Abstract
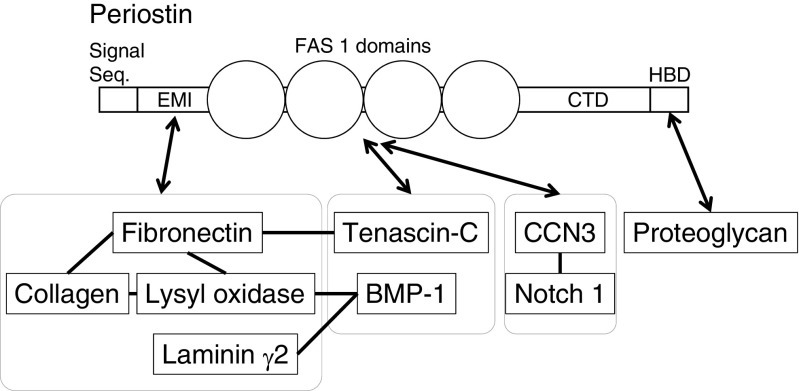
Periostin is a secretory protein with a multi-domain structure, comprising an amino-terminal cysteine-rich EMI domain, four internal FAS 1 domains, and a carboxyl-terminal hydrophilic domain. These adjacent domains bind to extracellular matrix proteins (type I collagen, fibronectin, tenascin-C, and laminin γ2), and BMP-1 that catalyzes crosslinking of type I collagen, and proteoglycans, which play a role in cell adhesion. The binding sites on periostin have been demonstrated to contribute to the mechanical strength of connective tissues, enhancing intermolecular interactions in close proximity and their assembly into extracellular matrix architectures, where periostin plays further essential roles in physiological maintenance and pathological progression. Furthermore, periostin also binds to Notch 1 and CCN3, which have functions in maintenance of stemness, thus opening up a new field of periostin action.
Keywords: Periostin, ECM, EMI, FAS 1, Fibronectin, Tenascin, Collagen, BMP-1, CCN3
Introduction
Periostin was originally identified as osteoblast-specific factor-2 (Osf-2) (Sugiura et al. 1995), with its roles being demonstrated as regulation of cell adhesion, cell differentiation, and organization of extracellular matrix. Periostin is a matricellular protein of 90 kDa, having a secretory signal peptide, followed by an amino-terminal cysteine-rich EMI domain, four internal FAS 1 domains, and a carboxyl-terminal domain (CTD) (Horiuchi et al. 1999; Kudo 2011; Sugiura et al. 1995) the sequence of which varies as a result of alternative splicing (Horiuchi et al. 1999; Hoersch and Andrade-Navarro 2010). Periostin has been demonstrated to behave as a scaffold for assembly of extracellular matrix proteins (type I collagen, fibronectin, tenascin-C, and laminin γ2) and accessory proteins (BMP-1 and CCN3), underlying sophisticated extracellular matrix architectures (Elliott and Hamilton 2011; Kii et al. 2010; Maruhashi et al. 2010; Snider et al. 2008). This scaffold function is made possible by the multi-domain structure of periostin, thereby enabling interacting proteins in close proximity to assemble into a large interacting complex. The contribution of periostin to the mechanical strength of tissues is due to the adjacent domains of periostin that interact with the different extracellular and accessory proteins, which function to maintain pathophysiological conditions.
The localization of periostin in mouse and human tissues has been examined by employing antibodies against the periostin domains (Horiuchi et al. 1999; Shimazaki et al. 2008), demonstrating that periostin physiologically localizes at collagen-rich regions in connective tissues such as the periodontal ligament (Horiuchi et al. 1999; Kii et al. 2006; Rios et al. 2005; Suzuki et al. 2004), periosteum (Horiuchi et al. 1999; Rios et al. 2005), cardiac valve (Hakuno et al. 2010; Norris et al. 2009a, b), and lung (Bozyk et al. 2012; Kondoh et al. 2016; Okamoto et al. 2011). Pathologically, periostin has also been localized in infarcted myocardium (Shimazaki et al. 2008; Oka et al. 2007), fibrosis (Okamoto et al. 2011; Ishikawa et al. 2014; Naik et al. 2012; Takayama et al. 2006; Uchida et al. 2012), tissues undergoing wound healing (Nishiyama et al. 2011; Norris et al. 2007; Ontsuka et al. 2012; Zhou et al. 2010), and cancer-associated stroma (Fukushima et al. 2008; Kashima et al. 2009; Kikuchi et al. 2008, 2014; Liu et al. 2014; Nitsche et al. 2016; Oskarsson and Massague 2012; Qin et al. 2016; Ruan et al. 2009; Sung et al. 2016; Tian et al. 2015; Underwood et al. 2015; Wang and Ouyang 2012). Taken together, periostin expression is well correlated with tissue regeneration (Conway et al. 2014).
Periostin interacts with extracellular matrix proteins
The EMI domain of periostin interacts with fibronectin as shown in Fig. 1. Periostin directly binds to fibronectin (Kii et al. 2010; Norris et al. 2007). A proximal localization between periostin and fibronectin was observed in the endoplasmic reticulum of fibroblastic cells (Kii et al. 2016), implying that periostin interacts with fibronectin before its secretion. Furthermore, periostin enhances secretion of fibronectin from the endoplasmic reticulum to the extracellular milieu (Kii et al. 2016), indicating an important role of periostin in fibronectin secretion. Periostin was detected in the Golgi apparatus and the endoplasmic reticulum in fibroblastic cells, suggesting a role in the protein secretory pathway (Kii et al. 2010, 2016; Kim et al. 2009). The mechanism of alternative splicing is essential for the regulation of periostin secretion followed by localization at ECMs as a determinant of differentiation (Horiuchi et al. 1999; Hoersch and Andrade-Navarro 2010). Similarly, splice variants of fibronectin containing either EDA or EDB domains can augment osteoblast differentiation or enhance mineralization by induced differentiation of osteoblasts, respectively (Sens et al. 2016). In periostin, the alternatively spliced region in the CTD has not been demonstrated as a target of any protein in biological analyses; thus its molecular function is not well understood.
Fig. 1.
