Abstract
Fluid resuscitation was used on aged patients with traumatic shock in their early postoperative recovery. The present study aimed to assess whether different fluid resuscitation strategies had an influence on aged patients with traumatic shock.
A total of 219 patients with traumatic shock were recruited retrospectively. Lactated Ringer and hydroxyethyl starch solution were transfused for fluid resuscitation before definite hemorrhagic surgery. Subjects were divided into 3 groups: group A: 72 patients were given aggressive fluid infusion at 20 to 30 mL/min to restore normal mean arterial pressure (MAP) of 65 to 75 mm Hg. Group B: 72 patients were slowly given restrictive hypotensive fluid infusion at 4 to 5 mL/min to maintain MAP of 50 to 65 mm Hg. Group C: 75 patients were given personalized infusion to achieve MAP of 75 to 85 mm Hg. Preoperative infusion volume, preoperative MAP, optimal initial points for surgery, postoperative shock time and mortality rates at 6 and 24 hours after surgery were determined.
No significant difference in clinical characteristics was found among the 3 groups. Amount of preoperative infusion was considerably lower in the restrictive group (P < .01, compared with group A). A significant difference in preoperative infusion volume was found between the personalized and other 2 groups (P < .01, compared with groups A and B). Patients in the personalized resuscitation group achieved a higher preoperative MAP (P < .01 compared with Group B; P < .05, compared with group A) and required less prepared time for surgery (P < .01 compared with groups A and B). In addition, a lower mortality rate at 6 and 24 hours after operation was observed in the subjects with personalized therapy (P < .05, compared with group B).
Personalized management of fluid resuscitation in traumatized aged patients with appropriate volume and speed of fluid transfusion, suggesting increased survival rate and less prepared time for surgery.
Keywords: fluid resuscitation, mean arterial pressure, operation, surgery, traumatic shock
1. Introduction
Markedly increased cases of traumatic injuries in fast-growing elderly population have posed a significant challenge to healthcare field. Possibly due to a combination of injury and pre-existing complications, the mortality rate of traumatic hemorrhagic shock was 2 to 3 times higher in the elderly than the young and middle-age patients.[1] Hemorrhage remains a major culprit of preventable death in traumatized patients.[2] Hemorrhagic shock was characterized by a pathologic state of impaired intravascular volume and oxygen delivery in patients. To promote recovery from hemorrhagic shock and prevent traumatic coagulopathy, resuscitative strategies including the procedures of fluid resuscitation, blood transfusion and use of vasopressors are applied by physicians as first-line interventions.[3] However, with decades’ evolvement of fluid resuscitation, the optimal resuscitative strategy focusing on types of loading fluids, volume and velocity of fluid administration, endpoints for resuscitation and regulation of perfusion pressure are still controversial.
Substantial animal and clinical studies have shown that aggressive intravenous fluids infusion quickly achieved the normal mean arterial pressure (MAP) before definitively controlling bleeding. However, this may decrease survival rates, even worsen conditions for patients with traumatic hemorrhagic shock due to hemodilution.[4,5] Subsequently, a concept of “hypotensive resuscitation” was proposed as an alternative to aggressive resuscitation. The restrictive administration of fluids in hypotensive therapy which considers a relatively low blood pressure as an endpoint may avoid related risk of bleeding and death,[6] but whether sufficient amount of bloodstream perfused in human organs is guaranteed remains unclear. Thus, this has led to a challenge for identifying an optimal strategy of fluid resuscitation for elderly patients; especially they commonly associated with a higher risk of impairment in their cardiovascular, respiratory, and renal systems, which may interfere with the prognosis of traumatic shock.
The optimal level of blood pressure during early management of traumatic shock is heavily debated. According to European guidelines for the management of bleeding trauma patients without brain injury, a targeted systolic blood pressure of 80 to 100 mm Hg is recommended until the bleeding is controlled.[7] Several clinical studies have been conducted to compare different choices of restored blood pressure through evaluating their clinical outcomes and adverse effects such as tissue hypoxia, increased bleeding, and clot formation. Morrison et al[8] concluded that hypotensive resuscitation therapy is a safe choice which reduces transfusion requirements and severe postoperative coagulopathy in patients with trauma. Although other studies found that there was no benefits or no reduced in-hospital mortality rate after titrating the initial therapy into hypotensive strategy by IV fluid administration.[9–11]
The objective of current study was to explore the optimal strategy of fluid resuscitation for aged patients with traumatic shock. We hypothesized that provided evidences which may serve as a guideline for aged traumatized patients, especially on consideration of the preoperative volume and speed of fluid resuscitation.
