Abstract
Light chain (AL) amyloidosis is caused by a usually small plasma-cell clone that is able to produce the amyloidogenic light chains. They are able to misfold and aggregate, deposit in tissues in the form of amyloid fibrils and lead to irreversible organ dysfunction and eventually death if treatment is late or ineffective. Cardiac damage is the most important prognostic determinant. The risk of dialysis is predicted by the severity of renal involvement, defined by the baseline proteinuria and glomerular filtration rate, and by the response to therapy. The specific treatment is chemotherapy targeting the underlying plasma-cell clone. It needs to be risk-adapted, according to the severity of cardiac and/or multi-organ involvement. Autologous stem cell transplant (preceded by induction and/or followed by consolidation with bortezomib-based regimens) can be considered for low-risk patients (~20%). Bortezomib combined with alkylators is used in the majority of intermediate-risk patients, and with possible dose escalation in high-risk subjects. Novel, powerful anti-plasma cell agents were investigated in the relapsed/refractory setting, and are being moved to upfront therapy in clinical trials. In addition, the use of novel approaches based on antibodies targeting the amyloid deposits or small molecules interfering with the amyloidogenic process gave promising results in preliminary studies. Some of them are under evaluation in controlled trials. These molecules will probably add powerful complements to standard chemotherapy. The understanding of the specific molecular mechanisms of cardiac damage and the characteristics of the amyloidogenic clone are unveiling novel potential treatment approaches, moving towards a cure for this dreadful disease.
Keywords: amyloidosis, light chains, diagnosis, therapy, response
Introduction
Immunoglobulin light chain (AL) amyloidosis is the most common form of systemic amyloidosis, accounting for approximately 70% of all subjects suffering from these diseases.1 It is caused by a plasma cell clone that infiltrates the bone marrow by less than 10% in half of the patients. Despite its relatively small size, the clone can set off a devastating multi-organ damage caused by the monoclonal light chain.2 The amyloidogenic light chain misfolds and aggregates, depositing in tissues in the form of amyloid fibrils.3 All organs, except for the central nervous system, can be affected by this process, that leads to irreversible organ dysfunction and death if unrecognized or treated ineffectively.3 In the last 15 years, we have made substantial progress in understanding the biology of the amyloid plasma cell clone and the mechanisms of organ damage. Moreover, with accurate prognostic stratification and response assessment based on biomarkers of clonal and organ disease, we have learnt to safely apply treatments originally developed for multiple myeloma, to the fragile patients with AL amyloidosis.2,4,5 Nevertheless, the timely recognition and the appropriate treatment of patients with AL amyloidosis remains challenging even for hematologists who are expert in multiple myeloma. In this review, we summarize the current knowledge on the pathogenesis of AL amyloidosis, and we focus on the clinical management of patients with this disease.
The Amyloid Clone and Mechanisms of Organ Damage
Not only is the amyloidogenic clone usually smaller in size than that causing multiple myeloma, but it is characterized by a significant frequency of chromosomal abnormalities, that can affect treatment outcomes. The most frequent is t(11;14) translocation, observed in almost 50% of patients.6 The presence of t(11;14) is associated with poorer outcome with bortezomib-based and immunomodulatory (IMiDs)-based therapy, even when cyclophosphamide is added.7,8 The adverse impact of t(11;14) can be overcome by melphalan, administered orally or in autologous stem cell transplant.9,10 Gain of 1q21 is less frequent in AL amyloidosis than in multiple myeloma, being found in less than 20% of patients.6 Patients harboring this abnormality have poorer outcome when treated with oral melphalan/dexamethasone (MDex) without the addition of bortezomib.11 Clonal plasma cells in AL amyloidosis have similar phenotypic and copy number alteration profiles as those found in multiple myeloma, but their gene expression profile is similar to that of normal plasma cells.12 A genome-wide association study showed a shared genetic susceptibility between AL amyloidosis and multiple myeloma, but cyclin D1 was a more prominent driver in AL amyloidosis.13 The plasma cells rely on the proteasome to cope with the proteotoxicity exerted by the misfolded, amyloidogenic light chains.14–16 This makes the amyloid plasma cell clone keenly sensitive to proteasome inhibitors.
The light chain variable region gene and the gene family of the clone can, at least in part, explain the variable organ tropism of AL amyloidosis. Indeed, three Vl genes, IGLV2–14, IGVL6-57, and IGLV3-1 contribute to encoding the majority of amyloidogenic l light chains.17–19 The germline gene LV6-57 is common in AL amyloidosis while it is exceedingly rare in normal B-cells, and it is associated with renal involvement.20 Usage of LV1-44 germline gene is linked to predominant cardiac involvement, whereas KV1-33 is associated with involvement of the liver.21
Since cardiac involvement is the main determinant of survival, efforts have been focused on unveiling the mechanisms of cardiac dysfunction in AL amyloidosis. The observation of complete clinical recovery of patients after effective chemotherapy in the absence of significant reduction of amyloid deposits indicates that the mass action caused by the deposits is not the only, and possibly not the main, determinant of organ dysfunction in AL amyloidosis. The availability of cardiac biomarkers, particularly N-terminal pro-natriuretic peptide type B (NT-proBNP) as a measure of amyloid cardiac dysfunction, showed that the clinical severity of heart failure and patient survival is linked to changes in the concentration of the circulating amyloidogenic free light chains rather than to changes in the amyloid load.22–24 Indeed, the infusion of light chain purified from the urine of patients with cardiac amyloidosis causes a rapid increase in end-diastolic pressure in isolated mouse hearts in a matter of few minutes, which is not observed with control light chains.25 Exposing Caenorhabditis elegans, a worm whose pharynx pulses rhythmically and is considered an analog of the vertebrate heart, to light chains of patients with cardiac AL amyloidosis, but not to control light chains, reduces the rate of pharynx contraction.26
Finally, the injection of light chains from patients with cardiac AL amyloidosis in the heart of zebrafish reduces the cardiac output and the lifespan of the fishes in the absence of amyloid deposits, which is not observed with control light chains.27 Overall, this clinical and experimental evidence point to the toxicity exerted by the circulating precursor as the main cause of cardiac dysfunction in AL amyloidosis.28,29
Clinical Presentation and Diagnosis
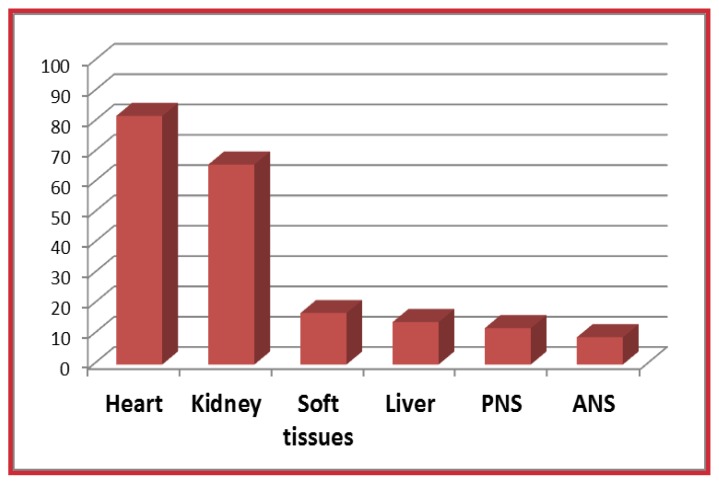
The clinical manifestations of AL amyloidosis depend on organ involvement (Figure 1) but are rarely specific. Involvement of the soft tissues with macroglossia, periorbital purpura, submandibular gland swelling, and shoulder pad sign can easily trigger the diagnosis but are uncommon. More frequently, AL amyloidosis manifests with sign and symptoms resembling those of more common conditions of the elderly. Cardiac involvement (approximately 80% of patients) manifests with heart failure with preserved ejection fraction. Echocardiography is the cornerstone of the assessment of amyloid cardiomyopathy revealing increased ventricular wall thickness and granular sparkling. While ejection fraction is usually preserved until late stages of the disease, longitudinal strain, and midwall fractional shortening are often altered and have prognostic relevance.30,31 Electrocardiogram usually shows low limb voltages in cardiac AL amyloidosis. Late gadolinium enhancement at cardiac magnetic resonance strongly points to the diagnosis of heart involvement; moreover, cardiac magnetic resonance can quantify the extracellular volume that may reflect the amyloid load.32 The scintigraphy tracers developed for imaging the amyloid deposits in the brain of patients with Alzheimer disease, can identify cardiac amyloidosis and are promising tools for detecting and possibly quantitating amyloid deposits also in systemic amyloidoses.33 The uptake of bone tracers in patients with AL amyloidosis is absent or moderate, differently from transthyretin cardiac amyloidosis, characterized by a strong uptake. This difference can be used to distinguish between the two forms.34 Increased concentrations of NT-proBNP are found in 100% of patients with cardiac AL amyloidosis, and precede symptoms and imaging alterations, allowing diagnosis at very early stages.22,35 The kidney is involved in two-thirds of patients with AL amyloidosis. The disease manifests with albuminuria, evolving in nephrotic syndrome and progressing to renal failure eventually leading to end-stage renal disease if unrecognized or ineffectively treated. Involvement of the liver is characterized by organ enlargement without scan defects and elevation of alkaline phosphatase. Peripheral neuropathy is axonal, predominantly sensory and centripetal. Involvement of the autonomic nervous system is common but usually asymptomatic, although it can often become manifest with inappropriate use of hypotensive drugs. It is characterized by postural hypotension that can be preceded by the “resolution” of a pre-existing hypertension, erection defects in males and disturbances in bowel movements. General symptoms, most commonly profound fatigue and malnutrition, often accompany more organ-specific manifestations.
Figure 1.
Organ involvement in 1065 patients with AL amyloidosis.
The patients were diagnosed between 2004 and 2015 at the Pavia Amyloidosis Research and Treatment Center. PNS, peripheral nervous system; ANS, autonomic nervous system.
