Abstract
Background:
Overactive bladder is stated as the occurrence of urinary urgency which will cause negative impacts and decrease patients’ health-related quality of life. The aim of this systematic review is to assess the efficiency and safety of acupuncture for adults with overactive bladder (OAB) comparing with sham-acupuncture, drugs, and acupuncture plus drugs.
Methods:
We independently searched 9 databases from beginning to August 15, 2017. Two writers extracted data at the same time independently. Study outcomes were calculated by standardized mean differences (SMD) with 95% confidence intervals (CIs) and mean difference (MD) with 95% CIs.
Results:
Ten randomized controlled trials (RCTs) with 794 patients were included in this systematic review. The combined results showed that electroacupuncture (EA) may be more effective than sham electroacupuncture (sham EA) in improving the 24-hour nocturia episodes and EA may enhance tolterodine for relieving voiding symptoms and enhancing patients’ quality of life. However, more trials with high quality and larger sample sizes will be needed in the future to provide sufficient evidence. Only 15 of 794 OAB patients from the included studies reported mild adverse reactions related to EA, therefore, acupuncture is safe for treating OAB.
Conclusion:
Acupuncture might have effect in decreasing the number of micturition episodes, incontinence episodes, and nocturia episodes. However, the evidence is insufficient to show the effect using acupuncture alone or the additional effect to drugs in treating OAB.
Keywords: acupuncture, meta-analysis, overactive bladder, randomized controlled trial, systematic review
1. Introduction
The International Continence Society (ICS) terms overactive bladder (OAB) as the occurrence of urinary urgency (all day long). Presence or absence of urge urinary incontinence, it typically attended by increased episodes and nocturia enuresis in defect of urinary tract infection or any other noticeable pathology.[1,2] Its prevalence ranges from 5.2% to 22% and increases with age in adults with OAB.[3,4] Symptoms of OAB not only have a bad influence on health-related quality of life during the daytime but also increase social problems.[5] Behavioral therapy is the first line treatment and patients need to invest effort and time to the therapy.[6,7] Oral anticholinergic drugs (solifenacin, tolterodine, etc.) are used on the second-line treatment. However, a headache, dry mouth, and vision irregularity are obvious observed in patients who take these drugs.[7–10] Percutaneous tibial nerve stimulation (PTNS) of the lower urinary tract, is a second-line treatment for refractory OAB[11] which is not widely used recently. Sacral nerve stimulation are used in the third line which is limited because of its invasive nature.[12,13] In recent years, acupuncture has been applied in doctoring OAB and has been stated effective in improving patients’ quality of life with only a few side effects.[14–17] A systematic review on OAB was published in Chinese,[18] however, the broad inclusion criteria and the small sample sizes of studies might bring some bias. The aim of this systematic review is to assess the efficiency and safety of acupuncture for adults with OAB comparing with sham-acupuncture, drugs, and acupuncture plus drugs.
2. Methods
According to our published protocol,[19] this systematic review was directed in keeping with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) statement.[20]
