This guideline seeks to summarize available data (including 2006 IPS Guidelines) on healthy ageing and rehabilitation needs of older adults, with the hope that this knowledge will help ensure uniform standards of rehabilitation care. This guideline in no way claims to be comprehensive or definitive. Mental health professional involved in caring for this special population group should consider, but not be limited by the recommendations made herein. Older adults in different settings need to be cared for in different ways. In this document we have tried to formulate types of care at all the possible levels. However, these might not be wholly suitable for all treatment settings.
This document must be regarded only as a preliminary effort, especially given the paucity of high level of evidence worldwide. It is expected that several modifications and revisions will be required to improve its usefulness. Hence, inputs and critical comments from mental health professionals across the country will be more than welcome, in this regard.
We will be talking about health and ageing with need of rehabilitation, and then will move onto disease perspective i.e., from rehabilitation in healthy ageing to rehabilitation in geriatric mental health illness.
As we have moved from “years to life” to “life to years”, rehabilitation has become an essential component of geriatric care and therapy.
1. Foreword
-
As per World Health Organization, rehabilitation intervention should be aimed at achieving following broad objectives:
- preventing the loss of function
- slowing the rate of loss of function
- improving or restoring function
- compensating for lost function
- maintaining current function
The goal of rehabilitation in older people, with or without any underlying psychiatric illness should be development of physical independence, and their ability to do as many daily living activities, as possible.
2. Problem statement:
-
Changing demographics: India is in a state of demographic transition.
- The improvements in health services have increased the life expectancy from 33 years (1951) to 69 years (2011).
- There has been a surge not only in general population but also in elderly population. The absolute number of elderly has increased to 97 million in 2017, compared to 12.5 million in 1951.
-
Morbidity challenges: Physical and Mental health morbidity for this population cohort:
- Prevalence of physical morbidity varies from 10-50%
- Prevalence of mental health morbidity is of 20%
Most common morbidity is related to vision (66.5%) followed by musculoskeletal problems (58.5%), anemia (43%), hypertension (27.5%), psychological problems (24.5%), hearing problems (11%) and, diabetes (6%).
-
Social Challenges:
- Burden of booming elderly population, especially from rural India (more than 70 % are hailing from rural India).
- Most belong to below poverty line, with poor financial and social support.
- Increasing feminization of the population. (Indian demographics is not much different from world demographics)
- Urbanization and migration associated social change and challenges.
- Nuclear family system.(decreases social support)
- Changing role of females from home maker to full time office goers.
3. Healthy ageing: Healthy ageing is a concept promoted by World Health Organization (WHO), that considers the ability of people of all ages to live a healthy, safe and socially inclusive lifestyle. It recognizes the factors beyond health and social care that have a major effect on health and well-being, and the contribution that must be made by all sectors with an influence on the determinants of health. Healthy ageing is a broad concept which includes many aspects of living, as shown in the figure 1.
Fig. 1.

Aspects of healthy ageing
Aspects of healthy living:
a) Health and health care: ‘He who has health has hope, and he who has hope has everything’, is a well known Arabic Proverb.
Healthy ageing with respect to health care implies, being able to continue to maintain a healthy lifestyle, regular physical activity and make accommodations for any changes in body function, e.g. hearing, vision, flexibility or strength.
Continue to engage in routine preventive health behaviors (e.g. participate in cancer screenings and stay physically and mentally active).
Continue to advocate for oneself and one's family in health care settings or bring a knowledgeable representative with oneself.
Keep an accurate record of all medications with dosing instructions to review with health care providers.
Maintain good stress management and emotional health. Socialization, activity, and access to quality health care and transportation will all help one remain healthy, happy and engaged as they age.
b) Legal and financial:
Careful monitoring of one's financial resources.
Examine any work-related benefits, such as social security or pension.
Review health care and insurance plans to make sure coverage is adequate for the needs.
Continue to consider one's health care wishes and discuss these with family members, friends and physicians.
Make a plan and leave instructions for any resources (financial or otherwise) that may survive you.
c) Work life and retirement:
Retirement planning is the process of gathering financial data, lifestyle information and insight into the three major activities at retirement: Leisure, Volunteer work and full or part-time paid work.
Transition into a less stressful career if one wishes. Consider a part-time “bridge job” that will not only ease transition into retirement but also reduce the overall financial need.
Become knowledgeable about the continuum of living arrangements and services available for older adults.
Go on fact finding trips to scout out places one might like to live after leaving the workforce, determining the best fit for later life interests.
Choose or make accommodations to a home in which one would want to live even when his physical abilities decline.
d) Psychological:
Psychological factors have a powerful influence on the experience of aging. These influences include one's identity and personality, spirituality, personal control, competence, emotional stability and ability to manage stress.
Those people who have a sense of involvement in the care of the next generation, have a positive outlook and find meaning in life.
Be mentally and physically active to help preserve cognitive skills and maintain overall health.
Maintain ties with friends and family to maximize the social support system.
Remain aware of new developments in the arts, sciences, politics, and other areas of cultural and social interest.
If one has religious beliefs, consider how it supports the understanding of the meaning of life.
‘It's a time to consider with compassion, new views and lifestyles of young people even when they clash with our own.’
e) Social roles and resources: Think of yourself as an age pioneer! Keep up with old interests and develop new ones.
Develop and maintain those aspects of life which enhance psychological, social and intellectual well-being.
Stable social relations can provide a sense of life-long continuity.
Nurture relationships among family and friends that are most important.
Change social activities as needed following retirement.
Develop new relationships that fill gaps created by losing important loved ones.
Anticipate and plan for the future—for good and bad times.
“Our social world is always changing, so plan for and adapt to that reality throughout our life span.”
4. Disability and its types: Disability is an umbrella term, covering impairment, activity limitation, and participation restriction. Impairment is a problem in body function or structure; an activity limitation is a difficulty encountered by an individual in executing a task or action; while a participation restriction is a problem experienced by an individual in involvement in life situations. It's a complex phenomenon, not just a health problem. It reflects the interaction between features of a person's body and features of the society in which he or she lives. Overcoming the difficulties faced by people with disabilities requires interventions to remove environmental and social barriers.
-
Various types of disabilities are as follows:
- Physical or movement problems: such as impaired motor control, loss of limbs, reduced balance, strength or cardiovascular fitness, fatigue, pain or stiffness.
- Sensory problems: such as impairment of vision or hearing, pain, loss of or altered sensation of touch.
- Cognitive or behavioral problems: such as lapses in memory and attention, difficulties in organization, planning and problem-solving.
- Communication problems: such as difficulties in speaking, using language to communicate and fully understanding what is said or written.
- Psychosocial and emotional problems: such as the effects on the individual, care giver and family of living with a long-term condition. These can include stress, depression, loss of self-image and cognitive or behavioral issues.
- Medically unexplained symptoms: where a holistic approach is needed to ensure the best possible support for both mental and physical wellbeing.
- Mental health conditions: such as anxiety and depression, obsessive/compulsive disorders, schizophrenia, eating disorders, post-traumatic stress disorder or dementia.
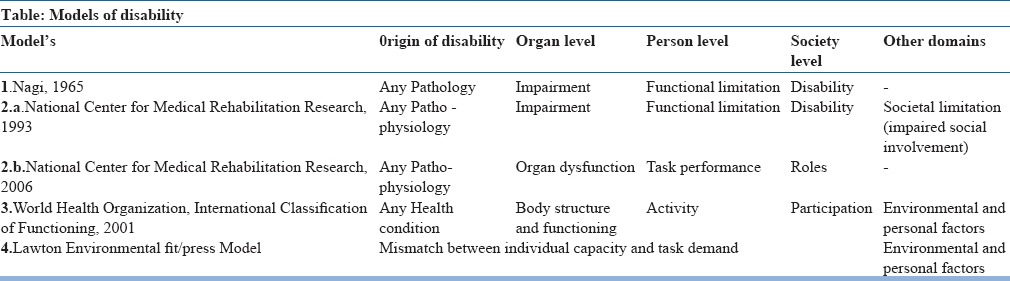
5. Conceptual models of disability:
NAGI's model: The first disablement model was introduced in 1965 by Saad Nagi, who noticed semantic and conceptual confusion in the disability literature regarding disability and its associated concepts. Nagi recognized the importance of the environment and that family, society and community factors could all influence disability. Nagi created a model with 4 components: physiological impairment, functional limitation, disability and handicap. This model is historical, however it provided standardized terminology for disability.