Periostin interacts with multiple extracellular proteins. The interactions of periostin with the extracellular/secretory proteins are depicted based on the multi-domain structure of periostin. CTD; carboxyl-terminal domain, HBD: heparin-binding domain
Periostin also interacts with collagens, which is in good agreement with its localization on collagen fibrils (Kii et al. 2006; Suzuki et al. 2004; Norris et al. 2007). Periostin was found to form a complex with collagen type I (Norris et al. 2007), and directly binds to collagen type V (Takayama et al. 2006), although the binding site for collagens has not been identified, marking the need for further studies on this interaction. Fibronectin has several interaction sites for collagens, suggesting that the EMI domain of periostin may indirectly interact with collagens. As a consequence of its interaction with fibronectin, which is a crucial factor for collagen fibrillogenesis (Kadler et al. 2008), periostin plays an important role in collagen fibrillogenesis (Norris et al. 2007).
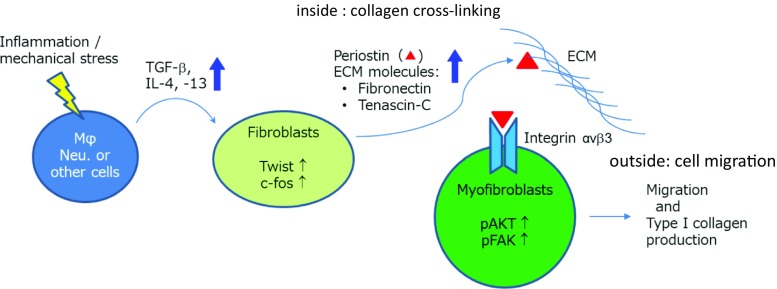
Collagen fibrillogenesis is a complicated multi-step process that is poorly understood (Canty and Kadler 2005). Molecular level studies on the interaction of periostin with collagen and fibronectin, both inside and outside cells, would contribute to elucidating the mechanism of collagen fibrillogenesis as shown in Fig. 2. At the first event of periostin regulation, the expression of TGFβ and/or IL-4 and IL-13 is induced in inflammation or mechanical stress. These cytokines trigger the expression of periostin and its splice variants together with primarily splice variants of fibronectin and tenascin-C. The splice variant of periostin is secreted and localized outside of the cell in the ECM, where it interacts with integrin αvβ3 on fibroblastic cells to induce their cell migration through downstream Akt and FAK phosphorylation. These fibroblastic cells produce type I collagen to repair tissues.
Fig. 2.
Periostin function at the inside or outside of cells. Inflammation or mechanical stress induces the expression of TGFβ and/or IL-4 and IL-13 in macrophages and neutrophils for inflammation or in other types of cells for mechanical stress. These cytokines induce the expression of periostin and other ECM molecules such as fibronectin and tenascin-C in fibroblasts, which proteins are mainly splice variants. The splice variant of periostin is secreted and localized outside the cell in the ECM, where it interacts with integrin αvβ3 on myofibroblasts to induce their cell migration through downstream signals of Akt and FAK phosphorylation. These myofibroblasts produce type I collagen to repair tissues. In this collagen production, periostin together with tenascin-C inside the cell forms a meshwork structure with fibronectin to constitute a scaffold for the cross-linking of type I collagen. This cross-linking is activated by periostin in association with BMP-1 to generate the active lysyl oxidase (LOX) for enhancement of cross-linking inside the cells
Periostin binds to tenascin, BMP-1, and CCN3
The FAS 1 domains of periostin bind to tenascin-C (Kii et al. 2010). Tenascin-C is an extracellular matrix protein, forming a hexamer by disulfide bond in the amino-terminal region. This disulfide-bonded multimerization results in a six-armed oligomer, accordingly termed a hexabrachion (Midwood et al. 2016). Immunoprecipitation experiments revealed the interaction of the FAS 1 domains with tenascin-C (Kii et al. 2010). Purified FAS 1 domains directly bind to tenascin-C. Notably, cleavage of the CTD of periostin is required for the interaction between the FAS 1 domains and tenascin-C (Kii et al. 2010). The CTD of periostin may be processed in the Golgi apparatus (Kii et al. 2010). Although this auto-inhibitory mechanism has not been understood, the intra-molecular interaction in periostin has been indicated (Takayama et al. 2006, 2009). Recombinant protein studies showed that CTD of periostin directly binds to the four FAS 1 domains (Takayama et al. 2009), suggesting that this intra-molecular interaction in periostin inhibits the interaction between the FAS 1 domains and tenascin-C.
The four FAS 1 domains interact with bone morphogenetic protein-1 (BMP-1). BMP-1 is a pro-collagen processing enzyme that removes the carboxyl-terminal propeptides (Vadon-Le Goff et al. 2015). Immunoprecipitation experiments have shown that the four FAS 1 domains interact with BMP-1 (Maruhashi et al. 2010). Moreover, in silico structural analysis indicated possible direct binding between the FAS 1 domains and BMP-1 (Hwang et al. 2014). This interaction enhances proteolytic activation of lysyl oxidase (LOX), which is associated with the EMI domain of periostin via fibronectin (Maruhashi et al. 2010; Garnero 2012). LOX is an enzyme that catalyzes intermolecular crosslinking between collagen molecules (Trackman 2016), which is crucial for collagen fibrillogenesis. Similarly, knockout of the periostin gene in mice caused reduction of cross-linking in collagens (Kii et al. 2010; Shimazaki et al. 2008; Norris et al. 2007). Taken together, the formation of the periostin-BMP-1-LOX complex may underlie the mechanical property of collagen fibers. Interestingly, the same FAS 1 domain (the first or third FAS 1 domain) of periostin can bind to BMP-1 and BMP-2, though the binding affinity for BMP-2 is lower (Hwang et al. 2014), suggesting a possible mechanism of binding switch due to the developmental stage.
The four FAS 1 domains have been demonstrated to interact with CCN3 (Takayama et al. 2017). CCN3 is composed of four domains: the insulin-like growth factor-binding protein-like domain (IGFBP), the von Willebrand type C-like domain (VWC), the thrombospondin type 1-like domain (TSP1), and the carboxyl-terminal domain (CT). The four FAS 1 domains interact with TSP1 and CT of CCN3 (Takayama et al. 2017). The role of periostin has been elucidated as an enhancer for the deposition of CCN3 on the extracellular matrix (Takayama et al. 2017). Similar to tenascin-C, BMP-1 and CCN3, periostin may function as the anchor for these proteins to the extracellular matrix.
The CTD of periostin was shown to inhibit the interaction of the FAS 1 domains with tenascin-C, and this interaction requires the cleavage of the CTD (Kii et al. 2010). This cleavage mechanism underlies the regulation of the interaction between periostin and tenascin-C. Identification of the enzymes that catalyze the CTD cleavage would shed light on the periostin-specific regulatory mechanism for construction of the extracellular architecture.