2.1. Studies
Randomized controlled trials (RCTs) in the language of English and Chinese of acupuncture therapy for OAB were encompassed in this systematic review without any restrictions of publication type.
2.2. Participants
With no restriction of race or gender, participants who were at least 18 years old and diagnosed with OAB (based on the ICS explanation and the standards of the American Urological Association (AUA)[13]) were included.
2.3. Interventions
Acupuncture is defined as insertion of the needle into acupoints. In order to regulate “energy” of meridians, the needle is manipulated to receive soreness, distention, numbness, and other sensations named “deqi.”[21] Therefore, electroacupuncture (EA), manual acupuncture, warm acupuncture, scalp acupuncture, and auricular acupuncture were included. The control intervention included sham/placebo acupuncture, no treatment, and any active treatments, such as bladder retraining, surgery, neurologic stimulation, and pharmacological therapies. Sham/placebo acupuncture is defined as minimal or no insertion into nonacupoints or acupoints. Moreover, trials evaluating acupuncture plus one active treatment versus the same active treatment were included.
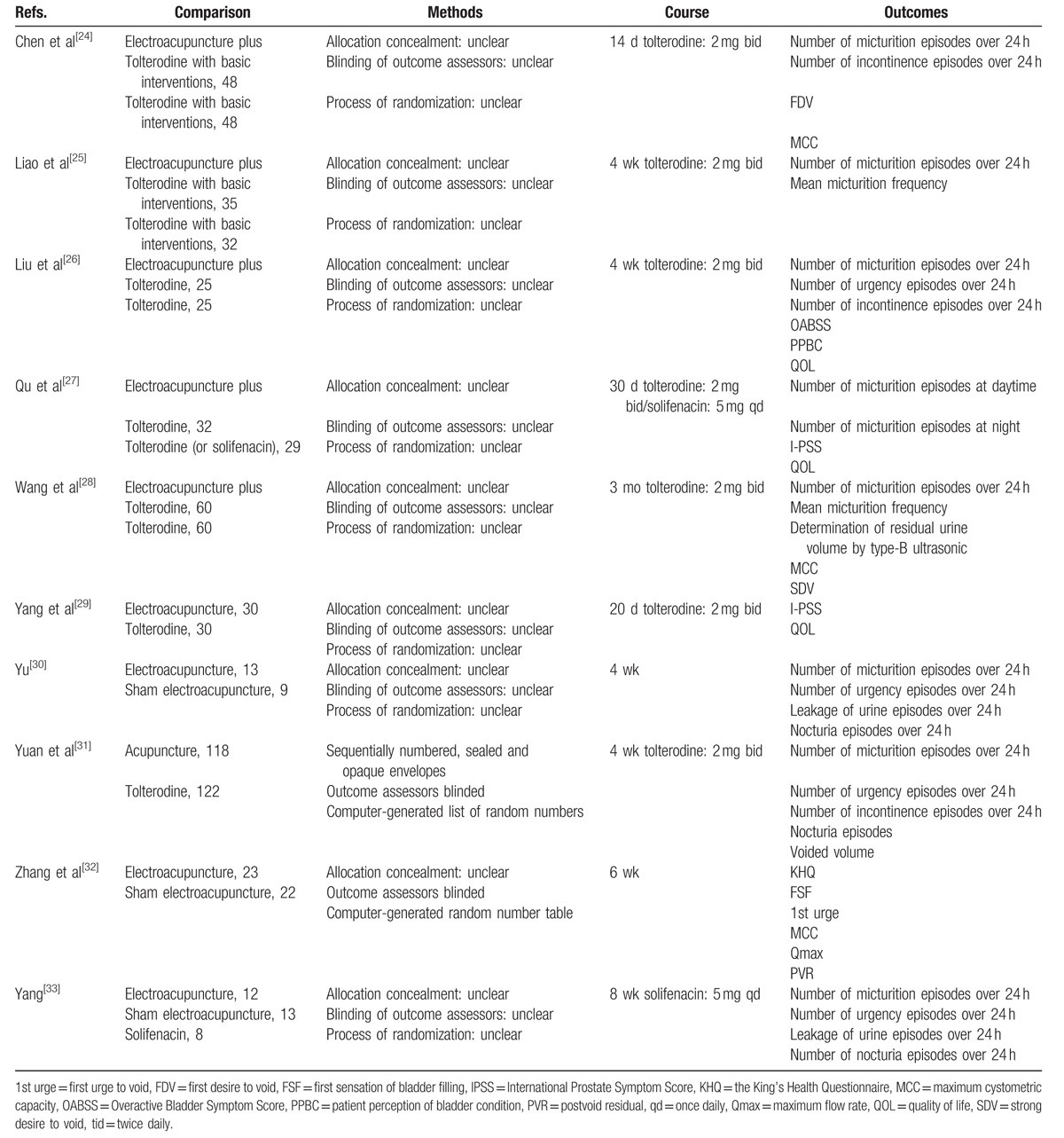
Studies comparing a combination of different types of acupuncture with other therapies or acupuncture compared with different one kind of acupuncture were also excluded, because it is problematic to evaluate the effectiveness of acupuncture in such studies. Furthermore, it is tough to assess the effectiveness of herbs, so studies comparing acupuncture with herbs were also excluded. Table 1 presents the types of acupuncture interventions included.
Table 1.
Summary of the included studies.
2.4. Outcome measures
The amount of micturition episodes and incontinence episodes were over 24 hours, and quality of life (QOL) were the main outcomes. Mean urine volume and cytometric maximum capacity were the secondary outcomes.
2.5. Search methods for study identification
Based on the Cochrane handbook guidelines,[22] a search strategy should be planned and used. So there were 23 terms in the search strategy which is presented in the protocol, such as a randomized controlled trial.pt, acupuncture.mp, OAB.tw, etc. Two reviewers (YZ and JZ) independently reviewed the next 9 databases from start to August 15, 2017: MEDLINE, EMBASE, The Cochrane Incontinence Group Trials Register, The Cochrane Central Register of Controlled Trials (CENTRAL), China National Knowledge Infrastructure (CNKI), Wan-Fang Data, Chinese Scientific Journal Database, Chinese Biomedical Literature Database (CBM), and Chinese Medical Current Content (CMCC). Acupuncture Research (1976–July 1998), the Journal of Clinical Acupuncture and Moxibustion (1985–July 1998), the Shanghai Journal of Acupuncture and Moxibustion (1982–July 1998), and Chinese Acupuncture and Moxibustion (1981–July 1998), which were printed out of the duration of the databases, were manually examined in libraries.
3. Data collection and analysis
3.1. Study selection
Those readings were simultaneously screened by 2 independent reviewers (YZ and QM). A third author (ZL) joined in the consultation or discussion with the 2 reviewers when any disagreements occurred. Figure 1 shows the study selection details.
Figure 1.
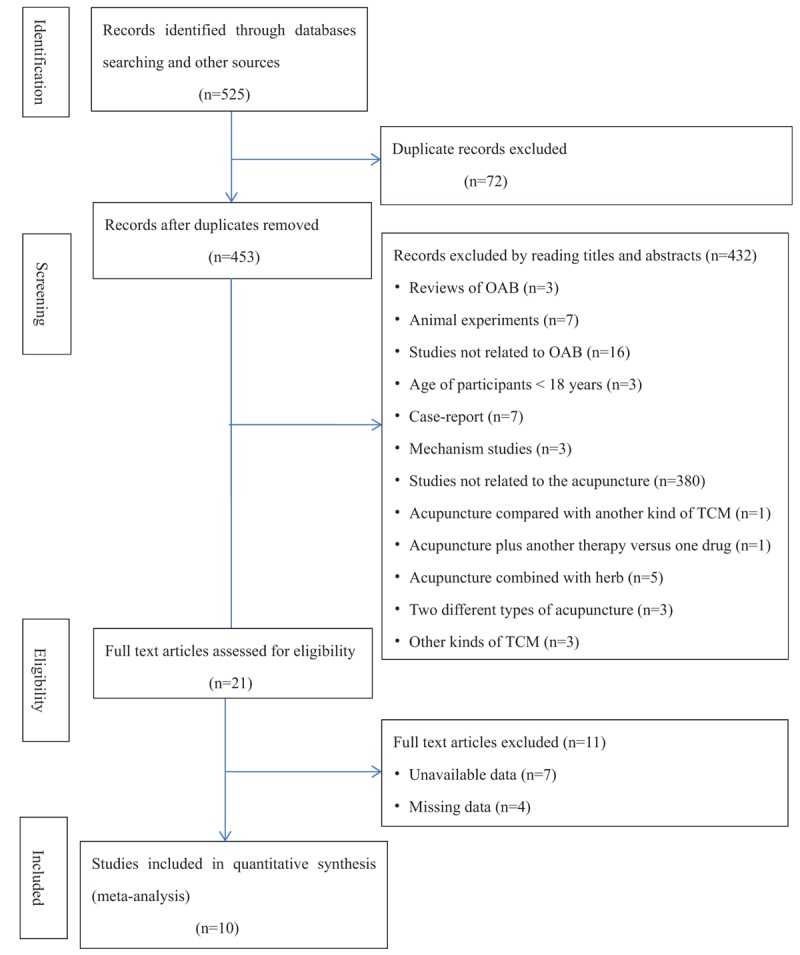
Study flow diagram.
