Abstract
Pulmonary arterial hypertension (PAH) affects the physical and emotional wellbeing of patients. More information is needed regarding mental problems and preferences for support. Qualitative interviews were used to explore mental problems and preference for support of PAH patients. Additionally, a survey was used to assess the presence of mental problems (Problem List), distress (Distress Thermometer) and the need for mental support. In 24 semi-structured interviews, the following problem themes were identified: energy balance; loss of abilities; feeling misunderstood; and handling of worries and emotions. Need for support was based on an interplay between resilience to psychological distress, additional life problems, age, disease status, attitude towards professional help, and experienced support from significant others. The results from the survey highlight the need for professional support, as 50.8% of the 67 patients who completed the survey would consider support when offered, specifically when offered by a pulmonary hypertension (PH) professional. Younger age (odds ratio [OR] = 0.97, P = 0.04), depression (OR = 11.435, P = 0.001) and possibly anxiety (OR = 3.831, P = 0.069) were related to need for support. In conclusion, many patients with PAH are in need of mental support, which should be offered by a PH professional and tailored to phase of the disease and personal characteristics.
Keywords: pulmonary hypertension, distress, anxiety and depression, health services, mixed methods
Pulmonary arterial hypertension (PAH) is a rare chronic lung disease characterized by an elevated pulmonary artery pressure (PAP; ≥25 mmHg at rest).1 To date, there is no cure for the disease and 40–50% of PAH patients die within five years of diagnosis, despite treatment with PAH-specific drugs within six months of diagnosis.2,3 Consequently, the main focus of treatment is on managing the physical symptoms caused by the disease and on prolonging life expectancy. Furthermore, efforts to improve quality of life in PAH patients are increasing.4 This is highly relevant, as it is widely known that PAH has a considerable impact on quality of life. In fact, the quality of life of PAH patients is reduced in almost all aspects of life, including energy, emotional reactions, pain, sleep, social isolation, and physical mobility.5,6
Recently, the relationship between mental problems and quality of life in PAH is drawing the attention of both clinicians and researchers.4,7,8 It seems that mental problems, specifically anxiety and depression, have a particularly negative influence on the quality of life of patients with PAH.5 This is an important finding, since the percentages of patients with clinical levels of depressive and anxiety symptoms among PAH patients are high, with prevalence rates of up to 40% for depression and 48% for anxiety.5,9–12 Furthermore, depression and anxiety have been linked to poorer health outcomes and even mortality in heart and lung disease.13,14 The high prevalence of mental problems in PAH patients and their negative influence on health and quality of life highlight the importance of decreasing mental distress. Guillevin et al. studied PAH patients’ perspectives on their situation and the healthcare provided to them. PAH patients frequently stated feelings of frustration, irritation, low self-esteem, feeling misunderstood and worthless, together with a fear for the future and isolation from their social environment.15 The majority of the patients stated a need for more information regarding the impact of PAH on their lives, and supplementary information about depression and other mental problems.15 A German study found that 57% of PAH patients report a wish for psychosomatic treatment.16
Nonetheless, it is still largely unknown what makes patients susceptible to experiencing mental problems and when and how mental healthcare for PAH patients should be provided. More information about which patient characteristics may be related to mental problems and need for mental support might help in the organization of mental support for this patient group. Therefore, the aim of this study is to identify mental problems (and pathways to them) experienced by PAH patients and their need for mental support.
Qualitative interviews and a survey were used to gather information about the perspectives of patients regarding their mental problems along with their needs regarding support. In addition, exploratory analyses were conducted to examine characteristics related to the need for support. Our hypothesis is that this research provides information that may facilitate the organization and content of mental support for PAH patients, and thereby contributes to a decrease in mental problems and an improvement in the quality of life.
Methods
Study design
Using a mixed methods analysis, the problems of PAH patients were identified together with their corresponding need regarding mental support. A qualitative study was performed to gather patient perspectives by conducting semi-structured interviews. To verify and generalize the qualitative data, triangulation was applied by conducting a quantitative study parallel to the qualitative study by means of a survey. The survey addressed the degree of distress, specific problems, and the need for mental support of patients with pulmonary hypertension (PH). Participants were asked for their written informed consent and there were no consequences for patients who were not willing to participate. No data were collected from patients who did not participate. Researchers conducting or analyzing the interviews and surveys were not involved in the treatment of the patient. The processing of the data was strictly confidential. The medical ethic of the VU medical center committee approved the study protocol.