Periostin paralogue, TGFBI (βig-h3)
The interaction between periostin and the periostin paralogue, TGFBI (βig-h3) likely results from hetero-multimerization via their EMI domains (Kim et al. 2009). This interaction was found to be essential for the proper secretion of a periostin/βig-h3 hetero-multimer. Furthermore, it has been demonstrated that βig-h3 directly binds to collagens type I, II and IV (Hashimoto et al. 1997), and localizes to the Golgi apparatus like periostin (Kim et al. 2009). These similarities in both proteins suggest the molecular function of these matricellular proteins as a modulator.
Periostin and βig-h3 generally have different expression patterns. However, in bone cells, periostin and βig-h3 are expressed in both osteoblasts and osteoclasts in vitro (Merie et al. 2014), suggesting that both genes possibly act co-operatively in bone formation. By contrast, after myocardial infarction, deletion of βig-h3 did not alter cardiac disease, in contrast to periostin-deficient mice, indicating a distinct action of βig-h3 (Schwanekamp et al. 2017). In addition, βig-h3 lacks an extended region equivalent to the CTD, suggesting that the CTD is of functional relevance and could modulate periostin function.
Periostin function in stemness
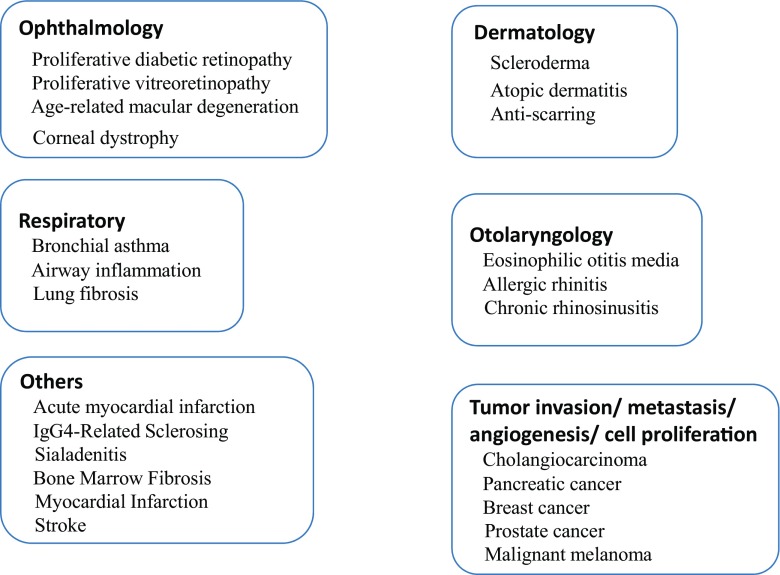
Periostin is regarded as a critical molecule that plays a progressive role in severe diseases, such as fibrosis in asthma, scar formation in infarcted myocardium, and tumorigenesis (Conway et al. 2014), as summarized in Fig. 3. Interestingly, there are several recent reports of periostin function in stem cells. Periostin has been shown to maintain hematopoietic stem cells (HSC) in a quiescent state through its interaction with integrin-αv of HSC in the bone marrow niche (Khurana et al. 2016); and another recent report showed that periostin secreted from stromal fibroblastic cells supports not only normal hematopoietic precursor cells but also leukemia-initiating cells (Tanaka et al. 2016). It has also been reported that periostin associates with a matricellular protein, CCN3 (also termed NOV), and that a functional relationship was observed in the periodontal ligament (Djokic et al. 2013). In this regard, CCN3 acts as a regulator of human HSC or hematopoietic progenitor cells as demonstrated by the loss of CCN3, which diminishes the functional capacity of the primitive hematopoietic compartment (Horiguchi et al. 2009). In mice, CCN3 plays a role in the HSC maintenance (Ishihara et al. 2014), suggesting a cooperative function of periostin together with CCN3 for HSC maintenance. In addition, the Notch signaling pathway is involved in HSC maintenance, and periostin-Notch1 and periostin-CCN3 interactions indicate a possible contribution of the functional complex of these three molecules, periostin-CCN3-Notch1, in HSC stemness. Periostin is secreted from mesenchymal stem cells to support tendon formation (Noack et al. 2014), characterized by the overexpression of periostin. Taken together, it can be speculated that periostin-CCN3 has become functional inside the bone after landing of animals (Gupta et al. 2007), initiating the building of the bone marrow microenvironment that supports hematopoietic stem cells by maintaining the hematopoietic compartment.
Fig. 3.
Periostin and related diseases
Periostin in mechanical stress
From expression profiling of periostin in periosteum and periodontal ligament, periostin has been expected to be mechanical stress-sensitive (Horiuchi et al. 1999), since the periosteum on the bone and the periodontal ligament in teeth are very sensitive to mechanical stress in order to aid tissue regeneration and development; however, no direct evidence of stress sensitivity has been reported. Interestingly, cathepsin K controls cortical bone formation by degrading periostin (Bonnet et al. 2017), since osteocytes expressing cathepsin K play a central role in the regulation of the biomechanical response in bone tissues, and degradation of periostin by cathepsin K occurs in osteocytes. Hence, cortical bone formation is regulated by the periostin-mediated blocking of random bone formation. Since peiostin is now known as an essential marker of periodontal ligament, the knowledge of which has helped to develop researches on periodontal ligament, and has clinical applications for periodontal diseases. A recent study demonstrated that periostin maintains stemness of periodontal ligament mesenchymal stem cells, and then promotes them into osteogenic differentiation through the JNK pathway under inflammatory conditions (Tang et al. 2017).
A functional link between the signaling cascades in mechanical stress and periostin gene expression was reported; it was found that both periostin and mammalian target of rapamycin (mTOR) are coordinately up-regulated by mechanical stress during the wound healing process to induce cell migration and proliferation (Rosselli-Murai et al. 2013), suggesting that the same signal originating from mechanical stress enhances both periostin and mTOR expression, after which periostin activates mTOR signals probably via integrin. Coincidently, the activated mTOR signaling pathway promotes osteoclast formation for bone remodeling (Dai et al. 2017), which reasonably suggests that periostin plays a role in the maintenance of bone mass (Kii et al. 2010). One of the candidate signals linking the mTOR and periostin activation is neuronal nitric oxide synthase (nNOS). In overload-induced skeletal muscle hypertrophy in mice, nNOS is transiently activated in a very short period after overloading, which activates the transient receptor potential cation channel, subfamily V member 1 (TRPV1), resulting in increased intracellular Ca2+ concentration that subsequently triggers mTOR activation (Ito et al. 2013).
