Abstract
Objective
We assessed the cross-sectional relationships of self-reported current occupational exposures to solvents, metals, and pesticides with metabolic syndrome and its components among 7127 participants in the Hispanic Community Health Study/Study of Latinos.
Methods
Metabolic syndrome was defined as a clustering of abdominal obesity, high triglycerides, low high-density lipoprotein cholesterol, high blood pressure, and/ or high fasting glucose. Regression models that incorporated inverse probability of exposure weighting were used to estimate prevalence ratios.
Results
Solvent exposure was associated with a 32% higher prevalence of high blood pressure (95% confidence interval: 1.09 to 1.60) than participants not reporting exposure. No associations were observed for occupational exposures with abdominal obesity, high triglycerides, low high-density lipoprotein, or metabolic syndrome.
Conclusion
Our findings suggest that solvent exposure may be an important occupational risk factor for high blood pressure among Hispanics/Latinos in the United States.
BACKGROUND
Hispanic/Latino adults in the United States are over-represented in occupations that are considered high risk because of exposure to physical and chemical hazards.1,2 Hispanic/Latino workers, especially those foreign-born, may be especially vulnerable to occupational hazards due to low socioeconomic status and language barriers.3 Several studies have observed associations between occupational exposures to solvents,4,5 metals,6–8 and pesticides9,10 with cardiovascular disease risk factors and endpoints. For example, employees at a car manufacturing plant exposed to mixed organic solvents were found to have an increased prevalence of hypertension compared with office workers at the same plant.4 Other studies have observed associations of occupational exposure to solvents, metals, and pesticides in relation to insulin resistance and type 2 diabetes.11,12
Metabolic syndrome is a risk factor for cardiovascular disease13 and is characterized as the co-occurrence of insulin resistance, obesity, dyslipidemia, and hypertension.14 There is no single cause of metabolic syndrome, but several pathways have been identified, including mitochondrial defects, inflammation, and endothelial dysfunction.15,16 Studies suggest that occupational exposures may be associated with individual components of metabolic syndrome, although the underlying mechanisms are unclear. Metals, such as arsenic, cadmium, and lead, have been shown to either directly or indirectly cause oxidative stress, which promotes pancreatic islet cell dysfunction that can lead to insulin resistance.17,18 Other studies suggest that solvents and pesticides, in addition to metals, may be endocrine disruptors and lead to weight gain.19,20 Some pesticides have also been shown to induce insulin resistance through multiple mechanisms, including the formation of advanced glycation end products, accumulation of lipid metabolites, activation of inflammatory pathways, generation of oxidative stress, and increased biosynthesis of triglycerides.21 These occupational exposures have also been linked to changes in blood pressure.4,5,7,20
As the largest and fastest growing minority group in the U.S., the prevalence of occupational exposures to contaminants within the Hispanic/Latino population represents a significant issue for the public and occupational health of this workforce. Moreover, to our knowledge, these workplace hazards have not yet been systematically evaluated as risk factors for adverse cardiometabolic health. Therefore, in this study, we present the prevalence of occupational exposures to solvents, metals, and pesticides, and further assess cross-sectional associations with metabolic syndrome and its component factors among a large and diverse cohort of Hispanic/Latino adults in the U.S.
METHODS
Study Population
The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) is a prospective cohort study of 16,415 self-identified Hispanic/Latino adults, aged 18 to 74 years at enrollment. Participants were recruited using population-based multistage probability sampling of households within census blocks across 4 field centers (Bronx, NY; Chicago, IL; Miami, FL; and San Diego, CA). Details of sampling methods used have been published elsewhere, and sample weights reflect the probability of selection at each stage.22,23 Enrollment examinations were performed between 2008 and 2011. All study participants provided written informed consent, and all field centers, the coordinating center, central laboratories, and reading centers obtained approval from their respective institutional review boards. For the present study, we restricted our analyses to participants reporting current employment at the enrollment interview (n = 8156).
Exposure Assessment
An interviewer-administered occupational questionnaire designed to assess current work environments was administered to participants who indicated full-time or part-time employment. The questionnaire was administered in either English or Spanish, based upon the participants’ preference. The Spanish translation of the questionnaire was certified by an independent translator, and tested by focus groups at each field center. Specifically, participants were asked “At the job you currently work the majority of your work hours per week, how often are you exposed to any type of organic solvents, for example styrene, trichloroethylene, toluene, or xylene?” and “At the job you currently work the majority of your work hours per week, how often are you exposed to metals such as manganese, lead, or mercury?”. Responses were recorded as 0%, 25%, 50%, 75%, or 100% of the time or occasional. Due to data sparseness of responses, exposures to solvents and metals were dichotomized as exposed (reported occasional exposures or reported exposures between 25% and 100% of the time) or unexposed (reported exposures 0% of the time). If participants were unfamiliar with the given terms (eg, styrene), responses were recorded as none of the time. Participants were also asked, “In your current job(s), are you exposed to pesticides?”. Responses to this question were recorded as yes or no. Approximately 10% of participants reported they worked at least one secondary job, for an average of 15 hours per week; pesticide exposure was ascertained with respect to primary and secondary jobs.
Outcome Assessment
Participants underwent a standardized clinical examination at enrollment that included anthropometric and laboratory measurements performed by trained research technicians. Participants were asked to fast, abstain from smoking for 12 hours, and abstain from vigorous physical activity the morning of the clinical examination. Waist circumference was used to describe abdominal obesity and was measured at the uppermost lateral border of the right ilium using measuring tape and recorded to the nearest 0.1 cm. Participants were asked to sit for 5 minutes before taking three systolic and diastolic blood pressure measurements each at 1-minute intervals using an automated sphygmomanometer (Omron model HEM-907 XL; Omron Healthcare Inc., Bannockburn, IL). The averages of the second and third readings were used.