More recent models of disablement however, have evolved from the Nagi model in an attempt to better encompass all the dimensions of disability and the external factors that influence disablement. Some adaptations have included the addition of socio-cultural factors, such as the social and physical environment and personal factors (including attitudes and lifestyle behaviors), as well as an emphasis on quality of life and focus on the interaction between health conditions and contextual factors. Of particular note is the National Center for Medical Rehabilitation Research model (NCMRR) given in 1993. This was revised again in 2006.
-
International Classification of Functioning disability and health (ICF) model: The disablement model created by the WHO in 1980 has been revised several times during the last 2 decades. The most recent model is the ICF, which was introduced in 2001 with the goal of creating a common international language for disability.
- Bio-psycho-social model: ICF model indicates that an individual's level of function (body function, ability to execute a task and participate in life activities) is determined by his or her health condition(s) within the context of environmental and personal factors.
- The rehabilitation services should target not just the impairment, activities and participation levels of the disablement process, but also the personal and environmental contextual factors that influence activity and participation.
Thus, effective treatment of late life disability is typically multimodal.
-
Lawton model of environmental press: Ecological, Person or Environmental fit model.
- Disability results from a mismatch between individual capacity and task demands, which in turn are influenced by the environment and the way in which tasks are performed.
- Remediation of disability occurs through treatments that either increase individual capacity or reduce task demand.
Medical or surgical treatments have the potential to increase capacity. Rehabilitation interventions may improve capacity, reduce task demands or accomplish both (Table-1: Summary of the Disability Models).
Table 1.
Summary of the Disability Models
6. Assessment of disability in an elderly:
A systematic approach is useful for the assessment of new onset or progressive disability in an older adult (Figure: 2).
Fig. 2.
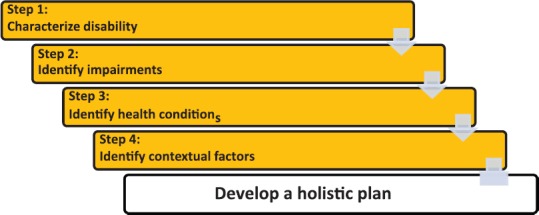
Flow chart for assessment of disabilities in elderly
Characterize the disability — clearly describe the disability, including its onset, time course and impact on patient and caregivers.
Identify impairments — Initial history and examination should focus on identifying the physical and psychiatric issues involved in causing the functional decline or disability.
Identify health conditions — once the problem area is identified, standard differential diagnostic methods are used to identify the specific health conditions underlying or contributing to the patient's disability.
Identify contextual factors — Understanding patient's physical environment, social support, and financial resources is important in developing a feasible management plan.
A comprehensive assessment of elderly is necessary, with focus on availability and accessibility of resources, affordability and acceptability of the patient and care giver. Important points for this are:
Perspectives of both the patient and caregiver are important to consider.
A brief screening test for physical and cognitive impairment should be performed in a patient with new or progressive disability, even if the patient does not endorse memory problems.
When feasible, a home visit is the best way to understand how the patient functions within his or her environmental and social context.
Physical or occupational therapy (OT) home health assessments or other community programs may help to accomplish this.
In patients with multiple health conditions, it is frequently impossible to identify a primary cause or trigger for the disability. Rather, identifying all contributing conditions, impairments and contextual factors and addressing these factors with appropriate interventions is the most effective means of reducing functional dependence.
Appendix contains commonly used assessment tools for quick assessment{(Physical cognitive balance screening test, Activities of daily living (ADL) and Instrumental activities of daily living (IADL)}.
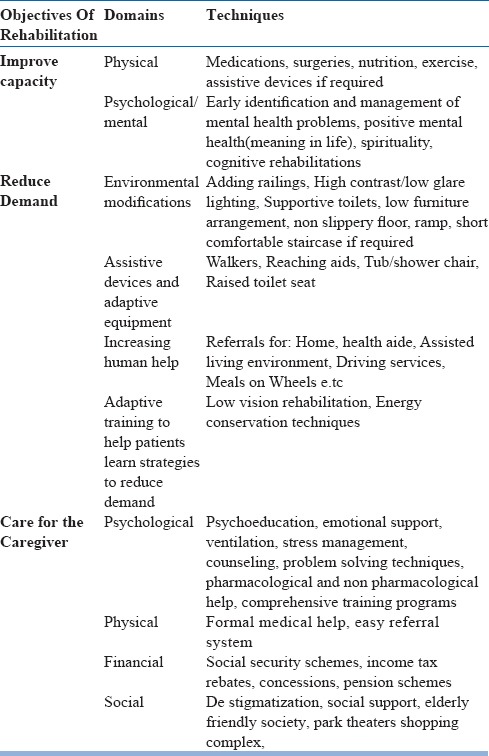
7. Approach to management of disability in an elderly:
Once the underlying health conditions, impairments and contextual factors are understood, a practical management plan can be developed with the patient and family.
These plans generally include strategies to enhance functional abilities (i.e. improve capacity), decrease functional demands (i.e. reduce demand), or both (Figure 3).
Strategies to improve capacity — clinician should identify ways to improve the patient's capacity to cope with physical and environmental challenges.
Fig. 3.
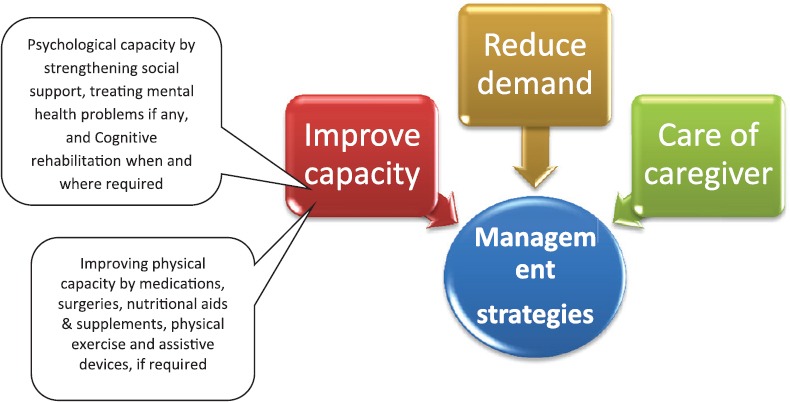
Approach to management of disability in elderly
a) Medications, e.g.:
Oxygen or cardiac medications to improve hemodynamics in patients with heart failure
Antidepressants for patients with depression
Analgesics for chronic pain
Discontinuing unnecessary medications that may have adverse side effects (e.g. chronic use of proton pump inhibitors has effects on cognition and bone health).
b) Surgery, e.g.:
Cataract excision to improve visual capacity
Joint replacement in disabling arthritis
c) Nutritional intervention, e.g.:
Weight loss for obesity
Nutritional supplements when nutrition is impaired
d) Exercise, e.g.:
General physical activity to improve aerobic capacity
Targeted exercises to address a specific impairment (e.g. range of motion and strengthening exercises for knee)
e) Prosthetics and assistive devices, e.g.:
Hearing aids
Artificial limbs
Ankle orthosis
f) Neuropsychological rehabilitation, e.g.:
Cognitive training
Reality orientation
-
Emotional retraining
- Strategies to reduce demand — If the patient's capacity for physical function cannot be sufficiently improved by treating the underlying health conditions and/or use of interventions such as exercise alone, then strategies to reduce the task demands should be considered.