Qualitative data
Study participants
Participants for the qualitative study were adults with a diagnosis of PAH, who were recruited by telephone or face-to-face by a physician assistant of the department of pulmonary medicine, VU University medical centre (VUmc), the Netherlands. Purposive sampling was performed in order to obtain a maximum of perspectives, based on the following factors: gender, age, diagnosis years, partner status, and having children. All participants provided written informed consent. The interviews were conducted face-to-face at the medical center between March and May 2014.
Methods
Semi-structured interviews were used to explore pathways to mental problems and patients’ needs for mental support. The interviews were supported by an interview guide that included a topic list. The topic list was based on literature, an interview with a social worker specialized in PAH, and a focus group with patients and professionals (specialized in PAH). The study used a combined deductive and inductive research method: the exact content of the topic list was the result of an iterative process in which relevant new topics were added during the interview period. The main focus of the interview was on the patients’ experienced problems, coping abilities, and need for mental support. Two research assistants with a bachelor’s degree (one nurse specialized in PAH and one master level student [SG] in health sciences) conducted the interviews, which lasted approximately 45 min. The interview was pilot-tested and the interviewers conducted the first three interviews together to create synergy. All interviews were audio-recorded and transcribed verbatim, and field notes were taken. The interviewers were trained and supervised by a psychologist (AM), who verified the (audio-taped) interviews and provided feedback at the frequent meetings to discuss the findings. Data collection ended when saturation was achieved.17 Data were analyzed according to the constant comparison method.13 The interviewers performed an open analysis of the transcripts and field notes of the first two interviews, after which they compared identified themes. Subsequently, they repeatedly compared themes and evaluated the findings from the interviews with a third researcher (AM). The qualitative data were processed in the qualitative data analysis software program MAXQDA.18 Data were collected and analyzed in accordance with the COREQ guidelines for qualitative studies.19
Quantitative data
Study participants
Participants in the survey were approached during the yearly patient meeting about PH at the VUmc on 29 March 2014. Because data were provided anonymously, no written informed consent was requested. For reasons of statistical power, both patients with PH and PAH were approached to complete the survey.
Methods
The anonymous survey was composed of questions regarding demographic information (age; gender; and year of diagnosis), validated scales concerning distress and experienced problems, and questions derived from the first set of qualitative interviews. The degree of distress was measured by the Dutch version of the Distress Thermometer.20 This is a validated scale, originally developed among cancer patients, scoring the degree of distress (on an illustration of a thermometer) from zero (no distress) to ten (extreme distress).20 Furthermore, the presence of problems in several areas was assessed using the Problem List, which is often used in combination with the Distress Thermometer. The Problem List consists of 47 problem items, divided into five categories: practical (seven items); social (three items); emotional (ten items); spiritual (two items); and physical (25 items) problems.20 Patients were asked to indicate which of these problems were present in the past week (yes/no). Additionally, we formulated six problem areas based on the first set of qualitative interviews: (1) a lack of understanding by others; (2) involuntary childlessness; (3) loneliness; (4) anxiety regarding their future; (5) worries concerning the heredity of PAH/PH; and (6) experiencing restrictions in autonomy (making your own choices). Patients were asked to rate how much they were bothered by these problems on a 4-point Likert scale (ranging from “not at all” to “very much”). Finally, the survey assessed if patients received professional support for psychological, social, or coping problems over the last 12 months, current need for support, and preferred professional for mental support. As the level of distress measured by the Distress Thermometer was not normally distributed, non-parametric tests (Mann–Whitney U and Spearman’s Rho) were executed to analyze the relationship between gender, age, and level of distress. Logistic regression analyses were performed to evaluate the relationship between need for support and demographic and clinical variables (gender, age, and level of distress). For the association between problems as rated on the Problem List and the need for support, a prediction model was created using logistic regression analysis with backward selection. The quantitative data analysis was performed using SPSS 20.0.21
Results
Qualitative data
Of the 27 patients who were approached, 24 patients were interviewed. One patient declined to participate (reason unknown) and two patients were unable to participate at the time because of personal circumstances. The majority of the participants were women (20 women, three men, and one transgender). The age of the participants was in the range of 26–69 years and they were diagnosed with PAH 0–16 years ago. In eight of the 24 interviews, the patients’ partner was present at the patient’s request. After 20 interviews, data saturation was achieved, which was confirmed in four extra interviews.