Fasting blood samples were collected and shipped to the HCHS/SOL Central Laboratory for processing. High-density lipoprotein cholesterol (HDL) was measured using a direct magnesium/dextran sulfate method (Roche Diagnostics, Indianapolis, IN). Serum triglycerides were measured via a Roche Modular P chemistry analyzer using a glycerol blanking enzymatic method. Fasting glucose was measured using a hexokinase enzymatic method (Roche Diagnostics). Participants were instructed to bring all medications taken in the past month (prescription and nonprescription) with them to the enrollment examination. Medications were scanned using Universal Product Code barcodes where available. Otherwise, medications were recorded using centralized manual coding. Medications were then inventoried and classified using a Master Drug Data Base (Medispan MDDB©).
Metabolic syndrome was defined as the presence of at least three of following five risk factors, based on the American Heart Association/National Heart, Lung, and Blood Institute 2009 Joint Scientific Statement (AHA/NHLBI) criteria13,24: abdominal obesity (waist circumference of ≥88 cm for women or ≥102 cm for men), high triglyceride levels (≥150 mg/dL), low HDL cholesterol levels (<50 mg/dL for women or < 40 mg/dL for men), high blood pressure (systolic blood pressure ≥130 mm Hg, diastolic blood pressure ≥85 mm Hg, or current use of medication to treat high blood pressure), or high fasting blood glucose levels (≥100 mg/dL or current use of medication to treat hyperglycemia).
Covariates
Sociodemographic, health behavior, and occupational covariates derived from the interviewer-administered enrollment questionnaire were included in our analyses. Hispanic/Latino background groups were categorized as Dominican, Central American, Cuban, Mexican, Puerto Rican, South American, and more than one heritage/other heritage. Nativity was categorized as birth within the U.S. (excluding territories) or outside of the U.S. Years of residence within the U.S. (excluding territories) and language preference (Spanish or English) were used as proxy measures for acculturation. Educational attainment was categorized as not having a high school diploma or GED, having a diploma or GED, or attaining an education beyond a high school equivalent (ie, college or vocational). Current health insurance coverage was assessed as coverage through an employer, individual plan, Medicaid/Medicare, military, Indian Health Services, or other coverage. Alcohol intake was categorized as none, low/moderate (defined as fewer than seven drinks per week for females or fewer than 14 drinks per week for males), or heavy (seven or more drinks per week for females or 14 or more drinks per week for males). Cigarette smoking status was categorized as never, former, or current. Cigarette pack-years were calculated as the number of years smoked multiplied by the average number of cigarettes smoked daily, divided by 20.
Full-time employment was defined as working more than 35 hours per week in one job or more than one job; part-time employment was defined as working 35 hours per week or fewer. The types of occupations ascertained in the HCHS/SOL were selected to reflect common occupational groups in the Hispanic/ Latino population, based on NIH-funded studies in developing countries. The occupations were categorized into five groups: nonskilled workers, service workers, skilled workers, professional/technical workers, and other. Participants were additionally asked to self-report their individual job titles.
Statistical Analyses
The weighted prevalence of current occupational exposures to solvents, metals, and pesticides, as well as metabolic syndrome and its individual components were calculated. The Rao–Scott Chi-squared test was used to compare occupational exposures and metabolic syndrome endpoints across categories.
To control for potential confounding, we used propensity score models to estimate the probability of self-reported occupational exposure to solvents, metals, or pesticides in the participant’s current job. Survey-weighted logistic regression models were defined a priori and included field center, age, sex, Hispanic/Latino background, country of birth, years residing in the U.S., educational attainment, language preference, alcohol use level, cigarette pack-years, smoking status, health insurance status, employment status (full- or part-time), and occupational group. Age and years residing in the U.S. were modeled using restricted cubic splines with four knots, at the 5th, 35th, 65th, and 95th percentiles to allow for nonlinearity and improve comparability between the exposed and unexposed.25 Cigarette pack-years was modeled as a continuous variable. Center, gender, Hispanic/Latino background, country of birth, educational attainment, health insurance status, language preference, smoking status, alcohol consumption level, employment status, and occupational group were modeled categorically using indicator variables.
Inverse probability of exposure weights was calculated using the predicted probabilities from the propensity score model. For participants currently occupationally exposed to solvents, metals, or pesticides, the inverse probability of exposure weight was equal to 1/probability of exposure. For participants not currently occupationally exposed to solvents, metals, or pesticides, the inverse probability of exposure weight was equal to 1/(1 − probability of exposure). Extreme inverse probability of exposure weights (ie, those below the 1st and above the 99th percentiles) was truncated. Analytic weights were then created by multiplying the inverse probability of exposure weights by the sampling weights.26 Balance between those exposed and unexposed was assessed using standardized differences, weighted by sampling weights and the analytic weights.27 Standardized differences less than 10% when using the analytic weights were considered to have an acceptable balance; in the event that a baseline covariate had a standardized difference greater than 10%, the covariate was additionally adjusted for in outcome models.
Prevalence ratios and their 95% confidence intervals (95% CIs) for metabolic syndrome and components were calculated using a modified Poisson regression model.28 Weighted means were calculated for continuous endpoints. The primary sampling unit, two-stage sampling design strata, and weights (sampling or analytic) were used in all analyses. As our hypotheses were specified a priori, we did not adjust for multiple comparisons. Finally, we coded self-reported job titles to a standard system (2010 Standard Occupational Classification, SOC 2010) using the Occupational Information Network (O*NET) database to further characterize the work of participants reporting occupational exposures of interest.29 Data management was performed using SAS 9.3 software (SAS Institute, Cary, NC), and all statistical analyses were conducted using Stata Statistical Software, Release 13 (StataCorp LP, College Station, TX).