These clinical manifestations are not only resembling those of more common conditions, but they are usually associated with advanced stages of the disease. All this, unfortunately, results in frequent diagnostic delays. A recent survey showed that 40% of patients with AL amyloidosis remain undiagnosed 1 year after the onset of symptoms.36 Similar delays are also observed in patients who are performing regular follow-up for monoclonal gammopathy of undetermined significance (MGUS) under the supervision of hematologists.37 This is because the classical workup of patients with MGUS does not include appropriate, sensitive tools for the detection of the onset of organ involvement. Thus, we advocated the inclusion of sensitive markers of cardiac (NT-proBNP) and renal (albuminuria) amyloidosis in the regular follow-up of patients with MGUS and abnormal free light chain (FLC) ratio.35,38
Once amyloidosis is suspected, the diagnosis requires the demonstration of amyloid deposits in a biopsy. The abdominal fat aspirate is simple and minimally invasive, although its interpretation requires expertise. In combination with biopsy of the bone marrow stained with Congo red and/or biopsy of a minor salivary gland, it can yield a diagnostic sensitivity of approximately 90%, thus sparing organ biopsies.39–41 Nevertheless, organ biopsies may need to be performed in subjects with strong clinical suspicion and negative fat, gland, and bone marrow. Typing of the amyloid deposits is mandatory, in order to avoid misdiagnosis between AL amyloidosis and other common forms of systemic amyloidosis (listed in Table 1), such as hereditary or wild-type (formerly senile) transthyretin amyloidosis, hereditary apolipoprotein AI amyloidosis, leucocyte chemotactic factor-2 amyloidosis, and amyloidosis reactive to chronic inflammation. Incorrect typing could lead to disastrous therapeutic errors.42–44 Unfortunately, light microscopy immunohistochemistry and immunofluorescence with commercial antibodies, the most commonly available techniques, are unreliable to characterize amyloid deposits.45,46 Thus, in most instances a reliable diagnosis requires referral of patients to specialized centers. Light microscopy immunohistochemistry can be reliably performed at referral centers using custom-made antibodies.47 Immunoelectron microscopy with commercial antibodies can correctly identify the amyloid type in almost 100% of patients.40 Mass spectrometry-based proteomics can be used on whole tissues or after laser capture microdissection to reliably type amyloid deposits.48,49
Table 1.
Common types of systemic amyloidosis.
| Amyloid type | Precursor protein | Acquired / Hereditary | Organ involvement |
|---|---|---|---|
| Systemic AL | Monoclonal LCs | Acquired | All organs (except the brain) |
| Localized AL | Monoclonal LCs | Acquired | Skin, tracheobronchial tree, lungs, urinary bladder, (others) |
| ATTRwt | Wild type transthyretin | Acquired | Heart, soft tissue, lung |
| ATTRm | Mutated transthyretin | Hereditary | Hear, PNS/ANS |
| AA | Apolipoprotein serum amyloid A | Acquired | Kidney, heart, liver, lung |
| ApoAI | Apolipoprotein AI | Hereditary | Liver, testis, heart, PNS |
| ALECT2 | Leukocyte Chemotactic Factor-2 | Acquired | Kidney, primarily |
The amyloid types are identified by acronyms where the letter “A” for amyloidosis is followed by the abbreviation of the protein forming the amyloid fibrils. ANS, autonomic nervous system; LCs, immunoglobulin light chains; PNS, peripheral nervous system.
Once the diagnosis and typing of AL amyloidosis have been established, the diagnostic workup is completed by assessing the burden and severity of clonal and organ disease, as summarized in Table 2. Given the small size of the amyloid plasma cell clone, the combination immunofixation of both serum and urine with measurement of circulating free light chain is required to grant adequate sensitivity.50–53 Assessment of organ involvement is based on biomarkers, electrocardiogram, and imaging studies.
Table 2.
Assessment of clonal and organ disease in patients with AL amyloidosis.
| Assessment of clonal disease |
|
| Assessment of organ disease |
Heart
|
FISH, fluorescence in situ hybridization; NT-proBNP, N-terminal natriuretic peptide type B; Cardiac MRI, cardiac magnetic resonance imaging; eGFR, estimated glomerular filtration rate; US, ultrasound-sonography; CT, computer tomography.
Staging
The survival of patients with AL amyloidosis is exceedingly heterogeneous, depending on the severity of cardiac dysfunction at the time of diagnosis: while patients who are diagnosed late, at a stage when heart damage is very advanced and not amenable of improvement with treatment survive only a few weeks, patients without heart involvement can survive years even if they fail to respond to therapy. This extreme heterogeneity requires accurate prognostic stratification for establishing the best therapeutic approach, balancing treatment intensity and rapidity of action with patients’ frailty, as well as for comparing results of clinical trials. The Mayo Clinic group established a simple and reliable staging system based on NT-proBNP and cardiac troponins, which was then modified by European investigators (Table 3).54,55 This staging system is now the most widely used for clinical trial design and patient management. Besides heart involvement, clonal burden, assessed by bone marrow plasma cell (BMPC) infiltration or dFLC (difference between involved and uninvolved circulating free light chains) has an independent impact on survival. Patients with AL amyloidosis and BMPC infiltrate >10% have a more reduced survival, which is comparable to that of patients who have concomitant overt multiple myeloma.56 Subjects who have a very low (<50 mg/L) dFLC level have a significantly better outcome across cardiac stages.57,58 The Mayo Clinic group has incorporated the dFLC level in the cardiac staging system (Table 3).59 The severity of renal involvement does not directly affect patient’s survival, but impacts the quality of life and reduces the access to effective therapy. A staging system predicting progression to dialysis has been proposed and validated by European investigators (Table 3).60 Similarly to heart involvement, recognition and prompt treatment of renal AL amyloidosis at early stages can almost abolish the risk of progression to dialysis, while late diagnosis at advanced stages is associated with higher risk of progression.
Table 3.
Staging of cardiac and renal damage in AL amyloidosis.
| Staging system | Markers and thresholds | Stages | Outcomes* |
|---|---|---|---|
| Cardiac54,55 | NT-proBNP >332 ng/L cTnT >0.035 ng/mL (or cTnI > 0.01 ng/mL) |
|
|
| Revised Mayo Clinic 139 | NT-proBNP >1800 ng/L cTnT >0.025 ng/mL dFLC >180 mg/L |
|
|
| Renal60 | eGFR <50 mL/min per 1.73 m2 proteinuria >5 g/24h |
|
|
cTn, cardiac troponin; dFLC, difference between involved (amyloidogenic) and uninvolved circulating free light chain; eGFR, estimated glomerular filtration rate; NT-proBNP, N-terminal pro-natriuretic peptide type-B.
Observed in 1065 patients with AL amyloidosis newly diagnosed at the Pavia Amyloidosis Research and treatment center.
Treatment
The complexity of AL amyloidosis, which is due to the unique coexistence of a clonal plasma cell disorder and dysfunction multiple vital organs, makes treatment of this disease a challenge even for hematologists who are experts in the field of multiple myeloma. Indeed, the availability of new drugs, directly targeting the amyloid deposits, will probably displace AL amyloidosis from the realm of exclusive hematologic therapy. The experience of treating physicians significantly impacts patients’ outcomes,61 and very few recent prospective controlled studies exist to guide the therapeutic strategy. Thus, whenever possible, patients should be referred to specialized centers for treatment. Indeed, the amyloid clone requires treatment even if in the vast majority of cases it does not meet the criteria for treating multiple myeloma.62 Moreover, differently from patients with multiple myeloma, subjects suffering from AL amyloidosis are at high risk of death and are extremely susceptible to treatment toxicity in the first few months after diagnosis; whereas, if they survive this first dangerous time, they enjoy a better long-term outcome compared to myeloma patients.63 For this reason, chemotherapy is usually delivered at the lowest effective dose during the first cycles. The treatment strategy needs to be adapted to early treatment efficacy and should not be planned in advance. The response should frequently be assessed, at least every 2 cycles, in order to allow rapid switch to rescue therapy in patients who do not achieve satisfactory response. The criteria for hematologic,57,58,64 cardiac,64 and renal60 response (summarized in Table 4) have been established and validated in a huge international effort and offer guidance to individual patients treatment, as well as surrogate endpoints for clinical trials.65 In particular, a new criterion where both hematologic and organ response can be assessed simultaneously early on in the treatment of AL amyloidosis was proposed to stratify the risk of patients, supporting its use as a surrogate end-point in clinical trials.66 In addition, a recent report from Mayo Clinic showed that the better survival was assessed in patients who obtained the deeper organs (heart, kidney, liver).67
Table 4.
Validated criteria for response assessment in AL amyloidosis. Response criteria are validated in independent patient populations for use at 3 and 6 months after treatment initiation.
| Hematologic response | Definition |
|---|---|
| Complete response (CR) | Negative serum and urine immunofixation and normal FLC ratio |
| Very good partial response (VGPR) | dFLC <40 mg/L |
| Partial response (PR) | dFLC decrease >50% compared to baseline |
| low-dFLC response* | dFLC <10 mg/L |
| Cardiac response | Definition |
| Pre-treatment NT-proBNP ≥650 ng/L | Decrease of NT-proBNP by >30% and 300 ng/L |
| Pre-treatment NYHA class III or IV | At least 2 points decrease of NYHA class |
| Renal response | Definition |
| Pre-treatment proteinuria >0.5 g/24h | At least 30% decrease in proteinuria or drop below 0.5 g/24 hour, in the absence of renal progression defined as a >25% decrease in eGFR |
in patients with baseline dFLC >20 mg/L and <50 mg/L.
FLC, free light chain; dFLC, difference between involved and uninvolved light chain; NT-proBNP, N-terminal pro natriuretic peptide type B; NYHA, New York Heart Association; eGFR, estimated glomerular filtration rate.
Chemotherapy targeting the amyloid plasma cell clone
Anti-plasma cell chemotherapy is the cornerstone of treatment of AL amyloidosis and was able to remarkably improve patients’ outcomes over the last decades.5 Treatment of AL amyloidosis should be adapted to the severity of organ involvement.
