Abstract
Rationale:
To report a case of late spontaneous reattachment of Descemet membrane (DM) detachment after deep anterior lamellar keratoplasty (DALK).
Patient concerns:
A 50-year-old woman with stromal corneal scarring underwent a DALK with the big bubble technique. The DM detachment and double anterior chamber were observed on the first day after operation.
Diagnoses:
Descemet membrane detachment after deep anterior lamellar keratoplasty [Oculus Dexter (OD), indicates right eye].
Interventions:
Sterile air injection was unsuccessful. Conservative observation was performed.
Outcomes:
During the follow-up, the donor cornea kept transparent and no edema was observed. The DM reattached spontaneously at the fifth months post-DALK.
Lessons:
The present case suggests that the retained host DM may result in DM detachment after DALK. For the DM detachment without roll rim, the detachment may spontaneously reattach in several months after surgery.
Keywords: deep anterior lamellar keratoplasty, Descemet membrane detachment, spontaneous reattachment
1. Introduction
Deep anterior lamellar keratoplasty (DALK) is an advanced corneal surgery using air-injection or other methods to dissect the corneal stroma from the Descemet membrane (DM).[1] Several advantages has been established for DALK over penetrating keratoplasty (PKP), such as lower rates of graft rejection, reduced complications, and comparative visual outcomes.[2] Technically, DALK is more challenging than PKP especially in the step of baring DM. DM detachment is one of the serious complications post-DALK which causes double anterior chamber and visual acuity impair. The managements of DM detachment usually include injecting air or gas into the anterior chamber, suturing the DM to its position, or repeating keratoplasty.[3] Spontaneous resolution of DM detachment after DALK is rare. Here, we report a case that DM detachment reattached spontaneously 5 months after DALK.
2. Case report
A 50-year-old female patient with a long history of recurrent herpes simplex keratitis, presented as stromal corneal scarring and vascularization in her right eye (Fig. 1A). The best-corrected visual acuity was hand motion 30 cm and the intraocular pressure (IOP) was 18.7 mm Hg. Her anterior segment optical coherence tomography (AS-OCT) images revealed increased corneal thickness and higher reflectivity in the stromal scar with 1060 μm in the thickest part (Fig. 1B).
Figure 1.
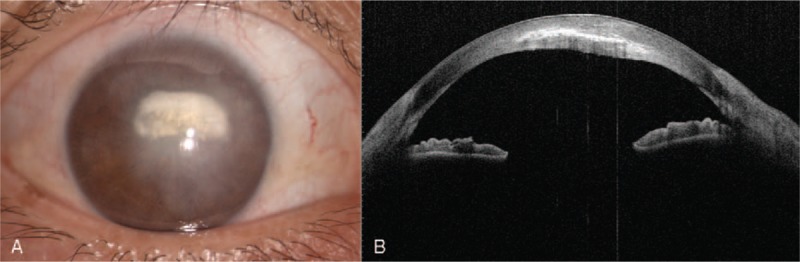
(A) Slit-lamp photo indicated a stromal corneal scar of the right eye. (B) Preoperative AS-OCT of the right eye. AS-OCT = anterior segment optical coherence tomography.
DALK was performed using the big-bubble technique to expose the DM. The cornea was partly trephinated by a 7.5-mm diameter trephine. Next, the anterior portion of the stroma was separated and removed carefully. A big bubble was formed between the DM and stroma by the injection of air through a 30-gauge needle. An incision was made by a 15° slit knife, and viscoelastic was gently injected to the interface. The deep stroma was cut down by a blunt-tipped Vanna scissors after dissecting the deep stroma into 4 parts. A 7.75-mm fresh donor cornea was fixed to the host cornea with 16 interrupted sutures by 10-0 nylon string without perforation.
On the first day postoperatively, the DM detachment was observed between the donor corneal graft and recipient DM, and a double anterior chamber occurred. Mild edema was observed in the donor cornea, with a visual acuity of 1/10.