RESULTS
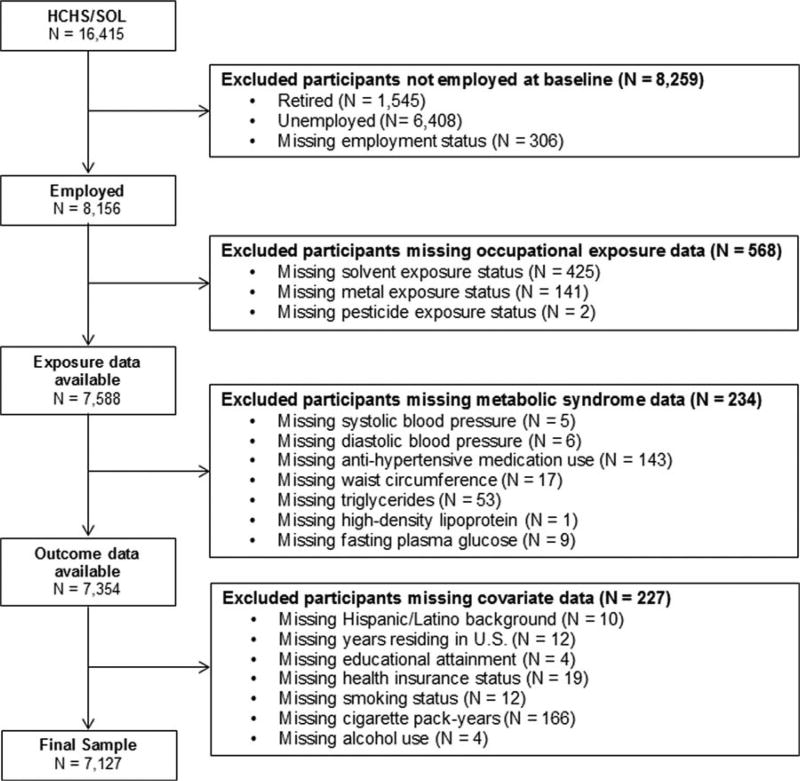
After excluding participants missing data on occupational exposures and other covariates, 7127 (weighted prevalence: 89.0%) of the 8156 participants who reported employment at the enrollment visit were included in analyses (Fig. 1). The weighted prevalence of metabolic syndrome and components among the selected study sample are summarized in Table 1. Abdominal obesity (49.2%) was the most common component of metabolic syndrome. The prevalence of high triglycerides, low HDL, high blood pressure, and high fasting glucose ranged from 26.9% to 38.4%. Metabolic syndrome was prevalent in 27.3% of participants.
FIGURE 1.
Inclusion/exclusion criteria flow diagram.
TABLE 1.
Selected Characteristics in Relation to Metabolic Syndrome Prevalence Among Participants Currently Employed in HCHS/SOL (n = 7,127)
| Abdominally Obese* |
High Triglycerides† |
Low HDL‡ |
High Blood Pressure§ |
High Fasting Glucose‖ |
Metabolic Syndrome¶ |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|||||||
| % | P | % | P | % | P | % | P | % | P | % | P | |
| Overall | 49.2 | 26.9 | 38.4 | 27.2 | 28.5 | 27.3 | ||||||
| Center | <0.01 | <0.01 | 0.09 | <0.01 | 0.45 | 0.02 | ||||||
| Bronx | 46.8 | 19.2 | 35.9 | 27.5 | 26.5 | 24.4 | ||||||
| Chicago | 45.5 | 28.6 | 42.0 | 19.7 | 29.5 | 24.7 | ||||||
| Miami | 49.0 | 29.4 | 39.4 | 33.2 | 29.4 | 29.6 | ||||||
| San Diego | 54.1 | 30.2 | 37.1 | 25.9 | 28.7 | 29.2 | ||||||
| Background | 0.04 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | ||||||
| Dominican | 51.6 | 12.0 | 30.9 | 31.1 | 20.8 | 20.9 | ||||||
| Central American | 48.3 | 33.2 | 42.3 | 26.0 | 25.4 | 27.6 | ||||||
| Cuban | 49.3 | 30.1 | 38.6 | 38.3 | 32.3 | 32.2 | ||||||
| Mexican | 50.6 | 29.1 | 39.6 | 22.9 | 30.6 | 27.6 | ||||||
| Puerto Rican | 49.0 | 22.8 | 40.7 | 31.3 | 29.2 | 29.0 | ||||||
| South American | 37.6 | 27.7 | 32.1 | 18.0 | 22.6 | 19.2 | ||||||
| Other/Mixed | 48.1 | 22.6 | 35.8 | 19.9 | 23.2 | 23.8 | ||||||
| Age, years | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | ||||||
| 18–24 | 33.5 | 10.4 | 34.5 | 7.5 | 11.6 | 7.4 | ||||||
| 25–34 | 43.2 | 22.3 | 40.0 | 13.7 | 17.7 | 18.3 | ||||||
| 35–44 | 53.2 | 32.7 | 42.7 | 23.8 | 30.9 | 30.9 | ||||||
| 45–54 | 55.6 | 34.3 | 37.3 | 39.5 | 37.5 | 36.6 | ||||||
| ≥55 | 60.8 | 31.9 | 33.5 | 62.8 | 50.0 | 45.8 | ||||||
| Gender | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | 0.39 | ||||||
| Female | 69.4 | 19.5 | 44.2 | 23.3 | 20.4 | 26.6 | ||||||
| Male | 32.5 | 32.9 | 33.5 | 30.4 | 35.2 | 27.8 | ||||||
| Country of Birth | 0.81 | <0.01 | 0.63 | <0.01 | <0.01 | <0.01 | ||||||
| U.S. (excluding territories) | 49.5 | 19.4 | 37.6 | 19.9 | 21.6 | 21.5 | ||||||
| Foreign | 49.0 | 28.9 | 38.6 | 29.3 | 30.4 | 28.9 | ||||||
| U.S. Residence Duration | <0.01 | 0.81 | 0.41 | <0.01 | 0.01 | <0.01 | ||||||
| <10 years | 40.8 | 27.2 | 37.2 | 23.9 | 25.5 | 23.4 | ||||||
| ≥10 years | 52.7 | 26.7 | 38.9 | 28.6 | 29.8 | 28.9 | ||||||
| Educational Attainment | 0.52 | <0.01 | 0.28 | <0.01 | <0.01 | <0.01 | ||||||
| No high school diploma/GED | 50.0 | 31.0 | 38.1 | 30.5 | 35.8 | 31.9 | ||||||
| High school diploma/GED | 47.5 | 25.4 | 40.4 | 23.1 | 26.6 | 24.4 | ||||||
| Greater than high school/GED | 49.7 | 25.4 | 37.2 | 27.9 | 25.5 | 26.3 | ||||||
| Current health insurance | 0.42 | <0.01 | 0.22 | 0.01 | 0.94 | 0.93 | ||||||
| No | 48.4 | 29.3 | 39.4 | 25.5 | 28.6 | 27.3 | ||||||