Low-risk patients represent approximately 15% of all subjects suffering from AL amyloidosis and can be considered for autologous stem cell transplantation (ASCT). This procedure is associated with a substantially higher risk of early mortality compared to multiple myeloma. However, refinement in selection criteria has reduced transplant-related mortality over time.61 Accumulation of expertise is also crucial, the outcome being significantly poorer at centers where less than four transplants per year are performed in patients with this disease.61 When an adequate selection of transplant candidates is applied at referral centers, the outcome is excellent, with hematologic response in 71% of subjects and complete response (CR) in 35–37%.61,68 These results in overall median survival of 7.6 years.68 The great majority of transplant-related mortality occur in patients with elevated cardiac biomarkers, and subjects whose NT-proBNP is >5000 ng/L and/or cTnT is >0.06 ng/mL should not be offered ASCT.69,70 Other eligibility criteria are ejection fraction >45% at echocardiography, New York Heart Association (NYHA) class <III, orthostatic systolic blood pressure >90 mmHg, age <65 years, performance status (Eastern Cooperative Oncology Group) ≤2, eGFR >50 mL/min per 1.73 m2 unless on dialysis, and lung CO diffusion capacity >50%.1,70,71 Patients who do not obtain CR after ASCT can receive bortezomib-based treatment. Overall, this sequential approach yields a 60% rate of CR.72 Induction therapy with bortezomib before ASCT improves outcomes in patients with a bone marrow plasma cell infiltrate >10%.73
Intermediate risk patients account for approximately 70% of patients with AL amyloidosis. They receive non-transplant chemotherapy. Until recently, a standard treatment for these patients has been oral melphalan and dexamethasone (MDex).74,75 This regimen is very well tolerated and yields a 76% overall hematologic response rate, with CR in 31% of cases.76 A randomized trial compared MDex to ASCT and failed to demonstrate an advantage for ASCT in terms of response rate and survival.77 This trial was performed before the availability of a biomarker-based selection of transplant candidates, and the results were considered influenced by very high transplant-related mortality. Nevertheless, a landmark analysis excluding early deaths confirmed these results. Bortezomib-based regimens are now considered upfront standards of care in most patients with AL amyloidosis. A large retrospective study and a prospective trial showed efficacy of bortezomib in relapsed / refractory patients.78–81 In the largest study of frontline treatment with cyclophosphamide, bortezomib and dexamethasone (CyBorD), the overall hematologic response rate was 60%, with CR in 23% of cases.82 Two retrospective case-control studies showed higher response rates with bortezomib in combination with alkylating agents and dexamethasone compared to the previous standards of care MDex and cyclophosphamide / thalidomide / dexamethasone, though without a survival benefit.83,84 An international phase III study (NCT01277016) comparing MDex with bortezomib plus MDex (BMDex) has recently been completed, showing significantly higher overall hematologic response rate with BMDex (81% vs. 57%, P=0.005).85 Based on this data, bortezomib should be offered to intermediate-risk patients, in the absence of contraindications such as peripheral neuropathy. The choice of the best combination should take into account clonal and patient characteristics. A recent study by Kastritis, et al. showed that addition of cyclophosphamide and higher doses of dexamethasone do not improve outcomes of patients with AL amyloidosis treated with bortezomib.86 Treatment with BMDex has the advantage of overcoming the effects of both gain 1q21 (poor outcome with oral melphalan) and t(11;14) (poor outcome with bortezomib).7,8,10,11 Oral melphalan should not reach the cumulative dose of 150 mg (not exceeding 2 cycles) in patients who may be selected for subsequent stem cell mobilization and harvest.87 Treatment with bortezomib / dexamethasone alone or in combination with cyclophosphamide is preferred in patients with potentially reversible contraindication to ASCT, being stem cell sparing, as well as in subjects with renal failure.
The remaining 15–20% of patients with AL amyloidosis are high-risk, most frequently because of advanced cardiac stage (IIIb) or severe heart failure (NYHA class III or IV). So far, no treatment approach, including those based on bortezomib, was able to overcome the poor prognosis of these patients, and median survival ranges from 3 to 7 months.88 Nevertheless, the few patients who survive long enough (at least 3 months) to take advantage of response to chemotherapy enjoy prolonged survival.82 A recent report from The United Kingdom Group showed that patients achieving a rapid response at day 30 or overall CR/VGPR at 6 months had markedly better survival.89 High-risk patients are treated with low-dose combinations, with weekly dose escalation based on tolerability under intensive monitoring.1
Relapsed patients have a good prognosis, with remarkably longer survival than refractory subjects.90 There is no consensus on criteria to start rescue therapy in relapsing subjects.91 Cardiac progression should not be awaited, because it is associated with shorter survival.90 Relapsing patients can be treated by repeating upfront therapy, if possible, although this is associated with shorter time to retreatment without reduction in overall survival.92 When this is not possible, relapsed patients should be treated as subjects failing to respond to upfront therapy. A recent report defined that a potential role of deferred ASCT in both a consolidation or relapse setting in selected patients with cardiac AL who have achieved organ responses.93 Immunemodulatory drugs (IMiDs) are the backbone of second-line therapy. Lenalidomide is able to overcome resistance to alkylating agents, proteasome inhibitors, and thalidomide.94–99 However, this drug can cause worsening renal failure in patients with renal AL amyloidosis with significant proteinuria.100 Lenalidomide combinations have been used also upfront with encouraging results.97,98,101–104 Pomalidomide is one of the most powerful agents in refractory AL amyloidosis, being able to rescue patients refractory to alkylators, first- and second-generation proteasome inhibitors, and lenalidomide.105–107 Hematologic response to pomalidomide is obtain rapidly, in a median time of 1 months, and is observed in more than 60% of patients.107 Complete responses are relatively rare with IMiDs in pre-treated patients. However, the use of IMiDs could result in long progression-free intervals and survival rates among patients with AL amyloidosis.108 Newer agents have been tested in the relapsed / refractory setting. The proteasome inhibitor carfilzomib yielded a hematologic response rate of 63% (CR 12%).109 In this study, 39% of patients had NT-proBNP progression, which was clinically relevant in 18% of cases. The cardiac toxicity of carfilzomib is a cause of concern in AL amyloidosis. The oral proteasome inhibitor ixazomib proved active in per-treated patients, particularly in those who were not previously exposed to bortezomib, and is currently being tested in a randomized phase III trial in relapsed / refractory patients (NCT01659658).110 Thus, ixazomib seems particularly suitable for upfront combinations, allowing oral proteasome inhibitor-based regimens. Indeed, 2 trials of ixazomib, cyclophosphamide and dexamethasone (NCT03236792, NCT01864018) are ongoing in the upfront setting. Daratumumab is one of the most promising new agents for the treatment of patients with AL amyloidosis. A recently published series of previously treated subjects who received daratumumab reported a rapid (median 1 months) hematologic response in 76% of patients with 36% CRs.111 In the 2017 American Society of hematology meeting, two different abstracts reported the preliminary data of prospective ongoing clinical trials about the use of daratumumab in relapse/refractory setting.112,113 Daratumumab will likely be moved to upfront therapy in combination with proteasome inhibitor-based regimens in the near future. Indeed, a phase III randomized trial of daratumumab in combination with CyBorD vs. CyBorD alone in newly-diagnosed patients will be opened shortly (NCT03201965).
Interfering with amyloidogenesis and organ damage and targeting the amyloid deposits
New, non-hematologic, approaches specifically targeting steps that are downstream in the pathogenic cascade are emerging as supplements of anti-plasma cell therapy, given in combination with chemotherapy or after achievement of hematologic response. Following the observation of the efficacy of the anthracycline 4′-iodo-4′-deoxy-doxorubicin on amyloidogenesis in vitro and reports of clinical improvements in subjects with AL amyloidosis, related non-cytotoxic and non-cardiotoxic compounds were investigated.114–118 Amongst them, doxycycline was able to disrupt amyloid fibrils in transgenic mouse models of systemic amyloidosis,119,120 and protected the C. elegans model from the effects of cardiotoxic amyloid light chains.26 In a retrospective case-control study the administration of doxycycline as antibiotic prophylaxis during chemotherapy for AL amyloidosis reduced early mortality, resulting in higher response rates and survival improvement.121 A phase III trial of chemotherapy with or without doxycycline is being designed. Polyphenols can redirect amyloidogenic polypeptides into unstructured, off-pathway oligomers.122 Amongst them epigallocatechin-3-gallate was tested (EGCG) showed promising activity on cardiac AL amyloidosis in case reports and retrospective series.123–125 In a phase II trial, EGCG was well tolerated and in some patients a decrease in albuminuria was observed.126
The amyloid deposits are natural targets of novel therapies. United Kingdom investigators designed a compound CPHPC that avidly binds to serum amyloid P component (SAP) a protein that coats the amyloid fibrils protecting them from degradation. This compound is used to remove SAP from the bloodstream127 before the administration of an anti-SAP antibody that promotes a complement-dependent, macrophage-derived reaction that removes visceral amyloid deposits.128 This combination approach was tested in a pilot clinical study,129 and a trial in patients with cardiac AL amyloidosis is ongoing (NCT03044353). The report of the ability of this approach to induce organ response measured with validated criteria is eagerly awaited. Antibodies directly targeting the amyloid deposits have also been developed. One of them, 11-1F4, has been tested in phase I clinical trial, showing promising organ response in an interim analysis.130 Those data were recently updated at the last ASH meeting.131 A different antibody, NEOD001 is currently in the most advanced stage of clinical development. In a phase I/II study in patients with AL amyloidosis who had completed chemotherapy, cardiac and renal response rates were 57% and 60%, respectively.132 Organ response to NEOD001 was independent of rate and depth of previous hematologic response.133 Two phase III randomized, placebo-controlled trials of NEOD001 combined with bortezomib-based chemotherapy in newly-diagnosed patients (NCT02312206), and as single agent in subjects who completed chemotherapy (NCT02632786) have recently completed enrollment and results are eagerly awaited.
Supportive therapy
Supportive treatment is vital in patients with AL amyloidosis, in order to sustain organ function while chemotherapy takes effect, and to improve quality of life. However, treatment of concomitant heart failure and nephrotic syndrome in patients who often have concomitant involvement of the autonomic nervous system is extremely complicated, and should be done under close supervisions of specialized cardiologists and nephrologists who have experience in the treatment of patients with systemic amyloidosis. In some patients, asymptomatic involvement of the autonomic nervous system134 could lead to overt, often severe hypotension when treatment with angiotensin-converting enzyme inhibitors is established. This therapy should be considered with caution and at the lowest effective dose. The development of a significant peripheral edema requires diuretics associated with dietary sodium restriction. Patients weigh themselves daily, and diuretic dosing should be titrated accordingly. It should be kept in mind that in patients with heat involvement cardiac function is preload dependent and reduction of intravascular volume should be avoided. Patients with recurrent arrhythmic syncope may benefit from pacemaker implantation; whereas, the use of implantable ICD is controversial. Gabapentin or pregabalin can be used to control neuropathic pain and octreotide can control diarrhea. Nutritional status is also frequently compromised in AL amyloidosis, independently affecting quality of life assessment.135–137 Nutritional counseling is effective in improving mental quality of life and is associated with better survival.138 Cardiac and renal transplant can be considered in patients who attain CR but are dialysis dependent or have persistent, severe heart failure. Moreover, young patients with isolated, advanced cardiac involvement may be considered for heart transplant followed by effective chemotherapy aiming at rapidly achieving CR.
