Abstract
Endoscopic retrograde cholangiopancreatography (ERCP) is an important treatment for inoperable hilar cholangiocarcinoma (HCC). The aim of the present study as to evaluate the clinical value of three-dimensional visualization (3DV) and 3D printing (3DP) technologies for ERCP in patients with HCC. The clinical data of 15 patients with HCC admitted for ERCP were analyzed retrospectively, including 9 males and 6 females. Thin-sliced data of computed tomography and magnetic resonance cholangiopancreatography (MRCP) were acquired and imported into Mimics Innovation Suite v17.0 software for 3D reconstruction. Standard Template Library files were exported for 3D printing. The target bile duct and Bismuth-Corlette (BC) classification were selected and performed respectively with the aid of Mimics Innovation Suite v17.0 software. The results were compared with the selected ones in ERCP. 3DV and 3DP models were successfully constructed for all patients, which presented the tumor, bile duct and the spatial relationship between them from multiple perspectives. The ERCP of all patients in the present study were performed successfully. The target bile duct screened by them had a high concordance rate of 86.7% with that in ERCP. The diagnostic accuracy of BC type results by 3DV and 3DP models was 93.3%. 3DV and 3DP technologies can accurately show the tumor and its associations with the surrounding bile duct, and it can be used to guide ERCP in HCC patients and improve the success rate of the operation.
Keywords: three-dimensional visualization, three-dimensional printing, endoscopic retrograde cholangiopancreatography, hilar cholangiocarcinoma
Introduction
Cholangiocarcinoma is a malignant neoplasm that originates from the epithelium of the biliary tree (1). Hilar cholangiocarcinoma (HCC) is the most common type of cholangiocarcinoma, accounting for about 50–60% (2,3). HCC arises from the right and left hepatic ducts, the confluence of the right and left hepatic bile ducts, and above cystic duct openings. At present, surgical resection is still the only effective way to cure HCC (4). However, because of its location, prone to local einvasion, adjacent structure infiltration and metastatisation, surgical operation is very difficult and quite often not radical. In addition, presenting with insidious onset and lacking specific symptoms, most patients are diagnosed in advanced stage and lost the opportunity of surgical treatment. Consequently, the radical (R0) resection rate is only 10–20% (5). The survival rates of five years after complete surgery range from 11 to 41% (6). So as a safe and effective palliative therapy, the biliary stent placed by endoscopic retrograde cholangiopancreatography (ERCP) may be the best choice for patients with unresectable HCC (7). However, violated by the tumor, the left and right hepatic bile ducts are not communicating with each other, which leads to the difficulty of superselective catheterization and the failure of ERCP. Correct and reasonable selection of the target bile duct is the key to superselective catheterization of bile duct successfully. At present, the choice of target bile duct is mainly based on preoperative CT, magnetic resonance cholangiopancreatography (MRCP) and intraoperative cholangiography. But for complex HCC, it is difficult to determine the target bile duct. So the ERCP is still full of challenge.
Since the early 2000s, three-dimensional printing (3DP) technologies have begun to be applied in medical domain (8). In recent years, the application of 3DP technologies is more and more extensive, such as personalized surgical planning and guidance, medical research and premedical education (8–11). Compared with CT, magnetic resonance imaging (MRI) and other two-dimensional images, three-dimensional visualization (3DV) and 3DP models are more intuitive and more accurate in displaying anatomical and spatial structure of the organs and have made great achievements. Their application value on surgical treatment of HCC has been affirmed (12,13). But the application of 3DV and 3DP technologies on ERCP is still in the early stage and less reported in the literature.
The objective of this study was to assess the role of ERCP for HCC based on 3DV and 3DP technologies at a center in China.
Materials and methods
Patients
The present study was in accordance with the ethical standards of the responsible committee on human experimentation (institutional or regional) and with the Helsinki Declaration of 1975, as revised in 2000. The Institutional Ethics Committee of our hospital approved this study, and written informed consent was obtained from each participant before the study. 15 patients with HCC who underwent ERCP were enrolled from January 2015 to January 2017, including 9 males and 6 females. CT and MRCP examination were acquired and 3DV models were constructed. The real three-dimensional models of the tumor and surrounding bile ducts were created by the 3DP technologies. Before the operation, all patients were informed of the indication and details of ERCP and the risks and complications of the operation.
Instruments
CT: The data of 1 mm slice thickness were acquired from the 64-MDCT provided by American GE Company. MRCP: The 1.5 T Signa HDxt provided by GE Healthcare Bio-Sciences (Pittsburgh, PA, USA) was utilized to obtain the 1.8 mm slice thickness.