| Yes | 50.0 | 24.0 | 37.2 | 29.1 | 28.4 | 27.2 | ||||||
| Language preference | 0.85 | <0.01 | 0.29 | <0.01 | <0.01 | <0.01 | ||||||
| Spanish | 49.1 | 28.7 | 39.0 | 29.2 | 30.4 | 29.1 | ||||||
| English | 49.4 | 21.0 | 36.4 | 21.0 | 22.5 | 21.7 | ||||||
| Current alcohol intake | <0.01 | 0.14 | <0.01 | 0.08 | 0.96 | 0.17 | ||||||
| None | 53.9 | 25.3 | 42.6 | 27.9 | 28.6 | 28.6 | ||||||
| Low/Moderate | 45.4 | 27.6 | 35.8 | 26.0 | 28.3 | 25.9 | ||||||
| Heavy | 48.3 | 30.9 | 30.7 | 32.5 | 29.2 | 29.3 | ||||||
| smoking | 0.04 | <0.01 | 0.09 | <0.01 | <0.01 | <0.01 | ||||||
| Never | 50.2 | 23.6 | 38.6 | 24.9 | 25.6 | 24.6 | ||||||
| Former | 50.2 | 35.3 | 34.8 | 37.5 | 40.4 | 35.6 | ||||||
| Current | 44.4 | 30.9 | 40.9 | 25.8 | 27.8 | 29.0 | ||||||
| Cigarette pack-years | 0.18 | <0.01 | 0.35 | <0.01 | <0.01 | <0.01 | ||||||
| 0 | 50.2 | 23.6 | 38.6 | 24.9 | 25.6 | 24.6 | ||||||
| 1–9 | 48.0 | 31.5 | 36.6 | 25.7 | 30.7 | 28.5 | ||||||
| ≥10 | 45.7 | 36.2 | 40.6 | 43.2 | 40.5 | 39.8 | ||||||
| Employment status | <0.01 | <0.01 | 0.05 | <0.01 | <0.01 | 0.47 | ||||||
| Part-time (≤35 hours/week) | 54.1 | 23.9 | 40.7 | 23.6 | 24.1 | 26.5 | ||||||
| Full-time (>35 hours/week) | 46.6 | 28.4 | 37.2 | 29.1 | 30.8 | 27.7 | ||||||
| Occupation | <0.01 | 0.79 | 0.24 | 0.14 | 0.05 | 0.62 | ||||||
| Nonskilled worker | 47.9 | 26.9 | 41.0 | 25.1 | 29.4 | 26.8 | ||||||
| Service worker | 56.0 | 27.0 | 38.7 | 29.9 | 28.5 | 29.2 | ||||||
| Skilled worker | 45.5 | 28.0 | 36.4 | 28.3 | 31.6 | 27.8 | ||||||
| Professional/technical | 52.5 | 24.6 | 38.6 | 25.2 | 24.1 | 25.2 | ||||||
| Other | 45.6 | 26.9 | 36.1 | 27.7 | 26.6 | 26.9 | ||||||
Abdominal obesity was defined as a waist circumference ≥88 cm for women or ≥102 cm for men.
High triglycerides was defined as ≥150 mg/dL.
Low HDL was defined as <50 mg/dL for women or <40 mg/dL for men.
High blood pressure was defined as systolic blood pressure ≥130 mm Hg, diastolic blood pressure ≥85 mm Hg, or current use of medication to treat high blood pressure.
High fasting blood glucose was defined as ≥100 mg/dL or current use of medication to treat hyperglycemia.
Metabolic syndrome was defined using the AHA/NHLBI definition of meeting at least 3 of the 5 criteria (abdominal obesity, high triglycerides, low HDL, high blood pressure, or high fasting blood glucose).
Participant characteristics associated with occupational exposures are displayed in Table 2. The prevalence of self-reported current occupational exposure to solvents, metals, and pesticides was 6.3% (n = 484), 8.6% (n = 571), and 4.7% (n = 321), respectively. Individuals with the highest prevalence of self-reported exposure to solvents in their primary job included those from the Chicago field center, of Central American background, who were male, preferred speaking Spanish, consumed alcohol, were current smokers, worked full-time, and were employed as skilled workers. Occupational metal exposure was most prevalent among the Chicago field center, Mexican background, younger age (25 to 34 years old), male sex, high school graduate/GED, no health insurance, Spanish language preference, heavy alcohol consumer, current tobacco consumer, full-time worker, and skilled worker participants. Prevalence of pesticide exposure was significantly associated with the Bronx field center, other/mixed background, male sex, living in the U.S. for at least 10 years, having health insurance, low/ moderate alcohol consumption, and current smoking.
TABLE 2.
