Abstract
Objective
Despite its association with increased severity and treatment resistance, relatively little is known about the correlates of early-onset childhood depression. Attention-deficit/hyperactivity disorder (ADHD) and executive functioning (EF) are each related to depression. Given their covariation, we tested the independent association of ADHD dimensions (i.e., inattention, hyperactivity) and EF with childhood depression using structural equation modeling to identify potential targets for intervention.
Method
Participants were 225 5-10 year-old children (68% male) with (n = 117) and without (n = 108) ADHD. Youth completed laboratory assessments of EF and parent, teacher, and youth reports of depression were gathered.
Results
With control of EF and anxiety, across informants, inattention, but not hyperactivity, was positively related to child depression. EF was positively associated with depression according to parent ratings only.
Conclusion
We consider the association of inattention and EF with childhood depression, including implications for intervention and prevention from a developmental psychopathology framework.
Keywords: ADHD, Executive Function, Depression, Structural Equation Modeling
There is meta-analytic evidence that childhood attention-deficit/hyperactivity disorder (ADHD) confers elevated risk for depression across clinic-referred and community based samples (Meinzer, Pettit, & Viswesvaran, 2014). Youth with co-occurring ADHD and depression are more likely to experience negative outcomes in a variety of domains relative to individuals with either disorder alone (Meinzer & Chronis-Tuscano, 2017). For example, they exhibit greater social deficits than youth with ADHD only (Blackman, Ostrander, & Herman, 2005) and adolescents with ADHD and depression also relapse following treatment more often than adolescents with depression alone (Rohde, Clarke, Lewinsohn, Seeley, & Kaufman, 2001). Perhaps most critically, individuals with comorbid ADHD and depression are at an increased risk for attempting and committing suicide (Chronis-Tuscano et al., 2010; Daviss, 2008; James, Lai, & Dahl, 2004). Given the significant vulnerability associated with co-occuring ADHD and depression, their clinical correlates must be better characterized. In particular, because ADHD and depression share clinical correlates, predictive models must be adequately specified to facilitate innovations in intervention and prevention.
Several mechanisms have been proposed to explain the relationship between ADHD depression. The dual-failure model suggests that depression develops from childhood ADHD through ADHD-related impairments such as substandard academic achievement and negative peer relationships (Hinshaw, 2002; Patterson, & Stoolmiller, 1991). Additionally, emotion regulation may mediate predictions of depression from ADHD in youth across both clinic-referred and community-based samples (Seymour et al., 2012; Seymour, Chronis-Tuscano, Iwamoto, Kurdziel, & MacPherson, 2014). Other clinical correlates common to both disorders (e.g., executive functioning) have not yet been thoroughly considered in the context of co-occurring ADHD and depression.
Executive functioning (EF) consists of distinct, yet related cognitive processes (i.e., set shifting, inhibitory control, working memory) involved in goal directed behavior (Pennington & Ozonoff, 1996). Across development, EF deficits frequently accompany ADHD, even with control of IQ (Willcutt, Doyle, Nigg, Faraone, & Pennington, 2005). Similarly, controlling for processing speed, EF deficits were positively associated with depression severity in a large meta-analysis (Snyder, 2013), although this was based largely on adults. However, the association of EF with childhood depression is less clear. For example, although set shifting was impaired in a subset of youth with depression, overall EF was unrelated to depression (Favre et al., 2008). This small study (N = 63) employed 8-17 year old youth, thereby precluding specific inferences about depression in childhood relative to adolescence (Favre et al., 2008). Notably, in a meta-analysis of under age 18 youth, depressed youth performed worse on multiple EF indicators, including inhibition, attention, and planning relative to healthy controls (Wagner, Müller, Helmreich, Huss, & Tadić, 2015), although once again, childhood depression was not specifically examined. Overall, given their significant covariation, ADHD and EF must be examined simultaneously to discern their potential independent association with childhood depression.
Recent studies have begun to consider EF in the context of co-occurring ADHD and depression. Among adolescents with ADHD only, depression only, comorbid ADHD and depression, and controls, youth with comorbid ADHD and depression exhibited worse working memory, a key component of EF, relative to youth with ADHD alone (Roy, Oldehinkel, & Hartman, 2016). However, the study did not address early-onset depression and key constructs relied exclusively on youth self-report, despite crucial advantages afforded by multiple methods and informants (Martel, Markon, & Smith, 2016). A two-year prospective study of 9-18 year-olds examined ADHD, EF, and depression simultaneously (Øie, Hovik, Andersen, Czajkowski, & Skogli, 2016). EF did not increment predictions of depression beyond ADHD symptoms (Øie et al., 2016). In the study, childhood depression was not focally examined and raw change scores (i.e., Time 2 minus Time 1), which are error prone (Johns, 1981), were employed. Nevertheless, these preliminary studies suggest that EF and depression are associated among youth with ADHD.
Multiple methodological and developmental innovations are needed to improve the nascent literature examining the relationship of ADHD and EF with childhood depression. First, studies infrequently dissociate inattention and hyperactivity (Meinzer et al., 2014; Ostrander, Crystal, & August, 2006), thereby obfuscating potentially more specific relationships with depression. This is a priority given that children diagnosed with the inattentive subtype of ADHD were more likely to experience depression or anxiety relative to individuals with the hyperactive subtype (Lahey, & Carlson, 1991; Lahey, Schaughency, Hynd, Carlson, & Nieves, 1987). Similarly, only inattention distinguished controls from youth with comorbid ADHD and depression suggesting that inattention symptoms, relative to hyperactivity, may be uniquely related to depression in this population (Blackman et al., 2005). Second, examining symptoms dimensionally is particularly important given that ADHD represents the extreme of a continuum of hyperactivity and inattention (Levy, Hay, McStephen, Wood, & Waldman, 1997; Lubke, Hudziak, Derks, van Bijsterveldt, & Boomsma, 2009). Third, multiple-informants are infrequently employed in studies of child depression, despite modest correspondence between adult- and child-report of internalizing symptoms (De Los Reyes & Kazdin, 2005). With respect to specificity, current studies examining childhood depression seldom control for anxiety, which is the most commonly co-occurring disorder with childhood depression (Cummings, Caporino, & Kendall, 2014). In considering EF, rigorous approaches to combat measurement effort should be prioritized because traditional measures of this construct have considerable error (Chaytor, Schmitter-Edgecombe, & Burr, 2006). Additionally, EF and IQ are significantly correlated (Arffa, 2007); therefore, controlling for the effect of IQ on EF is essential to determine whether EF is uniquely related to child depression. Finally, studies have examined the association of ADHD and EF with depression utilizing samples of adolescents or a wide age-range spanning all of middle childhood and adolescence (Øie et al., 2016; Roy et al., 2016) rather than examining youth with depression prior to adolescence.
