Abstract
Background
Much has been written about the impact of human immunodeficiency virus (HIV) among young (13–24) sexual minority men (SMM). Evidence for concern is substantial for emerging adult (18–24 years) SMM. Data documenting the burden and associated risk factors of HIV among adolescent SMM (<18 years) remain limited.
Methods
Adolescent SMM aged 13–18 years were recruited in 3 cities (Chicago, New York City, and Philadelphia) for interview and HIV testing. We used χ2 tests for percentages of binary variables and 1-way analysis of variance for means of continuous variables to assess differences by race/ethnicity in behaviors. We calculated estimated annual HIV incidence density (number of HIV infections per 100 person-years [PY] at risk). We computed Fisher’s exact tests to determine differences in HIV prevalence by selected characteristics.
Results
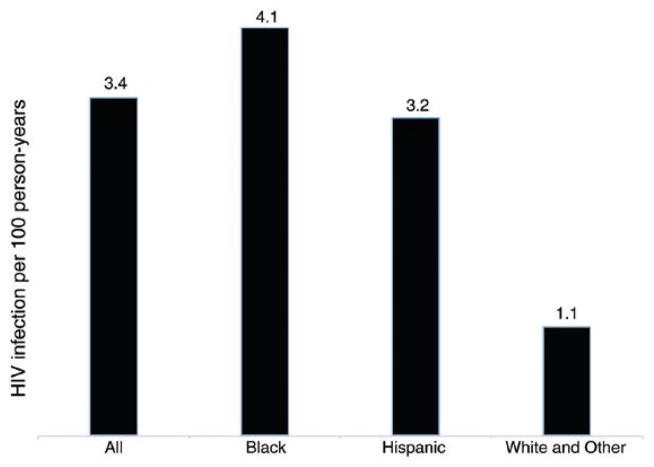
Of 415 sexually active adolescent SMM with a valid HIV test result, 25 (6%) had a positive test. Estimated annual HIV incidence density was 3.4/100 PY; incidence density was highest for blacks, followed by Hispanics, then whites (4.1, 3.2, and 1.1/100 PY, respectively). Factors associated with higher HIV prevalence included black race; ≥4 male partners, condomless anal sex, and exchange sex in the past 12 months; and a recent partner who was older, black, HIV-infected, or had ever been in jail or prison (P < .05).
Conclusions
HIV-related risk behaviors, prevalence, and estimated incidence density for adolescent SMM were high, especially for minority SMM. Our findings suggest that initiating intervention efforts early may be helpful in combating these trends.
Keywords: HIV incidence, HIV prevalence, HIV-related risk behaviors, adolescent sexual minority males
Young (13–24 years) sexual minority males (SMM)—those who identify as gay, bisexual, or who have sexual contact with persons of the same or both sexes—are disproportionally affected by human immunodeficiency virus (HIV) infection [1, 2]. The evidence for concern is substantial for the emerging adult segment of the young SMM population. In 2015, 81% of HIV diagnoses among young SMM were in those aged 20–24 years, and among all diagnoses of HIV among SMM, 22% were in this age group. The risk of HIV was even more notable for minority SMM [3]. There are also concerns about high HIV incidence among emerging adult SMM [4, 5]. In terms of the driving forces behind these statistics, there is a growing consensus that individual-level risk behaviors cannot adequately explain the HIV-related racial disparities observed. Rather, relationship and partner-level factors as well as sociocultural and structural determinants of health, including community, political, educational, and economic factors are now understood to play a key role in HIV risk [6–9].
In contrast to what is known about emerging adult SMM, the data documenting the burden and associated risk factors of HIV among adolescent SMM remain extremely limited. The numbers and rates of diagnoses of HIV infection in this group are small. Among all HIV diagnoses attributed to male-to-male sex, just 5% were among those aged 13–19 years [3]. However, the timing of infection relative to diagnosis is often unclear; if asymptomatic, many individuals are not diagnosed until years after they are infected. The high prevalence of diagnoses of HIV infection among SMM aged 20–24 years suggests that at least some of these infections occurred during adolescence [10].
Although estimates of HIV incidence are an essential element for monitoring the epidemic, very few studies to date have included adolescent SMM. A notable exception comes from Garofalo et al [11], who conducted a longitudinal study of HIV risk among 450 SMM (aged 16–20 years at baseline) in Chicago. HIV incidence was 5.2/100 PY for participants aged 16–17 years and 3.8/100 PY for those aged 18–20 years. In addition, a study of SMM attending New York City sexually transmitted disease clinics reported that HIV incidence was actually higher among males aged <20 years (5.7/100 PY) compared with other age groups [12]. In both studies, incidence was higher among minorities [11, 12].
The characteristics and behaviors associated with HIV risk and acquisition also remain largely unexplored for adolescent SMM. Research indicates that prevalence of risky sexual behavior is high [11, 13] and that this population is particularly vulnerable to risk associated with partner selection, partner characteristics, and other sociocultural and structural determinants [11, 13–15]. The 2015 National Youth Risk Behavior Survey highlighted the disparity in HIV-related risk behaviors among sexual minority students (grades 9–12) compared to heterosexual students. Among male students, the prevalence of having had sexual intercourse before age 13 years was higher and condom use at last sex was lower among those who had sexual contact with males than among those who had sexual contact with only females. Also, SMM students were more likely to have ever injected any illegal drug than their heterosexual counterparts [16].
