Abstract
Objective
The purpose of this study was to determine the proportion of children undergoing procedural sedation for fracture reduction in the emergency department (ED) observed to experience negative post-discharge behaviors. Predictors of negative behaviors were evaluated, including anxiety.
Methods
This was a prospective cohort study of children receiving intravenous ketamine sedation for ED fracture reduction. The child’s anxiety prior to sedation was measured with the Modified Yale Preoperative Anxiety Scale. Negative behavioral changes were measured with the Post-Hospitalization Behavior Questionnaire 1–2 weeks after discharge. Descriptive statistics and odds ratios were calculated. Chi square test was used for comparisons between groups. Multivariable logistic regression models evaluated predictors of negative behavioral change after discharge.
Results
97 patients were enrolled, 82 (85%) completed follow-up. Overall, 33 (40%) children were observed to be highly anxious pre-sedation and 18 (22%) had significant negative behavior changes after ED discharge. Independent predictors for negative behaviors were high anxiety (OR=9.0, 95% CI 2.3–35.7) and non-white race (OR= 6.5, 95% CI 1.7–25.0).
Conclusion
For children undergoing procedural sedation in the ED, two in five children have high pre-procedure anxiety and almost one in four have significant negative behaviors 1–2 weeks after discharge. Highly anxious and non-white children have increased risk of negative behavioral changes which have not been previously recognized in the ED setting.
Keywords: anxiety, behavior, children, emergency, pediatric, procedural sedation
Introduction
Background
Children in the Emergency Department (ED) frequently undergo procedures associated with significant distress despite appropriate pain control due to anxiety and the developmental stage of the child.1 Children can exhibit post-traumatic stress symptoms and negative responses to future visits when procedures are not accompanied by appropriate pain control or sedation.2 Children in the ED setting typically undergo procedural sedation in order to avoid this psychological trauma and permit safe completion of the procedure.
Although never previously evaluated for children that undergo ED procedural sedation, the link between anesthesia and negative behaviors during the weeks that follow has long been established in the surgical literature. Such a link was first described by Eckenhoff in 19533 in an observational study of 612 children who underwent general anesthesia. Personality changes were reported by the parents of 17% of children during the two months after the operation. Over the next 60 years, multiple researchers found similar links between anesthesia and negative behavioral outcomes, with short-term negative behavior rates ranging from 24% to 54% when assessed up to two weeks post-anesthesia.4–8 These negative behaviors were divided into behavioral subcategories with the most frequently reported behavioral changes being sleep anxiety, separation anxiety and apathy/withdrawal.6–7, 9–10
Many studies have shown a link between children who experience high anxiety prior to anesthesia and negative behaviors in the weeks to months after anesthesia. Children observed to be “very anxious” were 40% more likely to have a negative behavioral change.6 Other studies by Kain et al. have shown anxious children have a 3.5 times odds of negative behaviors9 and increased separation and general anxiety.10 Other researchers have demonstrated this relationship between anxiety and negative behavioral changes post-anesthesia including Zavras et al. who found that children with increased pre-anesthesia anxiety have almost five times the risk of post-anesthesia negative behavioral changes 4 and Beringer et al. who demonstrated that children with higher pre-anesthesia anxiety scores had increased negative behavioral changes.8
Importance
Though thousands of pediatric procedural sedations occur in the ED setting each year, there is only one pilot study evaluating negative behavioral changes post-discharge following ED procedural sedation.11 A study of 60 children undergoing either abscess drainage or laceration repair found 20% had negative behavioral changes at 1 week after discharge. Although laceration repair is typically considered a less painful procedure, both the laceration repair and the abscess drainage groups were found to have negative behavioral changes suggesting patient or procedural factors may be associated with negative outcomes. To date, no study has evaluated the factors associated with negative behavioral change nor specifically assessed the association between anxiety and negative post-discharge behaviors for children sedated in the ED.