On the second day postoperatively, the DM detachment was still present (Fig. 2 A). The AS-OCT examination confirmed the detachment (Fig. 2B). A small amount of sterile air was injected into the anterior chamber to ameliorate the endothelium–Descemet detachment. After operation, AS-OCT was performed again and the DM detachment seemed to disappear except for a circumscribed detachment on the temporal part of the cornea (Fig. 2C). One day after operation, the DM detachment relapsed and a shallow detachment still persisted on the second day with a visual acuity of 2/20. After careful consideration, we decided to wait and observe. The patient was seen for follow-up visits every month after surgery, and the host DM still remained detached (Fig. 3). The donor cornea kept transparent and no edema was observed during the initial 4 months postoperatively. At the end of the fourth month, grey haze was observed before the host DM. Interestingly, 5 months post-DALK, the DM detachment disappeared spontaneously without any further surgery, which was further confirmed by AS-OCT (Fig. 4).
Figure 2.
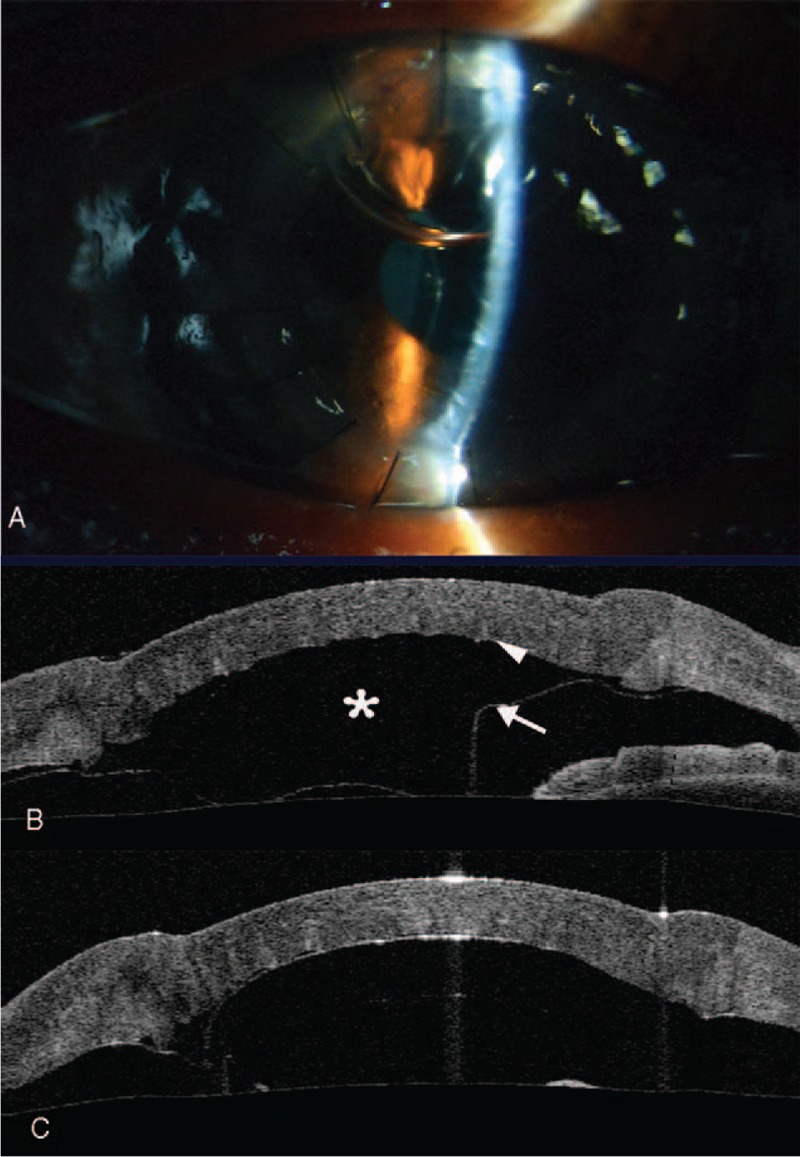
One-day postoperative appearance of the right eye showing DM detachment and a double anterior chamber. (A) Slit-lamp image and (B) AS-OCT image. (C) AS-OCT immediately after the air injection. The image showed that the resolution of DM detachment resolved except for a circumscribed detachment. Asterisk: detachment pool. Arrowhead: entrance pump. Arrow: exit pump. AS-OCT = anterior segment optical coherence tomography, DM = Descemet membrane.
Figure 3.