Research with adolescent SMM is imperative to fully understand and address the HIV epidemic among SMM as a whole. It is insufficient to infer results of studies of older SMM to adolescent SMM [17–20]. In light of the shortage of research among adolescent SMM relative to other SMM, in 2015, the Centers for Disease Control and Prevention (CDC) conducted an HIV behavioral surveillance project, the National HIV Behavioral Surveillance for Young Men Who Have Sex with Men (NHBSYMSM), to ascertain the prevalence of risk behaviors and HIV infection among this population. In this paper, we describe the sociodemographic characteristics of the sample, examine racial-ethnic variations in sexual partnerships and HIV-related risk behaviors, and provide estimates of HIV incidence and HIV prevalence among this group of adolescent SMM.
METHODS
Three cities implemented NHBS-YMSM: Chicago, New York City, and Philadelphia. Participants were eligible to enroll in the study if they met the following criteria: (1) between the ages of 13 and 18 years; (2) birth sex male and currently living as a male; (3) a resident of the Metropolitan Statistical Area; (4) able to complete the survey in English or Spanish; (5) reported any sexual contact with another male or self-identified as gay or bisexual or indicated same-sex attraction.
One of the original objectives of the NHBS-YMSM was to determine the most effective and feasible sampling method(s) to reach adolescent SMM. Therefore, 3 sampling methods were used to recruit participants into the project: venue-based sampling in New York City only, respondent-driven sampling in all 3 participating cities, and Facebook sampling in Philadelphia and Chicago. Venue-based sampling is a sampling strategy that utilizes venues (eg, clubs, organizations, street locations) within the project area to obtain the desired sample [21]. Respondent-driven sampling is a chain recruitment method that begins with a set of “seeds” who recruit members of their social networks to participate in project activities, who in turn recruit other members of their social networks [22, 23]. Facebook sampling employs targeted banner ads to identify and recruit adolescent SMM into the study.
Regardless of the sampling method, all NHBS-YMSM consenting participants underwent an in-person eligibility screening and, if eligible, completed the behavioral assessment with a trained interviewer. Anonymous HIV testing was offered to all participants regardless of self-reported HIV infection status. HIV testing was performed on blood specimens with rapid or laboratory-based testing and confirmed with Western blot or immunofluorescence. A nonreactive rapid test was considered a definitive negative result; a reactive (preliminary positive) rapid test result was considered a definitive positive result only when confirmed by supplemental laboratory testing (eg, Western blot or immunofluorescence assay). HIV-infected participants were assisted by project staff members for linkage to medical care and other supportive services.
Individuals were compensated for their participation in project activities, receiving approximately $25 for the behavioral assessment and $25 for HIV testing. NHBS-YMSM activities were approved by local institutional review boards in each participating city and approved by CDC. A waiver of documentation of informed consent was requested and received for all 3 locations. In addition, a waiver of parental permission for participants <18 years of age was requested and received in New York City (approved for 13–17 years of age), Philadelphia (approved for 14–17 years of age), and Chicago (approved for 16 and 17 years of age). The age categories included in the waiver of parental permission were determined by the local institutional review boards.
Data Analysis and Measures
Data were analyzed in aggregate as a convenience sample. Participants were included in this analysis if they had a completed, valid survey and reported ever having vaginal or anal sex with male or female partners (ie, sexually active). First, we described sociodemographic characteristics of adolescent SMM and examined racial-ethnic variations in sexual partnerships and HIV-related risk behaviors. During the NHBS-YMSM survey, participants were asked about characteristics of partnerships and behaviors that occurred over several time periods: ever in their life, during the past 12 months, and during the past 3 months. Participants were also asked about their 3 most recent sex partners in the past 3 months. If a participant had not had sex with anyone in the past 3 months, he was asked about the last person he had sex with in the past 12 months. For the current analysis, we utilized the information about the most recent sex partners to examine whether a participant had at least 1 sexual partnership (among 3 possible partnerships) with the characteristic or behavior of interest. Financial instability was assessed with the question, “was there a time when there was not enough money in your house for rent, food, or utilities such as gas, electric, or phone?” Exchange sex was defined as exchanging sex for something such as money or drugs. Partner concurrency was defined as the respondent or their partner probably or definitely having sex with other people during the time of a sexual relationship. We computed percentages for binary variables and means, standard errors, and ranges for continuous variables. We determined the statistically significant differences (P < .05) between the racial/ethnic groups using χ2 test for percentages of binary variables and 1-way analysis of variance for means of continuous variables.
Next, we derived estimates of annual HIV incidence density [4, 24], among participants who reported ever having anal sex with a male partner and had a valid NHBS-YMSM positive or negative NHBS-YMSM HIV test result (n = 371), by including the number who tested positive for HIV infection as the numerator and the total number of person-years at risk as the denominator. Person-years at risk was calculated by subtracting age at first anal sex with a male from first positive HIV test (for persons who reported having previously been diagnosed with HIV infection) or current age minus age at first anal sex with a male (for all others). About 20% of sexually active adolescent SMM who reported anal sex with a male were missing the age at first anal sex. Multiple imputation based on age, race, and ethnicity was used to impute the missing age at first anal sex for these participants. Using this method, we calculated estimated annual incidence density for the entire group, as well as by racial/ethnic group (black, Hispanic, white/other; note that participants of white and other races were grouped together). Finally, we present HIV prevalence overall and by selected characteristics among the adolescent SMM who had a valid positive or negative NHBS-YMSM HIV test result. We computed Fisher’s exact tests to determine statistically significant differences (P < .05).
