycho-educational approach and supportive psychotherapy. In general the basic principle which should guide any kind of supportive psychotherapy should involve use of adaptive strengths that have served the patient well in the past, increasing the patient's self-esteem, accepting feelings at face value, holding the prospect of hope and accepting anger and irritability.
While using psychotherapy, the frequency of sessions must be guided by type and goals of the psychotherapy, the frequency necessary to create and maintain a therapeutic relationship, the frequency of visits required to ensure treatment adherence, and the frequency necessary to monitor and address suicidality. Other factors which also influence the frequency of psychotherapy sessions include severity of illness, the patient's cooperation with treatment, the availability of social supports, cost, geographic accessibility, and presence of comorbid general medical problems.
Regardless of the type of psychotherapy selected, the response to treatment should be carefully monitored and if the patient's condition fails to stabilize or deteriorates, reassessment needs to be carried out. If after 4–8 weeks of treatment at least a moderate level of improvement is not observed, then a thorough review and reappraisal of the diagnosis, complicating conditions and issues, and treatment plan should be conducted. In many cases, the treatment plan can be revised by the addition or substitution of pharmacotherapy. Following any revision or refinement of treatment, the patient should continue to be closely monitored.
Medications plus psychotherapy: Available data supports the superiority of the combined treatment over the use of monotherapies. Selection of pharmacotherapy and psychotherapy in patients considered for combined treatment must be guided by the same variables, which determine the use of these treatments as monotherapies. While using combined treatment, same doses of antidepressant medication and the same frequency and course of psychotherapy should be used as is employed for patients receiving these as a monotherapy. Patients receiving combined antidepressant medication and psychotherapy should also be monitored closely for treatment effect, side effects, clinical condition, and safety. If after 4–8 weeks, there is not at least a moderate improvement, a thorough review should be conducted, including of the patient's adherence and pharmacokinetic/pharmacodynamic factors affecting treatment. The treatment plan can be revised by using many of the same therapeutic options described for patients who have not responded to treatment with either modality alone. Following any change in treatment, the patient should be monitored, and if at least a moderate improvement is not seen after an additional 4–8 weeks of treatment, another thorough review should be carried out.
Improve Social Support/family support: Addressing the issue of social support in elderly patients with depression is very important. In many elderly patients psychosocial issues like social isolation, neglect by the family etc contribute to the onset and or continuation of depression. Accordingly efforts must be made to improve the social support of the patient. Family members must be encouraged to provide emotional support and affection. Family members must be asked to show patience, listen to the patient, be understanding and encouraging. If patient expresses suicidal ideations, plans or talks about death, than they should take it seriously and family members should liaise with the treating agencies. Family members must be informed that they should refrain from being critical. Family members can also help in supervising the medications.
Life style modifications: Besides pharmacotherapy, psychotherapy and improving social support, it is important to look at the life style issues and patients must be encouraged to maintain a regular activity schedule, go for walks depending on the physical health status, socialize and engage themselves cognitively.
Other interventions: There is some data to suggest that aerobic exercises have a positive effect on depressive symptoms, executive function and psychological well being. It has also been shown that Yoga and mindfulness-based exercises can increase sense of emotional and physical wellbeing. Spirituality, religious beliefs and involvement with a faith group may be protective against development of mental illness while at the same time provide avenues for increased social connectedness.
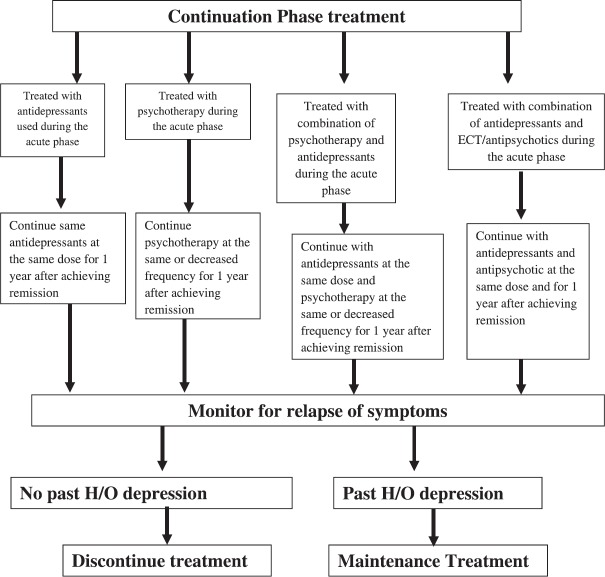
CONTINUATION PHASE
Aim of continuation phase treatment is to prevent relapse of depression and the same treatment as used during the acute phase need to be continued (Figure-5). During the continuation phase, patients who have been treated with antidepressant medications in the acute phase should be maintained on the same agent on the same dose. Although there is scarcity of data about use of psychotherapy in the continuation phase to prevent relapse, some experts support the use of a specific effective psychotherapy during the continuation phase. Use of ECT in the continuation phase has received little formal study. There is no consensus on the duration of continuation phase in elderly, but some experts suggest that treatment should be continued for 1 year after remission. The frequency of visits must be determined by the patient's clinical condition as well as the specific treatments being provided. For stable patients in whom the visits are for the purpose of providing psychiatric management, the frequency could be once every 2 weeks to 2 months. For other patients, such as those in whom active psychotherapy is being conducted, the frequency required may be as high as multiple times a week. If maintenance phase treatment is not indicated for patients who remain stable following the continuation phase, patients may be considered for discontinuation of treatment. If treatment is discontinued, patients should be carefully monitored for relapse, and treatment should be promptly reinstituted if relapse occurs.
