Abstract
Aims
Cardiac resynchronization therapy (CRT) is a recommended treatment of heart failure (HF) patients with depressed left ventricular ejection fraction and wide QRS. The optimal right ventricular (RV) lead position being a matter of debate, we sought to examine whether RV septal (RVS) pacing was not inferior to RV apical (RVA) pacing on left ventricular reverse remodelling in patients receiving a CRT-defibrillator.
Methods and results
Patients (n = 263, age = 63.4 ± 9.5 years) were randomly assigned in a 1:1 ratio to RVS (n = 131) vs. RVA (n = 132) pacing. Left ventricular end-systolic volume (LVESV) reduction between baseline and 6 months was not different between the two groups (−25.3 ± 39.4 mL in RVS group vs. −29.3 ± 44.5 mL in RVA group, P = 0.79). Right ventricular septal pacing was not non-inferior (primary endpoint) to RVA pacing with regard to LVESV reduction (average difference = −4.06 mL; P = 0.006 with a −20 mL non-inferiority margin). The percentage of ‘echo-responders’ defined by LVESV reduction >15% between baseline and 6 months was similar in both groups (50%) with no difference in the time to first HF hospitalization or death (P = 0.532). Procedural or device-related serious adverse events occurred in 68 patients (RVS = 37) with no difference between the two groups (P = 0.401).
Conclusion
This study demonstrates that septal RV pacing in CRT is non-inferior to apical RV pacing for LV reverse remodelling at 6 months with no difference in the clinical outcome. No recommendation for optimal RV lead position can hence be drawn from this study.
ClinicalTrials. gov number
Keywords: Cardiac resynchronization therapy, Right ventricular lead position, Right ventricular defibrillation lead, Left ventricular end-systolic volume
Introduction
Cardiac resynchronization therapy (CRT) is a recommended therapeutic strategy in the treatment of patients with symptomatic heart failure (HF) and depressed left ventricular ejection fraction (LVEF) and wide QRS.1 Cardiac resynchronization therapy is obtained by simultaneous or sequential pacing of the right and left ventricles. Despite such implantation is technically successful in >90% of patients;2–4 clinical improvement or left ventricular (LV) reverse remodelling is achieved in no more than 2/3 of the patients. Several reasons may explain such incomplete response: sub-optimal patients selection,1,4–8 inadequate LV lead position,9–12 and sub-optimal programming.13
Whether the right ventricular (RV) lead position may improve the response to CRT is a matter of debate. Apical position is conventional, especially in patients receiving a CRT-defibrillator (CRT-D) but long-term RV apical pacing may adversely affect cardiac function in intracardiac cardioverter defibrillator (ICD) recipients.14–16 Alternative RV pacing sites, mainly RV septal, have been recently proposed in CRT recipients. No significant benefit of these alternative RV pacing sites was demonstrated with the limitations of either retrospective analysis of large prospective trials,11,12 prospective non-randomized trials,10,17–21 or single-centre randomized study.22 We hence conducted a prospective randomized European multicentre trial to examine the effects of the RV lead positions, i.e. apical or septal, on the LV reverse remodelling in patients receiving a CRT-D.
Study design and objectives
SEPTAL CRT is a randomized, controlled, single-blind, multicentre trial, including two parallel patient groups receiving a CRT-D randomly assigned to implantation of the ICD lead at the RV mid-septum (RVS) or at the RV apex (RVA). This study was approved by the Ethics Committee of Rennes University Hospital, France. All patients signed written, informed consent prior enrolment in the study. The study complied with the Declaration of Helsinki.
The primary objective was to demonstrate that RVS pacing was not inferior to RVA pacing in terms of changes in the left ventricular end-systolic volume (LVESV) between baseline and 6 months.
The main secondary objectives were:
to assess the percentage of ‘echo-responders’ defined by a reduction in LVESV >15% at 6 months;
to assess the implant success rate of the ICD lead using pre-specified electrical criteria;
to compare the clinical outcome between the two groups using the 6 minutes' walk test (6 MWT) and the Milton Packer score;23 and
to assess the total mortality and HF hospitalizations at 12 months.
Patient selection
The patients included in this trial were ≥18 years of age and had indications for CRT-D implantation according to the 2008 European Society of Cardiology (ESC) guidelines,24 i.e. patients with a documented LVEF (assessed by the implanting centre) ≤35% in the last 3 months, a New York Heart Association (NYHA) class III or ambulatory class IV stable for the last month prior enrolment receiving optimal medical therapy for at least 1 month, a QRS ≥120 ms with a stable sinus rhythm. The inclusion criteria were modified after the release of the ESC updated Guidelines 201025 with extension of the inclusion to NYHA class II patients with a QRS ≥150 ms.
Implantable cardioverter-defibrillator lead implantation
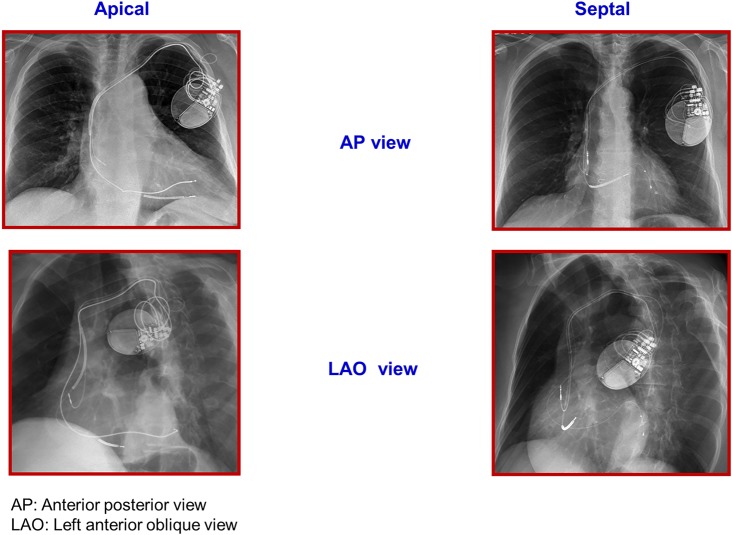
All patients received an ENDOTAK RELIANCE® G (Guidant/Boston Scientific, Natick, MA, USA) active fixation, single- or dual-coil ICD lead, implanted in the RVS vs. the RVA. Leads assigned to the RVS were considered optimally implanted when they were oriented frontally and towards the left in a 40–45° left anterior oblique fluoroscopic projection (Figure 1A). Leads assigned to the RVA group were advanced as far as possible towards the RV apex (Figure 1B).26 After implantation, the location of RV leads was reviewed by two physicians, in a blinded manner.
Figure 1.
Right ventricular lead apical and septal locations.
Lead implantation was considered successful when the four following electrical endpoints were obtained: (i) R wave amplitude >5 mV, (ii) RV capture threshold <1.5 V/0.5 ms, (iii) pacing lead impedance between 450 and 1800 Ω at a 5 V, all measured with a pacing system analyser, and (iv) a 10 J safety margin for defibrillation threshold. If all these criteria were not obtained, a second attempt in an adjacent assigned position was performed. In case of subsequent failure, the lead was repositioned at the alternative site.
Left ventricular lead implant
Left ventricular lead was inserted in the coronary sinus. The lateral position was targeted first, then the posterolateral position, and finally the posterior position. In case of coronary sinus lead implant failure, an epicardial lead was surgically implanted (n = 6).