RESULTS
The NHBS-YMSM total sample consisted of 569 participants with valid and complete interviews; of these, 453 (80%) reported being sexually active. Among sexually active participants, mean age was 16.7 years, 42% identified as black, 38% as Hispanic, and 16% as white, and 4% reported other or multiple race groups. Almost half (45%) grew up in a 2-parent household. Of the sample, 26% reported household financial instability during the past 12 months and 30% reported ever being kicked out of the house or running away. The majority of the adolescent men identified as gay (64%) or bisexual (33%). More than half (60%) had ever been tested for HIV and 54% had done so in the past 12 months. Ninety percent reported visiting a healthcare provider in the past 12 months (Table 1).
Table 1.
Selected Characteristics of Sexually Activea Adolescent Sexual Minority Males, National Human Immunodeficiency Virus Behavioral Surveillance for Young Men Who Have Sex with Men, 2015
| Characteristic | No. (N = 453) | % |
|---|---|---|
| Age, y | ||
| 13–15 | 44 | 10 |
| 16–17 | 267 | 59 |
| 18 | 142 | 31 |
| Race/ethnicity | ||
| Black | 188 | 42 |
| Hispanic | 174 | 38 |
| White | 71 | 16 |
| Otherb | 19 | 4 |
| Family structurec | ||
| 2 parents | 204 | 45 |
| Single parent | 194 | 43 |
| Other relatives | 41 | 9 |
| Other living situation | 14 | 3 |
| Household financial instabilityd, past 12 mo | ||
| No | 335 | 74 |
| Yes | 116 | 26 |
| Ever kicked out of the house or run away | ||
| No | 319 | 70 |
| Yes | 134 | 30 |
| Sexual identity | ||
| Gay | 287 | 64 |
| Bisexual | 148 | 33 |
| Heterosexual | 13 | 3 |
| Binge drinkinge, past 30 d | ||
| No | 319 | 71 |
| Yes | 133 | 29 |
| Marijuana use, past 12 mo | ||
| No | 213 | 47 |
| Yes | 240 | 53 |
| Stimulant usef, past 12 mo | ||
| No | 387 | 85 |
| Yes | 66 | 15 |
| Ever injection drug use | ||
| No | 450 | 99 |
| Yes | 3 | 1 |
| Health insurance | ||
| No | 25 | 6 |
| Yes | 421 | 94 |
| Visited healthcare provider, past 12 mo | ||
| No | 45 | 10 |
| Yes | 408 | 90 |
| Ever had oral sex with a male partner | ||
| No | 29 | 6 |
| Yes | 424 | 94 |
| Ever tested for HIV | ||
| No | 182 | 40 |
| Yes | 270 | 60 |
| Tested for HIV, past 12 mo | ||
| No | 208 | 46 |
| Yes | 243 | 54 |
| City | ||
| Chicago | 190 | 42 |
| New York City | 176 | 39 |
| Philadelphia | 87 | 19 |
| Recruitment methodg | ||
| Venue-based sampling | 130 | 29 |
| Respondent-driven sampling | 241 | 53 |
| Facebook sampling | 82 | 18 |
| Total | 453 | 100 |
Numbers might not add to total because of missing data. Abbreviation: HIV, human immunodeficiency virus.
Participants who ever had anal or vaginal sex.
Includes persons who indicated American Indian/Alaska Native, Asian, Native Hawaiian/Pacific Islander, or other race.
Family structure for most of respondent’s childhood. Two parents could be biological, adoptive, or a stepparent and biological/adoptive parent; single parent could be biological or adoptive; other living situation could include foster parent(s), another adult only, such as a stepparent, or other living situation such as a group home.
In the past 12 months, was there a time where there was not enough money in your house for rent, food, or utilities such as gas, electric, or phone?
Five or more alcoholic drinks in 1 sitting.
Cocaine, ecstasy, poppers (amyl nitrate), or methamphetamine.
Venue-based sampling was conducted in New York City; respondent-driven sampling was conducted in Chicago, New York City, and Philadelphia; and Facebook sampling was conducted in Chicago and Philadelphia.
The mean age of first anal sex with a male was 15 years and 82% had ever had anal sex with a male partner. In the past 12 months, 51% reported condomless anal sex with a male and 38% had ≥4 oral or anal male sex partners. Black adolescent SMM were more likely than white/other adolescent SMM to have ever had anal sex with a male partner (86% vs 74%), to have engaged in exchange sex in the past 12 months (7% vs 1%), to report sexual concurrency within a recent relationship (55% vs 40%), and to have a lower mean age of first vaginal or anal sex with a female partner (13.6 years vs 15.1 years) and less likely to report alcohol or drugs before or during last sex (23% vs 34%). Black adolescent SMM were more likely than Hispanic adolescent men to have an older partner (73% vs 60%). Black adolescent SMM were more likely than Hispanic and white/other adolescent SMM to have a black partner (76% vs 25% and 11%, respectively), and had a lower mean age of first oral sex with a male partner (14.0 years vs 14.6 years and 15.2 years, respectively). Both black adolescent SMM and Hispanic adolescent SMM were more likely than white/other SMM to have a partner who had ever been in prison or jail (20% and 16% vs 6%, respectively), whereas black and Hispanic SMM were less likely than white adolescent SMM to report sex within 1 week of meeting a new partner (24% and 19% vs 42%, respectively). Black adolescent SMM and Hispanic adolescent SMM had a lower mean age of first anal sex with a male partner (14.6 years and 15.0 years) compared with white/other adolescent SMM (15.9 years) (Tables 2 and 3).
Table 2.