3.2. Data extraction
The title and abstract of these studies were independently reviewed by 2 authors (YZ and QM) who identified RCTs. For those studies that could not be identified as an RCT by the title and abstract, the full text was independently reviewed by the same authors. The 2 reviewers (YZ and QM) used standard extraction forms to collect data from the included trials. A third author (ZL) judged the decisions after a discussion about the disagreements. Data extraction procedure followed the modified Standard for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA).[23]
3.3. Risk of bias in individual studies
Sequence generation, blinding or masks, allocation concealment, selective outcome reporting, incomplete data assessment, and other sources of bias making up the 6 domains of bias[22] as said by the Cochrane Handbook for Systematic Reviews of Interventions were applied to evaluate the risk of bias in each included study. Any disagreement was judged by discussion (ZL). However, assessment of publication bias and a funnel plot were prevented to use due to inadequate number of trials in this review.
3.4. Data synthesis
3.4.1. Measure the treatment's effectiveness
It is valid to use the risk ratio (RR) and 95% confidence interval (CI) for dichotomous data. Standardized mean differences (SMD) with 95% CIs or mean differences (MD) with 95% CI was used to analyze the primary and the secondary outcomes. The reviewers attempted to gather additional information by communicating with the authors via e-mail or phone to ask for the missing data. The analysis was based on the available statistics when we could not contact the study investigators. The Higgins I2 statistic was wielded to test the heterogeneity among the included trials. I2 ≥ 50% reflected that heterogeneity existed among the trials, and we analyzed the clinical and methodological heterogeneity to detect how they relate to the results. A subgroup analysis was conducted according to whether there were basic interventions (lifestyle modification, bladder training, pelvic floor muscle training, etc.) in the treatment group. A subgroup analysis was also conducted based on the patients’ gender and disease process when such data were available. The sensitivity analysis was led to assess the influence of many factors, such as study design, eligibility criteria, analysis methods, and methodological quality, and to evaluate the certainty of the results of this review.
4. Results
4.1. Selection of studies
In the aggregate, 525 records were included and 72 were excluded as duplicate records. After screening the title and abstract, another 453 records were disqualified. The full texts of 21 records were reviewed. Finally, 10 studies met all the inclusion criteria.[24–33] Except for 2 studies in English,[31,32] the other 8 studies were reported in Chinese.[24–30,33] The study screening and a summary of the included studies are presented in Fig. 1 and the details of the included studies are shown in Table 1. Descriptions of the acupuncture interventions are shown in Table 2.
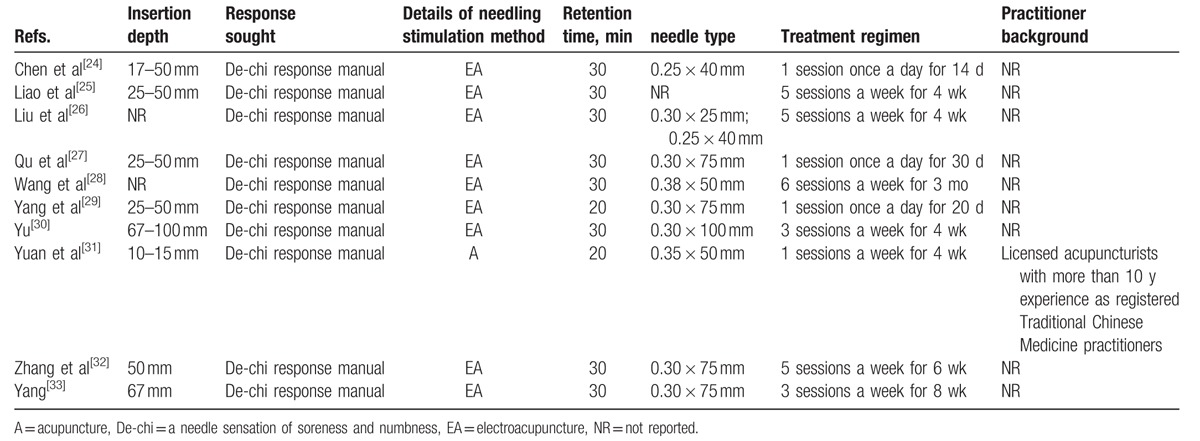
Table 2.
Descriptions of the acupuncture interventions.
4.2. Patients
The 10 studies[24–33] enrolled overall 794 participants (590 female and 84 male, 120 unstated). All patients were diagnosed with OAB according to the ICS. The age range of the participants was from 22 to 75.
4.3. Interventions
4.3.1. Acupuncture interventions
A majority of acupuncturists chose acupuncture points depending on the theory of Chinese medicine and their clinical experience. EA was used in nine studies,[24–30,32,33] and manual needle stimulation was performed in one trial.[31] Sanyinjiao (SP6), Pangguangshu (BL28), Ciliao (BL32), Taixi (KI3), and Shenshu (BL23) were the most commonly used points. The treatment period ranged from 2 weeks to 3 months. All the included studies reported using “de qi.”
4.3.2. Control inventions
Three[30,32,33] out of the 10 included studies compared acupuncture with sham-acupuncture (SA). Three studies[29,31,33] compared acupuncture with tolterodine or solifenacin. Five trials[24–28] compared acupuncture plus tolterodine with tolterodine.
4.4. Outcome measures
Seven[24–26,28,30,31,33] of the 10 studies used the amount of micturition episodes over 24 hours and 4 studies[24,26,31,33] used the amount of incontinence episodes over 24 hours to report clinical improvement. QOL[26,27,29] was used as the scoring system to measure the treatment outcome. Maximum cystometric capacity (MCC)[24,28,32] and the average micturition volume[25,27] were also used to measure the treatment outcome and to report clinical improvement.
4.5. Risk of bias
All of the RCTs mentioned randomization and 2 trials[31,32] reported adequate sequence generation. Two studies[31,32] used a computer-generated random number to allocate participants. One[31] of the 10 studies provides details about appropriate allocation concealment. Only 2 studies[31,32] in this review were measured to take a small risk of bias for outcome assessor blinding. None of the encompassed RCTs blinded the acupuncturists because of the nature of acupuncture. The assessment of the risk of bias is displayed in Fig. 2.
Figure 2.