Echocardiographic methods
In each centre, echocardiographic recordings were performed by cardiologists certified for this study. The main following parameters were assessed: Right and left pre-ejection delays and interventricular mechanical delay.
– Left ventricular end-systolic and end-diastolic diameters (LVESD and LVEDD),
– Left ventricular end-systolic volume and LVEDVs,
– Left ventricular ejection fraction calculated by the Simpson method, and
– Left ventricular filling time.
Left ventricular volumes were measured in the apical two and four chambers views and averaged. Left ventricular ejection fraction, left atrial area, and LV diameters were measured using standard methods. Echocardiograms were sent on digital storage media to an independent echocardiographic core laboratory (Genevieve Derumeaux, University Hospital, Créteil, France), where they were screened for quality. All measurements were made at baseline and in patients with echocardiograms available at 6 and 12 months. Core laboratory intra- and inter-observer variabilities of echocardiographic parameters measurements have been reported earlier and were, respectively, 12 and 16% for LVESV.27
Baseline data, follow-up, and data collection
Device interrogation was performed at pre-discharge, at 1, 6, and 12 months. Following tachycardia parameters were recommended for ICD programming: ventricular fibrillation (VF) zone ≥220 b.p.m. and in case of a ventricular tachycardia (VT) zone, a minimum of six anti-tachycardia pacing attempts before shock delivery. Electrical lead characteristics as well as arrhythmic events were collected at each interrogation. AV delay optimization was performed before discharge using the iterative mitral flow method under echocardiography. New York Heart Association class was assessed at each follow-up by a physician blinded to the lead position. The 6 MWT and the Milton Packer test were performed at baseline, 6, and 12 months and assessed by a blinded observer.
Statistical analysis
The study planned to include 240 patients to prove the non-inferiority of RVS pacing in terms of LVESV reduction at 6 months with a 90% power at 2.5% unilateral significance level, and a rate of 33% of non-available assessments at 6 months. The intention to treat (ITT) population included all randomized patients. Patients without at least one major deviation and with LVESV measurable at baseline represented the per protocol (PP) population.
The ITT population was analysed according to the randomized group while the PP population was analysed according to the implanted site. For both the ITT and PP populations, non-inferiority was analysed by examining the lower limit of the confidence interval of the difference in LVESV reduction between groups. If the lower limit was greater than the non-inferiority margin of −20 mL, the null hypothesis was rejected and the septal group was considered non-inferior with regard to the apical group. Superiority analysis was conducted if non-inferiority was achieved using bilateral t-test and analysis of variance adjusted on baseline value. The global alpha risk level was kept at 5%, according to the a priori ordered hypotheses theory. In addition, sensitivity analysis was performed by variance analysis, with the baseline LVESV value as adjustment factor.
Patients with a 6 months reduction >15% in LVESV were compared between groups using the χ2 test. Other criteria were analysed in the ITT population by the use of descriptive statistics and univariate tests (χ2 test or Fisher's exact test according to expected number in crossings for categorical variables, Kruskal–Wallis test for ordinal variables, and analyses of variance on ranked transformed variables for quantitative variables). Changes from baseline were tested by the use of the Wilcoxon sign-rank test. Time to appearance of adverse events was analysed by Kaplan–Meier estimates and comparison between groups was made using the log-rank test. As a conservative approach, the last observation carry forward method was used for echocardiographic data and 6 MWT. All statistical analyses were performed using the SAS software version 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
A total of 263 patients (72.6% male) were randomized to RVA (n = 132) or to RVS (n = 131) pacing in 25 centres, 16 in France and 9 in Spain (Appendix) and represent the ITT population. Crossover due to failure of fulfilling the RV implantation criteria in the randomized location was evenly distributed in both arms with two patients crossing over in each group. Two hundred and thirty-one patients reached the end of follow-up (death: n = 9, lost to follow-up: n = 10, and premature exit: n = 13). The mean follow-up was 11.04 ± 3.3 months.
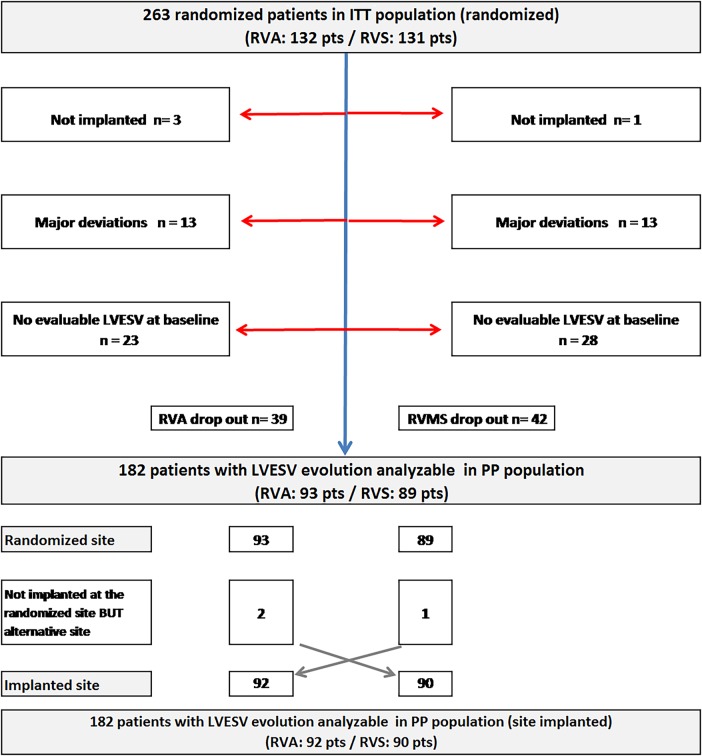
The PP analysis included 182 patients (RVA: n = 92) (Figure 2).
Figure 2.
Population flowchart.
Patient's characteristics of ITT and PP populations are reported in Tables 1 and 2 with no statistical difference between the the groups. Briefly, 72.6% were male, with approximately three of four of non-ischaemic cardiomyopathy and 88.5% were in NYHA class III. The mean age was 63.4 ± 9.5 years and the mean LVEF was 30 ± 8%.
Table 1.