Sexual Partnerships and Human Immunodeficiency Virus (HIV)–Related Risk Behaviors Among Sexually Activea Adolescent Sexual Minority Males, by Race/Ethnicity, National HIV Behavioral Surveillance for Young Men Who Have Sex With Men, 2015
| Characteristic | Total | Black | Hispanic | White/Otherb | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| (N = 453) | (n = 188) | (n = 174) | (n = 91) | |||||
|
|
|
|
|
|||||
| No. | % | No. | % | No. | % | No. | % | |
| Ever had vaginal or anal sex with a female partner | ||||||||
|
| ||||||||
| No | 285 | 63 | 114 | 61 | 108 | 62 | 63 | 70 |
|
| ||||||||
| Yes | 168 | 37 | 74 | 39 | 66 | 38 | 27 | 30 |
|
| ||||||||
| Ever had anal sex with a male partner | ||||||||
|
| ||||||||
| No | 82 | 18 | 26 | 14 | 33 | 19 | 23 | 26 |
|
| ||||||||
| Yes | 371 | 82 | 162 | 86c | 141 | 81 | 67 | 74c |
|
| ||||||||
| Condomless anal sex with a male partner, past 12 mo | ||||||||
|
| ||||||||
| No | 222 | 49 | 94 | 50 | 80 | 46 | 48 | 53 |
|
| ||||||||
| Yes | 231 | 51 | 94 | 50 | 94 | 54 | 42 | 47 |
|
| ||||||||
| ≥4 male partnersd, past 12 mo | ||||||||
|
| ||||||||
| No | 283 | 62 | 117 | 62 | 109 | 63 | 57 | 63 |
|
| ||||||||
| Yes | 170 | 38 | 71 | 38 | 65 | 37 | 34 | 37 |
|
| ||||||||
| Exchange sexe, past 12 mo | ||||||||
|
| ||||||||
| No | 434 | 96 | 175 | 93 | 169 | 97 | 89 | 99 |
|
| ||||||||
| Yes | 19 | 4 | 13 | 7c | 5 | 3 | 1 | 1c |
|
| ||||||||
| Exclusive receptive anal sex with male partners, past 3 mo | ||||||||
|
| ||||||||
| No | 274 | 67 | 105 | 62 | 111 | 71 | 57 | 70 |
|
| ||||||||
| Yes | 135 | 33 | 64 | 38 | 46 | 29 | 25 | 31 |
|
| ||||||||
| 3 most recent partnersf | ||||||||
|
| ||||||||
| Older partnerg | ||||||||
|
| ||||||||
| No | 121 | 33 | 35 | 27 | 63 | 40 | 23 | 30 |
|
| ||||||||
| Yes | 247 | 67 | 95 | 73h | 96 | 60h | 55 | 71 |
|
| ||||||||
| Black partner | ||||||||
|
| ||||||||
| No | 254 | 56 | 45 | 24 | 130 | 75 | 79 | 89 |
|
| ||||||||
| Yes | 197 | 44 | 143 | 76c,h | 43 | 25h | 10 | 11c |
|
| ||||||||
| HIV-infected partner | ||||||||
|
| ||||||||
| No | 440 | 97 | 180 | 96 | 170 | 98 | 89 | 99 |
|
| ||||||||
| Yes | 13 | 3 | 8 | 4 | 4 | 2 | 1 | 1 |
|
| ||||||||
| Partner of unknown HIV status | ||||||||
|
| ||||||||
| No | 286 | 63 | 122 | 65 | 114 | 66 | 49 | 54 |
|
| ||||||||
| Yes | 167 | 37 | 66 | 35 | 60 | 35 | 41 | 46 |
|
| ||||||||
| Met partner onlinei | ||||||||
|
| ||||||||
| No | 280 | 62 | 120 | 64 | 105 | 60 | 55 | 62 |
|
| ||||||||
| Yes | 172 | 38 | 68 | 36 | 69 | 40 | 34 | 38 |
|
| ||||||||
| Sexual concurrencyj | ||||||||
|
| ||||||||
| No | 227 | 50 | 85 | 45 | 88 | 51 | 54 | 60 |
|
| ||||||||
| Yes | 226 | 50 | 103 | 55c | 86 | 49 | 36 | 40c |
|
| ||||||||
| Partner ever injected drugs | ||||||||
|
| ||||||||
| No | 416 | 92 | 172 | 92 | 159 | 91 | 84 | 93 |
|
| ||||||||
| Yes | 37 | 8 | 16 | 9 | 15 | 9 | 6 | 7 |
|
| ||||||||
| Alcohol or drugs before or during last sex | ||||||||
|
| ||||||||
| No | 336 | 74 | 145 | 77 | 131 | 75 | 59 | 66 |
|
| ||||||||
| Yes | 117 | 26 | 43 | 23c | 43 | 25 | 31 | 34c |
|
| ||||||||
| Partner ever in jail or prison | ||||||||
|
| ||||||||
| No | 382 | 84 | 150 | 80 | 146 | 84 | 85 | 94 |
|
| ||||||||
| Yes | 71 | 16 | 38 | 20c | 28 | 16k | 5 | 6c,k |
|
| ||||||||
| Serious partnerl | ||||||||
|
| ||||||||
| No | 186 | 41 | 77 | 41 | 65 | 37 | 43 | 48 |
|
| ||||||||
| Yes | 267 | 59 | 111 | 59 | 109 | 63 | 47 | 52 |
|
| ||||||||
| Sex within a week of meeting | ||||||||
|
| ||||||||
| No | 336 | 74 | 142 | 76 | 141 | 81 | 52 | 58 |
|
| ||||||||
| Yes | 117 | 26 | 46 | 24c | 33 | 19k | 38 | 42c,k |
Numbers might not add to total because of missing data. Abbreviation: HIV, human immunodeficiency virus.
Participants who ever had anal or vaginal sex.
Includes persons who indicated American Indian/Alaska Native, Asian, Native Hawaiian/Pacific Islander, multiple races, or other race.