3DV and 3DP technologies
Data of CT and MRCP were imported into 3D visualization workstation that called Mimics Innovation Suite v17.0 software in DICOM format, where 3DV models of liver tumor and bile ducts were reconstructed. The reconstructed models were exported as Standard Template Library files. The topological correction, decimation, Laplacian smoothing, and local smoothing were needed to create a 3D model for 3DP. ProJet® 4500 3D printer (3D Systems Corp., Circle Rock Hill, SC, USA) was used to manufacture the models and the printing material was Visijet C4 Spectrum Core. Bismuth-Corlette (BC) type was performed and diameter of the dilated bile ducts was calculated. The bile duct with the largest diameter and the widest drainage area was selected as the target bile duct and compared with the actually selected ones in ERCP.
ERCP
Now it is still controversial whether unilateral or bilateral drainage is better in the treatment of HCC. Unilateral stenting appears to be adequate for relieving jaundice in most unresectable cases. And it is technically easier and less expensive than bilateral stenting, with reintervention for stent dysfunction also being considerably easier (14). At the same time, in consideration of the tolerance of surgery and postoperative complications, so unilateral stenting was performed for all patients in our study. At first, the drainage area and target bile duct were selected preliminarily on the basis of preoperative abdominal CT, MRCP image and intraoperative cholangiography. The bile duct was selectively cannulated using a guide wire. If encountered difficulties, the sphincterotomy was performed. The bile was extracted by a syringe after successful selective intrahepatic bile duct cannulation as much as possible to lower the pressure of the bile duct. The dilating bougie was used to dilate the stenosis along the guide wire. According to the patients' medical history, BC type, patients and their families' wishes, the biliary stents were chosen rationally. Finally, the metal or plastic stent was placed successfully and nasobiliary duct was inserted and fixed smoothly.
Results
3DV models were successfully manufactured for all patients that clearly displayed all the relevant structures, including intrahepatic bile ducts; size, shape, location of the tumor; anatomical structure between them; location and degree of the biliary stricture. Moreover, 3DV models could be amplified, rotated, and hyalinized to clarify the anatomic character of these structures with omnidirectional, multiple-angle, and multilevel views. The models can localize correctly the tumor and surrounding bile ducts, identify the extent of biliary stenosis and cholangiectasis, contribute to determining the target bile duct and make target bile duct be selected intuitively, concretely and objectively. The location and direction of target bile duct can be used to direct selective intrahepatic bile duct cannulation in ERCP. Furthermore, 3DV models can avoid the influence of subjective factors such as the operator's own experience, the level of imaging ability to ERCP, and the success rate is higher. Demographics and research variables are shown in the Table I. The target bile duct screened by the models had a high concordance rate of 86.7% with that in ERCP. The results were different in two patients. The target bile duct identified by 3DV and 3DP models was the right posterior lobe bile duct. However, selective cannulation of the right posterior lobe bile duct failed, we had to try the left lateral lobe bile duct and succeed. The diagnostic accuracy of BC type results by 3DV and 3DP models was 93.3%.
Table I.
Demographics and research variables.
| Variable | No. of patients (n=15) |
|---|---|
| Female/Male | 6/9 |
| Age, years | 65.4±14.9 |
| BC type (II/IIIA/IIIB/IV) | |
| Model | 2/4/4/5 |
| ERCP | 2/5/4/4 |
| Concordance rate | 14/15 (93.3%) |
| Target bile duct | |
| Model | R, R, L, L, R, R, L, R, R, R, L, R, R, L, L |
| ERCP | R, R, L, L, L, R, L, R, R, L, L, R, R, L, L |
| Concordance rate | 13/15 (86.7%) |
R, right posterior lobe bile duct; L, left lateral lobe bile duct; ERCP, endoscopic retrograde cholangiopancreatography; BC, Bismuth-Corlette.
ERCP was performed successfully for all patients. After ERCP, the malignant obstructive jaundice symptoms of 13 patients were alleviated or disappeared. Preoperative and postoperative laboratory features including white blood cell (WBC), neutrophil ratio (Neu%), alanine transaminase (ALT), aspartate transaminase (AST), total bilirubin (TBIL) and direct bilirubin (DBIL), are shown in Table II. The TBIL level of 2 cases did not decrease, or even increased. BC type for the two patients was both Type IV and the cancer metastasize to the liver and portal vein. Besides, cholangitis was induced by ERCP. So their prognosis was poor, just like the findings of Vienne and his colleagues. They thought complete resolution of jaundice might not occur for patients with Bismuth IV after ERCP because it was now thought that at least 50% of normal liver needs to be drained to achieve complete resolution of jaundice (15). The change of TBIL for all patients before and 3 days after operation was listed in Fig. 1. Cholangitis, postoperative pancreatitis and hyperamylasemia occurred in 2,1 and 4 cases respectively. And the patients were discharged in 6–20 days. All patients were followed up for three months to one year and three cases were died.
Table II.