DDR1 (Discoidin domain receptor 1) is a receptor tyrosine kinase that shows similar functions to periostin physiologically, and is pathologically specific to chronic kidney disease (CKD). Notch 1 is an interacting partner of DDR1, while type I collagen is a ligand of DDR1, indicating that activation of DDR1 receptor kinase through type I collagen binding induces Notch 1 signaling to promote cell survival (Kim et al. 2011). This activity is highly similar to periostin function (Tanabe et al. 2010) and probably involves CCN3 (Takayama et al. 2017). Further analyses of the synergy functioning between DDR1 and periostin would be very important to understand apoptosis induced by mechanical stress. In CKD, both periostin and DDR1 are involved in the regulation of inflammation and fibrosis. Thus, both proteins are novel biomarkers and therapeutic targets in CKD (Prakoura and Chatziantoniou 2017).
Clinical trials on periostin
Due to the increase in the number for periostin-related diseases (Fig. 3), some clinical trials have already underway. The first trial for clinical application of periostin demonstrated that gelform disks loaded with a recombinant periostin introduced into the pericardial cavity of pigs lead to increased cardiomyocyte cell cycle activity and angiogenesis (Polizzotti et al. 2012). Thereafter, inhibition of periostin action has been getting popular as clinical trials, because excessive activity of periostin induces severe fibrosis, generating deficiency of organ function. In this concept, a new RNAi agent had a pronounced inhibitory effect on lung fibrosis (Tomaru et al. 2017), choroidal neovascularization and choroidal fibrosis (Nakama et al. 2015) as well as retinal neovascularization (Nakama et al. 2017) and adhesion formation of abraded cecum after surgery (Takai et al. 2017). Similarly, intraperitoneal administration of the periostin-binding DNA aptamer significantly abrogated peritoneal fibrosis (Nam et al. 2017). In a new therapeutic method, overexpression of miR-599, which down-regulates periostin, inhibited glioma cell migration and invasion (Zhang et al. 2017).
In diagnostic applications, periostin is a useful marker of severe bronchial asthma. In patients with asthma, the high-Th2 phenotype has been associated with a high level of circulating periostin, which is induced by interleukin-13 (IL-13) and expressed by airway structural cells, and was detected by anti-periostin antibodies (Kraft 2011). The effect of anti-IL-13 antibody-based drug, termed lebrikizumab, on asthma was reported (Corren et al. 2011). Although there was a beneficial effect on airflow obstruction in all the patients treated with lebrikizumab, the effect was greater in patients who had circulating levels of periostin, indicating that periostin is a good biomarker for determining candidates for lebrikizumab treatment (Zhu et al. 2017). With regards to mechanical stress, under microgravity, periostin can be utilized as a marker of periosteal metabolism because of the fact that periostin concentration in serum increased transiently along with 15% increase in cortical porosity, which indicates that periostin is a good marker of cortical porosity (Vico et al. 2017).
Acknowledgements
We thank K. Yoshikawa in Aqua Therapeutics Co. for providing information. This work was supported by the Project for Cancer Research and Therapeutic Evolution (P-CREATE) (IK) from the Japan Agency for Medical Research and Development (AMED).
Contributor Information
Akira Kudo, Phone: +81-3-5734-3190, Email: akudo@bio.titech.ac.jp.
Isao Kii, Phone: +81-78-304-7162, Email: isao.kii@riken.jp.
References
- Bonnet N, Brun J, Rousseau J-C, Duong LT, Ferrari SL. Cathepsin K controls cortical bone formation by degrading periostin. J Bone Miner Res. 2017;7:1432–1441. doi: 10.1002/jbmr.3136. [DOI] [PubMed] [Google Scholar]
- Bozyk PD, Bentley JK, Popova AP, Anyanwu AC, Linn MD, Goldsmith AM, Pryhuber GS, Moore BB, Hershenson MB. Neonatal periostin knockout mice are protected from hyperoxia-induced alveolar simplication. PLoS One. 2012;7:e31336. doi: 10.1371/journal.pone.0031336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canty EG, Kadler KE. Procollagen trafficking, processing and fibrillogenesis. J Cell Sci. 2005;118(Pt 7):1341–1353. doi: 10.1242/jcs.01731. [DOI] [PubMed] [Google Scholar]
- Conway SJ, Izuhara K, Kudo Y, Litvin J, Markwald R, Ouyang G, Arron JR, Holweg CT, Kudo A. The role of periostin in tissue remodeling across health and disease. Cell Mol Life Sci. 2014;71:1279–1288. doi: 10.1007/s00018-013-1494-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corren J, Lemanske RF, Hanania NA, Korenblat PE, Parsey MV, Arron JR, et al. Lebrikizumab treatment in adults with asthma. N Engl J Med. 2011;365:1088–1098. doi: 10.1056/NEJMoa1106469. [DOI] [PubMed] [Google Scholar]
- Dai Q, Xie F, Han Y, Ma X, Zhou S, Jiang L, Zou W, Wang J. Inactivation of regulatory-associated protein of mTOR (Raptor)/mammalian target of rapamycin complex 1 (mTORC1) signaling in osteoclasts increases bone mass by inhibiting osteoclast differentiation in mice. J Biol Chem. 2017;292:196–204. doi: 10.1074/jbc.M116.764761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djokic J, Fagotto-Kaufmann C, Bartels R, Nelea V, Reinhardt DP. Fiblin-3,-4, and-5 are highly susceptible to proteolysis, interact with cells and heparin, and form multimers. J Biol Chem. 2013;288:22821–22835. doi: 10.1074/jbc.M112.439158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott CG, Hamilton DW. Deconstructing fibrosis research: do pro-fibrotic signals point the way for chronic dermal wound regeneration? J Cell Commun Signal. 2011;5:301–315. doi: 10.1007/s12079-011-0131-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukushima N, Kikuchi Y, Nishiyama T, Kudo A, Fukayama M. Periostin deposition in the stroma of invasive and intraductal neoplasms of the pancreas. Mod Pathol. 2008;21:1044–1053. doi: 10.1038/modpathol.2008.77. [DOI] [PubMed] [Google Scholar]