Baseline characteristics of the intention to treat population
| RVA (132) | RVS (131) | P-value | Total (263) | |
|---|---|---|---|---|
| Men (%) | 74.2 | 71.0 | 0.582 | 72.6 |
| Age (years) | 63.8 ± 9.5 | 63.1 ± 9.4 | 0.583 | 63.4 ± 9.5 |
| NYHA class II (%) | 6.9 | 7.8 | 0.707 | 7.3 |
| NYHA class III (%) | 88.5 | 88.4 | 88.5 | |
| NYHA class IV ambulatory (%) | 4.6 | 3.9 | 4.2 | |
| Ischaemic cardiomyopathy (%) | 27.3 | 26.0 | 0.889 | 26.6 |
| LVEF (%) | 30.0 ± 7.7 | 29.6 ± 8.1 | 0.858 | 30 ± 8 |
| LVESV (mL) | 154 ± 72 | 157 ± 80 | 0.794 | 155 ± 76 |
| Baseline medication (%) | ||||
| Diuretics (%) | 83.3 | 86.3 | 0.607 | 84.8 |
| ACE inhibitor or ARB (%) | 93.4 | 95.6 | 0.591 | 94.5 |
| Aldosterone antagonist (%) | 33.3 | 37.4 | 0.521 | 35.4 |
| Beta-blocker (%) | 88.6 | 90.1 | 0.842 | 89.4 |
| ICD indication for primary prevention (%) | 98.5 | 97.7 | 0.684 | 98.1 |
| QRS duration (ms) | 161.2 ± 21.4 | 161.0 ± 22.9 | 0.703 | 161.1 ± 22.1 |
| >150 ms (%) | 70.1 | 65.4 | 0.502 | 67.7 |
| LBBB (%) | 81.6 | 80.2 | 0.856 | 80.9 |
| Intrinsic QRS axis (°) | −11 ± 51 | −12 ± 45 | 0.295 | −12 ± 48 |
| RV lead procedural data | ||||
| R wave (mV) | 14.2 ± 6.9 | 13.8 ± 6.8 | 0.581 | 14.0 ± 6.8 |
| RV pacing threshold (V/0.5 ms) | 0.8 ± 0.3 | 0.7 ± 0.3 | 0.12 | 0.8 ± 0.3 |
| RV lead impedance (Ω) | 676.3 ± 146 | 761.5 ± 171.5 | <0.001 | 718.1 ± 164.6 |
| Paced QRS duration (ms) | 140.0 ± 26.0 | 136.6 ± 25.7 | 0.201 | 132 ± 53 |
| Paced QRS axis (°) | 31 ± 136 | 62 ± 103 | 0.06 | 47 ± 121 |
Values are means ± SD, or % unless otherwise indicated. All between-groups differences are statistically non-significant except for RV lead impedance.
NYHA, New York Heart Association; ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; LBBB, left bundle block branch.
Table 2.
Baseline characteristics of the per protocol population (site implanted)
| RVA (92) | RVS (90) | P-value | Total (182) | |
|---|---|---|---|---|
| Men (%) | 73.9 | 71.1 | 0.741 | 72.5 |
| Age (years) | 64.1 ± 9.7 | 62.5 ± 9.8 | 0.300 | 63.3 ± 9.8 |
| NYHA class II (%) | 5.4 | 10.1 | 0.376 | 7.7 |
| NYHA class III (%) | 90.2 | 85.4 | 87.8 | |
| NYHA class IV ambulatory (%) | 4.3 | 4.5 | 4.4 | |
| Ischaemic cardiomyopathy (%) | 27.2 | 25.6 | 0.867 | 26.4 |
| LVEF (%) | 29.9 ± 7.7 | 29.7 ± 8.2 | 0.940 | 30 ± 8 |
| LVESV (mL) | 154 ± 72 | 158 ± 83 | 0.734 | 156 ± 77 |
| Baseline medication | ||||
| Diuretics (%) | 83.7 | 86.7 | 0.678 | 85.2 |
| ACE inhibitor or ARB (%) | 93.7 | 95.7 | 0.747 | 94.7 |
| Aldosterone antagonist (%) | 38.0 | 40.0 | 0.879 | 39.0 |
| Beta-blocker (%) | 90.2 | 91.1 | 1.000 | 90.7 |
| ICD indication for primary prevention (%) | 98.9 | 97.8 | 0.619 | 98.4 |
| QRS duration (ms) | 160.1 ± 21.4 | 159.2 ± 23.0 | 0.730 | 159.6 ± 22.1 |
| >150 ms (%) | 70.8 | 62.5 | 0.267 | 66.7 |
| LBBB (%) | 85.7 | 81.8 | 0.643 | 83.8 |
| Intrinsic QRS axis (°) | −12 ± 53 | −12 ± 46 | 0.8 | −12 ± 49 |
| RV lead procedural data | ||||
| R wave (mV) | 14.1 ± 6.9 | 12.9 ± 6.5 | 0.256 | 13.5 ± 6.7 |
| RV pacing threshold (V/0.5 ms) | 0.8 ± 0.3 | 0.7 ± 0.3 | 0.035 | 0.8 ± 0.3 |
| RV lead impedance (Ω) | 761 ± 175 | 682.4 ± 165 | <0.001 | 721.7 ± 174 |
| Paced QRS duration (ms) | 140.0 ± 26.0 | 136.6 ± 25.7 | 0.201 | 138.3 ± 25.9 |
| Paced QRS axis (°) | 31 ± 136 | 56 ± 108 | 0.16 | 44 ± 123 |
Values are means ± SD, or % unless otherwise indicated. All between-groups differences are statistically non-significant except for RV lead impedance.
NYHA, New York Heart Association; ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; LBBB, left bundle block branch.
The targeted lateral or posterolateral LV lead positions were obtained in 89% of RVS randomized patients and in 91.3% of RVA randomized patients. In total, there was no statistical difference in LV position (P = 0.147) within the two groups. The number of epicardial lead was evenly distributed in both groups (three in each group). Implant duration time was 118 ± 55 min in the septal group and 112 ± 47 min in the apex group (P = 0.464), and the fluoroscopic time was 24 ± 18 vs. 22 ± 19 min, respectively (P = 0.175).
Primary endpoint
There was no difference in the LVESV at baseline between the two groups in the PP population (157.8 ± 82.5 mL in the RVS group and 153.5 ± 72.3 mL in the RVA group, P = 0.73). The mean LVESV decreased to 132.5 ± 85.9 mL (P < 0.001) in the RVS group and to 124.2 ± 66.9 mL (P < 0.001) in the RVA group (P = 0.61 between the two groups) at 6 months. The reduction in LVESV was not different between the two groups (−25.3 ± 39.4 mL in the RVS group and −29.3 ± 44.5 mL in the RVA group, P = 0.79) (Table 3) with no further significant changes at 12 months (Table 4). The primary endpoint, i.e. non-inferiority of RVS vs. RVA pacing in the LVESV change between baseline and 6-month follow-up, was reached with the lower limit of the unilateral 97.5% confidence interval equal to – 16.36 mL within the −20 mL non-inferiority margin with a mean difference = −4.06 mL (P = 0.006 for non-inferiority). When adjusted on baseline LVESV value, the lower limit of 97.5% confidence interval was −16.54 mL (the mean difference −4.72 mL, P = 0.006 for non-inferiority). In the ITT population, the reduction in LVESV between baseline and 6 months was not different between the two groups (−22.4 ± 37.3 mL in the RVS group and −29.1 ± 45.4 mL in the RVA group, P = 0.57). The lower bound of the confidence interval is −18.36 (P for non-inferiority = 0.013). The non-inferiority is also reached (−18.37 mL) after adjustment on the LVESV baseline value (P for non-inferiority = 0.013).
Table 3.