Figure 5.
Treatment algorithm for continuation phase treatment of depression in elderly
MAINTENANCE PHASE
As in young adults, the risk of recurrence is high among elderly, with rates of recurrence of 50 to 90 percent over a period of two to three years; hence, the goal of treatment should be not only to treat current episode, but also be prevention of recurrence in future. There is no consensus regarding the duration and when to give and when not to give maintenance treatment in elderly. There is agreement to large extent that patients who have history of three or more relapses or recurrences should be given long-term treatment, but maintenance treatment after 2 episodes is still debated.
In general, the treatment which was effective during the acute and continuation phases should be used in the maintenance phase (Figure-6). The same full antidepressant medication doses should be used. For psychotherapy during maintenance phase, treatments can involve fewer visits (e.g., once a month). Although the effectiveness of combinations of antidepressant medication and psychotherapy in the maintenance phase has not been well studied, such combinations may be an option for some patients. The frequency of clinic visits in maintenance phase can vary from once every several months for stable patients who require only psychiatric management and medication monitoring to as high as once or twice per week in those who are either receiving psychotherapy or severely medically compromised. The optimal length of maintenance treatment is not known and may also vary depending on the frequency and severity of recurrences, tolerability of treatments, and patient preferences. For some patients, maintenance treatment may be required indefinitely.
Figure 6.
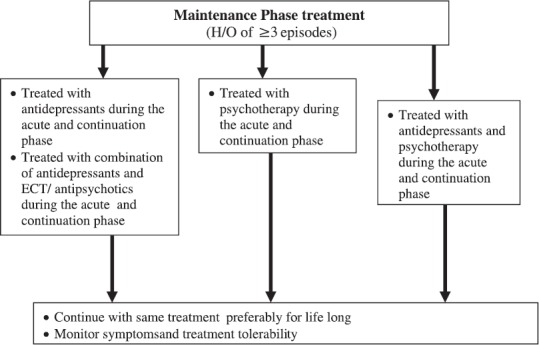
Treatment algorithm for continuation phase treatment of depression in elderly
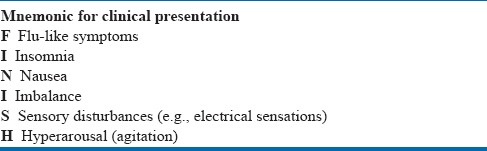
DISCONTINUATION OF ACTIVE TREATMENT
The decision to discontinue maintenance treatment should be based on the probability of future recurrence, the frequency and severity of previous episodes, the persistence of depressive symptoms after recovery, presence or absence of comorbid physical illnesses and psychiatric disorders, and patient preferences. If the decision is made to discontinue or terminate psychotherapy in the maintenance phase, it needs to be individualized as per the patient's needs. In case, it is decided to discontinue pharmacotherapy, it is advisable to taper the medication over the period of at least several weeks to few months. Such tapering allows for the detection of emerging symptoms or recurrences when patients are still partially treated and can help in returning to full therapeutic intensity. In addition, tapering also minimizes the risks of antidepressant medication discontinuation syndrome. Discontinuation syndrome is more frequently reported after discontinuation of medications with shorter half-lives. Accordingly, short-acting agents should be tapered more slowly. Paroxetine, venlafaxine, TCAs, and MAOIs tend to have higher rates of discontinuation symptoms while bupropion-SR, citalopram, fluoxetine, mirtazapine, and sertraline have lower rates. The symptoms of antidepressants discontinuation are given in Table-15. Reassurance may be sufficient for mild discontinuation symptoms. However, for mild to moderate discontinuation, short-term symptomatic treatment (analgesics, antiemetics, or anxiolytics) may be beneficial. If the discontinuation syndrome is severe, antidepressant should be reinstated and tapered off more slowly.