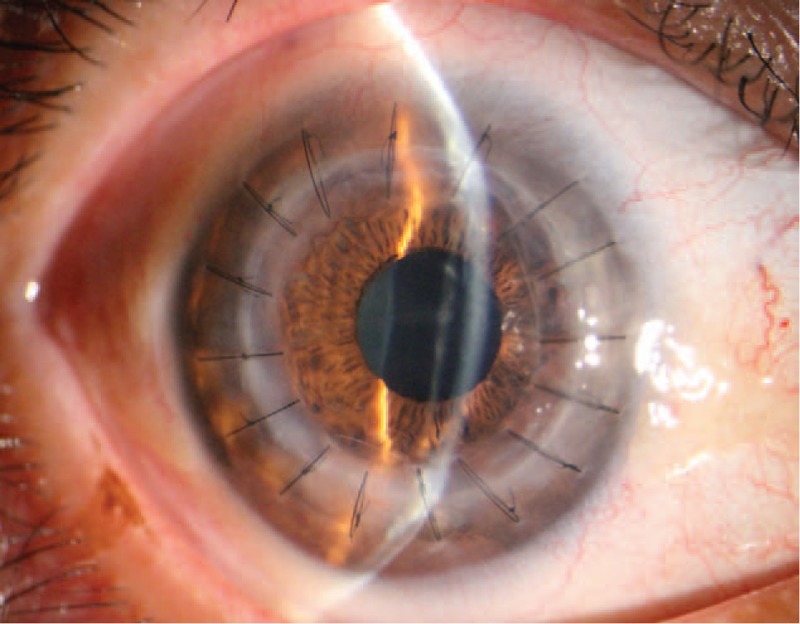
DM detachment still existed at 4-month post-DALK. DALK = deep anterior lamellar keratoplasty, DM = Descemet membrane.
Figure 4.
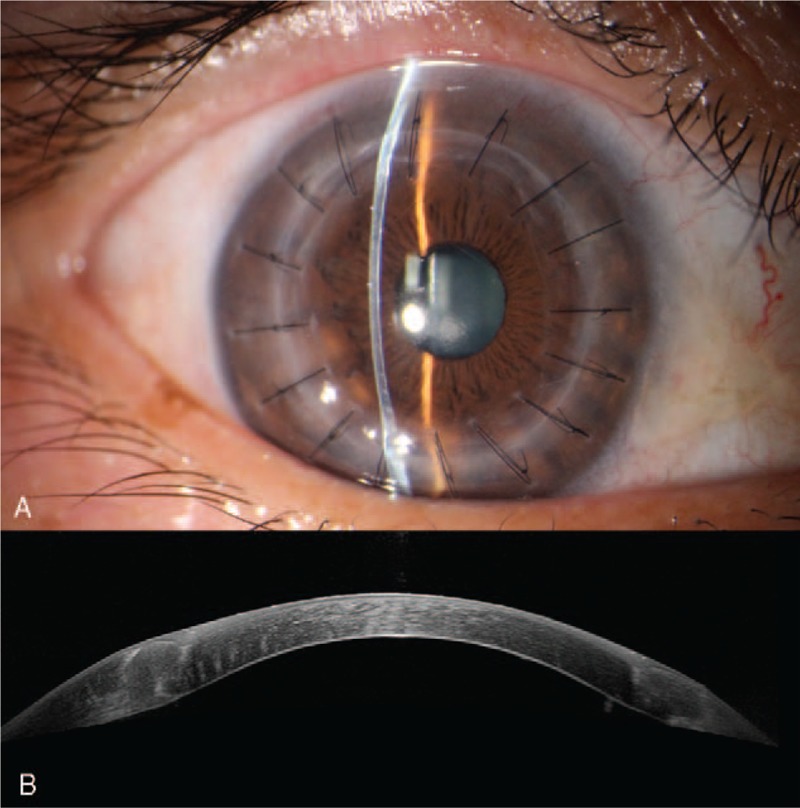
Five-month post-DALK appearance of the right eye. (A) Slit-lamp image and (B) AS-OCT indicated the DM reattached fully. AS-OCT = anterior segment optical coherence tomography, DALK = deep anterior lamellar keratoplasty, DM = Descemet membrane.
The study was approved by the Investigational Review Board of School of Ophthalmology and Optometry and Eye Hospital, Wenzhou Medical University, Wenzhou, China. The patient enrolled has given informed consent.