Echocardiographic measures—changes from baseline to 6 months—per protocol population
| RVA (n = 92) |
RVS (n = 90) |
P-value | |||||
|---|---|---|---|---|---|---|---|
| Baseline | 6 Months | Change | Baseline | 6 Months | Change | ||
| LVESV (mL) | |||||||
| Mean ± SD | 153.5 ± 72.3 | 124.2 ± 66.9 | −29.3 ± 44.5 | 157.8 ± 82.5 | 132.5 ± 85.9 | −25.3 ± 39.4 | 0.788 |
| Median | 134.0 | 115.0 | −20.0 | 141.5 | 110.0 | −19.5 | |
| Q1; Q3 | 105.5; 182.5 | 78.0; 154.0 | −47.5; 0.0 | 106.0; 191.0 | 84.0; 163.0 | −50.0; 0.0 | |
| LVESD (mm) | |||||||
| Mean ± SD | 62.0 ± 11 | 58.6 ± 13.4 | −3.4 ± 7.6 | 64.8 ± 11.8 | 61.4 ± 13 | −3.5 ± 7.2 | 0.681 |
| Median | 60.0 | 56.5 | 0.0 | 63.5 | 61.0 | −1.0 | |
| Q1; Q3 | 55.0; 70.0 | 50.0; 70.0 | −6.0; 0.0 | 56.5; 71.0 | 52.0; 69.0 | −6.0; 0.0 | |
| LVEDV (mL) | |||||||
| Mean ± SD | 215.2 ± 84 | 189.7 ± 77.1 | −25.5 ± 47 | 220.6 ± 93.8 | 195.3 ± 95.8 | −25.3 ± 47.7 | 0.959 |
| Median | 198.5 | 178.0 | −19.5 | 209.0 | 177.5 | −18.0 | |
| Q1; Q3 | 159.5; 247.0 | 134.0; 229.0 | −46.5; 0.0 | 156.0; 262.0 | 139.0; 227.0 | −48.0; 0.0 | |
| LVEDD (mm) | |||||||
| Mean ± SD | 72.2 ± 11.3 | 69.3 ± 12.8 | −2.9 ± 6.9 | 74.1 ± 11.4 | 71.6 ± 11.9 | −2.5 ± 7.4 | 0.925 |
| Median | 71.0 | 68.0 | 0.00 | 74.0 | 70.0 | 0.0 | |
| Q1; Q3 | 66.0; 77.0 | 61.0; 77.0 | −8.0; 0.0 | 65.5; 81.0 | 64.0; 78.0 | −5.0; 0.0 | |
| LVEF (%) | |||||||
| Mean ± SD | 30.0 ± 7.7 | 35.9 ± 10.2 | 6.0 ± 8.7 | 29.7 ± 8.2 | 35.5 ± 9.9 | 5.8 ± 9.1 | 0.770 |
| Median | 30.0 | 36.0 | 3.0 | 30.0 | 36.0 | 4.0 | |
| Q1; Q3 | 26.0; 34.0 | 29.0; 42.0 | 0.0; 10.0 | 25.0; 35.0 | 28.0; 41.0 | 0.0; 10.0 | |
| LV filling time (ms) | |||||||
| Mean ± SD | 383.9 ± 122.6 | 431.8 ± 127 | 48 ± 120 | 377.5 ± 155.4 | 431.2 ± 143.8 | 53.8 ± 133.7 | 0.353 |
| Median | 381.0 | 435.0 | 29.0 | 365.5 | 414.0 | 50.0 | |
| Q1; Q3 | 284.0; 452.0 | 341.0; 525.0 | 0.0; 97.0 | 275.5; 440.0 | 324.0; 512.0 | 0.0; 125.5 | |
LVESV, left ventricular end-systolic volume; LVESD, left ventricular end-systolic diameter; LVEDV, left ventricular end-diastolic volume; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction.
Table 4.
Echocardiographic measures—change from baseline to 12 months—per protocol population
| RVA (n = 92) |
RVS (n = 90) |
P-value | |||||
|---|---|---|---|---|---|---|---|
| Baseline | 12 Months | Change | Baseline | 12 Months | Change | ||
| LVESV (mL) | |||||||
| Mean ± SD | 153.5 ± 72.3 | 114.98 ± 67.79 | −38.55 ± 50.92 | 157.8 ± 82.5 | 125.77 ± 88.63 | −32.0 ± 43.21 | 0.472 |
| Median | 134.0 | 104.0 | −32.0 | 141.5 | 105.5 | −24.5 | |
| Q1; Q3 | 105.5; 182.5 | 68.0; 139.5 | −60.5; −2.0 | 106.0; 191.0 | 76.0; 144.0 | −58.0; 0.0 | |
| LVESD (mm) | |||||||
| Mean ± SD | 62.0 ± 11 | 56.70 ± 14.16 | −5.26 ± 8.33 | 64.8 ± 11.8 | 58.72 ± 12.91 | −6.11 ± 8.36 | 0.645 |
| Median | 60.0 | 55.5 | −2.5 | 63.5 | 57.0 | −4.0 | |
| Q1; Q3 | 55.0; 70.0 | 48.0; 67.0 | −10.0; 0.0 | 56.5; 71.0 | 50.0; 67.5 | −11.0; 0.0 | |
| LVEDV (mL) | |||||||
| Mean ± SD | 215.2 ± 84 | 178.08 ± 80.6 | −37.16 ± 55.87 | 220.6 ± 93.8 | 188.01 ± 99.03 | −32.63 ± 53.68 | 0.419 |
| Median | 198.5 | 168.0 | −34.0 | 209.0 | 166.0 | −21.0 | |
| Q1; Q3 | 159.5; 247.0 | 123.0; 211.0 | −62.0; 0.0 | 156.0; 262.0 | 129.0; 215.0 | −64.0; 4.0 | |
| LVEDD (mm) | |||||||
| Mean ± SD | 72.2 ± 11.3 | 68.93 ± 13.27 | −3.28 ± 6.59 | 74.1 ± 11.4 | 69.56 ± 12.34 | −4.55 ± 7.39 | 0.515 |
| Median | 71.0 | 67.0 | −1.0 | 74.0 | 68.0 | −3.0 | |
| Q1; Q3 | 66.0; 77.0 | 60.0; 76.0 | −9.0; 0.0 | 65.5; 81.0 | 60.0; 76.0 | −9.0; 0.0 | |
| LVEF (%) | |||||||
| Mean ± SD | 30.0 ± 7.7 | 38.15 ± 11.44 | 8.21 ± 10.04 | 29.7 ± 8.2 | 36.49 ± 10.32 | 6.78 ± 9.67 | 0.722 |
| Median | 30.0 | 39.0 | 7.0 | 30.0 | 36.5 | 7.5 | |
| Q1; Q3 | 26.0; 34.0 | 30.0; 44.0 | 0.0; 13.5 | 25.0; 35.0 | 30.0; 42.0 | 0.0; 14.0 | |
| LV filling time (ms) | |||||||
| Mean ± SD | 383.9 ± 122.6 | 442.38 ± 130.47 | 58.52 ± 110.94 | 377.5 ± 155.4 | 418.61 ± 124.37 | 41.16 ± 152.75 | 0.966 |
| Median | 381.0 | 433.0 | 39.0 | 365.50 | 416.00 | 55.0 | |
| Q1; Q3 | 284.0; 452.0 | 358.0; 536.0 | −10.0; 122.0 | 275.5; 440.0 | 338.0; 492.0 | −11.5; 129.0 | |
LVESV, left ventricular end-systolic volume; LVESD, left ventricular end-systolic diameter; LVEDV, left ventricular end-diastolic volume; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction.