-
a)
Environmental modifications, e.g.: Adding railings, High contrast/low glare lighting
-
b)
Assistive devices and adaptive equipment, e.g.: Walkers, Reaching aids, Tub/shower chair, Raised toilet seat
-
c)
Increasing human help, e.g. referrals for: Home health aide, Assisted living environment, Driving services, Meals on Wheels
-
d)
Adaptive training to help patients learn strategies to reduce demand, e.g.: Low vision rehabilitation, Energy conservation techniques
Care of the caregiver – Informal, lay caregiver or primary caregiver is still the anchor of the rehabilitation process in developing countries. Their needs and problems are still highly neglected. A large majority of caregivers experience fatigue, frustration, and stress as a result of care giving. Family members and other providers often accept responsibility for the care of those with chronic health needs. As time and illness progress, the responsibility may be met with decreasing enthusiasm, and caregivers may find themselves angry or resentful about this toll on their lives. Important aspects in assessment and management of care givers are:
a) Assessment of causes of burnout or burden.
b) Training programs for caregivers. (Table-2: Summary of Different Management Strategies).
Table 2.
Summary of Different Management Strategies
8. Multidisciplinary approach to rehabilitation:
Rehabilitation in elderly needs multidisciplinary approach keeping patient and care giver at the focus.
The geriatric mental health professional needs to liaise with a host of various specialists to device treatment strategies. This need for multidisciplinary approach is depicted in figure: 4.
Fig. 4.
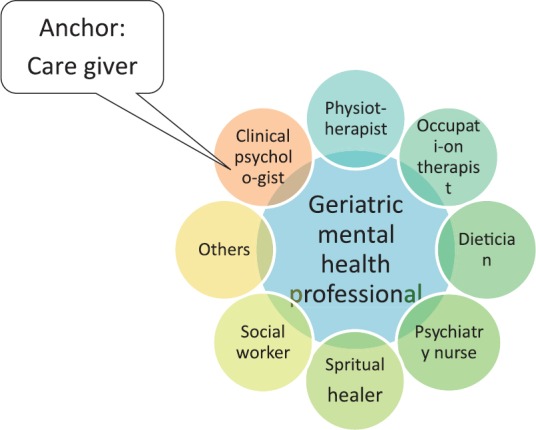
Multidisciplinary approach towards rehabilitation
There is a defined role for each of these specialists.
Clinical psychologist: Assessment and management of cognitive and behavioral problems, via cognitive, psychological and behavioral retraining. This is helpful especially for those who cannot or will not tolerate medication, are dealing with stressful interpersonal difficulties, have limited level of social support or have recurrent episodes of mental illness.
Nutrition therapist or dietician: Frailty as well as obesity should be targeted in time to prevent its long term consequences in form of fall factures, bed ridden, loss of independence and cognitive deprivation. Nutrition and physical activity are two important determinants of physical as well as mental health. Mental and physical health has a complex interplay with nutrition and physical activity, as shown in fig. 5.
Fig. 5.
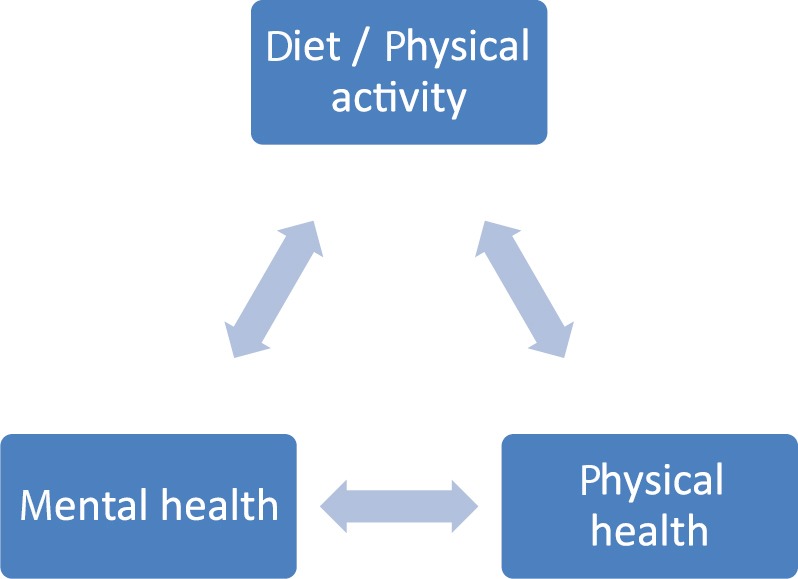
Role of nutrition and physical activity on mental health
For e.g., in dementia omega 3 fatty acids are protective or moderate alcohol intake may be protective for dementia which in turn may be caused by heavy drinking.
Illness per se effects nutritional status, e.g. in early phase of dementia there may be inability to prepare and procure food; leading to nutritional deficiency. During later stages there may be inability to consume sufficient oral meal.
Other conditions like depression, bipolar and other situational conditions (mood disorders: bereavement and loneliness), may cause decrease intake, leading to fraility, cachexia and anorexia.
Physiotherapist: Helps in assessment and management of mobility related issues of elderly. Interventions can be in form of aerobic exercises, yoga, and muscle strengthening activities to increase flexibility and improve balance. Development and implementation of an activity plan should be tailored according to individual capacity.
Occupational therapist: They plan various activities for the behavioral and cognitive stimulation of the patients. These should be individualized and based according to the resources available.
-
Psychiatric social worker: Helps in evaluation of the materialistic and manual resources of the subjects. Provides psycho education about the illness. It should be low and dose dependent. Family therapy is important component in geriatric rehabilitation. Important reminders are:
- Family care is an adaptive challenge
- Family rarely has one voice
- Few have only one to care at one time
- There is no one way or ideal way of family care
- Successful caregivers are flexible in adjusting to expectations of themselves and the patient
- Caregivers awareness to available services is important
- It is better to help them develop their way of handling situations
- Denial is common defense in caregivers to provide hopeful consistent daily care
- Help them understand and develop contingency plans
A social worker also help caregivers with different government and non-governmental information's, which will be of help to them i.e., pension scheme, income tax rebate, e.t.c.
Spiritual healer: Spirituality has been conceptualized as including an individual's transcendent relationship with a higher being or with the universe and has been positively linked to hope, coping and religiosity. It has been found to be particularly important among older adults and positively linked to self-appraised good health among elders.
Psychiatry nurse: Psychiatry nurses work in collaboration with older adults, their families, and communities to support healthy ageing, maximum functioning and quality of life.
Recreational therapist: Assessment and management of leisure preferences, adaption and integration into therapeutic plan e.g., art therapy or music therapy.
Helper: could be either a ward boy or a family member, who fits the role of support staff.
Others: These may be in the role of Orthotist, Prosthetist, Optometrist, Speech therapist, and other specialists as needed.
9. Planning a rehabilitative strategy:
Aims of the rehabilitation program are:
To make the life of elderly more meaningful and dignified.
To help them to be as much self-sufficient as possible.
To improve the overall quality of life by enhancing and ensuring optimal utilization of their preserved abilities, minimizing the need of their lost abilities and providing necessary assistance for better functioning.
-
Following are the steps of planning a comprehensive rehabilitation program for an elderly (Figure: 6)-
- Establish a rapport and a therapeutic alliance with the individual and his family members or caregivers. In order to get maximum benefit from the program, it is absolutely essential that the family members have understood the need for the program.
- Assessment of impairment: rehabilitation program has to be tailor made for each individual and so it will have to be planned depending on the nature and extent of impairment with due focus on the activities of daily living.
- Having assessed the impairment, one would like to develop strategies to overcome it. In order to do so, one would need to know about the available resources in the form of manpower (caregivers: trained/untrained), availability of rehabilitation centers, day-care centers, the medical and paramedical staffs and financial resources.
Fig. 6.

Steps for planning a rehabilitation program
Plan should be affordable, easily available, accessible and most important acceptable for the care giver.
Charting out a rehabilitation program: a comprehensive rehabilitation program would include certain common general measures which one would like to observe for all the patients and specific measures which are specifically tailor made for a particular patient.
Common general measures:
Maintain daily rhythm and daily schedule.
Maintain orientation to time, day, date, month, year, touch with recent events and new developments.
Maintain active participation in routine and extracurricular activities.
Practice to use of new devices, gadgets and instruments.
Make provisions for easy and well supported mobility.
Avoid frequent change in home and living arrangements.
Adapt an active life, and never retire.