- Garnero P. The contribution of collagen crosslinks to bone strength. Bonekey Rep. 2012;1:182. doi: 10.1038/bonekey.2012.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta R, Hong D, Iborra F, Sarno S, Enver T. NOV (CCN3) functions as regulator of human hematopietic stem of progenitor cells. Science. 2007;316:590–593. doi: 10.1126/science.1136031. [DOI] [PubMed] [Google Scholar]
- Hakuno D, Kimura N, Yoshioka M, Mukai M, Kimura T, Okada Y, Yozu R, Shukunami C, Hiraki Y, Kudo A, Ogawa S, Fukuda K. Periostin advances atherosclerotic and rheumatic cardiac valve degeneration by inducing angiogenesis and MMP production in humans and rodents. J Clin Invest. 2010;120:2292–2306. doi: 10.1172/JCI40973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashimoto K, Noshiro M, Ohno S, Kawamoto T, Satakeda H, Akagawa Y, Nakashima K, Okimura A, Ishida H, Okamoto T, Pan H, Shen M, Yan W, Kato Y. Characterization of a cartilage-derived 66-kDa protein (RGD-CAP/beta ig-h3) that binds to collagen. Biochim Biophys Acta. 1997;1355:303–314. doi: 10.1016/S0167-4889(96)00147-4. [DOI] [PubMed] [Google Scholar]
- Hoersch S, Andrade-Navarro MA. Periostin shows increased evolutionary plasticity in its alternatively spliced region. BMC Evol Biol. 2010;10:30. doi: 10.1186/1471-2148-10-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horiguchi M, Inoue T, Ohbayashi T, Hirai M, Noda K, Marmorstein LY, Yabe D, Takagi K, Akama TO. Kita T, Kimura T, Nakamura T. Fibulin-4 conducts proper elastogenesis via interaction with cross-linking enzyme lysyl oxidase. Proc Natl Acad Sci U S A. 2009;45:19029–19034. doi: 10.1073/pnas.0908268106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horiuchi K, Amizuka N, Takeshita S, Takamatsu H, Katsuura M, Ozawa H, Toyama Y, Bonewald LF, Kudo A. Identification and characterization of a novel protein, periostin, with restricted expression to periosteum and periodontal ligament and increased expression by transforming growth factor beta. J Bone Miner Res. 1999;14:1239–1249. doi: 10.1359/jbmr.1999.14.7.1239. [DOI] [PubMed] [Google Scholar]
- Hwang EY, Jeong MS, Park EK, Kim JH, Jang SB. Structural characterization and interaction of periostin and bone morphogenetic protein for regulation of collagen cross-linking. Biochem Biophys Res Commun. 2014;449:425–431. doi: 10.1016/j.bbrc.2014.05.055. [DOI] [PubMed] [Google Scholar]
- Ishihara J, Umemoto T, Yamato M, Shiratsuchi Y, Takaki S, Petrich BG, Nakauchi H, Eto K, Kitamura T, Okano T. Nov/CCN3 regulates long-term repopulating activity of murine hematopoietic stem cells via integrin avb3. Int J Hematol. 2014;99:393–406. doi: 10.1007/s12185-014-1534-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishikawa K, Yoshida S, Nakao S, Nakama T, Kita T, Asato R, Sassa Y, Arita R, Miyazaki M, Enaida H, Oshima Y, Murakami N, Niiro H, Ono J, Matsuda A, Goto Y, Akashi K, Izuhara K, Kudo A, Kono T, Hafezi-Moghadam A, Ishibashi T. Periostin promotes the generation of fibrous membranes in proliferative vitreoretinopathy. FASEB J. 2014;28:131–142. doi: 10.1096/fj.13-229740. [DOI] [PubMed] [Google Scholar]
- Ito N, Ruegg UT, Kudo A, Miyagoe-Suzuki Y, Takeda S. Activation of calcium signaling through Trpv1 by nNOS and peroxynitrite as a key trigger of skeletal muscle hypertrophy. Nat Med. 2013;19:101–106. doi: 10.1038/nm.3019. [DOI] [PubMed] [Google Scholar]
- Kadler KE, Hill A, Canty-Laird EG. Collagen fibrillogenesis: fibronectin, integrins, and minor collagens as organizers and nucleators. Curr Opin Cell Biol. 2008;20:495–501. doi: 10.1016/j.ceb.2008.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashima TG, Nishiyama T, Shimazu K, Shimazaki M, Kii I, Grigoriadis AE, Fukayama M, Kudo A. Periostin, a novel marker of intramembranous ossification, is expressed in fibrous dysplasia and in c-Fos-overexpressing bone lesions. Hum Pathol. 2009;40:226–237. doi: 10.1016/j.humpath.2008.07.008. [DOI] [PubMed] [Google Scholar]
- Khurana S, Schouteden S, Manesia JK, Sanamaria-Martinez A, Huelsken J, Lacy-Hulbert A, Verfaillie CM. Outside-in integrin signaling regulates haematopoietic stem cell function via Periostin-Itgav axis. Nat Commun. 2016;7:13500. doi: 10.1038/ncomms13500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kii I, Amizuka N, Minqi L, Kitajima S, Saga Y, Kudo A. Periostin is an extracellular matrix protein required for eruption of incisors in mice. Biochem Biophys Res Commun. 2006;342:766–772. doi: 10.1016/j.bbrc.2006.02.016. [DOI] [PubMed] [Google Scholar]
- Kii I, Nishiyama T, Li M, Matsumoto K, Saito M, Amizuka N, Kudo A. Incorporation of tenascin-C into the extracellular matrix by periostin underlies an extracellular meshwork architecture. J Biol Chem. 2010;285:2028–2039. doi: 10.1074/jbc.M109.051961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kii I, Nishiyama T, Kudo A. Periostin promotes secretion of fibronectin from the endoplasmic reticulum. Biochem Biophys Res Commun. 2016;470:888–893. doi: 10.1016/j.bbrc.2016.01.139. [DOI] [PubMed] [Google Scholar]
