Abstract
Mycobacterium species are a significant cause of morbidity and mortality worldwide. The present study was carried out to systematically evaluate the accuracy of Matrix-assisted laser desorption ionization–time of flight mass spectroscopy (MALDI-TOF MS) for the identification of clinical pathogenic mycobacteria. After a rigid selection process, 19 articles involving 2,593 mycobacteria isolates were included. The pooled result agreed with the reference method identification for 85% of the isolates to genus level, with 71% (95% CI of 69% to 72%) correct to the species level. The MALDI-TOF MS correctly identified 92% of the M.tuberculosis isolates (95% CI of 0.87 to 0.96), and 68% of M. bovisisolates (95% CI of 27% to 100%) to the species level. Mycobacterium tuberculosis complex in solid media with reference strains using augmented database showing more accurate identification. The identifying accuracy rate of bioMérieuxVitek MS was slight higher than Bruker MALDI Biotyper (75% vs 72%). However, opposite results were obtained in identifications of M. fortuitum, M. kansasii, M. marinum, and M. terrae with these two systems. In summary, our results demonstrate that application of MALDI-TOF MS in clinical pathogenic mycobacteria identification is less satisfactory to date. Increasing need for improvement is important especially at species level.
Introduction
Mycobacteria are group of pathogens that can cause a wide spectrum of pulmonary and extra-pulmonary infections1,2, which continue to be a major public health concern in developing and industrialized countries. Mycobacterium tuberculosis complex (MTC) remains the major causes of morbidity and mortality3, while non-tuberculous mycobacteria (NTM), are frequent primary or opportunistic pathogens, causing pulmonary infection and lymphadenitis in children, skin disease and other extra-pulmonary infections in immune-compromised individuals4,5. Early species- or complex-level identification is of utmost importance to differentiate tuberculosis-causing mycobacteria, for epidemiological, public health, and therapeutic reasons.
Conventionally, identification of mycobacteria has been based on well-established phenotypic traits and biochemical profiles. Regardless of improved culture methods, it’s still time-consuming and difficult for identification of less common species. Recently, molecular assays, including PCR sequencing, and PCR hybridization, have been shown to support phenotypic identification methods or as an additional test performed directly on clinical specimens to enable rapid identification6,7. Although these methods are highly specific and greatly improve the turnaround time to identification; evaluations of molecular assays have generally been shown to be restricted to a limited number of Mycobacterium species, show variable sensitivity and labor-intensity8. So then sequencing of other genomic regions or the whole genome is necessary for complete genotyping. However, it is technically demanding and relatively expensive but rapidly decreasing in cost. According to the limitations encountered with currently available methods for identification, an alternative strategy may become necessary for clinical laboratories to overcome this hurdle.
Matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS) is a new type of soft ionization mass spectrometry. An increasing number of clinical microbiological laboratories consider it as an innovative approach for bacterial identification. Our previous study evaluated the use of MALDI-TOF MS for rapid identification of the clinical streptococci9. As regards the identification of mycobacteria, lots of studies have identified matrix-assisted laser desorption ionization–time of flight mass spectrometry (MALDI-TOF MS) as a powerful, rapid, and cost-effective method10–14. However, those reports differed in types of isolation medium, extraction protocols and libraries used. Additionally, many studies only included a few strains, and some had inconsistent results. The purpose of this study was to evaluate the robust accuracy of MALDI-TOF MS using different systems and culture medium to identify clinically pathogenic mycobacteria to genus and species level, respectively, by performing a meta-analysis that combines a large number of studies to define the reliability of MALDI-TOF MS for this purpose.
Results
Eligible studies
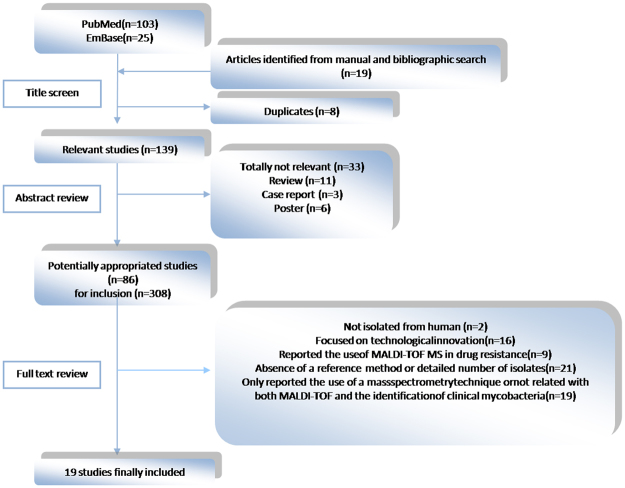
After a comprehensive literature search, 128 items were obtained by searching PubMed and EmBase with defined retrieval strings. After manual search and duplicate removal, a total of 86 articles remained for full-text scanning after title and abstract review. Among the excluded articles, 33 were excluded because they were not pertinent to the present study, including 3 case reports, 11 reviews and 6 posters. After the papers were screened, 2 studies were excluded because organisms were not isolated from humans; 16 were discarded as a result of technological innovation; 9 were excluded because they concerned identification of drug resistance; 21 were rejected because of the lack of reference method or detailed description of isolates; 19 were excluded because they reported mass spectrometry technique other than MALDI-TOF or because the identification of clinical mycobacteria were unrelated. As a result, 19 articles were included in this meta-analysis (Fig. 1).