Small frequent meals.
Easy to wear clothes, toiletry needs.
Reduction to complete stoppage of substances like alcohol-tobacco etc, regular sleeping pattern.
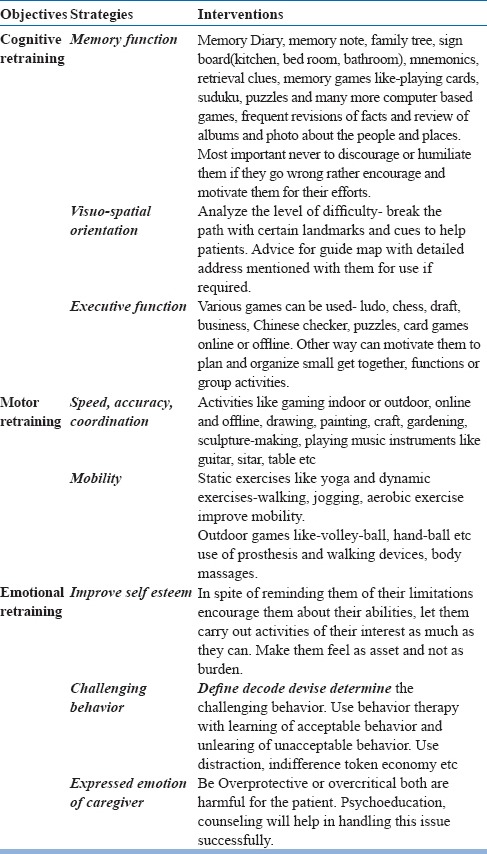
Specific Measures: These measures can be implemented at home with the help of relatives or community health workers, under supervision of a mental health professional, at the memory clinic or day-care-center with the help of trained staff, or at the residential care facility where the patient is staying.
Cognitive retraining: may be utilized to help the patients having cognitive deficits in various areas. This may improve some of the cognitive skills of the patient and may prevent or at least slow down the further decline in cognitive abilities.
-
a)
To improve the memory function: Patients may be asked to keep a memory aids, sign boards. Patients may be taught other methods to remember things like using mnemonics or using retrieval clues to remember certain things which patient wishes to remember. As an exercise to improve memory patient may be encouraged to play ‘playing card memory game’ or memory games on computers.
-
b)
To improve visuo-spatial orientation: Patients having problem in visuo-spatial orientation may get lost while traveling. A therapist can escort the patient on his traveling route and help him to recognize and remember certain landmarks and clues which will help patients to travel independently. Patient may also be given a cardwith a map and directions on it to carry with him. In case of difficulty in finding a way, he may show the card to a policeman or a shopkeeper and get the direction from them.
-
c)
To improve executive functions: Planning, organizing, decision making may be compromised in old age. Various games like Ludo, Chess, Draft, Chinese-checkers, puzzles, card-games etc. require these skills. Playing these games help in improving executive functions.
Motor retraining:
-
a)
To improve speed, accuracy and coordination: Many of the computer games improve our speed and accuracy. Usually these games have different levels. Playing these games regularly may improve the speed, accuracy and coordination. Activities like drawing, painting, craft or sculpture making also enhance these skills.
To improve mobility: With the advancing age and especially due to motor or sensory neurological deficits the mobility is very much compromised. Static exercises like yoga and dynamic exercises like walking, jogging, aerobics may be utilized to improve mobility. Participating in outdoor games like volley-ball, hand-ball etc may also be very useful. If required one may use various prosthesis and walking devices to improve the mobility. In past good body massage was used to rejuvenate the body and improve the mobility.
Emotional retraining:
-
a)
To improve the self-esteem and feelings of being a useful member of society: One of the most important parts of the rehabilitation program is to improve the self-esteem of the elderly individuals and make them feel that they are still very important and useful members of the society. Whenever appropriate, the family members should treat them as the heads of the family and seek their opinions, advice and guidance. They may be given some responsibilities according to their interest and abilities.
-
b)
To improve challenging behavior: Occasionally elderly individuals may show childish behavior or disinhibited behavior. One may have to deal appropriately using principles of behavior therapy in these kinds of situations.
-
c)
To improve adverse attitudes of family members & to provide support to family members: Some family members may be overprotective and may not allow the elderly individual in the family to do anything by themselves. On the other hand some family members may be overcritical and keep on condemning the elderly without realizing that the unusual behavior is not intentional but is due to cognitive deficits. In such situations, counseling the family members is very essential for the effective implementation of the rehabilitation program. Table 3 and Table 4 Summary of strategies for planning and execution of rehabilitation in elderly).
Table 3.
General Strategies for planning and execution of rehabilitation in elderly
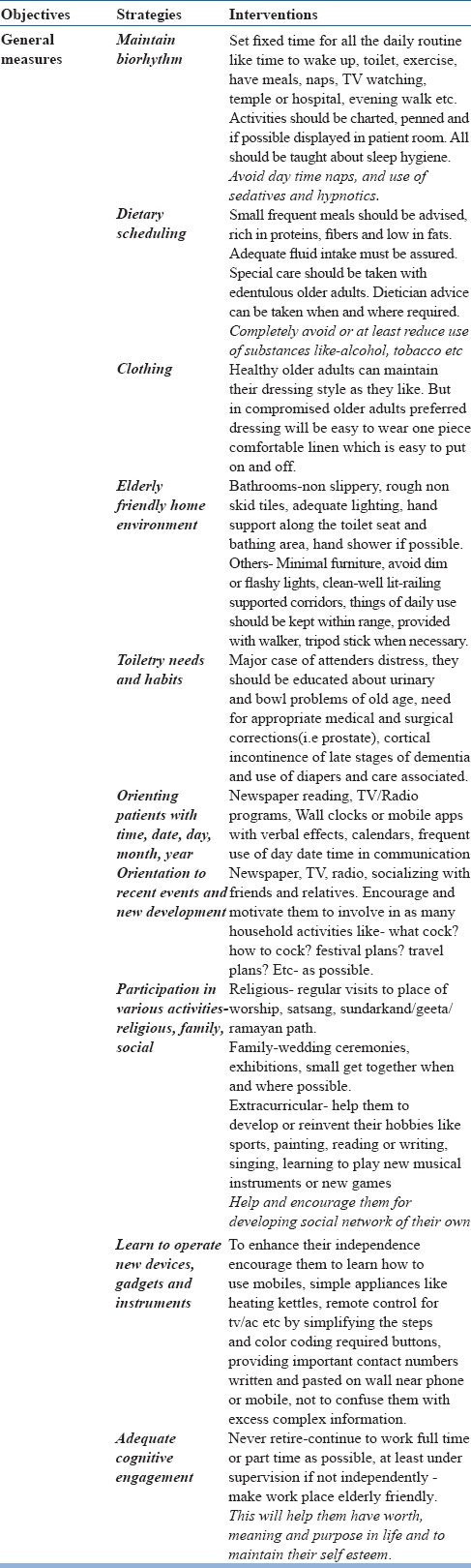
Table 4.
Specific Strategies for planning and execution of rehabilitation in elderly
Important issues while planning a rehabilitation program:
Rehabilitation program should be planned and implemented as early as possible.
The program should be comprehensive and tailored to help the individuals to overcome the practical difficulties in day-to-day life considering socio-cultural environment and urban or rural background.
As one may not be able to implement and achieve too many things simultaneously, it may be a good idea to decide one or two priority-goals at the beginning in the rehabilitation program and work on the other goals after achieving the priority goals.
Look around, think, ask, discuss and you may find an innovative solution to a problem.
One may have to modify the rehabilitation program from time to time according to the changing needs of the persons.
Be vigilant about the masked deficits: these are the deficits which may get unmasked when the individuals face more challenging circumstances.
Take into account the other associated problems: many of the senior citizens may have visual and auditory problems. They may also have other medical problems like arthritis, heart disease, diabetes, hypertension, nutritional deficiencies etc. One of the important issues to keep in mind is ‘elderly abuse’.
While providing the various facilities in a rehabilitation program one should strive to attain the best possible quality of care for our elderly individuals (Figure-7: Steps to be followed in planning of rehabilitation and it's follow up).