To improve traction on the unique associations among problems with considerable clinical significance, the current study tested the cross-sectional association of separate ADHD dimensions (i.e., inattention, hyperactivity) and EF (i.e., set shifting, working memory, inhibitory control) with depression in 5- to 10-year-old children. Capitalizing on multiple measures of parent-rated ADHD, child EF, as well as self-, parent- and teacher-rated child depression, we employed structural equation modeling (SEM) using data from 225 5-10 year-old children with and without ADHD. Importantly, we also controlled for the association of anxiety with depression and the covariation of age and full-scale IQ (FSIQ) with EF to improve specificity. We hypothesized that inattention, but not hyperactivity, would be positively correlated with childhood depression whereas EF would be inversely correlated with childhood depression. To our knowledge, this is the first study to test the independent association of inattention and hyperactivity, as well as EF, with early-onset depression in childhood using a latent variable approach, a key advantage given its maximization of statistical power.
Method
Participants
Two hundred and twenty-five ethnically diverse (51.1% Caucasian; 8.9% African American; 10.7% Hispanic; 3.6% Asian; 25.7% Mixed/Other/Unknown) 5-to-10 year-old (M = 7.44, SD = 1.14) youth (68% male) with (n = 117) and without (n = 108) ADHD, and their families were recruited from a large metropolitan city in the Western U.S. through advertisements at mental health service agencies, schools, and service providers. For the current study, inclusion criteria were English fluency and living with a biological caregiver (i.e., parent or grandparent) at least halftime. Exclusion criteria consisted of an IQ below 70 or seizure, autism spectrum, or other neurological condition.
Procedures
To determine study eligibility, families completed an initial phone screening. Eligible families and teachers were mailed rating scales to assess child functioning across both the home and school settings. Families were invited to complete a laboratory-based assessment conducted by well-trained graduate students in clinical psychology or B.A. level staff blind to youth diagnostic status. After obtaining informed consent from parents and child assent, youth completed tests of EF and academic achievement as well as interviews to evaluate socio-emotional functioning. Concurrently, parents completed structured diagnostic interviews and rating scales to assess child functioning. The IRB approved all study procedures.
Measures
Diagnostic Interview Schedule for Children (DISC-IV)
The ADHD module of the DISC-IV, Parent Edition (Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000) was conducted with parents to assess Diagnostic and Statistical Manual (DSM)-IV ADHD symptoms in children. The DISC-IV-P is a computer-assisted, structured interview with strong psychometric properties: it demonstrated a test–retest reliability of r = .79 after 1 year as well as an internal consistency of 0.84 for symptoms and 0.77 for criterion in a large community sample (see Shaffer et al., 2000). We analyzed the 9 inattention and 9 hyperactivity symptoms of the ADHD module.
Disruptive Behavior Disorder Rating Scale (DBD)
Parents rated DSM–IV DBD symptoms with response options ranging from 0 = not at all to 3 = very much (Pelham, Gnagy, Greenslade, & Milich, 1992). The 18 symptoms that compose DSM–IV ADHD were summed to create dimensional severity scores of inattention and hyperactivity symptoms respectively. Each subscale (i.e., inattention, hyperactivity) was split into odd and even item composites yielding 2 inattention severity scores and 2 hyperactivity severity scores. With respect to the current sample, the odd (r = .97, p < .001) and even (r = .94, p < .001) item composites of inattention significantly correlated with the total inattention composite. Likewise, the odd (r = .98, p < .001) and even (r = .94, p < .001) item composites of hyperactivity/impulsivity were significantly related to the total hyperactivity composite. Past work has demonstrated the validity of the DBD in assessing ADHD in school-age children (Owens & Hoza, 2003).
Trail Making Test Part B (TMT B)
We administered the child variation of the Trail Making Test (Reitan, 1979). Trail Making Test part A involves drawing lines to connect numbered circles in sequential order from 1 to 15 as quickly as possible without making errors. TMT B involves connecting numbers 1 through 13 and letters A through L in the proper numerical and alphabetical sequence. The time (min) to complete TMT B reflects the EF dimension of set shifting (Reitan, 1979). Research demonstrates that TMT B significantly differentiates youth with ADHD and controls (Martel, Nikolas, & Nigg, 2007). TMT B completion time was used to estimate set shifting. Because longer time to complete TMT B indicates worse set shifting, we used the inverse of the completion time for analyses. Using the inverse score ensured consistency in higher scores representing better EF across all EF tests.
Golden Stroop
Participants completed the Children’s Version of the Golden Stroop (Golden, Freshwater, & Zarabeth, 2003) to assess the inhibitory control facet of EF (Miyake, et al., 2000). Participants were first asked to read as many words (i.e., red, blue, green) as possible in 45 sec, followed by naming different colors of ink (i.e., red, blue, green) in condition 2. In the third and final condition (i.e., Color-Word), the names of colors are printed in discordant colors (e.g., “red” is printed in blue ink). Youth must name the color of the ink and inhibit the prepotent response of reading the word. The total score on the Color-Word condition is the number of ink colors named during the 45-second time limit. This Stroop Color-Word score has been shown to correlate with other measures of inhibitory control (e.g., Stop Signal, Antisaccade) and loaded on to a latent inhibition factor (Miyake et al., 2000).
Digit Span Backwards
Children completed the Digit Span subtest from the Wechsler Intelligence Scale for Children-IV (Wechsler, 2003) to estimate working memory. The forward condition requires recall of a string of numbers that were read aloud; the backward condition requires recalling the numbers in the reverse order. We analyzed the Digit Span Backwards raw score to estimate working memory given it loaded more strongly on a latent working memory factor of EF relative to the forward condition (Arán Filippetti, & Richaud, 2016).