- Kikuchi Y, Kashima TG, Nishiyama T, Shimazu K, Morishita Y, Shimazaki M, Kii I, Horie H, Nagai H, Kudo A, Fukayama M. Periostin is expressed in pericryptal fibroblasts and cancer-associated fibroblasts in the colon. J Histochem Cytochem. 2008;56:753–764. doi: 10.1369/jhc.2008.951061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kikuchi Y, Kunita A, Iwata C, Komura D, Nishiyama T, Shimazu K, Takeshita K, Shibahara J, Kii I, Morishita Y, Yashiro M, Hirakawa K, Miyazono K, Kudo A, Fukayama M, Kashima TG. The niche component periostin is produced by cancer-associated fibroblasts, supporting growth of gastric cancer through ERK activation. Am J Pathol. 2014;184:859–870. doi: 10.1016/j.ajpath.2013.11.012. [DOI] [PubMed] [Google Scholar]
- Kim BY, Olzmann JA, Choi SI, Ahn SY, Kim TI, Cho HS, Suh H, Kim EK. Corneal dystrophy-associated R124H mutation disrupts TGFBI interaction with Periostin and causes mislocalization to the lysosome. J Biol Chem. 2009;284:19580–19591. doi: 10.1074/jbc.M109.013607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H-G, Hwang S-Y, Aaronson SA, Mandinova A, Lee SW. DDR1 receptor tyrosin kinase promotes prosurvival pathway through notch 1 activation. J Biol Chem. 2011;286:17672–17681. doi: 10.1074/jbc.M111.236612. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Kondoh H, Nishiyama T, Kikuchi Y, Fukayama M, Saito M, Kii I, Kudo A. Periostin deficiency causes severe and lethal lung injury in mice with bleomycin administration. J Histochem Cytochem. 2016;64:441–453. doi: 10.1369/0022155416652611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraft M. Asthma phenotypes and interleukin-13--moving closer to personalized medicine. N Engl J Med. 2011;365:1141–1144. doi: 10.1056/NEJMe1108666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kudo A. Periostin in fibrillogenesis for tissue regeneration: periostin actions inside and outside the cell. Cell Mol Life Sci. 2011;68:3201–3207. doi: 10.1007/s00018-011-0784-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu AY, Zheng H, Ouyang G. Periostin, a multifunctional matricellular protein in inflammatory and tumor microenvironments. Matrix Biol. 2014;37:150–156. doi: 10.1016/j.matbio.2014.04.007. [DOI] [PubMed] [Google Scholar]
- Maruhashi T, Kii I, Saito M, Kudo A. Interaction between periostin and BMP-1 promotes proteolytic activation of lysyl oxidase. J Biol Chem. 2010;285:13294–13303. doi: 10.1074/jbc.M109.088864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merie B, Bouet G, Rousseau J-C, Betholon C, Garnero P. Periostin and transforming growth factor β-induced protein (TGFβIp) are both expressed by osteoblasts and osteoclasts. Cell Biol Int. 2014;38:398–404. doi: 10.1002/cbin.10219. [DOI] [PubMed] [Google Scholar]
- Midwood KS, Chiquet M, Tucker RP, Orend G. Tenascin-C at a glance. J Cell Sci. 2016;129:4321–4327. doi: 10.1242/jcs.190546. [DOI] [PubMed] [Google Scholar]
- Naik PK, Bozyk PD, Bentley JK, Popova AP, Birch CM, Wilke CA, Fry CD, White ES, Sisson TH, Tayob N, Carnemolla B, Orecchia P, Flaherty KR, Hershenson MB, Murray S, Martinez FJ, Moore BB, Investigators C. Periostin promotes fibrosis and predicts progression in patients with idiopathic pulmonary fibrosis. Am J Physiol Lung Cell Mol Physiol. 2012;303:L1046–L1056. doi: 10.1152/ajplung.00139.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakama T, Yoshida S, Ishikawa K, Kobayashi Y, Zhou Y, Nakao S, Sassa Y, Oshima Y, Takao K, Shimahara A, Yoshikawa K, Hamasaki T, Ohgi T, Hayashi H, Matsuda A, Kudo A, Nozaki M, Ogura Y, Kuroda M, Ishibashi T. Gene Ther. 2015;22:127–137. doi: 10.1038/gt.2014.112. [DOI] [PubMed] [Google Scholar]
- Nakama T, Yoshida S, Ishikawa K, Kubo Y, Kobayashi Y, Zhou Y, Nakao S, Hisatomi T, Ikeda Y, Takao K, Yoshikawa K, Matsuda A, Ono J, Ohta S, Izuhara K, Kudo A, Sonoda K, Ishibashi T. Mol Ther-Nucleic Acids. 2017;6:279–289. doi: 10.1016/j.omtn.2017.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nam BY, Park JT, Kwon YE, Lee JP, Jung JH, Kim Y, Kim S, Park J, Um JE, Wu M, Han SH, Yoo T-H, Kang S-W (2017) Mol Ther Nucleic Acids. doi: 10.1016/j.omtn.2017.05.001 [DOI] [PMC free article] [PubMed]
- Nishiyama T, Kii I, Kashima TG, Kikuchi Y, Ohazama A, Shimazaki M, Fukayama M, Kudo A. Delayed re-epithelialization in periostin-deficient mice during cutaneous wound healing. PLoS One. 2011;6:e18410. doi: 10.1371/journal.pone.0018410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nitsche U, Stangel D, Pan Z, Schlitter AM, Esposito I, Regel I, Raulefs S, Friess H, Kleeff J, Erkan M. Periostin and tumor-stroma interactions in non-small cell lung cancer. Oncol Lett. 2016;12:3804–3810. doi: 10.3892/ol.2016.5132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noack S, Seiffart V, Willbold E, Laggies S, Winkel A, Shahab-Osterloh S, Florkemeier T, Hertwig F, Steinhoff C, Nuber UA, Gross G, Hoffmann A. Periostin secreted by mesenchymal stem cells supports tendon formation in an ectopic mouse model. Stem Cells Dev. 2014;23:1844–1857. doi: 10.1089/scd.2014.0124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris RA, Damon B, Mironov V, Kasyanov V, Ramamurthi A, Moreno-Rodriguez R, Trusk T, Potts JD, Goodwin RL, Davis J, Hoffman S, Wen X, Sugi Y, Kern CB, Mjaatvedt CH, Turner DK, Oka T, Conway SJ, Molkentin JD, Forgacs G, Markwald RR. Periostin regulates collagen fibrillogenesis and the biomechanical properties of connective tissues. J Cell Biochem. 2007;101:695–711. doi: 10.1002/jcb.21224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris RA, Moreno-Rodriguez R, Hoffman S, Markwald RR. The many facets of the matricelluar protein periostin during cardiac development, remodeling, and pathophysiology. J Cell Commun Signal. 