Goal
The purpose of this study was to determine the proportion of children undergoing procedural sedation for fracture reduction in the ED observed to experience negative post-discharge behaviors. Predictors of negative behaviors were evaluated, including anxiety.
Methods
Study Design and Setting
This was a prospective cohort study at the Children’s Hospital of Wisconsin (CHW) ED in Milwaukee, Wisconsin from October 2014 to September 2015. This tertiary care ED has an annual volume of 65,000 pediatric visits. This study was approved by the CHW IRB.
Selection of Participants
Children eligible for the study were between the ages of 2 and 18 years who were discharged to home after receiving sedation with intravenous ketamine for fracture reduction. Children were excluded if they had moderate to severe developmental delay or were in non-English speaking families because the anxiety scoring tools used have not been validated in these populations. Children were also excluded if they were taking psychotropic medications or had an Emergency Severity Index (ESI) triage level of 1, who are considered critically ill patients requiring immediate life-saving interventions. Children were only eligible to be enrolled once. Informed consent was obtained from a parent or guardian, and assent obtained from all children 7 years and older.
Methods and Measurements
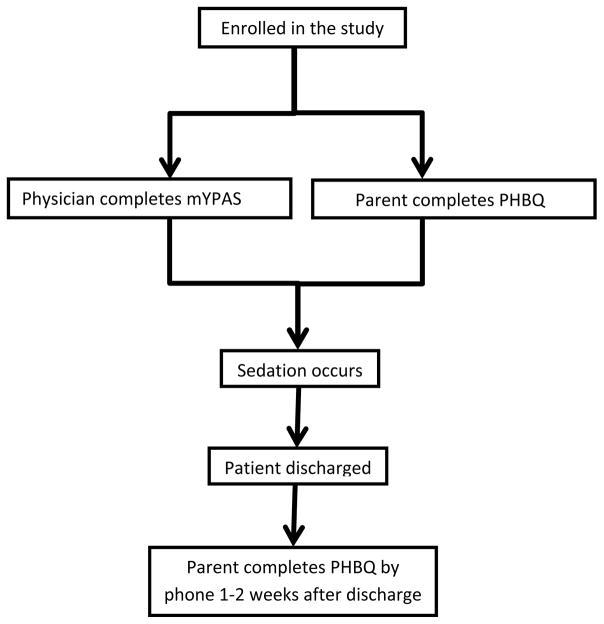
All ED care, sedation care, medication choices including concurrent use of any analgesics and discharge plans were at the physician discretion. Figure 1 shows a flow diagram of study procedures.
Figure 1.
Flow diagram of study procedures.
Predictors
Routine demographic data were collected including race (white or non-white), age (≤5 years or >5 years), gender, ethnicity (Hispanic or Non-Hispanic), and presence of a co-existing medical condition (ADHD, asthma, cardiac condition, liver disease, neurologic problem, pulmonary disorder, reactive airway disease, history of sedation failure, or seizures). Fracture type and whether patients were prescribed opiates for home was recorded. Sedation duration (time of ketamine administration to patient return to baseline determined by nursing of ≤30 minutes or >30 minutes), whether children received midazolam or analgesics prior to the sedation, cumulative dose of ketamine (mg/kg) given, adverse events during the sedation and whether children received an opiate prescription upon discharge were recorded. The cutoff points for age and sedation duration were chosen by expert opinion.
