Abstract
Background:
The most common neurodegenerative disease is dementia. Family of dementia patients says that their lives have been changed extensively after happening of dementia to their patients. One of the problems of family and caregivers is depression of the caregiver. In this study, we aimed to find the prevalence of depression and factors can affect depression in the dementia caregivers.
Materials and Methods:
This study was cross-sectional study with convenient sampling method. Our society was 96 main caregivers of dementia patients in the year 2015 in Iran. We had two questionnaires, a demographic and Beck Depression Inventory (BDI). BDI Cronbach's alpha is 0.86 for psychiatric patients and 0.81 for nonpsychiatric persons, and Beck's scores are between 0 and 64. We used SPSS version 22 for statistical analysis.
Results:
According to Beck depression test, 69.8% (n = 67 out of 96) of all caregivers had scores in the range of depression. In bivariate analysis, we found higher dementia severity and lower support of other family members from the caregiver can predict higher depression in the caregiver. As well, in regression analysis using GLM model, we found higher age and lower educational level of the caregiver can predict higher depression in the caregiver. Moreover, regression analysis approved findings about severity and support of other family members in bivariate analysis.
Conclusion:
High-level depression is found in caregivers of dementia patients. It needs special attention from healthcare managers, clinicians and all of health-care personnel who deals with dementia patients and their caregivers.
Keywords: Alzheimer, caregiver, dementia, depression, predictor
Introduction
The most common neurodegenerative disease is dementia. This disease affects memory, behavior, and mind of a patient.[1] It was estimated that the persons with dementia, was 35 million people, in 2010, worldwide and it will be 115 million in 2050.[2] Dementia's costs were $604bn in 2010 globally.[3] Not all of the costs are financial but emotional and physical demands of the patients can be a stressor for caregivers to cause adverse psychological and physical outcomes.[4]
There are different reasons that cause depression in the caregivers of dementia patients including neglecting their own health and social lives,[2] large burden on caregivers, deteriorating disability of dementia patients,[5] and emotional and physical demands of the patients as a stressor.[4] Depression is not only a psychological problem but also it can cause arterial hypertension, gastrointestinal problems, and other physical illnesses[2] and it can raise the risk of death.[1]
The family of dementia patients says that their lives have been changed extensively after happening of dementia to their patients.[6] A study in the USA by Givens et al. illustrated that 22% of caregivers of dementia have depressive symptoms. However, previous studies estimated that the depression prevalence is between 30% and 40%.[4] In a review article by Janevic et al. published in 2001, white caregivers had more depression and stress than African American ones, and they suggested that there may be different depression prevalence in different races, cultures, and nations.[7] De fazio et al.'s study illustrated, higher level of urbanity, advanced age, and lower socioeconomic status were associated with the depression in caregivers.[2] Givens et al. showed caregiver role captivity, dementia patients problematic behaviors and advanced age of caregivers have an association with depression in caregivers.[4]
According to different depression prevalence and predictors in different countries and cultures, we aimed to find the prevalence of depression and factors, inducing and reducing factors, can affect depression in the dementia caregivers in Iran. We aimed to find the prevalence of depression of main caregivers and its relation with age of caregivers and patients, gender of caregivers and patients, educational level of caregivers, severity of dementia illness, duration of dementia illness, support of other family members, and relationship of caregiver and patients. To the best of our knowledge, we are not aware of similar research in Iran.
Materials and Methods
This study was cross-sectional study with convenient sampling method. Our society was main caregivers of dementia patients who their patients visit the psychiatrist in clinics affiliated to Isfahan University of Medical Sciences in the year of 2015. With statistical calculation, we needed 96 samples for this study.
Inclusion criteria were: (1) being in the range of age 18–65 years old for caregivers, (2) being the main caregiver of demented person. We explained the study and its aims for all the caregivers, and they consented orally to participate in the study.
Our exclusion criteria were: (1) incomplete questionnaires, (2) known psychiatric illness or end stage dangerous physical illnesses of the caregiver.
As we mentioned before, we only included the main caregivers of the dementia patients. We know the main caregiver who spends a long time with the patient, more than others, support the patient physically and mentally and help the demented person in daily activities.
We had two questionnaires for this study. One of them was demographic data questionnaire. We collected demographic data such as the age of patient and caregiver, gender of each them, educational level of the main caregiver, support of other family members, health insurance of the patient, duration of dementia illness, patients’ economical independency/dependency to caregiver or others, and relationship of patient and caregiver.
We determined support of other family members by a question from main caregivers that how you know the support of other family members. They should have chosen between “good,” “poor,” and “no support.” As well, we determined the severity of dementia illness and diagnosis of dementia with psychiatric interview by an experienced psychiatrist.