2. Methods
2.1. Patients
A total of 219 aged patients with traumatic shocks, and then subsequently arranged with surgery were eligible for this study and outcomes were analyzed retrospectively. With change of perspective on fluid resuscitation, the patients were included in different years of patient admission in our study. Seventy-two cases treated with sufficient amount of fluids administration were in group A (July 2008–December 2010). Seventy-two cases treated with restrictive hypotensive fluid resuscitation were in group B (January 2011–June 2013). Seventy-five cases treated with personalized fluid resuscitation were in group C (July 2013–December 2015). This study was approved by the Ethic Committee of Hospital.
The inclusion criteria were as follows: patients was more than 60 years old; obvious symptoms of traumatic shock; an AIS 90-ISS: Abbreviated Injury Scale 90-Injury severity score was between 16 and 75, and a prehospital time was within the range of 15 minutes to 2 hours after injury. The exclusion criteria included cardiac arrest; hospital transfers; severe brain injury; severe heart, lung, and liver disorders; and other blood disorders. Informed consents were provided by each patient in this study.
2.2. Fluid resuscitation
The objective of fluid resuscitation was to achieve a state with a stable MAP ≥75 mm Hg, a urine volume per hour was >0.5 mL/kg, an approximate CVP8 was 12 mm Hg and ScvO2 was >70% within 6 hours after injury. Vital signs and acral circulation of the patients were under scrutiny and comprehensive evaluation. Clean airway and sufficient circulation were kept in all injured patients after assessments by the Airway, Breathing, Circulation, Disability, Exposure approach. Emergent surgical treatments were identified after evaluation of systemic conditions, including heart rate, breathing, blood pressure, and urine output. The blood pressure was determined by multifunctional monitors (Philips IntelliVue MP50 M8004A, Germany). Vasoactive activity was sustained by WZ-50C microinjection pump (Smiths Medical Instrument, Zhejiang, China) to restore arterial pressure.
Diagnosis and wound treatment were given simultaneously after admission into the hospital. Based on severity assessment of traumatic shock, different strategies of fluid resuscitation were made and multiple-channel intravenous infusion pump was set up. Lactated Ringer (RL) solution and hydroxyethyl starch (HES) solution were transfused for fluid resuscitation at the approximate ratio of 2:1 (crystalloid/colloid) before controlling bleeding. Patients in group A were quickly transfused with sufficient amount of aggressive fluid resuscitation at a speed of 20 to 30 mL/min to restore a normal arterial pressure (MAP) of 65 to 75 mm Hg before surgery. Subjects in group B were slowly given restrictive hypotensive fluid resuscitation at a speed of 4 to 5 mL/min to maintain a MAP of 50 to 65 mm Hg before surgery. Subjects in group C were transfused with a mixture of RL and HES at individual, necessary speed (approximately 10–15 mL/min), and amount of fluid infusion consistent with patients’ physiological conditions, to achieve higher-than-normal MAP of 75 to 85 mm Hg before surgery. Hemostatic surgery was given as soon as possible after reaching a certain level of blood pressure in 3 groups. Twenty-four hours after surgery, all patients received same and sufficient volume of fluid. The fluid used during resuscitation, adjuvant drugs and medical devices were kept the same in all patients.
2.3. Clinical outcomes
Basic demographic and clinical characteristics including age, locations, types and severity of injuries, and AIS 90-ISS scores were carefully assessed among the patients. The time interval from admission into emergency department to set-up of multichannel intravenous infusion pump was recorded. And time interval from the time of recovering to the beginning of surgery was also recorded. Other important indicators such as preoperative volume of fluid resuscitation (from admission into emergency department to definitive surgery), preoperative MAP, and postoperative volume of fluid administration within 24 hours were assessed and compared among the 3 groups. After fluid resuscitation and surgical operations, the time that was required to achieve the goal of fluid resuscitation, mortality rates at 6 and 24 hours after surgery were determined in the 3 groups.
