Abstract
Rationale:
We report 3 cases of a torn haptic after successful scleral fixation with a hydrophobic acrylic intraocular lens.
Patient concerns:
Patients complained of decreased visual acuity about 1 week to 1 month after scleral fixation.
Diagnoses:
In all 3 cases, the direction of the damaged haptic correlated with the direction of the pulling force made by the hung suture material. Observation of a cheese-wiring effect on scanning electron microscopy suggested that the haptic was cut by the suture.
Interventions:
Patients underwent re-scleral fixation with caution.
Ouctomes:
There was no complication of broken haptic after re-scleral fixation.
Lessons:
To avoid unexpected haptic tears, great caution is needed; surgeons should avoid applying excessive pulling force to the intraocular lens when performing scleral fixation using a hydrophobic acrylic intraocular lens.
Keywords: hydrophobic acrylic intraocular lens, scanning electron microscope, scleral fixation, torn haptic
1. Introduction
For scleral fixation, the intraocular lens (IOL) should be easily fixated by the suture material. In general, surgeons use an IOL with an eyelet, which facilitates easy fixation and stable positioning after surgery. In our hospital, we have used the CZ70BD IOL (Alcon Laboratories, Fort Worth, TX) for scleral fixation procedures for several years. It is a single piece of polymethyl methacrylate (PMMA) IOL that has eyelets located symmetrically in both haptics. This design permits stable fixation of the IOL without suture knot slippage or lens decentration or tilting.
Since the manufacturer has stopped making and selling the CZ70BD IOL, we and others have had to seek a replacement lens. An IOL containing an eyelet is desirable. The enVista aspheric hydrophobic acrylic single-piece IOL (Bausch & Lomb, Rochester, NY) has eyelets that are symmetrically positioned in both optic–haptic junctions. We thought this IOL would be a convenient and stable replacement for scleral fixation.
Following the introduction of the enVista IOL in our institute, we noted 3 cases of IOL failure due to a torn haptic after scleral fixation. These cases are reported herein. All 3 surgeries were done by the same surgeon (CKJ) using the modified cow hitch method for scleral fixation.[1] This case report was approved by the Institutional Review Board of Seoul St. Mary's Hospital, Seoul, Republic of Korea.
2. Case reports
2.1. Case 1
A 23-year-old man visited our clinic complaining of blurry vision in his right eye. He had received surgery for a traumatic cataract 10 years prior. The IOL was captured inferiorly on slit lamp examination. We planned IOL removal and scleral fixation with an enVista IOL. The IOL was fixated 2.5 mm from the limbus using 10-0 polypropylene sutures (Prolene, Ethicon, Somerville, NJ). Ten days after the surgery, the patient again experienced blurry vision in his right eye. An examination revealed that the IOL had dropped on the nasal side and seemed to still be hanging on the temporal side. We hypothesized that the suture might have loosened or become severed. We planned IOL removal and scleral fixation. However, during the surgery, we discovered that the haptic rather than the suture material was cut. After the surgery, we retrospectively reviewed the video of the first fixation operation. At first, modified cow-hitch knots were made on either side of the eyelets with the polypropylene in front of the complete scleral suture. Then, the IOL was sutured and tied tightly on the temporal scleral side first, pulled nasally using the already-hung suture material, and finally tied when the IOL was positioned in the center of the eye.
2.2. Case 2
A 64-year-old woman desired secondary IOL implantation surgery in her left eye. She had undergone cataract surgery in another eye clinic 1 month prior but could not undergo IOL implantation at that time because of a posterior capsule rupture. We planned scleral fixation using an enVista IOL. The surgery was done in the same manner as in case 1. One week postoperatively, she complained of decreased visual acuity. An examination revealed that the IOL had dropped to the temporal side. Given what we had learned from case 1, we suspected that the drop was due to a haptic tear instead of the suture being loosened or cut. Widefield fundus photography revealed a torn temporal haptic (Fig. 1). We decided to remove the IOL and do a repeat scleral fixation. After the surgery, we reviewed the video of the first fixation. After modified cow-hitch knots were made on both sides of the eyelets, the nasal haptic was sutured first and then the IOL was pulled temporally using the hung suture material. Because of our suspicion that the haptic was torn by the suture material, we took scanning electron microscopy images. The cut section looked like cheese that had been cut with cheese wire (Fig. 2A, B), which we termed the cheese-wiring effect.
Figure 1.