Conclusions
Despite the recent advances the management of AL amyloidosis remains highly challenging and characterized by still unmet needs. The appropriate management of AL amyloidosis requires 1) early diagnosis, 2) correct typing, 3) accurate risk stratification and effective therapy guided by frequent careful assessment of response. Early diagnosis lies in the hands of general hematologists who are responsible for the follow-up of patients with MGUS. The onset of cardiac and renal involvement by AL amyloidosis in these subjects can be detected at a pre-symptomatic stage with simple markers, albuminuria and NT-proBNP, that should be part of the follow-up panel of patients with MGUS and abnormal FLC ratio. Amyloid typing is mandatory but requires advanced technology that needs to be concentrated at referral centers. The lack of controlled prospective studies and the importance of a critical level of expertise in specific and supportive therapy, also requires referral of patients to specialized centers whenever possible. Coordinated national networks are vital in sharing knowledge at rendering it accessible to patients. In the near future, the availability of newer powerful anti-plasma cell drugs, combined with anti-amyloid agent will hopefully further improve the outcome of patients with AL amyloidosis. Still clinical practice and research cannot be disconnected in this complex and dreadful disease.
Footnotes
Competing interests: The authors have declared that no competing interests exist.
References
- 1.Palladini G, Merlini G. What is new in diagnosis and management of light chain amyloidosis? Blood. 2016;128(2):159–168. doi: 10.1182/blood-2016-01-629790. https://doi.org/10.1182/blood-2016-01-629790. [DOI] [PubMed] [Google Scholar]
- 2.Merlini G, Stone M. Dangerous small B-cell clones. Blood. 2006;108(8):2520–2530. doi: 10.1182/blood-2006-03-001164. https://doi.org/10.1182/blood-2006-03-001164. [DOI] [PubMed] [Google Scholar]
- 3.Merlini G. AL amyloidosis: from molecular mechanisms to targeted therapies. Hematology Am Soc Hematol Educ Program. 2017;2017(1):1–12. doi: 10.1182/asheducation-2017.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wechalekar AD, Gillmore JD, Hawkins PN. Systemic amyloidosis. Lancet. 2016;387(10038):2641–2654. doi: 10.1016/S0140-6736(15)01274-X. https://doi.org/10.1016/S0140-6736(15)01274-X. [DOI] [PubMed] [Google Scholar]
- 5.Muchtar E, Gertz MA, Kumar SK, et al. Improved outcomes for newly diagnosed AL amyloidosis between 2000 and 2014: cracking the glass ceiling of early death. Blood. 2017;129(15):2111–2119. doi: 10.1182/blood-2016-11-751628. https://doi.org/10.1182/blood-2016-11-751628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bochtler T, Hegenbart U, Cremer F, et al. Evaluation of the cytogenetic aberration pattern in amyloid light chain amyloidosis as compared with monoclonal gammopathy of undetermined significance reveals common pathways of karyotypic instability. Blood. 2008;111(9):4700–4705. doi: 10.1182/blood-2007-11-122101. https://doi.org/10.1182/blood-2007-11-122101. [DOI] [PubMed] [Google Scholar]
- 7.Bochtler T, Hegenbart U, Kunz C, et al. Translocation t(11;14) is associated with adverse outcome in patients with newly diagnosed AL amyloidosis when treated with bortezomib-based regimens. J Clin Oncol. 2015;33(12):1371–1378. doi: 10.1200/JCO.2014.57.4947. https://doi.org/10.1200/JCO.2014.57.4947. [DOI] [PubMed] [Google Scholar]
- 8.Muchtar E, Dispenzieri A, Kumar SK, et al. Interphase fluorescence in situ hybridization in untreated AL amyloidosis has an independent prognostic impact by abnormality type and treatment category. Leukemia. 2017;31(7):1562–1569. doi: 10.1038/leu.2016.369. https://doi.org/10.1038/leu.2016.369. [DOI] [PubMed] [Google Scholar]
- 9.Muchtar E, Dispenzieri A, Kumar SK, et al. Immunoparesis status in immunoglobulin light chain amyloidosis at diagnosis affects response and survival by regimen type. Haematologica. 2016;101(9):1102–1109. doi: 10.3324/haematol.2016.147041. https://doi.org/10.3324/haematol.2016.147041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bochtler T, Hegenbart U, Kunz C, et al. Prognostic impact of cytogenetic aberrations in AL amyloidosis patients after high-dose melphalan: a long-term follow-up study. Blood. 2016;128(4):594–602. doi: 10.1182/blood-2015-10-676361. https://doi.org/10.1182/blood-2015-10-676361. [DOI] [PubMed] [Google Scholar]
- 11.Bochtler T, Hegenbart U, Kunz C, et al. Gain of chromosome 1q21 is an independent adverse prognostic factor in light chain amyloidosis patients treated with melphalan/dexamethasone. Amyloid. 2014;21(1):9–17. doi: 10.3109/13506129.2013.854766. https://doi.org/10.3109/13506129.2013.854766. [DOI] [PubMed] [Google Scholar]
- 12.Paiva B, Martinez-Lopez J, Corchete LA, et al. Phenotypic, transcriptomic, and genomic features of clonal plasma cells in light-chain amyloidosis. Blood. 2016;127(24):3035–3039. doi: 10.1182/blood-2015-10-673095. https://doi.org/10.1182/blood-2015-10-673095. [DOI] [PubMed] [Google Scholar]
- 13.da Silva Filho MI, Försti A, Weinhold N, et al. Genome-wide association study of immunoglobulin light chain amyloidosis in three patient cohorts: comparison with myeloma. Leukemia. 2017;31(8):1735–1742. doi: 10.1038/leu.2016.387. https://doi.org/10.1038/leu.2016.387. [DOI] [PubMed] [Google Scholar]
- 14.Sitia R, Palladini G, Merlini G. Bortezomib in the treatment of AL amyloidosis: targeted therapy? Haematologica. 2007;92(10):1302–1307. doi: 10.3324/haematol.12136. https://doi.org/10.3324/haematol.12136. [DOI] [PubMed] [Google Scholar]
- 15.Bianchi G, Oliva L, Cascio P, et al. The proteasome load versus capacity balance determines apoptotic sensitivity of multiple myeloma cells to proteasome inhibition. Blood. 2009;113(13):3040–3049. doi: 10.1182/blood-2008-08-172734. https://doi.org/10.1182/blood-2008-08-172734. [DOI] [PubMed] [Google Scholar]
- 16.Oliva L, Orfanelli U, Resnati M, et al. The amyloidogenic light chain is a stressor that sensitizes plasma cells to proteasome inhibitor toxicity. Blood. 2017;129(15):2132–2142. doi: 10.1182/blood-2016-08-730978. https://doi.org/10.1182/blood-2016-08-730978. [DOI] [PubMed] [Google Scholar]
- 17.Comenzo R, Zhang Y, Martinez C, Osman K, Herrera G. The tropism of organ involvement in primary systemic amyloidosis: contributions of Ig V(L) germ line gene use and clonal plasma cell burden. Blood. 2001;98(3):714–720. doi: 10.1182/blood.v98.3.714. https://doi.org/10.1182/blood.V98.3.714. [DOI] [PubMed] [Google Scholar]
- 18.Perfetti V, Casarini S, Palladini G, et al. Analysis of V(lambda)-J(lambda) expression in plasma cells from primary (AL) amyloidosis and normal bone marrow identifies 3r (lambdaIII) as a new amyloid-associated germline gene segment. Blood. 2002;100(3):948–953. doi: 10.1182/blood-2002-01-0114. https://doi.org/10.1182/blood-2002-01-0114. [DOI] [PubMed] [Google Scholar]
- 19.Abraham R, Geyer S, Price-Troska T, et al. Immunoglobulin light chain variable (V) region genes influence clinical presentation and outcome in light chain-associated amyloidosis (AL) Blood. 2003;101(10):3801–3808. doi: 10.1182/blood-2002-09-2707. https://doi.org/10.1182/blood-2002-09-2707. [DOI] [PubMed] [Google Scholar]
- 20.Kourelis TV, Dasari S, Theis JD, et al. Clarifying immunoglobulin gene usage in systemic and localized immunoglobulin light-chain amyloidosis by mass spectrometry. Blood. 2017;129(3):299–306. doi: 10.1182/blood-2016-10-743997. https://doi.org/10.1182/blood-2016-10-743997. [DOI] [PubMed] [Google Scholar]
- 21.Perfetti V, Palladini G, Casarini S, et al. The repertoire of ? light chains causing predominant amyloid heart involvement and identification of a preferentially involved germline gene, IGLV1–44. Blood. 2012;119(1):144–150. doi: 10.1182/blood-2011-05-355784. https://doi.org/10.1182/blood-2011-05-355784. [DOI] [PubMed] [Google Scholar]
- 22.Palladini G, Campana C, Klersy C, et al. Serum N-terminal pro-brain natriuretic peptide is a sensitive marker of myocardial dysfunction in AL amyloidosis. Circulation. 2003;107(19):2440–2445. doi: 10.1161/01.CIR.0000068314.02595.B2. https://doi.org/10.1161/01.CIR.0000068314.02595.B2. [DOI] [PubMed] [Google Scholar]
- 23.Palladini G, Lavatelli F, Russo P, et al. Circulating amyloidogenic free light chains and serum N-terminal natriuretic peptide type B decrease simultaneously in association with improvement of survival in AL. Blood. 2006;107(10):3854–3858. doi: 10.1182/blood-2005-11-4385. https://doi.org/10.1182/blood-2005-11-4385. [DOI] [PubMed] [Google Scholar]
- 24.Palladini G, Barassi A, Klersy C, et al. The combination of high-sensitivity cardiac troponin T (hs-cTnT) at presentation and changes in N-terminal natriuretic peptide type B (NT-proBNP) after chemotherapy best predicts survival in AL amyloidosis. Blood. 2010;116(18):3426–3430. doi: 10.1182/blood-2010-05-286567. https://doi.org/10.1182/blood-2010-05-286567. [DOI] [PubMed] [Google Scholar]
