INTRODUCTION
Sexuality is an important component of emotional and physical intimacy that most men and women desire to experience throughout their lives. Although it is a fundamental driving force, human sexuality is frequently misunderstood. Even among clinicians who acknowledge the relevance of addressing sexual issues in their patients, there is a general lack of understanding of the optimal approach for sexual problem identification and evaluation.
In line with the worldwide trend the number of older adults is notable and is growing in India. The latest data by the Ministry of Statistics and programme implementation in 2016 shows that India has a total of 103.6 million elderly and their population has risen from 5.6% to 8.6% in the last 5 decades, thus this topic which is frequently neglected in the elderly takes on particular importance.
Sexual life continues to be important in later life and the elder often view sexuality as an expression of passion, affection, admiration and loyalty. Sexual activity is a means for elder to affirm physical functioning, to maintain a strong sense of identity and establish self-confidence. Studies show that sexual desire does not change with older age and it is important for both men and women. Even in elderly women after menopause, the sexual ability does not completely disappear but it is affected by sexual dysfunction, either in oneself or in the partner.
Sexual functioning is a complex combination of bio-psycho-social process which is coordinated by neurological, vascular and endocrine systems and any approach to the study of human sexuality that stresses only in one dimension is counter-productive. Recent studies suggest sexual functioning are influenced by factors representing three domains: biologic (the drive), psychological (the will), social context (the wish), and interactions between them.
Sexual function and activity are closely linked with physical health, hence understanding sexual function in the later life course is important from a medical standpoint. Poor sexual function can be due to an underlying serious health condition. For example, it has been found that erectile dysfunction in men may be a marker for asymptomatic coronary artery disease. Diabetes mellitus, which has vascular effects on blood vessels, is one of the most frequent systemic disorders associated with low sexual desire and other sexual problems in aging men whereas diabetic neuropathy can cause impaired sexual desire in women. Understanding the sexual behaviour may uncover protective health effects. Laumann and colleagues discovered an association between sexual well-being and happiness.
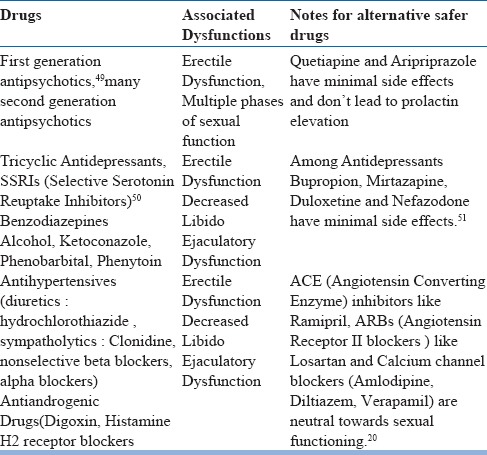
Numerous prescription drugs have adverse effects on sexual functioning including antidepressants especially SSRI's (causing anorgasmia, erectile dysfunction, decreased libido) and antihypertensives (Diuretics, calcium channel blockers). Moreover adverse drug effects are reported much more frequently in the aging population than in the general population. The use of prescribed medications and the rate of adverse effects of drug therapy are consistently higher in female than male elderly populations and they influence sexual responses including desire by non-specific effects on general well-being, energy levels and mood.
Psychological factors (the will) are major determinants of intensity of sexual desire. Psychological factors are independently related to sexual functioning. In addition emotional and interpersonal motivation mediates the effect of sexual drive which is characterized by willingness of person to behave sexually with a given partner and can compensate for diminished physiologic desire of sexual activity (eg as result of declining testosterone levels). Psychological condition such as depression is a risk factor for sexual dysfunction along with the medications associated with treating it.
Social context (the wish) also plays a crucial role in sexual function- a role that has been neglected in medical literature. For e.g availability of a partner, intimate communication, relationship duration, characteristics of an individual's sexual partner and cultural experiences. Furthermore, Laumann et al. discovered in their analyses of the Global Study of Sexual Attitudes and Behaviours that association among subjective sexual wellbeing and physical health, mental health, sexual practices, and relationship context were consistent in a broad variety of countries from each major world region. In addition, the authors found that men reported higher levels of subjective sexual well-being regardless of sociocultural context. They also established an overall correlation between subjective sexual well-being and happiness in men and women.
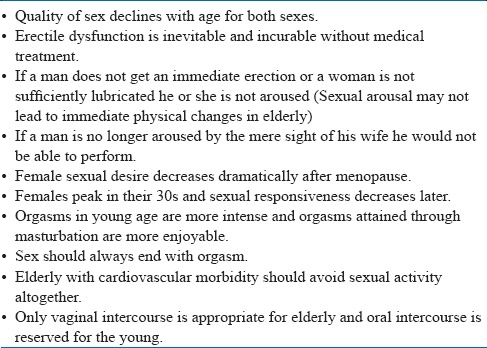
Despite the importance of sexual function sexual problems are highly prevalent yet frequently under-recognized and under diagnosed in clinical practice. Adequate attention to these aspects during the history taking will educate the patients regarding the complex nature of sexuality, and prepare them in understanding treatment and outcome realities. The rational selection of therapy by patients is only possible following appropriate education, including information about sexuality and all treatment options for sexual dysfunction. Although not always possible on the first visit, every effort should be made to involve the patient's sexual partner early in the therapeutic process. There are many myths (Table 1) prevailing in the society and the treating physician and collaborating specialist should possess broad knowledge about human sexuality.
Table 1.
Myths associated with Elderly Sexuality11
Psychosocial factors affecting sexuality in Elderly
Marriage;
For woman availability of a sexually willing, capable and socially sanctioned sexual partner appears to be the most important factor, but problems arise as women usually outlive men. Marital status appears to be less important in men regarding sexual activity. As society is moving from double standards for men and woman these differences are narrowing. More and more older people cohabit to avoid social insecurity; therefore one should not assume older unmarried people are sexually inactive. Extramarital issues should also be kept in mind.
Families;
Many traditional and joint families, particularly in rural areas fail to provide privacy to the elderly, young newly married occupying the private space. Families who do not accept the sexual needs of divorced or widowed elderly contribute to the negative feelings of the elderly about themselves. Medical and nursing staffs tendency to be judgmental about sexual needs of the elderly patients, gives the impression that this is abnormal. Total care of elderly should encompass addressing sexual feeling and the need for privacy.
Remarriage;
Remarriage in late life may be even more satisfying than first marriage. Remarriage is often threatening for grown up children who throw storm of protest. Remarriage should be encouraged as loneliness may lead to despair.
Sexuality, Education & Awareness; Education usually removes sexual inhibition and unnecessary anxiety, and enhances communication. Only education can give the right attitude regarding sexuality in elderly who are widowed, divorced or cohabiting.
Disparity in desire
Disparity in desire among couples may increase over years; difficulties arise when one is content with holding hands and the other partner has strong sexual urges.
Sexual interest
Individuals who enjoyed sex in younger years continue sexual interest when they grow older and remain sexually active in later years. Couples tend to become less inhibited and feel free to explore varying type of sexual stimulation as age advances.
Regular sexual expression
Regular sexual expression is important, especially for women. Lack of regular sexual expression and privacy correlates with a decrease interest in coitus.
Family climacteric; Faulty attitude to “change in life” may affect the couples response if they consider that it implies a change of status and the level of attractiveness, and the sexual activity is inappropriate.
Women may suffer from empty nest syndrome or boredom, and have little status of their own. They may have difficulty in re-entering the profession of their own, or picking up the threads of their own lives once their children have left home. Women may link sexual capacity to maternal capacity, and loss of reproductive capacity may be difficult for some to accept, depending on what fertility has meant, and whether they have had as many, too many or too few children compared to what they wanted. Problems faced during pregnancy, infertility and contraception also have an impact.
A small number of men over 60 years also experience a syndrome called male climacteric. This is characterized by four or more of the following symptoms; listlessness, weight loss, poor appetite, depressed libido, loss of erectile potency, impaired ability to concentrate, weakness, easy fatigability and irritability. The differentiating and deciding factor is level of testosterone.
