Abstract
Rationale:
Duplication of the extrahepatic bile duct is an extremely rare congenital anomaly of the biliary system.
Patient concerns:
A 44-year-old woman presented with a history of continuous upper abdominal pain and vomiting.
Diagnoses:
Magnetic resonance cholangiopancreatography (MRCP) disclosed diffuse dilatation of the intrahepatic and extrahepatic bile ducts. Endoscopic retrograde cholangiopancreatography (ERCP) showed the presence of two extrahepatic bile ducts with calculus at the distal end of the CBD.
Interventions:
Laparoscopic cholecystectomy (LC) was performed after an ERCP. Choledochoscopy, performed during the operation, showed duplicated common bile duct and the cystic duct was seen opening at the right side of the extrahepatic duct.
Outcomes:
The patient was doing well after 6 months of follow-up.
Lessons:
We reported a case of a double common duct with choledocholithiasis and gallstone. This rare anomaly may lead to cholangitis, common bile duct injury during surgery, malignancy occurrence, and should be treated with extreme care.
Keywords: case report, double common bile duct, duplication of the extrahepatic bile duct, duplication of the extrahepatic bile duct
1. Introduction
Duplication of the extrahepatic bile is an extremely rare congenital anomaly of the biliary system, which is characterized by the presence of a septum within the common bile duct or an accessory common bile duct.[1] The first double common bile-duct (DBCD) case was reported by Vesalius in 1543.[2] Before the year 2007, there were 4 identified types of such anomaly. In 2007, Choi et al. found a new type of DBCD and classified it as type V.[3] Since then, only 6 type V CBCD have been reported. In this case report, we present a recently recognized a rare case of type Vb duplicated common bile duct with choledocholithiasis and cholelithiasis.
2. Case report
A 44-year-old Chinese woman was admitted to a local hospital April 2017 due to persistent upper abdominal pain and vomiting for 12 days. The ultrasonography of the abdomen performed at the local hospital revealed a swollen gallbladder with the presence of gallstone and cholecystitis. The episodes of pain were not relieved by antibiotic treatment with cefuroxime. The patient then came to Sir Run Run Shaw Hospital for a second opinion and further treatment. At the time of admission, the patient's physical examination revealed severe tenderness in the upper right quadrant of the abdomen with positive Murphy sign without rebound tenderness or muscle tension. The patient's liver biochemistry indicated a cholesteric profile, including an alkaline phosphatase of 225 U/L (normal U/L), γ-glutamyl transferase value of 371 U/L (normal U/L), a total bilirubin of 80.5 U/L (normal U/L), and a direct bilirubin of 64.0 U/L (normal U/L). The results of the liver function test were evaluated, including an alanine aminotransferase of 164 U/L and an aspartate aminotransferase of 233 U/L. Serum amylase and lipase indicated an acute pancreatitis (serum amylase 2564 U/L; serum lipase 4495 U/L). Enhanced computed tomography (CT) examination performed at Sir Run Run Shaw Hospital revealed diffuse dilatation of the intrahepatic and extrahepatic bile ducts, with suspected common bile duct obstruction and gallstones. Magnetic resonance cholangiopancreatography (MRCP) also disclosed diffuse dilatation of the intrahepatic and extrahepatic bile ducts, but no obvious filling-defect was found in the CBD lumen (Fig. 1A). The levels of serum amylase and lipase decreased rapidly after conservative treatment, which included enough fluid support and antibiotic. Endoscopic retrograde cholangiopancreatography (ERCP) was subsequently performed and demonstrated the presence of 2 extrahepatic bile ducts with calculus at the distal end of the CBD. On ERCP, it was observed that the extrahepatic bile duct was separated into 2 ducts directly after the confluence of left and right hepatic ducts, and rejoined as a single duct and opened into the duodenum at the normal site (Fig. 1B). Laparoscopic cholecystectomy (LC) was performed after this patient recovered from ERCP. Choledochoscopy during the LC also showed common bile duct duplication, and the cystic duct was seen draining into the right-sided extrahepatic duct (Fig. 1C). This 44-year-old female patient was discharged 2 days after LC. Pathological examination of the resected gallbladder and duct revealed a benign gallbladder with chronic cholecystitis. The patient was doing well after 6 months of follow-up.
Figure 1.