3. Discussion
DM detachment is a rare but severe complication after DALK. It is often associated with the macro- or microperforations during the operation. The most common management for this complication is to inject sterile air or gas (SF6/C3F8) into the anterior chamber to drive the aqueous humor out from the endothelium–Descemet complex.[3] Most of the detachment will resolve after injection. While some subjects need repeated gas injection. However, some cases, DM detachment need further surgical managements including suture, PKP, or DSAEK (Descemet's stripping automated endothelial keratoplasty).[4]
In the present case, DM detachment was observed on the first day after uneventful DALK. No visible perforation of DM was observed during the surgery and it has been assured by the operation video replay. The sterile air injection was not effective and a shallow DM detachment still existed. However, the DM reattached spontaneously 5 months later. Passani et al[5] hypothesized that the DM detachment after DALK may be caused by the air penetrating through perforations into the anterior chamber, thereby creating a false pathway across the trabecular meshwork. The reason for the DM detachment in our case may be invisible microperforations during the step of air injection or corneal suture. Another reason is probably that, in this case, the fresh donor cornea retained DM and functional endothelium. The residual donor endothelium may retain some pump function and could be related to the host DM detachment. The study of Müller et al[6] also revealed that incomplete removal of the host DM would cause graft detachment after Descemet membrane endothelial keratoplasty.
The mechanism for the late spontaneous resolution of DM detachment is still elusive. In this case, we hypothesized that the sandwiched endothelium may act as 2 “pumps,” which could gradually emit and expel the aqueous humor between the graft–host interface. One is at the entrance of the “detachment pool,” the other is at the exit of the “detachment pool,” leading to a stable “detachment pool” as a “second anterior chamber” and keeping the transparency of cornea (Fig. 1D). When the “entrance pump” gradually lose function (death of donor endothelial cells), the “detachment pool” dry up, and reattachment of DM occurred. One reason for the death of donor endothelial cells may be the mechanical friction between donor and host corneas. Another reason may be that the accumulation of metabolic waste and lack of nutrients between the graft–host interface. The study of Hatanaka et al[7] showed that endothelial pump function would stop when the fluid circulation of the interface of the endothelium was suspended. To the best of our knowledge, this is the first case reporting spontaneous resolution of DM detachment after DALK with retained host DM and endothelium.
This case suggests that the retained host DM may be associated with DM detachment after DALK and surgeons should check whether donor DM layers are completely removed during DALK. For the DM detachment without roll rim, spontaneous reattachment may occur several months after surgery. We could wait and observe. In addition, AS-OCT is a good method to detect and monitor DM detachment.
Footnotes
Abbreviations: AS-OCT = anterior segment optical coherence tomography, DALK = deep anterior lamellar keratoplasty, DM = Descemet membrane, HM= hand motion, IOP = intraocular pressure, PKP = penetrating keratoplasty.
The authors have no conflicts of interest to disclose.
References
- [1].Melles GR, Lander F, Rietveld FJ, et al. A new surgical technique for deep stromal, anterior lamellar keratoplasty. Br J Ophthalmol 1999;83:327–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].MacIntyre R, Chow SP, Chan E, et al. Long-term outcomes of deep anterior lamellar keratoplasty versus penetrating keratoplasty in Australian keratoconus patients. Cornea 2014;33:6–9. [DOI] [PubMed] [Google Scholar]
- [3].Assia EI, Levkovich-Verbin H, Blumenthal M. Management of Descemet's membrane detachment. J Cataract Refract Surg 1995;21:714–7. [DOI] [PubMed] [Google Scholar]
- [4].Chow VW, Agarwal T, Vajpayee RB, et al. Update on diagnosis and management of Descemet's membrane detachment. Curr Opin Ophthalmol 2013;24:356–61. [DOI] [PubMed] [Google Scholar]
- [5].Passani A, Sframeli AT, Loiudice P, et al. Late spontaneous resolution of a double anterior chamber post deep anterior lamellar keratoplasty. Saudi J Ophthalmol 2017;31:58–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Müller TM, Verdijk RM, Lavy I, et al. Histopathologic features of Descemet membrane endothelial keratoplasty graft remnants, folds, and detachments. Ophthalmology 2016;123:2489–97. [DOI] [PubMed] [Google Scholar]
- [7].Hatanaka H, Koizumi N, Okumura N, et al. A study of host corneal endothelial cells after non-Descemet stripping automated endothelial keratoplasty. Cornea 2013;32:76–80. [DOI] [PubMed] [Google Scholar]


