Abstract
Aims
The targeted genetic screening of Sudden Arrhythmic Death Syndrome (SADS) probands in a molecular autopsy has a diagnostic yield of up to 35%. Exome sequencing has the potential to improve this yield. The primary aim of this study is to examine the feasibility and diagnostic utility of targeted exome screening in SADS victims, utilizing familial clinical screening whenever possible.
Methods and results
To determine the feasibility and diagnostic yield of targeted exome sequencing deoxyribonucleic acid (DNA) was isolated from 59 SADS victims (mean age 25 years, range 1–51 years). Targeted exome sequencing of 135 genes associated with cardiomyopathies and ion channelopathies was performed on the Illumina HiSeq2000 platform. Non-synonymous, loss-of-function, and splice-site variants with a minor allele frequency <0.02% in the NHLBI exome sequencing project and an internal set of control exomes were prioritized for analysis followed by <0.5% frequency threshold secondary analysis. First-degree relatives were offered clinical screening for inherited cardiac conditions. Seven probands (12%) carried very rare (<0.02%) or novel non-sense candidate mutations and 10 probands (17%) had previously published rare (0.02–0.5%) candidate mutations–a total yield of 29%. Co-segregation fully confirmed two private SCN5A Na channel mutations. Variants of unknown significance were detected in a further 34% of probands.
Conclusion
Molecular autopsy using targeted exome sequencing has a relatively low diagnostic yield of very rare potentially disease causing mutations. Candidate pathogenic variants with a higher frequency in control populations are relatively common and should be interpreted with caution.
Keywords: SADS, Sudden cardiac death, Molecular autopsy, Exome sequencing, Long QT syndrome, Brugada syndrome
What's new?
Molecular autopsy of Sudden Arrhythmic Death Syndrome victims is best undertaken in the context of a multidisciplinary assessment involving detailed clinical screening of first-degree relatives so that genetic results are interpreted in the context of the relatives’ phenotype.
Molecular autopsy utilizing targeted exome sequencing results in a high frequency of candidate pathogenic variants that require further evaluation to determine their clinical importance and should be interpreted with caution.
Introduction
Sudden Arrhythmic Death Syndrome (SADS) causes ∼500 deaths in England and Wales every year.1 International guidelines recommend clinical assessment of the surviving first-degree relatives of SADS victims to identify probable cause of death and protect surviving family members.2 Several studies have shown that clinical screening alone identifies an inherited cardiac condition in 22–53% of families.3 Targeted genetic screening of deoxyribonucleic acid (DNA) from deceased probands identifies pathological variants in genes coding for cardiac ion channels in up to 35% of cases (see Supplementary material online, References S1–S19). A recent study undertook exome sequencing in 28 sudden death cases with a diagnostic yield of 32% for rare variants in arrhythmia/cardiomyopathy genes.4 The primary aim of this study was to examine the feasibility and diagnostic utility of targeted exome screening in SADS victims, utilizing familial clinical screening whenever possible.
Methods
The study complies with the declaration of Helsinki and the project is approved by the UCL/UCLH Joint Research Ethics Committee. All families gave informed consent for genetic analysis in their deceased relative. The cohort consisted of families referred to specialist inherited cardiovascular disease clinics in seven European centres. Sudden Arrhythmic Death Syndrome families were enrolled when the deceased proband fulfilled the following criteria: (i) age 1–55 years (ii) no cause of death identified at post-mortem (iii) negative toxicology screen. The first-degree relatives were offered clinical screening for inherited channelopathies and cardiomyopathies using a standard protocol.3 This consisted of an outpatient consultation and resting and exercise 12 lead electrocardiogram (ECG), 24 h ECG, trans-thoracic echocardiography (±cardiac magnetic resonance if any abnormalities) and ajmaline challenge if there was a suspicion of Brugada syndrome from the 12 lead ECG or the mode of death of the proband, or if all other investigations are normal. This was not possible for every family member and the most significant contributing factor was families declining some (commonly an ajmaline test) or all of the screening. Co-segregation testing was performed in cases of definite pathological variants when thought clinically appropriate with family consent.
Controls
We used aggregate summary statistics data from the NHLBI exome sequencing dataset (up to 6500 exomes, either African-American or European-American). We also used an in-house collection of 4042 whole-exome sequences (UCL-exomes, or UCL-ex consortium). The UCL-ex collection (for which patient-level data, as opposed to summary statistics) consists of patients sequenced for genetic diagnosis at UCL or collaborating centres in the UK. We excluded from UCL-ex any patient referred for genetic diagnosis because of a trait related to heart disease and used genetic data to exclude all patients of non-European ancestry. These filters selected a subset of 2867 samples (70.9% of the cohort).