Selected Characteristics in Relation to Occupational Exposures Among Participants Currently Employed in HCHS/SOL (n = 7,127)
| Current Occupational Exposure | ||||||
|---|---|---|---|---|---|---|
|
|
||||||
| Solvents | Metals | Pesticides | ||||
|
|
|
|
||||
| % | P | % | P | % | P | |
| Overall | 6.3 | 8.6 | 4.7 | |||
| Center | <0.01 | <0.01 | <0.01 | |||
| Bronx | 4.6 | 7.9 | 6.6 | |||
| Chicago | 8.5 | 12.6 | 4.3 | |||
| Miami | 7.3 | 6.5 | 3.1 | |||
| San Diego | 5.3 | 8.7 | 4.8 | |||
| Background | 0.03 | 0.01 | 0.13 | |||
| Dominican | 4.7 | 7.5 | 5.8 | |||
| Central American | 9.2 | 9.5 | 4.2 | |||
| Cuban | 7.7 | 7.4 | 2.9 | |||
| Mexican | 6.3 | 10.4 | 4.7 | |||
| Puerto Rican | 4.8 | 7.4 | 6.3 | |||
| South American | 5.0 | 3.8 | 3.6 | |||
| Other/Mixed | 4.4 | 6.4 | 7.0 | |||
| age, years | 0.32 | <0.01 | 0.68 | |||
| 18–24 | 4.6 | 8.8 | 3.5 | |||
| 25–34 | 6.6 | 11.1 | 5.1 | |||
| 35–44 | 6.0 | 8.6 | 5.0 | |||
| 45–54 | 7.4 | 6.9 | 4.6 | |||
| ≥55 | 6.5 | 5.8 | 4.9 | |||
| Gender | <0.01 | <0.01 | <0.01 | |||
| Female | 2.8 | 3.5 | 2.8 | |||
| Male | 9.1 | 12.7 | 6.2 | |||
| Country of birth | 0.16 | 0.90 | 0.78 | |||
| U.S. (excluding territories) | 5.1 | 8.5 | 4.9 | |||
| Foreign | 6.6 | 8.6 | 4.6 | |||
| U.S. residence duration | 0.64 | 0.99 | 0.03 | |||
| <10 years | 6.0 | 8.6 | 3.5 | |||
| ≥10 years | 6.4 | 8.6 | 5.2 | |||
| Educational attainment | 0.24 | <0.01 | 0.36 | |||
| No high school diploma/GED | 7.0 | 10.2 | 5.7 | |||
| High school diploma/GED | 6.8 | 10.6 | 4.1 | |||
| Greater than high school/GED | 5.6 | 6.4 | 4.5 | |||
| Current health insurance | 0.11 | 0.02 | 0.03 | |||
| No | 6.9 | 9.6 | 3.9 | |||
| Yes | 5.7 | 7.4 | 5.6 | |||
| Language preference | <0.01 | 0.03 | 0.78 | |||
| Spanish | 6.9 | 9.1 | 4.6 | |||
| English | 4.5 | 6.9 | 4.9 | |||
| Current alcohol intake | 0.04 | <0.01 | <0.01 | |||
| None | 5.1 | 6.0 | 3.3 | |||
| Low/Moderate | 7.1 | 10.1 | 5.7 | |||
| Heavy | 7.2 | 12.9 | 5.6 | |||
| Smoking | 0.07 | <0.01 | 0.04 | |||
| Never | 5.7 | 7.6 | 4.2 | |||
| Former | 7.1 | 8.7 | 4.3 | |||
| Current | 7.8 | 12.0 | 7.0 | |||
| Cigarette pack-years | 0.05 | <0.01 | 0.15 | |||
| 0 | 5.7 | 7.6 | 4.2 | |||
| 1–9 | 7.3 | 11.4 | 5.2 | |||
| ≥10 | 7.8 | 8.4 | 6.6 | |||
| Employment status | <0.01 | <0.01 | 0.32 | |||
| Part-time (≤35 hours/week) | 4.3 | 6.3 | 4.2 | |||
| Full-time (>35 hours/week) | 7.4 | 9.7 | 4.9 | |||
| Occupation | <0.01 | <0.01 | 0.33 | |||
| Nonskilled worker | 7.1 | 10.5 | 5.0 | |||
| Service worker | 4.0 | 4.5 | 3.5 | |||
| Skilled worker | 9.7 | 12.3 | 4.7 | |||
| Professional/technical | 2.7 | 4.8 | 4.0 | |||
| Other | 6.1 | 8.2 | 6.1 | |||
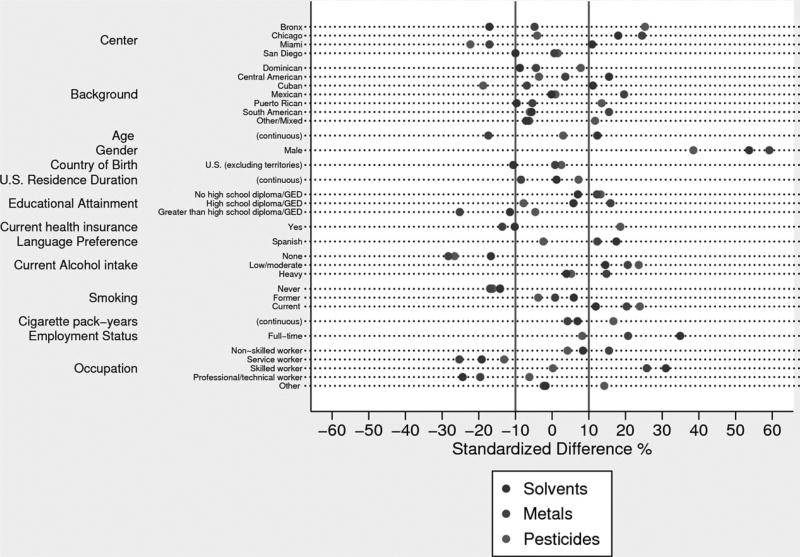
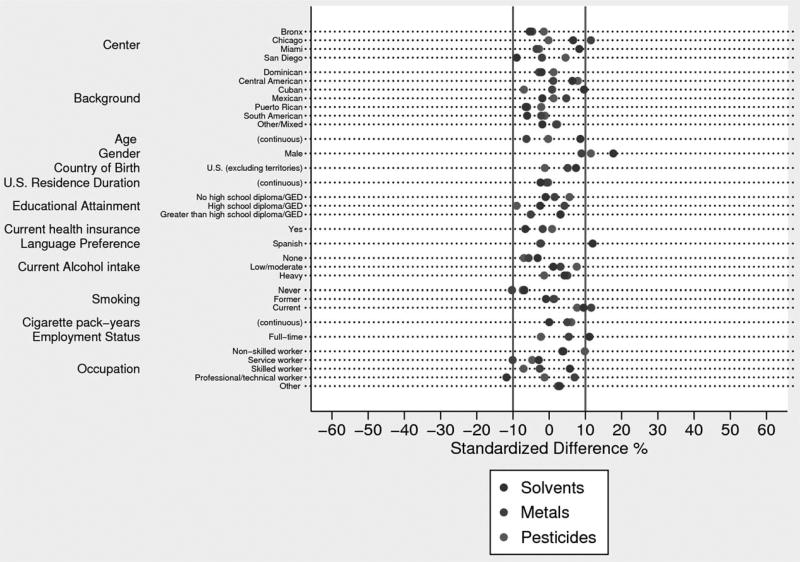
Standardized differences were used to assess balance in baseline covariates between those exposed and unexposed using sampling weights (Fig. 2) and analytic weights (Fig. 3). After implementing the analytic weights, the balance for most covariates was greatly improved (ie, <10%). As adjustments for covariates that had standardized differences greater than 10% (field center, sex, language preference, educational attainment, smoking status, employment status, and occupation) did not appreciably change our estimates, the presented results are unadjusted for residual confounders. We observed a significantly increased prevalence of high blood pressure (prevalence ratio = 1.32; 95% CI: 1.09 to 1.60) among individuals reporting occupational exposure to solvents (Table 3). This relationship was driven by higher systolic blood pressure among those reporting exposure to solvents (mean systolic blood pressure: 122 vs 119 mm Hg, Pe = 0.01) rather than diastolic blood pressure (mean diastolic blood pressure: 72 vs 72 mm Hg, P = 0.83) or differences in antihypertensive medication use (10.2% vs 8.6%, P = 0.33). All other cross-sectional associations between current occupational exposures to solvents, metals, and pesticides and metabolic syndrome and components were near null.