Figure 7.

Plan to be followed
10. Levels of care and rehabilitation:
Rehabilitative strategies could be implemented through community based approaches, institution based approaches or through outreach programs.
Community based rehabilitation: This is a strategy of developing rehabilitation services in the community, to provide equal opportunities to all. It attempts social integration of those in need of rehabilitation. There is a collective effort of disabled, family and community.
Institutional based rehabilitation: disabled persons are provided training in hospitals/rehabilitation centers. These function as referral center for community rehabilitation center.
Outreach programs: The experts from hospital visit the community or home for providing education and training to disabled in self care, ambulatory effect, communication, vocational guidance. Camps are also organized from time to time in rural area where community facility is not available. There is need to integrate community rehabilitation centers with institutions to provide maximum rehabilitation coverage to all parts of the country.
These programs depend on health set ups/centers to deliver care. Different communities have different structure of health care facilities which cater to the need of rehabilitation in elderly. Figure 8: Shows the hierarchy of health care system in India.
Fig. 8.
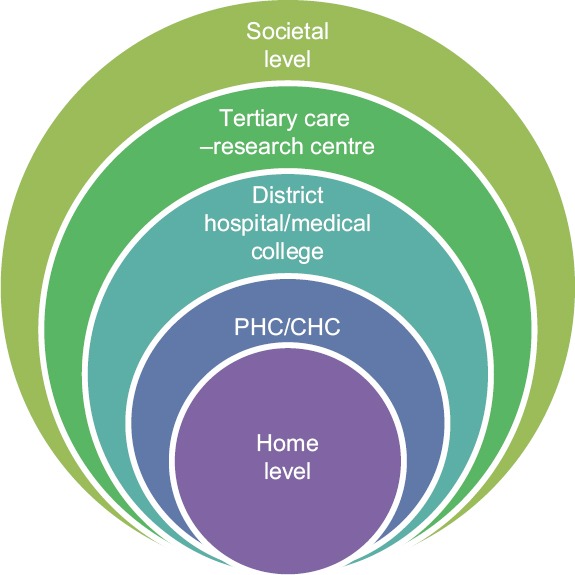
Levels of health care facilities involved in rehabilitation in elderly
Rehabilitative measures at individual level:
Home assisted care: For those individuals who cannot visit the day-care center, community health workers pay home visits to provide the necessary help to the patients and relatives. These are supervised by a mental health professional.
Daycare center: These serve the same purpose in elderly which the school serves in children. Occupational therapists, physiotherapist, and counselors can take classes for them. They will make them sing songs and recite poems, read-out stories to them and give them lessons in drawing, painting and craft. Senior citizens will also receive a sumptuous afternoon meal and supervised dose of medication.
Residential care facility: Senior citizens, who are unable to lead an independent life in their own homes, may require residential care facility. Senior citizens having dementia may also require hospitalization or residential care facility when they develop delirium and behavioral and psychological symptoms associated with dementia (BPSD). Frequently, these patients may have to be restrained and require sedatives and tranquilizers which sometimes may further worsen their situation. In order to provide better facilities to elderly patients and to those who require short-term or long-term hospitalization or institutionalization it is desirable to have good residential care facilities. Cognitive enhancers (Donepezil, Rivastigmine or Galantamine) and psychotropic medications may be sparingly used in the residential care facility. If a patient gets agitated or restless, instead of sedating him or tranquilizing him, he may be pacified using behavioral techniques in a nonthreatening environment. Though these setups are mostly unavailable in India but it is the need of the hour to have such facilities in India to cater the needs of growing population of elderly.
Self-help groups: A group of senior citizens can start a self-help group. This group, like other self-help groups, can meet on regular basis and help the other senior citizens and organize various activities for them on a regular basis.
HelpAge India has felt that field models have to be initiated to address this grave situations where in elders can be Sensitized/facilitated and capacity built to make themselves sustained and help their own peer groups and make themselves occupied. In this process, Elder Self Help Groups under Comprehensive Age Care Models started in the year 1999 to bring all the Active Poor Elders together on a single platform to encourage a social bonding and thrift practice among themselves. Today HelpAge has created 3241 Comprehensive Elder Self Help Group models in 20 States on PAN India basis, which are catering to varied needs of poor active elders as below. Develops strong we feeling and emotional support. Elders help each other in accessing all types of Resources like Govt Schemes, Health facilities, local market linkages. The Elder Group members provide counseling to their own group members and also to other elders living in their community in cases like death, family disputes etc. Internal Group Lending helps Elders to design small business models for Petty Business purposes and these results in achievement of Self Sustainability of Elders. Group members are able to re-join their families and Communities because of increased Financial Sustainability and Dignity of life
Psychiatric Intensive Care Unit (PsylCU): There should be provision for Psychiatric Intensive Care Unit (PsylCU), and rooms for terminally ill patients who are bedridden. These patients are not supposed to spend their 24 hours in the bed waiting for their last breath, and should engage in recreational activities, as feasible.
Rehabilitative measures at societal level:
At the societal level, special provisions should be made for accommodation, mobility, transportation, recreation and financial assistance for elderly.
Special provisions for accommodation: Senior citizens should have access to accommodation, on individual or on group basis.
Special provisions to enhance mobility and for transport: To facilitate the mobility and journey of senior citizens special amenities should be made available on the road, on the station, at other public places. Some seats may be reserved in the buses and trains for elderly individuals; there may be separate queues at the ticket windows and elevators & escalators at the shopping centers and movie theatres.
Financial assistance: Financial assistance in various forms such as pension, tax-rebate, soft loans, special interest rates and investment plans may be provided to improve the quality of life of our needy elderly individuals. Section 80DDB of the income tax act allows a medical expense deduction of up to Rs. 40,000 from the taxable income of patients with dementia. The maximum deduction permissible is Rs. 60,000 in the case of patients aged 65 years and above. If the patient is not an income tax payee but is the dependent of a caregiver who is income tax payee, the caregiver can claim the deduction. To be eligible for the deduction, the level of disability resultant from the dementia should be at least 40%.
Special provisions for recreational activities: Dedicated recreational places like “senior citizen parks” are coming up in some of the cities in India.
Special issues in rehabilitation:
Marriage, divorce and live in relationship: Even senior citizens have right to get married if they are single or have lost their spouse. They have a right to ask for divorce if they are unable to happily stay together; and they also have a right to enter into a live-in relationship. As the needs of the elderly population increases, one may have to have marriage bureaus for them and special counseling centers and courts to deal with divorce applications filed by them.
Foster families: The concept of foster family may work both the ways for senior citizens. They may either adopt a needy young individual or a couple and provide them accommodation, food and financial assistance in lieu of physical and nursing care provided by them or the young and working couple may adopt the elderly individuals or a couple and provide them accommodation, food and financial help in lieu of housekeeping and childcare provided to their children by the elderly individuals.
Legal will and advanced directives: Making will or giving advance directives about artificial sustenance of life or carrying out certain religious ceremonies after their death are some of the issues which get importance at this stage of life. Discussion at an individual level or in group may be very helpful for the clarity on these issues.
Security: The elderly are prone for robbery, theft, manhandling and at risk of life by antisocial elements. Thus, this issue should be focused and addressed.
11. Rehabilitation in geriatric mental illness:
Principles of rehabilitation in an elderly in presence of mental illness remain essentially the same, as for a healthy elderly. Thus far we have discussed rehabilitation needs of healthy elderly. This part of guideline will discuss specific requirements for rehabilitating an elderly with mental illness.
— Purpose: Restore and maintain the highest level of psychological, physical and social function despite the disabling effects of illness.
— Goal: The goal of management is to improve the quality of life for patients and caregivers, maintain optimal function and provide maximal comfort.
Disabilities associated with geriatric mental illness are:
Primary disability: Cognitive, emotional, motivational, behavioral
Secondary disability: Loss of self confidence, social withdrawal, loss of social role and negativism
Tertiary disability: Homelessness, poverty, social stigmata
Therapeutic (curative) and prosthetic (supportive and rehabilitative) approach should go hand in hand.