DNA extraction and sequencing
Genomic DNA from frozen blood or spleen tissue taken at post-mortem was extracted with the QIAamp DNA Mini and EZ1 DNA Tissue kits (Qiagen) following standard protocols. Quality and quantity of the extracted DNA were assessed by Qubit Fluorometer (Invitrogen) and Bioanalyser (Agilent) assays. Targeted exonic regions were captured with the Agilent SureSelect Human All Exon Kit (v4, 51 MB) following the manufacturer's protocol. Exome sequencing of captured DNA was performed on the Illumina HiSeq2000 platform with 100 bp paired-end reads at a minimum of 50× coverage. Analysis of sequence data was confined to a pre-defined list of 135 genes known to be associated with cardiomyopathies and/or ion channelopathies (see Supplementary material online, Table S1). Paired-end reads aligned using the Novoalign software on the human reference genome build hg19. Following the exclusion of PCR duplicate reads (using Picard tools v1.100), insertion–deletions (indels) and single-nucleotide polymorphisms (SNPs) were called using the single-sample gVCF Haplotype Caller module of the software (GATK) (version 3.2.0). gVCF were subsequently combined to emulate multi-sample calling jointly with the whole UCL-exome cohort (>4000 exomes). These calls were annotated using Annovar and the Ensembl gene annotation set. We used the recalibration strategy suggested in the GATK best practices (hard calling for indels, clustering-based recalibration for SNPs) and excluded samples that did not have a calibration threshold of variant rarity in the control population.
Principal component analysis to identify European individuals in UCL-ex
To ensure that the ethnic matching is correct between cases and UCL-ex controls, we used a principal component analysis to identify individuals of European descent. To maximize the resolution of ethnic ancestry, we combined the UCL-ex data with 1092 samples of known ethnicity from the 1000 genomes project (www.1000genomes.org) across 3012 common and well-covered SNPs chosen to discriminate across ethnic groups.
Variant filtering
Primary analysis
Sequence data were filtered using a strict minor allele frequency threshold of ≤0.02% based on the NHLBI exome sequencing project and our internal UCL-ex set of control exomes. We further restricted this list to putative functional variants, i.e. variants annotated as non-synonymous, loss of function, or splice altering (within 2 bp of the splice site).
Secondary analysis
A second analysis using a threshold of ≤0.5% was also performed.5 Candidate pathogenic variants in this secondary analysis were selected using the following criteria: In a parallel analysis, prediction of in silico pathogenicity for novel missense variants detected at a threshold of ≤0.5% was performed using Polyphen2 and SIFT prediction software. A variant was predicted to be pathogenic if it was classified as simultaneously ‘damaging’ by SIFT and ‘possibly’ or ‘probably damaging’ by Polyphen2.
Published pathogenic mutation
Variants supported by co-segregation and/or functional data.
Novel protein truncating (non-sense) or published missense mutation without definite co-segregation/functional data.
Novel missense variants of unknown significance (VUS).
Case–control analysis
We used a case–control strategy to test whether we could detect an excess of rare and potentially pathogenic variants in cases. We considered putative functional variants (i.e. annotated as splice altering, loss of function, or non-synonymous) in a list of 20 genes that, based on the scientific literature, are most likely to harbour rare pathogenic variants associated with sudden cardiac death [KCNQ1, KCNH2, HERG, MIRP1, SCN5A, KCNE1, KCNE2, CACNA1C, CACNB2, SCN10A, RYR2, DES, DSP, PKP2, DSG2, DSC2, MYH7, MYBPC3, TNNT2, lamin A/C protein (LMNA)]. We also considered only rare variants, on the basis that common variants with a sizable effect on sudden cardiac death are unlikely to exist. To define rare variants, we used a threshold of 0.2%, which was defined jointly based on the NHLBI dataset and 1000 individuals of UK descent from the UCL-ex cohort. This initial frequency threshold determination left 1867 UCL-ex that were used as controls for the 59 sudden death samples.
Results
Study cohort
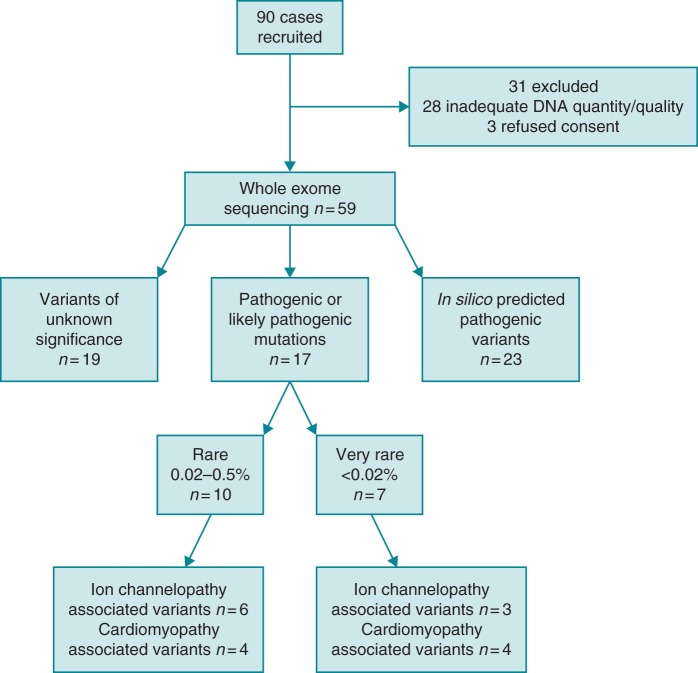
Ninety deceased probands met the inclusion criteria; 28 were rejected due to insufficient quantity or poor quality of DNA. The next of kin refused consent in an additional three cases. Table 1 summarizes the clinical characteristics of the 59 probands who underwent DNA analysis. Thirty-nine patients had structurally normal hearts and 20 had subtle cardiac structural abnormalities detected at post-mortem not reaching diagnostic criteria for a cardiomyopathy following expert cardiac pathologist review (i.e. fibrosis without disarray). Filtering the dataset for variants present in 135 target genes at a threshold of 0.5% generated a dataset of 80 coding variants (mean of 1.36 variants per proband). A single non-synonymous mutation was present in two samples (DMD gene, N1319K); hence, we found 79 distinct variants. Figure 1 illustrates the results of sequencing divided into three proband groups: pathogenic/likely pathogenic variants, in silico predicted pathogenic variants only, and VUS. Supplementary material online, Tables S2 and S3 show the distribution of variants in the 59 probands and the 23 probands with VUS predicted by in silico testing to result in disease, respectively. In total, 134 first-degree relatives from 54 (92%) families underwent some degree of clinical testing (mean 3 relatives per family). Data on clinical screening in families with rare variants are presented in Tables 2 and 3.