- 25.Liao R, Jain M, Teller P, et al. Infusion of light chains from patients with cardiac amyloidosis causes diastolic dysfunction in isolated mouse hearts. Circulation. 2001;104(14):1594–1597. [PubMed] [Google Scholar]
- 26.Diomede L, Rognoni P, Lavatelli F, et al. A Caenorhabditis elegans-based assay recognizes immunoglobulin light chains causing heart amyloidosis. Blood. 2014;123(23):3543–3552. doi: 10.1182/blood-2013-10-525634. https://doi.org/10.1182/blood-2013-10-525634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mishra S, Guan J, Plovie E, et al. Human amyloidogenic light chain proteins result in cardiac dysfunction, cell death, and early mortality in zebrafish. Am J Physiol Heart Circ Physiol. 2013;305(1):H95–103. doi: 10.1152/ajpheart.00186.2013. https://doi.org/10.1152/ajpheart.00186.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lavatelli F, Imperlini E, Orru S, et al. Novel mitochondrial protein interactors of immunoglobulin light chains causing heart amyloidosis. FASEB J. 2015;29(11):4614–4628. doi: 10.1096/fj.15-272179. https://doi.org/10.1096/fj.15-272179. [DOI] [PubMed] [Google Scholar]
- 29.Oberti L, Rognoni P, Barbiroli A, et al. Concurrent structural and biophysical traits link with immunoglobulin light chains amyloid propensity. Sci Rep. 2017;7(1):16809. doi: 10.1038/s41598-017-16953-7. https://doi.org/10.1038/s41598-017-16953-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Perlini S, Salinaro F, Musca F, et al. Prognostic value of depressed midwall systolic function in cardiac light-chain amyloidosis. J Hypertens. 2014;32(5):1121–1131. doi: 10.1097/HJH.0000000000000120. discussion 1131. https://doi.org/10.1097/HJH.0000000000000120. [DOI] [PubMed] [Google Scholar]
- 31.Buss SJ, Emami M, Mereles D, et al. Longitudinal left ventricular function for prediction of survival in systemic light-chain amyloidosis: incremental value compared with clinical and biochemical markers. J Am Coll Cardiol. 2012;60(12):1067–1076. doi: 10.1016/j.jacc.2012.04.043. https://doi.org/10.1016/j.jacc.2012.04.043. [DOI] [PubMed] [Google Scholar]
- 32.Fontana M, Chung R, Hawkins PN, Moon JC. Cardiovascular magnetic resonance for amyloidosis. Heart Fail Rev. 2015;20(2):133–144. doi: 10.1007/s10741-014-9470-7. https://doi.org/10.1007/s10741-014-9470-7. [DOI] [PubMed] [Google Scholar]
- 33.Park MA, Padera RF, Belanger A, et al. 18F-Florbetapir Binds Specifically to Myocardial Light Chain and Transthyretin Amyloid Deposits: Autoradiography Study. Circ Cardiovasc Imaging. 2015;8(8) doi: 10.1161/CIRCIMAGING.114.002954. https://doi.org/10.1161/CIRCIMAGING.114.002954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gillmore JD, Maurer MS, Falk RH, et al. Nonbiopsy Diagnosis of Cardiac Transthyretin Amyloidosis. Circulation. 2016;133(24):2404–2412. doi: 10.1161/CIRCULATIONAHA.116.021612. https://doi.org/10.1161/CIRCULATIONAHA.116.021612. [DOI] [PubMed] [Google Scholar]
- 35.Merlini G, Palladini G. Differential diagnosis of monoclonal gammopathy of undetermined significance. Hematology Am Soc Hematol Educ Program. 2012;2012:595–603. doi: 10.1182/asheducation-2012.1.595. [DOI] [PubMed] [Google Scholar]
- 36.Lousada I, Comenzo RL, Landau H, Guthrie S, Merlini G. Light Chain Amyloidosis: Patient Experience Survey from the Amyloidosis Research Consortium. Adv Ther. 2015;32(10):920–928. doi: 10.1007/s12325-015-0250-0. https://doi.org/10.1007/s12325-015-0250-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kourelis TV, Kumar SK, Go RS, et al. Immunoglobulin light chain amyloidosis is diagnosed late in patients with preexisting plasma cell dyscrasias. Am J Hematol. 2014;89(11):1051–1054. doi: 10.1002/ajh.23827. https://doi.org/10.1002/ajh.23827. [DOI] [PubMed] [Google Scholar]
- 38.Merlini G, Wechalekar AD, Palladini G. Systemic light chain amyloidosis: an update for treating physicians. Blood. 2013;121(26):5124–5130. doi: 10.1182/blood-2013-01-453001. https://doi.org/10.1182/blood-2013-01-453001. [DOI] [PubMed] [Google Scholar]
- 39.Foli A, Palladini G, Caporali R, et al. The role of minor salivary gland biopsy in the diagnosis of systemic amyloidosis: results of a prospective study in 62 patients. Amyloid. 2011;18(Suppl 1):80–82. doi: 10.3109/13506129.2011.574354029. https://doi.org/10.3109/13506129.2011.574354029. [DOI] [PubMed] [Google Scholar]
- 40.Fernandez de Larrea C, Verga L, Morbini P, et al. A practical approach to the diagnosis of systemic amyloidoses. Blood. 2015;125(14):2239–2244. doi: 10.1182/blood-2014-11-609883. https://doi.org/10.1182/blood-2014-11-609883. [DOI] [PubMed] [Google Scholar]
- 41.Muchtar E, Dispenzieri A, Lacy MQ, et al. Overuse of organ biopsies in immunoglobulin light chain amyloidosis (AL): the consequence of failure of early recognition. Ann Med. 2017;49(7):545–551. doi: 10.1080/07853890.2017.1304649. https://doi.org/10.1080/07853890.2017.1304649. [DOI] [PubMed] [Google Scholar]
- 42.Anesi E, Palladini G, Perfetti V, Arbustini E, Obici L, Merlini G. Therapeutic advances demand accurate typing of amyloid deposits. Am J Med. 2001;111(3):243–244. doi: 10.1016/s0002-9343(01)00774-4. https://doi.org/10.1016/S0002-9343(01)00774-4. [DOI] [PubMed] [Google Scholar]
- 43.Lachmann H, Booth D, Booth S, et al. Misdiagnosis of hereditary amyloidosis as AL (primary) amyloidosis. N Engl J Med. 2002;346(23):1786–1791. doi: 10.1056/NEJMoa013354. https://doi.org/10.1056/NEJMoa013354. [DOI] [PubMed] [Google Scholar]
- 44.Comenzo R, Zhou P, Fleisher M, Clark B, Teruya-Feldstein J. Seeking confidence in the diagnosis of systemic AL (Ig light-chain) amyloidosis: patients can have both monoclonal gammopathies and hereditary amyloid proteins. Blood. 2006;107(9):3489–3491. doi: 10.1182/blood-2005-10-4148. https://doi.org/10.1182/blood-2005-10-4148. [DOI] [PubMed] [Google Scholar]
- 45.Satoskar A, Burdge K, Cowden D, Nadasdy G, Hebert L, Nadasdy T. Typing of amyloidosis in renal biopsies: diagnostic pitfalls. Arch Pathol Lab Med. 2007;131(6):917–922. doi: 10.5858/2007-131-917-TOAIRB. [DOI] [PubMed] [Google Scholar]
- 46.Satoskar AA, Efebera Y, Hasan A, et al. Strong transthyretin immunostaining: potential pitfall in cardiac amyloid typing. Am J Surg Pathol. 2011;35(11):1685–1690. doi: 10.1097/PAS.0b013e3182263d74. https://doi.org/10.1097/PAS.0b013e3182263d74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schönland SO, Hegenbart U, Bochtler T, et al. Immunohistochemistry in the classification of systemic forms of amyloidosis: a systematic investigation of 117 patients. Blood. 2012;119(2):488–493. doi: 10.1182/blood-2011-06-358507. https://doi.org/10.1182/blood-2011-06-358507. [DOI] [PubMed] [Google Scholar]
- 48.Vrana J, Gamez J, Madden B, Theis J, Bergen Hr, Dogan A. Classification of amyloidosis by laser microdissection and mass spectrometry-based proteomic analysis in clinical biopsy specimens. Blood. 2009;114(24):4957–4959. doi: 10.1182/blood-2009-07-230722. https://doi.org/10.1182/blood-2009-07-230722. [DOI] [PubMed] [Google Scholar]
- 49.Brambilla F, Lavatelli F, Di Silvestre D, et al. Reliable typing of systemic amyloidoses through proteomic analysis of subcutaneous adipose tissue. Blood. 2012;119(8):1844–1847. doi: 10.1182/blood-2011-07-365510. https://doi.org/10.1182/blood-2011-07-365510. [DOI] [PubMed] [Google Scholar]
- 50.Katzmann J, Kyle R, Benson J, et al. Screening panels for detection of monoclonal gammopathies. Clin Chem. 2009;55(8):1517–1522. doi: 10.1373/clinchem.2009.126664. https://doi.org/10.1373/clinchem.2009.126664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bochtler T, Hegenbart U, Heiss C, et al. Evaluation of the serum-free light chain test in untreated patients with AL amyloidosis. Haematologica. 2008;93(3):459–462. doi: 10.3324/haematol.11687. https://doi.org/10.3324/haematol.11687. [DOI] [PubMed] [Google Scholar]
- 52.Palladini G, Russo P, Bosoni T, et al. Identification of amyloidogenic light chains requires the combination of serum-free light chain assay with immunofixation of serum and urine. Clin Chem. 2009;55(3):499–504. doi: 10.1373/clinchem.2008.117143. https://doi.org/10.1373/clinchem.2008.117143. [DOI] [PubMed] [Google Scholar]
- 53.Palladini G, Jaccard A, Milani P, et al. Circulating free light chain measurement in the diagnosis, prognostic assessment and evaluation of response of AL amyloidosis: comparison of Freelite and N latex FLC assays. Clin Chem Lab Med. 2017 doi: 10.1515/cclm-2016-1024. https://doi.org/10.1515/cclm-2016-1024. [DOI] [PubMed] [Google Scholar]
- 54.Dispenzieri A, Gertz M, Kyle R, et al. Serum cardiac troponins and N-terminal pro-brain natriuretic peptide: a staging system for primary systemic amyloidosis. J Clin Oncol. 2004;22(18):3751–3757. doi: 10.1200/JCO.2004.03.029. https://doi.org/10.1200/JCO.2004.03.029. [DOI] [PubMed] [Google Scholar]