Preoperative and postoperative laboratory features.
| Variable | Preoperative | Postoperative day 1 | Postoperative day 3 |
|---|---|---|---|
| WBC | 5.8±2.0 | 9.8±2.0 | 7.1±2.8 |
| Neu% | 71.0±11.6 | 82.5±10.7 | 77.6±9.6 |
| ALT | 156.1±148.3 | 92.6±89.1 | 81.3 ±91.2 |
| AST | 135.3±96.5 | 95.3±51.1 | 78.6±82.5 |
| TBIL | 237.5±97.6 | 226.6±102.8 | 186.2±112.7 |
| DBIL | 196.6±82.0 | 194.1±88.8 | 158.0±104.6 |
WBC, white blood cell; Neu, neutrophil ratio; ALT, alanine transaminase; AST, aspartate transaminase; TBIL, total bilirubin; DBIL, direct bilirubin.
Figure 1.
Change in TBIL for all patients prior to and 3 days following their operation. TBIL, total bilirubin.
The specific diagnosis and treatment process of a typical case were reported as follows: A 75-year-old male was admitted for yellow skin and mucosa for one week. And he had a medical history of hepatitis B cirrhosis. CT scan and MRCP showed a mass in hepatic portal and dilatation of intrahepatic bile ducts, and the BC type was type II (Fig. 2); The 3DV and 3DP model were constructed successfully and the BC type was type II (Fig. 3). However, in this model of the patient, because of severe dilatation, most of the left bile ducts fused together. But some bile ducts can still be distinguished. The diameters of the dilated bile ducts were calculated by Mimics Innovation Suite v17.0 software (Materialise, Leuven, Belgium),. The method was averaging the testing values of repeated measurements. The left and right hepatic bile ducts were marked with different colors and corresponding sequence numbers (Fig. 4A). The diameters of hepatic bile ducts were as follows (Table III).
Figure 2.
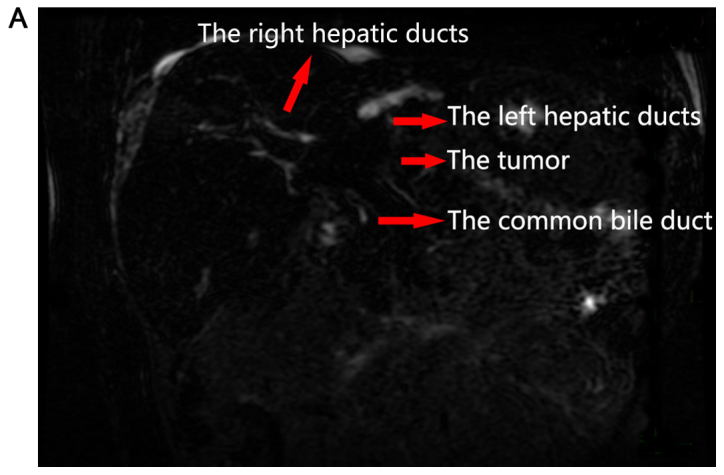
MRCP image of hilar cholangiocarcinoma (male patient, aged 75): Hepatic hilar mass and intrahepatic bile duct dilatation. (A) Two-dimensional image of MRCP. (B) The image of MRCP three-dimensional reconstruction. MRCP, magnetic resonance cholangiopancreatography.
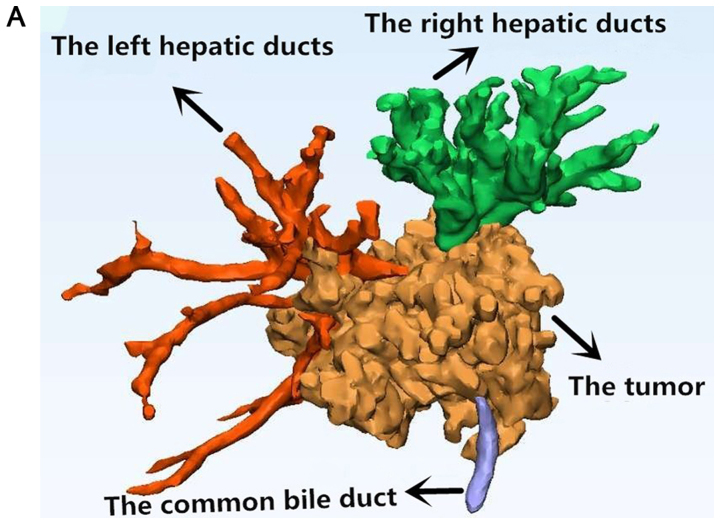
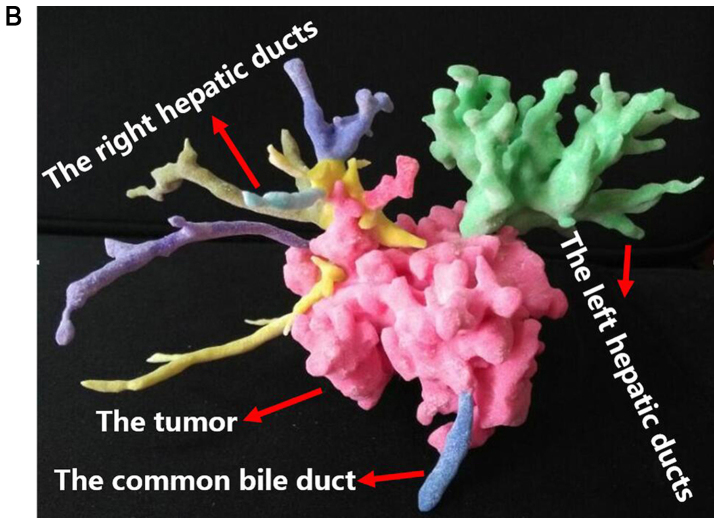
Figure 3.