HORMONES
Decrease in testosterone concentrations (normal 270-1100 ng/dl) are noted from the age of 50 years, at the rate of 100 ng/dl per decade and the sensitivity of androgen receptors decreases in men with age; however healthy aging men never become hypogonadal. Testosterone levels in saliva of heterosexual adolescent men correlate positively with the number of times they initiated sexual contact (although whether sexual contact led to the increase in androgens needs to be confirmed). In both men and women, orgasm (induced by masturbation) increases sympathetic activation leading to an increase in heart rate, blood pressure and plasma noradrenaline levels (transiently) an increase in plasma prolactin level for 30 min in men and 60 min in women. In women, sexual arousal increases plasma luteinizing hormone and testosterone levels. The neurohormone oxytocin is also released during orgasm and reinforces pleasure.
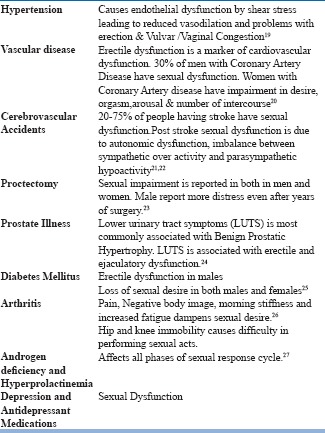
ILL HEALTH
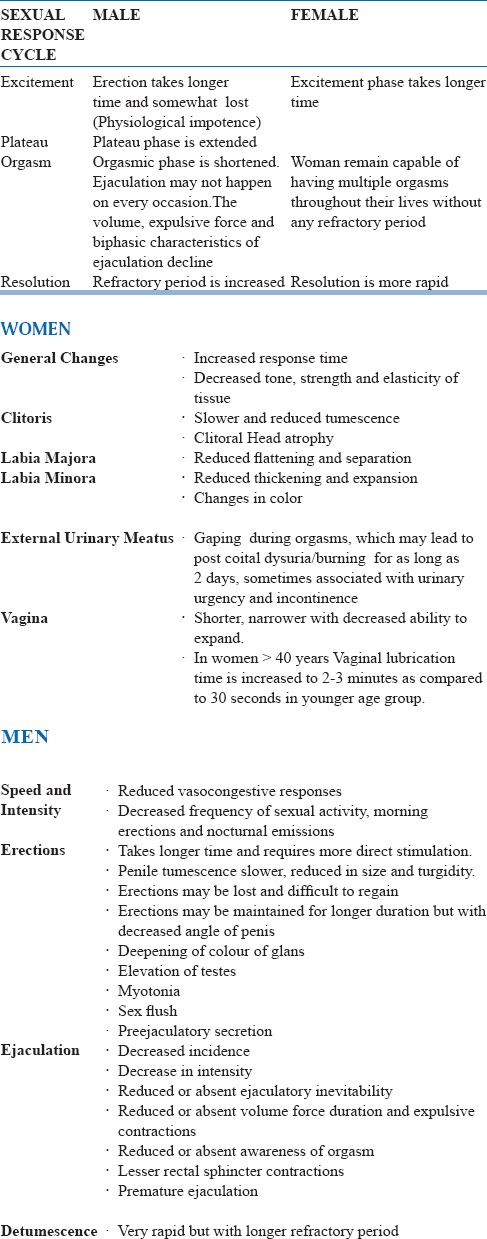
EFFECTS OF AGEING ON SEXUAL RESPONSE CYCLE
The capacity to respond to sexual stimulation is effectively retained, although the intensity of physical reaction is slowly reduced in all phases of sexual response cycle. Table 2 mentions the changes in sexual response seen with aging.
Table 2.
Changes in sexual response with aging
Sexual Problems: Classification and Epidemiology
The ‘Sexual Response Cycle’ was described first by Masters and Johnson in 1966 as the EPOR Model (Excitement, Plateau, Orgasmic and Resolution phases) and later modified by Kaplan in 1974 into the DEOR model (Desire, Excitement, Orgasmic and Resolution phases), which became the accepted model universally. Classically, sexual inadequacy refers to some specific disruption of the ‘Sexual Response Cycle’ (as described by Masters and Johnson in 1970). The clinicians initially faced the difficulty of ascertaining the threshold for sexual disorders. This difficulty was overcome by adopting a patient centered approach. Accordingly, a sexual problem is said to be present when an individual comes with difficulty in particular area of sexual functioning which may or may not be associated with behavioral, mood or cognitive symptoms. As per the DEOR model “Sexual dysfunction is referred to aproblem during any phase of the sexual response cycle that prevents the individual or couple from experiencing satisfaction from the sexual activity”. Gender identity disorders and paraphilias should be differentiated from sexual inadequacies. ‘Sex’ is most commonly referred to as what an individual is biologically, whereas ‘gender’ is what one becomes in the social context.
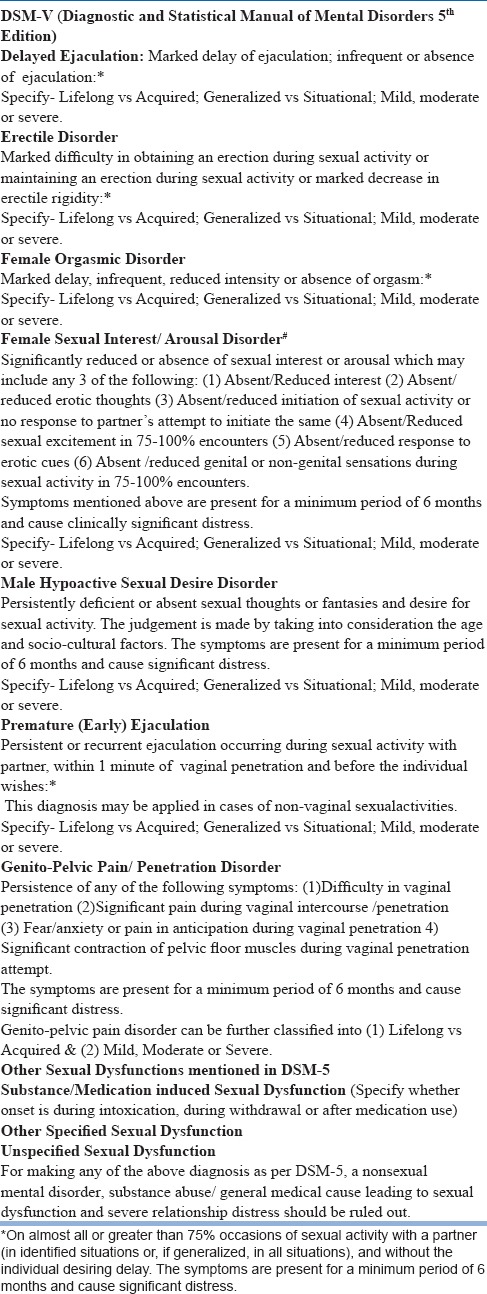
DSM-5 (Diagnostic and Statistical Manual of Mental Disorders 5th Edition) released in May 2013 defines Sexual Dysfunctions as “a heterogeneous group of disorders that are typically characterized by a clinically significant ‘disturbance in a person's ability to respond sexually or to sexual pleasure” Subtypes can be classified as Lifelong vs acquired and generalized vs situational. Other factors which may influence the symptom presentation include i) Partner's and individual vulnerability factors ii) Relationship issues iii) Psychiatric comorbidity iv) Cultural and v) General medical factors.
Common Sexual Problems and Dysfunctions
Classification in psychiatry has been a topic of debate and complex area of research. Some are of the opinion that classificatory system creates artificial boundaries between different category of problems; one the best examples for the same is merging of female sexual desire disorders and arousal disorders in DSM-5. Due to its eclectic approach the International classification of mental disorders (ICD-10) has been clinically acceptable in India. The DSM classificatory system by the American Psychiatric Society has been acceptable in academic institutions due to its pointwise approach. DSM 5 highlights the fact that clinical judgement needs to be applied to ascertain whether the sexual dysfunction is due to inadequate stimulation. DSM-5 subtypes include, lifelong which denotes that the problem has been present from the very beginning; acquired denotes that the problem started after a period of normal sexual functioning. Generalized (vs Situational) denotes that the sexual problem is present with all types of stimulation, all situations and partners. Other factors which need to be considered include: 1)Partner factors (sexual problems in the partner),2) Relationship factors, 3) Individual vulnerability factors (poor body image), 4) Cultural or religious factors, 5) Medical factors. As per DSM 5, if the sexual problem is due to a non -sexual mental disorder (anxiety, depression), substance use, other medical condition or severe relationship distress then a sexual dysfunction diagnosis is not made.Table 3 gives a comparison of sexual dysfunctions mentioned in DSM 5 and ICD 10 Classification of Mental and Behavioral Disorders (International Classification of diseases10th Revision) Table 4 gives a brief description of sexual dysfunctions mentioned in DSM 5.