Indicates significantly different values (P < .05) between black non-Hispanic and white non-Hispanic/other participants.
Had oral or anal sex.
Had sex in exchange for something such as money or drugs.
Participants were asked about their 3 most recent sex partners in the past 3 months. If the participant did not have sex with anyone in the past 3 months, they were asked about the last person he had sex with in the past 12 months. The “yes” category indicates that a participant had at least 1 sexual partnership (among a possible 3 partnerships) with the characteristic or behavior of interest.
Due to mandated reporting requirements, Philadelphia did not ask about partner’s age. Chicago and New York City asked whether the partner was younger, older, or the same age as the participant.
Indicates significantly different values (P < .05) between black non-Hispanic and Hispanic participants.
Met partner on the internet or through a mobile app (eg, Grindr, Jack’d, Scruff).
During the time of a sexual relationship, the participant was having sex with other people and/or the partner was probably or definitely having sex with other people.
Indicates significantly different values (P < .05) between Hispanic and white non-Hispanic/other participants.
A male with whom the participant has dated for a while and feels close to and may call a boyfriend or partner.
Table 3.
Sexual Partnerships and Human Immunodeficiency Virus (HIV)-Related Risk Behaviors Among Sexually Activea Adolescent Sexual Minority Males, by Race/Ethnicity, National HIV Behavioral Surveillance for Young Men Who Have Sex with Men, 2015
| Characteristic | Total | Black | Hispanic | White/Otherb | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||||||||
| (N = 453) | (n = 188) | (n = 174) | (n = 91) | |||||||||||||
|
|
|
|
|
|||||||||||||
| No. | Mean | (Range) | SD | No. | Mean | (Range) | SD | No. | Mean | (Range) | SD | No. | Mean | (Range) | SD | |
| Age at first oral sex with a male partner | 343 | 14.5 | (4–18) | 2.3 | 123 | 14.0c,d | (4–18) | 2.6 | 147 | 14.6d | (4–18) | 2.0 | 73 | 15.2c | (8–18) | 2.1 |
|
| ||||||||||||||||
| Age at first vaginal or anal sex with a female partner | 139 | 14.1 | (6–18) | 2.1 | 56 | 13.6c | (6–18) | 2.5 | 58 | 14.3 | (10–18) | 1.7 | 25 | 15.1c | (12–18) | 1.5 |
|
| ||||||||||||||||
| Age at first anal sex with a male partner | 298 | 15.0 | (6–18) | 2.1 | 111 | 14.6c | (6–18) | 2.4 | 127 | 15.0e | (6–18) | 2.0 | 60 | 15.9e | (12–18) | 1.5 |
|
| ||||||||||||||||
| No. of male anal sex partners, past 12 mo | 452 | 3.8 | (0–250) | 12.7 | 187 | 3.9 | (0–40) | 5.8 | 174 | 3.7 | (0–250) | 19.0 | 91 | 3.7 | (0–37) | 6.4 |
|
| ||||||||||||||||
| No. of condomless male anal sex partners, past 12 mo | 452 | 1.2 | (0–22) | 2.4 | 187 | 1.4 | (0–22) | 2.7 | 174 | 1.1 | (0–12) | 1.8 | 91 | 1.3 | (0–17) | 2.6 |
|
| ||||||||||||||||
| No. of anal sex acts, past 3 mo | 371 | 7.3 | (0–205) | 17.2 | 151 | 7.3 | (0–205) | 20.4 | 142 | 7.8 | (0–120) | 16.7 | 78 | 6.4 | (0–46) | 10.2 |
|
| ||||||||||||||||
| No. of condomless sex acts, past 3 mo | 304 | 7.7 | (0–145) | 16.8 | 125 | 7.0 | (0–145) | 18 | 119 | 8.4 | (0–120) | 17.8 | 60 | 7.9 | (0–60) | 11.4 |
Numbers might not add to total because of missing data. Abbreviation: SD, standard deviation.
Participants who ever had anal or vaginal sex.
Includes persons who indicated American Indian/Alaska Native, Asian, Native Hawaiian/Pacific Islander, multiple races, or other race.
Indicates significantly different values (P < .05) between black non-Hispanic and white non-Hispanic/other participants.
Indicates significantly different values (P < .05) between black non-Hispanic and Hispanic participants.
Indicates significantly different values (P < .05) between Hispanic and white non-Hispanic/other participants.
Overall, the estimated annual HIV incidence density was 3.4/100 PY. Incidence was 4.1/100 PY for blacks, 3.2/100 PY for Hispanics, and 1.1/100 PY for white/other (Figure 1). Table 4 examines characteristics associated with being HIV infected among 415 adolescent SMM who had a valid positive or negative NHBS-YMSM HIV test result. Of these, 25 (6%) were HIV infected. HIV prevalence was higher among black than white/other SMM (9% vs 1%) and among participants from Philadelphia as compared with Chicago (12% vs 4%). HIV prevalence was higher among adolescent SMM who reported ≥4 male partners (14% vs 4%), condomless anal sex with a male partner (10% vs 2%), and exchange sex (32% vs 5%) in the past 12 months compared to those who did not. Examining recent sexual partnerships, HIV prevalence was higher among adolescents who had at least 1 older partner (6% vs 1%), black partner (10% vs 3%), HIV-infected partner (25% vs 5%), and a partner who had ever been in jail or prison (15% vs 4%). Also HIV prevalence was higher among those who had sex within a week of meeting their sex partner (11% vs 4%).
Figure 1.