Another questionnaire of this study was Beck Depression Inventory (BDI). BDI Cronbach's alpha is 0.86 for psychiatric patients and 0.81 for nonpsychiatric persons. For psychiatric patients, the mean correlations of BDI samples with Hamilton Rating Scale for Depression (HRSD) and clinical rating are 0.73 and 0.72, respectively. For nonpsychiatric persons, the mean correlations of the BDI with the HRSD and clinical ratings were 0.74 and 0.60, respectively.[8] This questionnaire has 21 questions with four choices for each question, and its score is 0–3 for each question. The maximum total score is 64. If total questionnaire score is between 0 and 10, it means no depression, 11–17 means mild depression, 18–29 means moderate depression, and 30–64 means severe depression.[9]
We gave these two questionnaires to main caregivers who their patients visit the psychiatrists in clinics affiliated to Isfahan University of Medical Sciences to fulfill. They had enough time, and we wanted them to choose the answers that are closest to their feelings.
We input all demographic data and Beck questionnaire scores in SPSS version 22.(IBM corporation, New York, USA) We used independent T, Pearson correlation, one-way ANOVA, and regression analysis using GLM model after controlling other variables for analysis the data.
The study was approved by Isfahan University of Medical Sciences Ethics Committee. We paid attention to keep demographic data, and Beck questionnaire answers secure to save privacy of participants. The participants were free to participate or not participate in the study.
Results
According to BDI 69.8% (n = 67 out of 96) of all caregivers had scores in the range of depression. It showed that 20.8% (n = 20) of all caregivers had scores in the range of mild depression, 40.6% (n = 39) had scores in the range of moderate depression, and 8.3% (n = 8) had scores in the range of severe depression.
Demographic data and mean beck depression test scores can be found in Tables 1 and 2.
Table 1.
Relation between demographic variable and beck depression scores
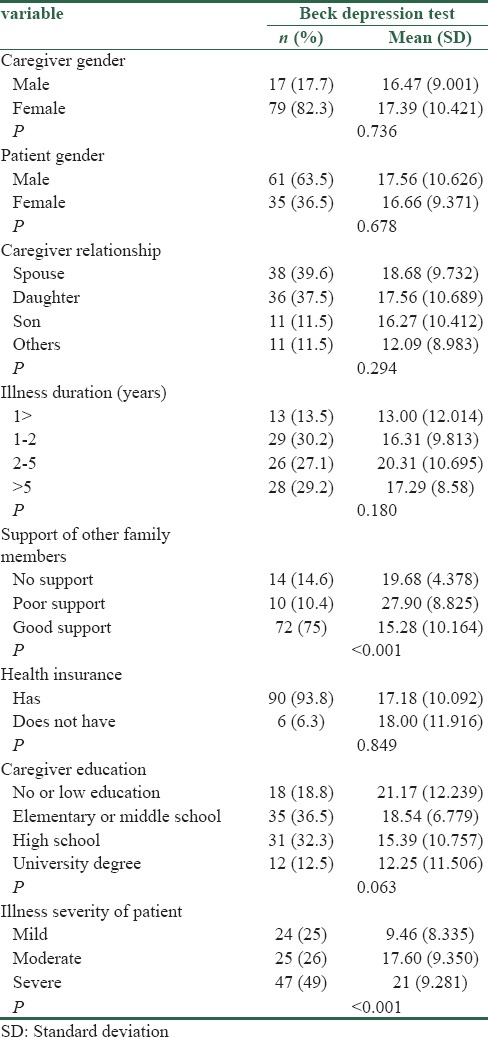
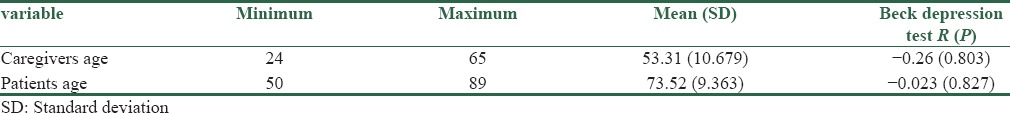
Table 2.
Pearson correlation of caregivers ages and patients ages with beck depression scores
We asked the caregivers to evaluate support of other family members by choosing it between “good,” “poor,” and “no support” choices. We found mean depression scores in good supporter families was 15.2 and in poor supporter was 27.9. This was a significant difference (P < 0.001, Table 1).
As we mentioned before, we evaluated the severity of dementia illness by psychiatric interview by experienced psychiatrists. We found that mean depression score of the caregivers of mild dementia patients had a significant difference with the caregivers of the moderate and severe dementia patients. Their P values were 0.006 and <0.001, respectively.
In bivariate analysis, we did not find any other significant relationship between demographic data beck scores [Table 1].