3DV and 3DP models. (A) The 3DV model generated by MIMICS v17.0 software of the hepatic bile duct system and the mass, including the tumor, the dilated bile duct and the 3D anatomical association between them. (B) The 3DP model presented the tumor and the entire bile duct tree. 3DV, three-dimensional visualization; 3DP, three-dimensional printing.
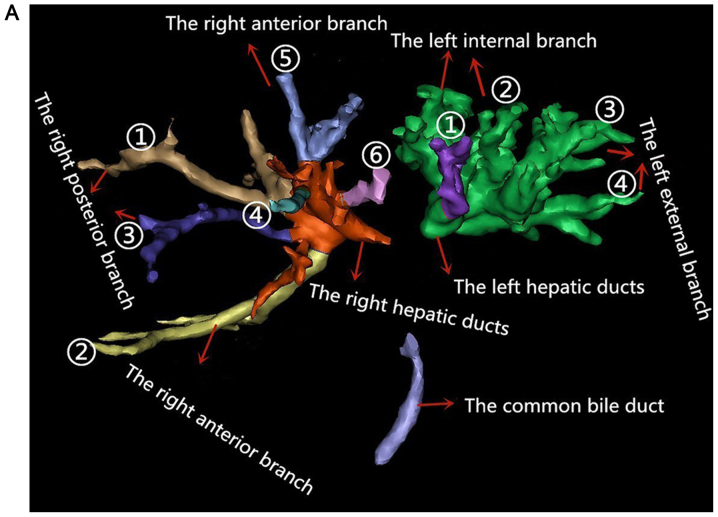
Figure 4.
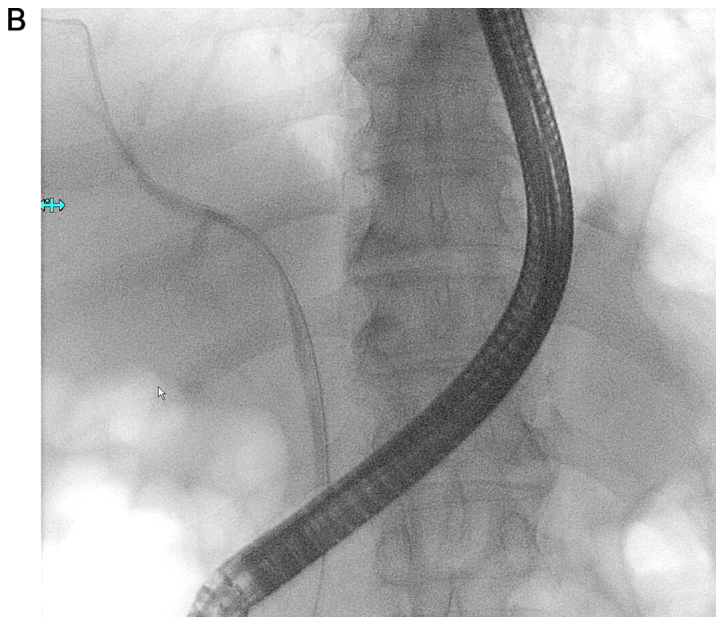
Bile ducts in 3DV model and the image of ERCP. (A) The liver bile duct system without the tumor and the bile ducts identified by different colors. In the right bile ducts, 1 and 3 belong to the right posterior branch, and 2 and 4–6 belong to the right anterior branch. In the left bile ducts, 1 and 2 belong to the left internal branch, and 3–5 belong to the left external branch. (B) The guide wire was inserted into the right hepatic duct in ERCP operation. 3DV, three-dimensional visualization; ERCP, endoscopic retrograde cholangiopancreatography.
Table III.