Secondary endpoints
The percentage of ‘echo-responders’ defined by a reduction in LVESV >15% at 6 months was not different (50% in both groups) (P = 1.000) in the PP population. Subgroup analysis revealed that none of the following parameters [i.e. age, sex, NYHA class, cardiomyopathy aetiology, intrinsic or paced QRS width or pattern (left bundle block branch (LBBB) or non-LBBB), LVEF, LV volumes] were associated with a further LVESV reduction. None of the studied parameters could predict whether one RV lead position was superior to the other. The implant success rate based on pre-specified RV lead electrical criteria was not inferior in the RVS group when compared with the RVA group (90.0% in RVS vs. 86.8% in RVA; lower limit of 97.5% confidence interval = −3.36% > −9% threshold). This relative low percentage of fulfilled electrical criteria requirement was mainly due to the non-completion of the defibrillation test (DFT) (n = 27) that was mandatory in the study, but not performed by the investigator due to poor haemodynamic status in most cases. Excluding DFT non-completion, the total implant success rate was 99%, with no difference in the two groups. The RV lead procedural data are displayed in Tables 1 and 2. There was no significant change in RV lead characteristics (R wave amplitude, RV pacing threshold and impedance) throughout the follow-up. Procedural or device-related serious adverse events (SAEs) occurred in 68 patients (RVS, n = 37) with no difference between the two groups (P = 0.401). These SAEs were mainly related to the LV lead (n = 30, septal: n = 15). The most common LV lead-related SAE was the loss of LV capture (n = 16, septal = 9) requiring seven LV lead replacements, septal = 5), eight LV lead repositioning (septal = 4), and one reprogramming (apex). Right ventricular lead SAE occurred in seven patients, three in the septal group and in four in the apical group (P = 1.000).
At baseline, 6 MWT was similar between the two groups (356 ± 113 vs. 352 ± 115 m, RVS vs. RVA, P = 0.750) with a significant increase between baseline and 6 months in both groups (+28 ± 85 m, P < 0.0001) with no difference between the two groups (P = 0.648).
Although not significant (P = 0.056), there was a trend towards a higher percentage of improved patients according to the Milton Packer score in the RVS group (85%) vs. the RVA group (76%).24
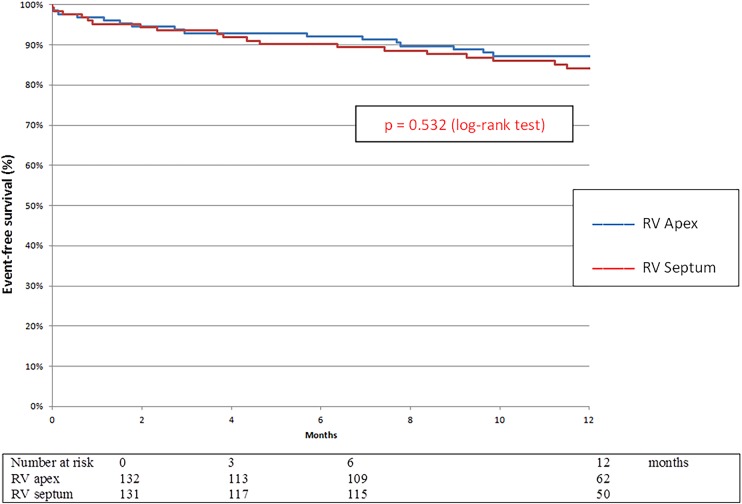
Nine patients died during the study, five in the RVS group and four in the RVA group (P = 0.749) (Table 5). The time to first HF hospitalization or death was not different between the two groups (P = 0.532) (Figure 3).
Figure 3.
Kaplan–Meier analysis of survival free from death and heart failure hospitalization in the right ventricular septum vs. right ventricular apex lead implantation group.
Discussion
This study demonstrates that RVS pacing in CRT is not inferior to RVA pacing for LV reverse remodelling with a similar reduction in the LVESV at 6 months. There was also no difference in the clinical outcome with an identical benefit in terms of 6 MWT and Milton Packer composite score. Finally, the composite endpoint including the time to first hospitalization for HF and total mortality was similar in both groups. Implantation success and complication rates were similar for both positions.
Cardiac resynchronization therapy is a widely accepted therapy for patients with LV systolic dysfunction and wide QRS complex.1 Clinical success and/or reverse LV remodelling can however only be achieved in 50–65% of patients. Among the potential solutions to increase this response rate, the optimal location of the RV lead remains a matter of debate. Apical RV lead position is conventional especially in patients receiving a CRT-D but there are convincing data on the harmful effects of long-term RV apical pacing.14,16
Several studies assessed the potential benefit of RVS pacing in patients with conventional PM indications, irrespective of LV function.1 The results of these studies are not uniform but there is a trend towards a beneficial effect of septal pacing. For example, de Cock et al.28 reported the haemodynamic effects of RV outflow tract pacing (septal pacing) in 217 patients included in 9 studies and found a significantly better haemodynamic effect (odds ratio 0.34, confidence interval 0.15, 0.53) of septal pacing compared with conventional RV pacing.
The feasibility and safety of septal ICD lead positioning have only been recently demonstrated in non-CRT patients. In a prospective study including 215 patients with ICD lead randomized to septal position or to apical position, Mabo et al.26 reported an identical implant success rate, based on strict electrical predefined criteria, in both groups (89.7% in the RVS group vs. 91.7% in the RVA group, P = 0.65) with no difference in the defibrillation success rate. In a similar non-CRT population, Kolb et al.,29 however, reported a tendency towards a higher defibrillation threshold in the mid-septal group. Our study confirms the feasibility of septal ICD RV lead implantation in a CRT population. Although non-significant, there was, however, a trend towards a prolongation in the total implant duration and fluoroscopic time in the septal group.
In CRT recipients, the results of alternative RV pacing sites, mainly septal, have recently been reported but the potential effects of the RV lead position are derived from post hoc analysis of large trials.12,30 Thebault et al.12 analysed the influence of RV and LV lead positions. A more favourable CRT outcome with regard to LV reverse remodelling and the composite of time to death or first HF hospitalization was observed when the LV lead was implanted in the lateral wall, away from the LV apex while no difference was observed between RV apical (n = 237) and RV non-apical (n = 108) lead position. Kutyifa et al.30 retrospectively analysed the influence of the RV lead position on the clinical outcome in 742 of the 1089 CRT patients (68%) included in the MADIT-CRT trial. Right ventricular lead position was classified as apical (n = 656) or non-apical (n = 86). There was no difference in the primary endpoint (HF or death) in patients with non-apical vs. patients with apical RV lead location (P = 0.983). However, a higher risk of VT/VF death (HR 2.45, P = 0.003) and VT/VF alone (HR 2.52, P = 0.002) predominantly in the first year after device implantation was reported with the non-apical lead position. Similar results with no difference between the two RV lead positions were also reported in small prospective non-randomized trials.10,17–21 Kristiansen et al.22 compared two RV lead locations in a prospective single-centre study. They included 85 consecutive CRT patients randomized to RV apex (n = 43) or high posterior septal (n = 42). They found no difference in terms of LV reverse remodelling at 6 months with a similar proportion of patients with a >15% reduction in LVESV in the RV high posterior septal group (n = 25, 64%) and in the RV apex group (n = 26, 65%) (P = 0.93). The results of the SEPTAL CRT study which included a larger population in a multicentre trial confirm these preliminary results. In other terms, from this study, it appears that in a general population, RV lead position does not appear to be of major importance. The implanting physician should thus implant the lead in the RV position he is the most familiar with. However, rather than an empiric predetermined (septal or apical) RV location, it could be hypothesized that the optimal RV lead location may also be tailored according to the LV position. Indeed, Merchant et al.31 found a significant correlation between LV–RV interlead distance and LV lead electrical delay with both parameters acting synergistically in predicting LV anatomic reverse remodelling. Miranda et al.32 prospectively assessed the influence of the RV lead in 50 patients randomized to apical or septal position, on the maximal electrical separation (MES) between the LV and RV leads. Interestingly, MES, commonly associated with a better clinical outcome, was significantly greater in the mid-septum (161 ± 23 ms) when compared with the apex (146 ± 26 ms) (P < 0.001), suggesting the potential favourable effects of chronic septal pacing in CRT recipients. Efforts to optimize both interlead distance and electrical delay may improve CRT outcomes.