Experienced problems
All patients experienced specific problems related to PAH, albeit in different degrees. Patients mentioned a low and fluctuating energy level, difficulties with a loss of abilities, worries, and feelings of insecurity with regard to future prospects. Patients also struggled with their restricted abilities in fulfilling their roles of being a parent, partner, or employee. Many patients felt misunderstood by others, which was mainly attributed to their confusingly healthy appearance and unfamiliarity of PAH within society.
“Because of the medication your veins are more open. So you always have a reddish glow on your face. Everybody is always saying: ‘You’re looking so good!’” (Patient 9)
The nature of experienced problems was related to the phase of the disease. For example, the period from the onset of symptoms until the diagnosis of PAH was perceived as very stressful, uncertain, and disturbing. In this period, survival was their main concern. After this initial period, when their condition was relatively stable, patients were more occupied with the impact PAH has on their daily lives. Patients mentioned that they felt anxious, frustrated, or depressed at times. The confrontation with an approaching death and the future of the patient or surviving relatives were often reasons for anxiety. Some patients mentioned an anxiety response provoked by the physical symptoms induced by PAH such as an elevated heart rate and shortness of breath.
“My heart would often start racing, beating very fast. Then it turned out that the disease had got worse, so they upped my medication a lot. Well, of course that makes you anxious.” (Patient 23)
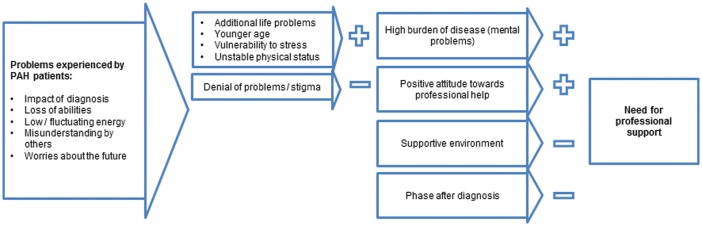
The relationship of experienced problems related to PAH and need for support is illustrated in Fig. 1.
Fig. 1.
Pathways to mental problems and need for professional support in PAH patients. PAH: pulmonary arterial hypertension.
Pathways to mental problems
Although many patients mentioned that negative emotions were frequently present, patients often stated these were of a transient nature and they were able to cope with them on their own. An important influence for the ability to cope with problems seemed to be the support from the environment. Many patients felt supported by their partner or others, strengthening their coping and resilience. Patients who were creative in finding alternative behavior seemed less affected by disability imposed by having PAH. For example, patients mentioned riding an electric bicycle to manage their limited amount of energy. Patients expressed a capability of putting things in perspective or employed positive thinking in order to cope with the difficulties related to PAH.
“I often push myself to the limit. And afterwards I have to take things very easily for a couple of days. But it’s my choice, because I love going to festivals. I only go for one day, and have to take it easy. […] Of course, I could cry about not being able to join my friends who all go for three days, but I’m glad I can still do it this way. Because before I couldn’t.” (Patient 5)
Certain problems or personal characteristics seemed to be related to the presence of psychological distress. For instance, women of childbearing age reported feelings of depression as a consequence of the PAH-induced inability (high risk of complications) to have children. A tendency to give up, deny, or continuing to resist declining abilities seemed to be related to experiencing mental problems such as anxiety and depression. Age also seemed to be related to the impact of PAH, with younger patients expressing more difficulties in adjusting and accepting PAH due to the influence of PAH on their young lives and future prospects. Also, patients mentioned that additional life problems, such as the loss of a loved one and financial or relationship problems, were affecting their emotional state.
“The year I got diagnosed I was also in the middle of a divorce. I had three small children to look after and I was working. It was a really difficult time for me.” (Patient 12)
Need for professional support
Some patients were not open to mental support, irrespective of their experienced problems. Patients who expressed no need for support mentioned facing few or no problems due to the PAH physically or emotionally, did not want to acknowledge or discuss the disease, they already received enough support and/or were able to cope with the disease themselves (Fig. 1).