Estimated human immunodeficiency virus (HIV) incidence density among adolescent sexual minority males, National HIV Behavioral Surveillance for Young Men Who Have Sex with Men (NHBS-YMSM), 2015. Analyses among participants who reported ever having anal sex with a male partner and had a valid positive or negative, NHBS-YMSM test result. Other race includes persons who indicated American Indian/Alaska Native, Asian, Native Hawaiian/Pacific Islander, multiple races, or other race. Estimated HIV incidence density was 3.4 per person-years (PY) at risk (24 HIV infections among 702 PY), 4.1/100 PY among black (15 infections among 367 PY), 3.2/100 PY among Hispanic (8 HIV infections among 247 PY), and 1.1/100 PY among white and other adolescent males (1 HIV infection among 87 PY). Abbreviation: HIV, human immunodeficiency virus.
Table 4.
Human Immunodeficiency Virus (HIV) Infectiona Among Sexually Activeb Adolescent Sexual Minority Males, by Selected Characteristics, National HIV Behavioral Surveillance for Young Men Who Have Sex with Men, 2015
| Characteristic | Total No. (n = 415) | HIV-Infected | ||
|---|---|---|---|---|
| No. | % | P Value | ||
| Age, y | ||||
| 13–15 | 37 | 2 | 5 | .9 |
| 16–17 | 245 | 14 | 6 | |
| 18 | 133 | 9 | 7 | |
| Race/ethnicity | ||||
| Black | 172 | 15 | 9 | .05c |
| Hispanic | 160 | 9 | 6 | |
| White/otherd | 82 | 1 | 1 | |
| Household financial instabilitye, past 12 mo | ||||
| No | 307 | 17 | 6 | .48 |
| Yes | 106 | 8 | 8 | |
| City | ||||
| Chicago | 187 | 8 | 4 | .06f |
| New York City | 143 | 7 | 5 | |
| Philadelphia | 85 | 10 | 12 | |
| Sexual identity | ||||
| Gay or bisexual | 399 | 24 | 6 | .3 |
| Heterosexual | 11 | 1 | 9 | |
| Anal sex before age 13 y | ||||
| No | 167 | 12 | 7 | .41 |
| Yes | 248 | 13 | 5 | |
| ≥4 male partnersg, past 12 mo | ||||
| No | 291 | 13 | 4 | .01 |
| Yes | 81 | 11 | 14 | |
| Condomless anal sex with a male partner, past 12 mo | ||||
| No | 173 | 4 | 2 | .003 |
| Yes | 218 | 21 | 10 | |
| Exchange sexh, past 12 mo | ||||
| No | 396 | 19 | 5 | <.0001 |
| Yes | 19 | 6 | 32 | |
| 3 most recent partnersi | ||||
| Female partner | ||||
| No | 367 | 23 | 6 | .75 |
| Yes | 48 | 2 | 4 | |
| Older partnerj | ||||
| No | 105 | 1 | 1 | .04 |
| Yes | 227 | 14 | 6 | |
| Black partner | ||||
| No | 227 | 7 | 3 | .01 |
| Yes | 186 | 18 | 10 | |
| HIV-infected partner | ||||
| No | 403 | 22 | 5 | .03 |
| Yes | 12 | 3 | 25 | |
| Partner of unknown HIV status | ||||
| No | 260 | 17 | 7 | .67 |
| Yes | 155 | 8 | 5 | |
| Met partner onlinek | ||||
| No | 250 | 11 | 4 | .09 |
| Yes | 164 | 14 | 9 | |
| Sexual concurrencyl | ||||
| No | 200 | 8 | 4 | .1 |
| Yes | 215 | 17 | 8 | |
| No | 382 | 21 | 5 | .13 |
| Yes | 33 | 4 | 12 | |
| Alcohol or drugs before or during last sex | ||||
| No | 307 | 14 | 5 | .06 |
| Yes | 108 | 11 | 10 | |
| Partner ever in jail or prison | ||||
| No | 348 | 15 | 4 | .003 |
| Yes | 67 | 10 | 15 | |
| Serious partnerm | ||||
| No | 166 | 9 | 5 | .83 |
| Yes | 249 | 16 | 6 | |
| Sex within a week of meeting | ||||
| No | 301 | 12 | 4 | .01 |
| Yes | 114 | 13 | 11 | |
Numbers might not add to total because of missing data. Abbreviation: HIV, human immunodeficiency virus.
Participants who had a valid positive or negative National HIV Behavioral Surveillance for Young Men Who Have Sex with Men test result are included in this analysis.
Participants who ever had anal or vaginal sex.
Indicates significantly different values (P < .05) between black non-Hispanic and white non-Hispanic/other participants.
Includes persons who indicated American Indian/Alaska Native, Asian, Native Hawaiian/Pacific Islander, multiple races, or other race.
In the past 12 months, was there a time where there was not enough money in your house for rent, food, or utilities such as gas, electric, or phone?
Indicates significantly different values (P < .05) between Chicago and Philadelphia.
Had oral or anal sex.
Had sex in exchange for something such as money or drugs.
Participants were asked about their 3 most recent sex partners in the past 3 months. If the participant did not have sex with anyone in the past 3 months, they were asked about the last person he had sex with in the past 12 months. The “yes” category indicates that a participant had at least 1 sexual partnership (among a possible 3 partnerships) with the characteristic or behavior of interest.
Due to mandated reporting requirements, Philadelphia did not ask about partner’s age. Chicago and New York City asked whether the partner was young, older, or the same age as the participant.
Met partner on the internet or through a mobile app (eg, Grindr, Jack’d, Scruff).
During the time of a sexual relationship, the participant was having sex with other people and/or the partner was probably or definitely having sex with other people.
A male with whom the participant has dated for a while and feels close to and may call a boyfriend or partner.