Principles of rehabilitation in geriatric mental illness:
— Focus on treatment at home, or close to home
— Ensure comprehensive assessment
— Encourage normal function
— Treat the treatable
— Analyze disabilities and chart progress
— Clarify team goal with patient, caregiver and support workers early
— Teach what can be relevant
— Adapt the adaptable
— Coordinate support and follow up
— Promote flexibility, ingenuity with realistic optimism
Approach for rehabilitation in this sub group should be multi-disciplinary, with need to liaise with primary care team, specialist psychiatric team, social workers and local authorities. The medical, social, financial and spiritual support system needs to be even more robust when dealing with elderly with mental illness.
— Indications of rehabilitation in geriatric mental illness:
Individuals having mild cognitive impairment.
Individuals having mild, moderate or severe dementia.
Individuals having neurological deficits.
Individuals having BPSD (Behavioral and Psychological Symptoms of dementia).
Individual with impaired Activities of daily living (ADL).
Rehabilitation needs in special conditions (Special focus on dementia):
Most elderly requiring geriatric mental health rehabilitation residing either in home, community or in a hospital set up suffer from cognitive complaints.
In adult population, rehabilitation in psychiatry is synonymous with long term Schizophrenia care. However, in old age, mental health problems other than dementia, like psychosis of late life, depression, bipolar affective disorders, situational disorders have good response to pharmacological and non-pharmacological treatments. Thus need of rehabilitation in these ailments is very rare.
Hence here we will be discussing about rehabilitation in cases with neuro-cognitive complaints. It can be further categorized in three groups as depicted in Figure 9.
Fig. 9.
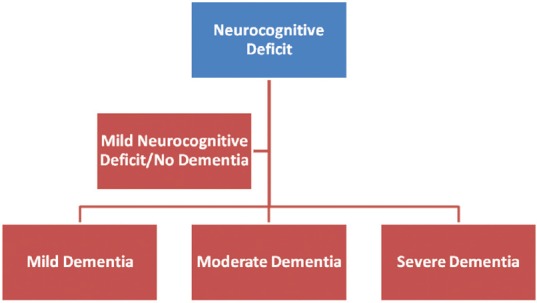
Neuro-cognitive Deficit Disorder
a) Mild Neuro-Cognitive disorder/cognitive impairment (No dementia):
This group is vulnerable for future cognitive decline (conversion rate of 5-20%), so there is need to address this group for primary prevention. Psycho-education about the services available, risk of disease progression and need of structured pharmacological and non pharmacological interventions is essential. Advice about advanced directives should be given when and where required.
Non-definitive treatment:
• Cognitive interventions
There is fair evidence that physicians and therapists should promote engagement in cognitive activity as part of an overall “healthy lifestyle” formulation for elderly individuals with and without memory loss.
• Physical exercise
There is fair evidence that physicians and therapists should promote physical activity, at an intensity level that is adapted to the person's overall physical capacities, as part of a “healthy lifestyle” for older individuals with and without memory loss.
Treatment ofvascular risk factors: As vascular risk factors and co-morbidities impact on the development and expression of dementia, they should be screened for and treated optimally in patients with mild cognitive impairment.
Treating hypertension: There is good evidence to treat systolic hypertension (> 160 mm Hg) in all older individuals. In addition to reducing the risk of stroke, the incidence of dementia may be reduced. The target systolic blood pressure should be 140 mm Hg or less There is some evidence that treating hypertension may prevent further cognitive decline associated with cerebrovascular disease. There is no compelling evidence that one class of agent is superior to another; calcium-channel blockers or angiotensin converting- enzyme (ACE) inhibitors may be considered.
Antiplatelet therapy with acetylsalicylic acid: There is currently no evidence to support the use of acetylsalicylic acid to specifically treat dementia associated with cerebrovascular disease. Acetylsalicylic acid or other antiplatelet therapies should be used for the prevention of recurrent ischemic stroke in appropriate patients.
Definitive treatment:
There is currently insufficient evidence to recommend the use of Cholinesterase inhibitors in mild cognitive impairment.
There is currently fair evidence to recommend against the use of Nonsteroidal anti-inflammatory drugs in mild cognitive impairment.
There is currently fair evidence to recommend against the use of Estrogen replacement therapy in mild cognitive impairment.
There is currently fair evidence to recommend against the use of Ginkgo biloba or Vitamin E in mild cognitive impairment.
b) Mild to Moderate Dementia-
Recommended actions to assist patients with mild to moderate dementia:
— Inform patient and family of the diagnosis
— Identify the caregiver and his/her needs
— Referrals, as needed
— Assess for safety risks
— Determine presence of any advanced planning document
— Assess patient's decision making capacity
— Inform about pharmacological and non-pharmacological treatment options, and research studies available
— Develop and implement a treatment plan with defined goals
— Assess and manage behavioural and psychological symptoms of dementia
— Monitor response to therapy
— Monitor and manage functional problems
— Monitor nutritional status
— Provide ongoing medical care
— Mobilize community based and facility based resources, as needed
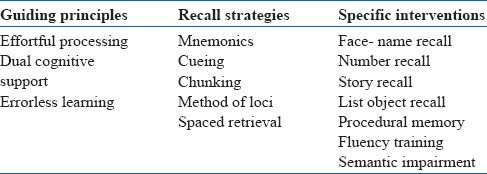
Table 5: Strategies and techniques for cognitive rehabilitation:
Table 5.
Rehabilitative interventions and strategies for mild-moderate Dementia
c) Severe Dementia-
General approach to the management of patients with severe dementia
— Patients should be monitored closely by health professionals
— Monitoring should involve assessment of the patient's cognition, function, behavior, and medical and nutritional status, as well as the caregiver's safety and health
— The goals of management are to improve the quality of life for patients and caregivers, maintain optimal function and provide maximum comfort
Medical management includes treating intercurrent medical conditions (e.g., infections, Parkinsonian symptoms, seizures or pressure ulcers), ameliorating pain, improving nutritional status and optimizing sensory function.
Patients should be monitored closely by mental health professionals. Monitoring should involve assessment of the patient's cognition, function, behavior, medical and nutritional status. Also assess caregiver's safety and physical and mental health.
Specific intervention for severe dementia involves principally motivation based techniques
Stimulation of island of preserved cognition, decompose complex task in simple task
Presentation of increasing complex task
Potentiating of brain plasticity
Induce use of implicit way of functioning
Implicit orientation, improved functioning and well being
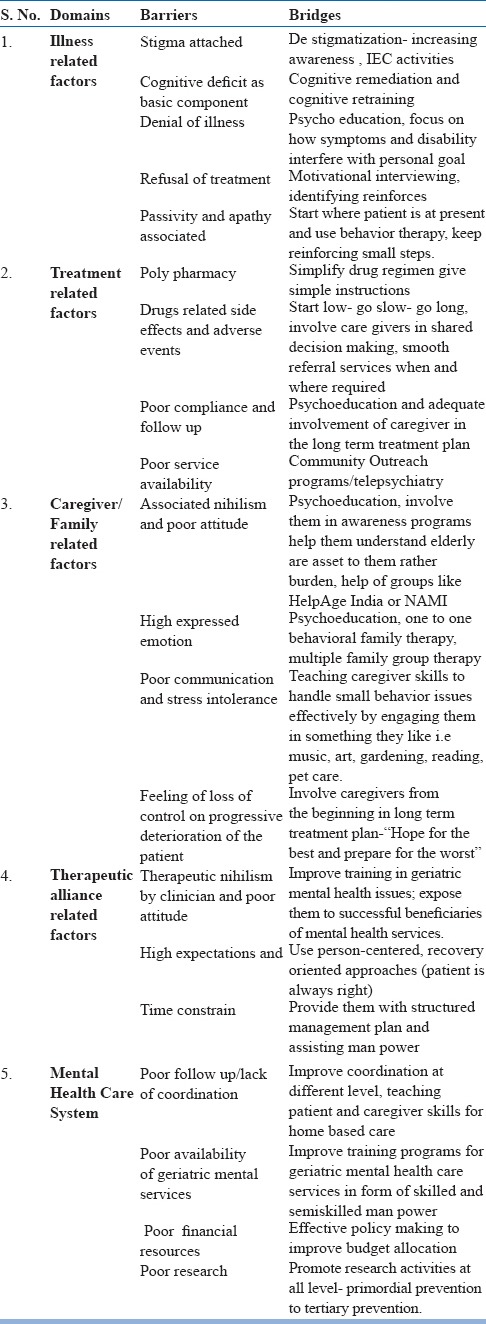
12. Barriers in rehabilitation:
Following are barriers in instituting a rehabilitation strategy effectively:
Lack of strategic planning
Lack of resources and health infrastructure
Lack of agency responsible to administer, coordinate, and monitor services
Inadequate health information systems and communication strategies
Complex referral systems limiting access
Lack of engagement with people with disabilities
Bridging the barriers:
These barriers to rehabilitation can be overcome through a series of actions. These include:
Reforming policies, laws, and delivery systems
Developing funding mechanisms: financing rehabilitation
Increasing human resources for rehabilitation
Expanding and decentralizing service delivery
Increasing the use and affordability of technology and assistive devices
Expanding research programs (Table-6: Barrier's in Rehabilitation and Bridges to them)
Table 6.