“Of course, it’s also difficult for him [partner] but he stands behind me all the way. And, umm, he has an understanding. When I can’t keep up, he adjusts his pace. […] So, when you see how helpful he is, that’s just so nice. He’s known about everything from the beginning and that feels really good.” (Patient 25)
Generally, most patients expressed some need for mental support, varying according to the phase of the disease, type of problems, experienced emotional distress, and availability of support from significant others. Concerning the period right after diagnosis, patients expressed a need for practical information, but virtually no need for mental support during this period, although some valued the idea that support was available when needed. Patients stated that they could use practical information and advice on how to deal with the consequences of PAH. A need for professional counseling or therapy was mainly desired by patients who experienced difficulties in coping with worries or emotions, who experienced low support from significant others, or who suffered from additional life events. Many patients preferred these needs to be met by a professional with specific knowledge of PAH, for instance explained thus by a female patient:
“Sometimes you have a problem […] but then it’s better to talk to someone professional [….] maybe find a solution together. That’s different from talking to your friends, who aren’t familiar with these issues.” (Patient 13)
Quantitative data
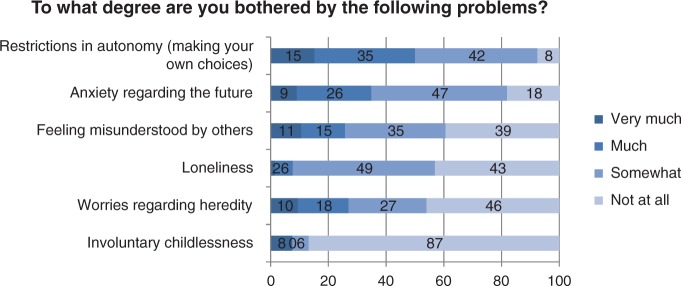
Of the 75 patients who attended the meeting, 67 PAH/PH patients completed the survey. Table 1 shows patients’ characteristics and scores on the questionnaires. From the problem themes identified in the qualitative study, “anxiety regarding the future” and “experienced restrictions in their autonomy” were most often recognized as burdensome (Fig. 2).
Table 1.
Characteristics of survey participants and results on the Distress Thermometer, Problem List, and help-seeking items (n = 67).
| n (%)/mean (SD) | |
|---|---|
| Age (years) (mean (SD)) | 55.2 (16.2) |
| Female (n (%)) | 51 (76) |
| Years lived with PAH/PH diagnosis (mean (SD)) | 6.5 (4.8) |
| Distress, mean (SD) | 5.35 (2.34) |
| Problem List, experiencing problem in the past week (n (%)) | |
| Practical problems | |
| Child care | 12 (18.8) |
| Housing | 11 (16.9) |
| Housekeeping | 38 (56.7) |
| Transportation | 13 (20) |
| Work/school/study | 17 (28.3) |
| Financial | 12 (18.5) |
| Insurance | 5 (7.7) |
| Family/social problems | |
| Dealing with partner | 9 (14.8) |
| Dealing with children | 11 (17.7) |
| Dealing with friends/family | 18 (27.7) |
| Emotional problems | |
| Keeping emotions under control | 27 (40.9) |
| Memory | 30 (45.5) |
| Self confidence | 27 (40.3) |
| Fears | 22 (33.3) |
| Depression | 24 (35.8) |
| Tension/nervousness | 27 (40.3) |
| Loneliness | 19 (29.2) |
| Concentration | 33 (50) |
| Feelings of guilt | 18 (28.1) |
| Loss of control | 19 (29.7) |
| Religious/spiritual concerns | |
| Meaning of life | 13 (20.3) |
| Trust in God/religion | 12 (17.9) |
| Physical problems | |
| Appearance | 17 (25.4) |
| Changes in urination | 14 (21.5) |
| Constipation | 12 (18.8) |
| Diarrhea | 18 (27.7) |
| Eating | 13 (19.4) |
| Feeling swollen | 27 (40.9) |
| Fever | 7 (10.8) |
| Mouth sores | 14 (21.2) |
| Nausea | 21 (32.3) |
| Nose dry/congested | 38 (57.6) |
| Pain | 26 (40.6) |
| Sexual | 11 (17.2) |
| Skin dry/itchy | 30 (46.2) |
| Sleep | 33 (51.6) |
| Shortness of breath/breathing | 40 (60.6) |
| Dizziness | 32 (49.2) |
| Speech/talking | 14 (21.2) |
| Taste | 8 (12.1) |
| Weight change | 26 (38.8) |
| Tingling in hands/feet | 24 (36.4) |
| Bathing/dressing | 21 (31.8) |
| Daily activities | 32 (48.5) |
| Fatigue | 58 (87.9) |
| Out of shape/condition | 54 (81.8) |
| Muscle strength | 45 (68.2) |
| Help seeking (n (%)) | |
| Did seek professional support in the previous 12 months | 15 (23.4) |
| In need for professional support, Yes/Maybe | 14 (23)/17 (27.9) |
PAH/PH: pulmonary arterial hypertension/pulmonary hypertension.