DISCUSSION
Overall, HIV prevalence and estimated incidence density for adolescent SMM in this study were high, driven primarily by the rates for black and Hispanic participants. Both individual behavior and partner characteristics were associated with being HIV infected. Similar to previous research [11, 14, 16], reported prevalence of several key HIV-related risk behaviors, including condomless anal sex with a male partner in the past 12 months, ≥4 oral or anal male sex partners in the past 12 months, and sexual concurrency with at least 1 recent partner, was high across all racial/ethnic groups in our sample.
We did find some racial/ethnic differences in HIV-related risk behaviors. Black adolescent SMM reported an earlier age of sexual debut, which provides an extended window of risk opportunity and could be a possible contributing factor in the disproportionate HIV rates by race/ethnicity [25, 26]. Black adolescent SMM were also more likely than their white/other adolescent SMM counterparts to have ever had anal sex with a male partner, have engaged in exchange sex in the past 12 months, and report sexual concurrency within a recent relationship. Consistent with previous literature [5, 27, 28], we also found differences in sexual partner characteristics and sexual network factors by race/ethnicity. In particular, black adolescent SMM were more likely than the other groups to have a black partner. Previous studies have proposed that the background prevalence rates in the population paired with racially homogenous sexual networks is a contributing factor to why HIV rates are disproportionately high among black SMM [8, 28, 29]. White/other adolescent SMM were more likely than black adolescent SMM to report alcohol or drugs before or during last sex and were more likely than both black and Hispanic SMM to report sex within 1 week of meeting a new partner. Although these behaviors place white/other adolescent SMM at risk for HIV and other sexually transmitted infections, the lower HIV prevalence in their partner pool may lower the impact of these risks for HIV acquisition.
This study has several limitations. First, the study is a convenience sample and the analyses do not account for the sampling design. Participants may not be representative of all SMM 13–18 years of age, and data are not weighted. Second, data were self-reported and may have associated biases. Third in the calculation of PY at risk for incidence density, we used age at diagnosis to approximate age at HIV infection, which likely inflates the denominator by increasing the estimate of years at risk. However, as this is a young population, we expect the amount of inflation to be small. On the other hand, only participants who reported ever having anal sex with a male partner were included for calculating PY at risk; if this behavior was misreported, we could have underestimated the denominator.
The findings from this study, including the early onset of sexual activity, high rates of HIV-related risk behavior, and elevated HIV prevalence and estimated incidence density, suggest that effective HIV prevention strategies, including “test and treat” and preexposure prophylaxis (PrEP), may be helpful in reducing HIV risk among adolescent SMM. Unfortunately, there is currently a dearth of HIV prevention interventions that focus on this population specifically, and to date, PrEP is not approved for use below the age of 18 [11, 30]. Therefore, it is imperative that future HIV prevention research examine interventions that not only include adolescent SMM but do so in a way that encompasses the developmental needs of the adolescent life stage [31–33].
Acknowledgments
This work is written by (a) US Government employee(s) and is in the public domain in the US. DOI: 10.1093/cid/cix902
We thank the young men who participated in this project.
Footnotes
Disclaimer. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC).
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Financial support. This study was funded through cooperative agreements from the CDC and through contracts from the Chicago Department of Public Health and from the Philadelphia Department of Public Health.
References
- 1.Johnson AS, Hall HI, Hu X, Lansky A, Holtgrave DR, Mermin J. Trends in diagnoses of HIV infection in the United States, 2002–2011. JAMA. 2014;312:432–4. doi: 10.1001/jama.2014.8534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. [Accessed 3 November 2017];HIV surveillance—men who have sex with men (MSM) through 2015. Available at: https://www.cdc.gov/hiv/library/slideSets/index.html.
- 3.Centers for Disease Control and Prevention. [Accessed 3 November 2017];HIV surveillance report. 2015 27 Available at: http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. [Google Scholar]
- 4.Balaji AB, Bowles KE, Le BC, Paz-Bailey G, Oster AM NHBS Study Group. High HIV incidence and prevalence and associated factors among young MSM, 2008. AIDS. 2013;27:269–78. doi: 10.1097/QAD.0b013e32835ad489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sullivan PS, Rosenberg ES, Sanchez TH, et al. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann Epidemiol. 2015;25:445–54. doi: 10.1016/j.annepidem.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13:482. doi: 10.1186/1471-2458-13-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poundstone KE, Strathdee SA, Celentano DD. The social epidemiology of human immunodeficiency virus/acquired immunodeficiency syndrome. Epidemiol Rev. 2004;26:22–35. doi: 10.1093/epirev/mxh005. [DOI] [PubMed] [Google Scholar]
- 8.Millett GA, Peterson JL, Flores SA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380:341–8. doi: 10.1016/S0140-6736(12)60899-X. [DOI] [PubMed] [Google Scholar]
- 9.Mustanski B, Birkett M, Kuhns LM, Latkin CA, Muth SQ. The role of geographic and network factors in racial disparities in HIV among young men who have sex with men: an egocentric network study. AIDS Behav. 2015;19:1037–47. doi: 10.1007/s10461-014-0955-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. [Accessed 3 November 2017];HIV surveillance report. 2014 26 Available at: http://www.cdc.gov/hiv/library/reports/surveillance/ [Google Scholar]