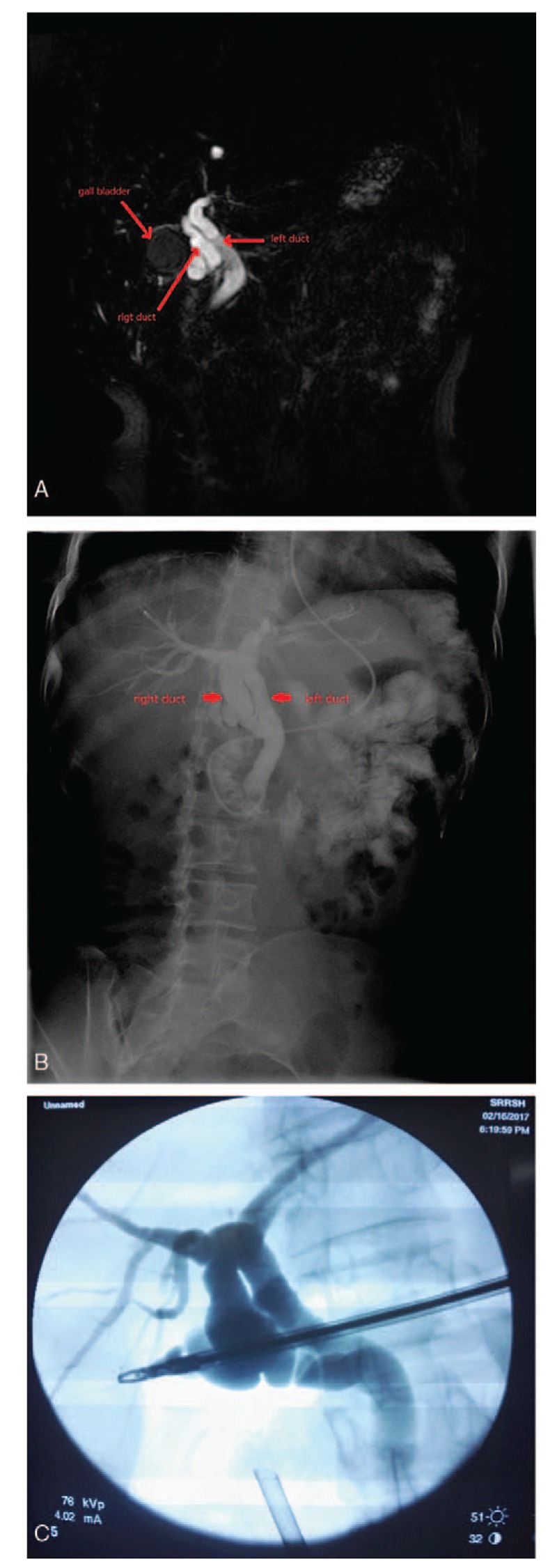
Magnetic resonance cholangiopancreatography showed common bile duct (A); double common bile duct was observed during the ERCP (B); diagram of the DCBD based on the intraoperative choledochoscopy (C). DCBD = double common bile duct, ERCP = endoscopic retrograde cholangiopancreatography.
3. Discussion
This case presents an extremely rare congenital anomaly of the adult human biliary system. Duplicated bile ducts are quite common in reptiles, birds, and fish; but in humans, they are very rare.[4] The mechanism of this anomaly is believed to be related to the disruption of early embryogenesis development and preservation of an extrahepatic accessory duct.[3] The real incidence rate of this anomaly might never be known because many individuals with this anomaly are asymptomatic throughout their whole lives, making it impossible to even suspect the presence of the anomaly.
Goor and Ebert first proposed the classification of DCBD based on the anatomical appearance.[1] The most widely used classification then, was modified by Choi et al.[3] in 2007. According to the Choi's classification, there are 5 types of DCBD (Fig. 2). Different from the western and Japanese population, the proportion of type I DCBD is higher in the Chinese population than any other types (western vs Japanese vs Chinese 3.6% vs 8.5% vs 58.3%).[2,5,6]
Figure 2.