Child anxiety was assessed using the Modified Yale Preoperative Anxiety Scale (mYPAS) by the pediatric emergency medicine (PEM) physician. The mYPAS is a validated instrument that has been widely used for assessing anxiety in children undergoing anesthesia.4, 7–9 It has been previously compared to the gold standard for anxiety assessment, the State-Trait Anxiety Inventory-Child (STAI-C), and found to have excellent reliability and validity.12 It has been validated in children 2 to 18 years.12 The board certified PEM physician or fellow caring for the child in the ED completed the mYPAS immediately prior to sedation. The child was evaluated in each of the 5 categories of the mYPAS (activity, vocalizations, emotional expressivity, state of apparent arousal and use of parents). A weighted score ranging from 23 to 100 was calculated using the published scoring methods. Based on prior literature, children were categorized into the high anxiety group if their score was 40 or greater.13
Outcomes
A parent or guardian reported the primary outcome measure, the Post-Hospitalization Behavior Questionnaire (PHBQ) at baseline in the ED and at phone follow-up 7 to 14 days after ED discharge. If phone contact was not made with the parent, the survey was mailed to the home. The PHBQ is a well-validated parent-report instrument designed to assess children’s behavior with 27 questions in 6 categories (general anxiety, separation anxiety, sleep anxiety, eating disturbance, aggression toward authority and apathy/withdrawal).14 Each category has a different number of possible questions ranging from 2 questions for “eating disturbance” to 8 questions for “general anxiety.” Parents rated the child’s behaviors as much less than before, less than before, same as before, more than before or much more than before. Parents completed the PHBQ in the ED based on the child’s behavior the week prior to the sedation to obtain a baseline value. The follow-up PHBQ assessed the child’s behavior during the week after the sedation. The difference in scores between the first and the follow-up PHBQs was calculated. Significant change is defined as 7 or more negative changes from the first to the follow-up questionnaire.6, 7 The PHBQ was originally designed to study negative behavioral changes in children after surgery or hospitalization but has been used in the ED setting.11
Analysis
The sample size was calculated to detect a 3.5 times increased incidence of post-sedation negative behavioral change in patients with high levels of anxiety.9 Children with low anxiety were estimated to have a 10% incidence of negative behavioral change. Based on a two-sided α level of 0.05 and a power of 0.80, we estimated that 24 patients were needed for each group. With an estimated 10% loss to follow-up rate, 27 children total were needed for each group for an enrollment of 54 children. The sample size was increased to 80 to include at least 10 children for each of the clinical factors hypothesized to be associated with a poor outcome that were included in the univariable analysis and considered for inclusion in the multivariable analysis; race, age, gender, ethnicity, sedation duration, presence of a co-existing medical condition, use of midazolam and anxiety.
Descriptive statistics were used to compare the patients included in the analysis to those who were lost to follow-up. Negative behavioral changes reported by parents were described across the six categories of the PHBQ. As has been done previously in the ED setting, we also described the percentage of patients showing greater than 50% of the potential changes in any given category to determine which specific behaviors were most frequent.11 Univariable analysis including chi square tests were used to assess differences in patient and procedural characteristics for children who displayed negative behavioral change and those with high pre-sedation anxiety. Odds ratios with 95% confidence intervals were calculated.
Multivariable logistic regression analysis was performed to examine factors associated with negative behavioral change. Predictors were included in the multivariable analysis if they had a p-value of <0.2 in the univariable analysis. P-value for the Hosmer and Lemeshow Goodness-of-Fit test was calculated to determine adequacy of the model. A statistical significance (α) level of 0.05 was used throughout, and SAS Studio Enterprise Edition, version 3.2 (SAS Institute, Cary NC) was used to perform all statistical analysis.