2009;3:275–286. doi: 10.1007/s12079-009-0063-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris RA, Potts JD, Yost MJ, Junor L, Brooks T, Tan H, Hoffman S, Hart MM, Kern MJ, Damon B, Markwald RR, Goodwin RL. Periostin promotes a fibroblastic lineage pathway in atrioventricular valve progenitor cells. Dev Dyn. 2009;238:1052–1063. doi: 10.1002/dvdy.21933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oka T, Xu J, Kaiser RA, Melendez J, Hambleton M, Sargent MA, Lorts A, Brunskill EW, Dorn GW, 2nd, Conway SJ, Aronow BJ, Robbins J, Molkentin JD (2007) Genetic manipulation of periostin expression reveals a role in cardiac hypertrophy and ventricular remodeling. Circ Res 101: 313–321. doi:10.1161/CIRCRESAHA.107.149047 [DOI] [PMC free article] [PubMed]
- Okamoto M, Hoshino T, Kitasato Y, Sakazaki Y, Kawayama T, Fujimoto K, Ohshima K, Shiraishi H, Uchida M, Ono J, Ohta S, Kato S, Izuhara K, Aizawa H. Periostin, a matrix protein, is a novel biomarker for idiopathic interstitial pneumonias. Eur Respir J. 2011;37:1119–1127. doi: 10.1183/09031936.00059810. [DOI] [PubMed] [Google Scholar]
- Ontsuka K, Kotobuki Y, Shiraishi H, Serada S, Ohta S, Tanemura A, Yang L, Fujimoto M, Arima K, Suzuki S, Murota H, Toda S, Kudo A, Conway SJ, Narisawa Y, Katayama I, Izuhara K, Naka T. Periostin, a matricellular protein, accelerates cutaneous wound repair by activating dermal fibroblasts. Exp Dermatol. 2012;21:331–336. doi: 10.1111/j.1600-0625.2012.01454.x. [DOI] [PubMed] [Google Scholar]
- Oskarsson T, Massague J. Extracellular matrix players in metastatic niches. EMBO J. 2012;31:254–256. doi: 10.1038/emboj.2011.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polizzotti BD, Arab S, Kuhn B. Intrapericardial delivery of gelform enables the targeted delivery of periostin peptide after myocardial infarction by inducing fibrin clot formation. PLoS One. 2012;7:e36788. doi: 10.1371/journal.pone.0036788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prakoura N, Chatziantoniou C. Periostin and discoidin domain receptor 1: new biomarkers or targets for therapy of renal disease. Front Med. 2017;4:52. doi: 10.3389/fmed.2017.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin X, Yan M, Zhang J, Wang X, Shen Z, Lv Z, Li Z, Wei W, Chen W. TGFbeta3-mediated induction of Periostin facilitates head and neck cancer growth and is associated with metastasis. Sci Rep. 2016;6:20587. doi: 10.1038/srep20587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rios H, Koushik SV, Wang H, Wang J, Zhou HM, Lindsley A, Rogers R, Chen Z, Maeda M, Kruzynska-Frejtag A, Feng JQ, Conway SJ. Periostin null mice exhibit dwarfism, incisor enamel defects, and an early-onset periodontal disease-like phenotype. Mol Cell Biol. 2005;25:11131–11144. doi: 10.1128/MCB.25.24.11131-11144.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosselli-Murai LK, Almeida LO, Zagni C, Galindo-Moreno P, Padial-Molina M, Volk SL, Murai MJ, Rios HF, Squarize CH, Castilho RM. Periostin responds to mechanical stress and tension by activating the MTOR signaling pathway. PLoS One. 2013;8:e83580. doi: 10.1371/journal.pone.0083580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruan K, Bao S, Ouyang G. The multifaceted role of periostin in tumorigenesis. Cell Mol Life Sci. 2009;66:2219–2230. doi: 10.1007/s00018-009-0013-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwanekamp JA, Lorts A, Sargent MA, York AJ, Grimes KM, Fischesser DM, Gokey JJ, Whitsett JA, Conway SJ, Molkentin JD (2017) TGFB1 functiones similar to periostin but is uniquely dispensable during cardiac injury. PLoS One. 10.1371/journal.pone.0181945 [DOI] [PMC free article] [PubMed]
- Sens C, Huck K, Pettera S, Uebel S, Wabnitz G, Moser M, Nakchbandi IA. Fibronectin containing extradomain A or B enhance osteoblast differentiation via distinct integrins. J Biol Chem. 2016;292:7745–7760. doi: 10.1074/jbc.M116.739987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimazaki M, Nakamura K, Kii I, Kashima T, Amizuka N, Li M, Saito M, Fukuda K, Nishiyama T, Kitajima S, Saga Y, Fukayama M, Sata M, Kudo A. Periostin is essential for cardiac healing after acute myocardial infarction. J Exp Med. 2008;205:295–303. doi: 10.1084/jem.20071297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snider P, Hinton RB, Moreno-Rodriguez RA, Wang J, Rogers R, Lindsley A, Li F, Ingram DA, Menick D, Field L, Firulli AB, Molkentin JD, Markwald R, Conway SJ. Periostin is required for maturation and extracellular matrix stabilization of noncardiomyocyte lineages of the heart. Circ Res. 2008;102:752–760. doi: 10.1161/CIRCRESAHA.107.159517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugiura T, Takamatsu H, Kudo A, Amann E. Expression and characterization of murine osteoblast-specific factor 2 (OSF-2) in a baculovirus expression system. Protein Expr Purif. 1995;6:305–311. doi: 10.1006/prep.1995.1040. [DOI] [PubMed] [Google Scholar]
- Sung PL, Jan YH, Lin SC, Huang CC, Lin H, Wen KC, Chao KC, Lai CR, Wang PH, Chuang CM, HH W, Twu NF, Yen MS, Hsiao M, Huang CY. Periostin in tumor microenvironment is associated with poor prognosis and platinum resistance in epithelial ovarian carcinoma. Oncotarget. 2016;7:4036–4047. doi: 10.18632/oncotarget.6700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki H, Amizuka N, Kii I, Kawano Y, Nozawa-Inoue K, Suzuki A, Yoshie H, Kudo A, Maeda T. Immunohistochemical localization of periostin in tooth and its surrounding tissues in mouse mandibles during development. Anat Rec A Discov Mol Cell Evol Biol. 2004;281:1264–1275. doi: 10.1002/ar.a.20080. [DOI] [PubMed] [Google Scholar]