Barrier's in Rehabilitation and Bridges to them
13. Summary:
The basic objective of rehabilitation is to restore the physical, social and psychological potential to a level, so that an individual can independently function and carry on an independent life. Rehabilitation should be aimed at primordial level (promotion of healthy ageing), primary level (universal, selective and indicative), secondary (early diagnosis and management) and tertiary- preventing disability and return to normalcy, to achieve maximum level of restoration through different interventions. These may involve training in vocational methods to suit working with residual disability. To summaries:
Ageing is inevitable and inescapable. Foresight and planning can lead to healthy ageing.
Rehabilitation should be initiated early, in health and in illness.
It is a long, dynamic and active process.
Multidisciplinary approach is the appropriate way of rehabilitation.
Instituting measures of rehabilitation are important for better prognosis and life quality.
Intervention is required for all conditions; however it should be tailored to fit each individual.
Ultimate goal should be to provide dignified life to elderly.
Need to change attitude of people towards mental illness.
Health staff needs to be trained and sensitized to needs of elderly in health or in mental illness.
Need to conduct outreach health programs to detect early those individuals in need of rehabilitation.
Data to support these recommendations is scarce. Need medical research for evidence based practice.
“Crutches should not be made of woods but of carer's/therapist's tolerance or patience”
APPENDIX
Important assessment scale in planning Rehabilitation are-
Katz Index of Activities of Daily Living Scale/EASI
Lawton Instrumental Activities of Daily Living Scale
Diagnostic evaluation for functional impairment
Screening tests to identify impairments and factors contributing to disability
Physiotherapy cum exercise regimen for average elderly is attached (Table-7).
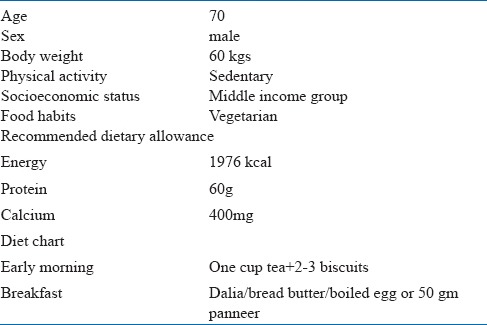
Diet schedule for normal average elderly (Table-8).
Table 7.
General physiotherapy instructions for average Indian elderly
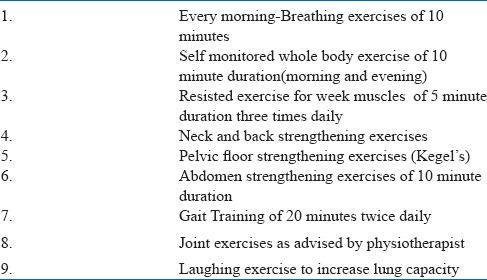
Table 8.
Standard Dietary regimen for ref. Indian Elderly(Male)
RESOURCES
A) List of journals related to geriatric mental heaLefth care
Clinical Geriatrics
Clinical Gerontologist
Geriatrics
Geriatrics & Aging Online
Gerontology
Gerontology and Geriatrics
Journal of Aging and Health
Journal of Applied Gerontology
Journal of Gerontology
Journal of Mental Health and Aging
Psychology and Aging
The Gerontologist
B) List of Evidence-based geriatric care books
-
1)
Drug Prescribing for Older Adults: An Evidence Based Approach. Rosanne M. Leipzig, ed., American College of Physicians, 2001.
-
2)
Evidence Based Dementia Practice. Nawab Qizilbash et al., ed. Blackwell Science Inc, 2001.
-
3)
Evidence-Based Rehabilitation: A Guide to Practice. Mary C. Law, ed. Slack, Inc., 2002.
-
4)
Geriatric medicine: An evidence-based approach. Christine K. Cassel, ed. 4th ed. New York:Springer, 2003.
-
5)
Handbook of Pain Relief in Older Adults: An Evidence-Based Approach. F. Michael Gloth Ed. Humana Press, 2004.
-
6)
Practicing Evidence-based Geriatrics. Sharon Straus, David Sackett BMJ Publishing Group, 1999.
C) List of the groups, associations, institutes & research centers working in the field of geriatric mental health
-
1)
Indian Association of Geriatric Mental Health
-
2)
Aging Clinical Research Center, Stanford University School of Medicine
-
3)
Alzheimers.com
-
4)
Alzheimer Europe
-
5)
Alzheimer's Disease International
-
6)
Alzheimer Italia
-
7)
Alzheimer Society of Alberta
-
8)
Alzheimer Society, Canada
-
9)
Alzheimer Society of Ottawa-Carleton
-
10)
Alzheimer Society Romania
-
11)
Alzheimer's Association Australia
-
12)
Alzheimer's Association of Australia
-
13)
Alzheimer's Association of South Australia
-
14)
Alzheimer's Association of Tasmania
-
15)
Alzheimer's Association Victoria, Australia
-
16)
Alzheimer's Association, New South Wales
-
17)
Alzheimer's Association, U.S.
-
18)
Alzheimer's Disease Society, UK
-
19)
Alzheimer Disease Research Center (ADRC)
-
20)
Alzheimer's Center, Stanford/VA
-
21)
Alzheimer Page, Washington University, St. Louis
-
22)
Alzheimer Research Forum
-
23)
The Alzheimer Research Forum
-
24)
Alzheimer Web
-
25)
American Association for Geriatric Psychiatry
-
26)
American Society on Aging
-
27)
Association France Alzheimer
-
28)
Alzheimer's Disease Research at Mass. General Hospital
-
29)
InsVtute tor Brain Aging and Dementia, University of California, Irvine
-
30)
Institute of Gerontology, Wayne State University
-
31)
LewyNet, Nottingham Medical School
-
32)
Michigan Alzheimer's Disease Research Center
-
33)
National Institute on Aging, U.S.
-
34)
National Ageing Research Institute, U.S.
-
35)
University Alzheimer Center, Case Western Reserve University
D) LIST OF HOMES AND REHABILITATION CENTERS FOR SENIOR CITIZENS
1) Directory of Old Age Homes in India, Research and Development Division, Help-Age India, 2016
OLD AGE HOME DIRECTORY
Help Age India's Directory of senior citizen's guide (2016). Old Age Home directory provides
comprehensive information on 1012 old age homes in India. For copies of this directory, kindly sendRs.65/- as handling charges (By DD/MO only in favor of Help Age India, New Delhi. Cheques from Delhi are acceptable). If you need the contact details of homes in any city or state, the same would besent by post/e-mail free of cost. Address: Research & Strategic Development Department HelpAge
India C-14, Qutab Institutional Area, New Delhi 110016.