FIGURE 2.
Standardized differences of covariates using sample weights.
FIGURE 3.
Standardized differences of covariates using analytic weights.
TABLE 3.
Adjusted* Associations Between Current Occupational Exposures and Metabolic Syndrome Endpoints
| Abdominal Obesity† PR (95% CI) |
High Triglycerides‡ PR (95% CI) |
Low HDL§ PR (95% CI) |
High Blood Pressure‖ PR (95% CI) |
High Fasting Glucose¶ PR (95% CI) |
Metabolic Syndrome# PR (95% CI) |
|
|---|---|---|---|---|---|---|
| Solvents | 1.00 (0.85–1.16) | 1.00 (0.80–1.26) | 0.81 (0.66–1.00) | 1.32 (1.09–1.60) | 1.01 (0.82–1.26) | 0.95 (0.75–1.20) |
| Metals | 1.00 (0.88–1.14) | 1.04 (0.86–1.27) | 1.06 (0.90–1.24) | 1.04 (0.86–1.27) | 0.99 (0.80–1.22) | 1.07 (0.88–1.31) |
| Pesticides | 0.98 (0.82–1.16) | 1.03 (0.80–1.31) | 0.93 (0.74–1.18) | 1.02 (0.81–1.30) | 1.13 (0.92–1.39) | 1.09 (0.87–1.38) |
95% CI, 95% confidence interval.
Adjusted for confounders using the analytic weights.
Abdominal obesity was defined as a waist circumference ≥88 cm for women or ≥102 cm inches for men.
High triglycerides was defined as ≥150 mg/dL.
Low HDL was defined as <50 mg/dL for women or <40 mg/dL for men.
High blood pressure was defined as systolic blood pressure ≥130 mm Hg, diastolic blood pressure ≥85 mm Hg, or current use of medication to treat high blood pressure.
High fasting blood glucose was defined as ≥100 mg/dL or current use of medication to treat hyperglycemia.
Metabolic syndrome was defined using the AHA/NHBLI definition of meeting at least 3 of the 5 criteria (abdominal obesity, high triglycerides, low HDL, high blood pressure, or high fasting blood glucose).
Among the 484 participants who self-reported exposure to solvents in their current job, the 10 most common titles based on O*NET-SOC 2010 taxonomy were as follows: construction laborer (n = 50, 10.3%); maintenance and repair workers (n = 31, 6.4%); maids and housekeeping cleaners (n = 29, 6.0%); janitors and cleaners (n = 24, 4.9%); painters, construction, and maintenance (n = 20, 4.1%); automotive master mechanics (n = 19, 3.9%); carpenters (n = 13, 2.7%); production workers (n = 12, 2.5%); automotive body and related repairers (n = 11, 2.3%); and computer-controlled machine tool operators (n = 11, 2.3%). The remaining job titles and frequencies are provided in the Supplemental Digital Content (see Supplemental Table 1, http://links.lww.com/JOM/A353).
DISCUSSION
In this large, population-based study of Hispanic/Latino adults in the U.S., we observed a significantly elevated prevalence of high blood pressure among individuals reporting occupational exposure to solvents. Several prior studies have observed higher blood pressures among solvent-exposed workers than control groups across a variety of industries, including manufacturing and construction.4,5,30–33 While not specifically assessed within this study, exposure durations and intensities appear to be important factors with longer durations and higher levels of exposure commensurate with higher systolic blood pressures reported in the literature.5,30,33 Positive associations of solvent exposures with diastolic blood pressures have also been observed, although this relationship is less consistent than that of systolic blood pressures.4 Two small cross-sectional studies (n = 433; n = 471) conducted in Iran further assessed the associations of solvent exposures with fasting blood sugar and lipid profiles.4,5 Both found null associations with these endpoints, comporting with our observed results. To our knowledge, this is the first study to evaluate occupational exposures to solvents with cardiometabolic health within the U.S. Organic solvents are common in products such as paints, adhesives, glues, coatings, and degreasing/cleaning agents, and are routinely used in the production of dyes, polymers, plastics, textiles, printing inks, agricultural products, and pharmaceuticals; thus, workplace exposures may be important risk factors for high blood pressure among American workers.