Table 1.
Summary of proband characteristics
| n | 59 |
| Mean age (range) | 25.3 (1–51) years |
| Sex | 76% male |
| Circumstances of death | |
| Daily activities | 37% |
| Sleep/at rest | 36% |
| Exercise | 17% |
| Acoustic stress | 2% |
| Unknown/not recorded | 8% |
| Previous symptoms | 20.3% |
| Syncope | 8 |
| Diagnosis of epilepsy | 2 |
| Aborted cot death | 1 |
| Chest pain | 1 |
| Previous 12 lead ECG | 13.6% |
| No specific finding | 5 |
| Inferior J point elevation | 1 |
| Non-specific intra-ventricular conduction delay | 1 |
| Anterior early repolarisation changes not diagnostic of Brugada phenotype | 1 |
| Family history of sudden cardiac death | 15.3% |
| Age at death <50 years | 5 |
| No age specified | 4 |
Figure 1.
Flow diagram of genetic and clinical diagnostic yield.
Table 2.
Seven probands with very rare variants identified (<0.02% in NHLBI and UCL-exomes cohorts)
| Age at death/sex | Circumstance of death (post-mortem findings) | Gene and disease associated | Amino acid change | Frequency in UCL-ex exomes (2867 individuals) | Frequency in NHLBI exome sequencing (6500 exomes) | Frequency in ExAC dataset (60 706 exomes) | Familial clinical evaluation |
|---|---|---|---|---|---|---|---|
| 4 years/female | Sleep (normal heart)* | SCN5A LQT6,7 |
R1623Q | 0 | 0 | 0 | Parents and siblings no LQT/BrS phenotype. All R1623Q negative |
| 6 years/male | Sleep (RV fat infiltration with no fibrosis)* | SCN5A LQT8–10 |
V411M | 0 | 0 | 0 | Parents and siblings no LQT/BrS phenotype. All V411M negative |
| 18 years/female | Daily activities (normal heart)* | TTN DCM/HCM |
E23106X | Undetermined | 0 | 0.00083 | Family declined screening |
| 26 years/female | Phone call (normal heart)* | RyR2 CPVT11 |
N1551S | 0 | 0 | 0.034 | Parents and siblings no CPVT phenotype but mother and sister positive N1551S and 4 sudden deaths on maternal side |
| 32 years/male | Sleep (normal heart)* | GJA5 Familial AF |
Y197X | 0 | 0 | 0 | Family declined screening |
| 39 years/male | Daily activities (fat infiltration both RV and LV, but no fibrosis)* | MYOT LGMD |
Q453X | 0 | 0 | 0.00165 | Family declined screening |
| 44 years/male | Daily activities (mild fibrosis with no disarray)* | DSC2 ARVC12 |
S868F | 0 | 0.0077 | 0.0058 | Young child normal ECG and echo |
All variant frequencies are listed as percentages. Expert cardiac pathology review denoted with an asterisk.
Table 3.