- 11.Garofalo R, Hotton AL, Kuhns LM, Gratzer B, Mustanski B. Incidence of HIV infection and sexually transmitted infections and related risk factors among very young men who have sex with men. J Acquir Immune Defic Syndr. 2016;72:79–86. doi: 10.1097/QAI.0000000000000933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pathela P, Jamison K, Braunstein SL, Schillinger JA, Varma JK, Blank S. Incidence and predictors of HIV infection among men who have sex with men attending public sexually transmitted disease clinics, New York City, 2007–2012. AIDS Behav. 2016 doi: 10.1007/s10461-016-1499-2. [DOI] [PubMed] [Google Scholar]
- 13.Halkitis PN, Kapadia F, Siconolfi DE, et al. Individual, psychosocial, and social correlates of unprotected anal intercourse in a new generation of young men who have sex with men in New York City. Am J Public Health. 2013;103:889–95. doi: 10.2105/AJPH.2012.300963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mustanski BS, Newcomb ME, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. J Sex Res. 2011;48:218–53. doi: 10.1080/00224499.2011.558645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Newcomb ME, Ryan DT, Garofalo R, Mustanski B. The effects of sexual partnership and relationship characteristics on three sexual risk variables in young men who have sex with men. Arch Sex Behav. 2014;43:61–72. doi: 10.1007/s10508-013-0207-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kann L, Olsen EO, McManus T, et al. Sexual identity, sex of sexual contacts, and health-related behaviors among students in grades 9–12—United States and selected sites, 2015. MMWR Surveill Summ. 2016;65:1–202. doi: 10.15585/mmwr.ss6509a1. [DOI] [PubMed] [Google Scholar]
- 17.Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. 2000;55:469–80. [PubMed] [Google Scholar]
- 18.Somerville LH, Jones RM, Casey BJ. A time of change: behavioral and neural correlates of adolescent sensitivity to appetitive and aversive environmental cues. Brain Cogn. 2010;72:124–33. doi: 10.1016/j.bandc.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spear LP. The adolescent brain and the college drinker: biological basis of propensity to use and misuse alcohol. J Stud Alcohol Suppl. 2002:71–81. doi: 10.15288/jsas.2002.s14.71. [DOI] [PubMed] [Google Scholar]
- 20.Loftus J. America’s liberalization in attitudes toward homosexuality. Am Sociol Rev. 2001;66:762–82. [Google Scholar]
- 21.MacKellar DA, Gallagher KM, Finlayson T, Sanchez T, Lansky A, Sullivan PS. Surveillance of HIV risk and prevention behaviors of men who have sex with men–a national application of venue-based, time-space sampling. Public Health Rep. 2007;122(Suppl 1):39–47. doi: 10.1177/00333549071220S107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heckathorn D. Respondent-driven sampling: a new approach to the study of hidden populations. Social Problems. 1997;44:174–99. [Google Scholar]
- 23.Heckathorn D. Respondent-driven sampling II: deriving valid population estimates from chain-referral samples of hidden populations. Social Problems. 2002;49:11–34. [Google Scholar]
- 24.Osmond DH, Page K, Wiley J, et al. HIV infection in homosexual and bisexual men 18 to 29 years of age: the San Francisco Young Men’s Health Study. Am J Public Health. 1994;84:1933–7. doi: 10.2105/ajph.84.12.1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Halkitis PN, Brockwell S, Siconolfi DE, et al. Sexual behaviors of adolescent emerging and young adult men who have sex with men ages 13–29 in New York City. J Acquir Immune Defic Syndr. 2011;56:285–91. doi: 10.1097/QAI.0b013e318204194c. [DOI] [PubMed] [Google Scholar]
- 26.Outlaw AY, Phillips G, 2nd, Hightow-Weidman LB, et al. Young MSM of Color SPNS Initiative Study Group. Age of MSM sexual debut and risk factors: results from a multisite study of racial/ethnic minority YMSM living with HIV. AIDS Patient Care STDS. 2011;25(Suppl 1):S23–9. doi: 10.1089/apc.2011.9879. [DOI] [PubMed] [Google Scholar]
- 27.Raymond HF, McFarland W. Racial mixing and HIV risk among men who have sex with men. AIDS Behav. 2009;13:630–7. doi: 10.1007/s10461-009-9574-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Clerkin EM, Newcomb ME, Mustanski B. Unpacking the racial disparity in HIV rates: the effect of race on risky sexual behavior among black young men who have sex with men (YMSM) J Behav Med. 2011;34:237–43. doi: 10.1007/s10865-010-9306-4. [DOI] [PubMed] [Google Scholar]
- 29.Matthews DD, Herrick AL, Coulter RW, et al. POWER Study Team. Running backwards: consequences of current HIV incidence rates for the next generation of black MSM in the United States. AIDS Behav. 2016;20:7–16. doi: 10.1007/s10461-015-1158-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.US Food and Drug Administration. [Accessed 3 November 2017];Truvada approved to reduce the risk of sexually transmitted HIV in people who are infected with the virus. Available at: https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm311821.htm.
- 31.Society for Adolescent Health and Medicine. Recommendations for promoting the health and well-being of lesbian, gay, bisexual, and transgender adolescents: a position paper of the Society for Adolescent Health and Medicine. J Adolesc Health. 2013;52:506–10. doi: 10.1016/j.jadohealth.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 32.Morris E, Topete P, Rasberry CN, Lesesne CA, Kroupa E, Carver L. School-based HIV/STD testing behaviors and motivations among black and Hispanic teen MSM: results from a formative evaluation. J Sch Health. 2016;86:888–97. doi: 10.1111/josh.12457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lesesne CA, Rasberry CN, Kroupa E, et al. Communicating with school staff about sexual identity, health and safety: an exploratory study of the experiences and preferences of black and Latino teen young men who have sex with men. LGBT Health. 2015;2:258–64. doi: 10.1089/lgbt.2014.0087. [DOI] [PMC free article] [PubMed] [Google Scholar]