FSIQ
We administered the Vocabulary, Symbol Search, and Arithmetic subtests of the WISC-IV (Wechsler, 2003). To estimate FSIQ, we summed the scaled scores of these three subtests, given their high correlation with IQ (r = 0.91) derived from the complete battery in the normative sample (Sattler & Dumont, 2004).
Children’s Depression Inventory (CDI)
The CDI, a 27-item, self-report measure, was completed by participating children (Kovacs, 1992). They were asked to endorse one of three descriptions that was most applicable to their experience over the past two weeks (e.g., “I feel like crying everyday,” “I feel like crying many days,” “I feel like crying once in awhile”). Each item is scored based on a 0-2 metric with 2 reflecting higher depression severity. The total raw score across all 27 items were converted to T-scores to adjust for child age and sex, including age 7 norms for younger youth. The CDI has shown strong convergent validity with key criteria including other internalizing disorders (e.g., anxiety) and disruptive behavior (e.g., ADHD; Timbremont, Braet, & Dreessen, 2004).
Child Behavior Checklist/Teacher Report Form (CBCL/TRF)
Parents completed the CBCL (Achenbach & Rescorla, 2001), a normed 113-item rating scale of youth behavior over the prior six months with each item rated from 0 (not true) to 2 (very true/often true). The CBCL yields eight narrowband syndrome scales, DSM-oriented scales, and broadband internalizing and externalizing scales. Teachers completed the TRF, which provides parallel scales as the CBCL. The CBCL and TRF are reliably correlated with DSM-based symptom measures and well validated (Achenbach & Rescorla, 2001). For the present study we used the T-scores, which adjust for child age and sex, from the Affective Problems Scale on the CBCL and TRF. The Affective Problems scale is associated with Major Depressive Disorder (MDD) and Dysthymic Disorders (Ebesutani et al., 2010). We also used the Anxiety Problems Scale T-score from the CBCL to control for anxiety on the depression variables.
Data analytic procedures
Data were initially compiled and tested for multivariate normality using Stata (Version 14.0); subsequent analyses were conducted using Mplus (Version 7.4 for Mac). To correct for biases due to random error and construct-irrelevant variance, we employed SEM (Bollen, 1989) to evaluate the associations among constructs of ADHD, EF, and multi-informant (i.e., self, parent, teacher) ratings of child depression. Mardia’s test of Skewness = 45.89, χ2(680) = 997.23, p < .001 and Mardia’s test of Kurtosis = 263.02, χ2 (1) = 4.00, p < .05 violated the criteria for multivariate normality. Missing data ranged from 32.9% on the CDI T-score to 0% on age and DISC-IV inattention and hyperactivity/impulsivity symptom counts. We implemented maximum likelihood robust procedures in Mplus (Muthén, & Muthén, 1998 –2010) to address non-normality and to accommodate missing data. Maximum likelihood estimation, a state-of-the-art missing data technique, enhances the accuracy and power of analyses relative to other approaches (Schaafer & Graham, 2002). To evaluate model fit, we examined the maximum likelihood chi-square, Comparative Fit Index (CFI), root mean square error of approximation (RMSEA) and standardized root mean square residual (SRMR). A non-significant chi-square statistic and CFI values ≥ .95 indicate good fit. Other measures of fit (i.e., RMSEA, SRMR) are more reliable. RMSEA estimates model fit with control of sample size and per degrees of freedom. Hu and Bentler (1998) endorse values of .06 or less for RMSEA and .08 or less for SRMR, which is highly sensitive to model misspecification, for good model fit.
To test their separate associations with depression, we created separate latent variables for inattention, hyperactivity, and EF. However, self-, parent-, and teacher- rated depression were not strongly correlated enough to form a latent factor (see Table 1; described further below). To achieve the minimum number of indicator variables (i.e., three) for inattention and hyperactivity, we divided these scales on the DBD into odd and even items and created two separate composite scores (Humphreys et al., 2013; Kellwoay, 1998) Notably, forming composites based on randomly assigned items (e.g., odd, even) results in better model fit than when using individual measure items in the creation of a latent variable (Landis, Beal, & Tesluk, 2000). This method yielded three indicator variables for inattention (i.e., DISC-IV, DBD odd, DBD even) and hyperactivity (i.e., DISC-IV, DBD odd, DBD even). The EF factor was created using TMT B, Stroop Color-Word, and Digit Span Backward. Because of modest fit across the three observed depression variables, the CDI, CBCL, and TRF depression T-scores were entered into the models simultaneously. Demographic factors were not covaried given that the T-scores are already adjusted for age and sex; therefore it would be redundant to additionally control for age on the depression variables. However, all models controlled for age and FSIQ on the EF factor given significant covariation. Additionally, to enhance specificity, we controlled for anxiety on each of the three depression variables.
Table 1.
Correlation Matrix for Study Variables
| Variable | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | −.06 | −.09 | .08 | −.03 | −.17** | −.01 | −.07 | −.13* | −.12 | .49*** | .40*** | .32*** | .04 | .17** | .04 |
| 2. Sex (boy = 1) | – | .11 | .08 | .11 | .19** | .07 | .09 | .15* | .16* | .00 | −.06 | .01 | −.15 | .08 | .04 |
| 3. FSIQ | – | −.09 | −.22*** | −.02 | −.26*** | −.18** | −.04 | −.10 | .35*** | .33*** | .32*** | −.15 | −.10 | −.11 | |
| 4. CBCL Anxiety Problems T-score | – | .33*** | .32*** | .31*** | .30*** | .33*** | .37*** | .08 | −.06 | .03 | .07 | .57*** | .18* | ||
| 5. DISC IN symptoms | – | .58*** | .78*** | .78*** | .59*** | .62*** | −.25*** | −.25*** | −.13* | .27*** | .43*** | .26*** | |||
| 6. DISC HY symptoms | – | .58*** | .55*** | .87*** | .81*** | −.17** | −.16* | −.15* | .12 | .34*** | .19* | ||||
| 7. DBD IN symptom score (odd items) | – | .84*** | .68*** | .74*** | −.21** | −.27*** | −.19** | .23** | .43*** | .23*** | |||||
| 8. DBD IN symptom score (even items) | – | .69*** | .71*** | −.25*** | −.29*** | −.09 | .17* | .39*** | .17* | ||||||
| 9. DBD HY symptom score (odd items) | – | .86*** | −.12 | −.16* | −.08 | .14* | .37*** | .20** | |||||||
| 10. DBD HY symptom score (even items) | – | −.18* | −.20** | −.12 | .12 | .36*** | .20* | ||||||||
| 11. TMT B (min) | – | .37*** | .45*** | −.07 | .06 | −.04 | |||||||||
| 12. Stroop Color-Word | – | .30*** | −.10 | −.06 | −.11 | ||||||||||
| 13. WISC-IV Digit Span Backwards | – | −.12 | .01 | −.02 | |||||||||||
| 14. CDI Total T-Score | – | .07 | .34*** | ||||||||||||
| 15. CBCL Affective Problems T-Score | - | .25** | |||||||||||||
| 16. TRF Affective Problems T-score | - | ||||||||||||||
| Mean (SD) or % |
68% | 106.89 (14.41) |
56.36 (7.54) |
4.53 (3.15) |
3.38 (3.07) |
6.72 (4.57) |
4.50 (3.28) |
6.30 (4.83) |
3.10 (2.60) |
−1.24 (.88) |
21.05 (6.36) |
5.86 (1.58) |
47.02 (7.41) |
57.00 (7.23) |
57.40 (7.81) |
Note.