Table 3.
Comparison of diagnostic categories of ICD.10 & DSM-5 of sexual disorders9
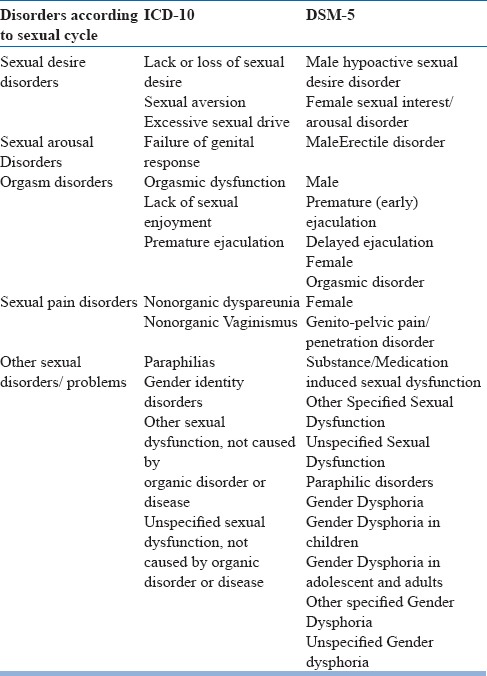
Table 4.
Brief description of sexual dysfunctions mentioned in DSM 5
Sexual Dysfunctions: Epidemiology
The frequency of reporting and seeking help for sexual problems varies due to a number of factors like availability of sexual health care facility, awareness about the problem and the social and cultural factors. Geriatric sexuality literature constitutes only 0.5 % of the total publications, and still very few from the developing world. Logistical issues, sexuality specific venues competing for publication and geriatric journals avoiding sexuality related topics in elderly, contributes to low research volume on geriatric sexuality. Studies involving both the genders in the age group more than 50 years, reports prevalence of sexual dysfunction to be around 50-80%.
Studies involving females in the age group of 50-70 years, reports prevelance of sexual dysfunction to be around 50-75%.
Sexual Dysfunctions: Etiology
Human sexual response is a complex biological phenomenon and is strongly influenced by interpersonal and socio-cultural factors. Generally speaking, sexual dysfunctions are multi-factorial in etiology. As mentioned, DSM-5 highlights the point that a sexual dysfunction diagnosis is not made if the problem is better explained by a nonsexual mental disorder, stressor, substance use or a general medical condition. Table 5 highlights the etiology of sexual disorders, whereas Table 6 and 7 mention the drugs most commonly associated with sexual dysfunction in the elderly male and female.
Table 5.
Etiology of sexual disorders
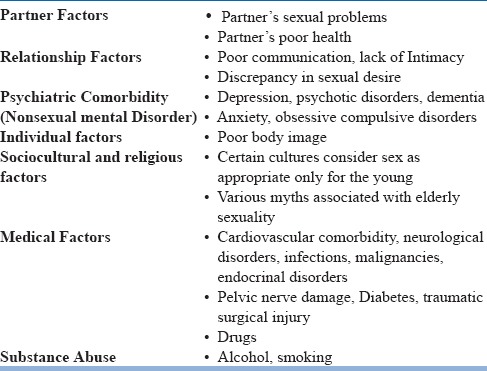
Table 6.
Common Drugs associated with male sexual dysfunction and alternative safer drugs available
MANAGEMENT OF SEXUAL INADEQUACIES
Diagnostic workup
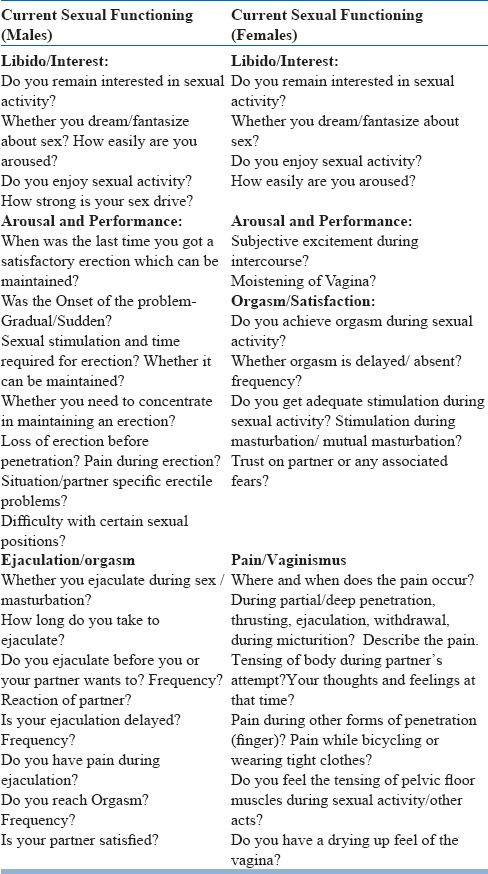
As in all psychiatric interviews one needs to develop rapport in an accepting atmosphere with a non-judgmental attitude. Sexual history needs to be more structured, though areas of concern for the patient should be explored positively. Both recent and early sexual histories need to be noted. The current sexual complaints, life stresses, sexual practices, contraceptive use, partners, relationship problems, sexual fantasies, masturbatory history, extramarital affairs and commitment to partner should be enquired into. If married courtship period, honeymoon and reproductive history should be looked into. Mutual physical attraction, temporary separation and the effect of children on couple's sexual life should be noted. Changes in sexual functioning and frequency and quality of sexual interactions with age should be detailed. The partner's contribution to the present distress, life style factors, psychiatric history including history of substance abuse should be ascertained. The patient's self-image as a sexual being through childhood and adolescence and people who contributed to patient's sexual education and identity needs to be detailed. Any history of group sex, homosexual encounters and abortions should be considered and enquired. Sexual orientation of the patient, any high risk sexual behaviour and sexual abuse history should be kept in mind. Regardless of sexual orientation, each phase of the sexual response cycle applies equally to both heterosexual and homosexual partners and methods and principles of treatment are similar.Table 8 highlights the points to be considered for taking a sexual history; whereas table 9 describes the assessment of current sexual functioning in males and females.
Table 8.
Taking a Sexual History53
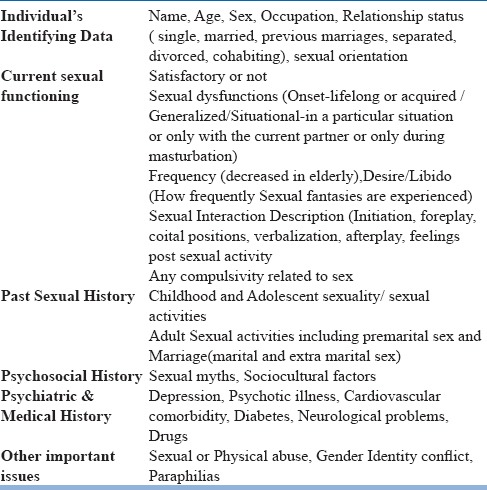
Table 9.
Assessment of current sexual functioning in males and females
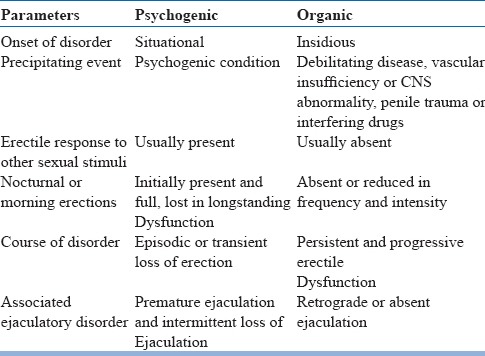
Careful history taking should be followed by a physical examination in all the cases after obtaining consent and maintaining privacy. Rule out organic disease and make a note of any contributing general medical illness. Laboratory studies include urine analysis, complete blood count, kidney and liver function tests, lipid profile, fasting blood sugar, ECG, thyroid function. Other endocrinal tests and Lab tests related to general medical illness if any or only when needed. Nocturnal penile tumescence, Intracavernosalinjection using avasodilating agent like papaverine, duplex color ultrasonography, dynamic infusioncavernosometry and cavernosography, pelvic penile angiography are the other tests in some selected cases and depends on what procedure is being planned. It is necessary to understand relationship difficulties among the couple, whether partner is sympathetic or not sympathetic towards the problem, their expectation and motivation for treatment. Differentiating features between organic and psychogenic sexual dysfunction need to be established well before the active management as mentioned in table 10.