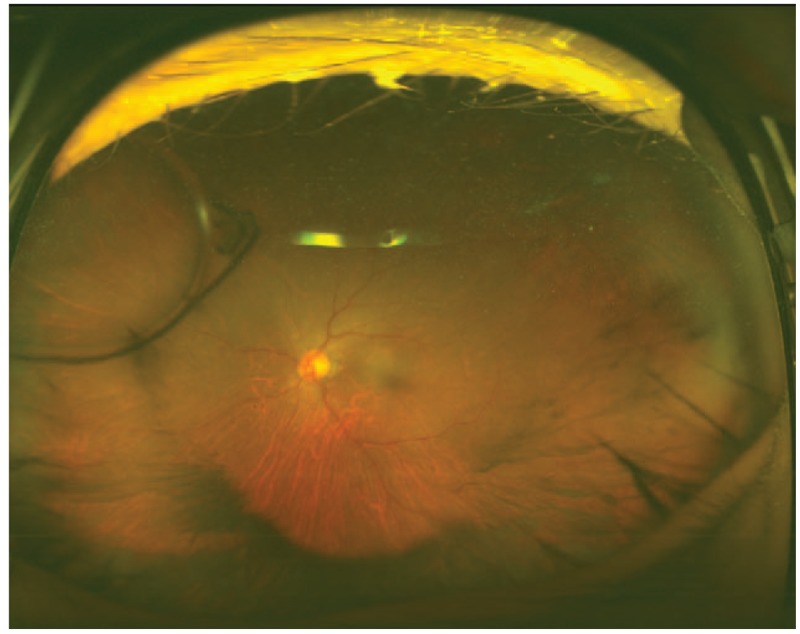
A torn temporal haptic was found on wide fundus photography.
Figure 2.
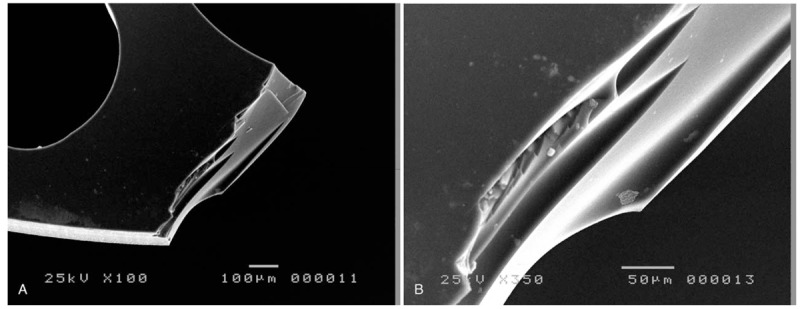
The cut section of the IOL looked like cheese that had been cut with cheese wire. A. Original magnification ×100. B. Original magnification ×350. IOL = intraocular lens.
2.3. Case 3
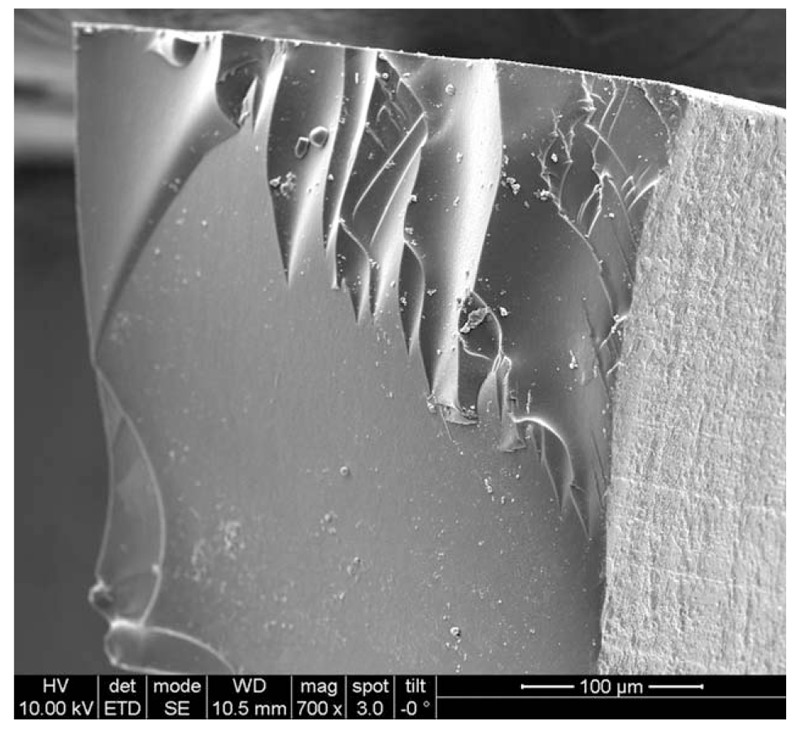
A 72-year-old man complained of ocular discomfort in his left eye. He had undergone cataract surgery using an anterior chamber IOL (ACL) 15 years previously. Three days prior to the visiting our clinic, he had fallen and injured his face upon impact with the floor. Slit lamp examination revealed dislocation of the superior haptic of the ACL behind the iris through the iridectomy site. We planned ACL removal and scleral fixation using an enVista IOL because the dislocated ACL haptic could cause ocular discomfort and a decrease in vision by pigment dispersion or iris bleeding owing to continuous friction between the iris and the haptic. One month postoperatively, IOL dislocation was discovered. We could not identify the exact reason for the dislocation because the pupil could not be fully dilated despite multiple mydriatic drops. During the surgery, a torn nasal haptic was discovered. In a retrospective review of the video of the first surgery, we saw that the IOL had been pulled nasally after temporal haptic fixation. When viewed by scanning electron microscopy, the cut section of the IOL displayed the aforementioned cheese-wiring effect of the suture material (Fig. 3).