Ten probands with rare variants identified (>0.02–0.5% of controls)
| Age at death/sex | Circumstance of death (post-mortem findings) | Gene and disease associated | Amino acid change | Frequency in UCL-ex exomes (2867 individuals) | Frequency in NHLBI exome sequencing (6500 exomes) | Frequency in ExAC dataset (60 706 exomes) | Familial clinical evaluation |
|---|---|---|---|---|---|---|---|
| 23 years/male | Daily activities (myocardial bridging of the LAD and fat infiltration of RV)* | CACNA1C BrS13,14 |
P817S | 0.7 | 0.33 | 0.0194 | Parents and sibling no BrS phenotype |
| 1 year/male | Daily activities (normal heart) | LMNA DCM23–25 |
R644C | 0.138 | 0.10 | 0.121 | Parents normal ECG and echo |
| 22 years/female | Sleep (normal heart) | RANGRF BrS9,17 |
E61X | 0.26 | 0.42 | 0.3947 | Parents normal ECG and echo (ajmaline challenge not done) |
| 11 years/male | Exercise (normal heart) | CACNA2D1 BrS13,14 |
S709N | 0.22 | 0.37 | 0.2677 | Family declined screening |
| 33 years/male | Daily activities (normal heart) | ANK2 LQT19–21 |
E1837K | 0.29 | 0.31 | 0.2677 | Parents no LQT phenotype |
| 27 years/male | Daily activities (inflammatory eosinophilic infiltrate in atria)* | KCNH2 LQT6,15,16 |
P347S | 0.16 | 0.0496 | 0.1293 | Parents and siblings no LQT phenotype |
| 41 years/male | Daily activities (normal heart) | MYPN HCM26 |
Y20C | 0 | 0.092 | 0.091 | Parent, siblings and children normal ECG, ETT, echo, and ajmaline |
| 28 years/male | Exercise (concentric LVH, no disarray)* | RBM20 DCM27 |
E1125K | 0.30 | 0.37 | 0.37 | Parents and siblings normal ECG, ETT, echo, and ajmaline |
| 14 years/male | Exercise (normal heart)* | DSP ARVC22 |
A2294G | 0.12 | 0.023 | 0.085 | Parents and siblings normal ECG, ETT, echo, and ajmaline |
| 34 years/male | Sleep (normal heart) | CACNA1C BrS13 |
G37R | 0.32 | 0.23 | 0.074 | Siblings positive ajmaline challenges |
All variant frequencies are listed as percentages. Expert cardiac pathology review denoted with an asterisk.
Sequence analysis
Primary analysis
Seven probands (12%) carried very rare variants (published missense mutations or novel non-sense mutations) found in <0.02% of the control population (Table 2).
Ion channel variants (frequency <0.02% of controls)
SCN5A R1623Q
A 4-year-old female, who died during sleep, carried the SCN5A variant R1623Q. This is frequently a de novo mutation associated with long QT syndrome in infancy.6,7 Clinical screening of the first-degree relatives revealed no evidence of QT prolongation and co-segregation analysis confirmed this was a private mutation in the deceased.
SCN5A V411M
A 6-year-old male, who died during his sleep, carried the SCN5A variant V411M. Post-mortem showed a macroscopically normal heart with large amount of fat in the right ventricle but no other features of arrhythmogenic right ventricular cardiomyopathy (ARVC). The variant is associated with long QT type 3.8–10 Family screening has revealed no evidence of QT prolongation, negative ajmaline provocation in the parents. The parents and two siblings do not carry the mutation.
Ryr2 N1551S
A 26-year-old female with a structurally normal heart on post-mortem whose death was triggered by an acoustic stress (phone call) carried the RyR2 variant N1551S. This variant has been published in a case of a 8-year-old proband with exertional syncope, family history of sudden cardiac death, and polymorphic ventricular tachycardia on exercise requiring resuscitation.11 Family screening revealed no clear phenotype for catecholaminergic polymorphic VT (CPVT); however, both the mother and sister of the proband have a history of palpitations and are positive for N1551S. There is a malignant family history with four sudden cardiac deaths on the maternal side, and the father and brother, who are asymptomatic, are negative for this variant.
Cardiomyopathy variants (frequency <0.02% of controls)
DSC2 (Desmocolin) S868F
Published desmosmal variant12 identified in a 14-year-old male who died playing basketball. Post-mortem demonstrated mild fibrosis and hypertrophy but no disarray/fibro-fatty replacement.
TTN E23106X
A very rare novel cardiomyopathy variant was discovered in an 18-year-old female who died during daily activities with a structurally normal heart on post-mortem.
MYOT Q453X
A very rare novel cardiomyopathy variant identified in a 39-year-old male who died during daily activities and was found to have fatty infiltration in the RV and localized LV walls without fibrosis.
GJA5 Y197X
A very rare novel variant in GJA5, responsible for coding the gap junction protein connexin 40, was found in a 21-year-old proband who died during their sleep. Post-mortem confirmed a structurally normal heart.
Secondary analysis
Candidate variants identified in >0.02–0.5% of controls
Ten probands (17%) had rare, previously reported pathological variants or variants likely to be pathogenic are summarized in Table 3.
Ion channel variants (frequency >0.02–0.5% of controls)
CACNA1C G37R
A 34-year-old male who died during his sleep carried the CACNA1C variant G37R. This variant occurs in a highly conserved region and has been identified in two cases of Brugada syndrome, a case of idiopathic ventricular fibrillation and early repolarisation syndrome.13 Two siblings had positive ajmaline provocation tests, but are yet to be tested for this variant in order to assess this mutation's clinical relevance.
CACNA1C P817S
A 23-year-old male died during daily activities and carried the published CACNA1C P817S variant associated with Brugada syndrome.13,14 The post-mortem showed myocardial bridging of the LAD and fatty infiltration of the RV with a minor degree of fibrosis not diagnostic for ARVC.