Figrue 1.
Flow diagram for systematic literature search.
Supplementary Table S1 showed the major characteristics of the enrolled studies. Among the 19 studies, two were prospective15,16. Six studies17–22 included reference strains, while other studies used only clinical isolates. Seven reports expanded an existing database by establishing reference spectra for clinical isolates15–17,20,23–25, while others used the databases from instrument suppliers. Only two articles clearly stated that a blinded method was used for their investigation18,20. The others did not specify use of a blinded method. Ten articles focused on identification of mycobacteria from solid cultures, while four incorporated both liquid and solid media cultures in the routine clinical microbiology setting17,19,26,27. Four studies evaluated the performance both of the Bruker Biotyper and Vitek MS MALDI-TOF MS systems for the identification of Mycobacterium24,28–30, while the others investigated only one or the other31–33.
Overall meta-analysis
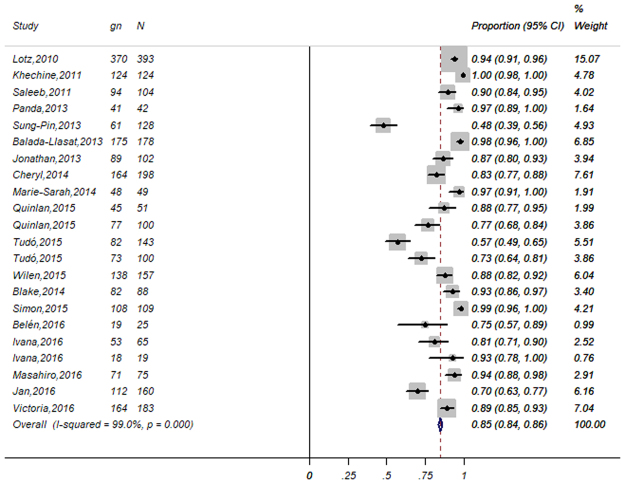
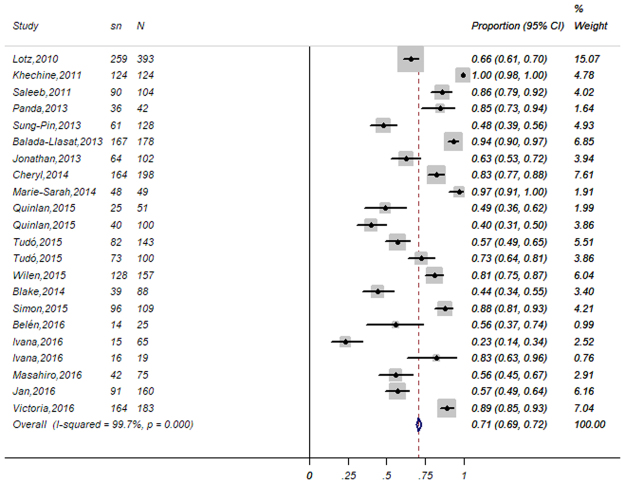
In the 19 enrolled studies, a total of 2,593 mycobacteria isolates were assessed. The overall statistical results of the meta-analysis at the genus and species level identification were summarized by forest plots of random-effects model (Figs 2 and 3). The gross correct identification ratios of MALDI-TOFMS for clinical mycobacteria ranged from 48% to 100% at the genus level and from 23% to 100% at the species level. Significant heterogeneity was found both at the genus level (P < 0.001; I2 = 99%) and the species level (P < 0.001; I2 = 99.7%). Of these, 2034 (85%; 95% CI of 84% to 0.86%) were correctly identified to the genus level while 1,841 (71%; 95% CI of 69% to 73%) were correctly identified to the species level by MALDI-TOF MS with random-effects model.
Figure 2.
Forest plot for the meta-analysis of the gross identification ratio at the genus level. CI, confidence interval; W, weight; gn, number of correct identifications; N, total number of identifications.
Figure 3.
Forest plot for the meta-analysis of the gross identification ratio at the species level. CI, confidence interval; W, weight; sn, number of correct identifications; N, total number of identifications.
The pooled identification results of MALDI-TOF MS by random-effects for the majority of Mycobacterium species was shown in Table 1. M. tuberculosis, the most important cause of tuberculosis, showed a high identification proportion at 92% with a 95% CI of 87% to 96%. As another member of MTC, M.bovis had a moderate identification proportion at 68% with a 95% CI of 27% to 100%. In NTM family, identification accuracy of M. haemophilum was the highest at 93% with a 95% CI of 87% to 100%, followed by M. marinum, M. fortuitum, M. peregrinum, M. xenopi, M. immunogenum, M. gordonae, M. smegmatis, M. abscessus, M. mucogenicum, M. kansasii and M. aviumwith an identification proportion above 80%. Identification accuracy of M. chelonae and M. lentiflavum and M. simiae were similar with an overall correct identification ratio at 70%. The lowest performance of MALDI-TOF MS was in M. malmoense and M. phlei, at ≤50%. Approximately 60% of M. intracellulare, M. maesiliense, M. neoaurum, M. parascrofulaceum, M. scrofulaceum and M. szulgai were correctly identified to the species level.