Limitations
The SEPTAL CRT study has some limitations:
– There is a substantial amount of echocardiographic missing data, leading to incomplete results, especially for the primary endpoint. This underlines the difficulties of echo recordings and the feasibility of echo in CRT trials due to technical limitations. On the other hand, the results are strengthened by a core laboratory analysis, and a conservative method was used for the analysis with the Last Carry Forward Value method.
– The determination of the anatomical distance and electrical delay between the LV and the RV leads and their potential influences on the change in the LVESV were not prospectively assessed in the present study.
Conclusion
This study demonstrates that septal RV pacing in CRT is non-inferior to apical RV pacing for LV reverse remodelling at 6 months, with no difference in the clinical outcome. No recommendation for optimal RV lead position can hence be drawn from this study. Further prospective information about the anatomical and electrical relationships between RV and LV lead positions may be one of the next steps in the CRT research agenda.
Funding
Funding to pay the Open Access publication charges for this article was provided by Boston Scientific.
Conflict of interest: C.L. reports other from Boston Scientific, during the conduct of the study; personal fees from Boston Scientific, personal fees from Medtronic, personal fees from St. Jude Medical, outside the submitted work. N.S. reports other from Boston Scientific, during the conduct of the study; personal fees from Boston Scientific France, personal fees from Biotronik France, personal fees from Medtronic France, personal fees from St. Jude Medical France, personal fees from Sorin France, outside the submitted work. L.M. reports personal fees from St. Jude Medical, Sorin Group, Biotronik, Medtronic, Boston Scientific, Biosense Webster; grants from St. Jude Medical, Medtronic, Boston Scientific, Biotronik, outside the submitted work. E.M. reports as being employee of Boston Scientific. G.D. reports other from Boston Scientific, during the conduct of the study; non-financial support from Toshiba, other from Servier, personal fees from Sanofi, personal fees from Actelion, outside the submitted work. I.F.-L. reports personal fees from Boston Scientific, personal fees from St. Jude Medical, during the conduct of the study.
Acknowledgements
We acknowledge all of the investigators and research coordinators who participated to the SEPTAL CRT study, as well as those involved from Boston Scientific, including Marie Lambiez as international study coordinator, Maria Paz Lopez-Chicharro as Spanish study coordinator, Carmen Braban and Stephanie Gautier for their study support. We thank Florence Mercier and Colleen Delaney, biostatisticians, for their assistance and critical comments.
Appendix
The following institutions and investigators participated in the SEPTAL trial
French centres
Centre Hospitalier Universitaire Angers: Jean-Marc Dupuis MD, Frédéric Rouleau MD, Aude Tassin MD. Centre Hospitalier Universitaire Haut Levêque, Bordeaux: Pierre Bordachar MD, Jacques Clémenty MD, Stephane Lafitte MD, SylvanPloux MD, Patricia Reant MD, Philippe Ritter MD. Centre Hospitalier Universitaire, Grenoble: Pascal Defaye MD, Peggy Jacon MD, Blandine Mondesert MD, Carole Saunier MD, Estelle Vautrin MD. Centre Hospitalier Universitaire, Lille: Salem Kacet MD, Laurence Guedon-Moreau MD, Didier Klug MD, Claude Kouakam MD, Sylvestre Marechaux MD, Christelle Marquie MD, Anne Sophie Polge MD, Marjorie Richardson MD. Centre Hospitalier Universitaire Louis Pradel, Lyon: Philippe Chevallier MD, Brigitte De Breyne MD, Marcin M Lotek MD, Emilie Nonin MD, Julien Pineau MD. Centre Hospitalier Universitaire La Timone Marseille: Jean-Claude Deharo MD, Emilie Bastard MD, Frédéric Franceschi MD, Gilbert Habib MD, Christophe Jego MD, Eric Peyrouse MD, Sebastien Prevot MD. Hôpital Saint-Joseph, Marseille: Michel Bremondy MD, Jacques Faure MD, Ange Ferracci MD, Jean Lefevre MD, Andre Pisapia MD. Centre Hospitalier Universitaire, Montpellier: Jean-Marc Davy MD, Frederic Cransac MD, Tien Tri Cung MD, Frederic Georger MD, Jean-Luc Pasquie MD, Franck Raczka MD, Catherine Sportouch-Dukhan MD. Centre Hospitalier Universitaire, Nancy: Nicolas Sadoul MD, Hugues Blangy MD, Jean-François Bruntz MD, Luc Freysz MD, Laurent Groben MD, Olivier Huttin MD. Nouvelles Cliniques Nantaises, Nantes: Antoine Bammert MD, Marc Burban MD, Jean-Pierre Cebron MD, Daniel Gras MD. Centre Hospitalier Universitaire La Pitié Salpêtrière, Paris: Robert Frank MD, Guillaume Duthoit MD, Françoise Hidden-Lucet MD, Caroline Himbert MD, Richard Isnard MD, Jérôme Lacotte MD, Françoise Pousset MD, ThierryZerah MD. Centre Hospitalier Universitaire, Rennes: Christophe Leclercq MD, AnnaïkBellouin MD, Christophe CrocqMD, Christian Deplace MD, Erwan Donal MD, Cécile Hamon MD, Philippe Mabo MD, Olivier Romain MD, Aude Solnon MD. Centre Hospitalier Universitaire, Rouen: Anselme Frederic MD, Fabrice Bauer MD, Mathieu Bernard MD, Benedicte Godin MD, Baptiste Kurtz MD, Arnaud Savoure MD. Centre Cardiologique du Nord, Saint-Denis: Xavier Copie MD, Gilles Lascault MD, Olivier Paziaud MD, Olivier Piot MD, Thierry Touche MD. Centre Hospitalier Universitaire, Toulouse Marc Delay MD, Talia Chilon MD, Nicolas Detis MD, Alexandre Duparc MD, Aurélien Hebrard MD, Pierre Massabuau MD, Philippe Maury MD, Pierre Mondoly MD, Philippe Rumeau MD. Clinique Pasteur, Toulouse: Serge Boveda MD, Laurence Adrover MD, Nicolas Combes MD, Antoine Deplagne MD, ,Isabelle Marco-Baertich MD, Olivier Fondard MD.