p ≤ .05,
p ≤ .01,
p ≤ .001.
DISC = Diagnostic Interview Schedule for Children; IN = inattention; HY = hyperactivity; DBD = Disruptive Behavior Disorder Rating Scale; TMT B = Trail Making Test Part B; WISC-IV = Wechsler Intelligence Scale for Children, Fourth Edition; CDI = Children’s Depression Inventory; CBCL = Child Behavior Checklist; TRF = Teacher Report Form.
Results
Table 1 displays descriptive statistics and bivariate correlations of ADHD, EF, and depression variables as well as child age, sex, and FSIQ. All measures of ADHD were significantly, positively correlated. Inattention variables were typically inversely associated with EF measures and positively related to depression measures. Generally, hyperactivity indicators were negatively associated with EF measures. All hyperactivity variables were positively correlated with CBCL parent-report and TRF teacher-report of depression, but were unrelated CDI child-report. Despite significant inter-correlation among all EF variables, they did not correlate significantly with any depression variables. CBCL and TRF depression were related, as was the CDI and TRF. However, CBCL parent-report and CDI child-report of depression were uncorrelated. Finally, with respect to control variables, age and FISQ were positively associated with all three EF measures and the CBCL Anxiety Problems Scale was positively correlated with depression across all informants.
Confirmatory Factor Analyses
We first conducted separate confirmatory factor analyses on each of the 4 proposed latent variables (i.e., inattention, hyperactivity, EF, depression). Because these proposed factors had 3 indicator variables each, no fit indices were calculated. However, the factor loadings for each latent variable are presented in Table 2. With the exception of depression, the factor loading of each observed variable on its respective factor was at least 0.5 exceeding the guidelines for loadings of at least 0.3 (Brown, 2014). The factor loadings for the depression variables were low and the residual covariance matrix was not positive definite given the inconsistent correlations among the variables. This is expected given that informant discrepancies for childhood internalizing disorders (e.g., depression) are common (De Los Reyes & Kazdin, 2005). Based on the overall CFA results, we modeled latent factors for inattention, hyperactivity, and EF; all observed depression variables were entered separately rather than as a latent factor.
Table 2.
CFA Factor Loadings for Latent Variables
| Factor | Factor Loading | SE | z | p |
|---|---|---|---|---|
| Inattention | ||||
| DISC IN symptoms | .86 | .02 | 36.02 | <.001 |
| DBD IN symptom score (odd items) | .92 | .02 | 48.93 | <.001 |
| DBD IN symptom score (even items) | .91 | .02 | 51.72 | <.001 |
| Hyperactivity | ||||
| DISC HY symptoms | .90 | .02 | 50.41 | <.001 |
| DBD HY symptom score (odd items) | .96 | .01 | 83.78 | <.001 |
| DBD HY symptom score (even items) | .90 | .02 | 48.24 | <.001 |
| Executive Functioning | ||||
| TMT B (min) | .78 | .08 | 9.60 | <.001 |
| Stroop Color-Word | .50 | .08 | 6.44 | <.001 |
| WISC-IV Digit Span Backwards | .57 | .08 | 7.44 | <.001 |
| Depression* | ||||
| CDI Total T-Score | .31 | .19 | 1.59 | .11 |
| CBCL Affective Problems T-Score | .21 | .13 | 1.65 | .10 |
| TRF Affective Problems T-Score | 1.06 | .55 | 1.93 | .05 |
Note.
Residual covariance matrix is not positive definite. DISC = Diagnostic Interview Schedule for Children; IN = inattention; HY = hyperactivity; DBD = Disruptive Behavior Disorder Rating Scale; TMT B = Trail Making Test Part B; WISC-IV = Wechsler Intelligence Scale for Children, Fourth Edition; CDI = Children’s Depression Inventory; CBCL = Child Behavior Checklist; TRF = Teacher Report Form.
Initial Structural Model
To examine the association of inattention, hyperactivity, and EF on self-, parent-, and teacher-ratings of child depression, we regressed each depression variable (i.e., CBCL and TRF Affective Problems T-score, CDI T-score), on the inattention, hyperactivity, and EF latent variables. We controlled for parent-reported anxiety (T-score) from the CBCL for each of the three separate depression variables and controlled for FSIQ and age on EF. The model fit was modest, χ2(67) = 136.51, p < .001, CFI = .96, RMSEA = .07, SRMR = .03. Although the CFI and SRMR values were acceptable, other indices suggested model misspecification. In examining the model paths, inattention was positively related to child- (β = .38, SE = .14, p < .01) and parent-report (β = .44, SE = .12, p < .001) of depression but unrelated to teacher-report (β = .21, SE = .14, p = .14). EF was positively correlated with parent-report of depression (β = .16, SE = .06, p < .01), but was unrelated to child- (β = −.02, SE = .10, p = .81) and teacher-report (β = .00, SE = .10, p = .99). Hyperactivity was unrelated to child (β = −.16, SE = .12, p = .17), parent (β = −.08, SE = .12, p = .51), and teacher (β = .01, SE = .14, p = .97) depression ratings; thus we removed the hyperactivity factor and reevaluated model fit.