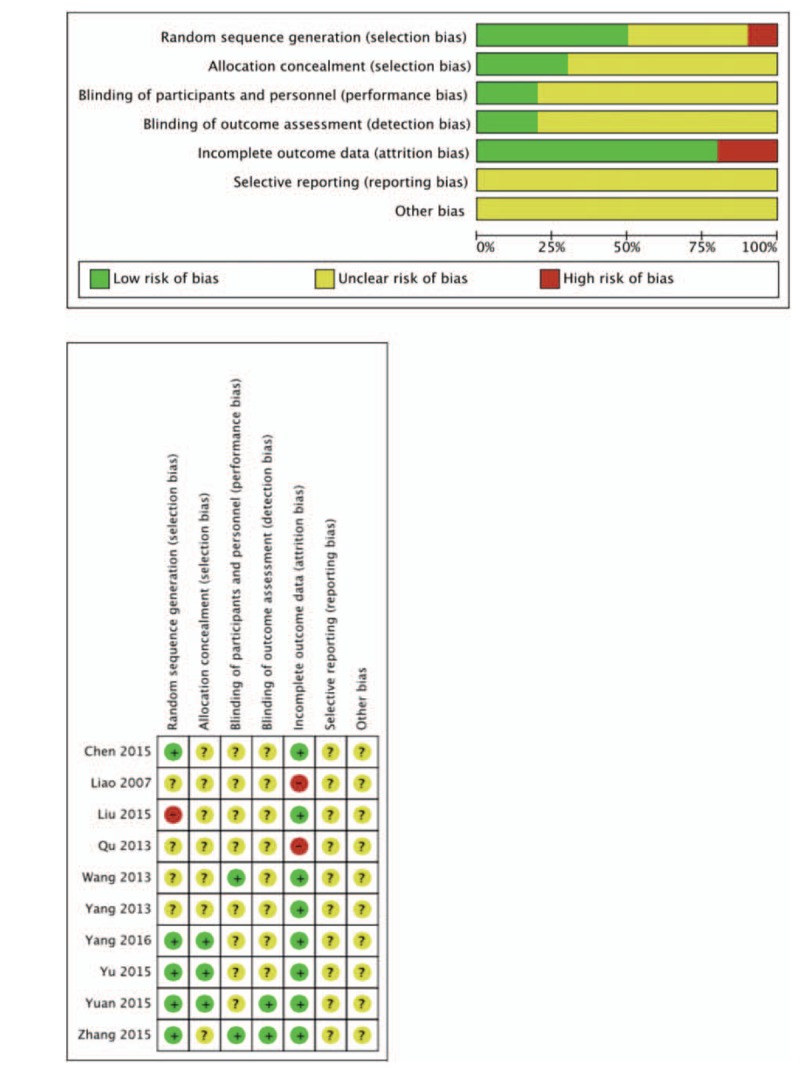
The assessment of the risk of bias.
4.6. Acupuncture versus sham acupuncture
Three of the trials[30,32,33]compared EA with sham electroacupuncture (sham EA). One trial[32] was not in the meta-analysis because of the different outcome assessments which were Overactive Bladder Symptom Score (OABSS) and the King's Health Questionnaire (KHQ).
4.6.1. 24-hour micturition episodes
Two trials were pooled together using the random effects model (MD 3.60, 95% CI: −0.42–7.63),[30,33] and the results showed high heterogeneity (I2 = 71%). There was no significant difference between EA and sham EA for decreasing the 24-hour micturition episodes (Fig. 3). As for only 2 trials included in meta-analysis, subgroup and sensitivity analysis could not be conducted.
Figure 3.
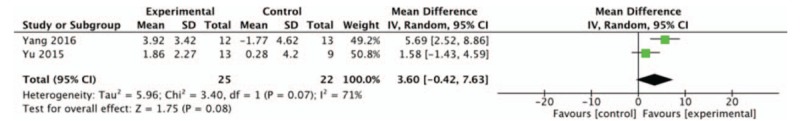
The effect of electroacupuncture versus sham electroacupuncture on the 24-hour micturition episodes (a forest plot using the random model).
4.6.2. 24-hour urgency episodes
Two trials were pooled together[30,33] using the fixed effects model (MD 1.76, 95% CI: −2.24–5.76) and the results showed no heterogeneity (I2 = 0%). There was no significant difference between EA and sham EA in improving 24-hour urgency episodes (Fig. 4).
Figure 4.
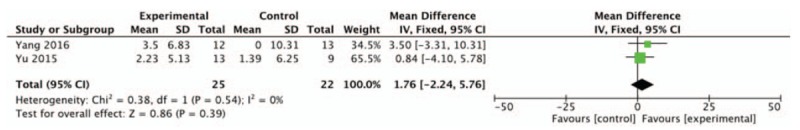
The effect of electroacupuncture versus sham electroacupuncture on the 24-hour urgency episodes (a forest plot using the fixed model).
4.6.3. 24-hour nocturia episodes
The results of the 2 pooled trials[30,32] using the fixed effects model (MD 1.76, 95% CI: 0.63–2.88) showed no heterogeneity (I2 = 0%). EA decreased more numbers of 24-hour nocturia episodes than sham EA (Fig. 5).
Figure 5.
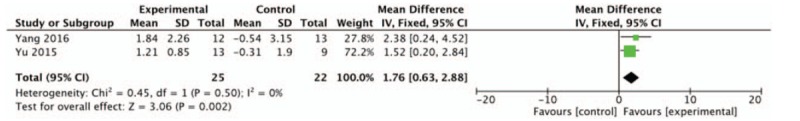
The effect of electroacupuncture versus sham electroacupuncture on the 24-hour nocturia episodes (a forest plot using the fixed model).
4.6.4. 24-hour incontinence episodes
The results of the 2 pooled trials[30,33] using the random effects model (MD 1.90, 95% CI: −1.79–5.59) were with substantial heterogeneity (I2 = 65%), which showed no statistical difference between EA and sham EA on the part of 24-hour incontinence episodes (Fig. 6).
Figure 6.
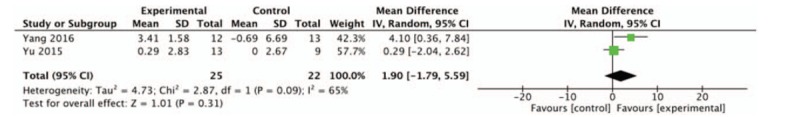
The effect of electroacupuncture versus sham electroacupuncture on the 24-hour incontinence episodes (a forest plot using the random model).