Table 10.
Differentiating features between organic and psychogenic sexual dysfunction9
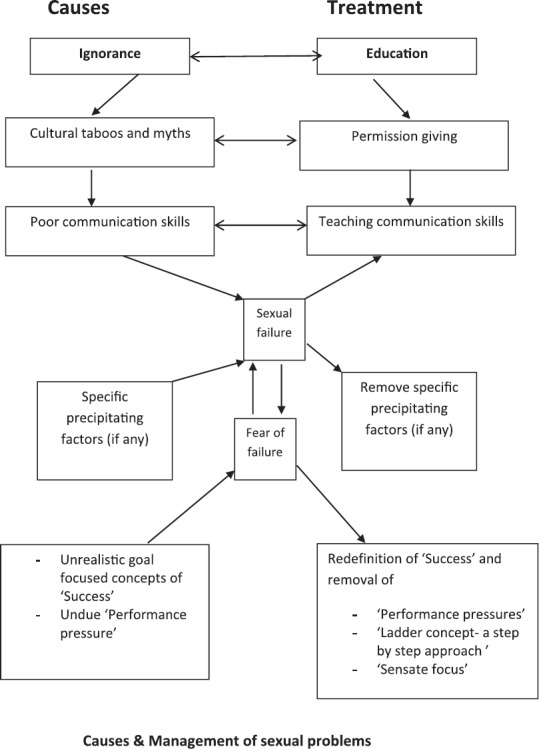
PSYCHOTHERAPEUTIC INTERVENTION
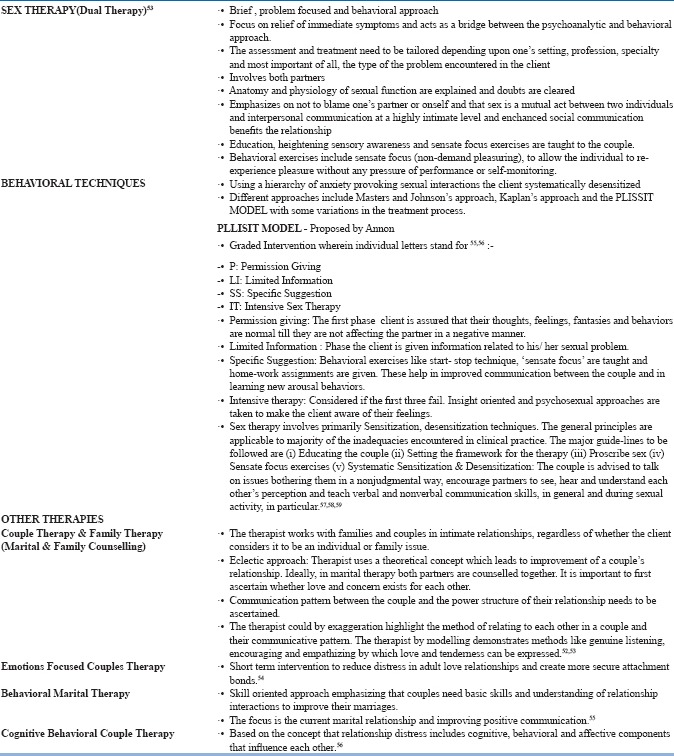
Sex therapy as it is referred to today is essentially a modified form of the original therapy (as founded by Masters and Johnson in 1970) and follows a brief, problem focused, and behavioral approach. Based on classic psychodynamic theories, resolution of early developmental conflicts, acceptance of sexual impulses to the ego and resolution of the problem was the main focus. The ‘new’ sex therapy focuses on relief of immediate symptoms and acts as a bridge between the psychoanalytic and behavioral approaches. Psychodynamic approaches are only used if the initial behavioral techniques do not produce symptom relief.
As elaborated by Masters and Johnson in 1970, sex therapy (dual sex therapy) ideally includes involvement of both the partners. Anatomy and physiology of sexual function are explained in brief and doubts are cleared. Therapy emphasizes that there is no use blaming one's partner or oneself, and sex is a mutual act between two individuals. Interpersonal communication at a highly intimate level and enhanced social communication benefits the relationship. Education, heightening sensory awareness and sensate focus exercises are taught to the couple. Behavioral exercises include sensate focus (non-demand pleasuring), to allow the individual to re-experience pleasure without any pressure of performance or self-monitoring. The assessment and treatment need to be tailored depending upon one's setting, profession, specialty and most important of all, the type of the problem encountered in the client, wherein different approaches may be helpful.
PHARMACOTHERAPY FOR SEXUAL DYSFUNCTION
Nitric oxide enhancers:
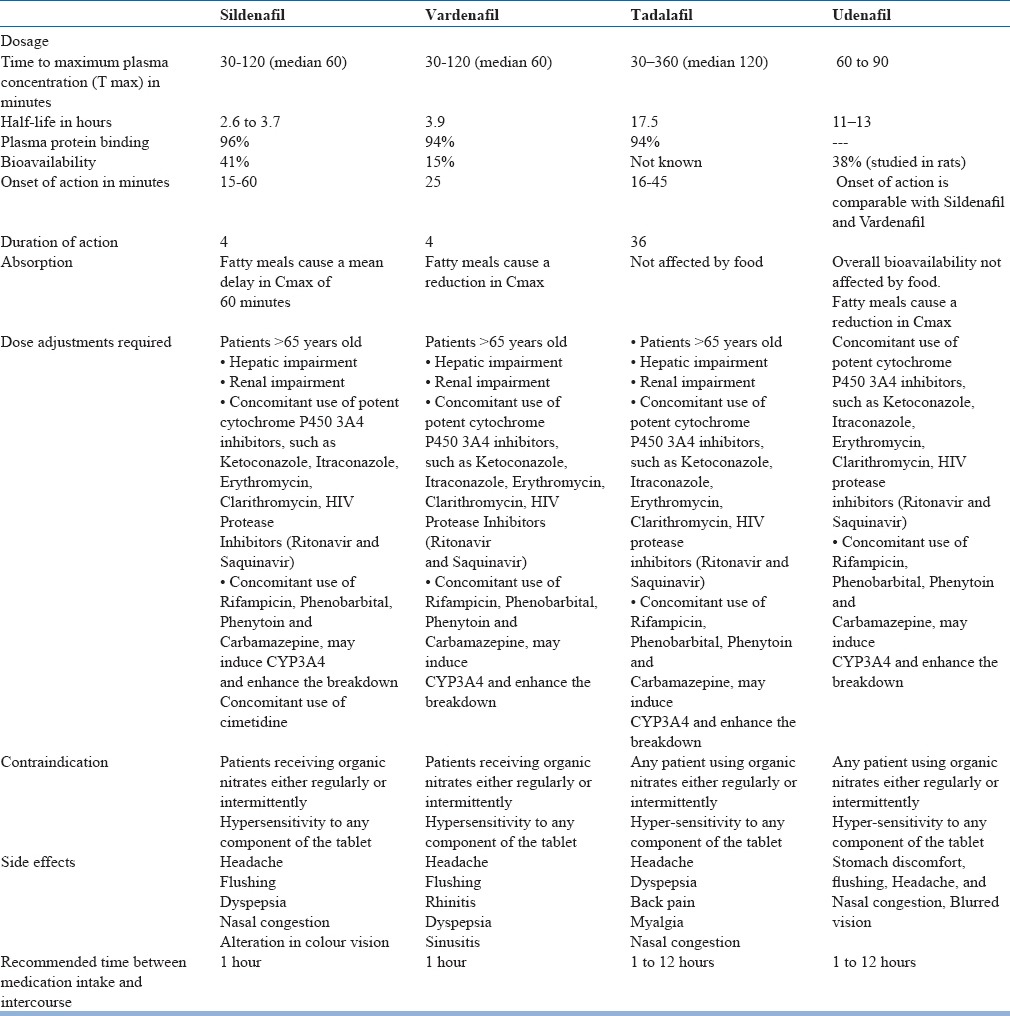
These drugs improve inflow of blood into the penis and improve erection. First drug developed in this class was sildenafil citrate. It acts on the nitric oxide mechanism by blocking PDE - 5 (Phosphodiesterase-5) enzyme. It is the first approved non-surgical treatment for erectile dysfunction and was approved by US Food and Drug Administration (US-FDA) in 1998 for prescription sale. It is rapidly absorbed after oral administration and has to be taken one hour before sexual activity which is the time required for peak plasma concentrations to be reached and the effect may last for upto 4 hours. The starting dose should be used on atleast four occasions to precisely access the efficacy and tolerability. If a satisfactory sexual performance is not achieved, the dose should be increased to the next higher level. Studies have clearly demonstrated that there is a dose-response curve with sildenafil and the best results are obtained upto a maximum dose of 100mg. However sildenafil has been used as a salvage therapy for severe erectile dysfunction at a maximum dose of 200 mg, but the incidence of side effects and discontinuation rates increase considerably. Very recent studies have reported that sildenafil does not worsen the cardiac profile of patients with Ischaemic heart disease, undergoing stress exercises. Sildenafil increases the time to developing symptoms of angina in symptomatic patients with Ischaemic heart diseaseundergoing a treadmill test. Sildenafil does not cause coronary steal or reflex tachycardia. For patients who experience an acute myocardial ischemia and who have taken sildenafil in the last 24 hours, administration of nitrates should be avoided. The American College of Cardiology and the American Heart Association have published recommendations for the use of sildenafil in patients with cardiac risk. Sildenafil should be used with caution in individuals maintained on multiple antihypertensive drugs. Adverse effects with sildenafil are dose dependent. Common adverse effects are headache (most common), flushing, rhinitis and visual disturbance changes in the perception of colour, hue or brightness. The adverse effects are usually mild and transient, lasting a few minutes to a few hours after drug administration. It is contraindicated in patients on concurrent organic nitrates. This is because it potentiates the hypotensive action of such drugs through its effects on nitric oxide/c-GMP mechanisms. It should be used with caution in persons with anatomical deformities of the penis (e.g. Angulation, Cavernosal fibrosis, Peyronie's disease), and in patients at risk for Priapism (e.gpatients with Sickle Cell anemia, Multiple Myeloma, Leukemia, Bleeding Disorders, Retinitis Pigmentosa). Rare side effect reported is Nonarteritic Ischemic Optic Neuropathy (NAION). Recent studies have reported that metformin and pioglitazone used in diabetes enhance the effect of Sildenafil in treating ED. Various PDE-5 inhibitors have been compared in table 11. A long acting PDE5 inhibitor should be considered for elderly men who frequently have sexual intercourse in the morning after waking up and patients who anticipate frequent sexual intercourse. Udenafil has clinical properties of both relatively rapid onset and long duration of action though it is not available in India.
Table 11.