Alternative Structural Model
With hyperactivity removed, we regressed all observed depression variables on latent inattention and EF factors (Figure 1). This model had improved fit χ2(39) = 50.02, p = .11, CFI = .99, RMSEA = .04, SRMR = .03. The Chi-square, CFI, RMSEA, SRMR all demonstrated excellent fit. Inattention was positively related to CDI self- (β = .26, SE = .10, p < .01), CBCL parent- (β = .38, SE = .07, p < .001), and TRF teacher-report (β = .20, SE = .08, p = .01) of child depression. EF was unrelated to CDI self- (β = −.02, SE = .10, p = .83) and TRF teacher-report (β = −.01, SE = .10, p = .95). In contrast, EF was positively correlated with CBCL parent-rated child depression (β = .16, SE = .06, p = .01).
Figure 1.
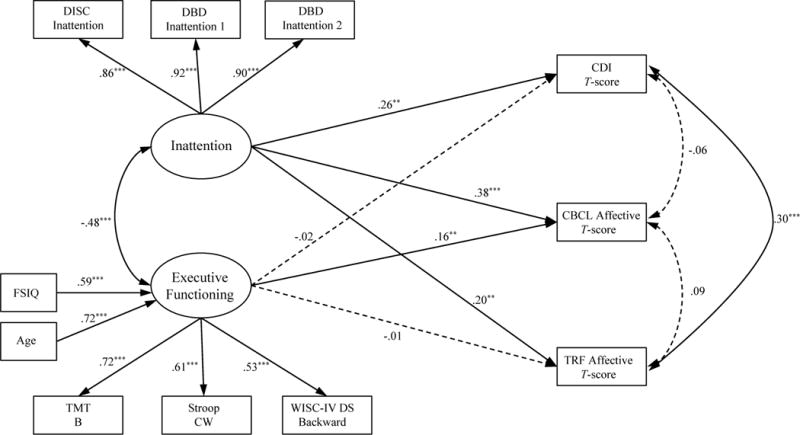
Model of the association of attention-deficit/hyperactivity disorder (ADHD) inattention and executive functioning (EF) with child self-, parent-, and teacher-report of depression (n = 225).
Note: DISC = Diagnostic Interview Schedule for Children; DBD = Disruptive Behavior Disorder Rating Scale; CDI = Children’s Depression Inventory; CBCL = Child Behavior Checklist; FSIQ = full-scale IQ; TRF = Teacher Report Form; TMT B = Trail Making Test Part B; CW = Color and Word; WISC-IV DS = Wechsler Intelligence Scale for Children–Fourth Edition Digit Span Backward. Standardized parameter estimations are shown; errors and control of CBCL Anxiety Problems T-score on observed depression variables not shown. Nonsignificant paths are represented by dotted lines.
*p ≤ .05. **p ≤ .01. ***p ≤ .001.
Multi-group Analysis
To further characterize association between EF and youth depression, we conducted follow-up multi-group analyses using a diagnostic ADHD variable from a fully structured DSM-IV interview with the parent. We regressed observed depression variables on the latent EF variable for youth with and without a diagnosis of ADHD, controlling for age and FSIQ on EF and anxiety on the depression variables. This model had poor fit χ2(45) = 111.72, p < .001, CFI = .79, RMSEA = .12, SRMR = .14. Thus, the association of EF and child depression did not differ between youth with versus without ADHD.
Discussion
There is limited knowledge about the association of inattention, hyperactivity, and EF with early-onset depression. Among 225 5-10 year-old children with and without ADHD, the association of latent inattention, hyperactivity, and EF variables, derived from multiple informants and methods, with child depression when controlling for and FSIQ on EF as well as anxiety on depression was tested. The preferred model, with good fit to the data, suggested that with hyperactivity excluded, inattention was positively related to child depression across separate self-, parent-, and teacher-report, beyond EF. Finally, childhood ADHD diagnostic status (i.e., ADHD versus non-ADHD comparison) did not moderate any association between EF and child depression.
Our findings are consistent with prior work that similarly demonstrated improved model fit of the association of ADHD with depression, following removal of hyperactivity (Humphreys et al., 2013). The finding that hyperactivity was unrelated to depression aligns with evidence that the inattention symptom of dimension of is ADHD more strongly related to depression (Blackman et al., 2005; Lahey, & Carlson, 1991; Lahey et al., 1987), however such studies evaluated diagnostic status. In contrast, when evaluating ADHD symptoms dimensionally, significant indirect effects of inattention and hyperactivity on depression via emotion regulation have been identified (Seymour et al., 2014), suggesting that hyperactivity is also relevant to depression. Because we evaluated both predictors (i.e., inattention, hyperactivity) simultaneously and the mean of inattention scores in our sample was somewhat larger than the mean of hyperactivity scores, it is likely that the effect of inattention resulted in the non-significant association between hyperactivity and depression.
Overall, inattention, but not hyperactivity, was positively associated with early expressions of depression. We note the robustness of this pattern given that this was observed across separate parent, teacher, and youth ratings, even with stringent control of EF, despite significant overlap between inattention and EF in this study and more generally (Diamond, 2013). Given that these data are cross-sectional, it is possible that depression directionally predicts inattention and/or that associations are enhanced by explicit item overlap (e.g., difficulty with concentration is a symptom of ADHD and depression; American Psychiatric Association, 2013). Phenomenologically, depression may precipitate symptoms of inattention given that attentional deficits often persist even after depression remission, at least in adults (Shilyansky et al., 2016). However, considering the current knowledge about the phenomenology and developmental nature of the disorders (e.g., age of onset), we contend that depression preceding ADHD is unlikely. We suggest that temporally-ordered tests of causal mediation are indicated to improve traction on the precise association of ADHD with depression (Meinzer et al., 2014).