Table 1.
identification accuracy rate of common species.
| Proportion | 95%CI | Weight% | |
|---|---|---|---|
| M. tuberculosis | 0.92 | 0.87–0.96 | 5.75 |
| M. bovis | 0.68 | 0.27–1.00 | 1.15 |
| M. abscessus | 0.82 | 0.75–0.88 | 7.64 |
| M. avium | 0.80 | 0.69–0.91 | 6.41 |
| M. chelonae | 0.78 | 0.69–0.86 | 6.61 |
| M. fortuitum | 0.88 | 0.83–0.93 | 7.22 |
| M. gordonae | 0.84 | 0.78–0.90 | 6.48 |
| M. haemophilum | 0.93 | 0.87–1.00 | 2.93 |
| M. intracellulare | 0.55 | 0.34–0.76 | 4.39 |
| M. immunogenum | 0.86 | 0.75–0.98 | 2.64 |
| M. kansasii | 0.81 | 0.75–0.88 | 6.52 |
| M. lentiflavum | 0.74 | 0.52–0.95 | 2.37 |
| M. marinum | 0.92 | 0.86–0.98 | 4.64 |
| M. malmoense | 0.42 | 0.13–0.71 | 1.59 |
| M. maesiliense | 0.54 | 0.09–0.99 | 1.50 |
| M. mucogenicum | 0.82 | 0.73–0.91 | 4.13 |
| M. neoaurum | 0.66 | 0.43–0.89 | 2.34 |
| M. parascrofulaceum | 0.68 | 0.00–0.15 | 1.87 |
| M. peregrinum | 0.88 | 0.80–0.97 | 2.03 |
| M. phlei | 0.40 | 0.13–0.68 | 2.03 |
| M. scrofulaceum | 0.69 | 0.51–0.88 | 3.16 |
| M. smegmatis | 0.84 | 0.75–0.94 | 2.91 |
| M. simiae | 0.74 | 0.61–0.86 | 4.13 |
| M. szulgai | 0.69 | 0.53–0.86 | 3.77 |
| M. xenopi | 0.87 | 0.80–0.94 | 5.78 |
| Total | 0.74 | 0.71–0.79 | 100 |
Subgroup meta-analyses
The heterogeneity and random-effects pooled ratios of subgroup analyses performed at the species level according to strain source (clinical isolates only or reference strains also), system database (commercial database only or self-established database also), system (Bruker MALDI Biotyper and the bioMérieuxVitek MS), culture media(liquid or solid), growth rate (fast or slow) and category of strain (MTC or NTM) are shown in Table 2. The correct identification ratios of MTC at the species level was 90% (95% CI of 86% to 94%), obviously higher than NTM groups at 74% with a 95% CI of 71% to 79%. The correct identification of bioMérieuxVitek MS slightly exceeded Bruker MALDI Biotyper (75% vs 72%), especially in the identification of M. abscessus, M. avium, M. chelonae, M. immunogenum, M. intracellulare, M. mucogenicum, M. scrofulaceum, M. simiae and M. szulgai, as shown in Table 3. No significant difference was observed between rapid and slow growing isolates, similar to the correct identification performances of overall meta-analysis. The correct identification performances of the sub-analyses on isolates on solid culture media, with reference strains and self-established database added outcomes were superior to the gross ratio in our meta-analysis and their respective compared group. However, the heterogeneity was not obviously decreased in subgroup meta-analyses.
Table 2.
The heterogeneity and pooled correct identification ratios in subgroup analysis.
| Subanalysis | No. of isolates | Within-group heterogeneity | Correct identification ratio (95%CI) | |
|---|---|---|---|---|
| P | I 2 | |||
| System database | ||||
| Commercial database only | 1299 | <0.001 | 98.0% | 0.70(0.61–0.78) |
| Commercial database plus self-established database | 1212 | <0.001 | 96.8% | 0.82(0.72–0.92) |
| Source of strain | ||||
| Clinical isolates only | 1746 | <0.001 | 96.8% | 0.67(0.557–0.78) |
| Clinical isolates plus reference strains | 765 | <0.001 | 98.5% | 0.77(0.63–0.91) |
| Culture media | ||||
| liquid | 458 | <0.001 | 85.4% | 0.57(0.45–0.68) |
| solid | 1734 | <0.001 | 95.3% | 0.70(0.59–0.74) |
| Growth rate | ||||
| fast | 1119 | <0.001 | 91.9% | 0.75(0.71–0.80) |
| slow | 1392 | <0.001 | 93.4% | 0.76(0.73–0.79) |
| Category of strain | ||||
| MTC | 454 | <0.001 | 91.9% | 0.90(0.86–0.94) |
| NTM | 2057 | <0.001 | 97.9% | 0.74(0.71–0.79) |
| System | ||||
| Bruker MALDI Biotyper | 1801 | <0.001 | 91.8% | 0.72(0.62–0.81) |
| bioMérieux Vitek MS | 786 | <0.001 | 95.4% | 0.75(0.68–0.82) |
Table 3.
comparison accuracy rate of two systems.