KCNH2 P347S
A 27-year-old male who died during his sleep had a past history of hypoacusia and epilepsy with seizures occurring during emotional stress, carried the KCNH2 variant P347S. The post-mortem showed an inflammatory eosinophilic infiltrate in the atrial myocardium near the AV node. The variant has been reported in multiple publications associated with long QT 2 syndrome6,15,16 but is also a rare variant in Caucasians, present in up to 0.15% of controls. Functional studies have demonstrated a reduction in IKr of 50–60%.
RANGRF E61X
A 22-year-old female, who died during sleep and with a structurally normal heart, carried the RANGRF E61X variant. This is a stop-gain (non-sense) mutation resulting in the truncation of more than two thirds of the encoded protein and has been previously reported as having a possible association with Brugada syndrome.9,17 Despite being present in a low frequency of controls, functional studies have demonstrated reduced cardiac sodium channel (Nav1.5) current due to decreased ion channel trafficking.
CACNA2D1 S709N
An 11-year-old male who died playing football and had a structurally normal heart at post-mortem carried the CACNA2D1 variant S709N. This variant is associated with Brugada syndrome13,14 but has recently been found in a higher prevalence of Danish controls than previously detected thus questioning its pathogenicity,18 parental ajmaline testing would enable pathological confirmation in this case if the family consented.
ANK2 E1837K
A 33-year-old male who died during normal daily activities carried the ANK2 variant E1837K which has been associated with long QT syndrome.19–21
Cardiomyopathy variants (frequency ≥0.02–0.5% of controls)
DSP A2294G
This desmoplakin variant, possibly associated with ARVC22 was discovered in a 42-year-old female who died during her sleep. Post-mortem concluded a structurally normal heart.
LMNA R644C
An 18-month-old infant who died during normal activities with a structurally normal heart on post-mortem carried the LMNA (lamin) variant R644C. This variant has been published as a disease causing mutation in more than one study associated with dilated cardiomyopathy.23–25 The variant affects a highly conserved region producing a change from a charged to an uncharged amino acid implying significant changes in physicochemical properties. It has been reported in controls with a frequency of 0.2%.
MYPN Y20C
Myopallidin MYPN Y20C published variant26 discovered in a 41-year-old male who died during daily activities. There was a prior history of syncope and an implantable loop recorder documented ventricular tachycardia on the day of his death. Post-mortem confirmed a structurally normal heart and prior ECG was also normal.
RBM20 E1125K
RNA binding motif protein 20 published variant27 was documented in a 28-year-old male who died during exercise who had concentric left ventricular hypertrophy (LVH) in the absence of disarray on post-mortem.
Case–control analysis
Our case–control analysis is based on 59 sudden cardiac death cases ethnically matched with 1867 UCL-ex control. Based on our filtering criteria (control frequency <0.2%, putatively functional in 20 strongest candidate genes, see Methods), we identified an average of 0.38 candidate variant per control compared with 0.51 variant per case. This difference is statistically non-significant (one-sided χ2 test P = 0.059), but is consistent with an excess of 7–8 candidate variants in the full set of 59 cases compared with controls. Nevertheless, this number of variants in excess is consistent with the fact that we have identified seven putatively functional variants in our primary list. Hence, the lack of statistical significance could be a consequence of the low yield of strong candidate variants for sudden cardiac death in cases.
Discussion
This study shows that a small number of individuals who die suddenly with no obvious identifiable cause at post-mortem harbour very rare potentially pathogenic DNA sequence variants in genes that are associated with disorders known to cause sudden cardiac death. Plausible disease associated ion channel mutations have been clearly identified in three (5%) probands with molecular autopsy providing a benefit for the family. Private mutations (SCN5A R1623Q and V411M) were confirmed in two of these families who had negative clinical screens for Brugada and LQT3 syndrome, and a RyR2 mutation detected in a family with a malignant history but no clear phenotype. A further six (10%) probands had rare ion channel variants which have been reported in association with Brugada syndrome and long QT syndrome, but were also identified in 0.02–0.5% of controls. Eight (14%) probands had very rare or rare cardiomyopathy variants detected. The significance of these is yet to be determined and there are no co-segregation data available in this cohort. It is plausible that an arrhythmia secondary to a cardiomyopathy maybe responsible for sudden cardiac death in the context of a structurally normal heart. A concealed phase of ARVC is recognized where electrophysiological abnormalities occur prior to any structural changes detectable on imaging.28 Similarly, PR prolongation and sudden cardiac death due to ventricular arrhythmia are known to occur before the development of dilated cardiomyopathy in cases of Lamin A/C mutations.29 The pathogenicity of the TTN variant reported is debatable. Its rarity makes it likely to be important statistically and, therefore, raises the suspicion of pathogenicity, although we have no co-segregation data. The gene encoding the huge titin protein is probably the most complex in the genome consisting of 363 exons used in different alternatively spliced transcripts.30 TTN mutations were identified in 3% of controls31 and, similarly, new population-based exome data have identified a high prevalence of previously reported cardiomyopathy associated variants.32 This highlights the clinical relevance of our study. Molecular autopsy using exome sequencing will lead to the identification of large numbers of VUS, many of which will be plausible candidate mutations and the challenge is to then ascertain their pathogenicity. At present, this approach will inform rather than replace the clinical screening of the surviving first-degree relatives and, in some cases, may raise more questions than it answers.