- 55.Wechalekar AD, Schonland SO, Kastritis E, et al. A European collaborative study of treatment outcomes in 346 patients with cardiac stage III AL amyloidosis. Blood. 2013;121(17):3420–3427. doi: 10.1182/blood-2012-12-473066. https://doi.org/10.1182/blood-2012-12-473066. [DOI] [PubMed] [Google Scholar]
- 56.Kourelis TV, Kumar SK, Gertz MA, et al. Coexistent multiple myeloma or increased bone marrow plasma cells define equally high-risk populations in patients with immunoglobulin light chain amyloidosis. J Clin Oncol. 2013;31(34):4319–4324. doi: 10.1200/JCO.2013.50.8499. https://doi.org/10.1200/JCO.2013.50.8499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dittrich T, Bochtler T, Kimmich C, et al. AL amyloidosis patients with low amyloidogenic free light chain levels at first diagnosis have an excellent prognosis. Blood. 2017;130(5):632–642. doi: 10.1182/blood-2017-02-767475. https://doi.org/10.1182/blood-2017-02-767475. [DOI] [PubMed] [Google Scholar]
- 58.Milani P, Basset M, Russo F, Foli A, Merlini G, Palladini G. Patients with light-chain amyloidosis and low free light-chain burden have distinct clinical features and outcome. Blood. 2017;130(5):625–631. doi: 10.1182/blood-2017-02-767467. https://doi.org/10.1182/blood-2017-02-767467. [DOI] [PubMed] [Google Scholar]
- 59.Kumar S, Dispenzieri A, Lacy MQ, et al. Revised prognostic staging system for light chain amyloidosis incorporating cardiac biomarkers and serum free light chain measurements. J Clin Oncol. 2012;30(9):989–995. doi: 10.1200/JCO.2011.38.5724. https://doi.org/10.1200/JCO.2011.38.5724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Palladini G, Hegenbart U, Milani P, et al. A staging system for renal outcome and early markers of renal response to chemotherapy in AL amyloidosis. Blood. 2014;124(15):2325–2332. doi: 10.1182/blood-2014-04-570010. https://doi.org/10.1182/blood-2014-04-570010. [DOI] [PubMed] [Google Scholar]
- 61.D’Souza A, Dispenzieri A, Wirk B, et al. Improved Outcomes After Autologous Hematopoietic Cell Transplantation for Light Chain Amyloidosis: A Center for International Blood and Marrow Transplant Research Study. J Clin Oncol. 2015;33(32):3741–3749. doi: 10.1200/JCO.2015.62.4015. https://doi.org/10.1200/JCO.2015.62.4015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rajkumar SV, Dimopoulos MA, Palumbo A, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014;15(12):e538–e548. doi: 10.1016/S1470-2045(14)70442-5. https://doi.org/10.1016/S1470-2045(14)70442-5. [DOI] [PubMed] [Google Scholar]
- 63.Dispenzieri A, Seenithamby K, Lacy MQ, et al. Patients with immunoglobulin light chain amyloidosis undergoing autologous stem cell transplantation have superior outcomes compared with patients with multiple myeloma: a retrospective review from a tertiary referral center. Bone Marrow Transplant. 2013;48(10):1302–1307. doi: 10.1038/bmt.2013.53. https://doi.org/10.1038/bmt.2013.53. [DOI] [PubMed] [Google Scholar]
- 64.Palladini G, Dispenzieri A, Gertz MA, et al. New criteria for response to treatment in immunoglobulin light chain amyloidosis based on free light chain measurement and cardiac biomarkers: impact on survival outcomes. J Clin Oncol. 2012;30(36):4541–4549. doi: 10.1200/JCO.2011.37.7614. https://doi.org/10.1200/JCO.2011.37.7614. [DOI] [PubMed] [Google Scholar]
- 65.Merlini G, Lousada I, Ando Y, et al. Rationale, application and clinical qualification for NT-proBNP as a surrogate end point in pivotal clinical trials in patients with AL amyloidosis. Leukemia. 2016;30(10):1979–1986. doi: 10.1038/leu.2016.191. https://doi.org/10.1038/leu.2016.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sidana S, Tandon N, Dispenzieri A, Gertz MA, Buadi FK, Lacy MQ, Dingli D, Fonder A, Hayman SR, Hobbs M, Gonsalves WI, Hwa YL, Kapoor P, Kyle RA, Leung N, Go RS, Lust JA, Russell SJ, Zeldenrust SR, Binder M, Rajkumar SV, Kumar SK. Composite Organ and Hematologic Response Model Risk Stratifies Patients with Light Chain Amyloidosis. Blood. 2017;130(Suppl 1):3046. [Google Scholar]
- 67.Muchtar E, Dispenzieri A, Lacy MQ, Leung N, Buadi FK, Grogan M, Hayman SR, Kapoor P, Hwa YL, Fonder A, Hobbs M, Chakraborty R, Gonsalves WI, Kourelis T, Warsame R, Russell SJ, Lust JA, Lin Y, Go RS, Zeldenrust S, Kyle RA, Rajkumar SV, Kumar SK, Gertz MA. Depth of Organ Response in Newly Diagnosed AL Amyloidosis Is Associated with Improved Survival: Improved Outcome Discrimination with Graded Organ Response. Blood. 2017;130(Suppl 1):3154. [Google Scholar]
- 68.Sanchorawala V, Sun F, Quillen K, Sloan JM, Berk JL, Seldin DC. Long-term outcome of patients with AL amyloidosis treated with high-dose melphalan and stem cell transplantation: 20-year experience. Blood. 2015;126(20):2345–2347. doi: 10.1182/blood-2015-08-662726. https://doi.org/10.1182/blood-2015-08-662726. [DOI] [PubMed] [Google Scholar]
- 69.Gertz MA, Lacy MQ, Dispenzieri A, et al. Refinement in patient selection to reduce treatment-related mortality from autologous stem cell transplantation in amyloidosis. Bone Marrow Transplant. 2013;48(4):557–561. doi: 10.1038/bmt.2012.170. https://doi.org/10.1038/bmt.2012.170. [DOI] [PubMed] [Google Scholar]
- 70.Dispenzieri A, Buadi F, Kumar SK, et al. Treatment of Immunoglobulin Light Chain Amyloidosis: Mayo Stratification of Myeloma and Risk-Adapted Therapy (mSMART) Consensus Statement. Mayo Clin Proc. 2015;90(8):1054–1081. doi: 10.1016/j.mayocp.2015.06.009. https://doi.org/10.1016/j.mayocp.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 71.Cibeira MT, Sanchorawala V, Seldin DC, et al. Outcome of AL amyloidosis after high-dose melphalan and autologous stem cell transplantation: long-term results in a series of 421 patients. Blood. 2011;118(16):4346–4352. doi: 10.1182/blood-2011-01-330738. https://doi.org/10.1182/blood-2011-01-330738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Landau H, Smith M, Landry C, et al. Long-term event-free and overall survival after risk-adapted melphalan and SCT for systemic light chain amyloidosis. Leukemia. 2017;31(1):136–142. doi: 10.1038/leu.2016.229. https://doi.org/10.1038/leu.2016.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hwa YL, Kumar SK, Gertz MA, et al. Induction therapy pre-autologous stem cell transplantation in immunoglobulin light chain amyloidosis: a retrospective evaluation. Am J Hematol. 2016;91(10):984–988. doi: 10.1002/ajh.24453. https://doi.org/10.1002/ajh.24453. [DOI] [PubMed] [Google Scholar]
- 74.Palladini G, Perfetti V, Obici L, et al. Association of melphalan and high-dose dexamethasone is effective and well tolerated in patients with AL (primary) amyloidosis who are ineligible for stem cell transplantation. Blood. 2004;103(8):2936–2938. doi: 10.1182/blood-2003-08-2788. https://doi.org/10.1182/blood-2003-08-2788. [DOI] [PubMed] [Google Scholar]
- 75.Palladini G, Russo P, Nuvolone M, et al. Treatment with oral melphalan plus dexamethasone produces long-term remissions in AL amyloidosis. Blood. 2007;110(2):787–788. doi: 10.1182/blood-2007-02-076034. https://doi.org/10.1182/blood-2007-02-076034. [DOI] [PubMed] [Google Scholar]
- 76.Palladini G, Milani P, Foli A, et al. Oral melphalan and dexamethasone grants extended survival with minimal toxicity in AL amyloidosis: long-term results of a risk-adapted approach. Haematologica. 2014;99(4):743–750. doi: 10.3324/haematol.2013.095463. https://doi.org/10.3324/haematol.2013.095463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jaccard A, Moreau P, Leblond V, et al. High-dose melphalan versus melphalan plus dexamethasone for AL amyloidosis. N Engl J Med. 2007;357(11):1083–1093. doi: 10.1056/NEJMoa070484. https://doi.org/10.1056/NEJMoa070484. [DOI] [PubMed] [Google Scholar]
- 78.Kastritis E, Wechalekar A, Dimopoulos M, et al. Bortezomib with or without dexamethasone in primary systemic (light chain) amyloidosis. J Clin Oncol. 2010;28(6):1031–1037. doi: 10.1200/JCO.2009.23.8220. https://doi.org/10.1200/JCO.2009.23.8220. [DOI] [PubMed] [Google Scholar]
- 79.Reece D, Sanchorawala V, Hegenbart U, et al. Weekly and twice-weekly bortezomib in patients with systemic AL amyloidosis: results of a phase 1 dose-escalation study. Blood. 2009;114(8):1489–1497. doi: 10.1182/blood-2009-02-203398. https://doi.org/10.1182/blood-2009-02-203398. [DOI] [PubMed] [Google Scholar]
- 80.Reece DE, Hegenbart U, Sanchorawala V, et al. Efficacy and safety of once-weekly and twice-weekly bortezomib in patients with relapsed systemic AL amyloidosis: results of a phase 1/2 study. Blood. 2011;118(4):865–873. doi: 10.1182/blood-2011-02-334227. https://doi.org/10.1182/blood-2011-02-334227. [DOI] [PubMed] [Google Scholar]
- 81.Reece DE, Hegenbart U, Sanchorawala V, et al. Long-term follow-up from a phase 1/2 study of single-agent bortezomib in relapsed systemic AL amyloidosis. Blood. 2014;124(16):2498–2506. doi: 10.1182/blood-2014-04-568329. https://doi.org/10.1182/blood-2014-04-568329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Palladini G, Sachchithanantham S, Milani P, et al. A European collaborative study of cyclophosphamide, bortezomib, and dexamethasone in upfront treatment of systemic AL amyloidosis. Blood. 2015;126(5):612–615. doi: 10.1182/blood-2015-01-620302. https://doi.org/10.1182/blood-2015-01-620302. [DOI] [PubMed] [Google Scholar]