COMPARISON OF PDE-5 INHIBITORS9
PSYCHOTHERAPEUTIC INTERVENTION KEY POINTS
Oral Phentolamine and Apomorphine are helpful as potency enhancers in minimal erectile dysfunction. Apomorphine effects are mediated through the autonomic nervous system causing arterial vasodilation and has dopamine receptor stimulating effect. Phentolamine decreases sympathetic stimulation and relaxes corporeal smooth muscle. Smooth Muscle relaxants like Papaverine, Phentolamine, Phenoxybenzamine are used in ICIVAD (Intracavernosal injection of vasoactive drugs) techniques for ED; Prostaglandin E (Alprostadil) through injection or through intraurethral insertion is an effective agent for ED; to improve erectile function in animal studies and is likely to be studied on humans 52 in near future. A topical cream containing 3 vasoactive agents: Aminophylline, Isosorbidedinitrate and Co-dergocrinemesylate with or without Alprostadil is helpful in ED. An Alprostadil cream and vaginally applied Phentolamine are helpful for female sexual arousal disorder. Yohimbine is a central Alpha 2 adrenoreceptor blocker and increases sympathetic drive. Its effectiveness is doubtful in ED. Horny Goat weed (Epimedium) has been used as a traditional remedy for ED in China. Trazodone, an antidepressant acts by inhibiting serotonin uptake and also by influencing alpha adrenergic and dopaminergic function. Results are inconsistent in erectile disorders.
Pharmacotherapy of premature ejaculation includes judicious use of tricyclic antidepressants, SSRIs and certain topical therapies.
Hormonal therapies:
Testosterone is definitively effective only in case of hypogonadism. It can increase the desire but has no effect on erectile functioning. Female low sex drive and anorgasmia can be tried under careful monitoring. Hormone Replacement Therapy (HRT) with estrogen in case of menopausal women as vaginal function, particularly lubrication is determined by them. Hyperprolactinaemia is treated by administration of dopaminergic drugs like bromocriptine.
Other drugs:
Naltrexone, an opiate antagonist, can antagonize the inhibition of sexual functions. Aswagandha, Shathavari, Korean red ginseng are helpful in enhancing sexual functioning in both males and females. Aswagandha (Indian ginseng) enhances sexual desire in men. Shathavari(Asparagus racemosus), a creeper which grows in low jungle areas throughout India is considered to be the women's equivalent to Ashwagandha and enhances female sexual functioning. Some of the traditional herbal medicines used in medieval Persia, have been shown to be helpful in ED by relatively recent research. These include ginger (Zingiberofficinale), almond (Amygdaluscommunis), spice commonly known as ‘grains of paradise; Melegueta pepper’ (Aframomummelegueta), and certain brassica species and seed of garden cress (Lepidium sp). Saffron (30 mg/day) has been shown to improve sexual function (arousal, lubrication and pain domain) in females with SSRI induced sexual dysfunction. Snacking on pistachio nuts, 100 gm/day for 3 weeks, has been shown to improve erectile dysfunction.
Flibanserin (Trade name-Addyi; now available in India by the name Fliban by Hindustan Unilever) is a medication approved by US-FDA for the treatment of pre-menopausal women with hypoactive sexual desire disorder (HSDD).
In some selected cases when psychotherapy, behaviour techniques and drugs fail or seen to be not very effective, vacuum devises, injections and implants, vibrators are found to be relatively effective. Ultimately, the success of sex therapy depends on a host of factors. Therapy duration ranges from 6 weeks to more than a year in occasional cases. Sexual dysfunctions respond to treatment better compared to gender identify disorders and paraphilias, which are very resistant to therapy. More than half of the cases of erectile dysfunction and almost all the cases of premature ejaculation respond to combination of therapies.
Gender Identity disorder / Gender Dysphoria
Although much has been written on diagnosis of gender dysphoria, emphasis has always been on younger individuals. While several researchers have alluded to the problems of the aging gender dysphoric patient the relationship between diagnosis and treatment has been neglected. As more older gender dysphoric patients request sex-reassignment surgery, there will be increasing demands for differential diagnoses and treatment strategies. Correct diagnosis is especially crucial since life stresses may lead some transvestites to clinically present as transsexuals desiring sex-reassignment surgery.
Sexual Variations, Paraphilia and Paraphilic Disorders
Sexual variations are very common in almost all age groups and elderly are no exception. The term ‘deviation’ refers to the existence of a norm and the deviation takes place. In sexuality no such norm exists, as standard varies from time to time, place to place and epoch to epoch and culture to culture. Homosexuality has gradually come to be considered as a variation of sexual activity rather than deviation. However, one may encounter issues related to them in the Indian context in the elderly and there is need to attend to them with utmost sensitivity.