Results
Characteristics of Study Subjects
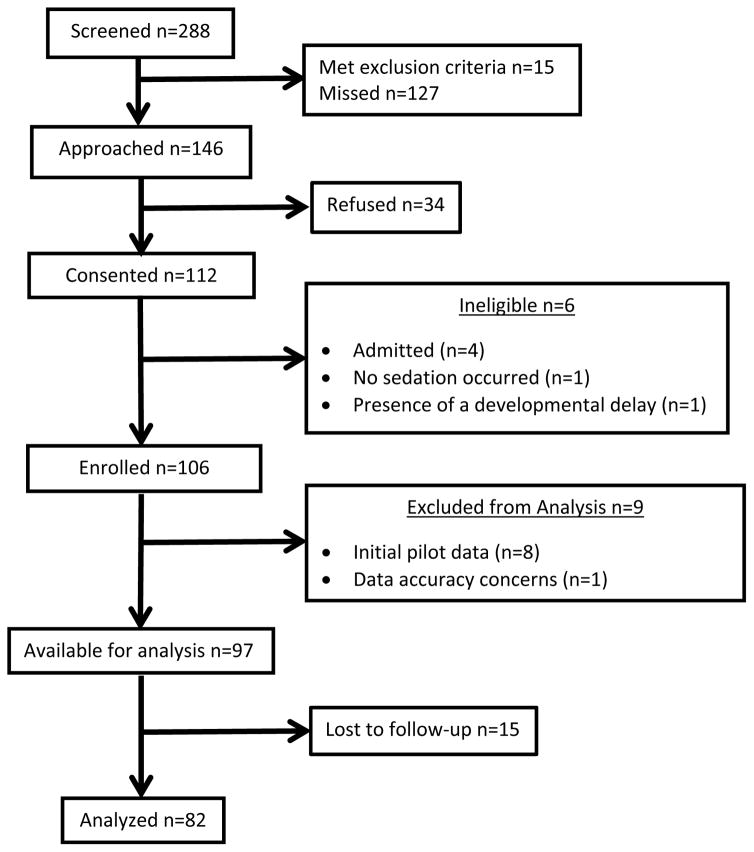
Two hundred eighty-eight children were eligible for inclusion in the study and 112 children consented (Figure 2: enrollment diagram). It was determined that 6 children were ineligible after consent was obtained as they met exclusion criteria. A total of 106 children were enrolled. Fifteen children did not complete the follow-up PHBQ either by phone or mail, leaving a total of 82 children (85%) who completed follow-up and were included in the final analysis.
Figure 2.
Flow diagram of study enrollment.
The majority of fractures were forearm fractures (89%). Ninety-three percent of children received analgesics for pain control prior to the procedure. The mean dose of ketamine was 1.73 mg/kg, standard deviation (SD) ±0.68 mg/kg. There were 2 adverse events (2.1%) reported which included one child with post-sedation emesis and one child with apnea for >30 seconds. This is comparable to our overall adverse event rate during ED sedations of 2.6%. Ninety-six percent of children received an opiate prescription for home. Demographics of the study population compared to those patients lost to follow-up are reported in Table 1. There were no significant differences in these characteristics between the group that was analyzed and the group that was lost to follow-up. The majority of children analyzed were greater than 5 years of age (66%), male (72%), white (72%), non-Hispanic (90%), and without any other medical conditions (85%). The majority of the sedations lasted greater than 30 minutes (84%) and only 9% received midazolam.
Table 1.
Demographics of analyzed patients and lost to follow-up patients.
| Analyzed n=82 (85%) |
Lost to follow-up n=15 (15%) |
p-value | |
|---|---|---|---|
|
| |||
| Age | |||
| >5 years | 54 (66) | 11 (73) | |
| ≤5 years | 28 (34) | 4 (27) | 0.57 |
|
| |||
| Gender | |||
| Female | 23 (28) | 6 (40) | |
| Male | 59 (72) | 9 (60) | 0.35 |
|
| |||
| Race | |||
| White | 59 (72) | 10 (67) | |
| Non-White | 21 (26) | 4 (27) | |
| Missing | 2 (2) | 1 (6) | 0.67 |
|
| |||
| Ethnicity | |||
| Non-Hispanic | 74 (90) | 11 (73) | |
| Hispanic | 8 (10) | 4 (27) | 0.07 |
|
| |||
| Medical conditions | |||
| No | 70 (85) | 12 (80) | |
| Yes | 12 (15) | 3 (20) | 0.60 |
|
| |||
| Anxiety | |||
| Low | 49 (60) | 8 (53) | |
| High | 33 (40) | 7 (47) | 0.64 |
|
| |||
| Sedation duration | |||
| >30 minutes | 69 (84) | 14 (93) | |
| ≤30 minutes | 13 (16) | 1 (7) | 0.35 |
|
| |||
| Midazolam given | |||
| No | 75 (91) | 14 (93) | |
| Yes | 7 (9) | 1 (7) | 0.81 |
Main Results
Overall, 18 (22%) children exhibited significant negative behavioral change after discharge following ED procedural sedation. The characteristics of children that experienced negative behavioral changes are shown in Table 2. The risk of negative behavioral changes is significantly higher for children with high anxiety and non-white race. The proportions of those patients with significant negative behavioral change who exhibited greater than 50% of potential changes in any given behavioral category is shown in Table 3. The most frequently seen behaviors were separation anxiety in 7 children (39%) and apathy/withdrawal in 8 children (44%). Overall, 33 (40%) children were observed to have high anxiety pre-sedation. Younger subjects were more likely to have high anxiety (73% vs. 26%, p<0.001).