Case–control analysis showed a suggestive but not statistically significant excess of candidate variants in cases. Limited case sample size, combined with our limited ability to identify functional and disease implicated variants, could explain the lack of power of this case–control analysis. Taken together, these findings indicate that molecular autopsy complements but does not substitute for clinical testing.
Variant interpretation
Evaluation of genetic variants in SADS victims is particularly difficult as the deceased probands have normal hearts and rarely have ante-mortem clinical phenotype data. The variable and often incomplete expression of most disorders that cause SCD also hampers co-segregation analysis of variants identified in the proband. One approach is to consider only extremely rare variants as potentially pathogenic, but a potential drawback is the exclusion of relatively common variants that are nevertheless disease causing or modify phenotypes.
To date there have been 19 published reports and series encompassing ∼540 cases of SADS with a diagnostic yield ranging from 0–35% (see Supplementary material online, References S1–S19). The lower yields occurred in studies using paraffin-embedded formalin-fixed tissue where degradation of DNA often prevents analysis. One recent study in 28 cases utilized exonic sequencing and identified rare variants in ion channel/cardiomyopathy genes in 32% cases,4 but did not evaluate the mutations in the context of family screening. This compares with a diagnostic yield of 29% of rare/very rare variants in this series. In contrast to previous studies, there was a lack of pathogenic mutations in RyR2 mutations in our series. Interestingly, this was also the case in the recent exonic study and maybe due to a more strict frequency cut-off for variant calling.4 To improve the specificity in detection of causative mutations, we defined pathogenicity using a strict frequency threshold of 0.02% in the general population which reduced the number of candidates to seven variants (12% of probands) that were either non-sense mutations which truncated the encoded protein or were previously reported in the literature as likely pathogenic on the basis of clinical or functional data. Raising the frequency threshold to a less stringent level of 0.5% increased the yield of candidate variants to 29% and reliance on in silico prediction would have further increased the yield of possible disease causing variants to a total of 66%.
In attempting to ascertain the pathogenicity of variants, their presence among the healthy population can be helpful, but is not the sole determinant of pathogenicity. A minor allele frequency cut-off of 1% is considered rare and is part of a proposed scoring system.33 Variants with a 0.5–0.02% yield are included in our analysis, but with clear separation from those variants with a lower yield <0.02% in controls. In three of these families, there has been a complete negative clinical screen of the first-degree relatives suggesting possible de novo disease in the proband. The proband with a CACNA1C variant G37R, there is a family history of Brugada syndrome and the mode of death was during sleep suggesting this is a plausible causative mutation (although co-segregation is required to prove this). Setting the bar too low may result in missing potentially harmful variants, and setting it too high and you run the risk of the important variants becoming overwhelmed by benign noise.
Ideally, all novel variants should be subjected to functional studies, but these are costly, time consuming and often impractical in the clinical setting. They also may not translate into clinically relevant phenotypes. For example, ∼4% of healthy white and 6–8% of black individuals harbour an amino acid-altering genetic variant in one of the three major long QT syndrome-susceptibility genes (KCNQ1, KCNH2, or SCN5A).15 In a recent study from the NHLBI GO Exome Sequencing Project, four variants KCNH2 P347S; SCN5A: S216L, V1951L; and CAV3 T78M with significant predicted functional effects were identified in 1:32 of a control population of 704 people. Only one individual had a corrected QT interval (QTc) of 462 ms and the rest of the carriers of these variants had a QTc <440 ms.16 Therefore, in this molecular autopsy series, we have deliberately distinguished the known clinically proven pathogenic mutations from those that have been shown to be possibly pathogenic from in silico prediction algorithms.
Clinical implications
This study suggests that the use of molecular autopsy is best undertaken in the context of a multidisciplinary assessment involving detailed clinical screening so that genetic results are interpreted in the context of the relatives' phenotype. When unequivocal mutations in a proband and subsequently the relative(s) are identified, management should be informed by the phenotype except in certain rare circumstances (e.g. DPP6 mutation carriers), where presence of the mutation alone may be sufficient to recommend therapy.34
Study limitations
A significant number of families refused access to DNA and could not be included in the study. Twenty-four percent of the collected DNA samples were unsuitable for analysis. This highlights the practical issues regarding the feasibility of tissue storage and DNA extraction for exome sequencing in real world practice. Comprehensive clinical screening of families was not completed, mostly due to the families declining any or further investigation. Co-segregation studies were not performed in several cases of rare variants with negative family screening, as there were concerns that this would not change clinical management or could promote increased patient anxiety.
Conclusions
Molecular autopsy using targeted exome sequencing of genes implicated in SADS has a relatively low diagnostic yield of very rare potentially disease causing mutations. Candidate pathogenic variants with a higher frequency in control populations are relatively common and should be interpreted with caution.