Diameter of bile ducts with different colors and the corresponding sequence numbers.
| A, Right hepatic duct system | ||
|---|---|---|
| No. | Color | Diameter of bile duct (mm) |
| 1 | Brown | 7.28 (8.45+5.95+6.74+7.97/4) |
| 2 | Yellow | 5.68 (6.09+5.49+5.44+5.69/4) |
| 3 | Blue | 3.77 (4.06+3.30+4.40+3.37/4) |
| 4 | Light blue | 3.72 (3.00+4.49+3.74+3.65/4) |
| 5 | Lilac | 6.77 (7.56+6.31+7.01+6.19/4) |
| 6 | Pink | 4.78 (4.93+4.47+4.50+5.24/4) |
| B, Left hepatic duct system | ||
| No. | Color | Diameter of bile duct (mm) |
| 1 | Purple | 7.01 (7.74+5.91+8.12+6.27/4) |
| 2 | Green | 9.12 (8.59+9.54+10.2+8.1/4) |
| 3 | Green | 13.57 (15.54+12.61+13.52+16.4/4) |
| 4 | Green | 12.00 (12.78+11.52+10.8+12.72/4) |
The final right target bile duct was the right brown bile duct and the corresponding serial number was ①, namely, the right posterior branch bile duct. And the final left target bile duct was ①, namely the left lateral branch. In ERCP, the bile duct of the right lobe (Fig. 4B) was the actual selected bile duct. The double-wire guided technique was applied. Along the guide wire, the nasobiliary duct was placed to the right lobe of the liver. The 3DV model was consistent with intraoperative condition in ERCP, and the selected bile duct was the same. After operation, the patient's symptoms were significantly relieved without complications and he was discharged on postoperative day 14, without any complications.
Discussion
HCC is a malignant tumour with high mortality. BC type can accurately delineate the anatomic location of tumor and the degree of invasion and is the most widely used preoperative reference system for predicting resectability and defining surgical strategy. And it also contributes to choose reasonable drainage way in endoscopic therapy and evaluating therapeutic effect. Since proposed by Bismuth and Corlette in 1975 (16), the method is still widely used today. The majority of patients with advanced HCC are inappropriate for surgical resection because of the tumor location in the hepatic hilum and adjacent areas, advanced tumor stage, or comorbidities. Additionally, some people are aged, bad general condition and seem hardly to tolerate surgical operation. Therefore, these patients often have a poor prognosis in terms of survival and quality of life. So as a nonsurgical and palliative treatment, biliary stent placed by ERCP may be the best choice for these people to relieve malignant obstructive jaundice and improve hepatic function, raise living quality and prolong survival time. This kind of treatment corresponds to the normal physiological characteristics. And compared with surgery, it is less invasive and has fewer postoperative complications.
Since 3DV and 3DP technologies are applied to the clinical medicine, they have been widely used in oral and maxillofacial surgery and orthopedics (17–19). 3D visualization and printing can successfully show the anatomic relationship between tissue organs and surrounding structures. 3DV models could be amplified, rotated, and hyalinized to clarify the anatomic character of tissue and organ structure with omnidirectional, multiple-angle, and multilevel views. And 3DV models can also be employed to accurately calculate the size and volume of a liver tumor, the diameter and length of blood vessels and bile ducts and the residual liver volume. These functions are also of important clinical significance for preoperative planning and guiding the actual surgical operations. However, compared with 3DP models, there is a certain sense of spatial distance in 3DV models. 3DP models are constructed based on 3DV images and can foresee anatomic structure at surgery truly from multiple dimensions before operation. In addition, 3DP models can be brought into the operation room, provide real-time navigation intuitively for key steps in operation and identify and locate key parts quickly. At present, the research and application of these technologies have also made significant achievements in liver surgery, such as liver transplantation, laparoscopic liver resection, hepatectomy for hepatolithiasis, hepatic hydatid disease (20–27). There also are researches on surgical treatment of HCC. Zeng and colleagues (12) applied 3DV and 3DP technologies to the surgery of HCC and found they played an important role in the accurate preoperative diagnosis, the establishment of the operation plan, precise operation in surgery and improvement of the success rate of surgery. With the help of these technologies, Oshiro Y and Ohkohchi N performed successfully left hepatic lobectomy and extrahepatic bile duct resection for a HCC patient (28).
But for the clinical application of 3DV and 3DP techniques for ERCP in patients with HCC, there were no reports and literature of the relevant studies. In our study, we discover that 3DV and 3DP technologies play a significant role in the successful implementation of ERCP in patients with HCC. This article mainly carries on the elaboration from the following three aspects.