In an effort to validate self-reported occupational exposure to solvents, we classified reported job titles based on the O*NET-SOC 2010 taxonomy. Among the HCHS/SOL participants who self-reported occupational exposure to solvents, individuals were most commonly employed in construction, maintenance, and housekeeping/janitorial jobs. Intensity ratings developed by O*NET, using data from the U.S. Department of Labor, suggest that these job environments have moderate-to-high levels of exposures to contaminants (ie, require working with pollutants, gases, dusts, or odors at least once a month).34 Therefore, we deem the self-reported exposure metric used in this analysis to be generally consistent with occupations having high likelihood of exposure to solvents.
Organic solvents represent a diverse group of chemicals with varying chemical structures and properties. They are often used in mixtures in industrial settings, rendering estimates of associated health effects difficult. The physiologic mechanisms by which solvent exposure could raise blood pressure are unclear. Animal studies suggest that solvents could inhibit endothelial nitric oxide synthase (eNOS).35 eNOS produces nitric oxide gas, an important regulator of vasorelaxation and consequently blood pressure.36 Alternatively, solvent exposure may cause changes in blood pressure through nephrotoxic effects and subsequent kidney damage.37
Our analysis has several important limitations. Occupational exposures to solvents, metals, and pesticides were qualitatively assessed through self-report, and may be subject to misclassification. However, it is likely that exposure misclassification was nondifferential, possibly resulting in underestimations of the underlying associations. Furthermore, the exposures were assessed as broad classes (solvents, metals, and pesticides), which did not enable us to evaluate the effects of specific compounds. We restricted our analyses to participants who were currently employed. This was done for practical reasons; unemployed and retired participants underwent a less detailed occupational interview due to survey skip patterns. Although these participants were asked about exposures to solvents/degreasers and pesticides in their longest held job, these data were not analyzed because of low response rates and concerns about recall bias. As a result of focusing on those employed at enrollment, our estimates may be further attenuated because of the healthy worker survivor effect. In addition, our data are cross-sectional precluding causal inferences. We specifically focused on chemical exposures in participants’ current job(s), which may not have entirely captured chronic exposures to solvents, metals, and pesticides or exposure from sources outside employment such as from dwellings. However, 69.6% of participants reported their current job was also their longest held job. Finally, we were unable to assess the dose–response relationships between exposures and metabolic syndrome because of sparse data.
Strengths of this study include the large and diverse population-based sample of Hispanics/Latinos, clinical assessments of metabolic syndrome components, and use of inverse probability weighting to control for confounding. Historically, studies of occupational health have largely ignored racial and ethnic minorities. Of the few occupational studies focused on Hispanic/Latino workers in the United States, most have been limited by industry or geographic location. The HCHS/SOL offered a unique opportunity to investigate associations between occupational exposures and metabolic syndrome, and the complex sampling design methodology used allows for the generalizability of findings to the U.S. Hispanic/Latino population aged 18 to 74 years living in the Bronx, Chicago, Miami, and San Diego.
CONCLUSION
This study examined cross-sectional associations of current occupational exposures to solvents, metals, and pesticides with metabolic syndrome and its components among a population-based cohort of Hispanics/Latinos in the U.S. Occupational exposure to solvents was associated with a greater prevalence of high blood pressure after controlling for potential confounders. Prospective analyses are needed to confirm these results.
Supplementary Material
Acknowledgments
The authors thank the staff and participants of HCHS/SOL for their important contributions (Investigators website: http://www.cscc.unc.edu/hchs/).
Catherine Bulka was supported by the National Heart, Lung, and Blood Institute (NHLBI) T32-HL125294. The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the NHLBI to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), University of Illinois at Chicago (HHSN268201300003I), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following Institutes/Centers/Offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: National Institute on Minority Health and Health Disparities, National Institute on Deafness and Other Communication Disorders, National Institute of Dental and Craniofacial Research, National Institute of Diabetes and Digestive and Kidney Diseases, National Institute of Neurological Disorders and Stroke, NIH Institution-Office of Dietary Supplements. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the U.S. Department of Health and Human Services.
Footnotes
The authors have no conflicts of interest.
Supplemental digital contents are available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal’s Web site (www.joem.org).