Spanish centres
Hospital General Alicante: Juan Gabriel Martínez MD, José Luis Ibañez Criado MD, Diego Ortuño MD. H. Clinic i Provincial Barcelona: Lluis Mont MD, Antonio Berruezo MD, BeluEduard MD, Ana Martín MD, Franco M. Merschon MD, Marta Sitges MD, José María Tolosana MD, Bárbara Vidal MD. H. Valle Hebron, Barcelona: Angel Moya i Mitjans MD, Oscar Alcalde Rodriguez MD, José Fernando Rodriguez Palomares MD, Nuria Rivas MD, Gisela Teixidó MD. H. Puerta de Hierro Madrid: Ignacio Fernández Lozano MD, Maria Lorena Ruiz Bautista MD, Victor Castro MD, Miguel Angel Cavero MD, Carlos Gutierrez MD, Natalia Ros MD. H. Virgen de la Victoria, Malaga: Francisco Javier Alzueta Rodriguez MD, Fernando Cabrera MD, Alberto Barrera Cordero MD, José Luis Peña MD. H. de Valme Sevilla: Juan Lealdel Ojo Gonzáles MD, Mª Dolores Garcia Medina MD, Ricardo Pavón Jiménez MD, David Villagomez MD. H. Virgen de la Salud Toledo: Eduardo Castellanos Martinez MD, Juan Alcalá MD, Carolina Maicas MD, Miguel Angel Arias Palomares MD, Alberto Puchol MD. H. La Fé Valencia: Joaquim OscaAsensi MD, Anastasio Quesada Carmona MD, Mª José Sancho-Tello De Carranza MD, José Olagüe De Ros MD, Enrique Castro Pareja MD, Oscar Cano Pérez MD, Ana Osa Saez MD. H. Rio Hortega, Valladolid: Benito HerrerosGuilarte MD, Juan Francisco Muñoz San Jose MD, Teresa Myriam Pérez Sanz MD.
Independent event review committee
Damien Logeart, MD, Centre Hospitalier Universitaire Lariboisière, Paris, France.
Maria Lopez Gil MD, Hospital 12 de Octubre, Madrid, Spain
Lead position core lab
Christophe Leclercq MD, Centre Hospitalier Universitaire, Rennes, France; Ignacio Fernandez Lozano MD, H. Puerta de Hierro, Madrid, Spain.
Echo core lab
Genevieve Derumeaux MD, PhD, FESC, DHU A-TVB, HôpitalHenri-Mondor, Créteil, France.
References
- 1. Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Ole-A Breithardt O, Cleland J, Deharo JC, Delgado V, Elliott PM, Gorenek B, Israel CW, Leclercq C, Linde C, Mont L, Padeletti L, Sutton R, Vardas PE. 2013 ESCGuidelines on cardiac pacing and cardiac resynchronization therapy. The Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC).Developed in collaboration with the European Heart Rhythm Association (EHRA). 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. The Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC).Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J 2013;34:2281–2329. [DOI] [PubMed] [Google Scholar]
- 2. Cleland JGF, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, Tavazzi L, for the Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med 2005;352:1539–1549. [DOI] [PubMed] [Google Scholar]
- 3. Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, De Marco T, Carson P, DiCarlo L, Demets D, White BG, DeVries DW, Feldman AM, for the Comparison of Medical Therapy, Pacing, and Defibrillation in Heart Failure (COMPANION) Investigators. Cardiac-resynchronization therapy with or without an implantable defibrillation advanced chronic heart failure .N Engl J Med 2004;350:2140–2150. [DOI] [PubMed] [Google Scholar]
- 4. Tang AS, Wells GA, Talajic M, Arnold MO, Sheldon R, Connolly S, Hohnloser SH, Nichol G, Birnie DH, Sapp JL, Yee R, Healey JS, Rouleau JL. Cardiac-resynchronization therapy for mild-to-moderate heart failure .N Engl J Med 2010;363:2385–2395. [DOI] [PubMed] [Google Scholar]
- 5. Zareba W, Klein H, Cygankiewicz I, Hall WJ, McNitt S, Brown M, Cannom D, Daubert JP, Eldar M, Gold MR, Goldberger JJ, Goldenberg I, Lichstein E, Pitschner H, Rashtian M, Solomon S, Viskin S, Wang P, Moss AJ. Effectiveness of cardiac resynchronization therapy by QRS morphology in the Multicenter Automatic Defibrillator Implantation Trial-Cardiac Resynchronization Therapy (MADIT-CRT). Circulation 2011;123:1061–1072. [DOI] [PubMed] [Google Scholar]
- 6. Gervais R, Leclercq C, Shankar A, Jacobs S, Eiskjær H, Johannessen A, Freemantle N, Cleland JGF, Tavazzi L, Daubert C. Surface electrocardiogram to predict outcome in candidates for cardiac resynchronization therapy: a sub-analysis of the CARE-HF trial. Eur J Heart Fail 2009;11:699–705. [DOI] [PubMed] [Google Scholar]
- 7. Cleland JC, Abraham WT, Linde C, Gold MR, Young JB, Daubert JC, Sherfesee L, Wells GA, Tang ASL. An individual patient meta-analysis of five randomized trials assessing the effects of cardiac resynchronization therapy on morbidity and mortality in patients with symptomatic heart failure. Eur Heart J 2013;34:3547–3556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Burri H, Domenichini G, Sunthorn H, Fleury E, Stettler C, Foulkes I, Shah D. Right ventricular systolic function and cardiac resynchronization therapy. Europace 2010;12:389–394. [DOI] [PubMed] [Google Scholar]
- 9. Ypenburg C, van Bommel RJ, Delgado V, Mollema SA, Bleeker GB, Boersma E, Schalij MJ, Bax JJ. Optimal left ventricular lead position predicts reverse remodeling and survival after cardiac resynchronization therapy. J Am Coll Cardiol 2008;52:1402–1409. [DOI] [PubMed] [Google Scholar]
- 10. Khan FZ, Virdee MS, Palmer CR, Pugh PJ, Halloran DO, Elsik M, Read PA, Begley D, Fynn SP, Dutka DP. Targeted left ventricular lead placement to guide cardiac resynchronization therapy: the TARGET Study: a randomized, controlled trial. J Am Coll Cardiol 2012;59:1509–1518. [DOI] [PubMed] [Google Scholar]
- 11. Singh JP, Klein HU, Huang DT, Reek S, Kuniss M, Quesada A, Barsheshet A, Cannom D, Goldenberg I, McNitt S, Daubertert JP, Zareba W, Moss AJ. Left ventricular lead position and clinical outcome in the Multicenter Automatic Defibrillator Implantation Trial–Cardiac Resynchronization Therapy (MADIT-CRT) Trial. Circulation 2011;123:1159–1166. [DOI] [PubMed] [Google Scholar]
- 12. Thebault C, Donal E, Meunier C, Gervais R, Gerritse B, Gold MR, Abraham WT, Linde C, Daubert JC. Sites of left and right ventricular lead implantation and response to cardiac resynchronization therapy observations from the REVERSE trial. Eur Heart J 2012;33:2662–2671. [DOI] [PubMed] [Google Scholar]
- 13. Daubert JC, Saxon L, Adamson PB, Auricchio A, Berger RD, Beshai JF, Breithard O, Brignole M, Cleland J, Delurgio DB, Dickstein K, Exner DV, Gold M, Grimm RA, Hayes DL, Israel C, Leclercq C, Linde C, Lindenfeld J, Merkely B, Mont L, Murgatroyd F, Prinzen F, Saba SF, Shinbane JS, Singh J, Tang AS, Vardas PE, Wilkoff BL, Zamorano JL, Anand I, Blomstrom-Lundqvist C, Boehmer JP, Calkins H, Cazeau S, Delgado V, Estes NA, Haines D, Kusumoto F, Leyva P, Ruschitzka F, Stevenson LW, Torp-Pedersen CT. 2012 EHRA/HRS expert consensus statement on cardiac resynchronization therapy in heart failure: implant and follow-up recommendations and management. A registered branch of the European Society of Cardiology (ESC), and the Heart Rhythm Society; and in collaboration with the Heart Failure Society of America (HFSA), the American Society of Echocardiography (ASE), the American Heart Association (AHA), the European Association of Echocardiography (EAE) of the ESC and the Heart Failure Association of the ESC (HFA). Endorsed by the governing bodies of AHA, ASE, EAE, HFSA, HFA, EHRA, and HRS . Europace 2012;14:1236–1286.22930717 [Google Scholar]