The role of 3DV and 3DP technologies in the selection of target bile duct: Correct and reasonable selection of the target bile duct are important to the successful selective intrahepatic bile duct cannulation in ERCP. There are two factors that determine the target bile duct: The dilatation of bile duct is distinct and the drainage range is extensive. In the present study, 15 patients had a high consistency rate of 86.7% on target bile duct selected by the 3DV models and ERCP respectively. Preoperative 3D reconstruction can clearly show the three-dimensional anatomy of the tumor, dilated bile duct and its anatomical relationship with the tumor (Fig. 3) (29,30). With the help of Mimics Innovation Suite v17.0 software (Materialise, Leuven, Belgium), the diameter of the proximal dilated bile ducts could be calculated directly and accurately, and the bile duct with the largest diameter and the most extensive drainage was selected as the target bile duct. The target bile duct is ordinarily selected based on CT, MRCP and intraoperative cholangiography and other two-dimensional images, which can not exhibit the spatial structure of the bile duct, causing the specific direction of the guide wire in superselective catheterization of bile duct is not completely clear, and even a blind insertion. So the success rate of operation is closely related to the operator's experience and the ability of interpreting the images. However, compared to 2D images, 3DV and 3DP models can show the biliary tree more intuitively, the width and direction of target bile duct more clearly, and can rotate by 360 degree and avoid the influence of subjective factors on ERCP.
The role of 3DV and 3DP technologies in guiding the selection and placement of a biliary stent: The location of drainage in patients with HCC can be selected as the left hepatic duct system, the right hepatic duct system or both. The key determinant is the site of the bile duct stricture. BC type is very important for the rational selection of the drainage site and the judgement of curative effect in endoscopic stent placement. Our study discovers that BC classification classified by the 3DV and 3DP models is more accurate, the 3DV and 3DP models can demonstrate the location of bile duct invaded by the tumor more accurately than CT and MRCP and can be used to guide the selection and placement of a biliary stent.
3DV and 3DP technologies can reduce the use of contrast media: Contrast agents are often needed to outline the stricture in ERCP. However, contrast media injection into intrahepatic ducts without adequate drainage easily leads to uncontrolled cholangitis and poor prognosis. The rate of cholangitis after ERCP was 1–5% (31–33). And what's worse, invaded by the tumor, intrahepatic biliary drainage is poor in HCC patients. To decrease the incidence of this complication, some studies have explored the usefulness of CT or MR cholangiography (MRC) prior to stenting (34,35). Once the bile duct tree is delineated by CT or MRC, selective guidewire cannulation and stenting of the targeted bile duct can be accomplished without contrast injection. Compared with CT/MRI, 3DV and 3DP models are more intuitive and more accurate (36). Consequently, they can reduce the use of contrast media. And we can speculate that 3DV and 3DP models can decrease the incidence of cholangitis. But further case control studies are needed to verify the hypothesis.
In conclusion, compared with 2D images, 3DV and 3DP models be amplified, rotated, and hyalinized to clarify the anatomic character of the tumor and its relationship with the surrounding bile ducts with omnidirectional, multiple-angle, and multilevel views. 3DV and 3DP technologies can help to determine the target bile duct, assist in selective cannulation, guide the selection and placement of biliary stent in ERCP, and reduce the use of contrast media. But our findings require further reverification, because the number of cases in this study is too small. More case studies are needed to further validate the conclusion.
Acknowledgements
The present study was supported by the scientific and technological project of Hubei Province (grant no. 2013BKB013), and Natural Science Foundation of Hubei Province in China (grant no, 2011CHB025).
References