| Species | System | |
|---|---|---|
| Bruker MALDI Biotyper | bioMérieux Vitek MS | |
| M. abscessus | 0.98(0.95–1.00) | 0.75(0.64–0.86) |
| M. avium | 0.96(0.91–1.00) | 0.74(0.63–0.85) |
| M. chelonae | 0.97(0.93–1.00) | 0.68(0.52–0.84) |
| M. fortuitum | 0.85(0.72–0.99) | 0.94(0.91–0.98) |
| M. gordonae | 0.79(0.66–0.92) | 0.77(0.66–0.87) |
| M. haemophilum | 0.95(0.85–1.00) | 0.93(0.81–1.00) |
| M. immunogenum | 0.92(0.81–1.00) | 0.81(0.59–1.00) |
| M. intracellulare | 0.77(0.59–0.95) | 0.63(0.43–0.84) |
| M. kansasii | 0.59(0.14–1.00) | 0.71(0.58–0.84) |
| M. marinum | 0.88(0.73–1.00) | 0.96(0.91–1.00) |
| M. mucogenicum | 0.95(0.88–1.00) | 0.65(0.47–0.83) |
| M. scrofulaceum | 0.75(0.56–0.93) | 0.32(0.00–0.67) |
| M. simiae | 0.75(0.61–0.99) | 0.61(0.28–0.94) |
| M. szulgai | 0.75(0.61–0.99) | 0.55(0.30–0.80) |
| M. terrae | 0.33(0.00–0.65) | 0.46(0.15–0.61) |
| M. xenopi | 0.82(0.59–1.00) | 0.77(0.65–0.88) |
Common misidentification pattern in these studies
Some species were not differentiated from each other very well by existing MALDI-TOF MS systems and commercial or laboratory-established databases including M. abscessus and M. massiliense, M. fortuitum and M. septicum, M. mucogenicum and M. phocaicum, M. parascrofulaceum and M. scrofulaceum (Table 4).
Table 4.
Common misidentification pattern in these studies.
| Sequence identification | MALDI-TOF MS identification | System | Reference |
|---|---|---|---|
| M. abscessus | M. massiliense | Bruker MALDI Biotyper | 20,23 |
| M. tuberculosis | Bruker MALDI Biotyper | 16 | |
| M aubagnense | M phocaicum | Bruker MALDI Biotyper | 27 |
| M. avium | M. intracellulare | Bruker MALDI Biotyper | 26 |
| M. chelonae | M. immunogenum/M. abscessus | Bruker MALDI Biotyper | 29 |
| M. chimaera | M. intracellulare | Bruker MALDI Biotyper | 23 |
| M. europaeum | M. scrofulaceum | bioMérieux Vitek MS | 24 |
| M. fortuitum | M. septicum | Bruker MALDI Biotyper | 19,26 |
| M. abscessus/M. chelonae | Bruker MALDI Biotyper | 19 | |
| M. franklinii | M. chelonae | bioMérieux Vitek MS | 16 |
| M. intracellulare | M. avium/M. abscessus | Bruker MALDI Biotyper | 16 |
| M.chimaera | Bruker MALDI Biotyper | 26 | |
| M. immunogenum | M abscessus | Bruker MALDI Biotyper | 27 |
| M. llatzerense | M phocaicum | Bruker MALDI Biotyper | 27 |
| M. malmoense | M. tuberculosis | Bruker MALDI Biotyper | 16 |
| M mucogenicum | M phocaicum | Bruker MALDI Biotyper | 19,23,27 |
| M. nebraskensec | M. avium | Bruker MALDI Biotyper | 28 |
| M. novocastrense | M. austro/M. africanum | Bruker MALDI Biotyper | 28 |
| M. paraffinicumc | M. bovis/M. avium/M. intracellulare | Bruker MALDI Biotyper | 28 |
| M. parascrofulaceum | M. scrofulaceum | Bruker MALDI Biotyper/ bioMérieux Vitek MS | 29 |
| M. avium | Bruker MALDI Biotyper | 28 | |
| M phocaicum | M mucogenicum | Bruker MALDI Biotyper | 27 |
| M porcinum | M. peregrinum/M conceptionense/M fortuitum | Bruker MALDI Biotyper | 27 |
| M pseudoshottsii | M. marinum | Bruker MALDI Biotyper | 27 |
| M. terrae | M. arupense | bioMérieux Vitek MS | 24 |
| M. tusciae | M. vaccae | Bruker MALDI Biotyper | 28 |
Assessment of publication bias and influence analysis
Little publication bias was detected at the species level by Begg rank correlation (with continuity correction) and Egger’s linear regression test of funnel plot asymmetry in this meta-analysis (z = −0.90 and P = 0.367 for Begg; t = −0.70 and P = 0.492 for Egger’s, see Supplementary Fig. S1).
Influence analysis showed that no individual study had any obvious influence on the combined gross ratio at the species level (see Supplementary Fig. S2).
Discussion
As an recent technology for the clinical identification of microorganisms, MALDI-TOF MS has many advantages over other current methods34. In this study, we performed a systematic review and meta-analysis of the current literature assessing diagnostic performance of MALDI-TOF MS in clinical applications. According to the inclusion and exclusion criteria, a total of 19 related articles were used in this review. The pooled result agreed with the reference method was 85% identification of the isolates to genus level, and 71% to the species level respectively, which still cannot meet with the need of clinical microbiology diagnostics so far. In these articles, we mainly focused on 25 mycobacterial species that are frequently isolated in clinical microbiology laboratories. The pooled identification ratio of these species was 74% with a 95% CI of 71% to 79%. Many reports have demonstrated the application of MALDI-TOF mass spectrometry in clinical diagnostic microbiology, including anaerobic bacteria, enterobacteriaceae, gram-positive aerobic bacteria, non-enterobacteriaceae gram-negative bacilli, yeasts and so on, showing correct identification ratio at species level above 77%35–39. Our previous study showed that MALDI-TOF MS correctly identified 96% of the streptococci and 99% of the Streptococcus pneumonia to species level9, much higher than the performance for mycobacteria in this study. In contrast to other bacteria, the cell walls of mycobacterial species contain variable amounts of mycolic acids, resulting in awaxy, hydrophobic structure40. Some of the studies included in this evaluation analyzed whole cells, while others followed the cell extracts procedure. It should be noted that different cell extract procedures would impact the MS spectra generated, leading to inconsistencies within databases and poorer identification performance. In addition to cell extraction procedures, identification ratios of MALDI-TOF MS can be affected by other variables (e.g., the grow rate of strain, the proportion of clinical and reference species, or the culture media) that were revealed by heterogeneity in subgroup analysis.