4.7. Acupuncture versus drugs
Three of the included trials[29,31,33] compared EA with tolterodine or solifenacin. These 3 trials could not be contained in meta-analysis because of the inconformity of the outcome measurements. Two trials[31,33] found that even though there was a significant enhancement in the EA group, there was no significant statistical difference between EA and drugs (tolterodine or solifenacin) in terms of decreasing the 24-hour urgency episodes, the 24-hour incontinence episodes, daytime micturition episodes and the nocturia episodes. Another trial[29] found statistical difference between EA and tolterodine in decreasing the International Prostate Symptom Score (I-PSS), but the score of QOL scale only improved in EA group.
4.8. Acupuncture plus drugs versus drugs
4.8.1. 24-hour micturition episodes
Four trials[24–26,28] compared the combination of EA and tolterodine with tolterodine alone were pooled together using the random effects model and the results showed substantial heterogeneity (I2 = 88%). A sensitivity analysis was performed and the heterogeneity might be caused by whether basic interventions (lifestyle modification, bladder training, pelvic floor muscle training, etc.) were administered in the treatment group. A subgroup analysis was conducted and the pooled analysis of 2 trials[24,25] revealed that there was statistically significant difference between EA combined with tolterodine and tolterodine in decreasing the 24-hour micturition episodes (MD −1.28, 95% CI: −1.62 to −0.94, I2 = 19%), but with the premise that both groups included a basic intervention. However, the pooled results of the other 2 trials[26,28] showed no significant difference between EA combined with tolterodine and tolterodine in terms of the 24-hour micturition episodes (MD −0.19, 95% CI: −0.49 to 0.11, I2 = 29%) (Fig. 7).
Figure 7.
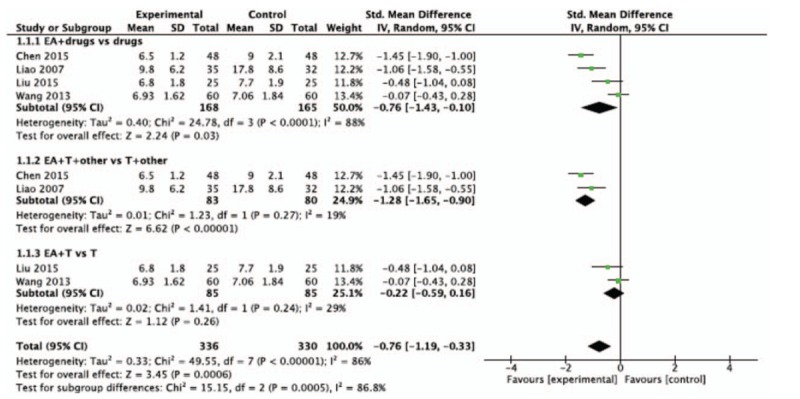
The effect of acupuncture plus drugs versus the same drugs on the 24-hour micturition episodes (a forest plot using the random model).
4.8.2. 24-hour incontinence episodes
Two trials were pooled together,[24,26] and the results were homogenous using the fixed effects model (MD −0.56, 95% CI: −0.83– −0.28, I2 = 0%). There was statistically significant difference between EA combined with tolterodine and tolterodine in decreasing the number of 24-hour incontinence episodes than tolterodine (Fig. 8).
Figure 8.
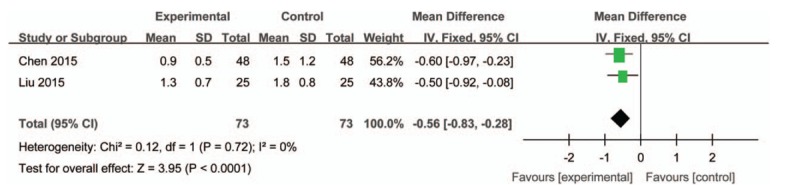
The effect of acupuncture plus drugs versus the same drugs on the number of 24-hour incontinence episodes (a forest plot using the fixed model).
4.8.3. Maximum cystometric capacity (MCC)
Two trials[24,28] were pooled by using the random effects model, and the MD was 44.05 (95% CI: 29.51–58.59, I2 = 78%). The results revealed that there was statistical difference between EA plus tolterodine and tolterodine in increasing MCC (Fig. 9).
Figure 9.
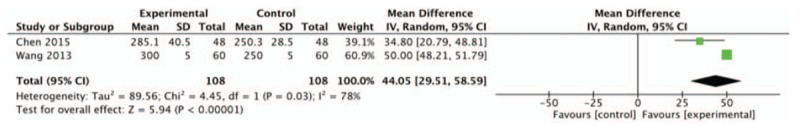
The effect of acupuncture plus drugs versus the same drugs on the MCC (a forest plot using the random model).
4.8.4. 24-hour micturition volume
Two trials[25,28] were pooled together by using random effects model and there was a high degree of heterogeneity (I2 = 88%). The pooled results revealed that there was statistical difference between EA plus tolterodine and tolterodine in increasing the 24-hour micturition volume (SMD 0.72, 95% CI: −0.21 to 1.65, I2 = 88%) (Fig. 10).
Figure 10.
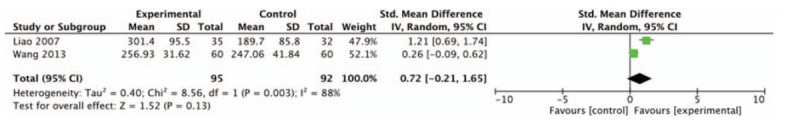
The effect of acupuncture plus drugs versus the same drugs on the 24-hour micturition volume (a forest plot using the random model).
4.8.5. Quality of life
Two trials[26,27] were pooled together using the fixed model. The results showed that there was statistical difference between EA plus tolterodine and tolterodine in decreasing the quality of life score (MD −1.35, 95% CI: −1.71 to −0.98, I2 = 0%) (Fig. 11).
Figure 11.
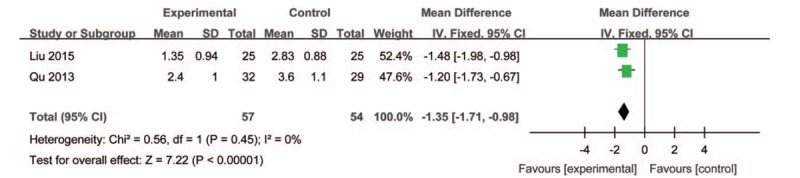
The effect of acupuncture plus drugs versus the same drugs on quality of life (a forest plot using the fixed model).