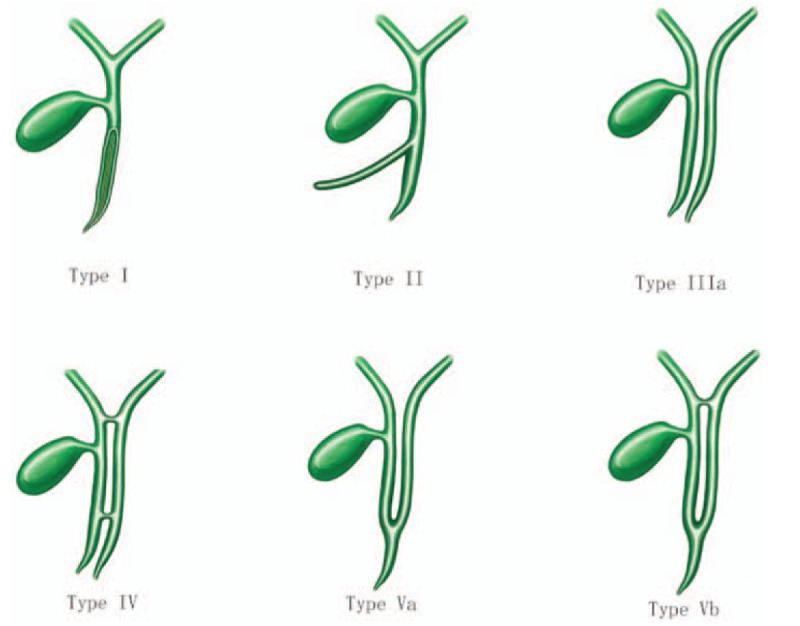
Modified double common bile duct classification. Type I, a septum within the CBD lumen; Type II, the distal bile duct bifurcates and each channel independently drains into the different sites (stomach, pancreas, and duodenum); Type III, duplicated extrahepatic bile ducts with (type IIIa) or without (type IIIb) intrahepatic communicating duct; Type IV, duplicated extrahepatic bile ducts with extrahepatic communicating channel or both intrahepatic and extrahepatic communicating channels; Type V, duplicated extrahepatic bile ducts join as a single duct and drain into the duodenum.
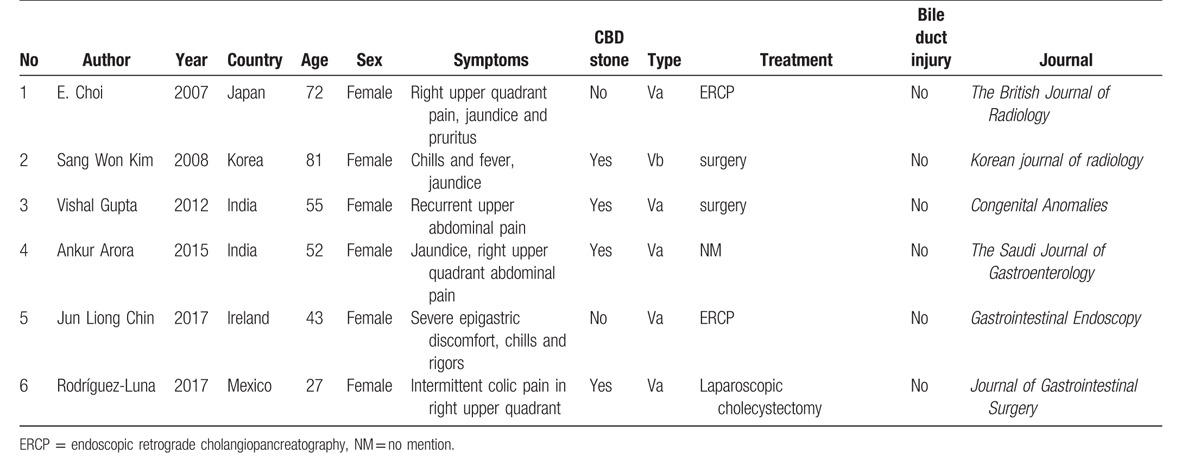
Our case was classified as type Vb common bile duct. To date, the current patient was the first type V case reported in the Chinese population and the second type Vb case in the world. The type V of double common bile duct is the rarest type of CBD. Only 6 type V double CBD cases had been reported so far. Five of them were of type Va,[3,7–10] and the remaining one was of type Vb[9] (Table 1). All the 7 patients, including our patient, were female and suffered from abdominal pain. Four cases were diagnosed as common bile duct stone, and the bile stone was removed by ERCP. The case reported by Choi et al. was the only case accompanied with malignant tumor.
Table 1.
The characteristics of Type V cases in previous literatures.
Despite it being a rarely encountered condition, it is necessary to fully understand this anomaly. Hoepfner et al. reported a case of common bile duct injury during surgery because of the existence of a duplicated CBD, which was not clearly identified during the first operation at a local hospital.[11] They performed a second operation at the University of Alabama School of Medicine Hospital to anastomose the right and left hepatic duct stumps with jejunum. Therefore, recognizing this malformation preoperatively can help avoid potential common bile duct injury intraoperatively. MRCP and ERCP are recommended when a patient is suspected with bile duct anomaly. Since ERCP is an invasive technique and might lead to potential serious complications, MRCP is preferred prior to ERCP.[3,5,9,12] For type I cases, it is harder to be identified. Only 4.2% type I cases can be diagnosed preoperatively.[5] It requires surgeons to carefully distinguish the anatomy and perform the intraoperative cholangiography if necessary to prevent CBD injury.