Figure 3.
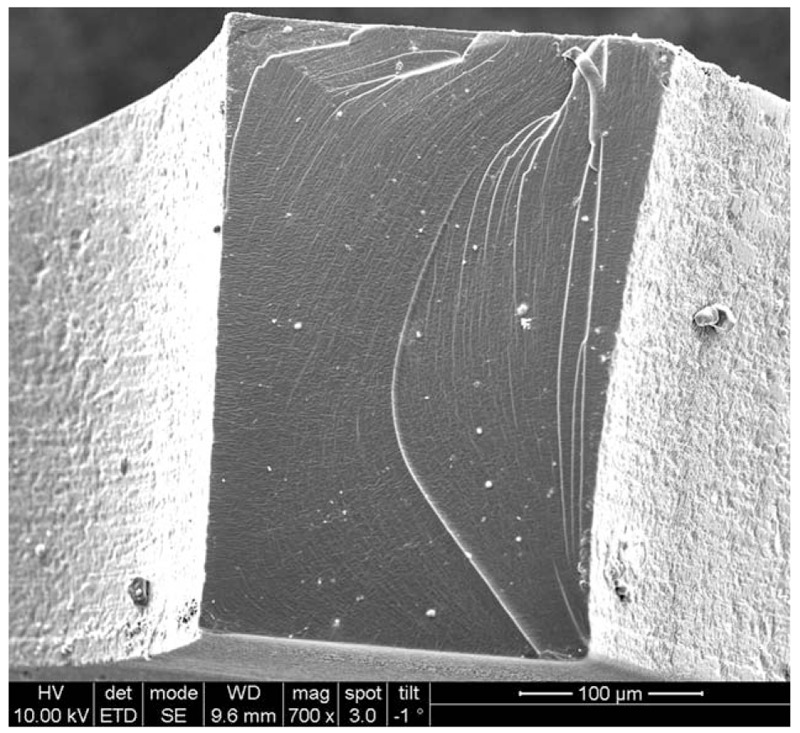
The cheese-wiring effect was visible on the cut section of the IOL (original magnification ×700). IOL = intraocular lens.
3. Discussion
Many methods of scleral fixation have been developed.[1–4] Our preference has been the modified cow hitch method,[1] as it provides more strength than the others. The strength is imparted by the 2 strings per haptic that are applied to hold the IOL in position. In addition, the method is more convenient for surgeons because it does not require multiple sutures in the IOL and a very simple knot is sufficient to hold the IOL in place. PMMA IOLs were not prone to tearing of the haptic after fixation. Unfortunately, the phase-out of this type of IOL necessitated the identification of a replacement. Our choice was a hydrophobic acrylic IOL. Its use in scleral fixation resulted in a torn haptic in the very first case (case 1). Two other instances occurred.
In all 3 cases, the side of the torn haptic correlated with the order of fixation; the haptic that was tied later was torn. This ran counter to our initial assumptions. We thought that the haptic that was tied earlier would be more fragile because of the tightness of the suture material. We thought that the tightness may have produced more traction force, which could have resulted in a markedly stronger cutting force when the IOL was pulled in the opposite haptic direction. The observation that the haptic that was tied later was prone to tearing instead suggests that it is not the tight suture, but rather the pulling itself, that damages the haptic located on the same side.
The flexibility of hydrophobic acrylic IOLs varies with temperature. This reflects increased and decreased water absorption as the temperature increases and decreases, respectively. Increased water absorption makes the IOL more flexible.[5] The IOL becomes smoother and more flexible when it is implanted into the anterior chamber. PMMA IOLs are more rigid, and therefore could be less prone to damage under conditions of tight suturing and pulling. However, the more flexible and foldable hydrophobic acrylic IOLs can more easily be cut by the suture material itself if the pulling force is excessive (Figs. 2A, B and 3), which is analogous to the effect of a cheese wire cutting through a block of cheese.
When the haptic was pulled apart by only manual traction force, and not by the suture material, during IOL removal, the cut edge showed a regular fine texture when examined microscopically (Fig. 4). Breakage of the IOL in a dry external environment produced a different result, with the cut section having a smooth, glass-like appearance (Fig. 5). We surmise that the cheese-wiring pattern is evidence that the IOL was cut by the suture material rather than by manual traction or during the manufacturing process.