2.4. Statistical analyses
All statistical analysis were performed by using SPSS, version 19.0 (IBM Inc., Chicago), and data of normal distribution were presented by mean ± standard deviation (mean ± SD), and otherwise were presented as median and range. The comparison among different groups was performed by analysis of variance. For categorical data, they are expressed as number of cases or percentage and the difference among different groups was measured by chi-square test of homogeneity. For non-normally distributed data, Kruskal–Wallis H test was used in our study as appropriate. Probability value of P < 0.05 was considered to be statistically significant.
3. Results
3.1. Demographic characteristics of aged patients with acute traumatic shock
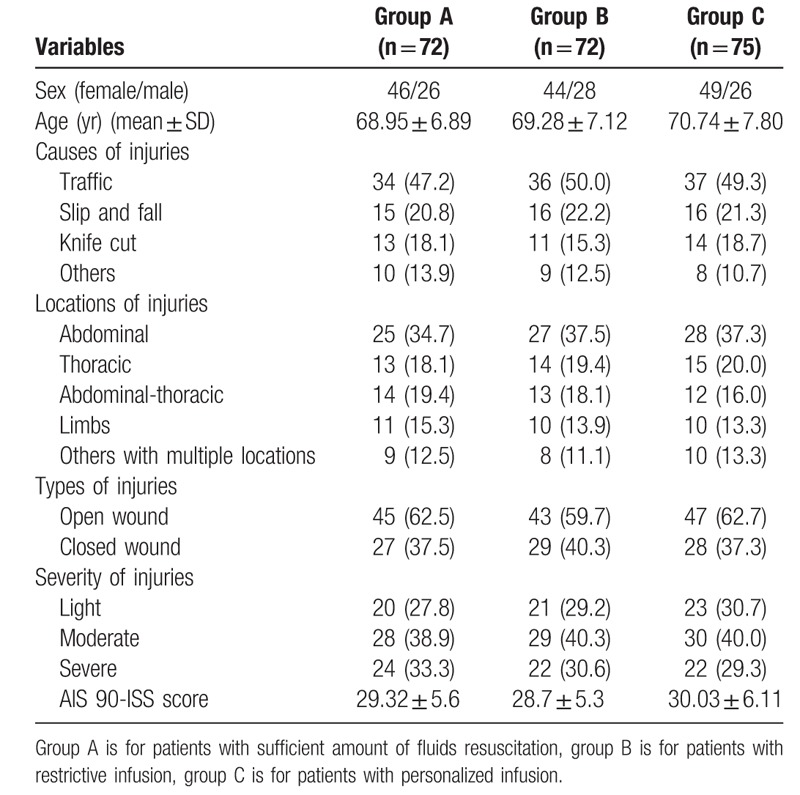
A total of 219 patients were included in this study. Demographic characteristics of study population including causes, types, locations and severity of injuries, age, and sex were reviewed from their medical records (Table 1). There were no statistically significant differences among the 3 groups for demographic characteristics for sex, age, causes of injuries, locations of injuries, type of injuries, and severity of injuries (P > .05), suggesting they were comparable for study on clinical outcomes of different types of fluid resuscitation. Enrolled aged patients with traumatic shock were more common occur in men than in women. The mean age of patients in group A, B, and C was 68.95, 69.28, and 70.74 years, respectively. The leading cause of injuries was traffic accidents, followed by slip or fall and knife cut. Most locations of injuries were abdomen and thorax, and a relatively small part of patients had injuries in limbs. Most of wounds were closed type rather than open type possibly due to the most of injuries in patient was caused by vehicle accidents and falling.
Table 1.
Demographic and clinical characteristics of aged patients with acute traumatic shock.