Fig. 2.
Perceived distress related to problem areas as reported by PAH/PH patients (n = 67).
Of the participants, 14 (23%) patients responded “yes” and 17 (27.9%) “maybe” to the question of whether they were in need of support for social or psychological problems, or for coping with PAH/PH. Age was significantly associated with level of distress, with younger patients reporting higher scores on the Distress Thermometer (Spearman’s Rho = –0.25, P = 0.05). Women reported a higher level of distress (M = 5.6; SD = 2.4) than men (M = 4.8, SD = 2.3), but this difference was not significant (Mann–Whitney U-test; z = 1.23, P = 0.22). Regarding the need for support, a significant association was found with age (odds ratio [OR] = 0.97, 95% confidence interval [CI] = 0.93–0.99, P = 0.04) but not with the level of distress (OR = 1.02, 95% CI = 0.99–1.04, P = 0.10). A multivariate logistic regression analysis for the emotional variables of the Problem List showed a trend for anxiety (OR = 3.83, 95% CI = 0.9–16.3, P = 0.07) and a significant association for depression (OR = 11.44, 95% CI = 2.7–48.7, P = 0.001) with need for support.
Discussion
This study confirms that although many patients are resilient to stress caused by PAH, mental problems are common. More than half of the patients are in need or may be considering professional support for mental problems or coping with PAH/PH. Patients expressing symptoms of depression had an increased need for mental or social support, together with younger patients, and possibly patients with anxiety symptoms.
Overall, PAH patients face similar problems related to their disease. Patients have to deal with the impact of the diagnosis, loss of abilities, finding a new balance in energy, worries, feelings of anxiety, frustration or depression, misunderstanding by others, and a changing role in life. The inability to have children due to the disease is particularly challenging for female patients of childbearing age. Also, unfamiliarity with a rare disease such as PAH and the healthy appearance of patients were specific aspects which led to misunderstandings between PAH patients and their social environment. Our results are in agreement with previous studies that mentioned similar themes.7,15 Our study adds to these results by focusing on pathways to mental problems and need for support. We found that experiencing problems related to PAH does not directly lead to having mental problems. Having a supportive environment, a stable physical condition, the ability to creatively adapt to new circumstances, and positive thinking all seem to make patients resilient to the stress caused by PAH. By contrast, additional life problems, a younger age, denial, or resisting problems caused by PAH and experienced low support from significant others were related to the expression of mental problems.
Although mental problems were frequently mentioned as a reason to seek mental support, this relationship was not exclusive. Some patients were not in need of support because they were able to cope with the disease on their own or received sufficient support from significant others. However, some patients did express mental problems due to PAH but were still unwilling to seek help. This may have to do with difficulties in acknowledging the existence of their problems and accepting psychological support, as was previously identified in COPD patients.22 Unwillingness to talk and fear of stigma were found in comparable studies as well.20,23
Patients also expressed different needs for support according to the phase of the disease and specific issues patients were dealing with. Immediately after diagnosis, patients were in need of practical information and advice; it was only later on in the disease process that patients more readily expressed a need for mental support.