Another serious issue is that duplicated common bile duct is probably associated with malignant tumor. In the review reported by Yamashita et al., 12, 47 enrolled patients were also diagnosed with different kinds of cancers including pancreatic cancer, gastric cancer, gallbladder cancer, and ampullary cancer.[6] This phenomenon may partly due to the continuous regurgitation of gastric or pancreatic juice into extrahepatic bile duct.[3] In addition, no Type I case presented with cancer was found in previous literatures; the reason for this phenomenon might be due to that type I DCMD patients have no anomalous pancreaticobiliary maljunction. For type I DCBD, simple resection of the septum is recommended instead of resection of the whole bile duct because of the low incidence of malignancy. On the other hand, for types II, III, and IV DCBD, patients should undergo operation to resect accessory duct, which opens into the stomach or pancreas and strict follow-up to monitor the possible malignancy occurrence.[13] However, the strategy for type V DCBD is still unclear. We think strict monitoring would be a proper strategy.
In conclusion, one of the rarest bile duct anomaly cases was reported in this paper. Although the incidence of duplication of the extrahepatic bile duct is extremely rare, DCBD often presents with choledocholithiasis, cholangitis, gallstone, and malignant tumor, and needs close monitoring in view of providing further treatment. The correct identification of DCBD would allow safer surgical interventions.
Footnotes
Abbreviations: CBD = common bile duct, CT = computed tomography, DCBD = double common bile duct, ERCP = endoscopic retrograde cholangiopancreatography, LC = laparoscopic cholecystectomy, MRCP = magnetic resonance cholangiopancreatography.
We have obtained informed consent from the patient.
Our study was not based on a previous communication to a society or meeting.
The authors report no conflicts of interest.
References
- [1].Goor DA, Ebert PA. Anomalies of the biliary tree. Report of a repair of an accessory bile duct and review of the literature. Arch Surg 1972;104:302–9. [DOI] [PubMed] [Google Scholar]
- [2].Teilum D. Double common bile duct. Case report and review. Endoscopy 1986;18:159–61. [DOI] [PubMed] [Google Scholar]
- [3].Choi E, Byun JH, Park BJ, et al. Duplication of the extrahepatic bile duct with anomalous union of the pancreaticobiliary ductal system revealed by MR cholangiopancreatography. Br J Radiol 2007;80:e150–4. [DOI] [PubMed] [Google Scholar]
- [4].Arora A, Sureka B, Kasana V, et al. Common bile duct duplication: the more the murkier. Saudi J Gastroenterol 2015;21:51–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Chen G, Wang H, Zhang L, et al. Double common bile duct with choledochal cyst and cholelithiasis: report of a case. Surg Today 2014;44:778–82. [DOI] [PubMed] [Google Scholar]
- [6].Yamashita K, Oka Y, Urakami A, et al. Double common bile duct: a case report and a review of the Japanese literature. Surgery 2002;131:676–81. [DOI] [PubMed] [Google Scholar]
- [7].Chin JL, Sengupta S, Morrin MM, et al. Common bile duct duplication: double bile ducts, double trouble. Gastrointest Endosc 2017;85:855–6. [DOI] [PubMed] [Google Scholar]
- [8].Gupta V, Chandra A. Duplication of the extrahepatic bile duct. Congenit Anom (Kyoto) 2012;52:176–8. [DOI] [PubMed] [Google Scholar]
- [9].Kim SW, Park DH, Shin HC, et al. Duplication of the extrahepatic bile duct in association with choledocholithiasis as depicted by MDCT. Korean J Radiol 2008;9:550–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Rodriguez-Luna MR, Guarneros-Zarate JE, Noriega-Usi VM, et al. A Rare but Important Anatomical Variation to Know. J Gastrointest Surg 2017;21:2124–5. [DOI] [PubMed] [Google Scholar]
- [11].Hoepfner L, Sweeney MK, White JA. Duplicated extrahepatic bile duct identified following cholecystectomy injury. J Surg Case Rep 2016;2016: pii: rjw064. doi: 10.1093/jscr/rjw064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Arase Y, Deguchi R, Tsukune Y, et al. Double common bile duct with ectopic drainage into the stomach found in asymptomatic. Tokai J Exp Clin Med 2016;41:108–11. [PubMed] [Google Scholar]
- [13].Djuranovic SP, Ugljesic MB, Mijalkovic NS, et al. Double common bile duct: a case report. World J Gastroenterol 2007;13:3770–2. [DOI] [PMC free article] [PubMed] [Google Scholar]