Supplementary material
Funding
This work was undertaken at UCLH/UCL who received a proportion of funding from the Department of Health's NIHR Biomedical Research Centres funding scheme; which awarded a project grant for this work and was also supported St Jude Medical; Rosetrees Trust; and the Stephen Lyness Research Fund. L.R.L. is supported by a grant from the Gulbenkian Doctoral Programme for Advanced Medical Education, sponsored by Fundação Calouste Gulbenkian, Fundação Champalimaud, Ministério da Saúde, and Fundação para a Ciência e Tecnologia, Portugal. E.Z. is supported by funding from Instituto de Salud Carlos III (RD12/0042/0029), Prometeo 2011/027, and Biobanco La Fe.
Conflict of interest: L.M.N. received an educational grant from St Jude Medical.
Supplementary Material
Acknowledgements
We thank Juan Giner MD PhD and Pilar Molina MD PhD, Department of Pathology, Institute of Legal Medicine of Valencia, Spain. Begoña Cardona MD PhD, Department of Pathology, Institute of Legal Medicine of Alicante, Spain.
References
- 1. Behr E, Casey A, Sheppard M, Wright M, Bowker T, Davies M et al. . Sudden Arrhythmic Death Syndrome: a national survey of sudden unexplained cardiac death. Heart 2007;93:601–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Priori SG, Wilde AA, Horie M, Cho Y, Behr ER, Berul C et al. . Executive summary: HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes. Europace 2013;15:1389–406. [DOI] [PubMed] [Google Scholar]
- 3. Nunn LM, Lambiase PD. Genetics and cardiovascular disease—causes and prevention of unexpected sudden adult death: the role of the SADS clinic. Heart 2011;97:1122–7. [DOI] [PubMed] [Google Scholar]
- 4. Bagnall R, Das J, Duflou J, Semsarian C. Exome analysis-based molecular autopsy in cases of sudden unexplained death in the young. Heart Rhythm 2014;11:655–62. [DOI] [PubMed] [Google Scholar]
- 5. Consortium TG. An integrated map of genetic variation from 1,092 human genomes. Nature 2012;491:56–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Splawski I, Shen J, Timothy K, Lehmann M, Priori S, Robinson J. Spectrum of mutations in long-QT syndrome genes. KVLQT1, HERG, SCN5A, KCNE1 and KCNE2. Circulation 2000;102:1178–85. [DOI] [PubMed] [Google Scholar]
- 7. Kambouris N, Nuss H, Johns D, Tomaselli G, Marban E, Balser J. Phenotypic characterization of a novel long-QT syndrome mutation (R1623Q) in the cardiac sodium channel. Circulation 1998;97:640–4. [DOI] [PubMed] [Google Scholar]
- 8. Tester D, Will M, Haglund C, Ackerman M. Compendium of cardiac channel mutations in 541 consecutive unrelated patients referred for long QT syndrome genetic testing. Heart Rhythm 2005;2:507–17. [DOI] [PubMed] [Google Scholar]
- 9. Kapplinger J, Tester D, Alders M, Benito B, Berthet M, Brugada J et al. . An international compendium of mutations in the SCN5A-encoded cardiac sodium channel in patients referred for Brugada syndrome genetic testing. Heart Rhythm 2010;7:33–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Goldenberg I, Horr S, Moss A, Lopes C, Barsheshet A, McNitt S et al. . Risk for life-threatening cardiac events in patients with genotype-confirmed long-QT syndrome and normal-range corrected QT intervals. J Am Coll Cardiol 2011;57:51–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kawamura M, Ohno S, Naiki N, Nagaoka I, Dochi K, Wang Q et al. . Genetic background of catecholaminergic polymorphic ventricular tachycardia in Japan. Circ J 2013;77:1705–13. [DOI] [PubMed] [Google Scholar]
- 12. Fressart V, Duthoit G, Donal E, Probst V, Deharo J, Chevalier P et al. . Desmosomal gene analysis in arrhythmogenic right ventricular dysplasia/cardiomyopathy: spectrum of mutations and clinical impact in practice. Europace 2010;12:861–8. [DOI] [PubMed] [Google Scholar]
- 13. Burashnikov E, Pfeiffer R, Barajas-Martinez H, Delpon E, Hu D, Desai M et al. . Mutations in the cardiac L-type calcium channel associated with inherited J wave syndromes and sudden cardiac death. Heart Rhythm 2010;7:1872–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Crotti L, Marcou C, Tester D, Castelletti S, Giudicessi J, Torchio M et al. . Spectrum and prevalence of mutations involving BrS1-through BrS12-susceptibility genes in a cohort of unrelated patients referred for Brugada syndrome genetic testing: implications for genetic testing. J Am Coll Cardiol 2012;60:1410–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kapa S, Tester D, Salisbury B, Harris-Kerr C, Pungliya M, Alders M et al. . Genetic testing for long-QT syndrome: distinguishing pathogenic mutations from benign variants. Circulation 2009;120:1752–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Refsgaard L, Holst A, Sadjadieh G, Haunsø S, Nielsen J, Olesen M. High prevalence of genetic variants previously associated with LQT syndrome in new exome data. Eur J Hum Genet 2012;20:905–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Olesen MS, Jensen NF, Holst AG, Nielsen JB, Tfelt-Hansen J, Jespersen T et al. . A novel nonsense variant in Nav1.5 cofactor MOG1 eliminates its sodium current increasing effect and may increase the risk of arrhythmias. Can J Cardiol 2011;27:523.e17–23. [DOI] [PubMed] [Google Scholar]