The results of the survey confirmed data from our qualitative study. Specific themes that were derived from the interviews (i.e. feeling misunderstood, anxiety/worries about the future, and restrictions in autonomy) were recognized in our quantitative study by a large proportion of patients. Furthermore, the survey confirmed the need for professional support as half of the patients stated they were in need of, or considering professional support for mental or social problems, or coping with PAH/PH. These results correspond to the 57% PH patients in need for support reported by Larisch et al.16 Results of the survey also confirmed that distress related to PAH/PH was quite high: the mean score on the Distress Thermometer was 5.35 and a score of >5 is generally considered to indicate clinical levels of distress.24 Although this seems counter-intuitive, the level of distress was not significantly related to a need for support. This finding is consistent with research in cancer patients24 and can also be explained by our qualitative results which stress the role of a supportive environment, the disease status, and cognitions about help seeking as significant factors in the relationship between mental distress and need for support. Results from the survey indicate that feelings of depression and anxiety, rather than general distress, are related to the need for support. This finding is important, as feelings of anxiety and depression have a significant influence on the quality of life and can be treated effectively.5,14,25 In fact, a recent meta-analytic review found positive effects of therapist-guided Internet-based cognitive behavioral therapy for patients with chronic conditions on generic psychological measures, physical measures, and disease impact.26 Younger patients in particular should be focused on, as findings from both our qualitative and quantitative study point to younger patients being more likely to express a need for professional support.
A strength of this study is the use of a mixed method analysis, as the quantitative data can verify and enrich qualitative data. Another strength is that two researchers performed the interviews, having the opportunity to exchange information, share visions, and discuss data (constant comparison method). A limitation of the study is that the presence of mental disorders was not systematically assessed. For pragmatic reasons, we did not include a quality-of-life questionnaire, which may limit comparison with other studies in this area. Additionally, the inability to distinguish PAH from PH patients in the quantitative analysis is considered as a limitation as well. PH includes several variants of the disease, which differ in cause and progression. As the physical condition and disabilities caused by PAH may be related to need for support, this may have influenced the quantitative results. Furthermore, as data for the quantitative study were collected at the yearly patient meeting, we may have reached a specific subgroup of PH patients. Unfortunately, we do not have information about differences between patients who do or do not attend these meetings. However, Larisch et al. found similar results regarding need for support in a sample of 187 PH patients.16
This study identified that patients with PAH experience comparable mental problems and about half of the PAH patients are in need of or are considering mental support. Common problems such as adjusting to a loss of abilities, finding a balance in energy level, coping with the social environment, and handling of worries and negative emotions should be addressed when supporting patients. Feelings of depression and (possibly) anxiety, rather than general distress level, were related to need for support. Need for support was based on an interplay between resilience, additional life problems, experienced support from significant others, phase of the disease, age and willingness to accept help. Future research should evaluate specific interventions to support patients with PAH to decrease mental distress. Preferably, this support is tailored to the phase of the disease and the personal needs of the patient and is offered by a PAH professional in standard treatment.
Acknowledgements
The authors thank physician’s assistant Martha Wagenaar (BSc) for assisting in the patient recruitment and specialist nurse Karin Taat (BSc) for assisting in data collection and analysis.
Conflict of interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Hoeper MM, Bogaard HJ, Condliffe R, et al. Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol 2013; 24: 42–50. [DOI] [PubMed] [Google Scholar]
- 2.Thenappan T, Shah SJ, Rich S, et al. Survival in pulmonary arterial hypertension: a reappraisal of the NIH risk stratification equation. Eur Respir J 2010; 35: 1079–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benza RL, Miller DP, Gomberg-Maitland M, et al. Predicting survival in pulmonary arterial hypertension. Circulation 2010; 122: 164–17. [DOI] [PubMed] [Google Scholar]
- 4.Delcroix M, Howard L. Pulmonary arterial hypertension: the burden of disease and impact on quality of life. Eur Respir Rev 2015; 24: 621–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harzheim D, Klose H, Pinado FP, et al. Anxiety and depression disorders in patients with pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension. Respiratory Research 2013; 14: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shafazand S, Goldstein MK, Doyle RL, et al. Health-related quality of life in patients with pulmonary arterial hypertension. Chest 2004; 126: 1452–1459. [DOI] [PubMed] [Google Scholar]
- 7.Aldrighetti R, Armstrong, I, Ferrari, P, et al. The impact of pulmonary arterial hypertension (PAH) on the lives of patients and carers: results from an international survey. Report. European Pulmonary Hypertension Association (PHA). http://www.phaeurope.org/wp-content/uploads/International-PAH-patient-and-Carer-Survey-Report-FINAL1.pdf (September 2012, accessed 26 July 2017).