References
- 1.National Research Council, (U.S.) Committee on Communicating Occupational Safety and Health Information to Spanish-speaking Workers. Safety is Seguridad: a Workshop Summary. Washington, DC: National Academies Press; 2003. [Google Scholar]
- 2.Stanbury M, Rosenman KD. Occupational health disparities: a state public health-based approach. Am J Ind Med. 2014;57:596–604. doi: 10.1002/ajim.22292. [DOI] [PubMed] [Google Scholar]
- 3.Eamranond PP, Hu H. Environmental and occupational exposures in immigrant health. Environ Health Insights. 2008;1:45–50. doi: 10.4137/EHI.S847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Attarchi M, Golabadi M, Labbafinejad Y, Mohammadi S. Combined effects of exposure to occupational noise and mixed organic solvents on blood pressure in car manufacturing company workers. Am J Ind Med. 2013;56:243–251. doi: 10.1002/ajim.22086. [DOI] [PubMed] [Google Scholar]
- 5.Mohammadi S, Golabadi M, Labbafinejad Y, Pishgahhadian F, Attarchi M. Effects of exposure to mixed organic solvents on blood pressure in non-smoking women working in a pharmaceutical company. Arh Hig Rada Toksikol. 2012;63:161–169. doi: 10.2478/10004-1254-63-2012-2186. [DOI] [PubMed] [Google Scholar]
- 6.Li H, Hedmer M, Karedal M, et al. A cross-sectional study of the cardiovascular effects of welding fumes. PLoS One. 2015;10:e0131648. doi: 10.1371/journal.pone.0131648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Caciari T, Sancini A, Fioravanti M, et al. Cadmium and hypertension in exposed workers: a meta-analysis. Int J Occup Med Environ Health. 2013;26:440–456. doi: 10.2478/s13382-013-0111-5. [DOI] [PubMed] [Google Scholar]
- 8.Cavallari JM, Eisen EA, Fang SC, et al. PM2.5 metal exposures and nocturnal heart rate variability: a panel study of boilermaker construction workers. Environ Health. 2008;7:36. doi: 10.1186/1476-069X-7-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Charles LE, Burchfiel CM, Fekedulegn D, et al. Occupational exposure to pesticides, metals, and solvents: the impact on mortality rates in the Honolulu Heart Program. Work. 2010;37:205–215. doi: 10.3233/WOR-2010-1071. [DOI] [PubMed] [Google Scholar]
- 10.Hung DZ, Yang HJ, Li YF, et al. The long-term effects of organophosphates poisoning as a risk factor of CVDs: a nationwide population-based cohort study. PLoS One. 2015;10:e0137632. doi: 10.1371/journal.pone.0137632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Won YL, Ko Y, Heo KH, et al. The effects of long-term, low-level exposure to monocyclic aromatic hydrocarbons on worker’s insulin resistance. Saf Health Work. 2011;2:365–374. doi: 10.5491/SHAW.2011.2.4.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Montgomery MP, Kamel F, Saldana TM, Alavanja MC, Sandler DP. Incident diabetes and pesticide exposure among licensed pesticide applicators: Agricultural Health Study, 1993–2003. Am J Epidemiol. 2008;167:1235–1246. doi: 10.1093/aje/kwn028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 14.Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 15.Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365:1415–1428. doi: 10.1016/S0140-6736(05)66378-7. [DOI] [PubMed] [Google Scholar]
- 16.Soleimani M. Insulin resistance and hypertension: new insights. Kidney Int. 2015;87:497–499. doi: 10.1038/ki.2014.392. [DOI] [PubMed] [Google Scholar]
- 17.Chen YW, Yang CY, Huang CF, et al. Heavy metals, islet function and diabetes development. Islets. 2009;1:169–176. doi: 10.4161/isl.1.3.9262. [DOI] [PubMed] [Google Scholar]
- 18.Khan AR, Awan FR. Metals in the pathogenesis of type 2 diabetes. J Diabetes Metab Disord. 2014;13:16. doi: 10.1186/2251-6581-13-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mostafalou S, Abdollahi M. Pesticides and human chronic diseases: evidences, mechanisms, and perspectives. Toxicol Appl Pharmacol. 2013;268:157–177. doi: 10.1016/j.taap.2013.01.025. [DOI] [PubMed] [Google Scholar]
- 20.Morton WE, Crawford ED, Maricle RA, Douglas DD, Freed VH. Hypertension in Oregon pesticide-formulating workers. J Occup Med. 1975;17:182–185. [PubMed] [Google Scholar]
- 21.Lasram MM, Dhouib IB, Annabi A, El Fazaa S, Gharbi N. A review on the molecular mechanisms involved in insulin resistance induced by organo-phosphorus pesticides. Toxicology. 2014;322:1–13. doi: 10.1016/j.tox.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 22.Lavange LM, Kalsbeek WD, Sorlie PD, et al. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:642–649. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sorlie PD, Aviles-Santa LM, Wassertheil-Smoller S, et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:629–641. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grundy SM, Brewer HB, Jr, Cleeman JI, et al. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109:433–438. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 25.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dugoff EH, Schuler M, Stuart EA. Generalizing observational study results: applying propensity score methods to complex surveys. Health Serv Res. 2014;49:284–303. doi: 10.1111/1475-6773.12090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–3107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 29.National Center for O*NET Development. [Accessed February 28, 2017];O*NET OnLine. Available at: https://www.onetonline.org/
- 30.Kotseva K, Popov T. Study of the cardiovascular effects of occupational exposure to organic solvents. Int Arch Occup Environ Health. 1998;71(Suppl):S87–S91. [PubMed] [Google Scholar]
- 31.Chang TY, Wang VS, Hwang BF, et al. Effects of co-exposure to noise and mixture of organic solvents on blood pressure. J Occup Health. 2009;51:332–339. doi: 10.1539/joh.l8121. [DOI] [PubMed] [Google Scholar]
- 32.Kaukiainen A, Riala R, Martikainen R, et al. Solvent-related health effects among construction painters with decreasing exposure. Am J Ind Med. 2004;46:627–636. doi: 10.1002/ajim.20107. [DOI] [PubMed] [Google Scholar]
- 33.Kaukiainen A, Martikainen R, Luoma K, et al. Effect of industrial solvent exposure on blood pressure and liver ultrasound echogenicity. Scand J Work Env Hea. 2006:54–60. [Google Scholar]
- 34.National Center for O*NET Development. O*NET OnLine. Work Context: Exposed to Contaminants. Available at: https://www.onetonline.org/find/descriptor/result/4.C.2.b.1.d?r=1.
- 35.Sun Y, Iemitsu M, Shimojo N, et al. 2,4,6-Trinitrotoluene inhibits endothelial nitric oxide synthase activity and elevates blood pressure in rats. Arch Toxicol. 2005;79:705–710. doi: 10.1007/s00204-005-0003-y. [DOI] [PubMed] [Google Scholar]
- 36.Dharmashankar K, Widlansky ME. Vascular endothelial function and hypertension: insights and directions. Curr Hypertens Rep. 2010;12:448–455. doi: 10.1007/s11906-010-0150-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jacob S, Hery M, Protois JC, Rossert J, Stengel B. Effect of organic solvent exposure on chronic kidney disease progression: the GN-PROGRESS cohort study. J Am Soc Nephrol. 2007;18:274–281. doi: 10.1681/ASN.2006060652. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.