- 14. Wilkoff BL, Cook JR, Epstein AE, Greene HL, Hallstrom AP, Hsia H, Kutalek SP, Sharma A. Dual chamber and VVI implantable defibrillator trial investigators. JAMA 2002;288:3115–3123. [DOI] [PubMed] [Google Scholar]
- 15. Barsheshet A, Moss AJ, McNitt S, Jons C, Glikson M, Klein HU, Huang DT, Steinberg JS, Brown MW, Zareba W, Goldenberg I, MADIT-II Executive Committee. Long-term implications of cumulative right ventricular pacing among patients with an implantable cardioverter-defibrillator. Heart Rhythm 2011;8:212–218. [DOI] [PubMed] [Google Scholar]
- 16. Steinberg JS, Fischer A, Wang P, Schuger C, Daubert J, Mcnitt S, Andrews M, Brown M, Hall WL, Zareba W, Moss AJ, for MADIT II investigators. The clinical implications of cumulative right ventricular pacing in the Multicenter Automatic Defibrillator Trial II. J Cardiovasc Electrophysiol 2005;16:359–365. [DOI] [PubMed] [Google Scholar]
- 17. Riedlbauchova L, Cihak R, Bytesnik J, Vancura V, Fridl P, Hoskova L, Kautzner J. Optimization of right ventricular lead position in cardiac resynchronisation therapy. Eur J Heart Fail 2006;8:609–614. [DOI] [PubMed] [Google Scholar]
- 18. Haghjoo M, Bonakdar HR, Jorat MV, Fazelifar AF, Alizadeh A, Ojaghi-Haghjghi Z, Esmaielzadeh M, Sadr-Ameli MA. Effect of right ventricular lead location on response to cardiac resynchronization therapy in patients with end-stage heart failure. Europace 2009;11:356–363. [DOI] [PubMed] [Google Scholar]
- 19. Hay I, Melenovsky V, Fetics BJ, Judge DP, Kramer A, Spinelli J, Reister C, Kass DA, Berger RD. Short-term effects of right-left heart sequential cardiac resynchronization in patients with heart failure, chronic atrial fibrillation, and atrioventricular nodal block. Circulation 2004;110:3404–3410. [DOI] [PubMed] [Google Scholar]
- 20. Bulava A, Lukl J. Similar long-term benefits conferred by apical versus mid-septal implantation of the right ventricular lead in recipients of cardiac resynchronization therapy systems. Pacing Clin Electrophysiol 2009;32:S32–S37. [DOI] [PubMed] [Google Scholar]
- 21. Shimano M, Inden Y, Yoshida Y, Tsuji Y, Tsuboi N, Okada T, Yamada T, Murakami Y, Takada Y, Hirayama H, Murohara T. Does RV Lead Positioning Provide Additional Benefit to Cardiac Resynchronization Therapy in Patients with Advanced Heart Failure? Pacing Clin Electrophysiol 2006;29:1069–1074. [DOI] [PubMed] [Google Scholar]
- 22. Kristiansen HM, Vollan G, Hovstad T, Keilegavlen H, Faerestrand S. A randomized study of haemodynamic effects and left ventricular dyssynchrony in right ventricular apical vs. high posterior septal pacing in cardiac resynchronization therapy. Eur J Heart Fail 2012;14:506–519. [DOI] [PubMed] [Google Scholar]
- 23. Packer M. Proposal for a new clinical end point to evaluate the efficacy of drugs and devices in the treatment of chronic heart failure. J Card Fail 2001;7:176–182. [DOI] [PubMed] [Google Scholar]
- 24. Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, Stromberg A, van Veldhuisen DJ, Atar D, Hoes AW, Keren A, Mebazaa A, Nieminen M, Priori SG, Swedberg K, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J 2008;29:2388–2442. [DOI] [PubMed] [Google Scholar]
- 25. Dickstein K, Vardas PE, Angelo Auricchio A, Daubert JC, Linde C, McMurray J, Ponikowski P, Priori SG, Sutton R, van Veldhuisen DJ. 2010 Focused Update of ESC guidelines on device therapy in heart failure An update of the 2008 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure and the 2007 ESC guidelines for cardiac and resynchronization therapyDeveloped with the special contribution of the Heart Failure Association and the European Heart Rhythm Association. Eur Heart J 2010;31:2677–2687. [DOI] [PubMed] [Google Scholar]
- 26. Mabo P, Defaye P, Mouton E, Cebron JP, Davy JM, Tassin A, Babuty D, Mondoly P, Paziaud O, Anselme F, Daubert JC. A randomized study of defibrillator lead implantations in the right ventricular mid-septum versus the apex: the SEPTAL study. J Cardiovasc Electrophysiol 2012;23:853–860. [DOI] [PubMed] [Google Scholar]
- 27. Ernande L, Bergerot C, Girerd N, Thibault H, Davidsen ES, Gautier Pignon-Blanc P, Amaz C, Croisille P, De Buyzere ML, Rietzschel ER, Gillebert TC, Moulin P, Altman M, Derumeaux G. Longitudinal myocardial strain alteration is associated with left ventricular remodeling in asymptomatic patients with type 2 diabetes mellitus. J Am Soc Echocardiogr 2014;24:479–487. [DOI] [PubMed] [Google Scholar]
- 28. de Cock CC, Giudici MC, Twisk JW. Comparison of the haemodynamic effects of right ventricular outflow-tract pacing with right ventricular apex pacing. A quantitative review. Europace 2003;5:275–278. [DOI] [PubMed] [Google Scholar]
- 29. Kolb C, Solzbach U, Biermann J, Semmler V, Kloppe A, Klein N, Lennerz C, Szendey I, Andrikopoulos G, Tzeis S, Asbach S, for the SPICE-investigators. Safety of mid-septal electrode placement in implantable cardioverter defibrillator recipients—results of the SPICE (Septal Positioning of ventricular ICD Electrodes) study. Int J Cardiol 2014;174:713–720. [DOI] [PubMed] [Google Scholar]
- 30. Kutyifa V, Bloch Thomsen PE, Huang DT, Rosero S, Tompkins C, Jons C, McNitt S, Polonsky B, Shah A, Merkely B, Solomon SD, Moss AJ, Zareba W, Klein HU. Impact of the right ventricular lead position on clinical outcome and on the incidence of ventricular tachyarrhythmias in patients with CRT-D. Heart Rhythm 2013;10:1770–1777. [DOI] [PubMed] [Google Scholar]
- 31. Merchant FM, Heist EK, Nandigam KV, Mulligan LJ, Blendea D, Riedl L, McCarty D, Orencole M, Picard MH, Ruskin JN, Singh JP. Interlead distance and left ventricular lead electrical delay predict reverse remodeling during cardiac resynchronization therapy. Pacing Clin Electrophysiol 2010;33:575–582. [DOI] [PubMed] [Google Scholar]
- 32. Miranda RI, Nault M, Johri A, Simpson CS, Michael KA, Abdollah H, Baranchuk A, Redfearn DP. Maximal electric separation-guided placement of right ventricular lead improves responders in cardiac resynchronization defibrillator therapy. Clinical Perspective Circ Arrhythm Electrophysiol 2012;5:927–932. [DOI] [PubMed] [Google Scholar]