Table 2.
Univariable analysis: Negative behavioral change after ED procedural sedation.
| Negative Behavioral Change n=18 (22%) |
No Behavioral Change N=64 (78%) |
OR (95% CI) | P-value | |
|---|---|---|---|---|
|
| ||||
| Age | ||||
| >5 years | 9 (50) | 45 (70) | Referent | |
| ≤5 years | 9 (50) | 19 (30) | 2.4 (0.8–6.9) | 0.11 |
|
| ||||
| Gender | ||||
| Female | 4 (22) | 19 (30) | Referent | |
| Male | 14 (78) | 45 (70) | 1.5 (0.4–5.1) | 0.54 |
|
| ||||
| Race* | ||||
| White | 8 (47) | 51 (81) | Referent | |
| Non-White | 9 (53) | 12 (19) | 4.8 (1.5–15.0) | 0.0072 |
|
| ||||
| Ethnicity | ||||
| Non-Hispanic | 17 (94) | 57 (89) | Referent | |
| Hispanic | 1 (6) | 7 (11) | 0.5 (0.06–4.2) | 0.51 |
|
| ||||
| Medical conditions | ||||
| No | 14 (78) | 56 (87) | Referent | |
| Yes | 4 (22) | 8 (13) | 2.0 (0.5–7.6) | 0.31 |
|
| ||||
| Anxiety | ||||
| Low | 5 (28) | 44 (69) | Referent | |
| High | 13 (72) | 20 (31) | 5.7 (1.8–18.2) | 0.0032 |
|
| ||||
| Sedation duration | ||||
| >30 minutes | 16 (89) | 53 (83) | Referent | 0.54 |
| ≤30 minutes | 2 (11) | 11 (17) | 0.6 (0.1–3.0) | |
|
| ||||
| Midazolam given | ||||
| No | 17 (94) | 58 (91) | Referent | |
| Yes | 1 (6) | 6 (9) | 0.6 (0.06–5.1) | 0.61 |
One patient in each group did not report race and were left out of the analysis in this category.
Table 3.
Proportion of patients with >50% of potential negative behavioral changes in each category of the PHBQ.
| PHBQ Behavioral Category | Greater than 50% of potential changes n=18 (%) |
|---|---|
| General Anxiety | 6 (33) |
| Separation Anxiety | 7 (39) |
| Sleep Anxiety | 4 (22) |
| Eating Disturbance | 6 (33) |
| Aggression Toward Authority | 6 (33) |
| Apathy/Withdrawal | 8 (44) |
Age, race, and anxiety all had p-values of <0.2 in the univariable analysis and were included in the multivariable analysis. Since age and anxiety were highly correlated and age was not significant, age was removed from the model. The final multivariable model which included race and anxiety (Table 4) identified highly anxious children to have 9.0 (95% CI 2.3–35.7) times the odds and children of non-white race to have 6.5 (95% CI 1.7–25.0) times the odds of negative behavioral change. Based on the Hosmer and Lemeshow Goodness-of-Fit Test, the predicted model is adequate (p=0.85).