Previous studies suggest that childhood EF and depression are inversely associated, but findings are inconsistent and based on problematic methods (Favre et al., 2008; Wagner et al., 2015), including failure to disentangle inattention from hyperactivity. Somewhat surprisingly, in the current study, EF and parent-rated child depression were positively correlated. The positive illusory bias is a known correlate of ADHD and demonstrates a tendency for individuals with ADHD over-estimate their competence relative to others’ assessment of their functioning (Owens, Goldfine, Evangelista, Hoza, & Kaiser, 2007); children with greater illusory bias demonstrate more EF deficits (McQuade et al, 2011). As EF is critical to self-monitoring and modifying behavior to attain goals, it is likely that children with ADHD and EF deficits struggle to evaluate their behavior. Thus, poor EF may contribute to a positive illusory bias that could subsequently buffer against depression. In contrast, children with ADHD and well-developed EF may monitor their (negative) behavior more accurately, including potential impairments in multiple domains (e.g., academic, social), thereby increasing their risk of depression. That a decrease in positive bias was accompanied by increased depression symptoms in youth with ADHD (Hoza, Murray-Close, Arnold, Hinshaw, & Hechtman, 2010) lends support to this formulation. Testing the positive illusory bias as a mechanism of the relationship between EF and depression in youth with ADHD is needed to improve understanding of this association. Finally, to identify potential subgroups of youth based on multiple dimensions, future studies should prosecute ADHD x EF interactions with respect to depression.
Notably, EF deficits were positively associated with youth depression according to parent ratings only, which may suggest that this is artifactual due to shared method variance (i.e., parent ratings for both constructs). The latent ADHD variables in this study reflect parent ratings only, suggesting that teacher ratings, for example, may have yielded meaningfully different patterns. Perceived distress in youth might also contribute to the present findings. For example, adolescents were less concerned about their own internalizing symptoms relative to their parents (Phares & Danforth, 1994). Additionally, deficits in key facets of EF are implicated in depressive rumination (i.e., persistent negative thoughts; Koster, De Lissnyder, Derakshan, & De Raedt, 2011). Therefore, youth with well-developed EF might be better able to inhibit negative thought patterns and minimize their perceived distress contributing to under-reporting of depressive symptoms relative to parent-report. Crucially, because these data were cross-sectional, depressive symptoms may also enhance EF in children with ADHD. Although uncharacteristic of populations with depression, perhaps depression interacts with ADHD in youth to improve EF as is sometimes observed in ADHD and other comorbid internalizing disorders. For example, there is replicated evidence that anxiety mitigates inhibitory control deficits in youth with ADHD (Schatz & Rostain, 2006), though further research is needed to determine whether depression similarly attenuates deficits in EF. As noted above, we recommend the use of temporally ordered EF and depression data to strengthen inferences of directional effects. Based upon these considerations, the preliminary finding that EF was positively related to parent-report of child depression requires further scrutiny, ideally with prospective data, to strengthen directional inferences.
The current study acknowledges several key limitations. As noted previously, the latent ADHD variables were derived from parent-report alone and utilized only two measures (i.e., DISC-IV, DBD) in the derivation of three indicator variables. Although splitting the DBD inattention and hyperactivity composites into odd and even item scores is not common, robust correlations of the odd and even scores with the original scale composites supports the use this approach. In future work, incorporating three separate measures of ADHD as well as teacher-report of ADHD symptoms to these factors may be an important addition. The EF latent variable was created using neuropsychological test-based indices of inhibitory control, set shifting, and working memory; however, such EF measures have long been challenged by concerns over limited ecological validity. Rather, some argue that informant report of youth EF would better capture the construct as it relates to functional impairments (Barkley, 2001); therefore, incorporation of informant report of EF might improve predictions and model fit. The factor loadings of the EF latent variable may represent another limitation because the loadings did not exceed 0.6, which some statisticians recommend as a cutoff (e.g., Field, 2005). Though factor loadings under 0.6 are normative across diverse samples in children and adults in the context of EF (Fournier-Vincente, Larigauderie, Gaonac’h, 2008; Friedman & Miyake 2004; Friedman et al., 2006; Hedden & Yoon, 2006; Miyake et al., 2000), utilizing informant ratings of EF as described above may improve factor loadings. Of note, the present study did not examine the association of Sluggish Cognitive Tempo (SCT) with depression. Recent work suggests that SCT is related to depression beyond ADHD (Becker, & Langberg, 2013), thus inclusion of SCT in future models of ADHD, EF, and depression is warranted. The depression scores in our sample are within the normal range. Although the findings are statistically significant, they must to be replicated in a sample of children with clinically significant levels of depression. Finally, the present study utilized cross-sectional data preventing causal interpretations.
The current study tested the association of ADHD and EF with depression in childhood using an SEM framework. A latent inattention variable was positively correlated with self-, parent-, and teacher-report of early-onset child depression over and above anxiety and EF, whereas the latent hyperactivity variable was unrelated. The latent EF factor, controlling for age and FSIQ, was positively associated with parent-rated child depression alone. These preliminary findings support the established association of ADHD and depression particularly via the dimension of inattention. Although the relationship between EF and child depression in individuals with ADHD requires further investigation, we contend that our findings demonstrate the importance of the inclusion of the EF construct in studies focused on co-occurring childhood ADHD and depression.
Biography
Michelle C. Fenesy, MA, is a graduate student in clinical psychology at UCLA. Her research interests include individual differences in executive functioning and associated mental health outcomes.
Steve S. Lee, PhD, is an associate professor in the department of psychology at UCLA with interests in developmental psychopathology of ADHD and disruptive behavior disorders.