- 1.Razumilava N, Gores GJ. Cholangiocarcinoma. Lancet. 2014;383:2168–2179. doi: 10.1016/S0140-6736(13)61903-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blechacz B, Komuta M, Roskams T, Gores GJ. Clinical diagnosis and staging of cholangiocarcinoma. Nat Rev Gastroenterol Hepatol. 2011;8:512–522. doi: 10.1038/nrgastro.2011.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rizvi S, Gores GJ. Pathogenesis, diagnosis, and management of cholangiocarcinoma. Gastroenterology. 2013;145:1215–1229. doi: 10.1053/j.gastro.2013.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paik WH, Loganathan N, Hwang JH. Preoperative biliary drainage in hilar cholangiocarcinoma: When and how. World J Gastrointest Endosc. 2014;6:68–73. doi: 10.4253/wjge.v6.i3.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li H, Qin Y, Cui Y, Chen H, Hao X, Li Q. Analysis of the surgical outcome and prognostic factors for hilar cholangiocarcinoma: A Chinese experience. Dig Surg. 2011;28:226–231. doi: 10.1159/000327361. [DOI] [PubMed] [Google Scholar]
- 6.Nagorney DM, Kendrick ML. Hepatic resection in the treatment of hilar cholangiocarcinoma. Adv Surg. 2006;40:159–171. doi: 10.1016/j.yasu.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 7.Gerges C, Schumacher B, Terheggen G, Neuhaus H. Expandable metal stents for malignant hilar biliary obstruction. Gastrointest Endosc Clin N Am. 2011;21:481–497. doi: 10.1016/j.giec.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 8.Rengier F, Mehndiratta A, von Tengg-Kobligk H, Zechmann CM, Unterhinninghfen R, Kauczor HU, Giesel FL. 3D printing based on imaging data: Review of medical applications. Int J Comput Assist Radiol Surg. 2010;5:335–341. doi: 10.1007/s11548-010-0476-x. [DOI] [PubMed] [Google Scholar]
- 9.Gross BC, Erkal JL, Lockwood SY, Chen C, Spence DM. Evaluation of 3D printing and its potential impact on biotechnology and the chemical sciences. Anal Chem. 2014;86:3240–3253. doi: 10.1021/ac403397r. [DOI] [PubMed] [Google Scholar]
- 10.Michalski MH, Ross JS. The shape of things to come: 3D printing in medicine. JAMA. 2014;312:2213–2214. doi: 10.1001/jama.2014.9542. [DOI] [PubMed] [Google Scholar]
- 11.Murphy SV, Atala A. 3D bioprinting of tissues and organs. Nat Biotechnol. 2014;32:773–785. doi: 10.1038/nbt.2958. [DOI] [PubMed] [Google Scholar]
- 12.Zeng N, Fang CH, Fan YF, Yang J, Xiang N, Zhu W, Liu J, Cai W, Mo ZK. The construction of three-dimensional visualization platform and its application in diagnosis and treatment for hilar cholangiocarcinoma. Zhonghua Wai Ke Za Zhi. 2016;54:680–685. doi: 10.3760/cma.j.issn.0529-5815.2016.09.007. (In Chinese) [DOI] [PubMed] [Google Scholar]
- 13.Ji GW, Zhu FP, Wang K, Jiao CY, Shao ZC, Li XC. Clinical implications of biliary confluence pattern for bismuth-corlette type IV hilar cholangiocarcinoma applied to hemihepatectomy. J Gastrointest Surg. 2017;21:666–675. doi: 10.1007/s11605-017-3377-2. [DOI] [PubMed] [Google Scholar]
- 14.Yasuda I, Mukai T, Moriwaki H. Unilateral versus bilateral endoscopic biliary stenting for malignant hilar biliary strictures. Dig Endosc. 2013;25(Suppl 2):S81–S85. doi: 10.1111/den.12060. [DOI] [PubMed] [Google Scholar]
- 15.Vienne A, Hobeika E, Gouya H, Lapidus N, Fritsch J, Choury AD, Chryssostalis A, Gaudric M, Pelletier G, Buffet C, et al. Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: The role of liver volume assessment. Gastrointest endosc. 2010;72:728–735. doi: 10.1016/j.gie.2010.06.040. [DOI] [PubMed] [Google Scholar]
- 16.Bismuth H, Corlette MB. Intrahepatic cholangioenteric anastomosis in carcinoma of the hilus of the liver. Surg Gynecol Obstet. 1975;140:170–178. [PubMed] [Google Scholar]
- 17.Lee KY, Cho JW, Chang NY, Chae JM, Kang KH, Kim SC, Cho JH. Accuracy of three-dimensional printing for manufacturing replica teeth. Korean J Orthod. 2015;45:217–225. doi: 10.4041/kjod.2015.45.5.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Obregon F, Vaquette C, Ivanovski S, Hutmache DW, Bertassoni LE. Three-dimensional bioprinting for regenerative dentistry and craniofacial tissue engineering. J Dent Res. 2015;94(9 Suppl):143S–152S. doi: 10.1177/0022034515588885. [DOI] [PubMed] [Google Scholar]
- 19.Wu XB, Wang JQ, Zhao CP, Sun X, Shi Y, Zhang ZA, Li YN, Wang MY. Printed three-dimensional anatomic templates for virtual preoperative planning before reconstruction of old pelvic injuries: Initial results. Chin Med J (Engl) 2015;128:477–482. doi: 10.4103/0366-6999.151088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ikegami T, Maehara Y. Transplantation: 3D printing of the liver in living donor liver transplantation. Nat Rev Gastroenterol Hepatol. 2013;10:697–698. doi: 10.1038/nrgastro.2013.195. [DOI] [PubMed] [Google Scholar]