Table 15.
The antidepressant discontinuation syndrome
After the discontinuation of active treatment, patients should be informed about the potential risk of relapse of depression. Early signs of depression should be reviewed, and a plan for seeking treatment in the event of recurrence of symptoms should be established. Patients should continue to be monitored over the next several months to identify those in whom a relapse has occurred. If a patient suffers a relapse upon discontinuation of medication, treatment should be promptly reinitiated. In general, the previous treatment regimen to which the patient responded in the acute and continuation phase should be considered.
MANAGEMENT OF TREATMENT RESISTANT DEPRESSION
The term Treatment resistant depression (TRD) is usually used, when the depression fails to respond to two adequate trials of antidepressant medications. It is estimated that only half of the elderly patients respond to first line treatment and <49% achieve remission. The poor response to treatment is usually attributed to the vascular component in the etiology of late onset depression. Available evidence has also shown association of cognitive impairment, especially executive dysfunction with poor treatment response among elderly. Many other factors also contribute to TRD. However, prior to considering a person to be having TRD, it is important to evaluate the patient properly. Initial reassessment need to focus on re-evaluating the diagnosis of depression. Next step involves evaluation of the fact that patient has received adequate doses of the antidepressant medications for the adequate duration with good compliance. Underlying organic factors need to be evaluated and if these are reversible (e.g., nutritional deficiencies), these must be addressed. Management of TRD involves either change of medication or augmentation of ongoing antidepressant medication. In term of augmentation strategies, although it has not been evaluated thoroughly, lithium is usually recommended as the first choice. When used the target serum levels of lithium for elderly must be in the range of 0.5 to 0.6 mmol/L and it need to be continued for a period of at least 1 year after achieving remission. There is some data to suggest the efficacy of aripiprazole in elderly patients with treatment refractory depression, when used as an augmenting agent with venlafaxine.
TREATMENT IMPLICATIONS OF CONCURRENT GENERAL MEDICAL DISORDERS
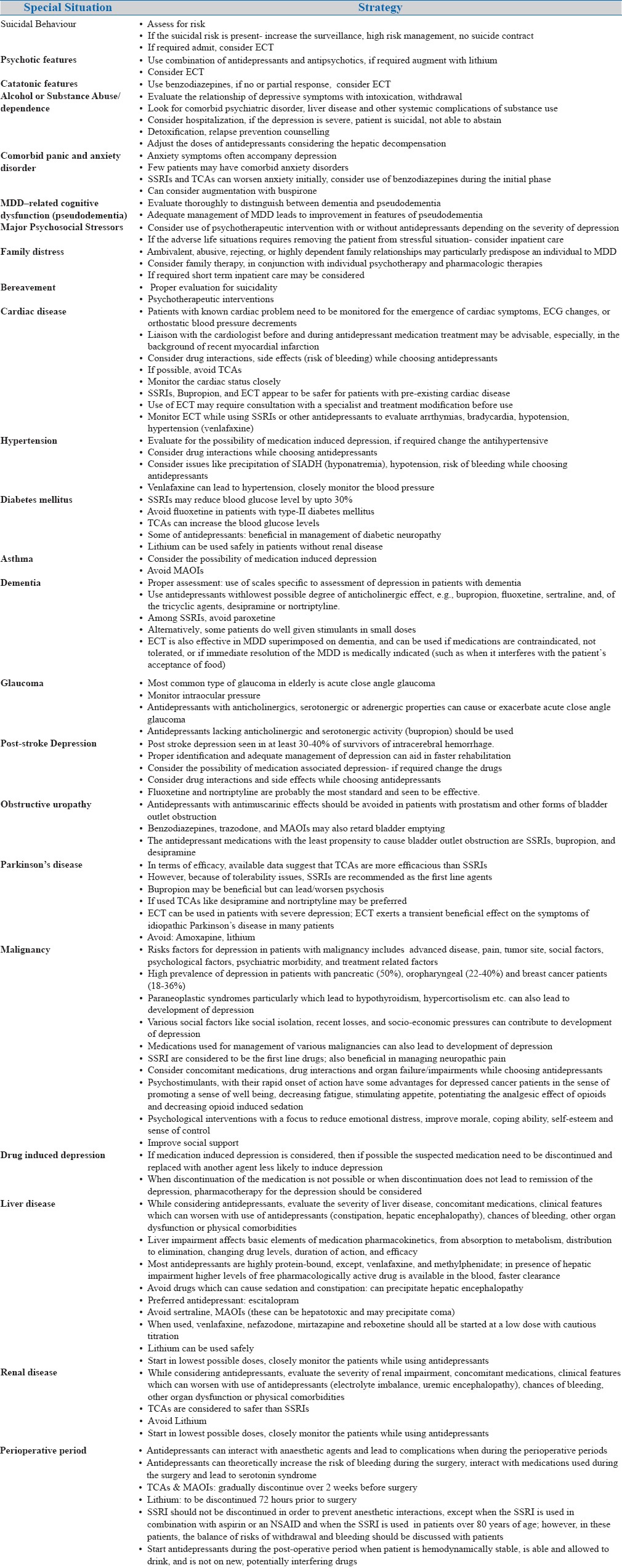
Many elderly patients present with physical illnesses which require special attention. Similarly, certain clinical situations also influence the decision making. Management in some of these difficult situations is summarized in table-16.