According to our results, no notable differences in the overall identification rates between rapid slowly-growing mycobcteria. A high number of replicates increase the probability of correct identification, especially for slowly-growing mycobacteria. In some cases, five replicates were required to obtain one good spectral acquisition17. The identification accuracy of MTC was higher than NTM partially because most studies were more interested in MTC. As frequently detected pathogenic Mycobacterium species, MTC have a facility for protein profile acquisition in existing databases, leading to more accurate identification than for NTM. Since NTM are attracting attention due to increase in the isolation frequency, especially in the countries with declining tuberculosis incidence41, the identification ratio of NTM may increase as databases expand to include more isolates.
In our study, different isolation media commonly used in laboratory for the recovery of mycobacteria gave different results. Although it is more convenient to use isolated colonies from solid media for MS analysis42, mycobacterial identification from liquid cultures can accelerate pathogen identification prior to growth on solid media43,44. There remnants of nutrient substances from liquid medium do not interfere substantially with the pattern of the mycobacterial spectra or impair the identification rate of VITKS MS when the modified protocol for processing liquid cultures, including a second ethanol washing step is used. Nevertheless, the percentage of isolates identified with a low confidence level (75–85%) was higher from liquid medium compared to solid medium, even when using a second ethanol washing step22. However, Aure´lieLotz et al. determined that identification results from growth in liquid medium were not as good as those obtained from solid medium either due to the low number of bacteria or to potential interference of the supplements such as PANTA and OADC included in the complex medium17.
In the meantime, we noticed differences in identification capabilities of the two commercial MALDI-TOFMS systems (the Bruker MALDI Biotyper and the bioMérieuxVitek MS). There are, in all, four reports comparing the two systems. Mather et al. used two simplified protein extraction protocols at the University Of Washington (UW) and by bioMérieux and both mass spectrometry platforms. Their results demonstrated that the identification performance of bioMérieuxVitek MS was better than Bruker MALDI Biotyper no matter which protocol was used by no naugmented database24. The report of Lévesque et al. indicated that the bioMérieux VITEK MS correctly identified more mycobacteria to species level than Bruker Biotyper30. However, Wilen and colleagues compared two MALDI-TOF MS instrumentation platforms and three databases: Bruker Biotyper Real Time Classification3.1 (Biotyper), Vitek MS Plus Saramis Premium (Saramis), and Vitek MS v3.0 (28). The levels of accuracy were not significantly different across the three platforms. However, the Vitek MS v3.0 database could offer modest advantages over the Biotyper and Saramis, especially by reducing the necessity of repeat identification attempts29.
It comes as no surprise that the identification accuracy of the clinical isolates plus reference strains was higher than that of the clinical isolates alone. This is because reference strains were more likely to have matching spectra in existing databases because of their inherent stable spectral profiles. The misidentification issues in Table 4 could be due to inherent unsatisfactory spectra from these species for highly similar spectral profiles from closely related species or subspecies within a complex, or insufficient numbers of spectra for uncommon species in reference libraries. Thus, it will be increasingly important to update these libraries include more reference spectra as well as the optimized extraction methods used to create the spectra.
Last but not least, there are still some limitations in our study. Firstly, Table 1 not showed all mycobacteria species because data of species with more than three reports were recalculate in this study for statistical reason. Moreover, some articles reported that MALDI-TOF MS identified isolates to “complex” level, such as “M. fortuitum complex”. We refer this situation as genus level; this may partially underestimate the accuracy of MALDI-TOF MS for identification of Mycobacteria to species level.
Different databases and system, differences in the preparation of sample spectra, and the composition of the species included in the study are probably responsible for observed differences in the overall identification rates in these studies. Despite our study demonstrated the use of MALDI-TOF MS as less reliable technique for the accurate identification of mycobacterial species, with the introduction of more spectra of representative organisms into the identification database and the development of a refined methodology, MALDI-TOFMS has become a promising tool for the identification of clinical pathogens to initiate early treatment and thus prevent drug resistance. Future studies to analyze the comprehensive capability of this technology for clinical microbiology diagnostics are warranted.
Materials and Methods
Search strategy
We queried PubMed (up to 1th March 2017) with the string “(maldi-ms [MeSH Terms] AND mycobacteria [MeSH Terms]) AND (identification [Title/Abstract] OR detection [Title/Abstract])” to identify relevant articles. We also searched Embase database with the words “maldi tof mass spectrometry,” “mycobacteria”, “mycobacterium,” “identification,” and “detection” with no language, publication status, and geographical distribution restriction. Two investigators (Yan Cao, Lei Wang) performed the literature search and data extraction independently. Disagreements were resolved by discussion and/or consultation with a third researcher (Bing Gu).