- 83.Palladini G, Milani P, Foli A, et al. Melphalan and dexamethasone with or without bortezomib in newly diagnosed AL amyloidosis: a matched case-control study on 174 patients. Leukemia. 2014;28(12):2311–2316. doi: 10.1038/leu.2014.227. https://doi.org/10.1038/leu.2014.227. [DOI] [PubMed] [Google Scholar]
- 84.Venner CP, Gillmore JD, Sachchithanantham S, et al. A matched comparison of cyclophosphamide, bortezomib and dexamethasone (CVD) versus risk-adapted cyclophosphamide, thalidomide and dexamethasone (CTD) in AL amyloidosis. Leukemia. 2014;28(12):2304–2310. doi: 10.1038/leu.2014.218. https://doi.org/10.1038/leu.2014.218. [DOI] [PubMed] [Google Scholar]
- 85.Kastritis E, Leleu X, Arnulf B, et al. A Randomized Phase III Trial of Melphalan and Dexamethasone (MDex) Versus Bortezomib, Melphalan and Dexamethasone (BMDex) for Untreated Patients with AL Amyloidosis. Blood. 2016;128(22) [Google Scholar]
- 86.Kastritis E, Gavriatopoulou M, Roussou M, et al. Addition of cyclophosphamide and higher doses of dexamethasone do not improve outcomes of patients with AL amyloidosis treated with bortezomib. Blood Cancer J. 2017;7(6):e570. doi: 10.1038/bcj.2017.47. https://doi.org/10.1038/bcj.2017.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sidana S, Tandon N, Gertz MA, et al. Impact of prior melphalan exposure on stem cell collection in light chain amyloidosis. Bone Marrow Transplant. 2017 doi: 10.1038/s41409-017-0020-5. https://doi.org/10.1038/s41409-017-0020-5. [DOI] [PubMed] [Google Scholar]
- 88.Palladini G, Milani P, Merlini G. Novel strategies for the diagnosis and treatment of cardiac amyloidosis. Expert review of cardiovascular therapy. 2015;13(11):1195–1211. doi: 10.1586/14779072.2015.1093936. https://doi.org/10.1586/14779072.2015.1093936. [DOI] [PubMed] [Google Scholar]
- 89.Manwani R, Foard D, Mahmood S, et al. Rapid hematological responses improve outcomes in patients with very advanced (Stage IIIb) cardiac immunoglobulin light chain amyloidosis. Haematologica. 2018 doi: 10.3324/haematol.2017.178095. https://doi.org/10.3324/haematol.2017.178095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Palladini G, Milani P, Foli A, et al. Presentation and outcome with second line treatment in AL amyloidosis previously sensitive to non-transplant therapies. Blood. 2017 doi: 10.1182/blood-2017-04-780544. [DOI] [PubMed] [Google Scholar]
- 91.Milani P, Gertz MA, Merlini G, Dispenzieri A. Attitudes about when and how to treat patients with AL amyloidosis: an international survey. Amyloid. 2017:1–4. doi: 10.1080/13506129.2017.1370421. https://doi.org/10.1080/13506129.2017.1370421. [DOI] [PubMed] [Google Scholar]
- 92.Tandon N, Sidana S, Gertz MA, et al. Treatment Patterns and Outcome Following Initial Relapse or Refractory Disease in Patients with Systemic Light Chain Amyloidosis. Am J Hematol. 2017 doi: 10.1002/ajh.24723. https://doi.org/10.1002/ajh.24723. [DOI] [PubMed] [Google Scholar]
- 93.Manwani R, Hegenbart U, Foard D, Mahmood S, Sachchithanantham S, Yong K, Popat R, Kyriakou C, Rabin N, Fontana M, Whelan C, Lachmann H, Lane T, Quarta C, Gillmore J, Dittrich T, Kimmich C, Hawkins P, Schönland S, Wechalekar AD. Safety and Efficacy of Deferred Autologous Stem Cell Transplantation in Patients with Systemic AL Amyloidosis with Significant Cardiac Involvement at Presentation. Blood. 2017;130(Suppl 1):1815. [Google Scholar]
- 94.Dispenzieri A, Lacy M, Zeldenrust S, et al. The activity of lenalidomide with or without dexamethasone in patients with primary systemic amyloidosis. Blood. 2007;109(2):465–470. doi: 10.1182/blood-2006-07-032987. https://doi.org/10.1182/blood-2006-07-032987. [DOI] [PubMed] [Google Scholar]
- 95.Sanchorawala V, Wright D, Rosenzweig M, et al. Lenalidomide and dexamethasone in the treatment of AL amyloidosis: results of a phase 2 trial. Blood. 2007;109(2):492–496. doi: 10.1182/blood-2006-07-030544. https://doi.org/10.1182/blood-2006-07-030544. [DOI] [PubMed] [Google Scholar]
- 96.Palladini G, Russo P, Foli A, et al. Salvage therapy with lenalidomide and dexamethasone in patients with advanced AL amyloidosis refractory to melphalan, bortezomib, and thalidomide. Ann Hematol. 2011 doi: 10.1007/s00277-011-1244-x. [DOI] [PubMed] [Google Scholar]
- 97.Kastritis E, Terpos E, Roussou M, et al. A phase 1/2 study of lenalidomide with low-dose oral cyclophosphamide and low-dose dexamethasone (RdC) in AL amyloidosis. Blood. 2012;119(23):5384–5390. doi: 10.1182/blood-2011-12-396903. https://doi.org/10.1182/blood-2011-12-396903. [DOI] [PubMed] [Google Scholar]
- 98.Kumar SK, Hayman SR, Buadi FK, et al. Lenalidomide, cyclophosphamide, and dexamethasone (CRd) for light-chain amyloidosis: long-term results from a phase 2 trial. Blood. 2012;119(21):4860–4867. doi: 10.1182/blood-2012-01-407791. https://doi.org/10.1182/blood-2012-01-407791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Mahmood S, Venner CP, Sachchithanantham S, et al. Lenalidomide and dexamethasone for systemic AL amyloidosis following prior treatment with thalidomide or bortezomib regimens. Br J Haematol. 2014;166(6):842–848. doi: 10.1111/bjh.12973. https://doi.org/10.1111/bjh.12973. [DOI] [PubMed] [Google Scholar]
- 100.Specter R, Sanchorawala V, Seldin DC, et al. Kidney dysfunction during lenalidomide treatment for AL amyloidosis. Nephrol Dial Transplant. 2011;26(3):881–886. doi: 10.1093/ndt/gfq482. https://doi.org/10.1093/ndt/gfq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Moreau P, Jaccard A, Benboubker L, et al. Lenalidomide in combination with melphalan and dexamethasone in patients with newly diagnosed AL amyloidosis: a multicenter phase 1/2 dose-escalation study. Blood. 2010;116(23):4777–4782. doi: 10.1182/blood-2010-07-294405. https://doi.org/10.1182/blood-2010-07-294405. [DOI] [PubMed] [Google Scholar]
- 102.Sanchorawala V, Patel JM, Sloan JM, Shelton AC, Zeldis JB, Seldin DC. Melphalan, lenalidomide and dexamethasone for the treatment of immunoglobulin light chain amyloidosis: results of a phase II trial. Haematologica. 2013;98(5):789–792. doi: 10.3324/haematol.2012.075192. https://doi.org/10.3324/haematol.2012.075192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cibeira MT, Oriol A, Lahuerta JJ, et al. A phase II trial of lenalidomide, dexamethasone and cyclophosphamide for newly diagnosed patients with systemic immunoglobulin light chain amyloidosis. Br J Haematol. 2015;170(6):804–813. doi: 10.1111/bjh.13500. https://doi.org/10.1111/bjh.13500. [DOI] [PubMed] [Google Scholar]
- 104.Hegenbart U, Bochtler T, Benner A, et al. Lenalidomide/ melphalan/dexamethasone in newly diagnosed patients with immunoglobulin light chain amyloidosis: results of a prospective phase 2 study with long-term follow up. Haematologica. 2017;102(8):1424–1431. doi: 10.3324/haematol.2016.163246. https://doi.org/10.3324/haematol.2016.163246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Dispenzieri A, Buadi F, Laumann K, et al. Activity of pomalidomide in patients with immunoglobulin light-chain amyloidosis. Blood. 2012;119(23):5397–5404. doi: 10.1182/blood-2012-02-413161. https://doi.org/10.1182/blood-2012-02-413161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sanchorawala V, Shelton AC, Lo S, Varga C, Sloan JM, Seldin DC. Pomalidomide and dexamethasone in the treatment of AL amyloidosis: results of a phase 1 and 2 trial. Blood. 2016;128(8):1059–1062. doi: 10.1182/blood-2016-04-710822. https://doi.org/10.1182/blood-2016-04-710822. [DOI] [PubMed] [Google Scholar]
- 107.Palladini G, Milani P, Foli A, et al. A phase 2 trial of pomalidomide and dexamethasone rescue treatment in patients with AL amyloidosis. Blood. 2017;129(15):2120–2123. doi: 10.1182/blood-2016-12-756528. https://doi.org/10.1182/blood-2016-12-756528. [DOI] [PubMed] [Google Scholar]
- 108.Warsame R, Laplant B, Laumann K, Kumar SK, Gertz MA, Kyle RA, Lacy MQ, Dingli D, Leung N, Buadi FK, Hayman SR, Kapoor P, Hwa YL, Fonder A, Hobbs M, Gonsalves WI, Kourelis T, Russell SJ, Zeldenrust S, Lin Y, Muchtar E, Go RS, Rajkumar SV, Dispenzieri A. Long-Term Outcomes of IMiD Based Trials in Patients with Immunoglobulin Light Chain Amyloidosis (AL): A Pooled Analysis. Blood. 2017;130(Suppl 1):1833. doi: 10.1038/s41408-019-0266-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Cohen A, Landau H, Scott E, et al. Safety and Efficacy of Carfilzomib (CFZ) in Previously-Treated Systemic Light-Chain (AL) Amyloidosis. Blood. 2016;128(22) [Google Scholar]