Table 16.
Management of Depression in Special Situations
REFERENCES
- 1.Alexopoulos GS, Katz IR, Bruce ML, Heo M, Have TT, Raue P, et al. Remission in depressed geriatric primary care patients: a report from the PROSPECT study. Am J Psychiatry. 2005;162(4):718–24. doi: 10.1176/appi.ajp.162.4.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Avasthi A, Grover S, Bharadwaj R. Shiv Gautam, Ajit Avasthi. Clinical Practice guidelines for treatment of depression in old age. Published by Indian Psychiatric Society. 2007;III:51–150. [Google Scholar]
- 3.Boylan LS, Haskett RF, Mulsant BF, et al. Determinants of seizure threshold in ECT: Benzodiazepine use, anesthetic dosage, and other factors. J ECT. 2000;16:3–18. doi: 10.1097/00124509-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Bruce ML, Seeman TE, Merrill SS, et al. The impact of depressive symptomatology on physical disability: MacArthur Studies of Successful Aging. Am J Public Health. 1994;84:1796–1799. doi: 10.2105/ajph.84.11.1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Calati R, Salvina Signorelli M, Balestri M. Antidepressants in elderly: metaregression of double-blind, randomized clinical trials. J Affect Disord. 2013;147:1–8. doi: 10.1016/j.jad.2012.11.053. [DOI] [PubMed] [Google Scholar]
- 6.Charles III FR, Kupfer DJ, Hoch CC, Stack JA, Houck PR, Sewitch DE. Two-year follow-up of elderly patients with mixed depression and dementia. Clinical and electroencephalographic sleep findings. J Am Geriatr Soc. 1986;34:793–9. doi: 10.1111/j.1532-5415.1986.tb03984.x. [DOI] [PubMed] [Google Scholar]
- 7.Clayton AH, Kennedy SH, Edwards JB, Gallipoli S, Reed CR. The effect of vilazodone on sexual function during the treatment of major depressive disorder. The journal of sexual medicine. 2013 Oct 1;10(10):2465–76. doi: 10.1111/jsm.12004. [DOI] [PubMed] [Google Scholar]
- 8.Cole MG, Bellavance F, Mansour A. Prognosis of depression in elderly community and primary care populations: a systematic review and meta-analysis. American Journal of Psychiatry. 1999 Aug 1;156(8):1182–9. doi: 10.1176/ajp.156.8.1182. [DOI] [PubMed] [Google Scholar]
- 9.Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and metaanalysis. Am J Psychiatry. 2003;160:1147–56. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- 10.Cuijpers P, Geraedts AS, van Oppen P, Andersson G, Markowitz JC, van Straten A. Interpersonal psychotherapy for depression: a meta-analysis. Am J Psychiatry. 2011 Jun 168;(6):581–92. doi: 10.1176/appi.ajp.2010.10101411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flint AJ, Gagnon N. Effective use of electroconvulsive therapy in late-life depression. Can J Psychiatry. 2002;47(8):734–41. doi: 10.1177/070674370204700804. [DOI] [PubMed] [Google Scholar]
- 12.Garekar H, Grover S. Electroconvulsive therapy in the elderly: Anaesthetic considerations and psychotropic interactions. J Geriatr Ment Health. 2017 in Press. [Google Scholar]
- 13.Gautam S, Jain A, Gautam M, Vahia VN, Grover S. Clinical practice guidelines for the management of depression. Indian Journal of Psychiatry. 2017 Jan 59;(Suppl 1):S34. doi: 10.4103/0019-5545.196973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Geiselmann B, Bauer M. Subthreshold depression in the elderly: Qualitative or quantitative distinction? Compr Psychiatry, 2000;41(2 suppl 1):32–38. doi: 10.1016/s0010-440x(00)80006-1. [DOI] [PubMed] [Google Scholar]
- 15.Glover JA, Srinivasan S. Assessment and treatment of late-life depression. JCOM. 2017;24(3):135–144. [Google Scholar]
- 16.Grover S, Malhotra N. Depression in elderly: A review of Indian research. J Geriatr Ment Health. 2015;2:4–15. [Google Scholar]