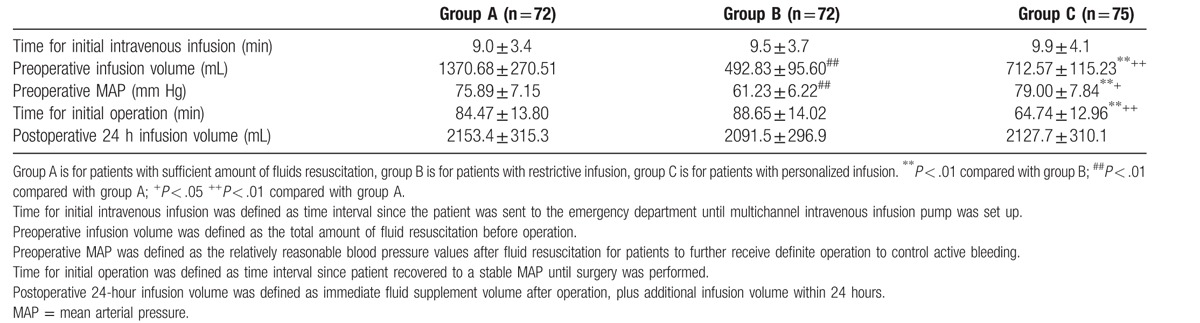
3.2. Personalized fluid resuscitation significantly shortened prepared time for surgery
To identify which type of fluid resuscitation was most efficient and economic, we examined the prepared time required to complete set-up of intravenous infusion and surgical operation after admission into the emergency department, respectively. Preoperative MAP and preoperative volume of fluid administration were measured accordingly. As indicated in Table 2, the time required to begin intravenous infusion showed no significant difference compared among the 3 groups (P > .05). Compared to the restrictive hypotensive fluid resuscitation, personalized and aggressive fluid resuscitation infused more volume of fluid and maintained higher preoperative MAP (P < .01). In addition, a relatively higher level of MAP was recovered in the personalized fluid resuscitation group (P < .05). More volume of fluids was saved compared to aggressive MAP (P < .01). In addition, we found that the similar sufficient amount of postoperative fluids administration among the 3 groups. Patients in the personalized fluid resuscitation group took the shortest waiting time before surgery, which suggested personalized fluid resuscitation had the advantage of quickly preparing for aged patients with surgical treatment.
Table 2.
Clinical outcomes compared among patients with sufficient, restrictive, and personalized infusion of fluid resuscitation.
3.3. Clinical outcomes among the 3 fluid resuscitation strategies
To compare the clinical outcomes among the 3 fluid resuscitation strategies, the time that was required to achieve the objectives of fluid resuscitation, mortality rates at 6 and 24 hours after surgery was recorded. As shown in Table 3 and Figure 1, personalized fluid resuscitation had significantly shortened time to achieve goals of fluid resuscitation and reduced mortality rates at 6 and 24 hours after surgery compared to aggressive and restrictive hypotensive therapy, suggesting that personalized fluid resuscitation had better effects on improving prognosis.
Table 3.
The comparison of clinical outcome measures in aggressive, restrictive and personalized fluid resuscitation.
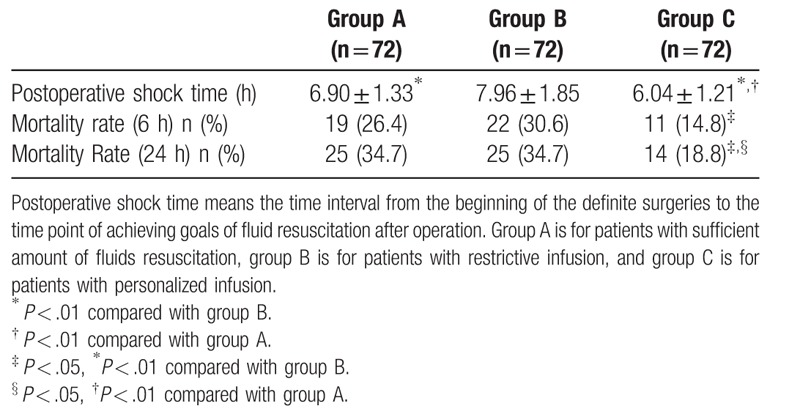
Figure 1.