4.9. Safety
Three of the included trials mentioned adverse effects. One trial[32] reported that 5 patients had minor pain when needling (3 in the EA group and 2 in the sham EA group). Needling pain was reported in nine cases in another trial.[31] The other trial[30] reported that 1 patient had subcutaneous bruises, which disappeared without any medical attention. No patient drop-out occurred in the included trials because of adverse effects.
5. Discussion
The purpose of this systematic review is to evaluate the effectiveness and safety of acupuncture for adults with OAB. Studies comparing acupuncture with sham-acupuncture or drugs and comparing acupuncture plus drugs with drugs were included. Although 10 RCTs with a total of 794 participants were included, there was still lack of strong evidence to show the effectiveness of acupuncture in treating OAB.
The symptom most disturbing to OAB patients was frequent urination followed by urinary urgency, urgency incontinence, and nocturia.[34] Urgency is considered as the brand symptom of OAB, however, it has proven problematic to exactly define or to describe for clinical goal or research. So for measuring treatment effectiveness, many studies have relied upon other measures such as the number of urination and of incontinence episodes.[35] Three trials[30,32,33] included comparisons of EA with sham EA for OAB; however, only 2 trials were contained in the meta-analysis due to the different outcome assessments. The pooled results indicated that EA was not better than sham EA in decreasing the number of 24-hour micturition episodes, 24-hour urgency episodes, and 24-hour incontinence episodes, except for the number of 24-hour nocturia episodes. However, these 2 trials did not evaluate the expected value of acupuncture and acupuncture points selected in these 2 trials for the sham EA group were the same as for the EA group. Therefore, the results of meta-analysis does not mean that EA is ineffective in treating OAB even though more trials with large sample sizes will be needed.
Three trials assessed the effectiveness of EA compared with drugs (tolterodine and solifenacin). The combined results of 2 trials[31,33] showed no difference between EA and drugs for improving the voiding symptoms even though another trial[29] reported that EA was more likely to improve patients’ quality of life. Because it is a differential design, it cannot be explained that the efficacy of EA is not inferior to that of positive drugs. Because the design of the 3 trials was to detect the inequality, the conclusion that EA is inferior to active drugs cannot be drawn. More trials will be needed to provide powerful evidence of the effect of acupuncture for treating OAB.
Three trials accessed the effectiveness of EA compared with drugs (tolterodine and solifenacin). Two trials[31,33] showed no difference between EA and drugs for improving the voiding symptoms even though another trial[29] reported that EA was more likely to improve the score of I-PSS. Nevertheless, more trials will be needed to provide powerful evidence of the effect of acupuncture for treating OAB.
Four trials[24–26,28] evaluating the additional effectiveness of acupuncture to tolterodine in improving the 24-hour micturition episodes were pooled together and subgroups analyses were conducted. The combined results of 2 trials[24,25] indicated that acupuncture plus tolterodine was more effective than tolterodine for improving the 24-hour micturition episodes on the basis of basic interventions (lifestyle modification, bladder training, pelvic floor muscle training, etc.). Due to the effect of basic interventions, it is hard to address the effectiveness of acupuncture as an adjuvant of tolterodine in treating OAB.[26,28] Moreover, the pooled results of the other 2 trials[24,26] showed that EA combined with tolterodine may have better effectiveness than tolterodine alone in decreasing 24-hour incontinence episodes, increasing MCC and improving OAB patients’ quality of life. However, only 2 trials were included in meta-analysis and an affirmative conclusion still cannot be drawn because of the small sample sizes and an insufficient number of RCTs.
Additionally, for the other outcomes described in the previous protocol, such as the amount of pads used over 24 hours and the number of nocturnal awakenings due to OAB over 24 hours, it is a lack of sufficient evidence to show the effectiveness of acupuncture in treating OAB.
Adverse reactions were reported descriptively. Totally 794 OAB patients treated by acupuncture or acupuncture plus other treatments underwent a safety assessment. Only 15 cases had mild adverse reactions related to EA, and none of them had severe adverse reactions during or after treatment. Thus, EA is safe for treating OAB patients. However, adverse events related to acupuncture need large surveys and studies.
All of the RCTs mentioned randomization and 2 trials[31,32] reported adequate sequence generation. Two studies[31,32] used a computer-generated random number to allocate participants. One[31] of the 10 studies provides details about appropriate allocation concealment. Only 2 studies[31,32] in this review were measured to take a small risk of bias for outcome assessor blinding. None of the included RCTs blinded the acupuncturists because of the characteristic of acupuncture. In order to avoid more bias, we conducted unified criteria of inclusion and exclusion firmly to decrease the clinical heterogeneity from different participants, interventions and outcome measures.
This systematic review and meta-analysis was conducted according to previous published protocol.[19] One published systematic review[36] in Chinese included 6 trials assessing the effect of acupuncture in OAB. The results showed that acupuncture might reduce the episodes of daily micturition episodes, micturition episodes over 3 days, and incontinence episodes. However, the diagnosis and design of included studies in this previous systematic review is not clear. According to our rigorous criteria in our study, 5[37–41] trials included in the previous study[36] were excluded. In addition, 1 trial[37] compared acupuncture with EA included in this previous systematic review were excluded in our study. Moreover, another 2 added databases Wan-Fang Data and Chinese Scientific Journal Database were searched in our study to receive wider retrieval range. Our systematic review also included RCTs that used sham EA in the control group in addition to drugs and other therapies, and different outcome measurements.
Recently, some studies[42–44] have confirmed the effectiveness of PTNS in treating OAB.[45] PTNS is a method based on the actual anatomical substrate,[11] which is different from the traditional acupuncture acting on “energy pathways.” The effectiveness of acupuncture lies on “de qi” which is defined as the sensation of sourness, numbness, distention, and pain after insertion of the needle into an acupoint. Therefore, studies accessing the effectiveness of PTNS for treating OAB were excluded in this systematic review.
6. Evidence quality
None of the trials comparing EA with sham EA mentioned the process of evaluating the credibility of the sham and whether the sham was indistinguishable from true acupuncture. The unblinding of patients and psychological effect may lead to the overestimation of the effects of acupuncture and performance bias. Moreover, although all of the trials mentioned randomization, few of them mentioned the randomization process or the allocation concealment. Additionally, the limited information about the included trials made it very difficult to evaluate detection, attrition, and reporting bias. Therefore, limited evidence and small sample sizes were underpowered to detect the efficacy of acupuncture, the benefit of acupuncture when compared with drugs and the additional effect of acupuncture to drugs.