- 18. Risgaard B, Jabbari R, Refsgaard L, Holst A, Haunsø S, Sadjadieh A et al. . High prevalence of genetic variants previously associated with Brugada syndrome in new exome data. Clin Genet 2013;84:489–95. [DOI] [PubMed] [Google Scholar]
- 19. Mohler P, Splawski I, Napolitano C, Bottelli G, Sharpe L, Timothy K et al. . A cardiac arrhythmia syndrome caused by loss of ankyrin-B function. Proc Natl Acad Sci USA 2004;101:9137–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mohler P, Le Scouarnec S, Denjoy I, Lowe J, Guicheney P, Caron L et al. . Defining the cellular phenotype of ‘ankyrin-B syndrome’ variants: human ANK2 variants associated with clinical phenotypes display a spectrum of activities in cardiomyocytes. Circulation 2007;115:432–41. [DOI] [PubMed] [Google Scholar]
- 21. Sherman J, Tester D, Ackerman M. Targeted mutational analysis of ankyrin-B in 541 consecutive, unrelated patients referred for long QT syndrome genetic testing and 200 healthy subjects. Heart Rhythm 2005;2:1218–23. [DOI] [PubMed] [Google Scholar]
- 22. Garcia-Pavia P, Syrris P, Salas C, Evans A, Mirelis J, Cobo-Marcos M et al. . Desmosomal protein gene mutations in patients with idiopathic dilated cardiomyopathy undergoing cardiac transplantation: a clinicopathological study. Heart 2011;97:1744–52. [DOI] [PubMed] [Google Scholar]
- 23. Genschel J, Bochow B, Kuepferling S, Ewert R, Hetzer R, Lochs H. A R644C mutation within lamin A extends the mutations causing dilated cardiomyopathy. Hum Mutat 2001;17:154. [DOI] [PubMed] [Google Scholar]
- 24. Genschel J, Schmidt H. Mutations in the LMNA gene encoding lamin A/C. Hum Mutat 2000;16:451–9. [DOI] [PubMed] [Google Scholar]
- 25. Rankin J, Auer-Grumbach M, Bagg W, Colclough K, Nguyen T, Fenton-May J et al. . Extreme phenotypic diversity and non-penetrance in families with the LMNA gene mutation R644C. Am J Med Genet A 2008;146:1530–42. [DOI] [PubMed] [Google Scholar]
- 26. Purevjav E, Arimura T, Augustin S, Huby A, Takagi K, Nunoda S et al. . Molecular basis for clinical heterogeneity in inherited cardiomyopathies due to myopalladin mutations. Hum Mol Genet 2012;21:2039–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Refaat M, Lubitz S, Makino S, Islam Z, Frangiskakis J, Mehdi H et al. . Genetic variation in the alternative splicing regulator RBM20 is associated with dilated cardiomyopathy. Heart Rhythm 2012;9:390–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gomes J, Finlay M, Ahmed AK, Ciaccio EJ, Asimaki A, Saffitz JE et al. . Electrophysiological abnormalities precede overt structural changes in arrhythmogenic right ventricular cardiomyopathy due to mutations in desmoplakin-A combined murine and human study. Eur Heart J 2012;33:1942–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hasselberg NE, Edvardsen T, Petri H, Berge KE, Leren TP, Bundgaard H et al. . Risk prediction of ventricular arrhythmias and myocardial function in Lamin A/C mutation positive subjects. Europace 2014;16:563–71. [DOI] [PubMed] [Google Scholar]
- 30. Punetha J, Hoffman EP. Short read (next generation) sequencing: a tutorial with cardiomyopathy diagnostics as an exemplar. Circ Cardiovasc Genet 2013;6:427–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Herman DS, Lam L, Taylor MRG, Wang L, Teekakirikul P, Christodoulou D et al. . Truncations of titin causing dilated cardiomyopathy. N Engl J Med 2012;366:619–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Andreasen C, Nielsen JB, Refsgaard L, Holst AG, Christensen AH, Andreasen L et al. . New population-based exome data are questioning the pathogenicity of previous cardiomyopathy-associated genetic variants. Eur J Hum Genet 2013;21:918–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Campuzano O, Allegue C, Fernandez A, Iglesias A, Brugada R. Determining the pathogenicity of genetic variants associated with cardiac channelopathies. Sci Rep 2015;5:7953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Postema P, Christiaans I, Hofman N, Alders M, Koopmann T, Bezzina C et al. . Founder mutations in the Netherlands: familial idiopathic ventricular fibrillation and DPP6. Neth Heart J 2011;19:290–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.