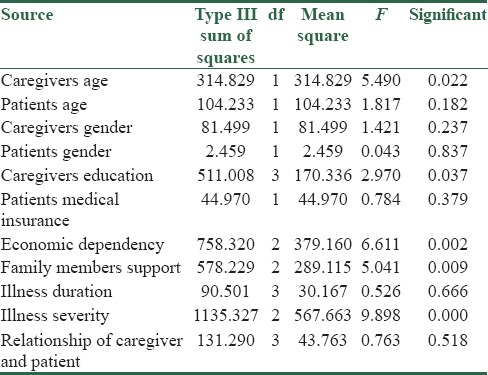
However, we found other significant relationship when we used regression analysis using GLM model after controlling other variables. In this analysis according to Table 3, the caregiver age and the caregiver education had a significant relationship with beck depression scores. Higher age of caregiver and lower education of his/her can predict higher depression in the caregiver. According to Table 3, other factors in this model that had significant results were the severity of illness of dementia and support of other family members which were a predictor for depression of the caregiver. It was like bivariate analysis.
Table 3.
Result of regression analysis by using GLM model after controlling other variables
Discussion
Depression prevalence between caregivers of dementia patients was reported in a wide range. Bednarek et al. release a research in 2016, has been done in Poland, they reported the prevalence of depression in dementia caregivers about four-tenth.[10] In 1991, Dura et al. in research in the USA reported one-fourth of the caregivers met depressive DSM criteria. It was three times more than matched control.[11] We found about seven-tenth of the caregivers had scores in the range of depression. All of above show the depression prevalence in dementia caregivers is very high, and it is considerably higher than normal populations and caregivers of other illnesses. Our findings showed higher prevalence than other two studies. It may be caused by different scale for checking depression, different cutoff points or the prevalence is really higher in Iran.
In this study, eight-tenth of the caregivers were female. It is like De Fazio et al. study[12] and most of other studies in this field. However, about six-tenth of the patients were male. In Abdollahpour et al. study in Iran, six-tenth of patients were female.[13] Since the Alzheimer disease is the most prevalent kind of dementia, and it is most common in females, we expected to have more female patients in this study. However, we had more male patients. One of the reasons may be caused by not differentiating a different kind of dementia. The other reason could be that the caregivers of female patients had lower attitude to participate in the study and talk about their patients due to cultural reasons.
In both bivariate analysis and regression analysis using GLM model after controlling other variables, we found severity of illness of dementia and support of other family members of the main caregiver can predict the depression caregiver. Higher severity of dementia and lower support of others can raise the depression of the caregiver. Effect of severity is like Garcia-Alberca et al. study.[14] It is very important to know that support of other family members has a strong effect on depression of the caregiver. Therefore, medical team and healthcare managers should encourage caregiver and his/her family to act as a team in caring or family help and support the caregiver as much as possible. Medical team also should reduce the dementia patient severity of illness by drugs or other treatments for dementia as much as possible. It does not only affect dementia patients but also affect the caregivers, which are dynamic and younger group, to have better feeling and life. In addition, future treatments for dementia will affect both patient and his/her caregiver, and should be strongly continued for a prevalent and growing population of dementia patients and their caregivers.
In addition, in regression analysis using GLM model, we found that the age of caregiver and caregiver education could predict the severity of depression in the caregiver. Low level of education and higher age of the caregiver can make higher depression in the caregiver. Givens et al. in research in the USA demonstrated the same result about age.[4]
Ostojic et al. in a research in Croatia that is published in 2014 demonstrated female caregivers feel more depression and younger age of caregiver predicts more depression.[1] However, in both field of age and gender, we found different results. As we mentioned before, higher age of caregivers predicts more depression in caregivers and we did not find any significant difference between different gender results. As well, we did not find any significant depression scores between the different relationship between caregiver and patient, different duration of illness and different genders of patients. In other words, the relationship between caregiver and patient, duration of illness, the patient gender and the caregiver gender do not affect the depression of the caregiver.
In study has been published by Goren et al. in 2016 in Japan, in the comparison between dementia caregivers and noncaregivers, they found more frequent insomnia, hypertension, pain, anxiety, and diabetes in dementia caregivers.[15]
One of our study limitations was convenient sampling. We could only include caregiver of patients who visited doctors and took treatment for their dementia. Patients who are not visited by doctors may have more severe dementia. Since this study showed more severe dementia could make more depression in caregivers, we can have even more depression in caregivers of these dementia patients. Another limitation was using a questionnaire for finding the depression. This questionnaire reliability and validity has been proven, but we did not use the clinical interview for finding and evaluating depression in the caregivers.
Conclusion
As a conclusion, high-level depression is found in caregivers of dementia patients. It needs special attention from healthcare managers, clinicians, and all of the health-care personnel who deals with dementia patients and their caregivers. Physicians and psychiatrist who deals with dementia patients should have attention to caregivers and their depression as well especially in Iran that we found caregiver's depression may be higher than other researches in other countries. As we mentioned before, higher severity and lower support of other family members can raise depression of caregivers. Therefore, present, new, and future treatments of dementia for reducing the severity of illness can also affect feelings of caregivers as growing, younger, and more dynamic population. As we mentioned before, caring should be encouraged to be done as a group work or if it is not possible, helping and supporting of the main caregiver as much as possible should be recommended.