- 110.Sanchorawala V, Palladini G, Kukreti V, et al. A phase 1/2 study of the oral proteasome inhibitor ixazomib in relapsed or refractory AL amyloidosis. Blood. 2017;130(5):597–605. doi: 10.1182/blood-2017-03-771220. https://doi.org/10.1182/blood-2017-03-771220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kaufman GP, Schrier SL, Lafayette RA, Arai S, Witteles RM, Liedtke M. Daratumumab yields rapid and deep hematologic responses in patients with heavily pretreated AL amyloidosis. Blood. 2017 doi: 10.1182/blood-2017-01-763599. https://doi.org/10.1182/blood-2017-01-763599. [DOI] [PubMed] [Google Scholar]
- 112.Sanchorawala V, Sarosiek S, Sloan JM, Brauneis D, Migre ME, Mistark M, Santos S, Fennessey S, Shelton AC. Safety and Tolerability of Daratumumab in Patients with Relapsed Light Chain (AL) Amyloidosis: Preliminary Results of a Phase II Study. Blood. 2017;130(Suppl 1):507. [Google Scholar]
- 113.Roussel M, Stoppa A, Perrot A, Karlin L, Arnulf B, Macro M, Huart A, Frenzel L, Morel P, Boyle E, Dorvaux V, Merlini G, Palladini G, Lavergne D, Bridoux F, Jaccard A. A Prospective Phase II of Daratumumab in Previously-Treated Systemic Light-Chain (AL) Amyloidosis. Blood. 2017;130(Suppl 1):508. doi: 10.1182/blood.2019004369. [DOI] [PubMed] [Google Scholar]
- 114.Merlini G, Ascari E, Amboldi N, et al. Interaction of the anthracycline 4′-iodo-4′-deoxydoxorubicin with amyloid fibrils: inhibition of amyloidogenesis. Proc Natl Acad Sci U S A. 1995;92(7):2959–2963. doi: 10.1073/pnas.92.7.2959. https://doi.org/10.1073/pnas.92.7.2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Merlini G, Anesi E, Garini P, et al. Treatment of AL amyloidosis with 4′-lodo-4′-deoxydoxorubicin: an update. Blood. 1999;93(3):1112–1113. [PubMed] [Google Scholar]
- 116.Palha JA, Ballinari D, Amboldi N, et al. 4′-Iodo-4′-deoxydoxorubicin disrupts the fibrillar structure of transthyretin amyloid. Am J Pathol. 2000;156(6):1919–1925. doi: 10.1016/S0002-9440(10)65065-1. https://doi.org/10.1016/S0002-9440(10)65065-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Cardoso I, Merlini G, Saraiva MJ. 4′-iodo-4′-deoxydoxorubicin and tetracyclines disrupt transthyretin amyloid fibrils in vitro producing noncytotoxic species: screening for TTR fibril disrupters. FASEB J. 2003;17(8):803–809. doi: 10.1096/fj.02-0764com. https://doi.org/10.1096/fj.02-0764com. [DOI] [PubMed] [Google Scholar]
- 118.Gertz M, Lacy M, Dispenzieri A, et al. A multicenter phase II trial of 4′-iodo-4′deoxydoxorubicin (IDOX) in primary amyloidosis (AL) Amyloid. 2002;9(1):24–30. doi: 10.3109/13506120209072441. https://doi.org/10.3109/13506120209072441. [DOI] [PubMed] [Google Scholar]
- 119.Cardoso I, Saraiva MJ. Doxycycline disrupts transthyretin amyloid: evidence from studies in a FAP transgenic mice model. FASEB J. 2006;20(2):234–239. doi: 10.1096/fj.05-4509com. https://doi.org/10.1096/fj.05-4509com. [DOI] [PubMed] [Google Scholar]
- 120.Ward JE, Ren R, Toraldo G, et al. Doxycycline reduces fibril formation in a transgenic mouse model of AL amyloidosis. Blood. 2011;118(25):6610–6617. doi: 10.1182/blood-2011-04-351643. https://doi.org/10.1182/blood-2011-04-351643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wechalekar AD, Whelan C. Encouraging impact of doxycycline on early mortality in cardiac light chain (AL) amyloidosis. Blood Cancer J. 2017;7(3):e546. doi: 10.1038/bcj.2017.26. [DOI] [PMC free article] [PubMed] [Google Scholar]; Edwards CV, Gould J, Langer AL, et al. Interim analysis of the phase 1a/b study of chimeric fibril-reactive monoclonal antibody 11-1F4 in patients with AL amyloidosis. Amyloid. 2017;24(supp1):58–59. doi: 10.1080/13506129.2017.1292900. [DOI] [PubMed] [Google Scholar]
- 122.Ehrnhoefer DE, Bieschke J, Boeddrich A, et al. EGCG redirects amyloidogenic polypeptides into unstructured, off-pathway oligomers. Nat Struct Mol Biol. 2008;15(6):558–566. doi: 10.1038/nsmb.1437. https://doi.org/10.1038/nsmb.1437. [DOI] [PubMed] [Google Scholar]
- 123.Hora M, Carballo-Pacheco M, Weber B, et al. Epigallocatechin-3-gallate preferentially induces aggregation of amyloidogenic immunoglobulin light chains. Sci Rep. 2017;7:41515. doi: 10.1038/srep41515. https://doi.org/10.1038/srep41515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hunstein W. Epigallocathechin-3-gallate in AL amyloidosis: a new therapeutic option? Blood. 2007;110(6):2216. doi: 10.1182/blood-2007-05-089243. https://doi.org/10.1182/blood-2007-05-089243. [DOI] [PubMed] [Google Scholar]
- 125.Mereles D, Buss SJ, Hardt SE, Hunstein W, Katus HA. Effects of the main green tea polyphenol epigallocatechin-3-gallate on cardiac involvement in patients with AL amyloidosis. Clin Res Cardiol. 2010;99(8):483–490. doi: 10.1007/s00392-010-0142-x. https://doi.org/10.1007/s00392-010-0142-x. [DOI] [PubMed] [Google Scholar]
- 126.Meshitsuka S, Shingaki S, Hotta M, et al. Phase 2 trial of daily, oral epigallocatechin gallate in patients with light-chain amyloidosis. Int J Hematol. 2017;105(3):295–308. doi: 10.1007/s12185-016-2112-1. https://doi.org/10.1007/s12185-016-2112-1. [DOI] [PubMed] [Google Scholar]
- 127.Pepys M, Herbert J, Hutchinson W, et al. Targeted pharmacological depletion of serum amyloid P component for treatment of human amyloidosis. Nature. 2002;417(6886):254–259. doi: 10.1038/417254a. https://doi.org/10.1038/417254a. [DOI] [PubMed] [Google Scholar]
- 128.Gillmore JD, Tennent GA, Hutchinson WL, et al. Sustained pharmacological depletion of serum amyloid P component in patients with systemic amyloidosis. Br J Haematol. 2010;148(5):760–767. doi: 10.1111/j.1365-2141.2009.08036.x. https://doi.org/10.1111/j.1365-2141.2009.08036.x. [DOI] [PubMed] [Google Scholar]
- 129.Richards DB, Cookson LM, Berges AC, et al. Therapeutic Clearance of Amyloid by Antibodies to Serum Amyloid P Component. N Engl J Med. 2015;373(12):1106–1114. doi: 10.1056/NEJMoa1504942. https://doi.org/10.1056/NEJMoa1504942. [DOI] [PubMed] [Google Scholar]
- 130.Edwards CV, Gould J, Langer AL, et al. Interim analysis of the phase 1a/b study of chimeric fibril-reactive monoclonal antibody 11-1F4 in patients with AL amyloidosis. Amyloid. 2017;24(supp1):58–59. doi: 10.1080/13506129.2017.1292900. [DOI] [PubMed] [Google Scholar]
- 131.Edwards CV, Gould J, Langer AL, Mapara MY, Radhakrishnan J, Maurer MS, Raza S, Mears JG, Leng S, Wall JS, Eisenberger A, Solomon A, Lentzsch S. Final Analysis of the Phase 1a/b Study of Chimeric Fibril-Reactive Monoclonal Antibody 11-1F4 in Patients with Relapsed or Refractory AL Amyloidosis. Blood. 2017;130(Suppl 1):509. [Google Scholar]
- 132.Gertz MA, Landau H, Comenzo RL, et al. First-in-Human Phase I/II Study of NEOD001 in Patients With Light Chain Amyloidosis and Persistent Organ Dysfunction. J Clin Oncol. 2016;34(10):1097–1103. doi: 10.1200/JCO.2015.63.6530. https://doi.org/10.1200/JCO.2015.63.6530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Gertz M, Comenzo R, Landau H, et al. Patients with light chain amyloidosis treated with neod001 achieve rapid organ responses that are independent of previous plasma cell-directed therapies. Haematologica. 2017;102:3–3. [Google Scholar]
- 134.Bernardi L, Passino C, Porta C, Anesi E, Palladini G, Merlini G. Widespread cardiovascular autonomic dysfunction in primary amyloidosis: does spontaneous hyperventilation have a compensatory role against postural hypotension? Heart. 2002;88(6):615–621. doi: 10.1136/heart.88.6.615. https://doi.org/10.1136/heart.88.6.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Caccialanza R, Palladini G, Klersy C, et al. Nutritional status of outpatients with systemic immunoglobulin light-chain amyloidosis. American Journal of Clinical Nutrition. 2006;83(2):350–354. doi: 10.1093/ajcn/83.2.350. [DOI] [PubMed] [Google Scholar]
- 136.Caccialanza R, Palladini G, Klersy C, et al. Nutritional status independently affects quality of life of patients with systemic immunoglobulin light-chain (AL) amyloidosis. Ann Hematol. 2012;91(3):399–406. doi: 10.1007/s00277-011-1309-x. https://doi.org/10.1007/s00277-011-1309-x. [DOI] [PubMed] [Google Scholar]
- 137.Caccialanza R, Palladini G, Klersy C, et al. Malnutrition at diagnosis predicts mortality in patients with systemic immunoglobulin light-chain amyloidosis independently of cardiac stage and response to treatment. JPEN J Parenter Enteral Nutr. 2014;38(7):891–894. doi: 10.1177/0148607113501328. https://doi.org/10.1177/0148607113501328. [DOI] [PubMed] [Google Scholar]
- 138.Caccialanza R, Palladini G, Cereda E, et al. Nutritional counseling improves quality of life and preserves body weight in systemic immunoglobulin light-chain (AL) amyloidosis. Nutrition. 2015;31(10):1228–1234. doi: 10.1016/j.nut.2015.04.011. https://doi.org/10.1016/j.nut.2015.04.011. [DOI] [PubMed] [Google Scholar]
- 139.Kumar S, Dispenzieri A, Lacy MQ, et al. Revised prognostic staging system for light chain amyloidosis incorporating cardiac biomarkers and serum free light chain measurements. J Clin Oncol. 2012;30(9):989–995. doi: 10.1200/JCO.2011.38.5724. https://doi.org/10.1200/JCO.2011.38.5724. [DOI] [PMC free article] [PubMed] [Google Scholar]