References
- Achenbach TM, Rescorla L. ASEBA school-age forms & profiles. Burlington: Aseba; 2001. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, D.C: American Psychiatric Association; 2013. [Google Scholar]
- Arán Filippetti V, Richaud MC. A structural equation modeling of executive functions, IQ and mathematical skills in primary students: Differential effects on number production, mental calculus and arithmetical problems. Child Neuropsychology. 2016:1–25. doi: 10.1080/09297049.2016.1199665. [DOI] [PubMed] [Google Scholar]
- Arffa S. The relationship of intelligence to executive function and non-executive function measures in a sample of average, above average, and gifted youth. Archives of Clinical Neuropsychology. 2007;22(8):969–978. doi: 10.1016/j.acn.2007.08.001. [DOI] [PubMed] [Google Scholar]
- Barkley RA. The executive functions and self-regulation: An evolutionary neuropsychological perspective. Neuropsychology Review. 2001;11(1):1–29. doi: 10.1023/A:1009085417776. [DOI] [PubMed] [Google Scholar]
- Becker SP, Langberg JM. Sluggish cognitive tempo among young adolescents with ADHD: relations to mental health, academic, and social functioning. Journal of Attention Disorders. 2013;17(8):681–689. doi: 10.1037/a0023961.. [DOI] [PubMed] [Google Scholar]
- Blackman GL, Ostrander R, Herman KC. Children with ADHD and depression: a multisource, multimethod assessment of clinical, social, and academic functioning. Journal of Attention Disorders. 2005;8(4):195–207. doi: 10.1177/1087054705278777. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Structural equations with latent variables. NewYork, NY: Wiley; 1989. [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. Guilford Publications; 2014. [Google Scholar]
- Chaytor N, Schmitter-Edgecombe M, Burr R. Improving the ecological validity of executive functioning assessment. Archives of Clinical Neuropsychology. 2006;21(3):217–227. doi: 10.1016/j.acn.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Molina BS, Pelham WE, Applegate B, Dahlke A, Overmyer M, Lahey BB. Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 2010;67(10):1044–1051. doi: 10.1001/archgenpsychiatry.2010.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings CM, Caporino NE, Kendall PC. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychological Bulletin. 2014;140(3):816–845. doi: 10.1037/a0034733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daviss WB. A review of co-morbid depression in pediatric ADHD: etiologies, phenomenology, and treatment. Journal of Child and Adolescent Psychopharmacology. 2008;18(6):565–571. doi: 10.1089/cap.2008.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychological Bulletin. 2005;131(4):483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Diamond A. Executive functions. Annual Review of Psychology. 2013;64:135–168. doi: 10.1146/annurev-psych-113011-143750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebesutani C, Bernstein A, Nakamura BJ, Chorpita BF, Higa-McMillan CK, Weisz JR, Research Network on Youth Mental Health Concurrent validity of the Child Behavior Checklist DSM-oriented scales: Correspondence with DSM diagnoses and comparison to syndrome scales. Journal of Psychopathology and Behavioral Assessment. 2010;32(3):373–384. doi: 10.1007/s10862-009-9174-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Favre T, Hughes C, Emslie G, Stavinoha P, Kennard B, Carmody T. Executive functioning in children and adolescents with major depressive disorder. Child Neuropsychology. 2008;15(1):85–98. doi: 10.1080/09297040802577311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field A. Factor analysis using SPSS. Retrieved March. 2005;17:2009. [Google Scholar]
- Golden CJ, Freshwater SM, Zarabeth G. Stroop Color and Word Test Children’s Version for ages 5-14: A Manual for Clinical and Experimental Uses. Stoelting; 2003. [Google Scholar]
- Hoza B, Murray-Close D, Arnold LE, Hinshaw SP, Hechtman L. Time- dependent changes in positively biased self-perceptions of children with attention- deficit/hyperactivity disorder: A developmental psychopathology perspective. Development and Psychopathology. 2010;22(02):375–390. doi: 10.1017/S095457941000012X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinshaw SP. Is ADHD an impairing condition in childhood and adolescence? In: Jensen PS, Cooper JR, editors. Attention-deficit hyperactivity disorder: State of the Science, Best Practices. Kingston, NJ: Civic Research Institute; 2002. pp. 5-1–5-21. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Humphreys KL, Katz SJ, Lee SS, Hammen C, Brennan PA, Najman JM. The association of ADHD and depression: Mediation by peer problems and parent–child difficulties in two complementary samples. Journal of Abnormal Psychology. 2013;122(3):854. doi: 10.1037/a0033895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James A, Lai FH, Dahl C. Attention deficit hyperactivity disorder and suicide: a review of possible associations. Acta Psychiatrica Scandinavica. 2004;110(6):408–415. doi: 10.1111/j.1600-0447.2004.00384.x. [DOI] [PubMed] [Google Scholar]
- Johns G. Difference score measures of organizational behavior variables: A critique. Organizational Behavior and Human Performance. 1981;27(3):443–463. doi: 10.1016/0030-5073(81)90033-7. [DOI] [Google Scholar]
- Koster EH, De Lissnyder E, Derakshan N, De Raedt R. Understanding depressive rumination from a cognitive science perspective: The impaired disengagement hypothesis. Clinical Psychology Review. 2011;31(1):138–145. doi: 10.1016/j.cpr.2010.08.005. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Manual for the Children’s Depression Inventory. North Tonawanda, NJ: Multi-Health Systems; 1992. [Google Scholar]
- Kelloway EK. Using LISREL for structural equation modeling: A researcher’s guide. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Landis RS, Beal DJ, Tesluk PE. A comparison of approaches to forming composite measures in structural equation models. Organizational Research Methods. 2000;3(2):186–207. doi: 10.1177/109442810032003. [DOI] [Google Scholar]
- Levy F, Hay DA, McStephen M, Wood C, Waldman I. Attention-deficit hyperactivity disorder: a category or a continuum? Genetic analysis of a large-scale twin study. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(6):737–744. doi: 10.1097/00004583-199706000-00009. [DOI] [PubMed] [Google Scholar]
- Lubke GH, Hudziak JJ, Derks EM, van Bijsterveldt TC, Boomsma DI. Maternal ratings of attention problems in ADHD: evidence for the existence of a continuum. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48(11):1085–1093. doi: 10.1097/chi.0b013e3181ba3dbb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM, Markon K, Smith GT. Research Review: Multi-informant integration in child and adolescent psychopathology diagnosis. Journal of Child Psychology and Psychiatry. 2016 doi: 10.1111/jcpp.12611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel M, Nikolas M, Nigg JT. Executive function in adolescents with ADHD. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46(11):1437–1444. doi: 10.1111/jcpp.12464. [DOI] [PubMed] [Google Scholar]