Moreover, a plan can be obtained to evaluate the depression in caregivers of dementia patients in whole society as a screening method to find depressed caregivers and to refer them to psychiatrists. We recommend for future research to do interventions to reduce depression and then evaluate depression in study groups. Some of the examples of intervention methods can be family meetings, support from health-care system, and visiting of psychiatrists by caregivers every few months then evaluate the depression to find if these interventions can reduce depression in caregivers or not.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ostojic D, Vidovic D, Bacekovic A, Brecic P, Jukic V. Prevalence of anxiety and depression in caregivers of Alzeheimer's dementia patients. Acta Clin Croat. 2014;53:17–21. [PubMed] [Google Scholar]
- 2.De Fazio P, Ciambrone P, Cerminara G, Barbuto E, Bruni A, Gentile P, et al. Depressive symptoms in caregivers of patients with dementia: Demographic variables and burden. Clin Interv Aging. 2015;10:1085–90. doi: 10.2147/CIA.S74439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boots LM, de Vugt ME, van Knippenberg RJ, Kempen GI, Verhey FR. A systematic review of Internet-based supportive interventions for caregivers of patients with dementia. Int J Geriatr Psychiatry. 2014;29:331–44. doi: 10.1002/gps.4016. [DOI] [PubMed] [Google Scholar]
- 4.Givens JL, Mezzacappa C, Heeren T, Yaffe K, Fredman L. Depressive symptoms among dementia caregivers: Role of mediating factors. Am J Geriatr Psychiatry. 2014;22:481–8. doi: 10.1016/j.jagp.2012.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jensen M, Agbata IN, Canavan M, McCarthy G. Effectiveness of educational interventions for informal caregivers of individuals with dementia residing in the community: Systematic review and meta-analysis of randomised controlled trials. Int J Geriatr Psychiatry. 2015;30:130–43. doi: 10.1002/gps.4208. [DOI] [PubMed] [Google Scholar]
- 6.Garlo K, O’Leary JR, Van Ness PH, Fried TR. Burden in caregivers of older adults with advanced illness. J Am Geriatr Soc. 2010;58:2315–22. doi: 10.1111/j.1532-5415.2010.03177.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Janevic MR, Connell CM. Racial, ethnic, and cultural differences in the dementia caregiving experience: Recent findings. Gerontologist. 2001;41:334–47. doi: 10.1093/geront/41.3.334. [DOI] [PubMed] [Google Scholar]
- 8.Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 9.Omranifard V, Masaeli N, Emami Ardestani P. Prevalence of depression and anxiety in caregivers of patients in psychiatric wards (2006) J Semnan Univ Med Sci. 2008;9:223–7. [Google Scholar]
- 10.Bednarek A, Mojs E, Krawczyk-Wasielewska A, Glodowska K, Samborski W, Lisinski P, et al. Correlation between depression and burden observed in informal caregivers of people suffering from dementia with time spent on caregiving and dementia severity. Eur Rev Med Pharmacol Sci. 2016;20:59–63. [PubMed] [Google Scholar]
- 11.Dura JR, Stukenberg KW, Kiecolt-Glaser JK. Anxiety and depressive disorders in adult children caring for demented parents. Psychol Aging. 1991;6:467–73. doi: 10.1037//0882-7974.6.3.467. [DOI] [PubMed] [Google Scholar]
- 12.Xiao LD, Wang J, He GP, De Bellis A, Verbeeck J, Kyriazopoulos H. Family caregiver challenges in dementia care in Australia and China: A critical perspective. BMC Geriatr. 2014;14:6. doi: 10.1186/1471-2318-14-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abdollahpour I, Noroozian M, Nedjat S, Majdzadeh R. Caregiver burden and its determinants among the family members of patients with dementia in Iran. Int J Prev Med. 2012;3:544–51. [PMC free article] [PubMed] [Google Scholar]
- 14.García-Alberca JM, Lara JP, Berthier ML. Anxiety and depression in caregivers are associated with patient and caregiver characteristics in Alzheimer's disease. Int J Psychiatry Med. 2011;41:57–69. doi: 10.2190/PM.41.1.f. [DOI] [PubMed] [Google Scholar]
- 15.Goren A, Montgomery W, Kahle-Wrobleski K, Nakamura T, Ueda K. Impact of caring for persons with Alzheimer's disease or dementia on caregivers’ health outcomes: Findings from a community based survey in Japan. BMC Geriatr. 2016;16:122. doi: 10.1186/s12877-016-0298-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