Table 4.
Multivariable analysis: Negative behavioral change after ED procedural sedation.
| AOR* (95% CI) | p-value | |
|---|---|---|
|
| ||
| Anxiety | ||
| Low | 1.0 | 0.0018 |
| High | 9.0 (2.3–35.7) | |
|
| ||
| Race | ||
| White | 1.0 | 0.006 |
| Non-White | 6.5 (1.7–25.0) | |
adjusted odds ratio
Discussion
Overall 18 children who underwent fracture reduction with procedural sedation displayed a negative behavioral change 1–2 weeks after ED discharge. Risk factors associated with these negative changes were high anxiety and non-white race. The anesthesia literature describes a similar association between highly anxious patients and negative outcomes post-operating room.4,6,8–10 Prior difficult healthcare experiences, which is often considered a proxy for anxiety,5,7 has been shown in several studies to be associated with increased behavioral problems after post-operative discharge. While in the ED setting, pre-procedure agitation has been shown to have a moderate correlation with recovery agitation15, no study has investigated pre-procedural anxiety with behavioral changes post-discharge following procedural sedation. Additionally, this study found race to be associated with an increased odds of negative behavioral change after ED procedural sedation. This association has not previously been described in either the anesthesia or emergency medicine literature. The role of race in these behavioral changes is unknown. Several possible confounders not measured in this study that may be implicated in the relationship between race and behavioral change include socioeconomic status, family structure, prior healthcare experiences, at home pain scores and parental/caregiver anxiety. Future studies should take these variables into account to explore the effects of each on behavioral change.
Overall, 33 (40%) children undergoing intravenous ketamine sedation for fracture reduction in the ED were observed by the ED physician to be highly anxious pre-sedation. This is a large proportion of children which is realistic given the ED experience but has not been previously reported in the ED setting. Younger patients may be more likely to be categorized as highly anxious because it is more difficult to rationalize and explain procedural sedation to this age-group resulting in uncertainty and confusion that may lead to increased anxiety.
Given the prevalence of significant negative behavioral changes after ED sedation and the strong association that high anxiety prior to sedation had with these changes, a potential solution to mediate these changes is to treat children’s anxiety prior to the procedural sedation. Preoperative anxiolysis with midazolam6, 9, 16, 17 and clonidine18–20 have already been shown in the anesthesia literature to decrease the incidence of preoperative anxiety. Furthermore, Kain et al. have shown that anxiolysis with midazolam significantly decreases the incidence of negative behavioral changes after general anestheia.21 In the ED setting, pre-procedure midazolam has not been shown to decrease agitation/emergence phenomena in the immediate recovery period.15, 22 However, no studies in the ED setting have investigated the effect of treatment of pre-procedural anxiety on negative behavioral changes at home after procedural sedation. At our institution, the use of pre-sedation anxiolysis in conjunction with sedation is not routinely used with only 9% of children receiving midazolam.
In summary, for 82 children undergoing procedural sedation for fracture reduction in the ED setting 18 had negative behavioral changes 1–2 weeks after discharge. These experiences mirror the published findings in the anesthesia literature.5–7 Additionally, 33 of these ED patients were highly anxious. Highly anxious and non-white children have increased odds of negative behavioral changes which have not been previously recognized in the ED setting. The identification of factors associated with poor post-sedation behavioral outcomes is a first step toward the development of personalized patient care protocols in the ED setting which may result in improved patient outcomes.