Study selection criteria and data extraction
The inclusion and exclusion criteria were established by the investigators prior to the review of literature. The accuracy of MALDI-TOF MS for identification of clinical mycobacteria isolates confirmed by gold standard methods was considered eligible for the meta-analysis. Studies or data were excluded as follows: case reports/reviews/posters; studies applying MALDI-TOF MS to identify industrial/environmental isolates; studies on technological innovations; in drug resistance; lack of a reference method or detailed number of isolates. The numbers of isolates correctly identified and of total isolates at the genus and species levels were abstracted according to the category of strain, the MS system or database used, and the culture method used.
Quality assessment
The quality of eligible studies was assessed by using the Quality Assessment of Diagnostic Accuracy Studies(QUADAS) guide lines45 to assess the quality of original studies: study design, system database, reference methods, category of strains, and blinded status (see Supplementary Table 1).
Data synthesis and analysis
The identification ratio was calculated as the number of correctly identified isolates divided by the total number of isolates46. The double arcsine-transformed ratios were subsequently pooled in random-effects model when significant heterogeneity was present. Pooled transformed estimate formulas were back-transformed into the original ratios47 for better understanding. Subgroup analyses at the species level were performed according to: strain, culture media, source of strain, and system database.
I2 measure was used to estimate heterogeneity between studies. The rank correlation method of Begg and Egger’s regression were used to evaluate publication bias48. All analyses were performed with Stata Statistical Software Package, version 1 1.0 (Stata Corp LP, College Station USA).
Electronic supplementary material
Acknowledgements
This research was supported by the National Natural Science Foundation of China (81471994), Jiangsu Privincial Natural Science Foundation (BK20151154), Jiangsu Privincial Medical Talent (ZDRCA2016053), Six talent peaks project of Jiangsu Province (WSN-135), and Advanced health talent of six-one project of Jiangsu Province (LGY2016042).
Author Contributions
Yan Cao, Lei Wang independently performed the literature search and data extraction. Fan Wenting conducted the statistical analysis. Ping ma and Shaoqing Ju interpreted the paper and revised the manuscript. Bing Gu supervised all phases of this study and revised the critically manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Yan Cao and Lei Wang contributed equally to this work.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-22642-w.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bing Gu, Email: gb20031129@163.com.
Shaoqing Ju, Email: jsq814@hotmail.com.
References
- 1.Matteelli A, et al. Tuberculosis elimination and the challenge of latent tuberculosis. Presse Med. 2017;46:e13–e21. doi: 10.1016/j.lpm.2017.01.015. [DOI] [PubMed] [Google Scholar]
- 2.Nahid P, Menzies D. Update in tuberculosis and nontuberculous mycobacterial disease 2011. Am J Respir Crit Care Med. 2012;185:1266–70. doi: 10.1164/rccm.201203-0494UP. [DOI] [PubMed] [Google Scholar]
- 3.McBryde ES, et al. The risk of global epidemic replacement with drug-resistant Mycobacterium tuberculosis strains. Int J Infect Dis. 2017;56:14–20. doi: 10.1016/j.ijid.2017.01.031. [DOI] [PubMed] [Google Scholar]
- 4.Griffith DE, Aksamit TR. Understanding nontuberculous mycobacterial lung disease: it’s been a long time coming. F1000Res. 2016;5:2797. doi: 10.12688/f1000research.9272.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Ingen J. Diagnosis of nontuberculous mycobacterial infections. Semin Respir Crit Care Med. 2013;34:103–9. doi: 10.1055/s-0033-1333569. [DOI] [PubMed] [Google Scholar]
- 6.Zumla A, et al. Rapid point of care diagnostic tests for viral and bacterial respiratory tract infections–needs, advances, and future prospects. Lancet Infect Dis. 2014;14:1123–1135. doi: 10.1016/S1473-3099(14)70827-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Costa P, Botelho A, Couto I, Viveiros M, Inacio J. Standing of nucleic acid testing strategies in veterinary diagnosis laboratories to uncover Mycobacterium tuberculosis complex members. Front Mol Biosci. 2014;1:16. doi: 10.3389/fmolb.2014.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Woo PC, Lau SK, Teng JL, Tse H, Yuen KY. Then and now: use of 16S rDNA gene sequencing for bacterial identification and discovery of novel bacteria in clinical microbiology laboratories. Clin Microbiol Infect. 2008;14:908–34. doi: 10.1111/j.1469-0691.2008.02070.x. [DOI] [PubMed] [Google Scholar]
- 9.Fan WT, et al. Performance of the matrix-assisted laser desorption ionization time-of-flight mass spectrometry system for rapid identification of streptococci: a review. Eur J Clin Microbiol Infect Dis. 2017;36:1005–1012. doi: 10.1007/s10096-016-2879-2. [DOI] [PubMed] [Google Scholar]