Tel. No.:+91-11-1688955-59, 26966641, Fax : 91-11-26852916
Email: helpage@nde.vsnl.net.in or email to: anupama@helpageindia.org
info@helpageindia.org Website: http://www.helpageindia.org
2) Website for the list of old age homes in different states http://www.seniorindian.com/index.htm
E) LIST OF THE VARIOUS ORGANIZATIONS WORKING FOR SENIOR CITIZENS
1) Website for the list of NGOs working in India http://www.ngosindia.com
F) SENIOR CITIZEN SECURITY CELL
For example: The senior citizen security cell of Delhi.
The Senior Citizen Security Cell was set up on June 22nd, 2004 under the orders of CP/Delhi.
Objectives: The main objective of the cell is to coordinate, monitor and advise the area police regardinq the security and safety of the Senior Citizens.
Location: It is located on 1*’ Floor, Police Headquarters, M.S.O. Building, I. P. Estate, New r
Supervision: It is working under the supervision of Additional Commissioner of Police Crime, Lie
Telephone Nos.: Direct: 23490233 (Tele-Fax) PHQ Exchange: 23490010/4336
REFERENCES
- 1.APA online. Public Policy office. (July 2003) Respite care significantly benefits caregivers and recipients of care. http://www.apa.org/ppo/issues/respitefact03. html. [Google Scholar]
- 2.Beers M, Jones TV, et al. The Merck Manual of Geriatrics. 3rd ed. 2000. Retrieved on 6* September2006 from world wide web http://www.merck.com/mrkshared/mmg/sec3/ch28/ch28a.jsp .
- 3.Borgenicht K, Carty E, Feigenbaum L Z. Community resources for frail older patients. Care Management Journal. 2005;6(2):80. [PMC free article] [PubMed] [Google Scholar]
- 3.Cahn - Weiner DA, Malloy PF, et al. Results of a Randomized Placebo-Controlled Study of Memory Training for Mildly Impaired Alzheimer's Disease Patients. Applied Neuropsychohgy. 2003\1;0(4):215–23. doi: 10.1207/s15324826an1004_3. [DOI] [PubMed] [Google Scholar]
- 4.Clare L. Rehabilitation for people with dementia. December, 17, 2001 In Neuropsychological Rehabilitation: theory and practice. In: Wilson BA, editor. In Press:Swets & Zeitlinger; Available at Http://Members.Aol.Com/Morrisff/Clare.Html . [Google Scholar]
- 5.Clyburn LD, Stones MJ, Hadjistavropoulos T, et al. Predicting Caregiver Burden and Depression in Alzheimer's Disease. Gerontol B Psychol Sci Soc Sci. 2000 Jan;55(1) doi: 10.1093/geronb/55.1.s2. S2-13(283) [DOI] [PubMed] [Google Scholar]
- 6.Dean M. A law that would care for the carers. Lancet. 1995;345(8957):1101. doi: 10.1016/s0140-6736(95)90827-7. Department of Health and Human Services, elder care locator (07/06/2005). Retrieved on 6thSeptember 2006 http://www.eldercare.gov/eldercare/Public/resources/fact_sheets/respite care.asp . [DOI] [PubMed] [Google Scholar]
- 7.Donaldson C, Burns A. Burden of Alzheimer's Disease: Helping the Patient and Caregiver. Geriatric Psychiatry and Neurology. 1999;12(1):21–8. doi: 10.1177/089198879901200106. [DOI] [PubMed] [Google Scholar]
- 8.Doolittle M, Bray J, Rosenbaum EH. Relaxation, Self-Care and Activities of Daily Living. 1999. May 1, Available at http//www.cancersupportivecare.com/selfcare.html . Retrieved September 6th 2006 Encyclopedia of Mental Disorders: Cognitive retraining, 2006. Available at http://www.minddisorders.com/Br-Del/Cognitive-retraining.html .
- 9.Fillenbaum G. Activities of Daily Living. In: Maddox GL, editor. The Encyclopedia of Aging. New York: Springer; 1987. pp. 3–4. [Google Scholar]
- 10.Gelder M, Mayou R, Cowen P, editors. In Shorter Oxford textbook of Psychiatry. 4m ed. Oxford: Oxford university press; 2001. Psychiatry of the elderly. [Google Scholar]
- 11.Gormley N. The role of dementia training programs in reducing care giver burden. Psychiatric bulletin. 2000;24:41–42. [Google Scholar]
- 12.Gravis - Graham Vikas Vigyan Samiti. 2004. retrieved September, 5, 2006 from the world wide web http://www.gravis.org. in’elderly.htm .
- 13.Hinchliffe AC, Hyman I L, Blizard B, et al. Behavioral complications of dementia - can they be treated? International Journal of Geriatric Psychiatry. 1995;10:839–847. [Google Scholar]
- 14.Hutchinson SG, Tarrant J, Severs MR. An inpatient bed for acute nursing home admissions. AgeAgeing. 1998 Mar;27(2):95–8. doi: 10.1093/ageing/27.2.95. [DOI] [PubMed] [Google Scholar]
- 15.Kasuya RT, Polgar-Bailey P, Takeuchi R. Caregiver burden and burnout: a guide for primary carephysicians. Postgraduate Medicine. 2000;108(7):119–23. doi: 10.3810/pgm.2000.12.1324. [DOI] [PubMed] [Google Scholar]
- 16.Kennell D, Alecxih L, Erickson P, et al. The Estimated Costs of a Proposed Home Care Program: final report to the Commonwealth Fund Commission on Elderly People Living Alone. 1989 May 22; [Google Scholar]
- 17.Kramer AF. 2006. Fitness Training and the Brain: From Molecules to Minds: Session 2028 - Invited Symposium: Optimal Aging and Cognition - Moderators of Cognitive Change and Decline at APA. [Google Scholar]
- 18.Larkin M. Reality Orientation. 1994. Available at: http://www.zarcrom.com/users/alzheimers/t-02. html . Retrieved 6th September, 2006.
- 19a.National Institute of Social Defense, Ministry of Social Justice and Empowerment, Govt Of India(2005, March, 17) retrieved September, 5, 2006 from the world wide web http://nice.nisd.gov.in/publications.php .
- 19b.Proctor R, Burns A, Powell HS, et al. Behavioral management in nursing and residential homes: arandomized controlled trial. Lancet. 1999;3(354(9172)):26–9. doi: 10.1016/S0140-6736(98)08237-3. http://www.censusindia.gov.in/2011-Common/CensusData201120 . [DOI] [PubMed] [Google Scholar]
- 21.Rao VA. Family jointness, family and social integration among the elderly. Indian Journal of SocialPsychiatry. 1987;3:81. [Google Scholar]
- 22.Rivlin, Alice M, Joshua M W, et al. Caring for the Disabled Elderly: Who Will Pay? Washington, DC: The Brookings Institution; 1988. [Google Scholar]
- 23.Sawhney M. The Non Governmental Organization's Commitment to the Elderly in India. In: Liebig PS, Rajan SI, editors. An Aging India : Perspectives, Prospects, and Policies. New Delhi: Rawat; 2005. [Google Scholar]
- 24.Shah B. Tradition and the future in India. 2006. Retrieved on 6tt5 September. http://www.islamset.com/healnews/aged/Bela_Shah.html .
- 25.Shapiro A, Taylor M. Effects of a Community-Based Early Intervention Program on the SubjectiveWeil-Being, Institutionalization, and Mortality of Low-Income Elders. The Gerontologist. 2002;42:334–341. doi: 10.1093/geront/42.3.334. [DOI] [PubMed] [Google Scholar]
- 26.Teri L, Logsdon RG, Uomoto, et al. Behavioral treatment of depression in dementia patients: a controlledclinical trial. Journal of Gerontology. 1997;52B:159–166. doi: 10.1093/geronb/52b.4.p159. [DOI] [PubMed] [Google Scholar]
- 27.Reardon M, Holmon R, Dewhurst G. Diagnosis and Management of Dementia: A Manual for Memory Disorder Teams. A survey of domiciliary consultations in medicine for the elderly. In: Wilcock G K, Bucks R S, Rockwood K, editors; Public Health 1995. 3. Vol. 109. Oxford: Oxford University Press; 1999. pp. 187–90. [DOI] [PubMed] [Google Scholar]
- 28. http://www.who.int/mental_health/en .