Limitations
There are limitations to this study. A convenience sample was enrolled. Analysis of the children eligible and not enrolled and enrolled but not completing follow-up revealed no difference in patient characteristics, however we cannot be sure that those children who were not approached for enrollment do not differ from our study patients. Kannikeswaran et al. found in 2016 that anywhere from 7 to 19% of patients undergoing ED procedural sedation with intravenous ketamine have some recall of the painful procedure.23 We did not evaluate for patient recall in this study and so cannot be certain of this effect if any on our results. There are also multiple variables that could influence children’s behaviors: stress in the home environment, trauma of the initial accident, and stress from the ED visit itself, to name a few. While these factors may also influence the post-discharge negative outcomes, they are known to exist in the ED population and should be included in discussions about negative outcomes. Many of these factors are difficult to measure or control for but may be an important avenue for future research studies.
Footnotes
Prior Presentations: This work has been presented at the Pediatric Academic Societies Annual Meeting 2016 and Society for Academic Emergency Medicine Annual Meeting 2016.
Funding Sources/Disclosures: JP, AD, DB, KH, RH and KY report no conflicts of interest. This project was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number UL1TR001436. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
References
- 1.Fein JA, Zempsky WT, Cravero JP. Relief of pain and anxiety in pediatric patients in emergency medical systems. Pediatrics. 2012;13:1391–1405. doi: 10.1542/peds.2004-1752. [DOI] [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics, American Academy of Pediatric Dentistry. Cote CJ, Wilson S. Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures: An update. Pediatrics. 2006;118:2587–2602. doi: 10.1542/peds.2006-2780. [DOI] [PubMed] [Google Scholar]
- 3.Eckenhoff JE. Relationship of anesthesia to postoperative personality changes in children. Am J Dis Child. 1953;86:587–591. doi: 10.1001/archpedi.1953.02050080600004. [DOI] [PubMed] [Google Scholar]
- 4.Zavras N, Tsamoudaki S, Ntomi V, Yiannopoulos I, Christianakis E, Pikoulis E. Predictive factors of postoperative pain and postoperative anxiety in children undergoing elective circumcision: A prospective cohort study. Korean J Pain. 2015;28:244–253. doi: 10.3344/kjp.2015.28.4.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kotiniemi L, Ryhänen P, Moilanen I. Behavioural changes in children following day-case surgery: A 4-week follow-up of 551 children. Anaesthesia. 1997;52:970–976. doi: 10.1111/j.1365-2044.1997.202-az0337.x. [DOI] [PubMed] [Google Scholar]
- 6.Kain ZN, Mayes LC, O’Connor TZ, Cicchetti DV. Preoperative anxiety in children: Predictors and outcomes. Arch Pediatr Adolesc Med. 1996;150:1238–1245. doi: 10.1001/archpedi.1996.02170370016002. [DOI] [PubMed] [Google Scholar]
- 7.Stargatt R, Davidson AJ, Huang GH, Czarnecki C, Gibson MA, Stewart SA, et al. A cohort study of the incidence and risk factors for negative behavior changes in children after general anesthesia. Pediatr Anesth. 2006;16:846–859. doi: 10.1111/j.1460-9592.2006.01869.x. [DOI] [PubMed] [Google Scholar]
- 8.Beringer RM, Segar P, Pearson A, Greamspet M, Kilpatrick N. Observational study of perioperative behavior changes in children having teeth extracted under general anesthesia. Pediatr Anesth. 2014;24:499–504. doi: 10.1111/pan.12362. [DOI] [PubMed] [Google Scholar]