7. Implications of the review for practice and research
Firstly, for studies using sham EA as the control group compared with true acupuncture, some types of sham EA have psychological effects that may affect the results. Therefore, objective outcomes are better to show efficacy of acupuncture. Secondly, when acupuncture is compared with drugs, blinding of patients and the expectation effects of acupuncture should be measured appropriately. Thirdly, 1 review[46] found that subjective outcomes offer a valuable complement to objective measures, so combining with subjective and objective assessments could make assessments more complete. Lastly, none of the included RCTs mentioned how long the effect of treatment will last, so the follow-up period should be designed in future research to observe the long-term effect of acupuncture.
8. Limitations
Several limitations of this review should be assessed. Even though hand-searching the journals not included in the electronic database could minimize publication bias, it was difficult to obtain all of the unpublished data. Moreover, the bias introduced by the inclusion of RCTs only in Chinese or English cannot be avoided. Because of the inadequate number of trials with small sample sizes, the effectiveness of acupuncture in different forms cannot be evaluated.
9. Conclusion
According to the results of meta-analysis, acupuncture might have effect in decreasing the number of micturition episodes, incontinence episodes, and nocturia episodes. However, the evidence is insufficient to show the effect using acupuncture alone or the additional effect to drugs in treating OAB. Nevertheless, acupuncture is comparatively with few adverse reactions and safe. In the future, studies with high methodological quality and larger sample sizes are required.
Acknowledgment
All authors of this manuscript would like to give our sincere thanks to the editors from American Journal Experts who have helped us modify the language.
Footnotes
Abbreviations: 1st urge = first urge to void, AUA = the American Urological Association, CBM = Chinese Biomedical Literature Database, CENTRAL = The Cochrane Central Register of Controlled Trials, CI = confidence interval, CMCC = Chinese Medical Current Content, CNKI = China National Knowledge Infrastructure, EA = electroacupuncture, FDV = first desire to void, FSF = first sensation of bladder filling, ICS = The International Continence Society, IPSS = International Prostate Symptom Score, KHQ = the King's Health Questionnaire, MCC = maximum cystometric capacity, MD = mean difference, NR = not reported, OAB = overactive bladder, OABSS = Overactive Bladder Symptom Score, PPBC = patient perception of bladder condition, PRISMA = the Preferred Reporting Items for Systematic Reviews and Meta-analyses, PTNS = percutaneous tibial nerve stimulation, PVR = postvoid residual, qd = once daily, Qmax = maximum flow rate, QOL = quality of life, RCTs = randomized controlled trials, RR = risk ratio, SA = sham-acupuncture, SDV = strong desire to void, sham EA = sham electroacupuncture, SMD = standardized mean differences, STRICTA = Standard for Reporting Interventions in Clinical Trials of Acupuncture, T = tolterodine, tid = twice daily.
Funding: This study was supported by the National Natural Science Foundation of China (grant no. 81173353 and grant no. 81373732).
YZ and JZ are the cofirst authors of this systematic review.
Protocol registration: PROSPERO CRD42014006756.
Protocol published in BMJ-open.
The authors have no conflicts of interest to disclose.
References
- [1].Wein AJ, Rovner ES. Definition and epidemiology of overactive bladder. Urology 2002;60:7–12. [DOI] [PubMed] [Google Scholar]
- [2].Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 2010;29:4–20. [DOI] [PubMed] [Google Scholar]
- [3].Wang Y, Xu K, Hu H, et al. Prevalence, risk factors, and impact on health-related quality of life of overactive bladder in China. Neurourol Urodyn 2011;30:1448–55. [DOI] [PubMed] [Google Scholar]
- [4].Irwin DE, Milsom I, Hunskaar S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 2006;50:1306–14. [DOI] [PubMed] [Google Scholar]
- [5].Coyne KS, Sexton CC, Kopp ZS, et al. The impact of overactive bladder on mental health, work productivity and health-related quality of life in the UK and Sweden: results from EpiLUTS. BJU Int 2011;108:1459–71. [DOI] [PubMed] [Google Scholar]
- [6].Burgio KL, Goode PS, Johnson TM, et al. Behavioral versus drug treatment for overactive bladder in men: the Male Overactive Bladder Treatment in Veterans (MOTIVE) Trial. J Am Geriatr Soc 2011;59:2209–16. [DOI] [PubMed] [Google Scholar]
- [7].Hartmann KE, McPheeters ML, Biller DH, et al. Treatment of overactive bladder in women. Evid Rep Technol Assess (Full Rep) 2009;187:1–20. [PMC free article] [PubMed] [Google Scholar]
- [8].Staskin DR, Oefelein MG. A systematic review and meta-analysis of randomized controlled trials with antimuscarinic drugs for overactive bladder. Eur Urol 2008;54:740–64. [DOI] [PubMed] [Google Scholar]
- [9].Maman K, Aballea S, Nazir J, et al. Comparative efficacy and safety of medical treatments for the management of overactive bladder: a systematic literature review and mixed treatment comparison. Eur Urol 2014;65:755–65. [DOI] [PubMed] [Google Scholar]
- [10].Buser N, Ivic S, Kessler TM, et al. Efficacy and adverse events of antimuscarinics for treating overactive bladder: network meta-analyses. Eur Urol 2012;62:1040–60. [DOI] [PubMed] [Google Scholar]
- [11].de Wall LL, Heesakkers JP. Effectiveness of percutaneous tibial nerve stimulation in the treatment of overactive bladder syndrome. Res Rep Urol 2017;9:145–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Tang H, Chen J, Wang Y, et al. Combination of sacral neuromodulation and tolterodine for treatment of idiopathic overactive bladder in women: a clinical trial. Urol J 2014;11:1800–5. [PubMed] [Google Scholar]
- [13].Gormley EA, Lightner DJ, Burgio KL, et al. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline. J Urol 2012;188:2455–63. [DOI] [PubMed] [Google Scholar]