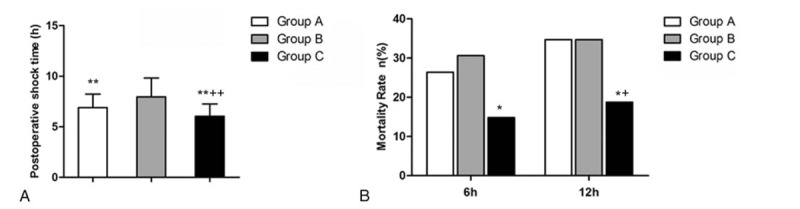
Clinical outcome measures in aggressive (A), restrictive (B), and personalized fluid resuscitation (C). A, Postoperative shock time (h). B, Mortality rate (6 and 12 h) (%). ∗indicate P < .05, ∗∗indicate P < .01 compared with group B; + indicate P < .05, ++ indicate P < .01 compared with group A.
4. Discussion
Many developing countries have accepted chronological age of 60 years or older as the elderly in contrast to 65 years old accepted in most developed countries.[12] According to previous studies, age may cause differences in targeted ideal resuscitation pressure,[13] which is consistent with that the criteria for normal blood pressure is increased with age. The elderly subjects have reduced ability of regulating homeostasis, decreased myocardial contractility, and impaired diastolic function, which may affect the status of hemodynamics and significantly increase susceptibility for multiple diseases. For patients with traumatic shocks, the loss of blood could result in dehydration and destroy cardiac function, which may endanger the lives of patients.
Insufficient amount of fluid administration may result in reperfusion injury among multiple organs and tissues.[14] Compared to the young, the aged patients had increased blood viscosity and higher risk of reperfusion injury in organs after surgery. In addition, the elderly show reduced tolerance to anesthesia and intensified drug reactions especially when fluids are administrated under less-than-normal blood pressure.[15] However, in comparison with aggressive resuscitation, hypotensive resuscitation could avoid severe hemodilution and coagulation disturbance caused by rapid administration of large volume of fluids and attenuate inflammatory and oxidative response.[16] Balancing volume of the fluids for resuscitation during treatments is critical for improving patients’ clinical outcome. Thus, maintaining a relatively high MAP and administrating moderate volume of fluids is a possible solution to this dilemma.
The time interval from the onset of the injury is extremely important for survival of patients with traumatic shock. As reported in other studies, a large proportion of patients with severe injury died of traumatic hemorrhagic shock, and the mortality rate within 24 hours after the onset of injury reached >50%.[17,18] Thus, saving prepared time for surgery may increase the survival rate for patients with traumatic shock. Because of the heterogeneity of cardiovascular conditions among aged persons, a general therapy may not be suitable or effective for the recovery of patients with traumatic shock. To increase efficiency and effectiveness of fluid resuscitation, we have taken individual characteristics of each patient into consideration in our study, which lessened the restriction of infusion volume meanwhile quickly achieved a relatively higher preoperative MAP. Based on our results, the personalized therapy administrated more fluids than hypotensive resuscitation but significantly less than aggressive resuscitation. In addition, it maintained a higher MAP than aggressive and hypotensive resuscitation. After measuring prepared time that required to begin the surgery and postoperative mortality rates, we found personalized could significantly shorten prepared time required for surgery and reduce mortality rates within 6 and 24 hours compared to aggressive and hypotensive resuscitation, which suggested that personalized therapy is a better choice for aged patients with traumatic shock.
Here, we concluded several advantages of personalized therapy over aggressive and hypotensive resuscitation. Retain a stable MAP for surgery consistent with physiological conditions of aged patients who usually demonstrate a higher level of blood pressure compared to young adults. Save prepared time for patients to accept surgical treatment and increase survival rate. Recover blood perfusion in organs and tissues but without interfering the homeostasis by large amount of fluid administration. Avoid the risk of accidents during the process of anesthesia due to hypotension. Our study provided possible guidelines of fluid resuscitation for aged patients. However, our study is limited by its retrospective design and relatively small sample size. Thus, we suggest a larger-scale prospective study be conducted in future, also enlarge our focus for the aged patients such as patients in ICU and include more clinical measures to further identify optimal fluid resuscitation.
Footnotes
Abbreviations: HES = hydroxyethyl starch, MAP = mean arterial pressure, RL = lactated Ringer.