Figure 4.
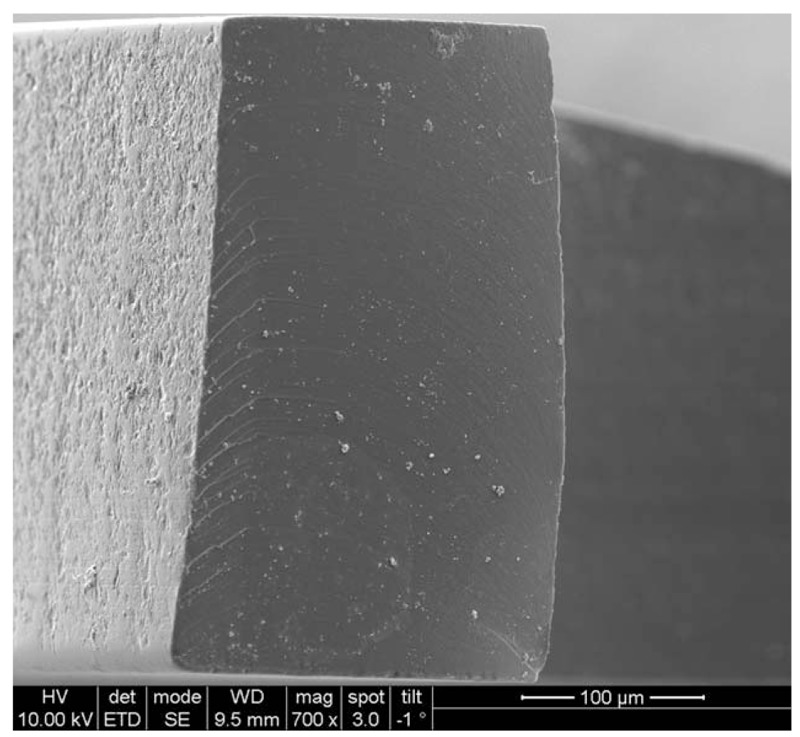
A torn haptic that was pulled apart by only manual traction force, and not by the suture material, with a regular fine texture rather than a cheese-wire pattern (original magnification ×700).
Figure 5.
The cut section showed a smooth, glass-like appearance following IOL breakage in a dry environment (original magnification ×700). IOL = intraocular lens.
The enVista IOL is advantageous in scleral fixation because of its symmetric eyelet design, which promotes easy fixation and positional stability by preventing slippage of the suture knots. However, because of the intrinsic properties of hydrophobic acrylate, this IOL becomes softer and more fragile when it absorbs water at body temperature. This fragility increases the risk of haptic tear when the IOL is pulled strongly in the wet intraocular environment. The enVista IOL is not alone in carrying this risk; the other available hydrophobic acrylic IOLs carry the same risk of haptic tear.
The 3 cases presented here highlight the risk of a tear in a hydrophobic acrylic IOL caused by the pulling force, and reveal that the affected haptic side is the side being pulled. We suggest that the degree of the forced used to pull the IOL should be adjusted according to the IOL material during scleral fixation. Hydrophobic acrylic IOLs should be fixated with minimum pulling force to prevent haptic tears after surgery.
Footnotes
Abbreviations: ACL = anterior chamber IOL, IOL = intraocular lens, PMMA = polymethyl methacrylate.
This work was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2016R1A6A1A03010528).
Financial Disclosure: None of the authors has a financial or proprietary interest in any material or method mentioned.
The authors report no conflicts of interest.
References
- [1].Chen SX, Lee LR, Sii F, et al. Modified cow-hitch suture fixation of transscleral sutured posterior chamber intraocular lenses: long-term safety and efficacy. J Cataract Refract Surg 2008;34:452–8. [DOI] [PubMed] [Google Scholar]
- [2].Wallmann AC, Monson BK, Adelberg DA. Transscleral fixation of a foldable posterior chamber intraocular lens. J Cataract Refract Surg 2015;41:1804–9. [DOI] [PubMed] [Google Scholar]
- [3].Long C, Wei Y, Yuan Z, et al. Modified technique for transscleral fixation of posterior chamber intraocular lenses. BMC Ophthalmol 2015;15:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Kulkarni K, Zarbin M, Del Priore LV, et al. Ab externo technique for accurate haptic placement of transscleral sutured posterior chamber intraocular lenses. Ophthalmic Surg Lasers Imaging 2007;38:72–5. [DOI] [PubMed] [Google Scholar]
- [5].Gregori NZ, Spencer TS, Mamalis N, et al. In vitro comparison of glistening formation among hydrophobic acrylic intraocular lenses. J Cataract Refract Surg 2002;28:1262–8. [DOI] [PubMed] [Google Scholar]