- 10.Suarez S, Nassif X, Ferroni A. [Applications of MALDI-TOF technology in clinical microbiology] Pathol Biol (Paris). 2015;63:43–52. doi: 10.1016/j.patbio.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 11.Seng P, et al. MALDI-TOF-mass spectrometry applications in clinical microbiology. Future Microbio.l. 2010;5:1733–54. doi: 10.2217/fmb.10.127. [DOI] [PubMed] [Google Scholar]
- 12.Niitsuma K, Saito M, Koshiba S, Kaneko M. Identification of mycobacteria by matrix-assisted laser desorption-ionization time-of-flight mass spectrometry–using reference strains and clinical isolates of Mycobacterium. Kekkaku. 2014;89:555–63. [PubMed] [Google Scholar]
- 13.Samli A, Ilki A. Comparison of MALDI-TOF MS, nucleic acid hybridization and the MPT64 immunochromatographic test for the identification of M. tuberculosis and non-tuberculosis Mycobacterium species. New Microbiol. 2016;39:259–263. [PubMed] [Google Scholar]
- 14.Wattal C, Oberoi JK, Goel N, Raveendran R, Khanna S. Matrix-assisted laser desorption ionization time of flight mass spectrometry (MALDI-TOF MS) for rapid identification of micro-organisms in the routine clinical microbiology laboratory. Eur J Clin Microbiol Infect Dis. 2017;36:807–812. doi: 10.1007/s10096-016-2864-9. [DOI] [PubMed] [Google Scholar]
- 15.El Khechine A, Couderc C, Flaudrops C, Raoult D, Drancourt M. Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry identification of mycobacteria in routine clinical practice. PLoS One. 2011;6:e24720. doi: 10.1371/journal.pone.0024720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tudo G, et al. Implementation of MALDI-TOF MS technology for the identification of clinical isolates of Mycobacterium spp. in mycobacterial diagnosis. Eur J Clin Microbiol Infect Dis. 2015;34:1527–32. doi: 10.1007/s10096-015-2381-2. [DOI] [PubMed] [Google Scholar]
- 17.Lotz A, et al. Rapid identification of mycobacterial whole cells in solid and liquid culture media by matrix-assisted laser desorption ionization-time of flight mass spectrometry. J. Clin Microbiol. 2010;48:4481–6. doi: 10.1128/JCM.01397-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Panda A, et al. Rapid identification of clinical mycobacterial isolates by protein profiling using matrix assisted laser desorption ionization-time of flight mass spectrometry. Indian J Med Microbiol. 2013;31:117–22. doi: 10.4103/0255-0857.115217. [DOI] [PubMed] [Google Scholar]
- 19.Balada-Llasat JM, Kamboj K, Pancholi P. Identification of mycobacteria from solid and liquid media by matrix-assisted laser desorption ionization-time of flight mass spectrometry in the clinical laboratory. J. Clin Microbiol. 2013;51:2875–9. doi: 10.1128/JCM.00819-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fangous MS, et al. Classification algorithm for subspecies identification within the Mycobacterium abscessus species, based on matrix-assisted laser desorption ionization-time of flight mass spectrometry. J. Clin Microbiol. 2014;52:3362–9. doi: 10.1128/JCM.00788-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rodriguez-Sanchez B, et al. Evaluation of MALDI Biotyper Mycobacteria Libraryv3.0 for Identification of Nontuberculous Mycobacteria. J. Clin Microbiol. 2016;54:1144–7. doi: 10.1128/JCM.02760-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kehrmann J, et al. Performance of Vitek MS in identifying nontuberculous mycobacteria from MGIT liquid medium and Lowenstein-Jensen solid medium. Diagn Microbiol Infect Dis. 2016;84:43–7. doi: 10.1016/j.diagmicrobio.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 23.Saleeb PG, Drake SK, Murray PR, Zelazny AM. Identification of mycobacteria in solid-culture media by matrix-assisted laser desorption ionization-time of flight mass spectrometry. J. Clin Microbiol. 2011;49:1790–4. doi: 10.1128/JCM.02135-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mather CA, Rivera SF, Butler-Wu SM. Comparison of the Bruker Biotyper and Vitek MS matrix-assisted laser desorption ionization-time of flight mass spectrometry systems for identification of mycobacteria using simplified protein extraction protocols. J. Clin Microbiol. 2014;52:130–8. doi: 10.1128/JCM.01996-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Girard V, et al. Identification of mycobacterium spp. and nocardia spp. from solid and liquid cultures by matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS) Diagn Microbiol Infect Dis. 2016;86:277–283. doi: 10.1016/j.diagmicrobio.2016.07.027. [DOI] [PubMed] [Google Scholar]
- 26.Quinlan P, Phelan E, Doyle M. Matrix-assisted laser desorption/ionisation time-of-flight (MALDI-TOF) mass spectrometry (MS) for the identification of mycobacteria from MBBacT ALERT 3D liquid cultures and Lowenstein-Jensen (LJ) solid cultures. J. Clin Pathol. 2015;68:229–35. doi: 10.1136/jclinpath-2014-202374. [DOI] [PubMed] [Google Scholar]
- 27.Buchan BW, Riebe KM, Timke M, Kostrzewa M, Ledeboer NA. Comparison of MALDI-TOF MS with HPLC and nucleic acid sequencing for the identification of Mycobacterium species in cultures using solid medium and broth. Am J Clin Pathol. 2014;141:25–34. doi: 10.1309/AJCPBPUBUDEW2OAG. [DOI] [PubMed] [Google Scholar]