The term paraphilia denotes a persistent sexual interest other than sexual interest in genital stimulation with phenotypically normal, mature and consenting human partners. These may include the person's erotic activities or targets. Previously considered perversions implying sexually arousing fantasies, activities and gratification other than by willing genital intercourse between partners and a departure from the cultural norm. Normal sexual relationship implies activities which are acceptable and pleasurable to both the partners without the degradation, exploitation or distress to either of them. Contrary to the long held belief many paraphilic behaviours are predominantly male, does not involve offences and practices remain intensely private. DSM 5 recognizes and differentiates innocuous paraphilic behaviours from paraphilic disorders. A paraphilic disorder is a paraphilia causing distress to the individual with or without risk of harm to self or others. Example persistent interest in whipping or strangulating another person. A paraphilia is a necessary but not the only condition for diagnosing a paraphilic disorder. Among elderly they may represent some other primary cause and ruling out dementia, mood disorders and personality disorders is a must. Sexually inappropriate conduct often accompanies the disinhibition associated with dementia and neuropsychologic deficits. A detailed evaluation is mandatory. The treatment involves medications, behaviour modification therapies, family and psychotherapy and where necessary sex therapy like reinforcement of socially acceptable sexual function and management of erectile and ejaculatory impairment.
CONCLUSION
Conclusions:
A. Quality of Life
Aging typically entails some degree of change in men's and women's capacities for sexual performance from strictly physiological standpoint, yet research data suggests that an equalnumber of people in late life find sex satisfying, if not more so, than in their youth.
It is important to recognize that older people are at risk of severalhealth-related, psychosocial, environmental circumstances that can hinder sexual expression and functioning. Although some of these barriers cannot be prevented entirely, education, advocacy andeffective coping strategies can soften their impact considerably.
An understanding of the sexual changes that accompany normalaging may help physicians give patients realistic and encouragingadvice on sexuality.
It is important that older men and women do not fall into the psychosocial trap of expecting (or worse, trying to force) the kind and degree of sexual response characteristic of their youth, it is equally as important that they not fall prey to the negative folklore according to which decreased physical intimacy is an inevitable consequence of the passage of time.
Early adoption of healthy lifestyles may be the best approach to reducing the burden of erectile and other sexual dysfunctions on the health and well being of elderly.
B. Sexual Rights
Sexual rights embrace human rights that are already recognized in international human rights documents and other consensus statements and they include the rights of all persons, free of coercion, discrimination and violence, to the highest attainable standard of sexual health, including access to sexual and reproductive health care services.
C. Guiding Principles for Affirmative Action propounded by WHO implies Affirmative approach to sexuality, Autonomy and self-determination and responsiveness to changing needs, Comprehensive understanding of sexuality, Confidentiality and privacy, Advocacy and Equity, Non-judgementaland Accessible services and programmes to the elderly.
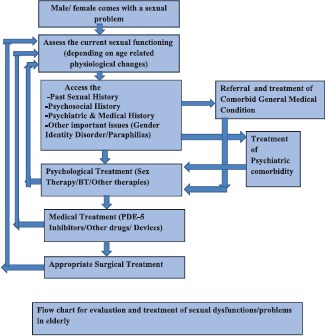
The following flowchart gives the treatment of sexual disorders in elderly.
REFERENCES
- 1.Hatzichristou D, Rosen RC, Broderick G, Clayton A, Cuzin B, Derogatis L, Litwin M, Meuleman E, O’Leary M, Quirk F, Sadovsky R, Seftel A. Clinical evaluation and management strategy for sexual dysfunction in men and women. Journal of Sexual Medicine, 2004;1:49–57. doi: 10.1111/j.1743-6109.2004.10108.x. [DOI] [PubMed] [Google Scholar]
- 2.Kalra G, Subramanyam A, Pinto C. Sexuality: Desire, activity and intimacy in the elderly. Indian Journal of Psychiatry. 2011;53(4):300–306. doi: 10.4103/0019-5545.91902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Umidi S, et al. “Affectivity and sexuality in the elderly; Often neglected aspects”. Archives of Gerontology & Geriatrics. 2007;44:413–417. doi: 10.1016/j.archger.2007.01.058. [DOI] [PubMed] [Google Scholar]
- 4.Choi KB, Jang SH, Lee MY, Kim KH. Sexual life and self-esteem in married elderly. Arch GerontolGeriatr. 2011 Jul-Aug;53(1):e17–20. doi: 10.1016/j.archger.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 5.Wolfe L. D. Sexuality across the life course. In: Rossi A.S, editor. Am. J. Hum. Biol. Vol. 7. Chicago: The University of Chicago Press 1994 $3495 (cloth); 1995. pp. 278–279. xvii + 418. [Google Scholar]
- 6.John D. DeLamater& Morgan Sill (2005) Sexual desire in later life. The Journal of Sex Research. 42(2):138–149. doi: 10.1080/00224490509552267. [DOI] [PubMed] [Google Scholar]
- 7.Schiavi R, Stimmel B, Mandeli J, Rayfield E. Diabetes mellitus and male sexual function: A control study. Diabetologia. 1993;36:745–751. doi: 10.1007/BF00401146. [DOI] [PubMed] [Google Scholar]
- 8.Laumann EO, Das A, Waite LJ. Sexual dysfunction among older adults: prevalence and risk factors from a nationally representative U.S. probability sample of men and women 57–58 years of age. J Sex Med. 2008;5(10):2300–11. doi: 10.1111/j.1743-6109.2008.00974.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schiavi R. Cambridge: Cambridge University Press; 1999. Impact of medical illnesses on sexuality. In Aging and Male Sexuality; pp. 124–146. [Google Scholar]
- 10.Avasthi A, Grover S, SathyanarayanaRao TS. Clinical Practice Guidelines forManagement of Sexual Dysfunction. Indian Journal of Psychiatry. 2017 Jan;59(Suppl1):S91–S115. doi: 10.4103/0019-5545.196977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Block J D. Create a Sexy Frame of Mind. Sex over 50. A Perigee Book, published by the Penguin Group, USA. 2008:1–16. Ch 1. [Google Scholar]
- 12.Kinsey, Pomeroy, Martin . Sexual behavior in human female. Philladelphia: Saunders; 1953. [Google Scholar]
- 13.Kinsey, Pomeroy, Martin . Sexual behavior in human male. Philladelphia: Saunders; 1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.A health practitioners Text. 2nd Ed. Ballitmore: Williama and Wilkins; 1980. Pfeiffer.e.Sexuality and the ageing patient.R.Green.Human sexuality; pp. 125–133. [Google Scholar]
- 15.Kolodny R C, Masters W.H, Johnson V.E. Boston: Little, Brown; 1979. Textbook of sexual medicine. [Google Scholar]
- 16.Amore M, Di Donato P, Berti A, Palareti A, Chirico C, Papalini A, Zucchini S. Sexual and psychological symptoms in the climacteric years. Maturitas. 2007 Mar 20;56(3):303–11. doi: 10.1016/j.maturitas.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 17.Kruger T, Exton MS, Pawlak C, von zurMuhlen A, Hartmann U, Schedlowski M. Neuroendocrine and cardiovascular response to sexual arousal and orgasm in men. Psychoneuroendocrinology. 1998;23:401–411. doi: 10.1016/s0306-4530(98)00007-9. [DOI] [PubMed] [Google Scholar]