- Takai S, Yoshino M, Takao K, Yoshikawa K, Jin D. Periostin antisense oligonucleotide prevents adhesion formation after surgery in mice. J Pharmacol Sci. 2017;133:65–69. doi: 10.1016/j.jphs.2016.10.009. [DOI] [PubMed] [Google Scholar]
- Takayama G, Arima K, Kanaji T, Toda S, Tanaka H, Shoji S, McKenzie AN, Nagai H, Hotokebuchi T, Izuhara K. Periostin: a novel component of subepithelial fibrosis of bronchial asthma downstream of IL-4 and IL-13 signals. J Allergy Clin Immunol. 2006;118:98–104. doi: 10.1016/j.jaci.2006.02.046. [DOI] [PubMed] [Google Scholar]
- Takayama I, Kii I, Kudo A. Expression, purification and characterization of soluble recombinant periostin protein produced by Escherichia coli. J Biochem. 2009;146:713–723. doi: 10.1093/jb/mvp117. [DOI] [PubMed] [Google Scholar]
- Takayama I, Tanabe H, Nishiyama T, Ito H, Amizuka N, Li M, Katsube KI, Kii I, Kudo A. Periostin is required for matricellular localization of CCN3 in periodontal ligament of mice. J Cell Commun Signal. 2017;11:5–13. doi: 10.1007/s12079-016-0371-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanabe H, Takayama I, Nishiyama T, Shimazaki M, Kii I, Li M, Amizuka N, Katsube K, Kudo A. Periostin associates with Notch 1 precursor to maintain Notch 1 expression under a stress condition in mouse cells. PLoS One. 2010;5:e12234. doi: 10.1371/journal.pone.0012234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka S, Maekawa A, Matsubara L, Imanishi A, Yano M, Roeder RG, Hasegawa N, Asano S, Ito M. Periostin supports hematopoietic progenitor cells and niche-dependent myeloblastoma cells in vitro. Biochem Biophys Res Commun. 2016;478:1706–1712. doi: 10.1016/j.bbrc.2016.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang Y, Liu L, Wang P, Chen D, Wu Z, Tang C. Periostin promotes migration and osteogenic differentiation of human periodontal ligament mesenchymal stem cells via the Jun amino-terminal kinases (JNK) pathway under inflammatory conditions. Cell Prolif. 2017;2017:e12369. doi: 10.1111/cpr.12369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian Y, Choi CH, Li QK, Rahmatpanah FB, Chen X, Kim SR, Veltri R, Chia D, Zhang Z, Mercola D, Zhang H. Overexpression of periostin in stroma positively associated with aggressive prostate cancer. PLoS One. 2015;10:e0121502. doi: 10.1371/journal.pone.0121502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomaru A, Kobayashi T, Hinneh JA, Tonto PB, D’Alessandro-Gabazza CN, Fujimoto H, Fujiwara K, Takahashi Y, Ohnishi M, Yasuma T, Nishihama K, Yoshino M, Takao K, Toda M, Totoki T, Takei Y, Yoshikawa K, Taguchi O, Gabazza EC (2017) Oligonucleotides targeting periostin ameliorates pulmonary fibrosis. Gene Ther. 10.1038/gt.2017.80 [DOI] [PubMed]
- Trackman PC. Enzymatic and non-enzymatic functions of the lysyl oxidase family in bone. Matrix Biol. 2016;52-54:7–18. doi: 10.1016/j.matbio.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchida M, Shiraishi H, Ohta S, Arima K, Taniguchi K, Suzuki S, Okamoto M, Ahlfeld SK, Ohshima K, Kato S, Toda S, Sagara H, Aizawa H, Hoshino T, Conway SJ, Hayashi S, Izuhara K. Periostin, a matricellular protein, plays a role in the induction of chemokines in pulmonary fibrosis. Am J Respir Cell Mol Biol. 2012;46:677–686. doi: 10.1165/rcmb.2011-0115OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Underwood TJ, Hayden AL, Derouet M, Garcia E, Noble F, White MJ, Thirdborough S, Mead A, Clemons N, Mellone M, Uzoho C, Primrose JN, Blaydes JP, Thomas GJ. Cancer-associated fibroblasts predict poor outcome and promote periostin-dependent invasion in oesophageal adenocarcinoma. J Pathol. 2015;235:466–477. doi: 10.1002/path.4467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vadon-Le Goff S, Hulmes DJ, Moali C. BMP-1/tolloid-like proteinases synchronize matrix assembly with growth factor activation to promote morphogenesis and tissue remodeling. Matrix Biol. 2015;44-46:14–23. doi: 10.1016/j.matbio.2015.02.006. [DOI] [PubMed] [Google Scholar]
- Vico L, Rietbergen BV, Vilayphiou N, Linossier M-T, Locrelle H, Normand M, Zouch M, Gerbaix M, Bonnet N, Novikov V, Thomas T, Vassilieva G (2017) Cortical and trabecular bone microstructure did not recover at weight-bearing skeletal sites and progressively deteriorated at non-weight-bearing sites during the year following International Space Station missions. J Bone Miner Res. 10.1002/jbmr.3188 [DOI] [PubMed]
- Wang Z, Ouyang G. Periostin: a bridge between cancer stem cells and their metastatic niche. Cell Stem Cell. 2012;10:111–112. doi: 10.1016/j.stem.2012.01.002. [DOI] [PubMed] [Google Scholar]
- Zhang T, Ma G, Zhang Y, Huo H, Zhao Y (2017) miR-599 inhibits proliferation and invasion of glioma by targeting periostin. Biotechnol Lett. 10.1007/s10529-017-2365-7 [DOI] [PubMed]
- Zhou HM, Wang J, Elliott C, Wen W, Hamilton DW, Conway SJ. Spatiotemporal expression of periostin during skin development and incisional wound healing: lessons for human fibrotic scar formation. J Cell Commun Signal. 2010;4:99–107. doi: 10.1007/s12079-010-0090-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu R, Zheng Y, Dirks NL, Vadhavkar S, Jin JY, Peng K, Holweg CTJ, Olsson J, Matthews JG, Putnam WS (2017) Model-based clinical pharmacological profiling and exposure-response relationships of the efficacy and biomarker of lebrikizumab in patients with moderate-to-serve asthma. Pulm Pharmacol Ther. 10.1016/j.pupt.2017.08.010 [DOI] [PubMed]