- 28.Chen JH, et al. Advantages of using matrix-assisted laser desorption ionization-time of flight mass spectrometry as a rapid diagnostic tool for identification of yeasts and mycobacteria in the clinical microbiological laboratory. J. Clin Microbiol. 2013;51:3981–7. doi: 10.1128/JCM.01437-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilen CB, McMullen AR, Burnham CA. Comparison of Sample Preparation Methods, Instrumentation Platforms, and Contemporary Commercial Databases for Identification of Clinically Relevant Mycobacteria by Matrix-Assisted Laser Desorption Ionization-Time of Flight Mass Spectrometry. J. Clin Microbiol. 2015;53:2308–15. doi: 10.1128/JCM.00567-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Levesque S, et al. A Side by Side Comparison of Bruker Biotyper and VITEK MS: Utility of MALDI-TOF MS Technology for Microorganism Identification in a Public Health Reference Laboratory. PLoS One. 2015;10:e0144878. doi: 10.1371/journal.pone.0144878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tseng SP, et al. Rapid identification of M. abscessus and M. massiliense by MALDI-TOF mass spectrometry with a comparison to sequencing methods and antimicrobial susceptibility patterns. Future Microbiol. 2013;8:1381–9. doi: 10.2217/fmb.13.115. [DOI] [PubMed] [Google Scholar]
- 32.Marekovic I, et al. Evaluation of Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry in Identification of Nontuberculous Mycobacteria. Chemotherapy. 2016;61:167–70. doi: 10.1159/000442517. [DOI] [PubMed] [Google Scholar]
- 33.Kodana M, et al. Utility of the MALDI-TOF MS method to identify nontuberculous mycobacteria. J. Infect Chemother. 2016;22:32–5. doi: 10.1016/j.jiac.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 34.Angeletti S. Matrix assisted laser desorption time of flight mass spectrometry (MALDI-TOF MS) in clinical microbiology. J. Microbiol Methods. 2017;138:20–29. doi: 10.1016/j.mimet.2016.09.003. [DOI] [PubMed] [Google Scholar]
- 35.Garner O, et al. Multi-centre evaluation of mass spectrometric identification of anaerobic bacteria using the VITEK(R) MS system. Clin Microbiol Infect. 2014;20:335–9. doi: 10.1111/1469-0691.12317. [DOI] [PubMed] [Google Scholar]
- 36.Richter SS, et al. Identification of Enterobacteriaceae by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry using the VITEK MS system. Eur J Clin Microbiol Infect Dis. 2013;32:1571–8. doi: 10.1007/s10096-013-1912-y. [DOI] [PubMed] [Google Scholar]
- 37.Rychert J, et al. Multicenter evaluation of the Vitek MS matrix-assisted laser desorption ionization-time of flight mass spectrometry system for identification of Gram-positive aerobic bacteria. J. Clin Microbiol. 2013;51:2225–31. doi: 10.1128/JCM.00682-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Manji R, et al. Multi-center evaluation of the VITEK(R) MS system for mass spectrometric identification of non-Enterobacteriaceae Gram-negative bacilli. Eur J Clin Microbiol Infect Dis. 2014;33:337–46. doi: 10.1007/s10096-013-1961-2. [DOI] [PubMed] [Google Scholar]
- 39.Westblade LF, et al. Multicenter study evaluating the Vitek MS system for identification of medically important yeasts. J. Clin Microbiol. 2013;51:2267–72. doi: 10.1128/JCM.00680-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guillet V, et al. Insight into Structure-Function Relationships and Inhibition of the Fatty Acyl-AMP Ligase (FadD32) Orthologs from Mycobacteria. J. Biol Chem. 2016;291:7973–89. doi: 10.1074/jbc.M115.712612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jankovic M, et al. Geographical distribution and clinical relevance of non-tuberculous mycobacteria in Croatia. Int J Tuberc Lung Dis. 2013;17:836–41. doi: 10.5588/ijtld.12.0843. [DOI] [PubMed] [Google Scholar]
- 42.Kohlmann R, Hoffmann A, Geis G, Gatermann S. MALDI-TOF mass spectrometry following short incubation on a solid medium is a valuable tool for rapid pathogen identification from positive blood cultures. Int J Med Microbiol. 2015;305:469–79. doi: 10.1016/j.ijmm.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 43.Hines N, Payeur JB, Hoffman LJ. Comparison of the recovery of Mycobacterium bovis isolates using the BACTEC MGIT 960 system, BACTEC 460 system, and Middlebrook 7H10 and 7H11 solid media. J. Vet Diagn Invest. 2006;18:243–50. doi: 10.1177/104063870601800302. [DOI] [PubMed] [Google Scholar]
- 44.Scarparo C, et al. Evaluation of the BACTEC MGIT 960 in comparison with BACTEC 460 TB for detection and recovery of mycobacteria from clinical specimens. Diagn Microbiol Infect Dis. 2002;44:157–61. doi: 10.1016/S0732-8893(02)00437-6. [DOI] [PubMed] [Google Scholar]
- 45.Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25. doi: 10.1186/1471-2288-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ling H, Yuan Z, Shen J, Wang Z, Xu Y. Accuracy of matrix-assisted laser desorption ionization-time of flight mass spectrometry for identification of clinical pathogenic fungi: a meta-analysis. J. Clin Microbiol. 2014;52:2573–82. doi: 10.1128/JCM.00700-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72:39. doi: 10.1186/2049-3258-72-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen D-G, Peace KE. Applied meta-analysis with R. J. Applied Statistics. 2015;42:914–919. doi: 10.1080/02664763.2014.989464. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.