- 18.Exton MS, Bindert A, Kruger T, Scheller F, Hartmann U, Schedlowski M. Cardiovascular andendocrine alterations after masturbation-induced orgasm in women. Psychosom Med. 1999;61:280–289. doi: 10.1097/00006842-199905000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Holly N T, Evans G W, Berlowtiz D R, Chertow G M, Conroy M B, Foy C G, Glasser S P, Lewis C E, et al. SPRINT Study Group; Antihypertensive medications and sexual function in women: Baseline data from the Systolic Blood Pressure Intervention Trial (SPRINT) J Hypertens. 2016 Jun;34(6):1224–31. doi: 10.1097/HJH.0000000000000911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Assari S. Intercourse avoidance among women with coronary artery disease. J Sex Med. 2014 Jul;11(7):1709–16. doi: 10.1111/jsm.12459. [DOI] [PubMed] [Google Scholar]
- 21.Salavati A1, Mehrsai A1, Allameh F1, Alizadeh F1, Namdari F1, Hosseinian M1, Salimi E1, Heidari F1, Pourmand G. Is Serum Uric Acid Level Correlated with Erectile Dysfunction in Coronary Artery Disease Patients? Acta Med Iran. 2016 Mar;54(3):173–5. [PubMed] [Google Scholar]
- 22.Al-Qudah Z, Yacoub H, Souayah N. Disorders of the Autonomic Nervous System after Hemispheric Cerebrovascular Disorders: An Update. J VascInterv Neurol. 2015 Oct;8(4):43–52. [PMC free article] [PubMed] [Google Scholar]
- 23.Jong-Ho Park, Bruce Ovbiagele, Wuwei Feng. Stroke and sexual dysfunction — A narrative review. Journal of the Neurological Sciences. 2015 Mar 15;350(1):7–13. doi: 10.1016/j.jns.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 24.Pozo ME, Fang SH. Watch and wait approach to rectal cancer: A review. World J Gastrointest Surg. 2015 Nov 27;7(11):306–12. doi: 10.4240/wjgs.v7.i11.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hackett G, Krychman M, Baldwin D, Bennett N, El-Zawahry A, Graziottin A, Lukasiewicz M, McVary K, Sato Y, Incrocci L. Coronary Heart Disease, Diabetes, and Sexuality in Men. J Sex Med. 2016 Jun;13(6):887–904. doi: 10.1016/j.jsxm.2016.01.023. [DOI] [PubMed] [Google Scholar]
- 26.Almeida PH, Castro Ferreira Cd, Kurizky PS, Muniz LF, Mota LM. How the rheumatologist can guide the patient with rheumatoid arthritis on sexual function. Rev Bras Reumatol. 2015 Sep-Oct;55(5):458–63. doi: 10.1016/j.rbr.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 27.Corona G, Isidori AM, Aversa A, Burnett AL, Maggi M. Endocrinologic Control of Men's Sexual Desire and Arousal/Erection. J Sex Med. 2016 Mar;13(3):317–37. doi: 10.1016/j.jsxm.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 28.Shearer M.R. Shearer.Sexuality and sexual counseling in the elderly. ClinicalObstretics and Gynaecology. 20(11977):197–208. doi: 10.1097/00003081-197703000-00024. [DOI] [PubMed] [Google Scholar]
- 29.Shiri, Koskimäki J, Häkkinen J, et al. “Effects of age, comorbidity and lifestyle factors on erectile function: Tampere Ageing Male Urological Study (TAMUS),”. European Urology. 2004;45(5):628–633. doi: 10.1016/j.eururo.2003.11.020. [DOI] [PubMed] [Google Scholar]
- 30.Rosen RC. Reproductive health problems in ageing men. Lancet. 2005;366:183–185. doi: 10.1016/S0140-6736(05)66885-7. Shiri R et al. Prevalence and severity of erectile dysfunction in 50 to 75 year old Finnish men. J Urol 2003; 170: 2342–2344. [DOI] [PubMed] [Google Scholar]
- 31.Diagnostic and Statistical Manual of Mental Disorders:DSM-5. 5th Ed. Washington DC: American Psychiatric Publishing; 2013. pp. 423–460. 685-706. [Google Scholar]
- 32.Hogan Douglas R. The effectiveness of sex therapy: A review of literature. In: LoPicolo Joseph, LoPicolo Leslie., editors. Handbook of sex therapy. New York: Plenum Press; 1978. pp. 57–84. [Google Scholar]
- 33.SathyanarayanaRao T.S, Shahajan Ismail, Darshan MS, Abhinav Tandon. Sexual disorders among elderly: An epidemiological study in south Indian rural population. Indian Journal of Psychiatry. 2015;57(3):236–241. doi: 10.4103/0019-5545.166618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shifran JL, Monz BU, Russo PA, et al. Sexual problems and distress in United States women. Obs And Gyn. 2008;112(5):970. doi: 10.1097/AOG.0b013e3181898cdb. [DOI] [PubMed] [Google Scholar]
- 35.Bertschneider J, Macoy N. Sexual minterest and behavior in healthy 80-102 years old.actions of sexual behavior. 1988;17:109. doi: 10.1007/BF01542662. [DOI] [PubMed] [Google Scholar]
- 36.Feldman H. A, Goldstein I, Hatzichristou D. G, Krane R. J, McKinlay J. B. “Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study,”. The Journal of Urology. 1994;151(1):54–61. doi: 10.1016/s0022-5347(17)34871-1. [DOI] [PubMed] [Google Scholar]
- 37.Corona G, Lee D. M, Forti G, et al. “Age-related changes in general and sexual health in middle-aged and older men: results from the European Male Ageing Study (EMAS),”. The Journal of Sexual Medicine. 2010;7(4):1362–1380. doi: 10.1111/j.1743-6109.2009.01601.x. [DOI] [PubMed] [Google Scholar]
- 38.Shiri R, Koskimäki J, Häkkinen J, et al. “Effects of age, comorbidity and lifestyle factors on erectile function: Tampere Ageing Male Urological Study (TAMUS),”. European Urology. 2004;45(5):628–633. doi: 10.1016/j.eururo.2003.11.020. [DOI] [PubMed] [Google Scholar]
- 39.Rosen RC. Reproductive health problems in ageing men. Lancet. 2005;366:183–185. doi: 10.1016/S0140-6736(05)66885-7. Shiri R et al. Prevalence and severity of erectile dysfunction in 50 to 75 year old Finnish men. J Urol 2003; 170: 2342–2344. [DOI] [PubMed] [Google Scholar]
- 40.George LK, Weiler SJ. Sexuality in middle and late life. Arch Gen Psychiatry. 1981;38:919. doi: 10.1001/archpsyc.1981.01780330077008. [DOI] [PubMed] [Google Scholar]
- 41.Renshaw DC. Sex, intimacy and the older women. Women Health. 1983;8:43. doi: 10.1300/J013v08n04_05. [DOI] [PubMed] [Google Scholar]
- 42.Derogatis LR, Burnett AL. The epidemiology of sexual dysfunctions. J Sex Med. 2008;5(2):289. doi: 10.1111/j.1743-6109.2007.00668.x. [DOI] [PubMed] [Google Scholar]
- 43.Greendale GA, Hogan P, Shumaker S, et al. Sexual function in Postmenopausal women: The Postmenopausal Estrogen/Progestin Intervention (PEPI) trial. J Women Health. 1996;5:445. [Google Scholar]
- 44.LeIblum, Sandra R, Koochaki, et al. Hypoactive sexual desire disorder inpostmenopausalwomen : US Result from Women International Study of health and sexuality (WISHeS) Menopause. 2006;13(1):46. doi: 10.1097/01.gme.0000172596.76272.06. [DOI] [PubMed] [Google Scholar]
- 45.Shifran JL, Monz BU, Russo PA, et al. Sexual problems and distress in United States women. Obs And Gyn. 2008;112(5):970. doi: 10.1097/AOG.0b013e3181898cdb. [DOI] [PubMed] [Google Scholar]
- 46.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999;281(6):537–544. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 47.Lindau ST, Schumm LP, Laumann EO, Levinson W, O’Muircheartaigh CA, Waite LJ. A study of sexuality and health among older adults in the United States. N Engl J Med. 2007;357(8):762–774. doi: 10.1056/NEJMoa067423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen LW, Chen MY, Chen KY, Lin HS, Chien CC, Yin HL. Topiramate-associated sexual dysfunction: A systematic review. Epilepsy Behav. 2017 Jun 9;73:10–17. doi: 10.1016/j.yebeh.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 49.Mahmoud A, Hayhurst KP, Drake RJ, Lewis SW. Second generation antipsychotics improve sexual dysfunction in schizophrenia:A randomized controlled trial. Schizophrenia Research and Treatment. 2011 doi: 10.1155/2011/596898. Article ID 596898, 6 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rosen RC, Lane RM, Menza M. Effects of SSRIs on sexual function: a critical review. J ClinPsychopharmacol. 1999;19:67–85. doi: 10.1097/00004714-199902000-00013. [DOI] [PubMed] [Google Scholar]