- 21.Zein NN, Hanouneh IA, Bishop PD, Samaan M, Eghtesad B, Quintini C, Miller C, Yerian L, Klatte R. Three-dimensional print of a liver for preoperative planning in living donor liver transplantation. Liver Transpl. 2013;19:1304–1310. doi: 10.1002/lt.23729. [DOI] [PubMed] [Google Scholar]
- 22.Baimakhanov Z, Soyama A, Takatsuki M, Hidaka M, Hirayama T, Kinoshita A, Natsuda K, Kuroki T, Eguchi S. Preoperative simulation with a 3-dimensional printed solid model for one-step reconstruction of multiple hepatic veins during living donor liver transplantation. Liver Transpl. 2015;21:266–268. doi: 10.1002/lt.24019. [DOI] [PubMed] [Google Scholar]
- 23.Velayutham V, Fuks D, Nomi T, Kawaguchi Y, Gayet B. 3D visualization reduces operating time when compared to high-definition 2D in laparoscopic liver resection: A case-matched study. Surg Endosc. 2016;30:147–153. doi: 10.1007/s00464-015-4174-1. [DOI] [PubMed] [Google Scholar]
- 24.Xie A, Fang C, Huang Y, Fan Y, Pan J, Peng F. Application of three-dimensional reconstruction and visible simulation technique in reoperation of hepatolithiasis. J Gastroenterol Hepatol. 2013;28:248–254. doi: 10.1111/jgh.12066. [DOI] [PubMed] [Google Scholar]
- 25.He YB, Bai L, Aji T, Jiang Y, Zhao JM, Zhang JH, Shao YM, Liu WY, Wen H. Application of 3D reconstruction for surgical treatment of hepatic alveolar echinococcosis. World J Gastroenterol. 2015;21:10200–10207. doi: 10.3748/wjg.v21.i35.10200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fang C. Minimally invasive digital technology: A new edge tool for the diagnosis and treatment of hepatolithiasis. Dig Med. 2016;2:1–5. doi: 10.4103/2226-8561.182299. [DOI] [Google Scholar]
- 27.Koganemaru M, Horiuchi H, Abe T. Treatment of hypohepatia after transplantation of liver from a living donor liver by transcatheter embolization, using a simulated 3-dimensional printing vascular model. Gastroenterology. 2016;151:e11–e13. doi: 10.1053/j.gastro.2016.02.020. [DOI] [PubMed] [Google Scholar]
- 28.Oshiro Y, Ohkohchi N. Three-dimensional liver surgery simulation: Computer-assisted surgical planning with three-dimensional simulation software and three-dimensional printing. Tissue Eng Part A. 2017;23:474–480. doi: 10.1089/ten.tea.2016.0528. [DOI] [PubMed] [Google Scholar]
- 29.Fang CH, Zhu W, Wang H, Xiang N, Fan Y, Yang J, Wang X, Zhong Sz. A new approach for evaluating the resectability of pancreatic and periampullary neoplasms. Pancreatology. 2012;12:364–371. doi: 10.1016/j.pan.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 30.Fang CH, Liu J, Fan YF, Yang J, Xiang N, Zeng N. Outcomes of hepatectomy for hepatolithiasis based on 3-dimensional reconstruction technique. J Am Coll Surg. 2013;217:280–288. doi: 10.1016/j.jamcollsurg.2013.03.017. [DOI] [PubMed] [Google Scholar]
- 31.Katsinelos P, Lazaraki G, Chatzimavroudis G, Gkagkalis S, Vasiliadis I, Papaeuthimiou A, Terzoudis S, Pilpilidis I, Zavos C, Kountouras J. Risk factors for therapeutic ERCP-related complications: An analysis of 2,715 cases performed by a single endoscopist. Ann Gastroenterol. 2014;27:65–72. [PMC free article] [PubMed] [Google Scholar]
- 32.Iorgulescu A, Sandu I, Turcu F, Iordache N. Post-ERCP acute pancreatitis and its risk factors. J Med Life. 2013;6:109–113. [PMC free article] [PubMed] [Google Scholar]
- 33.Kostrzewska M, Baniukiewicz A, Wroblewski E, Laszewicz W, Swidnicka-Siergiejko A, Piotrowska-Staworko G, Dlugosz JW, Dabrowski A. Complications of endoscopic retrograde cholangiopancreatography (ERCP) and their risk factors. Adv Med Sci. 2011;56:6–12. doi: 10.2478/v10039-011-0012-4. [DOI] [PubMed] [Google Scholar]
- 34.Hintze RE, Abou-Rebyeh H, Adler A, Veltzke-Schlieker W, Felix R, Wiedenmann B. Magnetic resonance cholangiopancreatography-guided unilateral endoscopic stent placement for Klatskin tumors. Gastrointest Endosc. 2001;53:40–46. doi: 10.1067/mge.2001.111388. [DOI] [PubMed] [Google Scholar]
- 35.Freeman ML, Overby C. Selective MRCP and CT-targeted drainage of malignant hilar biliary obstruction with self-expanding metallic stents. Gastrointest Endosc. 2003;58:41–49. doi: 10.1067/mge.2003.292. [DOI] [PubMed] [Google Scholar]
- 36.Fang CH, Tao HS, Yang J, Fang ZS, Cai W, Liu J, Fan YF. Impact of three-dimensional reconstruction technique in the operation planning of centrally located hepatocellular carcinoma. J Am Coll Surg. 2015;220:28–37. doi: 10.1016/j.jamcollsurg.2014.09.023. [DOI] [PubMed] [Google Scholar]