- 17.Grover S, Somaiya M. ECT in the Elderly: A Review. J Geriatr Ment Health. 2017 in Press. [Google Scholar]
- 18.Judd LL, Hagop SA, Maser JD, et al. A prospective 12 year study of subsyndromal and syndromal depressive symptoms in unipolar major depressive disorders. Arch Gen Psychiatry. 1998;55:694–700. doi: 10.1001/archpsyc.55.8.694. [DOI] [PubMed] [Google Scholar]
- 19.Kok RM, Heeren TJ, Nolen WA. Continuing treatment of depression in the elderly: a systematic review and metaanalysis of double-blinded randomized controlled trials with antidepressants. Am J Geriatr Psychiatry. 2011;19:249–255. doi: 10.1097/jgp.0b013e3181ec8085. [DOI] [PubMed] [Google Scholar]
- 20.Kok RM, Nolen WA, Heeren TJ. Efficacy of treatment in older depressed patients: a systematic review and meta-analysis of double-blind randomized controlled trials with antidepressants. J Affect Disord. 2012;141:103–115. doi: 10.1016/j.jad.2012.02.036. [DOI] [PubMed] [Google Scholar]
- 21.Kok RM, Nolen WA, Heeren TJ. Efficacy of treatment in older depressed patients: a systematic review and meta-analysis of double-blind randomized controlled trials with antidepressants. J Affect Disord. 2012;141:103–115. doi: 10.1016/j.jad.2012.02.036. [DOI] [PubMed] [Google Scholar]
- 22.MacQueen GM, Frey BN, Ismail Z, Jaworska N, Steiner M, Lieshout RJ. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 6. special populations: youth, women, and the elderly. Can J Psychiatry. 2016;61(9):588–603. doi: 10.1177/0706743716659276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mulsant BH, Blumberger DM, Ismail Z, Rabheru K, Rapoport MJ. A systematic approach to pharmacotherapy for geriatric major depression. Clinics in geriatric medicine. 2014 Aug 31;30(3):517–34. doi: 10.1016/j.cger.2014.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Institute for Health and Clinical Excellence (NICE) Depression: management of depression in primary and secondary care (Clinical guideline 23) 2004 [Google Scholar]
- 25.Olin JT, Schneider LS, Katz IR, et al. Provisional diagnostic criteria for depression of Alzheimer disease. Am J Geriatr Psychiatry. 2002;10:125–128. [PubMed] [Google Scholar]
- 26.Pinquart M, Duberstein PR, Lyness JM. Treatments for late-life depressive conditions: a meta-analytic comparison of pharmacotherapy and psychotherapy. Am J Psychiatry. 2006;163:1493–501. doi: 10.1176/ajp.2006.163.9.1493. [DOI] [PubMed] [Google Scholar]
- 27.Rangaswamy SM. World Health Report: Mental Health: New understanding New Hope. Switzerland: The World Health Organization; 2001. [Google Scholar]
- 28.Riva-Posse P, Hermida AP, McDonald WM. The role of electroconvulsive and neuromodulation therapies in the treatment of geriatric depression. Psychiatr Clin North Am. 2013 Dec 31;36(4):607–30. doi: 10.1016/j.psc.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 29.Sahoo S, Grover S. Hyponatremia and psychotropics. J Geriatr Ment Health. 2016;3:108–22. [Google Scholar]
- 30.Tedeschini E, Levkovitz Y, Iovieno N, et al. Efficacy of antidepressants for late-life depression: a meta-analysis and meta-regression of placebo-controlled randomized trials. J Clin Psychiatry. 2011;72:1660–1668. doi: 10.4088/JCP.10r06531. [DOI] [PubMed] [Google Scholar]
- 31.Wen XJ, Wang LM, Liu ZL. Meta-analysis on the efficacy and tolerability of the augmentation of antidepressants with atypical antipsychotics in patients with major depressive disorder. Braz J Med Biol Res. 2014;47:605–16. doi: 10.1590/1414-431X20143672. [DOI] [PMC free article] [PubMed] [Google Scholar]