- 9.Kain ZN, Wang SM, Mayes LC, Caramico LA, Hofstadter MB. Distress during the induction of anesthesia and postoperative behavioral outcomes. Anesth Analg. 1999;88:1042–1047. doi: 10.1097/00000539-199905000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Kain ZN, Mayes LC, Caldwell-Andrews AA, Karas DE, McClain BC. Preoperative anxiety, postoperative pain, and behavioral recovery in young children undergoing surgery. Pediatrics. 2006;118:651–658. doi: 10.1542/peds.2005-2920. [DOI] [PubMed] [Google Scholar]
- 11.Brodzinski H, Iyer S. Behavior changes after minor emergency procedures. Pediatr Emerg Care. 2013;29:1098–1101. doi: 10.1097/PEC.0b013e3182a5ff07. [DOI] [PubMed] [Google Scholar]
- 12.Kain ZN, Mayes LC, Cicchetti DV, Bagnall AL, Finley JD, Hofstadter MB. The yale preoperative anxiety scale: How does it compare with a” gold standard”? Anesth Analg. 1997;85:783–788. doi: 10.1097/00000539-199710000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Kim JE, Jo BY, Oh HM, Choi HS, Lee Y. High anxiety, young age and long waits increase the need for preoperative sedatives in children. J Int Med Res. 2012;40:1381–1389. doi: 10.1177/147323001204000416. [DOI] [PubMed] [Google Scholar]
- 14.Vernon DT, Schulman JL, Foley JM. Changes in children’s behavior after hospitalization: Some dimensions of response and their correlates. Am J Dis Child. 1966;111:581–593. doi: 10.1001/archpedi.1966.02090090053003. [DOI] [PubMed] [Google Scholar]
- 15.Sherwin TS, Green SM, Khan A, Chapman DS, Dannenberg B. Does Adjunctive Midazolam Reduce Recovery Agitation After Ketamine Sedation for Pediatric Procedures? A Randomized, Double-Blind, Placebo-Controlled Trial. Ann Emerg Med. 2000;35:229–238. doi: 10.1016/s0196-0644(00)70073-4. [DOI] [PubMed] [Google Scholar]
- 16.Kain Z, Wang S, Mayes L, Caramico LA, Hofstadter MB. Parental presence during induction of anesthesia vs. sedative premedication: Which intervention is more effective? Anesthesiology. 1998;89:1147–1156. doi: 10.1097/00000542-199811000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Davis PJ, Tome JA, McGowan FX, Cohen IT, Latta K, Felder H. Preanesthetic medication with intranasal midazolam for brief pediatric surgical procedures effect on recovery and hospital discharge times. Anesthesiology. 1995;82:2–5. doi: 10.1097/00000542-199501000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Bergendahl H, Lönnqvist P, Eksborg S. Clonidine in paediatric anaesthesia: Review of the literature and comparison with benzodiazepines for premedication. Acta Anaesthesiol Scand. 2006;50:135–143. doi: 10.1111/j.1399-6576.2006.00940.x. [DOI] [PubMed] [Google Scholar]
- 19.Almenrader N, Passariello M, Coccetti B, Haiberger R, Pietropaoli P. Premedication in children: A comparison of oral midazolam and oral clonidine. Pediatr Anesth. 2007;17:1143–1149. doi: 10.1111/j.1460-9592.2007.02332.x. [DOI] [PubMed] [Google Scholar]
- 20.Cao J, Shi X, Miao X, Xu J. Effects of premedication of midazolam or clonidine on perioperative anxiety and pain in children. Biosci Trends. 2009;3:115–118. [PubMed] [Google Scholar]
- 21.Kain ZN, Mayes LC, Wang S, et al. Postoperative behavioral outcomes in children effects of sedative premedication. Anesthesiology. 1999;90:758–765. doi: 10.1097/00000542-199903000-00018. [DOI] [PubMed] [Google Scholar]
- 22.Wathen JE, Roback MG, Mackenzie T, Bothner JP. Does Midazolam Alter the Clinical Effects of Intravenous Ketamine Sedation in Children? A Double-Blind, Randomized, Controlled, Emergency Department Trial. Ann Emerg Med. 2000;26:579–588. doi: 10.1067/mem.2000.111131. [DOI] [PubMed] [Google Scholar]
- 23.Kannikeswaran N, Lieh-Lai M, Malian M, Wang B, Farooqi A, Roback MG. Optimal dosing of intravenous ketamine for procedural sedation in children in the ED—a randomized controlled trial. Am J Emerg Med. 2016;34:1347–1353. doi: 10.1016/j.ajem.2016.03.064. [DOI] [PubMed] [Google Scholar]