This research is supported by 3 grants. One is The Planning Program of Zhejiang Science and Technology Department (grant No: 2014C33134). The second one is The Medical science and technology plan of Zhejiang Province (grant number: 2014KYB265). The third one is The Medical science and technology plan of Zhejiang Province (grant number: 2018ZH041).
The authors report no conflicts of interest.
References
- [1].Perdue PW, Watts DD, Kaufmann CR, et al. Differences in mortality between elderly and younger adult trauma patients: geriatric status increases risk of delayed death. J Trauma Acute Care Surg 1998;45:805–10. [DOI] [PubMed] [Google Scholar]
- [2].Kauvar DS, Wade CE. The epidemiology and modern management of traumatic hemorrhage: US and international perspectives. Crit Care 2005;9:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Bouglé A, Harrois A, Duranteau J. Resuscitative strategies in traumatic hemorrhagic shock. Ann Intensive Care 2013;3:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Lira A, Pinsky MR. Choices in fluid type and volume during resuscitation: impact on patient outcomes. Ann Intensive Care 2014;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Santry HP, Alam HB. Fluid resuscitation: past, present, and the future. Shock 2010;33:229–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Mapstone J, Roberts I, Evans P. Fluid resuscitation strategies: a systematic review of animal trials. J Trauma 2003;55:571–89. [DOI] [PubMed] [Google Scholar]
- [7].Rossaint R, Bouillon B, Cerny V, et al. Management of bleeding following major trauma: an updated European guideline. Crit Care 2010;14:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Morrison CA, Carrick MM, Norman MA, et al. Hypotensive resuscitation strategy reduces transfusion requirements and severe postoperative coagulopathy in trauma patients with hemorrhagic shock: preliminary results of a randomized controlled trial. J Trauma Acute Care Surg 2011;70:652–63. [DOI] [PubMed] [Google Scholar]
- [9].Dutton RP, Mackenzie CF, Scalea TM. Hypotensive resuscitation during active hemorrhage: impact on in-hospital mortality. J Trauma Acute Care Surg 2002;52:1141–6. [DOI] [PubMed] [Google Scholar]
- [10].Haut ER, Kalish BT, Cotton BA, et al. Prehospital intravenous fluid administration is associated with higher mortality in trauma patients: a National Trauma Data Bank analysis. Ann Surg 2011;253:371–7. [DOI] [PubMed] [Google Scholar]
- [11].Kentner R, Safar P, Prueckner S, et al. Titrated hypertonic/hyperoncotic solution for hypotensive fluid resuscitation during uncontrolled hemorrhagic shock in rats. Resuscitation 2005;65:87–95. [DOI] [PubMed] [Google Scholar]
- [12].Orimo H, Ito H, Suzuki T, et al. Reviewing the definition of “elderly”. Geriatr Gerontol Int 2006;6:149–58. [Google Scholar]
- [13].Li T, Zhu Y, Tian K, et al. Ideal resuscitation pressure for uncontrolled hemorrhagic shock in different ages and sexes of rats. Crit Care 2013;17:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Ozciftci S, Gamli M, Ornek D, et al. An evaluation of the effects of perioperatively administered fluids on ischemia/reperfusion injury. Pak J Med Sci 2015;31:1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Li T, Lin X, Zhu Y, et al. Short-term, mild hypothermia can increase the beneficial effect of permissive hypotension on uncontrolled hemorrhagic shock in rats. J Am Soc Anesthesiologists 2012;116:1288–98. [DOI] [PubMed] [Google Scholar]
- [16].Zhang Y-m, Gao B, Wang J-j, et al. Effect of hypotensive resuscitation with a novel combination of fluids in a rabbit model of uncontrolled hemorrhagic shock. PLoS One 2013;8:e66916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Lomas-Niera J, Perl M, Chung C-S, et al. Shock and hemorrhage: an overview of animal models. Shock 2005;24:33–9. [DOI] [PubMed] [Google Scholar]
- [18].Nunez TC, Cotton BA. Transfusion therapy in hemorrhagic shock. Curr Opin Crit Care 2009;15:536–41. [DOI] [PMC free article] [PubMed] [Google Scholar]