- 8.Mathai SC, Ghofrani HA, Mayer E, et al. Quality of life in patients with chronic thromboembolic pulmonary hypertension. Eur Respir J 2016; 48: 526–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Badesch D, Raskob G, Elliott C, et al. Pulmonary arterial hypertension: baseline characteristics from the REVEAL registry. Chest 2010; 137: 376–387. [DOI] [PubMed] [Google Scholar]
- 10.Lowe B, Grafe K, Ufer C, et al. Anxiety and depression in patients with pulmonary hypertension. Psychosom Med 2004; 66: 831–836. [DOI] [PubMed] [Google Scholar]
- 11.McCollister DH, Beutz M, McLaughlin V, et al. Depressive symptoms in pulmonary arterial hypertension: prevalence and association with functional status. Psychosomatics 2010; 51: 339–339. [DOI] [PubMed] [Google Scholar]
- 12.Van Hoof J, Delcroix M, Vandevelde E, et al. Emotional symptoms and quality of life in patients with pulmonary arterial hypertension. J Heart Lung Transplant 2014; 33: 800–808. [DOI] [PubMed] [Google Scholar]
- 13.Watkins LL, Koch GG, Sherwood A, et al. Association of anxiety and depression with all-cause mortality in individuals with coronary heart disease. J Am Heart Assoc 2013; 19: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Panagioti M, Scott C, Blakemore A, et al. Overview of the prevalence, impact, and management of depression and anxiety in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2014; 9: 1289–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guillevin L, Armstrong I, Aldrighetti R, et al. Understanding the impact of pulmonary arterial hypertension on patients’ and carers’ lives. Eur Respir Rev 2013; 22: 535–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Larisch A, Neeb C, De Zwaan M, et al. Mental distress and wish for psychosomatic treatment of patients with pulmonary hypertension. Psychother Psychosom Med Psychol 2014; 64: 384–389. [DOI] [PubMed] [Google Scholar]
- 17.Boeije H. A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Quality and Quantity 2002; 36: 391–409. [Google Scholar]
- 18.MAXQDA, software for qualitative data analysis, 1989–2015, VERBI Software – Consult. Berlin, Germany: Sozialforschung GmbH, 2015.
- 19.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007; 19: 349–357. [DOI] [PubMed] [Google Scholar]
- 20.Tuinman MA, Gazendam-Donofrio SM, Hoekstra-Weebers JE. Screening and referral for psychosocial distress in oncologic practice. Cancer 2008; 113: 870–878. [DOI] [PubMed] [Google Scholar]
- 21.IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.
- 22.Ellison L, Gask L, Bakerly ND, et al. Meeting the mental health needs of people with chronic obstructive pulmonary disease: a qualitative study. Chronic Illn 2012; 8: 308–320. [DOI] [PubMed] [Google Scholar]
- 23.Baker-Glenn EA, Park B, Granger L, et al. Desire for psychological support in cancer patients with depression or distress: validation of a simple help question. Psychooncology 2011; 20: 525–531. [DOI] [PubMed] [Google Scholar]
- 24.Tuinman MA, Van Nuenen FM, Hagedoorn M, et al. Distress, problems and referral wish of cancer patients: differences according to relationship status and life phase. Psychooncology 2015; 24: 699–704. [DOI] [PubMed] [Google Scholar]
- 25.Van Beek MH, Oude Voshaar RC, Beek AM, et al. A brief cognitive-behavioral intervention for treating depression and panic disorder in patients with noncardiac chest pain: a 24-week randomized controlled trial. Depress Anxiety 2013; 30: 670–678. [DOI] [PubMed] [Google Scholar]
- 26.Van Beugen S, Ferwerda M, Hoeve D, et al. Internet-based cognitive behavioral therapy for patients with chronic somatic conditions: a meta-analytic review. J Med Internet Res 2014; 16: e88. [DOI] [PMC free article] [PubMed] [Google Scholar]