- [14].Ernst E, White AR. Prospective studies of the safety of acupuncture: a systematic review. Am J Med 2001;110:481–5. [DOI] [PubMed] [Google Scholar]
- [15].Park J, Sohn Y, White AR, et al. The safety of acupuncture during pregnancy: a systematic review. Acupunct Med 2014;32:257–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Adams D, Cheng F, Jou H, et al. The safety of pediatric acupuncture: a systematic review. Pediatrics 2011;128:1575–87. [DOI] [PubMed] [Google Scholar]
- [17].Lin JG, Chen YH, Gao XY, et al. Clinical efficacy, mechanisms, and safety of acupuncture and moxibustion. Evid Based Complement Alternat Med 2014;2014:356258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Xu HR, Liu ZS, Zhao H. Acupuncture for adults with overactive bladder—a systematic review. J Integr Tradit Chin West Med 2011;4:393–9. [Google Scholar]
- [19].Mo Q, Wang Y, Ye Y, et al. Acupuncture for adults with overactive bladder: a systematic review protocol. BMJ Open 2015;5:e006756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;349:g7647. [DOI] [PubMed] [Google Scholar]
- [21].Zhou K, Fang J, Wang X, et al. Characterization of de qi with electroacupuncture at acupoints with different properties. J Altern Complement Med 2011;17:1007–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. Cochrane Collab 2011;1–552. [Google Scholar]
- [23].MacPherson H, Altman DG, Hammerschiag R, et al. Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT statement. PLoS Med 2010;7:e1000261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Chen X, Chen J, Tang SL. Clinical observation of 48 cases of electroacupuncture combined with Luoding in the treatment of female overactive bladder. Hainan Med J 2015;1:127–8. [Google Scholar]
- [25].Liao XQ, Tang H, Xiao P. 35 cases of electro-acupuncture at BL23 for overactive bladder. J Clin Acupunct 2007;1:35–6. [Google Scholar]
- [26].Liu Z, Chen HL, Wu W, et al. Clinical observation and treatment of tolterodine combined with electro-acupuncture for overactive bladder. Chin Med Innov 2015;1:52–4. [Google Scholar]
- [27].Qu YW, Chen XY, Qu ML, et al. 32 cases of electro-acupuncture of overactive bladder. Chian Healthcare Nutr 2013;3:641. [Google Scholar]
- [28].Wang YF, Pan ZL, Chen JJ, et al. Clinical study of electro-acupuncture for overactive bladder. Pract Clin Med 2013;3:1–3. [Google Scholar]
- [29].Yang YJ, Guo BY, Liu JX, et al. Clinical observation on 30 cases of female urethral syndrome treated by electroacupuncture. Nei Mongol J Tradit Chin Med 2013;17:38. [Google Scholar]
- [30].Yu HZ. Electro-acupuncture treatment of overactive bladder. Beijing Univ Chin Med 2015;1–45. [Google Scholar]
- [31].Yuan ZY, He CX, Yuan SB, et al. Acupuncture for overactive bladder in female adults: a randomized controlled trial. World J Urol 2015;33:1303–8. [DOI] [PubMed] [Google Scholar]
- [32].Zhang J, Cheng W, Cai MM. Effects of electroacupuncture on overactive bladder refractory to anticholinergics: a single-blind randomised controlled trial. Acupunct Med 2015;33:368–74. [DOI] [PubMed] [Google Scholar]
- [33].Yang WY. Electro-acupuncture treatment of overactive bladder with Baliao and Huiyang. Beijing Univ Chin Med 2016;1–36. [Google Scholar]
- [34].Mitchell SA, Brucker BM, Kaefer D, et al. Evaluating patients’ symptoms of overactive bladder by questionnaire: the role of urgency in urinary frequency. Urology 2014;84:1039–43. [DOI] [PubMed] [Google Scholar]
- [35].Gormley EA, Lightner DJ, Burgio KL, et al. Diagnosis and Treatment of Overactive Bladder (Non-Neurogenic) in Adults: AUA/SUFU Guideline. 2014;Linthicum, Maryland: American Urological Association Education and Research, Inc., 1–11. [Google Scholar]
- [36].Xu HR, Liu ZS, Zhao H. Systematic evaluation for treatment with acupuncture for overactive bladder syndrome. Mod J Integr Tradit Chin West Med 2011;20:393–9. [Google Scholar]
- [37].Li GX. Clinical observation of electro-acupuncture at Baliao acupoints in the treatment of overactive bladder. Fujiang Univ Chin Med 2008;1–59. [Google Scholar]
- [38].Zheng XQ. Clinical observation on acupuncture treatment of overactive bladder in stroke patients. J Clin Exp Med 2006;5:1830–1. [Google Scholar]
- [39].Song LG, Su XZ. Treatment of 80 cases of overactive bladder after cerebral infarction with acupuncture and moxibustion. Tradit Chin Med Res 2007;20:54–5. [Google Scholar]
- [40].Emmons SL, Otto L. Acupuncture for overactive bladder: a randomized controlled trial. Obstet Gynecol 2005;106:138–43. [DOI] [PubMed] [Google Scholar]
- [41].Pan ZL, Wang YF. Acupuncture treatment of overactive bladder: a report of 30 cases. Shandong Med J 2008;48:84. [Google Scholar]
- [42].Del Rlo-Gonzalez S, Aragon IM, Castillo E, et al. Percutaneous tibial nerve stimulation therapy for overactive bladder syndrome: clinical effectiveness, urodynamic, and durability evaluation. Urology 2017;108:52–8. [DOI] [PubMed] [Google Scholar]
- [43].Scaldazza CV, Morosetti C, Giampieretti R, et al. Percutaneous tibial nerve stimulation versus electrical stimulation with pelvic floor muscle training for overactive bladder syndrome in women: results of a randomized controlled study. Int Braz J Urol 2017;43:121–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Kizilyel S, Karakeci A, Ozan T, et al. Role of percutaneous posterior tibial nerve stimulation either alone or combined with an anticholinergic agent in treating patients with overactive bladder. Turkish J Urol 2015;41:208–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Preyer O, Umek W, Laml T, et al. Percutaneous tibial nerve stimulation versus tolterodine for overactive bladder in women: a randomised controlled trial. Eur J Obstet Gynecol Reprod Biol 2015;191:51–6. [DOI] [PubMed] [Google Scholar]
- [46].Abramsa P, Artibanib W, Gajewskic JB, et al. Assessment of treatment outcomes in patients with overactive bladder: importance of objective and subjective measures. Urology 2006;68:17–28. [DOI] [PubMed] [Google Scholar]