- 51.Vester-Blokland ED, Van der Flier S, Rapid Study Group . Program and abstracts of the American Psychiatric Association 156th Annual Meeting. San Francisco, California: 2003. May 17-22, Sexual functioning of patients with major depression treated with mirtazapine orally disintegrating tablet or sertraline. Abstract NR494. [Google Scholar]
- 52.Corona G, Lee D. M, Forti G, et al. “Age-related changes in general and sexual health in middle-aged and older men: results from the European Male Ageing Study (EMAS),”. The Journal of Sexual Medicine. 2010;7(4):1362–1380. doi: 10.1111/j.1743-6109.2009.01601.x. [DOI] [PubMed] [Google Scholar]
- 53.Sadock VA. Sadock BJ, Sadock VA, Ruiz P. Kaplan and Sadock's Comprehensive Textbook of Psychiatry. Ninth Edition. 18.1a. Lippincott Williams and Wilkins; 2009. Normal Human Sexuality and Sexual Dysfunctions; pp. 2027–59. [Google Scholar]
- 54.Clayton AH, Hamilton DV. Female sexual dysfunction. Psychiatric Clin N Am. 2010;33(2):323. doi: 10.1016/j.psc.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 55.AvasthiA& Banerjee ST. Guidebook on sex education. Marital and Psychosexual Clinic, Department of Psychiatry, PGIMER, Chandigarh. 2002 [Google Scholar]
- 56.Hogan, Douglas R. The effectiveness of sex therapy: A review of literature. In: LoPicolo Joseph, LoPicolo Leslie., editors. Handbook of sex therapy. New York: Plenum Press; 1978. pp. 57–84. [Google Scholar]
- 57.Annon, Jack S. New York: Harper & Row; 1976. The behavioral treatment of sexual problems:Brief Therapy. [Google Scholar]
- 58.Kaplan HS. New York: Brunner/Mazel; 1974. The new sex therapy: Active treatment of sexual dysfunctions. [Google Scholar]
- 59.Hawton K. The behavioral treatment of sexual dysfunction. British J Psychiatry. 1982;140:94–101. doi: 10.1192/bjp.140.1.94. [DOI] [PubMed] [Google Scholar]
- 60.Gholamine B, Shafiei M, Motevallian M, Mahmoudian M. Effects of pioglitazone on erectile dysfunction in sildenafil poor-responders: a randomized, controlled study. J Pharm Pharm Sci. 2008;11(1):22–31. doi: 10.18433/j3tg6h. [DOI] [PubMed] [Google Scholar]
- 61.Gasto´ N J. Rey-Valzacchi, Pablo R. Costanzo, Luis A. Finger, Alberto O. Layus, Guillermo M. Gueglio, Leo´ N E. Litwak. pabloknoblovits Addition of metformin to sildenafil treatment for erectile dysfunction in eugonadalnondiabetic men with insulin resistance A prospective, randomized, double-blind pilot study. Journal of andrology. 2012 Jul-Aug;33(4) doi: 10.2164/jandrol.111.013714. [DOI] [PubMed] [Google Scholar]
- 62.Min ChulCho, Jae-Seung Paick. Udenafil for the treatment of erectile dysfunction. TherClin Risk Manag. 2014;10:341–354. doi: 10.2147/TCRM.S39727. Published online 2014 May 14. doi: 10.2147/TCRM.S39727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Van Ahlen H, Piechota H.J, Kias H.J, Brennemann W, Klingmuller D. Opiate antagonistsin erectile dysfunction: a possible new treatmentoption Results of a pilot study with Naltrexone? European Urology. 1995;28:246–250. doi: 10.1159/000475059. [DOI] [PubMed] [Google Scholar]
- 64.Padma-Nathan H. Efficacy and tolerability of Tadalafil, a novel phosphodiesterase 5 inhibitor in treatment of erectile dysfunction. American Journal of Cardiology. 2003;92:19M–25M. doi: 10.1016/s0002-9149(03)00828-2. [DOI] [PubMed] [Google Scholar]
- 65.Bella A.J, Brock G.B. Intracavernous Pharmacotherapy for erectile dysfunction. Endocrine. 2004;23:149–155. doi: 10.1385/ENDO:23:2-3:149. [DOI] [PubMed] [Google Scholar]
- 66.Fink HA, MacDonald R, Rutks IR, Wilt TJ. Trazodone for erectile dysfunction: a systemic review and meta-analysis. British Journal of Urology International. 2003;92:441–446. doi: 10.1046/j.1464-410x.2003.04358.x. [DOI] [PubMed] [Google Scholar]
- 67.Chen J, Mabjeesh N.J, Matkzin H, Greenstein A. Efficacy of sildenafil as adjuvant therapy to selective serotonin reuptake inhibitor in alleviating premature ejaculation. Urology. 2003;61:197–200. doi: 10.1016/s0090-4295(02)02075-7. [DOI] [PubMed] [Google Scholar]
- 68.Linet OI, Ogrinc FG. Efficacy and safety of intracavernosalalprostadil in men with erectile dysfunction. TheAlprostadil Study Group, New England Journal of Medicine. 1996;334:873–877. doi: 10.1056/NEJM199604043341401. [DOI] [PubMed] [Google Scholar]
- 69.Ghadiri MK, Gorji A. Review of Impotence: Natural remedies for impotence in medieval Persia. International Journal of Impotence Research. 2004;16:80–83. doi: 10.1038/sj.ijir.3901153. [DOI] [PubMed] [Google Scholar]
- 70.Shelly TE, McInnis DO. Exposure to ginger root oil enhances mating success of irradiated, mass-reared males of Mediterranean fruit fly (Diptera: Tephritidae) J Econ Entomol. 2001;94:1413–1418. doi: 10.1603/0022-0493-94.6.1413. [DOI] [PubMed] [Google Scholar]
- 71.Qureshi S, Shah AH, Tariq M, Ageel AM. Studies on herbal aphrodisiacs used in Arab system of medicine. Am J Chin Med. 1989;17:57–63. doi: 10.1142/S0192415X89000103. [DOI] [PubMed] [Google Scholar]
- 72.Kamtchouing P, et al. Effects of Aframomummelegueta and Piper guineenseon sexual behaviour of male rats. BehavPharmacol. 2002;13:243–247. doi: 10.1097/00008877-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 73.Gonzales GF, et al. Effect of Lepidiummeyenii (Maca), a root with aphrodisiac and fertility-enhancing properties, on serum reproductive hormone levels in adult healthy men. J Endocrinol. 2003;176:163–168. doi: 10.1677/joe.0.1760163. [DOI] [PubMed] [Google Scholar]
- 74.Kashani L, Raisi F, Saroukhani S, et al. Saffron for treatment of fluoxetine-induced sexual dysfunction in women: Randomized double-blind placebo-controlled study. Hum PsychopharmacolClin Exp. 2012;28(1):54–60. doi: 10.1002/hup.2282. [DOI] [PubMed] [Google Scholar]
- 75.Aldemir M, Okulu E, Neselioglu S, Erel O, Kayigil O. Pistachio diet improves erectile function parameters and serum lipid profiles in patients with erectile dysfunction. Int J Impot Res. 2011;23(1):32–38. doi: 10.1038/ijir.2010.33. [DOI] [PubMed] [Google Scholar]
- 76.SathyanarayanaRao T.S, Chittaranjan Andrade. Flibanserin: Approval of a controversial drug for a controversial disorder. Indian Journal of Psychiatry. 2015;57(3):221–223. doi: 10.4103/0019-5545.166630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.SathyanaryanaRao T S, Gupta S, Tandon A. Intimacy Matters: Elderly Sexuality. Indian Association for Geriatric Mental Health. 2011:70–118. [Google Scholar]
- 78.Lothstein L. M. The Aging Gender Dysphoria (Transsexual) Patient. Archives of Sexual Behavior. 1979;8(5) doi: 10.1007/BF01541199. [DOI] [PubMed] [Google Scholar]
- 79.Raphael J. Leo, Kye Y.Kim. Clomipramine Treatment of Paraphilias in Elderly Demented Patients. Journal of Geriatric Psychiatry and Neurology. 8(2):123–124. doi: 10.1177/089198879500800210. [DOI] [PubMed] [Google Scholar]
- 80.Esther Sapire K. Contraception and Sexuality in Health and Disease. McGraw-Hill Book Company (UK) Limited; 1990. [Google Scholar]
- 81.SathyanarayanaRao T.S. Psychobiology of love and sexual relationships in elderly: Issue in management. Journal of Geriatric Mental Health. 2016 Jul-Dec;3(2):91–99. [Google Scholar]
- 82.Geneva: WHO; 2006. Defining sexual health Report of a technical consultation on sexual health 28–31 January 2002. [Google Scholar]