- McQuade JD, Tomb M, Hoza B, Waschbusch DA, Hurt EA, Vaughn AJ. Cognitive deficits and positively biased self-perceptions in children with ADHD. Journal of Abnormal Child Psychology. 2011;39(2):307–319. doi: 10.1007/s10802-010-9453-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinzer MC, Chronis-Tuscano A. ADHD and the Development of Depression: Commentary on the Prevalence, Proposed Mechanisms, and Promising Interventions. Current Developmental Disorders Reports. 2017;4(1):1–4. doi: 10.1007/s40474-017-0106-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinzer MC, Pettit JW, Viswesvaran C. The co-occurrence of attention- deficit/hyperactivity disorder and unipolar depression in children and adolescents: a meta-analytic review. Clinical Psychology Review. 2014;34(8):595–607. doi: 10.1016/j.cpr.2014.10.002. [DOI] [PubMed] [Google Scholar]
- Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, Wager TD. The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: A latent variable analysis. Cognitive Psychology. 2000;41(1):49–100. doi: 10.1006/cogp.1999.0734. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6th ed. Los Angeles, CA: Author; 1998–2010. [Google Scholar]
- Øie M, Hovik KT, Andersen PN, Czajkowski NO, Skogli EW. Gender differences in the relationship between changes in ADHD symptoms, executive functions, and self-and parent-report depression symptoms in boys and girls with ADHD: A 2-year follow-up study. Journal of Attention Disorders. 2016 doi: 10.1177/1087054716664407. [DOI] [PubMed] [Google Scholar]
- Ostrander R, Crystal DS, August G. Attention deficit-hyperactivity disorder, depression, and self-and other-assessments of social competence: a developmental study. Journal of Abnormal Child Psychology. 2006;34(6):772–786. doi: 10.1007/s10802-006-9051-x. [DOI] [PubMed] [Google Scholar]
- Owens JS, Goldfine ME, Evangelista NM, Hoza B, Kaiser NM. A critical review of self-perceptions and the positive illusory bias in children with ADHD. Clinical Child and Family Psychology Review. 2007;10(4):335–351. doi: 10.1007/s10567-007-0027-3. [DOI] [PubMed] [Google Scholar]
- Owens J, Hoza B. Diagnostic utility of DSM-IV-TR symptoms in the prediction of DSM-IV-TR ADHD subtypes and ODD. Journal of Attention Disorders. 2003;7(1):11–27. doi: 10.1177/108705470300700102. [DOI] [PubMed] [Google Scholar]
- Patterson GR, Stoolmiller M. Replications of a dual failure model for boys’ depressed mood. Journal of Consulting and Clinical Psychology. 1991;59:491–498. doi: 10.1037/0022-006X.59.4.491. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Jr, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM–III–R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Pennington BF, Ozonoff S. Executive functions and developmental psychopathology. Journal of Child Psychology and Psychiatry. 1996;37(1):51–87. doi: 10.1111/j.1469-7610.1996.tb01380.x. [DOI] [PubMed] [Google Scholar]
- Phares V, Danforth JS. Adolescents’, parents’, and teachers’ distress over adolescents’ behavior. Journal of Abnormal Child Psychology. 1994;22(6):721–732. doi: 10.1007/BF02171998. [DOI] [PubMed] [Google Scholar]
- Reitan RM. Manual for administration of neuropsychological test batteries for adults and children. Neuropsychology Laboratory, Indiana University Medical Center; 1979. [Google Scholar]
- Rohde P, Clarke GN, Lewinsohn PM, Seeley JR, Kaufman NK. Impact of comorbidity on a cognitive-behavioral group treatment for adolescent depression. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(7):795–802. doi: 10.1097/00004583-200107000-00014. [DOI] [PubMed] [Google Scholar]
- Roy A, Oldehinkel AJ, Hartman CA. Cognitive functioning in adolescents with self-reported ADHD and depression: results from a population-based study. Journal of Abnormal Child Psychology. 2016:1–13. doi: 10.1007/s10802-016-0160-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schatz DB, Rostain AL. ADHD with comorbid anxiety a review of the current literature. Journal of Attention Disorders. 2006;10(2):141–149. doi: 10.1177/1087054706286698. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological Methods. 2002;7(2):147–176. doi: 10.1037/1082-989X.7.2.147. [DOI] [PubMed] [Google Scholar]
- Seymour KE, Chronis-Tuscano A, Halldorsdottir T, Stupica B, Owens K, Sacks T. Emotion regulation mediates the relationship between ADHD and depressive symptoms in youth. Journal of Abnormal Child Psychology. 2012;40(4):595–606. doi: 10.1007/s10802-011-9593-4. [DOI] [PubMed] [Google Scholar]
- Seymour KE, Chronis-Tuscano A, Iwamoto DK, Kurdziel G, MacPherson L. Emotion regulation mediates the association between ADHD and depressive symptoms in a community sample of youth. Journal of Abnormal Child Psychology. 2014;42(4):611–621. doi: 10.1007/s10802-013-9799-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC–IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Shilyansky C, Williams LM, Gyurak A, Harris A, Usherwood T, Etkin A. Effect of antidepressant treatment on cognitive impairments associated with depression: a randomised longitudinal study. The Lancet Psychiatry. 2016;3(5):425–435. doi: 10.1016/s2215-0366(16)00012-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR. Major depressive disorder is associated with broad impairments on neuropsychological measures of executive function: a meta-analysis and review. Psychological bulletin. 2013;139(1):81–132. doi: 10.1037/a0028727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiger JH. Understanding the limitations of global fit assessment in structural equation modeling. Personality and Individual Differences. 2007;42(5):893–898. doi: 10.1016/j.paid.2006.09.017. [DOI] [Google Scholar]
- Timbremont B, Braet C, Dreessen L. Assessing depression in youth: relation between the Children’s Depression Inventory and a structured interview. Journal of Clinical Child and Adolescent Psychology. 2004;33(1):149–157. doi: 10.1207/S15374424JCCP3301_14. [DOI] [PubMed] [Google Scholar]
- Vandenberg RJ. Statistical and methodological myths and urban legends: Where, pray tell, did they get this idea? Organizational Research Methods. 2006;9(2):194–201. doi: 10.1177/1094428105285506. [DOI] [Google Scholar]
- Wagner S, Müller C, Helmreich I, Huss M, Tadić A. A meta-analysis of cognitive functions in children and adolescents with major depressive disorder. European Child & Adolescent Psychiatry. 2015;24(1):5–19. doi: 10.1007/s00787-014-0559-2. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Intelligence Scale for Children, Fourth Edition: Administration and scoring manual. San Antonio, TX: Psychological Corporation; 2003. [Google Scholar]
- Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biological Psychiatry. 2005;57(11):1336–1346. doi: 10.1016/j.biopsych.2005.02.006. [DOI] [PubMed] [Google Scholar]


